Abstract
Background:
Ethical discourse in the scientific community facilitates the humane conduct of research. The urgent response to COVID-19 has rapidly generated a large body of literature to help policymakers and physicians address novel pandemic challenges. Plastic surgeons, in particular, have to manage the postponement of elective procedures and safely provide care for non–COVID-19 patients. Although COVID-19 research may provide guidance on these challenges, the extent to which ethical discussions are present in these publications remains unknown.
Methods:
Articles were identified systematically by searching the PubMed, Embase, Central, and Scopus databases using search terms related to ethics and COVID-19. The search included articles published during the first 9 months of the COVID-19 pandemic. The following data were extracted: presence of an ethical discussion, date of publication, topic of ethical discussion, and scientific discipline of the article.
Results:
One thousand seven hundred fifty-three articles were included, of which seven were related to plastic surgery. The ethical principle with the greatest representation was nonmaleficence, whereas autonomy had the least representation. Equity and access to care was the most common topic of ethical discussion; the mental health effects of COVID-19 were the least common. The principle of justice had the greatest variation in representation.
Conclusions:
In a systematic review of COVID-19–related articles that were published during the first 9 months of the pandemic, the ethical principles of autonomy and justice are neglected in ethical discussions. As ethical dilemmas related to COVID-19 remain prevalent in plastic surgery, attention to ethical discourse should remain a top priority for leaders in the field.
The COVID-19 pandemic presented policymakers and hospital administration with numerous ethical dilemmas, including rationing of medical supplies, delaying nonemergent surgery, and staggering the distribution of vaccines to vulnerable populations.1,2 Plastic surgeons cancelled procedures to preserve resources, supplies, and physicians in an effort to curtail the spread of COVID-19.3 Cosmetic procedures, both surgical and minimally invasive, declined by approximately 15 percent in 2020 compared to 2019.4 Leaders empowered with fulfilling these responsibilities did not have clear definitions of “elective and nonessential” procedures, and were left to decide which services should be restricted, leading to variable access to care across the country.5 To respond to these and other novel challenges, policymakers and physicians look to COVID-19 research to assist with their decisions and management of the pandemic within their clinic, hospital, and community. As the pandemic continues, complicated by the return of previously postponed activities, it is critical that ethical considerations are articulated alongside new discoveries and guidelines.
Rapid publication of high-quality research was essential for the development of effective therapeutics and vaccines in the fight against COVID-19. However, the urgency to study COVID-19 and its effects must be balanced with the obligation of researchers to adhere to high ethical standards and consider the moral implications of research findings. In the United States, biomedical ethics is based on the moral theory of principlism, established by Beauchamp and Childress in 1979. They established four ethical principles: respect for autonomy, beneficence, nonmaleficence, and justice. Table 1 describes each principle and presents corresponding examples.6 Given the urgency for COVID-19 research and the novel ethical dilemmas faced by health care systems and policymakers worldwide, recognizing and discussing the ethical implications of COVID-19 research is critical.
Table 1.
Definitions and Examples of the Ethical Principles Defined by Beauchamp and Childress*
| Principles | Definition | Examples |
|---|---|---|
| Respect for autonomy | Respecting the decision-making capacities of autonomous persons | Informed consent; respecting the freedom of privacy and confidentiality during COVID-19 tracing; transparent communication of risks and benefits of procedures or treatments; transparent communication of risks of elective surgery during COVID-19 surges |
| Nonmaleficence | Avoiding the causation of harm | Providing innovative COVID-19 treatment only when appropriate and in accordance with guidelines; avoiding undue risk by considering individual risks before performing elective surgery; preventing COVID-19 exposure or risk of spread during care |
| Beneficence | Providing benefits and balancing benefits against risks and costs | Providing care to patients with aim to benefit them and without undue risk; consideration of all treatment options and weighing of risks and benefits of each; identification of potential adverse events for novel treatments |
| Justice | Distributing benefits, risks, and costs fairly | Offering equal access to available resources to all patients; ensuring fair allocation of scare resources; providing fair access to care to all populations and minimizing unequal treatment; respecting individual legal and human rights |
*Adapted from Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 8th ed. New York: Oxford University Press; 2019.
