Abstract
Epidemiological studies have suggested that childhood maltreatment increases suicidal ideation, and dissociative symptoms and hopelessness are involved in this relation. To better address this issue, we used a path analysis model to examine the role of different types of childhood maltreatment on suicidal ideation, investigating whether hopelessness and dissociative symptoms mediated this relation. A sample of 215 adult psychiatric inpatients was enrolled between January 2019 and January 2020, at the psychiatric unit of Sant’Andrea Medical Center in Rome, Italy. The Childhood Trauma Questionnaire (CTQ), Beck Hopelessness Scale (BHS), Dissociative Experiences Scale (DES-II), and Columbia-Suicide Severity Rating Scale (C-SSRS) were used to test the hypotheses. Results revealed that the presence of sexual abuse directly affected suicidal ideation (β = 0.18, SE = 0.8, p < 0.05), while emotional abuse and neglect indirectly increased suicidal ideation via dissociation (β = 0.05, SE = 0.02, 95% C.I. 0.01/0.09) and hopelessness (β = 0.10, SE = 0.03, 95% C.I. = 0.04/0.16). Professionals working with children should be aware of the long-term consequences of childhood maltreatment, particularly suicide risk. Furthermore, professionals working with adults should inquire about past childhood maltreatment.
Keywords: suicide, suicidal ideation, childhood maltreatment, trauma, dissociative symptoms, hopelessness
1. Introduction
Epidemiological studies have shown that childhood maltreatment, including physical, sexual, emotional abuse, and neglect, is present in about 30% of the population [1,2,3,4]. In addition, childhood maltreatment increases the risk of mental health consequences in adulthood, including depression, anxiety, psychosis, posttraumatic stress disorders, dissociative disorders, and personality disorders [5]. Risky sexual behavior and drug and/or alcohol addiction may also be present [6,7].
Several studies have also demonstrated an association between childhood maltreatment and suicidal ideation, defined as thoughts about a wish to be dead or active thoughts of wanting to end one’s life [8,9,10,11]. A recent meta-analysis of 68 studies showed that all types of childhood maltreatment were associated with significantly increased odds for suicidal ideation in adults. Notably, sexual abuse and emotional abuse were associated with a two-fold increased risk for suicidal ideation, physical abuse was associated with a 2.5-fold increased risk for suicidal ideation, and emotional and physical neglect was associated with a 1.5-fold increased risk for suicidal ideation [12]. A subsequent meta-analysis of 79 studies with 337,185 participants concluded that sexual abuse in young people was associated with 4.0-fold increased odds for suicide plans [13]. Several studies have also indicated that different types of childhood maltreatment predicted adult suicidal ideation [14,15,16]; Barbosa et al. [17], for example, found that childhood neglect, as well as physical and sexual abuse, were each associated with a threefold—and for emotional abuse a sixfold—increased risk of suicidal ideation in individuals aged 14–35 years. Moreover, childhood maltreatment is associated with suicide risk among patients with various psychiatric disorders. For example, Prokopez et al. [18] analyzed a sample of patients with schizophrenia and found that patients who experienced five or more adverse childhood experiences reported higher levels of suicidal ideation and more suicide attempts. An inclusive systematic review and meta-analysis [19] demonstrated that the presence of childhood maltreatments predicted a global clinical worsening and a higher suicidal risk in patients diagnosed with bipolar disorder. Furthermore, in a cross-sectional study on 473 patients with major depression, De Mattos Souza et al. [16] observed that emotional abuse and neglect were risk factors for suicidal ideation. Finally, in patients with psychotic disorders, childhood maltreatment was found to be associated with both clinical course and treatment outcomes [20].
Dissociative symptoms and hopelessness may play an important role among the various psychopathological features involved in the relation between childhood maltreatment and suicidal ideation. Dissociation is a complex psychopathological construct, defined as “disruption of and/or discontinuity in the normal integration of consciousness, memory, identity, emotion, perception, body representation, motor control, and behavior” [21]. The development of dissociative symptoms is considered a psychological adaptation strategy that allows a child to survive severe and prolonged abuse [22,23]. In contrast, hopelessness is a negative expectation toward oneself and the future [24]. According to Mueller-Pfeiffer et al. [25], childhood maltreatment is a strong predictor of dissociation.
Furthermore, Courtney et al. [26] demonstrated that childhood maltreatment predicted higher levels of hopelessness and depressive symptoms in adolescents. Indeed, hopelessness is one of the most prominent risk factors for suicide, as reported in several studies [27,28,29,30]. Finally, a recent meta-analysis [31] found that dissociative symptoms were strongly associated with suicidal risk; in an ideation-to-action framework to suicide, the progression from suicidal ideation to lethal suicidal attempts can be understood as a distinct process that includes dissociation as a factor that diminishes fear of pain, injury, and death and increases a person’s capability to attempt suicide [32].
