Abstract
COVID-19 has impacted children’s immunization rates, putting the lives of children at risk. The present study assesses the impact of phone-call counseling, on immunization uptake during the pandemic. Families of babies discharged from the SNCUs in six government centers in three South Indian states were recruited. Calls were made 10 days after the immunization due date. Missed vaccinees were counseled and followed up on 7 and 15 days. Of 2313 contacted, 2097 completed the survey. Respondents were mostly mothers (88.2%), poor (67.5%), and had secondary level education (37.4%). Vaccinations were missed due to the baby’s poor health (64.1%), COVID-19 related concerns (32.6%), and lack of awareness (16.8%). At the end of the intervention, the immunization uptake increased from 65.2% to 88.2%. Phone-call intervention can safely support immunization and lower the burden on health workers.
Keywords: SNCU babies, COVID, immunization uptake
1. Introduction
Vaccine-preventable diseases (VPDs) such as rubella, measles, polio, and diphtheria, contribute significantly to child mortality and morbidity. Globally, they account for approximately 1.5 million deaths and 19.5 million serious morbidities among infants annually [1]. Full immunization can be a key, easy and cost-effective way to protect children from VPDs during the first 5 years of their life and improve child survival rates [2,3]. Globally, an estimated 2–3 million deaths could be prevented every year if every child completes the vaccination schedule [4]. However, most low-to-middle income countries (LMICs) such as Mediterranean, South-East Asia, and African regions, have less immunization coverage (80%) compared to high-income WHO regions (90%) [5].
Like most LMICs, India has been struggling to meet its immunization coverage goals. India has the largest birth cohort in the world and contributes significantly to child mortality and morbidity resulting from VPDs [6]. India has shown approximately a 19-percentage point increase in the national average of full immunization (BCG, Measles, and three doses each of Polio and DPT) since the NFHS-4 (2005-06). This might be one of the reasons for the recent decline in child mortality rates. However, India has a long way to reach its Sustainable Development Goal (SDG) [7]. Thus, increasing universal vaccination coverage continues to be a key strategy to achieve this goal. Additionally, in recent years, increasing resistance has been observed among parents to vaccinate their children between ages 12 and 23 years. Negative attitudes and beliefs about vaccines, lack of adequate information, distrust in the sources of information, and negative propaganda in social media (i.e., WhatsApp and Facebook) are believed to be primary reasons behind their hesitation [8,9].
The COVID-19 pandemic is expected to add to these existing challenges around maternal and child health care [10]. In April 2020, routine postnatal check-ups and immunization visits reportedly decreased compared to the previous year, thus putting mothers and children at higher risk of contracting VPDs [10,11,12]. In late March 2020, WHO recommended several LMICs to temporarily suspend routine immunization services and divert all health care resources towards controlling the COVID-19 pandemic [11]. In addition to the temporary hold on primary health services put by the Government of India, the shortage of frontline workers, frequent lockdowns, and lack of transportation during the pandemic period could have slowed down the utilization of most preventive services [10]. Simultaneously, fear of COVID-19 infection, lack of social distancing, and inadequate infection control practices affected health-seeking behaviour in general [10]. In light of all these challenges, there were concerns raised regarding relapse in immunization rates for India, Pakistan, and Nepal [12]. This highlights the need for appropriate efforts to continue immunization uptake in LIMCs [13]. Sick Neonatal Care Units’ (SNCUs) babies, due to their comorbidities, are prone to serious infections, making full immunization and adequate postnatal care even more important. Encouraging caregivers to immunize these babies in critical circumstances such as the COVID-19 pandemic is important.
The primary goal of the present study was to examine the impact of a phone-based intervention on immunization uptake in SNCU babies. In addition, we also assessed the extent of existing immunization coverage and reasons for not vaccinating the child.
2. Methods
2.1. Study Sites
The study was conducted in six health care facilities—(1) Niloufer Hospital, Hyderabad in the state of Telangana; (2) Rajiv Gandhi Institute of Medical Sciences (RIMS), Kadapa; (3) Maharani Hospital, Vizianagaram; and (4) Visakhapatnam Institute of Medical Sciences and Hospital (VMH), Visakhapatnam in the state of Andhra Pradesh; (5) Raichur Institute of Medical Sciences (RIMS), Raichur; and (6) Yadgir District Hospital in the State of Karnataka. Surveys were conducted from June to September 2020.