We aim to quantify the prevalence of ethical discussions and representation of the four ethical principles in COVID-19 research, and to identify which principles and topics are underrepresented across scientific disciplines. Given the rapid publishing rate and urgent need for guidance, we hypothesize that ethical considerations will be neglected in certain domains. We also hypothesize that original research articles, which will need to consider participant safety and informed consent, will most frequently discuss the principle of autonomy.
PATIENTS AND METHODS
Search Strategy
We performed a systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.7 We searched the PubMed, Embase, Central, and Scopus databases for articles related to COVID-19. A medical librarian assisted in developing the search strategy. Search terms included those related to principlism and SARS-CoV-2 (COVID-19). (See Appendix, Supplemental Digital Content 1, which shows the search strategy, http://links.lww.com/PRS/F32.) Only articles published from January 1, 2020, to September 30, 2020, were considered, as the unidentified pneumonia outbreak in Wuhan was first reported to the World Health Organization on December 31, 2019.8 We included original and nonoriginal research. Nonoriginal research articles were defined as reviews, editorials/commentaries, letters to the editor, position papers/guidelines, and correspondences.
Screening and Data Extraction
The titles and abstracts were uploaded to Rayyan, a systematic review software, for initial evaluation.9 Three independent reviewers (A.V.S., S.M.W., and R.L.K.) screened the articles, and disagreement was resolved through discussion among reviewers. We excluded articles that were not explicitly connected to COVID-19 or did not directly relate to or impact humans. This included laboratory studies or basic research that did not involve humans. Furthermore, included articles needed a sufficient ethical discussion, which we defined as having a subheading related to an ethical issue or at least one paragraph dedicated to the discussion of ethical principles.
Full-text articles were obtained of the remaining articles. Three reviewers (A.V.S., S.M.W., and Noreen F. Khan) independently extracted article characteristics using Microsoft Excel (Microsoft Corp., Redmond, Wash.). The following variables were collected: presence of an ethical discussion, month published, type of article, ethical principles discussed (autonomy, beneficence, nonmaleficence, justice), topic of ethical discussion, and scientific discipline. “Topic of ethical discussion” referred to the central ethical issues discussed in the article. We retrospectively categorized each article into one of several scientific disciplines: surgery, social sciences, public health, internal medicine and critical care, clinical research during COVID-19, pharmacology/treatments, obstetrics and gynecology and reproductive health, and psychiatry and behavioral sciences. Any disagreements were discussed and resolved among the reviewers. A spreadsheet was used to calculate the frequencies of ethical principles, article characteristics, ethical topics, scientific disciplines, and number of articles published per month. Subgroup analyses were conducted for these characteristics to identify variation in ethical principle representation.
