Abstract
Purpose
To report a case with unusual initial manifestation of uveal melanoma in a 46-year-old adult.
Observations
A 46-year-old man demonstrated a mid-peripheral temporal partially hyperpigmented lesion in his left eye. Initial clinical appearance as well as multimodal imaging approaches were similar to a chorioretinitic disease. Over the course of 9 months, a massive tumor growth and exudative retinal detachment could be observed. The diagnosis of choroidal melanoma was histopathologically confirmed after endoresection.
Conclusions and importance
Classical choroidal melanoma manifest as pigmented, prominent tumors with >2 mm tumor thickness, exudative retinal detachment, and orange pigment. In our case, none of these classical clinical characteristic signs of melanoma were present at initial presentation, but the tumor underwent progressive development with significant tumor growth and exudative retinal detachment during the following 9 months.
Keywords: Choroidal melanoma, Uveal melanoma, Unusual manifestation, Masquerade syndrome
1. Introduction
Uveal melanoma is a rare condition, but it is still the most common primary intraocular malignant tumor with an incidence of 6–7.5 cases per one million.1 Most of the cases have a typical clinical appearance and the diagnosis can easily be made on indirect ophthalmoscopy, multimodal imaging and ultrasonography. Especially in small lesions, it sometimes remains challenging due to unusual manifestation or other ocular conditions mimicking a choroidal melanoma.
This case represents a 46-years-old adult with a flat irregular pigmented mid-peripheral chorioretinal lesion, which turned out to be a choroidal melanoma in the course of 9 months. This case followed the principles of the Declaration of Helsinki and informed consent was obtained from the participant.
2. Case report
A 46-year-old man had a history of glaucoma suspect optic disc in both eyes and was referred to our clinic for evaluation of an incidental finding during a planned ophthalmic examination in his left eye. He complained about some photopsia and flashes in both eyes for a couple of weeks preceding the examination.
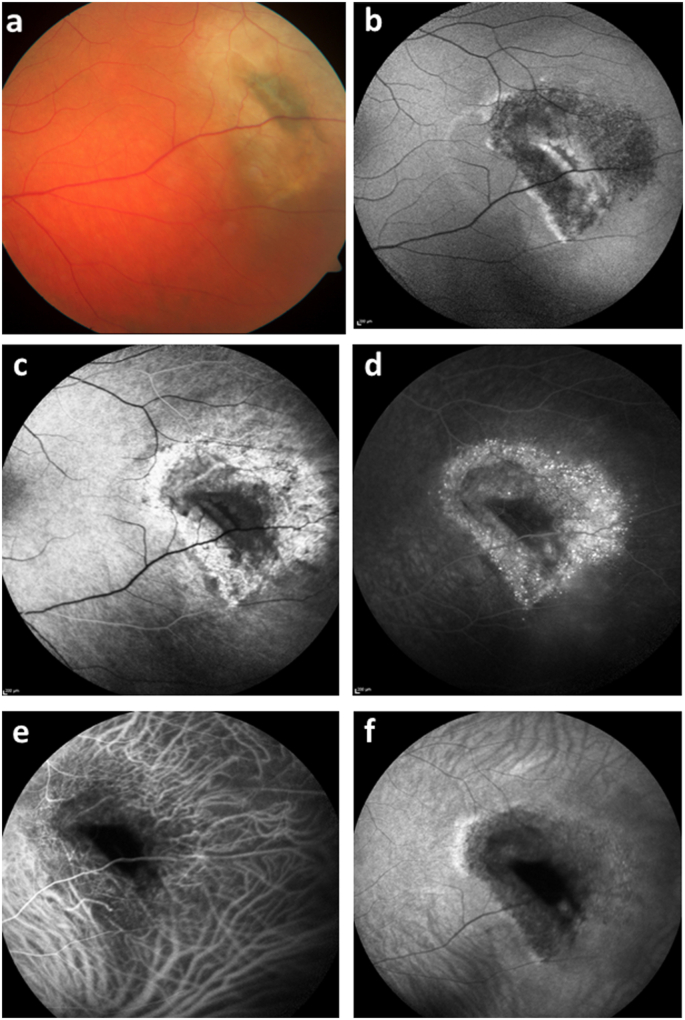
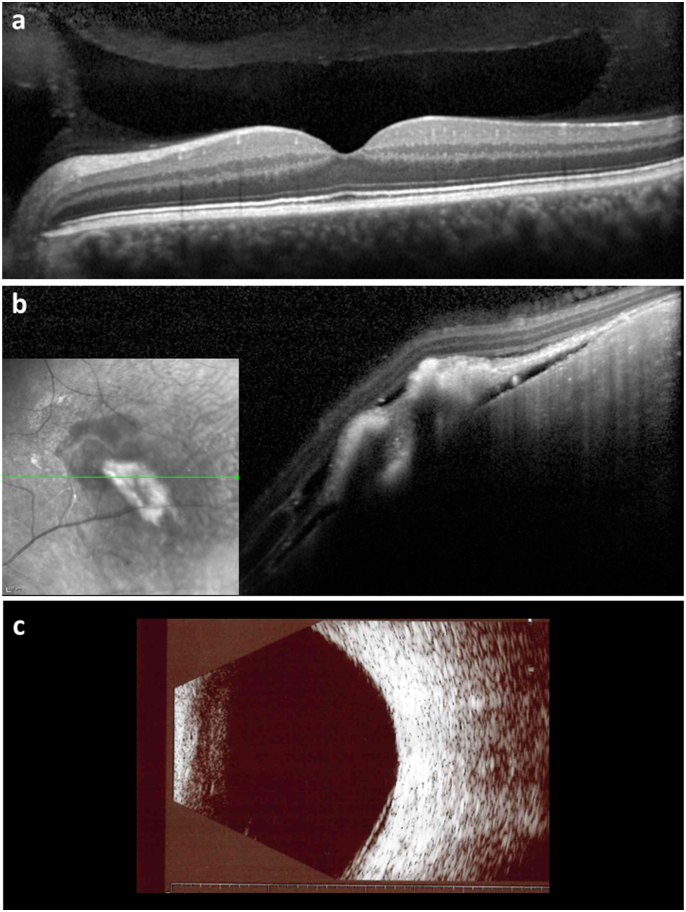