2.2. Study Participants
As shown in Table 1, a list of families (n = 3115) who had a baby discharged from the SNCU wards was obtained from respective facilities. Of these 3115, 802 (25.7%) families were excluded due to reasons such as the baby or mother’s death before or after discharge or they were unreachable by phone (i.e., switched off phones or invalid numbers). The remaining 2313 families who were eligible to participate were those who had reported the baby and mother alive during the time of call, spoke at least one of three languages (Hindi, Kannada, and Telugu), and had a valid phone number. From these 2313 families, 2097 (90.6%) families successfully completed the survey.
Table 1.
Selection criteria for study participants.
| Reason | Population Size (N) | Sample Size (n) | % |
|---|---|---|---|
| List of Families Obtained from the Hospital | 3115 | ||
| Excluded from the study | 3115 | 802 | 25.7% |
| Baby/mother died before discharge | 802 | 173 | 21.5% |
| Baby/mother died after discharge | 802 | 91 | 11.3% |
| Invalid/wrong number | 802 | 197 | 24.5% |
| Switched off phones | 802 | 332 | 41.4% |
| Data enumerator spoke a different language | 802 | 9 | 1.1% |
| Included in the Study | 3115 | 2313 | 74.3% |
| Included in the study and survey complete | 2313 | 2097 | 90.6% |
| Included in the study but survey not complete | 2313 | 216 | 9.3% |
| • Not available | 216 | 71 | 32.8% |
| • Not picked up or answered the call | 216 | 61 | 28.2% |
| • The family refused to participate | 216 | 51 | 23.6% |
| • Baby not yet discharged | 216 | 18 | 8.3% |
| • Other reasons * | 216 | 15 | 6.9% |
* Patient not responding, the baby born in another hospital, call disconnected or completed by another investigator.
2.3. Study Procedures
Face validity of the structured questionnaire was established by experts and was pilot-tested with ten respondents. After taking oral consent from each respondent, tele-trainers collected information on the respondent’s socio-demographic background, baby’s health (i.e., age, last recorded weight, and immunization status), and detailed reasons for non-vaccination through a phone call. The initial call was made seven to ten days after the due date for immunization. Survey CTO software version 2.70 was used to record responses [14]. At the end of each call, families who had not vaccinated their baby or had missed the scheduled vaccine were counseled for immunization. During counseling, tele-trainers emphasized the role of vaccines in the baby’s health; addressed any fears, myths, or doubts the family had; gave information about where they can vaccinate their baby; and, if asked, gave the contact details of the local ASHA worker. Families who had not vaccinated their baby or were unreachable during the initial call were followed-up on after seven days. If families did not vaccinate their baby at the first follow-up call, they were further counseled. The second follow-up call was conducted fifteen days after the initial call (Figure 1). Immunization status self-reported by the participant was recorded at each time point. Ethical approval for the study was obtained from the ACE Independent Ethics Committee.
Figure 1.
Follow-up schedule.
3. Findings
3.1. Sociodemographic Characteristics
Respondents were mostly mothers, the majority of whom owned a below poverty level (BPL) card and had no education or less than secondary level education. Most families had received a vaccination card that contained information regarding routine immunization schedules for the baby. A small percentage of families had received the card but did not have it with them at the time of the survey (Table 2).
Table 2.
Characteristics of study participants (N = 2097).
| Variables | n | % |
|---|---|---|
| State-wise Respondents | ||
| Andhra Pradesh | 948 | 45.2% |
| Karnataka | 732 | 34.9% |
| Telangana | 417 | 19.9% |
| Respondents | ||
| Mother | 1849 | 88.2% |
| Father | 128 | 6.1% |
| Other | 120 | 5.7% |
| Education Level | ||
| No education | 399 | 19.0% |
| No formal education but can read and write | 23 | 1.1% |
| Up to 5th standard | 126 | 6.0% |
| 6th to 10th standard | 785 | 37.4% |
| 11th standard to degree/diploma | 575 | 27.4% |
| Graduate | 137 | 6.5% |
| Post-graduate | 52 | 2.5% |
| Owns BPL * Card | 1415 | 67.5% |
| Received Vaccination Card | 1996 | 95.2% |
| Received and accessible at home | 1922 | 96.3% |
| Received but not accessible | 74 | 3.7% |
| Did not receive | 101 | 4.8% |
* BPL Below Poverty Line.