RESULTS
Characteristics of Included Studies
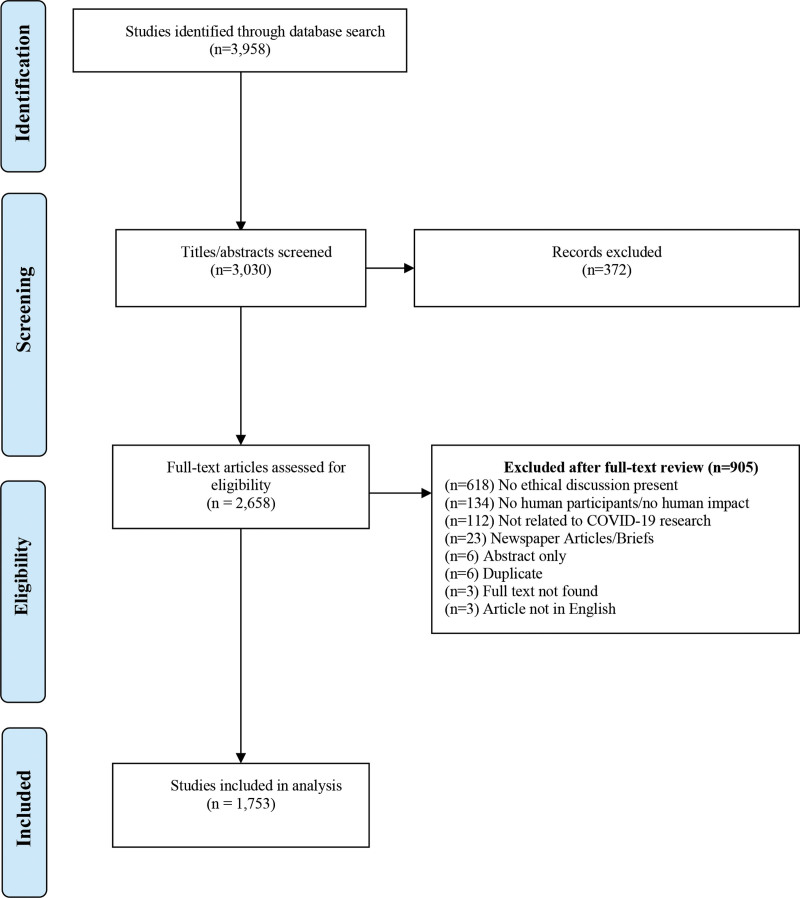
A total of 3958 articles were identified in the initial search; 2658 were included after abstract and title screening. The full texts of the remaining 2658 articles were further evaluated, with 1753 articles remaining for analysis after applying inclusion and exclusion criteria (Fig. 1). Nonoriginal [n = 1455 (83 percent)] research made up the majority of included articles compared to original research [n = 298 (17 percent)] articles. Editorials [n = 674 (46 percent)] and cross-sectional [n = 85 (29 percent)] studies were the most common type of nonoriginal and original research articles, respectively. The majority of the research articles, original and nonoriginal, were related to public health [n = 630 (36 percent)] and internal medicine specialties and critical care [n = 531 (30 percent)]. The remaining articles were distributed relatively evenly across the other scientific disciplines, except for treatments [n = 66 (4 percent)]. The most frequently discussed ethical topic was decision-making and resource allocation, which was the central focus of 488 articles (n = 27 percent) (Table 2). Finally, COVID-19 research reached peak publication during the month of June (n = 436).
Fig. 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of included studies. (From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 2009;6:e1000097.)
Table 2.
Article Characteristics
| Characteristics | No. | % |
|---|---|---|
| Article type | ||
| Nonresearch | 1455 | 83.0 |
| Original research | 298 | 17.0 |
| Types of original research | ||
| Cross-sectional | 85 | 28.5 |
| Case study/series | 67 | 22.5 |
| Retrospective cohort | 46 | 15.4 |
| Mixed methods | 29 | 9.7 |
| Model/simulation | 21 | 7.1 |
| Prospective cohort | 18 | 6.0 |
| Systematic review | 13 | 4.4 |
| Content analysis | 10 | 3.4 |
| Meta-analysis | 7 | 2.3 |
| RCT | 2 | 0.7 |
| Types of nonresearch | ||
| Editorial/commentary | 674 | 46.3 |
| Position/guidelines | 372 | 25.6 |
| Review | 239 | 16.4 |
| Letter to editor | 118 | 8.1 |
| Correspondence | 52 | 3.6 |
| Scientific disciplines | ||
| Public health | 630 | 36.0 |
| Internal medicine specialties and critical care | 531 | 30.3 |
| Social sciences | 155 | 8.8 |
| Surgery | 110 | 6.3 |
| Clinical research during COVID-19 | 104 | 5.9 |
| Psychiatry and behavioral sciences | 101 | 5.7 |
| Treatments | 66 | 3.8 |
| Obstetrics/gynecology and reproductive health | 56 | 3.2 |
| Topics* | ||
| Decision-making and resource allocation | 488 | 27.8 |
| Equity and access to care | 381 | 21.7 |
| Rights of patients and essential workers | 341 | 19.5 |
| Minimizing COVID-19 exposure | 210 | 12.0 |
| COVID-19 diagnosis, treatments, and complications | 178 | 10.2 |
| Communication and informed consent | 162 | 9.2 |
| Mental health effects of COVID-19 | 48 | 2.7 |
RCT, randomized controlled trial.
