Abstract
Three simple approaches to forecast the COVID-19 epidemic in Jordan were previously proposed by Hussein, et al.: a short-term forecast (STF) based on a linear forecast model with a learning database on the reported cases in the previous 5–40 days, a long-term forecast (LTF) based on a mathematical formula that describes the COVID-19 pandemic situation, and a hybrid forecast (HF), which merges the STF and the LTF models. With the emergence of the OMICRON variant, the LTF failed to forecast the pandemic due to vital reasons related to the infection rate and the speed of the OMICRON variant, which is faster than the previous variants. However, the STF remained suitable for the sudden changes in epi curves because these simple models learn for the previous data of reported cases. In this study, we revisited these models by introducing a simple modification for the LTF and the HF model in order to better forecast the COVID-19 pandemic by considering the OMICRON variant. As another approach, we also tested a time-delay neural network (TDNN) to model the dataset. Interestingly, the new modification was to reuse the same function previously used in the LTF model after changing some parameters related to shift and time-lag. Surprisingly, the mathematical function type was still valid, suggesting this is the best one to be used for such pandemic situations of the same virus family. The TDNN was data-driven, and it was robust and successful in capturing the sudden change in +qPCR cases before and after of emergence of the OMICRON variant.
Keywords: linear forecast, short/long-term forecast, hybrid forecast (HF), herd immunity
1. Introduction
After the outbreak of the severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), which was by the end of year 2019, many models have been developed to forecast/predict the Coronavirus Disease (COVID-19) epidemic temporal variation. Some of these models were based on Artificial Intelligence (AI) and Machine Learning (ML) or to some extent based on a simple mathematical model [1,2,3]. Modelling is an effective tool in studying the qualitative properties and dynamical behaviors of different diseases [4,5,6], and especially in improving the prognostic processes of COVID-19. Nevertheless, these models have several limitations, including reporting quality, understanding of factors related to social and clinical measures, slow development of spatial risk maps, and vaccination strategies [7,8,9,10,11,12,13]. Ultimately, some of these predictive models were utilized for limiting the spread of COVID-19 in an intervention of optimized strategies [14,15,16,17,18,19]. They can also be useful in developing public health measures to contain the spread of the virus.
There have been several attempts at modeling the COVID-19 pandemic outbreak in Jordan during the early stage of the COVID-19 pandemic outbreak [20,21,22,23]. However, they were limited to the lockdown period and did not span a long enough time to cover the alternating waves of outbreaks, making them outdated to handle the complete picture of the COVID-19 epidemic over a long-term period. Besides this, they did not include vaccination scenarios on limiting the COVID-19 infection rates. As one of the disadvantages, these models were complicated and difficult to be interpreted. Recently, Hussein, et al. [1] proposed three simple approaches to forecast the COVID-19 epidemic in Jordan; see also Section S1 in Supplementary Materials:
Short-term forecast (STF) model;
Long-term forecast (LTF) model;
Hybrid forecast (HF) model.
As will be illustrated in the next section, the STF and the HF suggest approaches fairly predicting the COVID-19 pandemic curve in Jordan. The LTF approach deviated from the real epi curve, and this might be explained when taking into account herd immunity and the vaccination trend in Jordan. However, with the emergence of the OMICRON variant, the LTF totally failed to forecast the COVID-19 pandemic due to a vital reason related to infection rate and the speed of the OMICRON variant, which is faster than the previous variants. However, the STF remained capable of predicting the sudden changes in the epi curve, because these simple models learn from the previous data of reported cases. This required a revisit for the suggested approaches to include the emergence of the OMICRON variation in Jordan.
In this study, we aim at introducing a simple modification for the LTF and the HF models, which were previously published by Hussein, et al. [1], in order to better forecast the COVID-19 pandemic by considering the OMICRON variant. A time-delay neural network (TDNN) to model the data of the +qPCR cases before and after of emergence of the OMICRON variant is also proposed.