3.2. Immunization Coverage
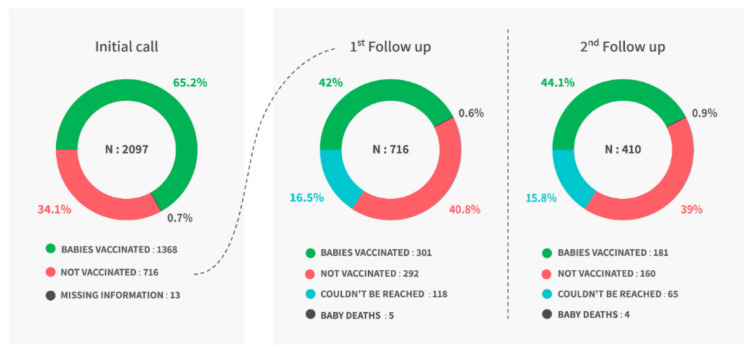
During the initial call, 1368 (65.2%) babies were fully immunized (i.e., had not missed any scheduled vaccines), whereas 716 babies (34.1%) had missed at least one of the scheduled vaccines. Families of these 716 babies were counseled for immunization. During the first follow-up call, tele-trainers found that 301 (42%) of these 716 families vaccinated their baby, 292 (42.0%) had not vaccinated their baby, 5 babies had died, and 118 (16.5%) families could not be reached. These 410 (292 + 118) families were called after seven days from the first follow-up. During the second follow-up, an additional 181 (44.1%) babies were vaccinated, 160 (39.0%) were not vaccinated, 65 (15.8%) could not be reached and four (1.0%) babies had died (Figure 1).
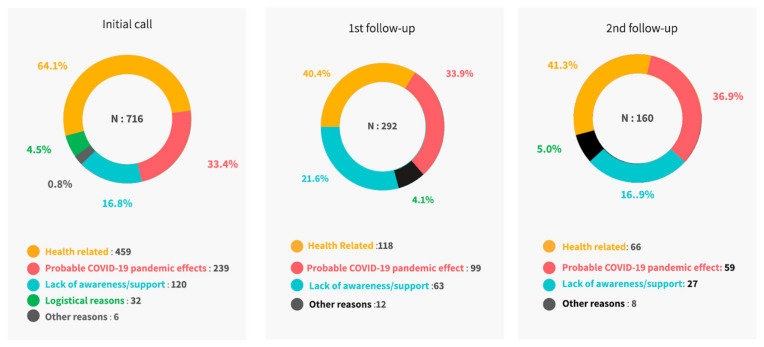
Overall, the baby’s health status, probable COVID-19 pandemic effect, and lack of awareness or support (Figure 2) were reported as primary reasons for non-vaccination. Detailed responses at each timepoint are specified in Table 3.
Figure 2.
Overall reasons for non-vaccination.
Table 3.
Detailed reasons for non-vaccination during each call.