Moreover, dissociative symptomatology has been proposed as one possible mediator in the link between childhood maltreatment and suicide risk, including suicide ideation and attempt [22,33,34,35,36,37,38]. Rodriguez-Srednicki [34] has analyzed the role of childhood sexual abuse on suicidal risk. Tamar-Gurol et al. [36] focused on the prevalence and correlates of dissociative disorders in a sample of drug addicts. Recently, Bertule et al. [38] conducted a study on patients with depression in a community sample, highlighting the complex interconnections between childhood abuse, dissociation, and suicidality. The authors demonstrated that emotional abuse was linked to dissociation, which, in turn, was related to depression and depression was linked to suicide ideation.
Previous studies have also suggested that hopelessness is related to childhood maltreatment [39,40]. Moreover, hopelessness is associated with suicide risk among psychiatric patients [41], particularly in those patients who have experienced childhood abuse and neglect [42]. Gibb et al. [43], inspired by the “hopelessness model” of suicide risk [44], hypothesized that childhood maltreatment might contribute to the development of a negative cognitive style that exacerbates hopelessness, which, in turn, triggers suicidal ideation and behaviors. Meadows and Kaslow [45] explored a sample of abused participants and found that hopelessness mediated the association between childhood maltreatment and suicide attempt.
Understanding the role of dissociative symptoms and hopelessness as possible mediators in the relation between the various types of childhood maltreatment and suicidal risk will advance our understanding of the association among these variables. To confirm and extend a previous path analysis study [38] that examined the associations between childhood trauma abuse, depressive symptoms, dissociative symptoms, and suicidality in patients with depression, the present study investigates the association between childhood maltreatment (both abuse and neglect) and suicidal ideation in patients with various psychiatric disorders. We hypothesized that different types of childhood maltreatment would be related to higher levels of hopelessness and dissociative symptoms, which would increase suicidal ideation in psychiatric patients. Moreover, dissociative symptoms and hopelessness would mediate the relationship between childhood maltreatment and suicidal ideation. Specifically, we have investigated the role of different types of childhood maltreatment (emotional neglect, emotional abuse, sexual abuse, and physical neglect and abuse) in suicidal ideation among patients with psychiatric disorders. Accordingly, we tested a path analysis model that belongs to a family of statistical techniques known as structural equation modeling (SEM), to assess the relationship between different types of childhood maltreatment, dissociative symptoms, hopelessness, and suicidal ideation.
2. Materials and Methods
2.1. Participants
This study was conducted on 215 adult psychiatric inpatients (46.5% women). The mean age of the patients was 39.72 years (standard deviation (SD) = 14.16 years; age range = 18–75 years). Patients were enrolled between January 2019 and January 2020 at the psychiatric ward of Sant’Andrea Medical Center, a teaching hospital of Sapienza University of Rome, Italy. Inclusion criteria were adult inpatients aged ≥ 18 years with a diagnosis of psychiatric disorder, according to DSM-5 [21]. Exclusion criteria were degenerative neurological diseases or comorbidities with alcohol or substance use disorders that prevented the patients from understanding and completing the questionnaires. All participants received a comprehensive explanation of the study procedures and goals, consistent with the Declaration of Helsinki. After signing a written informed consent form, all patients voluntarily participated in this study. The assessment of psychiatric patients with particular attention to suicide risk is part of several investigations approved by the local ethics review board.
2.2. Measures
Psychiatric diagnoses were made according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) criteria [21] and supported by the Structured Clinical Interview for DSM-5 Disorders (SCID-5) [46]. A psychiatric diagnosis was made during the first days of hospitalization (48 h of the admission). Trained psychiatrists assessed suicide ideation when the patient arrived at the emergency department and admitted to the psychiatric ward. According to the definition adopted by Silverman for the assessment of suicide ideation, psychiatrists evaluated the presence and the degree of suicidal intent. Moreover, they investigated the presence of suicide attempts as self-inflicted, potentially injurious behaviors with a nonfatal outcome. There is explicit or implicit evidence of intent to die [47,48].