2. Materials and Methods
2.1. Reported COVID-19 Pandemic Data in Jordan
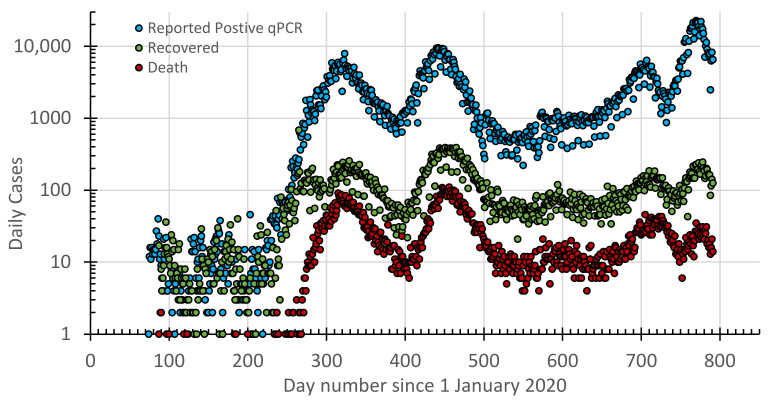
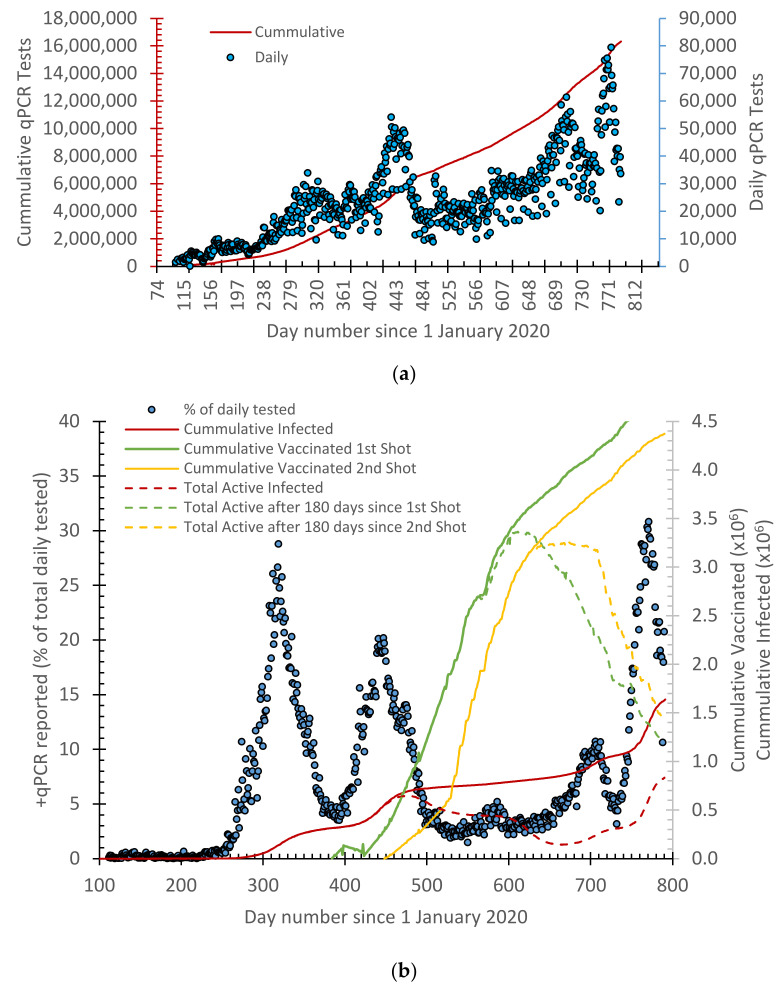
A COVID-19 database was cumulated from daily official reports by the Ministry of Health in Jordan. This included the daily reported positive cases of the qPCR tests, recovered cases, deaths, and vaccination shots (Figure 1 and Figure 2).
Figure 1.
Timelines for the reported daily cases of +qPCR tests, those recovered, and deaths since 14 March 2020 in Jordan.
Figure 2.