This percentage will not equal 100 percent as an article may represent multiple topics.
Representation of Ethical Principles
Of the 1753 articles included, nonmaleficence was the most common ethical principle [n = 922 (53 percent)], followed by beneficence [n = 854 (49 percent)], justice [n = 790 (45 percent)], and autonomy [n = 172 (10 percent)]. This pattern held true for most scientific disciplines, including general surgery and public health. Although plastic surgery constituted a small percentage of the total articles [n = 7 (0.4 percent)], a similar trend in representation of ethical principles was observed. Of the 1753 included articles, 170 (10 percent) contained an ethical discussion that considered all four ethical principles. Table 3 provides an in-depth review of the representation of ethical principles across study types. Beneficence was the most common principle across original research, whereas nonmaleficence was the most common across nonoriginal research. Autonomy remained the least discussed ethical principle by a relatively large margin for both original and nonoriginal research, and across all scientific disciplines (Tables 4 and 5). Nonmaleficence and beneficence were commonly discussed in all fields, whereas the representation of justice varied across disciplines. For instance, justice was discussed in only 11 percent of articles related to treatments, whereas beneficence was represented in 89 percent of treatment articles. Similar to the ethical representation across scientific disciplines, autonomy was substantially underrepresented across ethical topics (Table 6).
Table 3.
Overall Ethical Principle Representation
| Ethical Principle | No. | % |
|---|---|---|
| All | 170 | 9.7 |
| Autonomy | 172 | 9.8 |
| Beneficence | 854 | 48.7 |
| Nonmaleficence | 922 | 52.6 |
| Justice | 790 | 45.0 |
Table 4.
Representation of Primary Ethical Principles per Article Type
| Article Type | Overall | All Principles | Autonomy | Beneficence | Nonmaleficence | Justice |
|---|---|---|---|---|---|---|
| Original research | 298 | 6 | 11 | 173 | 142 | 65 |
| Cross-sectional | 85 | 1 | 6 | 43 | 39 | 28 |
| Case study/series | 67 | 1 | 3 | 37 | 38 | 2 |
| Retrospective cohort | 46 | 1 | 1 | 33 | 16 | 5 |
| Mixed methods | 29 | 1 | 1 | 17 | 16 | 16 |
| Model/simulation | 21 | 0 | 0 | 13 | 9 | 6 |
| Prospective cohort | 18 | 0 | 0 | 9 | 9 | 3 |
| Systematic review | 13 | 0 | 0 | 9 | 7 | 4 |
| Content analysis | 10 | 1 | 0 | 6 | 5 | 1 |
| Meta-analysis | 7 | 1 | 0 | 4 | 2 | 0 |
| RCT | 2 | 0 | 0 | 2 | 1 | 0 |
| Nonresearch | 1455 | 164 | 162 | 680 | 780 | 725 |
| Editorial/commentary | 674 | 84 | 86 | 279 | 337 | 372 |
| Position/guidelines | 372 | 40 | 48 | 211 | 220 | 181 |
| Review | 239 | 28 | 16 | 122 | 132 | 95 |
| Letter to editor | 118 | 11 | 10 | 44 | 55 | 54 |
| Correspondence | 52 | 1 | 2 | 24 | 36 | 23 |
| Total | 1753 | 170 | 173 | 853 | 922 | 790 |
RCT, randomized controlled trial.
Table 5.