The Columbia-Suicide Severity Rating Scale (C-SSRS) [49,50] is a semi-structured interview used to evaluate suicide ideation and behaviors in individuals aged 12 years and older [50]. The C-SSRS consists of two sections, all of which maintain binary responses (yes/no) to indicate the presence or absence of the item. The first section evaluates the presence of suicidal ideation from the desire to be dead up to the presence of suicidal intentions with the planning of a specific method. The second section assesses suicide behaviors including actual, aborted, and interrupted attempts, preparatory and non-suicidal self-injurious behaviors and lethality of the attempts.
We only considered the first five items that investigate lifetime suicidal ideation for the study. The first two items assess the respondent’s wish to be dead (e.g., “Have you wished you were dead or wished you could go to sleep and not wake up?”) and nonspecific active suicidal thoughts (e.g., “Have you actually had any thoughts of killing yourself?”). If the patient replies affirmatively to either of these two items, the clinician asks three additional questions that assess active suicidal ideation with any method but with no plan or intent to act; active suicidal ideation with some intent to act but no plan; and active suicidal ideation with a specific plan and intent. The severity of suicidal ideation ranges from 0 (absence of suicidal ideation) to 5 (from 1 to 5, patients were considered at some degree of risk for suicide), based on the maximum suicidal category observed (the higher item with a positive answer). This section showed excellent reliability (α = 0.916).
The Childhood Trauma Questionnaire (CTQ) [51,52] is a 28-item self-report questionnaire to assess emotional and physical abuse, sexual abuse, and emotional and physical neglect. Each item begins with the anchor, “when I was growing up” and respondents indicate the frequency of a particular incident on a 5-point Likert scale (1 = never true; 5 = very often true). Each 5-item subscale ranges from 5 (no history of abuse) to 25 (very extreme history of abuse). Each scale has a different cut-off score and can detect four levels of maltreatment (none or minimal, low to moderate, moderate to severe, severe to extreme); in our study, mean scores for each subscale indicated a low to moderate level of maltreatment [52]. Subscale reliability in this study were emotional neglect α = 0.771, emotional abuse α = 0.776, sexual abuse α = 0.895, physical neglect α = 0.402, and physical abuse α = 0.795.
The Beck Hopelessness Scale (BHS) [53,54] is a 20-item self-report scale that measures negative attitudes about the future (e.g., “I look forward to the future with hope and enthusiasm”, “I might as well give up because I can’t make things better for myself”). This powerful predictor of eventual suicide addresses three major aspects of hopelessness: feelings about the future, loss of motivation, and expectations. In Italy, validation studies have been conducted on samples of medical patients, university students, and psychiatric inpatients and have demonstrated satisfactory psychometric properties [55]. Several studies indicated that, in psychiatric samples, the BHS is a valid measure for predicting subsequent suicide behavior [56,57]. For example, a score of ≥9 is able to detect patients at risk for suicide [57,58]. In the current study, the scale had good reliability (α = 0.890).
The Dissociative Experiences Scale (DES) [59] is a self-rating instrument comprising 28 items that build on the assumption of a “dissociative continuum” ranging from mild normative to severe pathological dissociation. Patients were asked to circle the percentage of time in which they had the experience described, including questions on experiences of amnesia, absorption, depersonalization, and derealization (e.g., “Some people have the experience of driving a car and suddenly realizing that they don’t remember what has happened during all or part of the trip”). A score ≥ 30 can be used to distinguish those patients with mild and severe levels of dissociation [60]. In the present study, we used the Dissociative Experiences Scale–II (DES-II) [59], a revised version of the scale, developed because the former version’s scoring procedure was time-consuming. DES-II uses an 11-point Likert scale ranging from 0 to 100, demonstrating excellent reliability (α = 0.945). In this study, we administered the Italian version of the scale [61]
2.3. Statistical Analysis
Descriptive analysis was performed with the Statistical Package for Social Sciences (IBM SPSS Statistics for Mac, v.25, Armonk, NY, USA) and reported with means, standard deviations (e.g., age), and percentages (e.g., sex, job, diagnosis). To test the study hypotheses, a path analysis model was performed with Mplus v.8 software (Muthén & Muthén, Los Angeles, CA, USA) [62]. Unweighted least square (ULS) estimator was used to control for the non-normal variable distribution after evaluating the study’s variables for skewness and kurtosis. The model included pathways through which childhood maltreatment dimensions, hopelessness, and dissociation contribute to suicidal ideation in a sample of psychiatric inpatients with various diagnoses. Suicidal ideation was considered as a categorical variable. The goodness of fit was examined using standard fit statistics such as chi-square statistics, the Tucker–Lewis index (TLI), the root mean square error of approximation (RMSEA), and the standardized root mean square residual (SRMR). Acceptable model fit was reached with a non-significant chi-square test, TLI and CFI values of 0.90 or above, RMSEA values < 0.080, and SRMR values below 0.060 [63]. Indirect effect estimates were tested through empirical sampling distributions by calculating confidence limits and testing statistical significance of indirect effects through 0 within the interval. All path coefficients were reported as standardized estimates. A path diagram representing the model was constructed, with straight arrows representing significant regression paths, dashed arrows representing non-significant regression paths, and curved arrows representing correlations. All tests were considered significant with a p value < 0.05.