(a) qPCR tests performed in Jordan since 14 March 2020 and (b) percentage +qPCR cases overlayed with cumulative curves for the vaccination (first and second shots), as well as active cases representing herd immunity.
2.2. A Modified Model to Describe the OMICRON Variant
In order to include the OMICRON outbreak, we followed a similar approach in defining a LTF model as the one in Equation (S2) (Section S1 in Supplementary Materials) with the parameters A, a, b, δ, and c defined as 185, −0.003, 9.01, 1080, and 0.07, respectively. This is described by Hussein, et al. [1]. The STF model was unchanged, and the HF model was set up as described in Section S1 in Supplementary Materials [1].
2.3. Time Delay Neural Network (TDNN)
Time Delay Neural Network (TDNN) is a general class of dynamic networks that is well suited to deal with the time-series problems and temporal dependencies in large and small data. TDNN is similar to the feed-forward networks, but the input weight in the TDNN has a delay associated with it. In the regular feed-forward network, the input is multiplied by the weights, then passed to the nonlinear activation function such as the sigmoid function to produce the output layer. In the TDNN, a delay interval from D1 to Dn is added to the current input, then the input is multiplied by a specific weight to be compared with the past history of events, and this makes the input layer dynamic [24,25,26]. The output of the TDNN is estimated through the activation function like a regular feed-forward neural network to optimize the network weights.
In this case, TDNN is used to predict the +qPCR cases reported in Jordan, , through the function of the previous number of cases, f(x,w), to optimize the weight, w. The architecture of the network is composed of one input layer, one hidden layer, and one output layer. In order to attain the time delay, the input layer uses a delay component embedded in the input units. The number of these delay components used in the network to give the best output estimation is still a challenging issue to be resolved. More details about the utilized TDNN model are found in Section S2 in the Supplementary Materials.
3. Results and Discussion
3.1. The History of the COVID-19 Pandemic in Jordan
In Jordan, the COVID-19 epidemic consisted of three waves before the OMICRON variant. These waves are summarized in Table 1. The first case was reported on 14 March 2020. After that, the Jordanian government took a series of immediate actions (“lockdown” and “curfew”) to limit the spread of SARS-COV-2. The first wave started in late September 2020, reaching its maximum in the middle of November 2020 with about 29% +qPCR cases. This first wave was over by mid-January 2021, when the +qPCR testes were as low as 4%. The second wave triggered in early February 2021, reaching its maximum around mid-March 2021, and was over in mid-May 2021, with about 20% +qPCR cases reported. A minor wave, which is referred to here as the undeveloped third wave, was reported in the first week of August 2021, with maximum +qPCR cases reported at about 5%. This undeveloped wave was over around mid-November 2021. The fourth wave was reported around mid-December 2021 with maximum +qPCR tests around 11%. This wave started to decline, reaching about 3% +qPCR tests by New Year’s Eve. These waves are summarized in Table 1.
Table 1.
A summary about the pandemic waves in Jordan.
| Wave | Start | End | Peak |
|---|---|---|---|
| First 1 | September 2020 | Mid-January 2021 | Mid-November 2020 |
| Second 2 | February 2021 | Mid-May 2021 | Mid-March 2021 |
| Third 3 | August 2021 | Mid-November 2021 | Mid-August 2021 |
| Fourth 4 | December 2021 | New Year Eve | Mid-December 2021 |
1 Peak value was about 29% +qPCR cases, and lowest value was as low as 4%. 2 Peak value was about 20% +qPCR cases, and lowest value was as low as 2%. 3 Undeveloped wave with peak value at about 5% +qPCR cases, and lowest value was as low as 2%. 4 Uncompleted wave with peak value at about 11% +qPCR cases, and it never reached its minimum, as the OMICRON variant wave started and overlapped with the end of this fourth wave.
The previously described waves were reported as outbreaks of the COVID-19 variations before the OMICRON variant. The first cases of the OMICRON variant were reported in Jordan during early January 2022, when the epi curve climbed aggressively, reporting the fifth wave with a maximum during the first week of February 2022, reaching about 31% +qPCR tests.