At initial presentation, visual acuity in both eyes was 20/20 with an unremarkable anterior segment. No pathological findings on the clinical examination of the right eye fundus could be seen. Posterior segment examination of the left eye revealed a mid-peripheral temporal partially hyperpigmented lesion with a small area of exudation around it (Fig. 1). No vitreous inflammation signs were present. Spectral-domain optical coherence tomography (SD-OCT) of the left macula showed no abnormalities, while SD-OCT scan through the peripheral lesion demonstrated subretinal hyperreflective material with thickening of retinal pigment epithelium and a shallow serous detachment of the neurosensory retina around it (Fig. 2). On ultrasonography, a flat detachment possibly due to the detachment of the neurosensory retina with no evidence of prominence could be seen (Fig. 2). The fundus autofluorescence image (FAF) revealed some hyperautofluorescent areas corresponding to central hyperpigmentation on the color fundus photography with a surrounding hypoautofluorescent ring (Fig. 1). Fluorescein angiography (FA) showed hypofluorescence in the central part of the lesion corresponding to the hyperautofluorescence in autofluorescence imaging (Fig. 1). The surrounding hypoautofluorescent part of the lesion was hyperfluorescent on FA with some pinpoint leakage. On indocyanin green angiography (ICGA), the lesion remained hypofluorescent with no evidence of tumor vessels (Fig. 1).
Fig. 1.
Multimodal imaging of the suspected retinal lesion in the left eye at initial presentation. a. Color fundus photograph of the left eye with peripheral temporal partially hyperpigmented lesion with small area of exudation around it, the size of lesion was approximately 1 disc diameter. b. Autofluorescence imaging of the same region with hyperautofluorescent area corresponding to central hyperpigmentation on the color fundus photography with surrounding hypoautofluorescent ring. c. Fluorescein angiography image of the early phase with hypoautofluorescent central areas and some hyperfluorescence surrounding the lesion. d. Fluorescein angiography image of the late phase with remaining hypofluorescence in the central part surrounded by hyperfluorescence with pinpoint leakage. e-f. Indocyanin green angiography with hypofluorescent lesion from early till the late phase. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Spectral-domain optical coherence tomography and ultrasonography at initial presentation. a. Spectral-domain optical coherence tomography of the macula with no pathological findings. b. Spectral-domain optical coherence tomography through the suspected lesion showing subretinal hyperreflective material with thickening of retinal pigment epithelium and a shallow serous detachment of the neurosensory retina around it. A breakthrough in retinal pigment epithelium should be suspected on the top of the lesion an on the central margin. c. B-scan ultrasonography showed low-lying retinal detachment.