| Reasons |
Initial Call
(N = 716) |
1st Follow-Up Call
(N = 292) |
2nd Follow-Up Call (N = 160) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Health-related | 459 (64.1) | 118 (40.4) | 66 (41.3) |
| Underweight | 211 (29.5) | 81 (27.7) | 45 (28.1) |
| Child ill and not brought to the facility | 106 (14.8) | 36 (12.3) | 18 (11.3) |
| Doctors not recommended | 62 (8.7) | 1 (0.3) | 3 (1.9) |
| Baby born prematurely | 39 (5.4) | none | None |
| Child ill, brought but not given vaccines | 34 (4.7) | none | None |
| Delay in previous vaccination | 7 (1) | none | None |
| Probable COVID-19 pandemic effects | 239 (33.4) | 99 (33.9) | 59 (36.9) |
| Lockdown | 86 (12.0) | 57 (19.5) | 29 (18.1) |
| Transportation problem | 60 (8.4) | none | None |
| Insufficient staff (ASHA/ANMs) | 29 (4.1) | 40 (13.7) | 30 (18.8) |
| Fear of coronavirus affecting the child | 24 (3.4) | none | None |
| Not knowing time/place for vaccination | 20 (2.8) | none | None |
| Insufficient vaccines | 11 (1.5) | 2 (0.7) | 2 (1.3) |
| ASHA/ANM having COVID-19 | 4 (0.6) | none | None |
| Long wait | 3 (0.4) | none | None |
| Insufficient number of babies | 2 (0.3) | none | None |
| Lack of awareness/support | 120 (16.8) | 63 (21.6) | 27 (16.9) |
| Lack of awareness about vaccine | 43 (6) | 27 (9.2) | 11 (6.9) |
| Community worker/ANM did not inform | 42 (5.9) | 36 (12.3) | None |
| Lack of awareness about schedule | 25 (5.7) | none | 15 (9.4) |
| Fear/rumours about side effects/no faith | 10 (1.4) | none | None |
| Logistical Reasons * | 32 (4.5) | none | None |
| Other Reasons † | 6 (0.8) | 12 | 8 (5.0) |
* mother too busy, family problems, out of the station, and mismatch of vaccination day and when they planned a visit. † baby crying, rain, festivals, and other personal reasons.
3.3. Post Call Change in Immunization Uptake
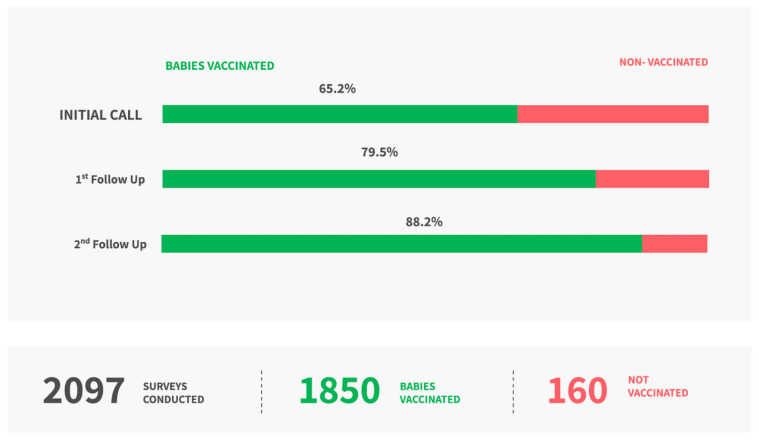
At the first follow-up call, the immunization rate changed from 65.2% to 79.5% (22% increase). At the second follow-up call, the immunization rate changed from 79.5% to 88.2% (11% increase). Overall, at the end of 2–3 weeks a total of 1850 babies (i.e., 482 additional) were vaccinated and a 35% increase was seen in immunization uptake reducing the immunization gap in this sample (Figure 3).
Figure 3.
Immunization uptake at the end of the study.
We did not intend to measure the cost incurred during the study. However, post-study calculations showed an approximate expenditure of EUR 2 per conversion from non-vaccinated to vaccinated status. This included the cost of resources for training, training time, running phone costs, and time of data enumerators for making calls. It does not include other administrative costs and the time of experts for planning and executing the study.
4. Discussion
Child mortality due to inadequate or non-immunization is a serious public health issue in India. Every year, thousands of children die and several hundred are left at risk of developing serious disabilities because they are either partially or not vaccinated [15]. In India, although rates of full immunization have increased, there are geographical differences, with rural and low resource areas showing lower rates [16,17].