Ethical Representation of Scientific Disciplines
| Scientific Disciplines | Total | All Principles | Autonomy | Beneficence | Nonmaleficence | Justice | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | No. | % | No. | % | No. | % | No. | % | No. | % | |
| Public health | 630 | 51 | 8.1 | 69 | 11 | 268 | 42.5 | 288 | 45.7 | 332 | 52.7 |
| Internal medicine specialties and critical care | 531 | 57 | 10.7 | 38 | 7.2 | 304 | 57.3 | 323 | 60.8 | 159 | 29.9 |
| Social sciences | 155 | 15 | 9.7 | 18 | 11.6 | 52 | 33.6 | 64 | 41.3 | 120 | 77.4 |
| Surgery | 110 | 10 | 9.1 | 11 | 10 | 46 | 41.8 | 83 | 75.5 | 32 | 29.1 |
| Clinical research during COVID-19 | 104 | 16 | 15.4 | 14 | 13.5 | 57 | 54.8 | 59 | 56.7 | 36 | 34.6 |
| Psychiatry and behavioral sciences | 101 | 9 | 8.9 | 12 | 11.9 | 52 | 51.5 | 48 | 47.5 | 54 | 53.5 |
| Treatments | 66 | 6 | 9.1 | 3 | 4.5 | 59 | 89.4 | 32 | 48.5 | 7 | 10.6 |
| Obstetrics/gynecology and reproductive health | 56 | 9 | 16.1 | 10 | 17.9 | 19 | 33.9 | 28 | 50 | 21 | 37.5 |
Table 6.
Principle Representation of Ethical Topics
| Ethical Topics | Total | All Principles | Autonomy | Beneficence | Nonmaleficence | Justice | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | No. | % | No. | % | No. | % | No. | % | No. | % | |
| Decision-making and resource allocation | 488 | 61 | 13 | 125 | 26 | 204 | 41.8 | 207 | 42.4 | 181 | 52.7 |
| Equity and access to care | 381 | 40 | 11 | 70 | 18 | 162 | 42.5 | 178 | 46.7 | 111 | 29.9 |
| Rights of patients and essential workers | 341 | 42 | 12 | 127 | 37 | 140 | 41.1 | 136 | 39.9 | 306 | 77.4 |
| Minimizing COVID-19 exposure | 210 | 21 | 10 | 26 | 12 | 113 | 53.8 | 155 | 73.8 | 52 | 29.1 |
| COVID-19 diagnosis, treatments, and complications | 178 | 6 | 3.4 | 35 | 20 | 100 | 56.2 | 88 | 49.4 | 153 | 34.6 |
| Communication and informed consent | 162 | 15 | 9.3 | 62 | 38 | 83 | 51.2 | 77 | 47.5 | 66 | 53.5 |
| Mental health effects of COVID-19 | 48 | 4 | 8.3 | 16 | 33 | 20 | 41.7 | 22 | 45.8 | 22 | 10.6 |
DISCUSSION
The four principles of bioethics, first described by Beauchamp and Childress, provide a framework for ethical considerations and facilitate the ethical conduct of research.6 Our study aimed to identify the prevalence and distribution of these ethical principles in research publications related to COVID-19; to our knowledge this had not yet been studied. In addition, we determined which topics of ethical discussions have the greatest representation across various scientific disciplines. Among ethical discussions in the COVID-19 literature, we found that the principle of autonomy was neglected across numerous scientific disciplines. Early COVID-19 research focused on epidemiology and public health interventions, with the goal of reducing exposure to the virus, saving lives, and ultimately preventing harm.2,10 Therefore, it is reasonable that our study showed that the majority of COVID-19–related articles published in the first 9 months of the pandemic framed ethical discussions around the principle of nonmaleficence. This goal of reducing exposure and preventing harm is relevant to all specialties as procedures are rescheduled and physicians are deployed to assist with COVID-19 surges.11 Articles related to plastic surgery demonstrated a similar pattern, although only seven articles related to the specialty were identified. Discussions of ethical issues in plastic surgery related to the COVID-19 pandemic included decision-making and resource allocation, equity and access to care, and minimizing COVID-19 exposure. This remarkably low subset of articles in plastic surgery indicates the urgent need for increased research and guidance for plastic surgeons to navigate ethical dilemmas related to the ongoing pandemic.