3. Results
3.1. Descriptive Analysis
The sociodemographic and clinical characteristics of the sample are reported in Table 1. Most patients were male (53.5%), single (57.2%), employed (50.2%), and well educated (54%). The mean age of the sample was 39.7 (SD = 14.1, age-range = 18/75 years). Regarding psychiatric diagnoses, 36.2% of patients had a diagnosis of schizophrenia or other psychoses, 38.1% had mood disorders (25.1% bipolar disorders; 13% major depression), and 10.7% had other psychiatric disorders. Concerning lifetime suicidal ideation, 23.7% of the patients referred absence of suicidal ideation, 7.4% referred a wish to be dead, 10.3% referred suicidal thoughts, 18.6% referred suicidal intent, and 40% of the patients referred suicidal intent with a specific plan. Moreover, 54.9% of patients referred at least one lifetime suicide attempt. Regarding the type of childhood maltreatment, 53% of patients referred to the presence of emotional abuse, 29.8% referred to physical abuse, 37.8% sexual abuse, 67.9% emotional neglect, and 50.2% of the patients referred to physical neglect.
Table 1.
Sociodemographic and clinical characteristics of the sample (N = 215).
| Variables | N | % |
|---|---|---|
| Sex | ||
| Male | 115 | 53.5 |
| Female | 100 | 46.5 |
| Age—M ± SD | 39.72 ± 14.1 | |
| Marital status | ||
| Married | 65 | 30.2 |
| Divorced or widowed | 27 | 12.6 |
| Single | 123 | 57.2 |
| Job | ||
| Employed | 108 | 50.2 |
| Unemployed | 93 | 43.3 |
| Other | 14 | 6.5 |
| Years of education | ||
| <8 years | 62 | 28.8 |
| 9–15 years | 116 | 54.0 |
| >16 years | 37 | 17.2 |
| Diagnosis | ||
| Schizophrenia and other psychoses | 78 | 36.2 |
| Bipolar disorders | 54 | 25.1 |
| Major depression | 28 | 13.0 |
| Other | 23 | 10.7 |
| Comorbidity | ||
| Personality disorder | 27 | 12.6 |
| Addiction | 5 | 2.3 |
| Severity of suicidal ideation M ± SD | 3.08 ± 2.1 | |
| Lifetime suicide attempt | 118 | 54.9 |
| Emotional abuse M ± SD | 9.69 ± 4.6 | |
| Emotional neglect M ± SD | 12.29 ± 5.1 | |
| Sexual abuse M ± SD | 7.24 ± 4.3 | |
| Physical abuse M ± SD | 7.19 ± 3.5 | |
| Physical neglect M ± SD | 7.80 ± 3.0 | |
| BHS M ± SD | 8.55 ± 5.4 | |
| DES-II M ± SD | 24.4 ± 17.8 |
3.2. Path Analysis
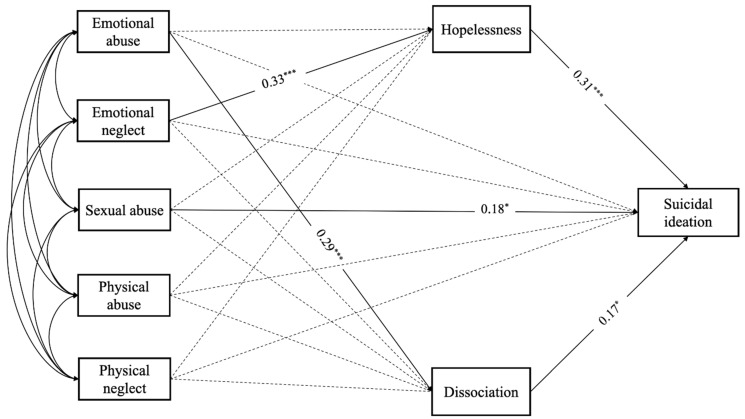
Path analysis is shown in Figure 1. The model fit information follows: χ2 1 = 0.277, p = 0.598; CFI = 1.0; RMSEA (90% C.I. = 0.00 (0.00–0.15)); SRMR = 0.006. Overall, the R-square index showed that the childhood trauma dimensions, hopelessness, and dissociation were able to explain 22% of the total variance in the suicidal ideation (R2 = 0.218, p < 0.001).