A detailed history of the patient revealed a close contact with sharps and pigeons, as he was living on an animal farm. Furthermore, he had been using a nasal spray with corticosteroids for several months due to sinus inflammation. A light blunt trauma of the left eye several years ago with no need for further treatment had also been reported.
As the patient's ophthalmic presentation and previous history was suggestive of a systemic process, a comprehensive diagnostic approach to rule out possible infectious diseases was arranged. Magnet resonance imaging (MRI) of the brain, orbits and the lung failed to show any pathological findings. Interim laboratory evaluations were also negative for the following: hepatitis B/C virus, human immunodeficiency virus, herpes simplex virus, Epstein–Barr virus, varicella zoster virus, cytomegalovirus, tuberculosis, Lyme disease, syphilis, toxoplasmosis, rickettsiosis, Bartonella henselae, sarcoidosis, lupus. A consultation at the department for infectious diseases and abdominal ultrasound were also unremarkable.
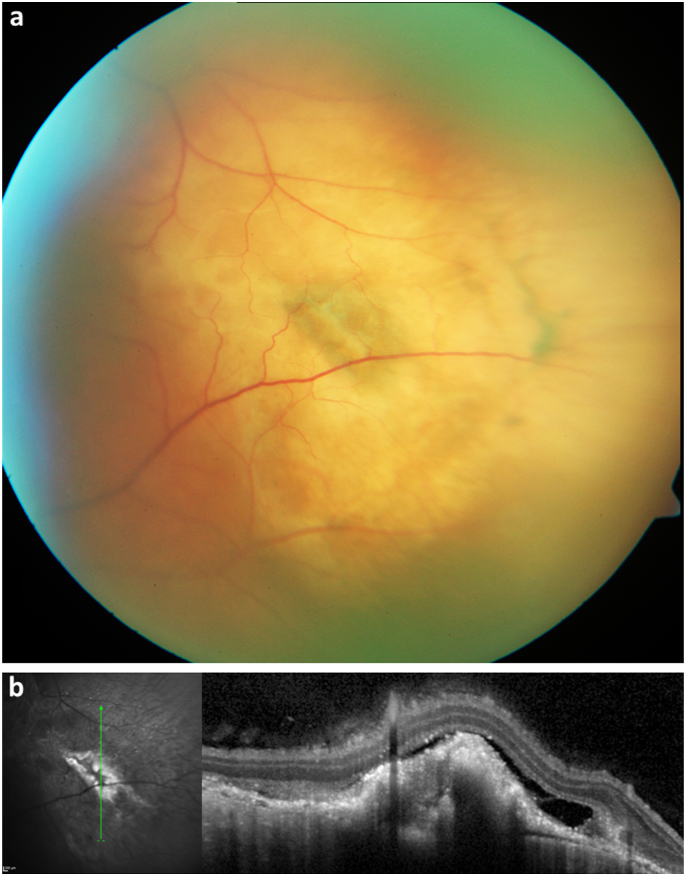
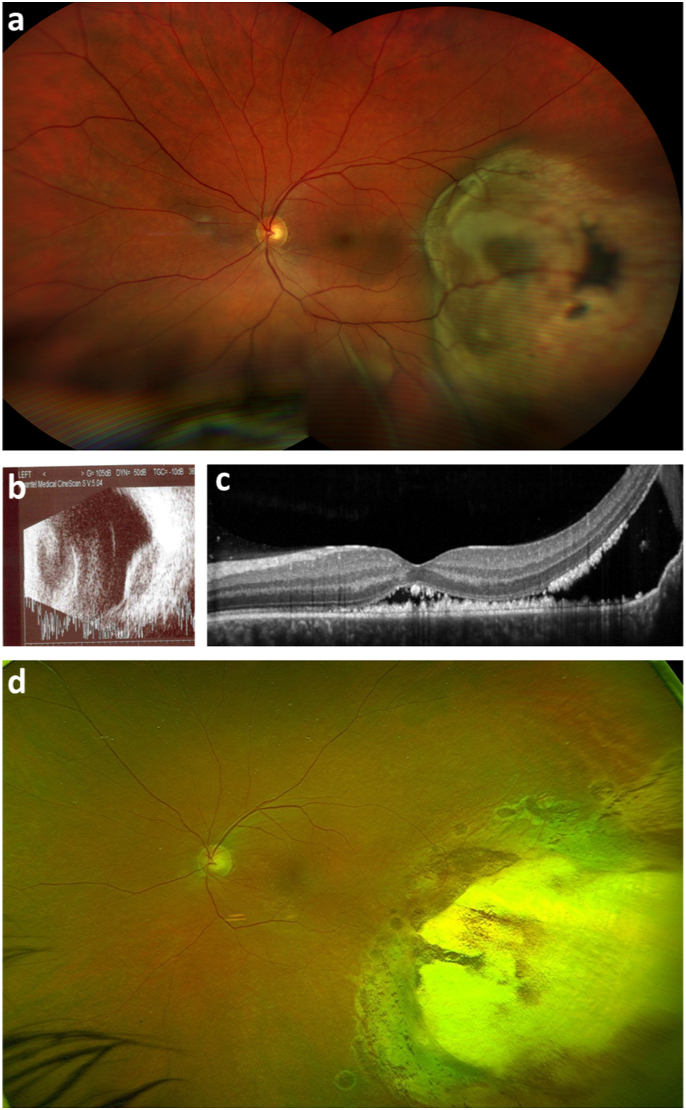
Over the next 4 months, the patient was treated with systemic antibiotics (doxycycline) and steroids according to the initial suspicion of a chorioretinitic disease. Afterwards, the patient presented with a slightly increased area of exudation on color fundus photography, while the central hyperpigmentation zone was much more pale with the same contour as before (Fig. 3). On SD-OCT, the subretinal hyperreflective material was slightly progressive (Fig. 3). After 4 more months, a remarkable progression could be seen with a massive growth of the tumor in the whole temporal area with exudative retinal detachment in the inferior and central part of the fundus (Fig. 4). The new MRI of the brain and orbit supported the diagnosis of choroidal melanoma of the left eye. The patient was then treated with proton beam therapy and pars plana vitrectomy with endoresection afterwards (Fig. 4). Twelve months after the last surgery, the visual acuity remained stable at 20/80. No systemic metastatic disease could be found till now.
Fig. 3.
Images of the left eye after 4 months with systemic antibiotic and corticosteroid treatment. a. Color fundus photograph with fading central hyperpigmentation, but slightly increasing exudative reaction. b. Spectral-domain optical coherence tomography through the suspected lesion showing increased subretinal hyperreflective mass and a flat serous neurosensory retinal detachment. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Fig. 4.
