Introduction
Extramammary Paget disease (EMPD) is a cutaneous malignancy that occurs predominately on apocrine gland-containing skin such as the anogenital area and axilla. Primary EMPD involving more than 1 site, known as double and triple EMPD, is very rare with most cases reported in the Japanese literature.1, 2, 3, 4 We present a case of primary multisite EMPD in a Caucasian man with involvement of the axilla, scrotum, and perineum following an extensive negative diagnostic workup for underlying malignancy. This case highlights the importance of recognizing multisite EMPD as an entity in order to avoid misdiagnosis and promote earlier detection of this disease.
Case report
A 79-year-old man presented to our Mohs micrographic surgery department with a 3-year history of scaling, erythematous plaques in the groin. There was no known family history of skin or systemic malignancy. A previous surgical excision at an outside facility revealed EMPD of the scrotum with a component of invasive moderately-differentiated adenocarcinoma involving the lateral margins.
A full skin examination was performed. There was faint erythema of the scrotum and inguinal folds, with well-healed surgical scars. A 2-cm erythematous, scaling plaque was noted on the right axilla (Fig 1). He had been treating the axillary lesion with topical triamcinolone without improvement. There was no palpable lymphadenopathy. A biopsy from the right side of the axilla, as well as scouting biopsies of the inguinal folds, perineum, and scrotum were performed for surgical mapping (Fig 2) and were histologically consistent with EMPD (Fig 3). Extensive malignancy screening, including computed tomography (chest/abdomen/pelvis), positron emission tomography, cystoscopy, prostate-specific antigen, urinalysis, urine cytology, carcinoembryonic antigen, esophagogastroduodenoscopy, mammography, and colonoscopy, was unrevealing for underlying malignancy or metastatic disease. He was diagnosed with primary, multisite EMPD.
Fig 1.
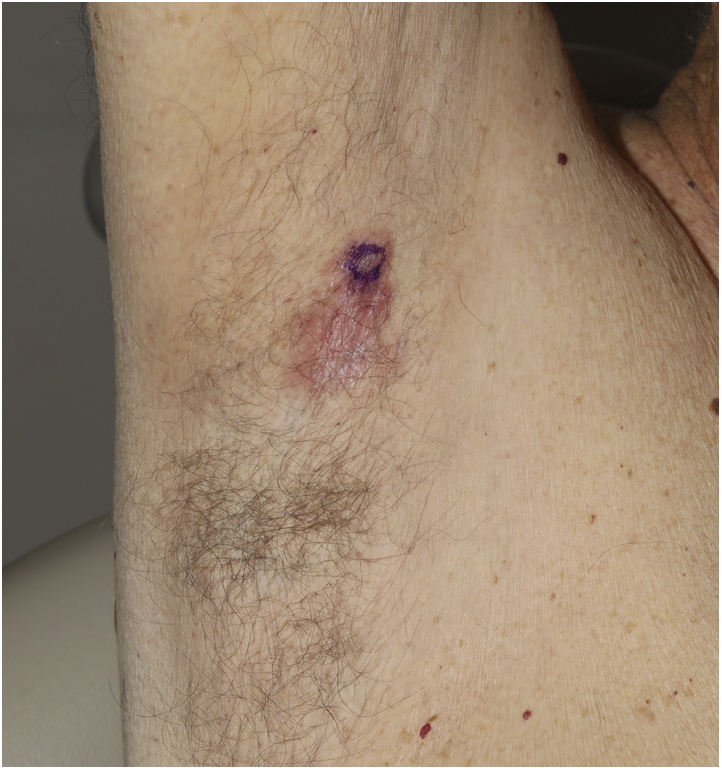
Extramammary Paget disease of the axilla: Erythematous scaly plaque with erosions on the right axilla incidentally noted during full skin examination. The biopsy site was marked at the superior aspect.
Fig 2.

Extramammary Paget disease of the scrotum and perineum: Erythematous scaly patches. Purple marker depicts the location of scouting biopsies.
Fig 3.