Figure 1.
Path analysis. All reported parameters are standardized. * p < 0.05; *** p < 0.001. For ease of interpretation, the effects of covariates are not shown in the figure.
Results for emotional abuse indicated a significant total effect on suicidal ideation (β = 0.19, p < 0.05). The total indirect effect was significant (β = 0.10, SE = 0.03, 95% C.I. = 0.04/0.15); in particular, emotional abuse had an indirect effect on suicidal ideation via dissociation (β = 0.05, SE = 0.02, 95% C.I. 0.01/0.09). Specifically, emotional abuse had a positive and significant effect on levels of dissociation (β = 0.29, p < 0.001); in turn, dissociation had a positive effect on suicidal ideation (β = 0.17, p < 0.05).
Emotional neglect did not have a significant total effect on suicidal ideation; however, the total indirect effect was significant (β = 0.10, SE = 0.04, 95% C.I. = 0.03/0.16) and, in particular, emotional neglect had an indirect effect on suicidal ideation via hopelessness (β = 0.10, SE = 0.03, 95% C.I. = 0.04/0.16). Specifically, emotional neglect had a significant effect on levels of hopelessness (β = 0.33, p < 0.001) and, in turn, hopelessness had a positive effect on suicidal ideation (β = 0.31, p < 0.001).
Sexual abuse was found to have a significant total effect on suicidal ideation (β = 0.20, p < 0.05); in particular, sexual abuse had a positive and direct effect on suicidal ideation (β = 0.18, SE = 0.8, p < 0.05), while no indirect effects were significant.
Lastly, neither physical abuse nor physical neglect showed significant effects on suicidal ideation.
4. Discussion
The present study results have shown that emotional abuse was related to suicidal ideation through the mediating role of dissociation. Furthermore, emotional neglect was related to suicidal ideation through the mediating role of hopelessness. Finally, sexual abuse directly affected suicidal ideation, whereas physical abuse and neglect were not associated directly or indirectly—through the mediators—with suicidal ideation.
Regarding emotional abuse, we found a relation to suicidal ideation through the mediating role of dissociation. These results confirm previous studies that demonstrated the role of emotional maltreatment on psychopathological consequences [64,65,66,67,68]. Recently, Bertule et al. [38] conducted a path analysis highlighting the complex interconnections between childhood abuse (emotional, physical, and sexual), dissociation, and suicidality among patients with depression in a community sample. Specifically, emotional abuse was linked to dissociation, which, in turn, was related to depression and ultimately predictive of suicide ideation. However, this study only included patients with a single psychiatric diagnosis.
Furthermore, the results indicated that emotional neglect was associated with suicidal ideation through the mediating role of hopelessness. Interestingly, the results suggested two different pathways for emotional abuse and neglect. In particular, emotional abuse was linked to suicidal ideation through dissociation, while emotional neglect through hopelessness. Consistent with the hopelessness theory [69], we hypothesized that emotionally neglected children develop a negative perception of themselves, of others, and of the future (hopelessness), increasing suicide risk. Otherwise, people who experienced emotional abuse may develop dissociative symptoms [70]. These findings can be partially explained because childhood emotional abuse is often inflicted by somebody close to the victim, producing dissociative experiences that protect the child’s internal self [70]. Moreover, our results have shown that sexual abuse directly affected suicidal ideation [71,72,73]. Childhood sexual abuse has serious, long-term medical and psychological consequences [74,75], and produces a cascade of neurobiological events linked also to suicidal ideation [76].
Finally, through the mediators, physical abuse and neglect were not associated directly or indirectly with suicidal ideation. This result is consistent with the findings of Gibb and colleagues [43], who demonstrated that only emotional maltreatment was associated with suicidal ideation across a 2.5-year follow-up. However, it is in contrast with many other studies that have highlighted the contributory role of physical maltreatment on suicidal ideation and behavior [12,77]. Hence, it is important to conduct further studies to investigate the association between these variables more thoroughly.
Assessing the relationship between different types of childhood maltreatment and suicide risk in psychiatric patients is fundamental for a more appropriate multidisciplinary management of these patients. Several studies suggested a neuropsychological relation between childhood maltreatment and suicide risk in psychiatric patients. Savitz et al. [78] reported an association between emotional, physical, and sexual abuse with poorer cognitive performances in patients with bipolar spectrum disorders. McLaughlin et al. [79] proposed a transdiagnostic model to explain better the association between childhood trauma and psychopathology, based on elevated emotional reactivity to threat-related stimuli, low emotional awareness, and difficulties with emotional learning and emotion regulation. Furthermore, childhood maltreatment has been shown to contribute to many structural and functional changes in the brain, including such structures as the hippocampus and amygdala, associated with several psychiatric disorders and suicide risk [80].