Interestingly, the first two waves as well as the undeveloped wave were separated by 6 weeks, and each wave spanned about three months (Figure 2). The fourth wave did not develop, reaching its end because the OMICRON variant wave kicked in and overlapped with it.
Reading the vaccination and infection curves (Figure 2b), clearly suggests that vaccination and herd immunity had an effect on lowering (i.e., weakening) the second wave and, to some extent, the non-development of the third wave. However, the vaccination trend slowed down, and people’s awareness decreased, which led to an aggressive emergence of the OMICRON wave in January 2022. While reporting this here, the OMICRON wave has not yet reached its end.
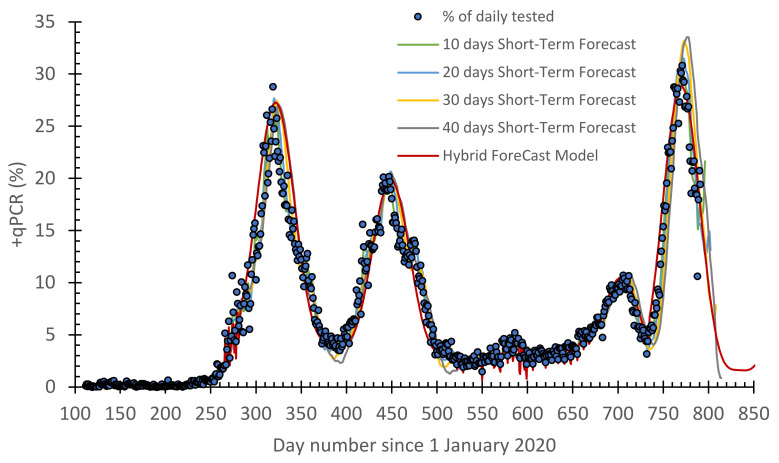
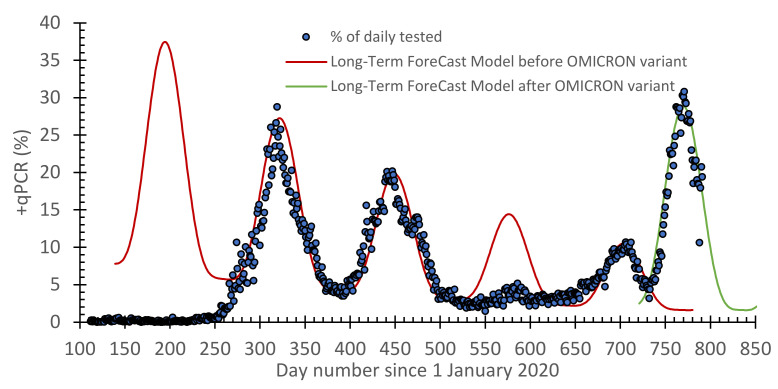
3.2. A Modified Forecast Model to Describe the OMICRON Variant Wave
As previously noted, the best STF model was the one based on the learning period as 10–20 days (Figure 3). Since the STF model has a fast response, it is capable of predicting the OMCIRON wave. As for the LTF model (Figure 4), the selected function is still capable of forecasting the reported COVID-19 cases before and after the OMCIRON variant. It only needed the parameters A, a, b, δ, and c in Equation (S2) (Section S1 in Supplementary Materials) to be redefined. After a slight modification, the HF model is still capable of forecasting the epidemic. This will be shown later in this section.
Figure 3.
A timeline for the daily reported +qPCR tests overlayed by the short-term forecast (STF, with 10–40 days learning) model and compared with the hybrid forecast (HF) model for the COVID-19 pandemic in Jordan.
Figure 4.
A timeline for the daily reported +qPCR tests overlayed by the long-term forecast (LTF) model predictions for the COVID-19 pandemic in Jordan before and after the emergence of the OMCIRON variant.