Interruption or temporary suspension of child immunization during the COVID-19 pandemic is expected to reduce the ability of healthcare systems to meet the need for routine maternal and child healthcare services [13]. Studies conducted around the 2014 Ebola outbreak show that disruption of the routine childcare services during the period had resulted in a second public health crisis in Africa [18]. In some communities of Sierra Leone, the age-eligible measles vaccination rate was reduced by 25.9 percentage points from 71.3% (before the Ebola outbreak) to 45.7% (during the outbreak) [19]. In our study population, conducted after the first wave of the COVID-19 pandemic, we found that 34.1% of families were not able to vaccinate their baby or had missed the vaccination schedule. COVID-19 pandemic challenges (such as lockdown, fear of infection, misinformation) were amongst the primary reasons for the delayed vaccination.
Studies evaluating the effect of programs to improve immunization uptake in LMICs are very limited. Programs that create awareness, provide health education to the community, and teach preventive behaviours are found to help increase knowledge and change attitudes and behaviours of the community [20,21,22,23]. Specifically, targeted interventions such as community or facility-based educational programs to caregivers, providing reminder cards to mothers, home visits by ASHAs or ANMs, and integrating immunization with other primary health care services have been found to be somewhat effective in increasing immunization uptake in LMICs [24]. For instance, after the Ebola outbreak, an 11-percentage point increase was found in measles vaccination rates after vaccinators visited home to educate parents and encourage them to vaccinate their babies [25]. A randomized controlled trial conducted in an urban area of Pakistan showed a 31% increase in the completion rate of the third dose of diphtheria–pertussis–tetanus (DPT3) among the intervention group (i.e., mothers who received a redesigned immunization card and canter-based education) compared with the standard of care group [26]. We did not find reports on phone-based interventions in crisis situations targeted at improving immunization.
The present study, conducted during the COVID-19 pandemic, includes a large sample of SNCU babies across three states in South India from six government facilities. We found that it was necessary to reach families and provide targeted information and counselling about vaccination to increase immunization during the COVID-19 pandemic. Considering the challenges the healthcare system faced during this period, a simple and remote intervention to counsel families was attempted. An increase in child immunization observed after two rounds of follow-up phone calls in our study needs further consideration and study to understand if it could be a viable additional support system.
The study has a few limitations. Selection bias could have occurred due to the fact that those people who had active phone connections and picked up calls were included. Therefore, the results of this study could only be applicable to similar populations. Immunization data were self-reported and did not corroborate hospital records. This might result in self-reporting bias. To minimize the impact of this bias on study results, we considered verifying vaccination status by asking participants to upload their vaccination cards. However, an initial exploration during the pilot study showed that challenges such as lack of smartphone availability, unfamiliarity with technology to upload photos, and quality of photos shared made it unfeasible. Furthermore, cross verifying with government records was also not possible given the issue of lack of access to personalized health records. We did not collect the vaccination date within the village and went by the birth date. However, we gave a gap of 10 days after the due date to ensure that this was not a limiting criterion. Data collection extended over a long period and continued after lockdowns were lifted. Thus, it is possible that factors such as the lifting of lockdowns, catch-up immunization drives might contribute to the intervention effect to some extent. However, since the majority of the data were collected after the lockdown was lifted and 33.3% of families reported COVID-19 and lockdown-related reasons for non-vaccination, we assume that this would have played a minor role. The results of this study are generalizable only to other high-risk babies with similar sociodemographic profiles and in similar health systems.
5. Conclusions
Upsurge in immunization uptake in this study revealed that persistent reminder phone calls that provide information and confidence to families could be a potentially viable, quick, safe, and convenient option to support the existing health system. When used in conjunction with existing interventions, these reminder calls can help connect with hard-to-reach populations and address their health-related needs in critical situations such as the COVID-19 pandemic. The results of our study are encouraging, but further studies are needed to address some of the limitations to build evidence. We believe that the learnings from this implementation research study may be applicable to other similar geographies and health systems, not only for this pandemic but other crisis situations as well.
Author Contributions
Conceptualization, S.R.S.V.; Data curation, S.C.P.; Formal analysis, S.C.P.; Funding acquisition, D.T. and S.A.; Investigation, S.S.D. and S.C.P.; Methodology, S.M. and S.R.S.V.; Project administration, S.S.D. and T.S.P.; Resources, T.S.P., D.T., M.A. and H.S.; Software, S.C.P.; Supervision, S.S.D., S.R.S.V., S.A., M.A. and H.S.; Visualization, S.S.D.; Writing—original draft, S.M. and M.S.; Writing—review & editing, S.M., M.S., S.S.D., S.C.P., S.D.Y., T.S.P., D.T., S.R.S.V., S.U., S.A., M.A. and H.S. All authors have read and agreed to the published version of the manuscript.