Although it may be necessary to postpone elective procedures to increase resource availability for COVID-19 patients, it is also critical to ensure that non–COVID-19 patients are not suffering from inadequate treatment. Elective procedures in plastic surgery can reduce discomfort and increase quality of life, and in some health care systems plastic surgery accounts for the largest proportion of elective cases across subspecialties.12 With no end in sight of the current pandemic, it may be impractical to continue cancelling all nonemergent procedures when COVID-19 cases surge; rather, physicians and patients may work together to find new solutions to safely provide elective care. This may be accomplished by adopting a standardized and explicit definition of all procedures that are considered “elective” and creating a strategy to continuously weigh the risk and benefit of providing nonemergent surgery during the COVID-19 pandemic. This strategy may be guided by all four ethical principles; for example, Brown et al. developed a triage algorithm for delivering surgical care during the COVID-19 pandemic that maintained the goal of prioritizing beneficence and nonmaleficence, while respecting patient autonomy and justice.13 This was accomplished by adapting an existing triage protocol, which focused primarily on procedure type and risk factors, to account for local variability in resources and disease burden to improve justice. Furthermore, these authors recognize the challenge of preserving autonomy when individual decision-making may impact the safety of others. They suggest respecting autonomy by giving patients the decision not to receive care, reducing strain on their health care system.13 Although each health care and hospital system is unique, a similar algorithm may be used to ensure that elective care decisions are ethical and consider the complexities of COVID-19.
Postponing elective procedures, such as gender-affirming surgery, can adversely impact patient mental health and well-being.14 Marginalized groups, such as lesbian, gay, bisexual, transgender, and queer or questioning populations, face worse mental health disparities and disproportionate effects of COVID-19.14 In addition to affecting vulnerable individuals, COVID-19 has worsened existing mental health conditions and increased anxiety and depressive symptoms in those without previous mental health conditions.15 It is therefore concerning that mental health effects of COVID-19 was the least represented ethical topic. In January of 2021, approximately four in 10 adults in the United States reported symptoms of anxiety or depressive disorder, up from one in 10 during 2019.15 Furthermore, it has been reported that an additional 75,000 deaths could result from alcohol and drug abuse during COVID-19.16 Despite the known impacts of COVID-19 on mental health, much of the related discourse is dedicated to describing the problem rather than proposing concrete intervention methods.17 Some researchers have attempted to minimize the mental health effects for these vulnerable populations. For example, Drabble and Eliason advocate for the recategorization of gender-affirming care as nonelective to ensure access to therapy, hormones, and treatment during the pandemic.18 Other researchers have developed an app designed to target emotional skills, healthy lifestyle behavior, burnout, and social support for health care workers.19 Mental health challenges will continue after the pandemic has subsided; it is necessary that research confronts this and determines interventions that can mitigate these effects.
COVID-19 is the first pandemic in which social media played a central role in the spread of information, which introduced the novel challenge of an “infodemic” of misinformation.20 This infodemic is associated with reduced public compliance with safety measures, such as social distancing or vaccinations.20 Even brief exposure to vaccine-critical websites has been shown to heighten the perception of vaccine risk.21 In addition, many individuals are spending more time on social media during COVID-19.22 These individuals are at a greater risk of being exposed to misinformation and the associated negative effects. Physicians have a responsibility to avoid contributing to the spread of misinformation and directly address COVID-19 inaccuracies. Plastic surgeons—many of whom are active on social media—may be in a unique position to promote awareness of evidence-based COVID-19 information for their followers. All physicians, regardless of specialty, can use their platform to influence COVID-19 messaging by encouraging vaccination, promoting updated mask and distancing policies, and addressing false beliefs. By replacing misinformation with neutral, evidence-based facts, providers can ensure that patient decision-making remains rooted in the best available evidence.