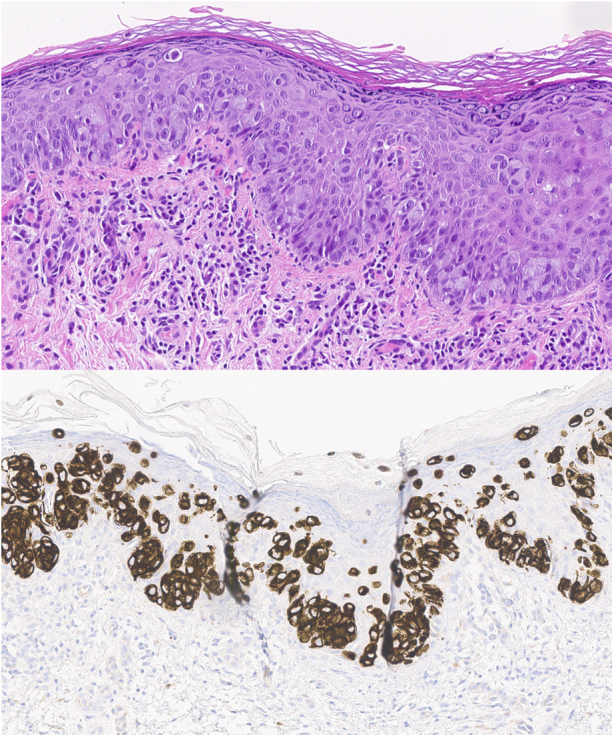
Extramammary Paget disease. Upper panel, Histopathology from the right axillary biopsy shows Paget cells with abundant pale cytoplasm and large nuclei lined above the dermoepidermal junction percolating up through the epidermis in a “buckshot scatter” pattern (hematoxylin-eosin stain; original magnification: ×20). Lower panel, Immunohistochemistry stain depicting the same malignant cells with uniform positivity for cytokeratin 7. Stains for CD20 and CDX2 were notably negative (cytokeratin 7 stain; original magnification: ×20)
Given the presence of invasive disease on initial biopsy, we opted to proceed with definitive surgical resection rather than nonsurgical therapy, with staged surgical excision of the groin and axilla with complete circumferential peripheral and deep margin assessment. This was performed in conjunction with urology. The groin and axilla sites both required 2 stages over the course of 2 days to obtain clear peripheral margins. In the first layer from the axilla, there was moderately-differentiated adenocarcinoma arising from a background of EMPD involving the deep margin. No invasive component was identified from the scrotum/inguinal folds, but peripheral margins were initially involved. The final peripheral clinical margins were 2.0 cm. The following day, he underwent extirpation of the central island of tissue on the scrotum with urology in the operating room. The perineal and scrotal skin was dissected along the adipose tissue plane with sparing of the tunica vaginalis and dartos (Fig 4). The area was then dressed and left to heal by secondary intention. The deep margins were clear. Four weeks later, he met with plastic surgery to discuss options for reconstruction and ultimately decided to allow the sites to heal through second intention. He will continue frequent clinical followup with his local dermatologist.
Fig 4.

Staged excision of Extramammary Paget disease: Scrotum and perineum following extirpation of the central island of skin after obtaining clear peripheral margins. Deep margins were free of malignancy.
Discussion
Due to its rarity, the exact incidence of EMPD is unknown. Single-site disease most commonly affects Caucasian females, but cases of double and triple EMPD have been reported predominantly in Asian males. According to Van Hamme et al5 and other previous literature reviews, there have been a total of 28 reported cases from Japan prior to 2002. Since then, our review of the literature identified 9 additional cases with only 1 case report of triple EMPD from Belgium and 1 from the United States, although the latter did not specify race and ethnicity.2, 3, 4, 5, 6, 7, 8
EMPD is characteristically slow growing, and clinical features include pink or white scaly ulcerated plaques often described as “strawberries and cream.”9 The pathogenesis of primary EMPD is not well understood but has been thought to arise from pluripotent intraepithelial or adnexal cells. Toker cells, which are mammary gland-related cells, have also been implicated as a precursor.9 Common diagnostic pitfalls are plentiful and include dermatophytosis, chronic dermatitis, inverse psoriasis, and intertrigo. Biopsy is essential for diagnosis, which typically reveals large cells with abundant amphophilic cytoplasm in a “buckshot scatter” throughout the epidermis. Immunohistochemistry can be helpful as Paget cells are usually positive for both cytokeratin 7 and epithelial membrane antigen. Cytokeratin 20 is typically positive in secondary EMPD and negative in primary EMPD.