Funding
The research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Delaration of Helsinki, and approved by the ACE Independent Ethics Committee (protocol code YOSA00002) on 13 June 2020.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to participant’s privacy.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization Immunization Coverage. [(accessed on 5 October 2020)]. Available online: https://www.who.int/en/news-room/fact-sheets/detail/immunization-coverage.
- 2.United Nations Children Funds (UNICEF) Child Mortality and COVID-19. [(accessed on 10 March 2021)]. Available online: https://data.unicef.org/topic/child-survival/covid-19/
- 3.World Health Organization WHO MDG 4: Reduce Child Mortality. [(accessed on 8 February 2021)]. Available online: https://www.who.int/topics/millennium_development_goals/child_mortality/en/
- 4.United Nations Children Funds (UNICEF) Newborn and Child Health: Let’s Ensure Newborns Survive and Thrive. [(accessed on 11 October 2021)]. Available online: https://www.unicef.org/india/what-we-do/newborn-and-child-health.
- 5.Vakili R., Hashemi A.G., Khademi G., Abbasi M.A., Saeidi M. Immunization Coverage in WHO Regions: A Review Article. Int. J. Pediatrics. 2015;3:111–118. [Google Scholar]
- 6.Laxminarayan R., Ganguly N.K. India’s Vaccine Deficit: Why More than Half of Indian Children Are Not Fully Immunized, and What Can—And Should—Be Done. Health Aff. Proj. Hope. 2011;30:1096–1103. doi: 10.1377/hlthaff.2011.0405. [DOI] [PubMed] [Google Scholar]
- 7.Vashishtha V.M., Kumar P. 50 Years of Immunization in India: Progress and Future. Indian Pedia. 2013;50:111–118. doi: 10.1007/s13312-013-0025-0. [DOI] [PubMed] [Google Scholar]
- 8.Newtonraj A. India’s Fight against Vaccine-Preventable Diseases; Newer Changes and Challenges. J. Med. Soc. 2019;33:64–65. doi: 10.4103/jms.jms_90_18. [DOI] [Google Scholar]
- 9.Palanisamy B., Gopichandran V., Kosalram K. Social Capital, Trust in Health Information, and Acceptance of Measles-Rubella Vaccination Campaign in Tamil Nadu: A Case-Control Study. J. Postgrad. Med. 2018;64:212–219. doi: 10.4103/jpgm.JPGM_249_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kasi S.G., Dhir S.K., Verma S., Pemde H.K., Balasubramanian S., Shah A.K., Shivananda S., Marathe S., Chatarjee K., Kalyani S., et al. Immunization During the COVID-19 Pandemic: Recommendations From Indian Academy of Pediatrics Advisory Committee on Vaccines and Immunization Practices. Indian Pediatrics. 2020;57:1147–1152. doi: 10.1007/s13312-020-2071-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adamu A.A., Jalo R.I., Habonimana D., Wiysonge C.S. COVID-19 and Routine Childhood Immunization in Africa: Leveraging Systems Thinking and Implementation Science to Improve Immunization System Performance. Int. J. Infect. Dis. 2020;98:161–165. doi: 10.1016/j.ijid.2020.06.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization WHO. UNICEF Warn of a Decline in Vaccinations during COVID-19. [(accessed on 9 February 2021)]. Available online: https://www.who.int/news/item/15-07-2020-who-and-unicef-warn-of-a-decline-in-vaccinations-during-covid-19.
- 13.Hossain M.M., Abdulla F., Karimuzzaman M., Rahman A. Routine Vaccination Disruption in Low-Income Countries: An Impact of COVID-19 Pandemic. Asia. Pac. J. Public Health. 2020;32:509–510. doi: 10.1177/1010539520957808. [DOI] [PubMed] [Google Scholar]
- 14.Dobility Inc . SurveyCTO. Dobility, Inc.; Cambridge, MA, USA: 2020. [Google Scholar]
- 15.National Health Portal Immunization in India. [(accessed on 3 October 2019)]; Available online: https://www.nhp.gov.in/Immunization_ms.