The principle of justice was largely underrepresented in original research and articles related to COVID-19 treatments, appearing in 77 percent of social science articles but only 11 percent of COVID-19 treatment–related articles. As treatments are better understood for their effectiveness and safety, a greater emphasis should be placed on resolving unequal access to care and improving outcomes in these populations. COVID-19 exacerbated existing inequities among minority groups and contributed to worse outcomes for people of color.23 Other factors such as discrimination, access to care, and housing conditions impact individuals’ exposure to COVID-19 and quality of treatment.24 The Centers for Disease Control and Prevention recognized the effect of social factors on health outcomes and created the Social Vulnerability Index to identify communities that may need support before, during, or after disasters. Originally developed to guide decision-making in natural disasters, the Social Vulnerability Index has been adapted to include COVID-19 metrics.25,26 Similar initiatives can be used to continue this collaborative effort in areas such as treatment allocation and access to care. Fair distribution of essential resources and treatments can help to improve overall COVID-19 outcomes, especially for the most vulnerable individuals.
This study has several limitations. Although multiple databases were included, fewer than expected original research articles were retrieved. One reason may be the timing of the search, which ended in September of 2020. Between January and July of 2020, 44,013 articles on COVID-19 had been published; this number increased to 87,515 by September of 2020.27 Nevertheless, it is worthwhile to determine the representation of ethical principles in COVID-19 research at the start of the pandemic, as this is a critical time for information spread. Another limitation is the use of principlism as our guiding framework for evaluating ethical discussions. Although this framework is routinely applied to bioethics, alternative frameworks such as narrative ethics, which prioritizes the history and desires of an individual throughout the decision-making process, have been cited as being more useful in a clinical setting.28 Therefore, articles that interpreted ethical dilemmas in other frameworks may have been excluded from our search, which focused specifically on the theory of principlism.
CONCLUSIONS
As the COVID-19 pandemic persists, new ethical dilemmas in health care continue to emerge. We found that several ethical issues, such as resource allocation and access to care, were addressed across a variety of specialties; however, there are gaps in the literature that require additional attention. Now that the management of COVID-19 has improved and multiple vaccines exist, increased focus should be given to topics such as mental health effects and postponement of elective care, which remain relevant after immediate concern for the virus has decreased. Furthermore, prioritizing research of known vulnerable populations, such as children and minority groups, can support the principle of justice in the public health response. As new COVID-19 variants emerge and novel challenges remain unresolved, policymakers and physicians can improve their responses by approaching all research and care with an ethical, evidence-based focus.
Supplementary Material
Footnotes
Related digital media are available in the full-text version of the article on www.PRSJournal.com.
Disclosure: Dr. Chung receives funding from the National Institutes of Health and book royalties from Wolters Kluwer and Elsevier. The remaining authors have no financial interests to report.
REFERENCES
- 1.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. [DOI] [PubMed] [Google Scholar]
- 2.Harkin DW. Ethics for surgeons during the COVID-19 pandemic, review article. Ann Med Surg (Lond.) 2020;55:316–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hollier LH, Jr, Tanna N, Kasabian AK, et al. The COVID-19 pandemic: Crisis management for plastic surgeons. Plast Reconstr Surg. 2020;146:1197–1206. [DOI] [PubMed] [Google Scholar]
- 4.American Society of Plastic Surgeons. American Society of Plastic Surgeons unveils COVID-19’s impact and pent-up patient demand fueling the industry’s current post-pandemic boom. Available at: https://www.plasticsurgery.org/news/press-releases/american-society-of-plastic-surgeons-unveils-covid19s-impact-and-pent-up-patient-demand-fueling-the-industrys-current-post-pandemic-boom. Accessed September 8, 2021
- 5.Stuart B. How the COVID-19 pandemic has affected provisions of elective services: The challenges ahead. Health Affairs Blog. October 8, 2020. Available at: https://www.healthaffairs.org/do/10.1377/forefront.20201006.263687/full/. Accessed September 8, 2021. [Google Scholar]