Our study has several limitations. First, temporal ordering between the predictor and outcome of interest (i.e., childhood sexual abuse occurring before 18 years of age and outcome measurement occurring after 18) was not part of the inclusion criteria. This feature may have increased the possibility of conflating childhood abuse’s short-term effects on long-term adult consequences. Second, we did not investigate maltreatment duration nor the age at which it occurred, and no information was collected regarding who inflicted the maltreatment. Third, our sample may not be sufficiently representative. Moreover, psychiatric conditions may affect suicidal risk, regardless of the role of childhood maltreatment, hopelessness, and dissociation, limiting the study results’ generalizability to the general population. Fourth, the cross-sectional design retrospectively assessed self-report data and, thus, possible memory bias regarding child maltreatment should be considered when interpreting our results. Furthermore, patients tend to under-report abuse and suicide-related constructs, so social-desirability bias should be considered.
5. Conclusions
The present study results demonstrate that different types of childhood maltreatment increase suicidal risk in adult psychiatric patients and that hopelessness and dissociation are important mediators of this association. Moreover, an interesting result is represented by the different paths of emotional abuse and emotional neglect on suicidal ideation, suggesting the importance of conducting additional studies. In addition to psychiatric diagnoses, many psychological factors play a role in suicide. Professionals working with children should be aware of the long-term consequences of childhood maltreatment, particularly suicidal ideation. Consequently, it is important to identify factors that promote resiliency among individuals who have experienced maltreatment and protect them against increased suicide risk.
Furthermore, our results emphasize the importance for professionals working with adults to inquire about past childhood maltreatment, given the relationship between childhood maltreatment, poor clinical course, and treatment response in several psychiatric populations. Therefore, clinicians should consider the paths to suicide risk and implement interventions that take specific risk factors, such as childhood maltreatment, dissociation, and hopelessness, into account. Future studies are needed to verify and explain the relationship between childhood maltreatment and mental disorders. These studies should utilize larger prospective samples and instruments to complement self-rating scales and control for additional demographic features.
Author Contributions
Conceptualization, I.B. and M.P.; methodology, S.S. and M.I.; software, S.S. and M.I.; investigation, E.R., C.G. and D.E.; resources, E.R. and D.E.; writing—original draft preparation, I.B.; writing—review and editing, I.B. and D.A.L.; supervision, D.A.L. and M.P.; project administration, I.B. and M.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
As the assessment of psychiatric patients with particular attention to suicide risk is part of several investigations approved by the local ethics review board, the present study was derived during the previously approved recruitment of suicide risk patients. (Review Board research ethics review board approved the study protocol of Sant’ Andrea Hospital—Sapienza University of Rome, Italy (RIF. CE: 4646_2017). The study was conducted according to the guidelines of the Declaration of Helsinki.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data available on request due to restrictions, e.g., privacy or ethical. The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hussey J.M., Chang J.J., Kotch J.B. Child Maltreatment in the United States: Prevalence, Risk Factors, and Adolescent Health Consequences. Pediatrics. 2006;118:933–942. doi: 10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- 2.Finkelhor D., Turner H.A., Shattuck A., Hamby S.L. Violence, Crime, and Abuse Exposure in a National Sample of Children and Youth: An Update. JAMA Pediatr. 2013;167:614–621. doi: 10.1001/jamapediatrics.2013.42. [DOI] [PubMed] [Google Scholar]