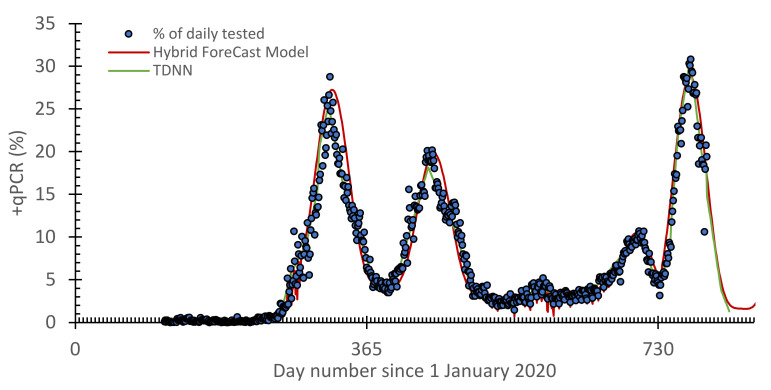
3.3. Time Delay Neural Network (TDNN)
The results obtained from the training TDNN to model positive cases in Jordan are given in Figure 5 with a comparison with the HF model. The performance metrics of modeling using positive cases in Jordan were tested according to R2, RMAE, and MSE. The performance values are given in Table 2. Quantitatively, these were 0.97, 1.2, and 0.7 for R2, RMAE, and MSE, respectively.
Figure 5.
Comparison between the time delay neural network (TDNN) model and the hybrid forecast (HF) model for the +qPCR cases.
Table 2.
Evaluation metrics of the three forecasting models: short-term forecast (STF), hybrid forecast (HF), and time delay neural network (TDNN) model for the whole COVID-19 pandemic thus far in Jordan, including before and after the emergence of OMICRON variant.
| Model | Number of Learning Days | R 2 | RMSE | MAE |
|---|---|---|---|---|
| STF | 5 | 0.99 | 0.62 | 0.37 |
| 10 | 0.98 | 0.87 | 0.52 | |
| 15 | 0.98 | 1.04 | 0.65 | |
| 20 | 0.97 | 1.22 | 0.75 | |
| 25 | 0.96 | 1.47 | 0.88 | |
| 30 | 0.94 | 1.77 | 1.04 | |
| 35 | 0.93 | 2.07 | 1.19 | |
| 40 | 0.90 | 2.35 | 1.33 | |
| HF | 0.95 | 1.89 | 1.09 | |
| TDNN | 0.97 | 1.15 | 0.74 |
The analysis of the results shows that the forecasting model, TDNN, made an accurate prediction despite changing the statistical properties of the target data (with the appearance of the Omicron version) over time. The data-driven models can be a valuable tool to understand and analyze phenomena (such as COVID-19) and make predictions.
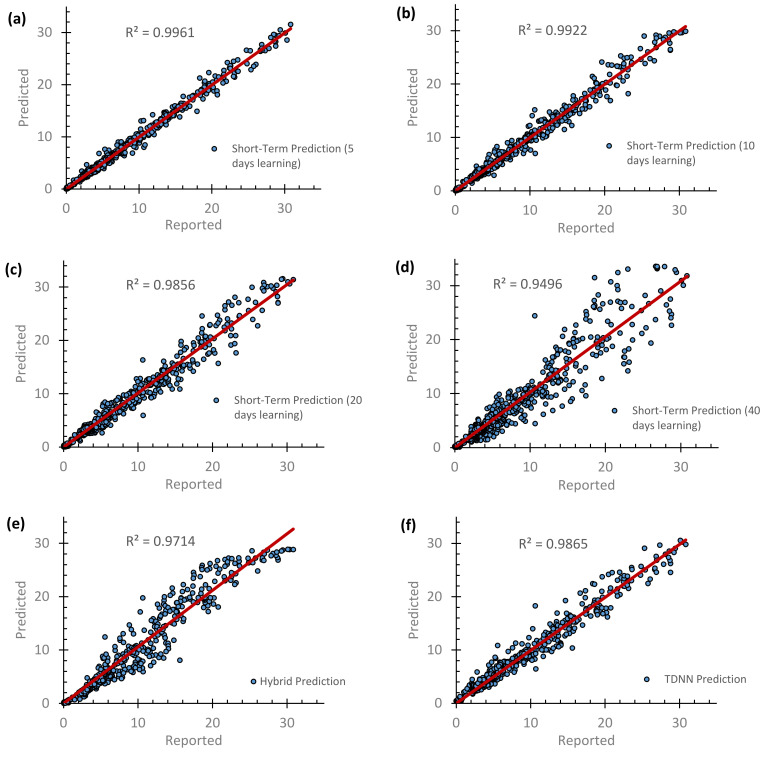
After all, the scatter plots for the predicted −qPCR daily cases against the reported ones are presented in Figure 6. Together with the performance of the models (i.e., Table 2), this shows that increasing the number of learning days reduced the R2 value and also the performance of the STF model. However, a five-days learning approach should be avoided because it is not realistic, as it replicates the reported data. Taking 40 days gives a time-lag in the forecasted data. As such, a reasonable learning period can be 10–20 days. Interestingly, the selected mathematical function of the LTF model, which is also impeded in the HF model, is capable of forecasting the reported COVID-19 cases before the emergence of the OMICRON variation. However, the same function was still valid with a slight change to its parameters. The overall performance of the HF model was 0.95, 1.9, and 1.1 for R2, RMAE, and MSE, respectively.
Figure 6.
Comparisons of the forecasted versus the reported +qPCR daily cases, including the periods before and after the emergence of the OMICRON variant, using (a–d) STF model prediction that takes 5, 10, 20 and 40 days of learning, (e) HF model prediction and (f) TDNN prediction.