- 16.Dhirar N., Dudeja S., Khandekar J., Bachani D. Childhood Morbidity and Mortality in India—Analysis of National Family Health Survey 4 (NFHS-4) Findings. Indian Pediatrics. 2018;55:335–338. doi: 10.1007/s13312-018-1276-6. [DOI] [PubMed] [Google Scholar]
- 17.International Institute for Population Sciences (IIPS) National Family Health Survey (NFHS-5), 2019–2021: India. International Institute for Population Sciences (IIPS); Mumbai, India: 2021. [Google Scholar]
- 18.Takahashi S., Metcalf C.J.E., Ferrari M.J., Moss W.J., Truelove S.A., Tatem A.J., Grenfell B.T., Lessler J. Reduced Vaccination and the Risk of Measles and Other Childhood Infections Post-Ebola. Science. 2015;347:1240–1242. doi: 10.1126/science.aaa3438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sun X., Samba T.T., Yao J., Yin W., Xiao L., Liu F., Liu X., Zhou J., Kou Z., Fan H., et al. Impact of the Ebola Outbreak on Routine Immunization in Western Area, Sierra Leone—A Field Survey from an Ebola Epidemic Area. BMC Public Health. 2017;17:363. doi: 10.1186/s12889-017-4242-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cowling B.J., Chan K.-H., Fang V.J., Cheng C.K.Y., Fung R.O.P., Wai W., Sin J., Seto W.H., Yung R., Chu D.W.S., et al. Facemasks and Hand Hygiene to Prevent Influenza Transmission in Households: A Cluster Randomized Trial. Ann. Intern. Med. 2009;151:437–446. doi: 10.7326/0003-4819-151-7-200910060-00142. [DOI] [PubMed] [Google Scholar]
- 21.Cowling B.J., Fang V.J., Riley S., Malik Peiris J.S., Leung G.M. Estimation of the Serial Interval of Influenza. Epidemiol. Camb. Mass. 2009;20:344–347. doi: 10.1097/EDE.0b013e31819d1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stebbins S., Downs J.S., Vukotich C. Using Nonpharmaceutical Interventions to Prevent Influenza Transmission in Elementary School Children: Parent and Teacher Perspectives. J. Public Health Manag. Pract. JPHMP. 2009;15:112–117. doi: 10.1097/01.PHH.0000346007.66898.67. [DOI] [PubMed] [Google Scholar]
- 23.Vukotich C.J., Coulborn R.M., Aragon T.J., Baker M.G., Burrus B.B., Aiello A.E., Cowling B.J., Duncan A., Enanoria W., Fabian M.P., et al. Findings, Gaps, and Future Direction for Research in Nonpharmaceutical Interventions for Pandemic Influenza. Emerg. Infect. Dis. J. 2010;16 doi: 10.3201/eid1604.090719. [DOI] [PubMed] [Google Scholar]
- 24.Oyo-Ita A., Wiysonge C.S., Oringanje C., Nwachukwu C.E., Oduwole O., Meremikwu M.M. Interventions for Improving Coverage of Childhood Immunisation in Low- and Middle-income Countries. Cochrane Database Syst. Rev. 2016 doi: 10.1002/14651858.CD008145.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization First Large Scale Maternal and Child Health Campaign Underway after End of Ebola Outbreak in Sierra Leone. [(accessed on 24 November 2021)]. Available online: https://www.afro.who.int/news/first-large-scale-maternal-and-child-health-campaign-underway-after-end-ebola-outbreak-sierra.
- 26.Usman H.R., Akhtar S., Habib F., Jehan I. Redesigned Immunization Card and Center-Based Education to Reduce Childhood Immunization Dropouts in Urban Pakistan: A Randomized Controlled Trial. Vaccine. 2009;27:467–472. doi: 10.1016/j.vaccine.2008.10.048. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to participant’s privacy.