- 6.Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 8th ed. New York: Oxford University Press; 2019. [Google Scholar]
- 7.Moher D, Shamseer L, Clarke M, et al.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allam Z. The first 50 days of COVID-19: A detailed chronological timeline and extensive review of literature documenting the pandemic. In: Surveying the Covid-19 Pandemic and Its Implications: Urban Health, Data Technology and Political Economy. Amsterdam: Elsevier Science; 2020:1–7. [Google Scholar]
- 9.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan: A web and mobile app for systematic reviews. Syst Rev. 2016;5:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang J, Hong N. The COVID-19 research landscape: Measuring topics and collaborations using scientific literature. Medicine (Baltimore) 2020;99:e22849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar SI, Borok Z. Filling the bench: Faculty surge deployment in response to the Covid-19 pandemic. N Engl J Med Catalyst. October 29, 2020. Available at: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0511. Accessed March 17, 2022. [Google Scholar]
- 12.Berman ZP, Diep GK, Alfonso AR, et al. Plastic surgery amidst the pandemic: The New York University experience at the epicenter of the COVID-19 crisis. Plast Reconstr Surg. 2021;148:133e–139e. [DOI] [PubMed] [Google Scholar]
- 13.Brown NJ, Wilson B, Szabadi S, et al. Ethical considerations and patient safety concerns for cancelling non-urgent surgeries during the COVID-19 pandemic: A review. Patient Saf Surg. 2021;15:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kidd JD, Jackman KB, Barucco R, et al. Understanding the impact of the COVID-19 pandemic on the mental health of transgender and gender nonbinary individuals engaged in a longitudinal cohort study. J Homosex. 2021;68:592–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Panchal NRK, Cynthia C, Garfield R; Kaiser Family Foundation. The implications of COVID-19 for mental health and substance use. Available at: https://www.kff.org/coronavirus-covid-19/issue-brief/the-implications-of-covid-19-for-mental-health-and-substance-use/. Accessed June 5, 2021
- 16.Well Being Trust. Projected deaths of despair during COVID-19. Available at: https://wellbeingtrust.org/wp-content/uploads/2020/05/WBT_Deaths-of-Despair_COVID-19-FINAL-FINAL.pdf. Accessed June 5, 2021.
- 17.Gilbody S, Littlewood E, Gascoyne S, et al. Mitigating the impacts of COVID-19: Where are the mental health trials? Lancet Psychiatry 2021;8:647–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drabble LA, Eliason MJ. Introduction to special issue: Impacts of the COVID-19 pandemic on LGBTQ+ health and well-being. J Homosex. 2021;68:545–559. [DOI] [PubMed] [Google Scholar]
- 19.Fiol-DeRoque MA, Serrano-Ripoll MJ, Jiménez R, et al. A mobile phone-based intervention to reduce mental health problems in health care workers during the COVID-19 pandemic (PsyCovidApp): Randomized controlled trial. JMIR Mhealth Uhealth 2021;9:e27039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Managing the COVID-19 infodemic: Promoting healthy behaviors and mitigating the harm from misinformation and disinformation. Available at: https://www.who.int/news/item/23-09-2020-managing-the-covid-19-infodemic-promoting-healthy-behaviours-and-mitigating-the-harm-from-misinformation-and-disinformation. Accessed June 24, 2021
- 21.Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16:2586–2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singh S, Dixit A, Joshi G. Is compulsive social media use amid COVID-19 pandemic addictive behavior or coping mechanism? Asian J Psychiatr. 2020;54:102290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vasquez Reyes M. The disproportional impact of COVID-19 on African Americans. Health Hum Rights 2020;22:299–307. [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Health equity considerations & racial ethnic minority groups. Available at: https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html. Accessed June 5, 2021
- 25.Agency for Toxic Substances and Disease Registry. CDC/ATSDR Social Vulnerability Index. Available at: https://www.atsdr.cdc.gov/placeandhealth/svi/index.html. Accessed June 16, 2021
- 26.Schmidt H, Pathak P, Sönmez T, Ünver MU. Covid-19: How to prioritize worse-off populations in allocating safe and effective vaccines. BMJ 2020;371:m3795. [DOI] [PubMed] [Google Scholar]
- 27.Cai X, Fry CV, Wagner CS. International collaboration during the COVID-19 crisis: Autumn 2020 developments. Scientometrics 2021;126:3683–3692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCarthy J. Principlism or narrative ethics: Must we choose between them? Med Humanit. 2003;29:65–71. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.