4. Conclusions
Herein, a simple prediction approach was proposed to forecast COVID-19 reported cases in Jordan for a trail to include the OMICRON variant. The basic principle was built on our previous approaches [1]: short-term forecast (STF) model, long-term forecasting (LTF) model, and hybrid approach. In the end, the best model was the TDNN, followed by the HF model that included the LTF models before and after the OMICRON variant outbreak. When the LTF model failed to cope with the sudden temporal variation of the pandemic, the parameters of the STF model were reconsidered. The outcomes of this investigation can be applied to COVID-19 pandemic cases that are similar to the Jordanian case.
Acknowledgments
The authors would like to thank Azmi Mahafza (Microbiology and Immunology at the Department of Pathology Forensic Medicine, School of Medicine, University of Jordan) for valuable advice and discussion. T.H. acknowledges support by the Eastern Mediterranean and Middle East Climate and Atmosphere Research (EMME-CARE) project, which has received funding from the European Union’s Horizon 2020 Research and Innovation Programme (grant agreement number 856612) and the Government of Cyprus. The sole responsibility of this publication lies with the authors. Open access funding provided by University of Helsinki.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines10040569/s1, Section S1. Forecast Models for the Postive qPCR Tests. Figure S1. Scheme showing the short-term forecast (STF) model. This Figure was adopted from Hussein, et al. [1]. Figure S2. A scheme showing the long-term forecast (LTF) model. This Figure was adopted from Hussein, et al. [1]. Figure S3. A scheme showing the hybrid forecast (HF) model. This Figure was adopted from Hussein, et al. [1]. Section S2. Time Delay Neural Network (TDNN). FigureS4: The time-delay neural network (TDNN) architecture.
Author Contributions
Conceptualization, T.H., N.E., D.W. and O.S.; methodology, T.H., N.E. and O.S.; software, O.S. and M.A.; validation, T.H., O.S. and M.A.; formal analysis, T.H., N.E., P.L.F., M.A.Z. and M.H.H.; investigation, T.H. and M.H.H.; resources, T.H., D.W. and N.E.; data curation, T.H., N.E., M.H.H., P.L.F. and O.S.; writing—original draft preparation, T.H.; writing—review and editing, T.H., M.H.H., O.S., M.A., P.L.F., M.A.Z., D.W. and N.E.; visualization, T.H., M.H.H. and P.L.F.; project administration, T.H.; funding acquisition, T.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by generous funding by the Deanship of Scientific Research at the University of Jordan.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is available upon request.