- 3.Merrick M.T., Ford D.C., Ports K.A., Guinn A.S. Prevalence of Adverse Childhood Experiences from the 2011–2014 Behavioral Risk Factor Surveillance System in 23 States. JAMA Pediatr. 2018;172:1038–1044. doi: 10.1001/jamapediatrics.2018.2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Giano Z., Wheeler D.L., Hubach R.D. The Frequencies and Disparities of Adverse Childhood Experiences in the US. BMC Public Health. 2020;20:1327. doi: 10.1186/s12889-020-09411-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walsh K., McLaughlin K.A., Hamilton A., Keyes K.M. Trauma Exposure, Incident Psychiatric Disorders, and Disorder Transitions in a Longitudinal Population Representative Sample. J. Psychiatr. Res. 2017;92:212–218. doi: 10.1016/j.jpsychires.2017.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keyes K.M., Eaton N.R., Krueger R.F., McLaughlin K.A., Wall M.M., Grant B.F., Hasin D.S. Childhood Maltreatment and the Structure of Common Psychiatric Disorders. Br. J. Psychiatry. 2012;200:107–115. doi: 10.1192/bjp.bp.111.093062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Varese F., Smeets F., Drukker M., Lieverse R., Lataster T., Viechtbauer W., Read J., van Os J., Bentall R.P. Childhood Adversities Increase the Risk of Psychosis: A Meta-Analysis of Patient-Control, Prospective-and Cross-Sectional Cohort Studies. Schizophr. Bull. 2012;38:661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pompili M., Innamorati M., Lamis D.A., Erbuto D., Venturini P., Ricci F., Serafini G., Amore M., Girardi P. The Associations among Childhood Maltreatment, “Male Depression” and Suicide Risk in Psychiatric Patients. Psychiatry Res. 2014;220:571–578. doi: 10.1016/j.psychres.2014.07.056. [DOI] [PubMed] [Google Scholar]
- 9.Zatti C., Rosa V., Barros A., Valdivia L., Calegaro V.C., Freitas L.H., Ceresér K.M.M., Rocha N.S.D., Bastos A.G., Schuch F.B. Childhood Trauma and Suicide Attempt: A Meta-Analysis of Longitudinal Studies from the Last Decade. Psychiatry Res. 2017;256:353–358. doi: 10.1016/j.psychres.2017.06.082. [DOI] [PubMed] [Google Scholar]
- 10.Thompson M.P., Kingree J.B., Lamis D. Associations of Adverse Childhood Experiences and Suicidal Behaviors in Adulthood in a US Nationally Representative Sample. Child Care Health Dev. 2019;45:121–128. doi: 10.1111/cch.12617. [DOI] [PubMed] [Google Scholar]
- 11.Posner K., Oquendo M.A., Gould M., Stanley B., Davies M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): Classification of Suicidal Events in the FDA’s Pediatric Suicidal Risk Analysis of Antidepressants. Am. J. Psychiatry. 2007;164:1035–1043. doi: 10.1176/ajp.2007.164.7.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Angelakis I., Gillespie E.L., Panagioti M. Childhood Maltreatment and Adult Suicidality: A Comprehensive Systematic Review with Meta-Analysis. Psychol. Med. 2019;49:1057–1078. doi: 10.1017/S0033291718003823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Angelakis I., Austin J.L., Gooding P. Association of Childhood Maltreatment with Suicide Behaviors among Young People: A Systematic Review and Meta-Analysis. JAMA Netw. Open. 2020;3:e2012563. doi: 10.1001/jamanetworkopen.2020.12563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dervic K., Grunebaum M.F., Burke A.K., Mann J.J., Oquendo M.A. Protective Factors against Suicidal Behavior in Depressed Adults Reporting Childhood Abuse. J. Nerv. Ment. Dis. 2006;194:971–974. doi: 10.1097/01.nmd.0000243764.56192.9c. [DOI] [PubMed] [Google Scholar]
- 15.Beristianos M.H., Maguen S., Neylan T.C., Byers A.L. Trauma Exposure and Risk of Suicidal Ideation among Ethnically Diverse Adults. Depress. Anxiety. 2016;33:495–501. doi: 10.1002/da.22485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Mattos Souza L.D., Molina M.L., da Silva R.A., Jansen K. History of Childhood Trauma as Risk Factors to Suicide Risk in Major Depression. Psychiatry Res. 2016;246:612–616. doi: 10.1016/j.psychres.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Barbosa L.P., Quevedo L., da Silva G.D.G., Jansen K., Pinheiro R.T., Branco J., Lara D., Oses J., da Silva R.A. Childhood Trauma and Suicide Risk in a Sample of Young Individuals Aged 14–35 Years in Southern Brazil. Child Abus. Negl. 2014;38:1191–1196. doi: 10.1016/j.chiabu.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 18.Prokopez C.R., Vallejos M., Farinola R., Alberio G., Caporusso G.B., Cozzarin L.G., Chiapella L.C., Fuentes P., Daray F.M. The History of Multiple Adverse Childhood Experiences in Patients with Schizophrenia Is As-Sociated with More Severe Symptomatology and Suicidal Behavior with Gender-Specific Characteristics. Psychiatry Res. 2020;293:113411. doi: 10.1016/j.psychres.2020.113411. [DOI] [PubMed] [Google Scholar]