Multimodal imaging 9 months after initial presentation. a. Color fundus photograph with a massive tumor growth and exudative retinal detachment inferior, reaching the posterior pole. b. B-scan ultrasonography showing a prominent lesion with lower echo within the melanoma and shadowing in the orbit. c. Spectral-domain optical coherence tomography image of the macula with serous neurosensory retinal detachment reaching the foveal region. d. Color fundus photograph 2 months after silicon oil removal and 8 months after pars plana vitrectomy with endoresection and silicon oil tamponade. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
The histology of the tumor material gained during endoresection confirmed the diagnosis of a choroidal melanoma, showing fragments of a neoplasia with spindle cells and focal epitheloid cells with prominent nucleoles. Immunohistochemistry showed a distinct expression for Melan A, S100, and HMB45. The proliferation rate was 3% (Ki-67). BAP1 staining showed a largely preserved nuclear BAP1 expression, which is associated with less aggressive metastatic behaviour.
3. Discussion
Choroidal melanoma can nowadays be correctly diagnosed in more than 95% of the cases with indirect ophthalmoscopy,2 especially in tumors showing the highly typical collar button configuration. However, they can also be dome shaped or present as flat melanoma. The amount of pigment may vary and the tumors can be totally or partially amelanotic. Orange pigment and exudative retinal detachment are typical clinical features of this condition.1 However, orange pigment and exudative retinal detachment are neither obligatory nor pathognomonic for uveal melanoma. They can for example also appear in uveal metastasis.2 The diagnostic accuracy of FA and ICGA in melanoma diagnostics is limited.3 The ultrasonography with an acoustically silent zone within the melanoma, choroidal excavation and shadowing in the orbit is a very reliable investigative method for carrying out the right diagnosis, but requires sufficient tumor thickness.1
Furthermore it cannot be stressed enough that uveal melanoma can be (totally or partially) amelanotic and that melanoma can be collarbutton shaped or domeshaped but can also present as so called flat melanoma.