Conflicts of Interest
The author declares no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hussein T., Hammad M.H., Fung P.L., Al-Kloub M., Odeh I., Zaidan M.A., Wraith D. COVID-19 Pandemic Development in Jordan—Short-Term and Long-Term Forecasting. Vaccines. 2021;9:728. doi: 10.3390/vaccines9070728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Handelman G.S., Kok H.K., Chandra R.V., Razavi A.H., Lee M.J., Asadi H. eDoctor: Machine learning and the future of medicine. J. Intern. Med. 2018;284:603–619. doi: 10.1111/joim.12822. [DOI] [PubMed] [Google Scholar]
- 3.Sidey-Gibbons J.A.M., Sidey-Gibbons C.J. Machine learning in medicine: A practical introduction. BMC Med. Res. Methodol. 2019;19:64. doi: 10.1186/s12874-019-0681-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baleanu D., Abadi M.H., Jajarmi A., Vahid K.Z., Nieto J.J. A new comparative study on the general fractional model of COVID-19 with isolation and quarantine effects. Alex. Eng. J. 2022;61:4779–4791. doi: 10.1016/j.aej.2021.10.030. [DOI] [Google Scholar]
- 5.Hussain S., Madi E.N., Khan H., Etemad S., Rezapour S., Sitthiwirattham T., Patanarapeelert N. Investigation of the Stochastic Modeling of COVID-19 with Environmental Noise from the Analytical and Numerical Point of View. Mathematics. 2021;9:3122. doi: 10.3390/math9233122. [DOI] [Google Scholar]
- 6.Deressa C.T., Duressa G.F. Investigation of the dynamics of COVID-19 with SEIHR nonsingular and nonlocal kernel fractional model. Int. J. Model. Simul. 2021:1–19. doi: 10.1080/02286203.2021.2012636. [DOI] [Google Scholar]
- 7.Wynants L., Van Calster B., Collins G.S., Riley R.D., Heinze G., Schuit E., Bonten M.M.J., Dahly D.L., Damen J.A., Debray T.P.A., et al. Prediction models for diagnosis and prognosis of covid-19: Systematic review and critical appraisal. BMJ. 2020;369:m1328. doi: 10.1136/bmj.m1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riley P., Riley A., Turtle J., Ben-Nun M. COVID-19 deaths: Which explanatory variables matter the most? medRxiv. 2020:1–21. doi: 10.1101/2020.06.11.20129007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mollalo A., Rivera K.M., Vahedi B. Artificial Neural Network Modeling of Novel Coronavirus (COVID-19) Incidence Rates across the Continental United States. Int. J. Environ. Res. Public Health. 2020;17:4204. doi: 10.3390/ijerph17124204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li M., Zhang Z., Cao W., Liu Y., Du B., Chen C., Liu Q., Uddin N., Jiang S., Chen C., et al. Identifying novel factors associated with COVID-19 transmission and fatality using the machine learning approach. Sci. Total Environ. 2021;764:142810. doi: 10.1016/j.scitotenv.2020.142810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alsayed A., Sadir H., Kamil R., Sari H. Prediction of Epidemic Peak and Infected Cases for COVID-19 Disease in Malaysia, 2020. Int. J. Environ. Res. Public Health. 2020;17:4076. doi: 10.3390/ijerph17114076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aguiar M., Ortuondo E.M., Van-Dierdonck J.B., Mar J., Stollenwerk N. Modelling COVID 19 in the Basque Country from introduction to control measure response. Sci. Rep. 2020;10:17306. doi: 10.1038/s41598-020-74386-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kannan S., Subbaram K., Ali S., Kannan H. The Role of Artificial Intelligence and Machine Learning Techniques: Race for COVID-19 Vaccine. Arch. Clin. Infect. Dis. 2020;15:e103232. doi: 10.5812/archcid.103232. [DOI] [Google Scholar]
- 14.Mohamed S., Giabbanelli P., Alvarez-Lopez F., Adly A.S., Adly A.S., Adly M.S. Approaches Based on Artificial Intelligence and the Internet of Intelligent Things to Prevent the Spread of COVID-19: Scoping Review. J. Med. Internet Res. 2020;22:e19104. doi: 10.2196/19104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lalmuanawma S., Hussain J., Chhakchhuak L. Applications of machine learning and artificial intelligence for Covid-19 (SARSCoV-2) pandemic: A review. Chaos Solitons Fractals. 2020;139:110059. doi: 10.1016/j.chaos.2020.110059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO Non-Pharmaceutical Public Health Measures for Mitigating the Risk and Impact of Epidemic and Pandemic Influenza. A Checklist for Pandemic Influenza Risk and Impact Management: Building Capacity for Pandemic Response. 2019. [(accessed on 1 July 2021)]. Available online: https://www.who.int/publications/i/item/non-pharmaceutical-public-health-measuresfor-mitigating-the-risk-and-impact-of-epidemic-and-pandemic-influenza.