Diagnostic workup for underlying malignancy is important because EMPD can be secondary to intraepithelial extension of an underlying malignancy, most commonly from the prostate, urinary tract, or breast.9 A recent review article reported the incidence of intraepithelial extension as 4% to 58%.9 A broad panel of immunohistochemical stains to rule out prostate, urinary tract, and breast primary adenocarcinomas is typically utilized during the investigation. In addition, screening should include a complete review of systems, full skin examination, clinical lymph node examination, and pelvic examination. The clinician should also consider additional studies such as imaging, cystoscopy, urinalysis, urine cytology, prostate-specific antigen, colonoscopy, mammography, and serum carcinoembryonic antigen for invasive cases.
Treatment of EMPD is challenging because of its ill-defined clinical margins, which leads to high recurrence rates. When available, Mohs micrographic surgery with cytokeratin 7 immunostains or staged excision with complete circumferential peripheral and deep margin assessment are the gold standards of treatment and associated with lower recurrence rates versus standard excision.9 The treatment options that have been described include wide local excision6,7 and nonsurgical options such as radiotherapy,5 topical imiquimod,10 and systemic chemotherapy for advanced or metastatic disease.1
Conclusion
EMPD is a challenging disease to treat due to high rates of recurrence and subsequent morbidity. Early detection is important to minimize surgical morbidity and prompt screening for an underlying internal malignancy. We report a unique case of a Caucasian man in the United States with known genital EMPD, who was subsequently diagnosed with axillary involvement of EMPD. This contributes to the current and evolving understanding of multisite EMPD and requires the clinician to maintain a high level of suspicion to avoid misdiagnoses and allow earlier diagnosis and treatment.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Inui S., Fukuhara S., Asada H., Tadokoro T., Yoshikawa K., Itami S. Double involvement of extramammary Paget's disease in the genitalia and axilla. J Dermatol. 2000;27(6):409–412. doi: 10.1111/j.1346-8138.2000.tb02194.x. [DOI] [PubMed] [Google Scholar]
- 2.Hatta N., Yamada M., Hirano T., Fujimoto A., Morita R. Extramammary Paget's disease: treatment, prognostic factors and outcome in 76 patients. Br J Dermatol. 2008;158(2):313–318. doi: 10.1111/j.1365-2133.2007.08314.x. [DOI] [PubMed] [Google Scholar]
- 3.Ohnishi T., Shibuya S., Nemoto I., et al. Evidence from mucin core protein expression that some Paget's disease on areola can be of extramammary-like histogenesis and part of multisite disease. Br J Dermatol. 2004;151(3):688–692. doi: 10.1111/j.1365-2133.2004.06087.x. [DOI] [PubMed] [Google Scholar]
- 4.Takahashi N., Hirabayashi M., Hoashi T. Double extramammary Paget disease of both the umbilicus and scrotum. Dermatol Surg. 2016;42(3):436–438. doi: 10.1097/DSS.0000000000000611. [DOI] [PubMed] [Google Scholar]
- 5.Van Hamme C., Marot L., Dachelet C., Dumont M., Salamon E., Lachapelle J.M. Paget's extramammary disease of the axillae and perineum. Article in French. Ann Dermatol Venereol. 2002;129(5 Pt 1):717–719. [PubMed] [Google Scholar]
- 6.Li B., Ding Q. Extramammary Paget's disease involving the penis, scrotum and the axilla. Australas J Dermatol. 2011;52(1):e18–e20. doi: 10.1111/j.1440-0960.2009.00619.x. [DOI] [PubMed] [Google Scholar]
- 7.Leelavathi M., Norazirah M.N., Nur Amirah A.P. Multiple concurrent primary extramammary Paget's disease. Malays Fam Physician. 2016;11(1):18–21. [PMC free article] [PubMed] [Google Scholar]
- 8.Wolf K., Stewart L., Rapini R., Mutyambizi K. Multifocal extramammary Paget's disease-associated adenocarcinoma: a rare condition of flexoral skin of multiple sites. Dermatol Online J. 2016;22(1) 13030/qt8bp3138w. [PubMed] [Google Scholar]
- 9.Asel M., LeBoeuf N.R. Extramammary Paget's disease. Hematol Oncol Clin North Am. 2019;33(1):73–85. doi: 10.1016/j.hoc.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Green J.S., Burkemper N.M., Fosko S.W. Failure of extensive extramammary Paget disease of the inguinal area to clear with imiquimod cream, 5%: possible progression to invasive disease during therapy. Arch Dermatol. 2011;147(6):704–708. doi: 10.1001/archdermatol.2011.121. [DOI] [PubMed] [Google Scholar]