Unusual manifestation of choroidal melanoma as well as other conditions mimicking choroidal melanoma might represent a diagnostic challenge. There are several publications describing confirmed uveal melanoma, presenting with secondary glaucoma or choroidal hemorrhage resulting from diverse ocular conditions such as hypotonia, inflammation, trauma with intraocular foreign body or vascular diseases.4,5 Choroidal hemorrhages may mimic an uveal melanoma due to their prominence and variable color image during blood reorganization. On the other hand, several case reports have been published with inflammatory conditions like scleritis posterior or hemorrhagic lesions, which were mistakenly being diagnosed as choroidal melanoma.6, 7, 8
In our case, the choroidal melanoma was captured at initial stage, which is rarely seen in everyday practice. Asymptomatic tumors are often incidental findings. Neither orange pigment nor retinal detachment could be seen at initial presentation. Further difficulty for the right diagnosis was lying in the absence of typical prominence of the lesion. Therefore, it was not possible to investigate the echo of the lesion on ultrasonography and on the initial MRI investigation, the lesion could also not be found. Regarding the initial clinical appearance of the lesion – flat character with partially hyperpigmented central area and ill-defined borders with surrounding subretinal exudation - and the previous history of the patient with a close animal contact, an infectious chorioretinitic disease was mistakenly suggested.
According to clinical appearance as well as FA and ICGA images, differential diagnosis of a tumor of the retinal pigment epithelium should also be considered, especially regarding the irregular lesion character with intense pigmentation in the center. Furthermore, at initial presentation with a history of a blunt trauma in the left eye, reactive hyperplasia of the retinal pigment epithelium might also be a possible differential diagnosis. However, this could be ruled out in the course of the disease given the clinical progression.
4. Conclusion
Our findings demonstrate an early unusual choroidal melanoma manifestation without classical signs (pigmented, prominent tumors with >2 mm tumor thickness, exudative retinal detachment and orange pigment), presenting as a flat partially pigmented chorioretinitic lesion in a 46-year-old otherwise healthy adult.
Patient consent
The patient consented to publication of the case in writing.
Funding
No funding was received for this work.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
No conflict of interest exists.
Acknowledgements
None.
References
- 1.Singh P., Singh A. Choroidal melanoma. Oman J Ophthalmol. 2012;5(1):3–9. doi: 10.4103/0974-620X.94718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shields C.L., Shields J.A., Gross N.E., Schwartz G.P., Lally S.E. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997;104:1265–1276. doi: 10.1016/s0161-6420(97)30148-1. [DOI] [PubMed] [Google Scholar]
- 3.Char D.H., Stone R.D., Irvine A.R., et al. Diagnostic modalities in choroidal melanoma. Am J Ophthalmol. 1980;89:223–230. doi: 10.1016/0002-9394(80)90115-4. [DOI] [PubMed] [Google Scholar]
- 4.Nicoletti A.G.B., Costa D.S., Ghanem R.C., et al. Atypical choroidal melanoma: report of three cases. Clinics. 2006;61(1):79–82. doi: 10.1590/s1807-59322006000100014. [DOI] [PubMed] [Google Scholar]
- 5.Shields J.A., Augsburger J.J., Brown G.C., et al. The differential diagnosis of posterior uveal melanoma. Ophthalmology. 1980;87:518–522. doi: 10.1016/s0161-6420(80)35201-9. [DOI] [PubMed] [Google Scholar]
- 6.Liu A.T., Luk F.O., Chan C.K. A case of giant nodular posterior scleritis mimicking choroidal malignancy. Indian J Ophthalmol. 2015;63(12):919–921. doi: 10.4103/0301-4738.176038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shukla D., Kim R. Giant nodular posterior scleritis simulating choroidal melanoma. Indian J Ophthalmol. 2006;54:120–122. doi: 10.4103/0301-4738.25835. [DOI] [PubMed] [Google Scholar]
- 8.Sridharan S., Juneja R., Hussain A., et al. Giant nodular posterior scleritis mimicking choroidal tumor. Retin Cases Brief Rep. 2007;1:65–67. doi: 10.1097/01.ICB.0000264802.71612.1c. [DOI] [PubMed] [Google Scholar]