- 17.Porgo T.V., Norris S.L., Salanti G., Johnson L.F., Simpson J.A., Low N., Egger M., Althaus C.L. The use of mathematical modeling studies for evidence synthesis and guideline development: A glossary. Res. Synth. Methods. 2019;10:125–133. doi: 10.1002/jrsm.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Godio A., Pace F., Vergnano A. SEIR Modeling of the Italian Epidemic of SARS-CoV-2 Using Computational Swarm Intelligence. Int. J. Environ. Res. Public Health. 2020;17:3535. doi: 10.3390/ijerph17103535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parham P.E., Michael E. Outbreak properties of epidemic models: The roles of temporal forcing and stochasticity on pathogen invasion dynamics. J. Theor. Biol. 2011;271:1–9. doi: 10.1016/j.jtbi.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 20.Hadid S.B., Ibrahim R.W., Altulea D., Momani S. Solvability and stability of a fractional dynamical system of the growth of COVID-19 with approximate solution by fractional Chebyshev polynomials. Adv. Differ. Equ. 2020;2020:338. doi: 10.1186/s13662-020-02791-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar S., Kumar R., Momani S., Hadid S. A study on fractional COVID-19 disease model by using Hermite wavelets. Math. Methods Appl. Sci. 2021:1–17. doi: 10.1002/mma.7065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saidan M.N., Shbool M.A., Arabeyyat O.S., Al-Shihabi S.T., Al Abdallat Y., Barghash M.A., Saidan H. Estimation of the probable outbreak size of novel coronavirus (COVID-19) in social gathering events and industrial activities. Int. J. Infect. Dis. 2020;98:321–327. doi: 10.1016/j.ijid.2020.06.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kheirallah K.A., Alsinglawi B., Alzoubi A., Saidan M.N., Mubin O., Alorjani M.S., Mzayek F. The Effect of Strict State Measures on the Epidemiologic Curve of COVID-19 Infection in the Context of a Developing Country: A Simulation from Jordan. Int. J. Environ. Res. Public Health. 2020;17:6530. doi: 10.3390/ijerph17186530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peddinti V., Povey D., Khudanpur S. A time delay neural network architecture for efficient modeling of long temporal contexts; Proceedings of the Sixteenth Annual Conference of the International Speech Communication Association; Dresden, Germany. 6–10 September 2015; pp. 3214–3218. [Google Scholar]
- 25.Waibel A., Hanazawa T., Hinton G., Shikano K., Lang K.J. Phoneme recognition using time-delay neural networks. IEEE Trans. Acoust. Speech Signal Process. 1989;3:328–339. doi: 10.1109/29.21701. [DOI] [Google Scholar]
- 26.Medsker L., Jain L.C. Recurrent Neural Networks: Design and Applications. CRC Press; Boca Raton, FL, USA: 1999. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is available upon request.