- 19.Agnew-Blais J., Danese A. Childhood Maltreatment and Unfavourable Clinical Outcomes in Bipolar Disorder: A Systematic Review and Meta-Analysis. Lancet Psychiatry. 2016;3:342–349. doi: 10.1016/S2215-0366(15)00544-1. [DOI] [PubMed] [Google Scholar]
- 20.Thomas S., Höfler M., Schäfer I., Trautmann S. Childhood Maltreatment and Treatment Outcome in Psychotic Disorders: A Systematic Review and Meta-Analysis. Acta Psychiatr. Scand. 2019;140:295–312. doi: 10.1111/acps.13077. [DOI] [PubMed] [Google Scholar]
- 21.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; Washington, DC, USA: 2013. [Google Scholar]
- 22.Ford J.D., Gómez J.M. Self-Injury and Suicidality: The Impact of Trauma and Dissociation. J. Trauma Dissociation. 2015;16:225–231. doi: 10.1080/15299732.2015.989648. [DOI] [PubMed] [Google Scholar]
- 23.Connors R. Self-Injury in Trauma Survivors: 1. Functions and Meanings. Am. J. Orthopsychiatry. 1996;66:197–206. doi: 10.1037/h0080171. [DOI] [PubMed] [Google Scholar]
- 24.Serafini G., Lamis D.A., Aguglia A., Amerio A., Nebbia J., Geoffroy P.A., Pompili M., Amore M. Hopelessness and Its Correlates with Clinical Outcomes in an Outpatient Setting. J. Affect. Disord. 2020;263:472–479. doi: 10.1016/j.jad.2019.11.144. [DOI] [PubMed] [Google Scholar]
- 25.Mueller-Pfeiffer C., Moergeli H., Schumacher S., Martin-Soelch C., Wirtz G., Fuhrhans C., Hindermann E., Rufer M. Characteristics of Child Maltreatment and Their Relation to Dissociation, Posttraumatic Stress Symptoms, and Depression in Adult Psychiatric Patients. J. Nerv. Ment. Dis. 2013;201:471–477. doi: 10.1097/NMD.0b013e3182948096. [DOI] [PubMed] [Google Scholar]
- 26.Courtney E.A., Johnson J.G., Alloy L.B. Associations of Childhood Maltreatment with Hopelessness and Depression among Adolescent Primary Care Patients. Int. J. Cogn. Ther. 2008;1:4–17. doi: 10.1521/ijct.2008.1.1.4. [DOI] [Google Scholar]
- 27.Kuo W.H., Gallo J.J., Eaton W.W. Hopelessness, Depression, Substance Disorder, and Suicidality—A 13-Year Community-Based Study. Soc. Psychiatry Psychiatr. Epidemiol. 2004;39:497–501. doi: 10.1007/s00127-004-0775-z. [DOI] [PubMed] [Google Scholar]
- 28.David Klonsky E., Kotov R., Bakst S., Rabinowitz J., Bromet E.J. Hopelessness as a Predictor of Attempted Suicide among First Admission Patients with Psychosis: A 10-Year Cohort Study. Suicide Life-Threat. Behav. 2012;42:1–10. doi: 10.1111/j.1943-278X.2011.00066.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Franklin J.C., Ribeiro J.D., Fox K.R., Bentley K.H., Kleiman E.M., Huang X., Musacchio K.M., Jaroszewski A.C., Chang B.P., Nock M.K. Risk Factors for Suicidal Thoughts and Behaviors: A Meta-Analysis of 50 Years of Research. Psychol. Bull. 2017;143:187–232. doi: 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- 30.Berardelli I., Belvisi D., Corigliano V., Costanzo M., Innamorati M., Fabbrini G., Berardelli A., Pompili M. Suicidal Ideation, Perceived Disability, Hopelessness and Affective Temperaments in Patients Affected by Parkinson’s Disease. Int. J. Clin. Pract. 2018;19:e13287. doi: 10.1111/ijcp.13287. [DOI] [PubMed] [Google Scholar]
- 31.Calati R., Bensassi I., Courtet P. The Link between Dissociation and Both Suicide Attempts and Non-suicidal Self-Injury: Meta-Analyses. Psychiatry Res. 2017;251:103–114. doi: 10.1016/j.psychres.2017.01.035. [DOI] [PubMed] [Google Scholar]
- 32.Brokke S.S., Bertelsen T.B., Landrø N.I., Haaland V.Ø. The Effect of Sexual Abuse and Dissociation on Suicide Attempt. BMC Psychiatry. 2022;22:29. doi: 10.1186/s12888-021-03662-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Freeman T.W., Keesee N., Thornton C., Gillette G., Young K. Dissociative Symptoms in Posttraumatic Stress Disorder Subjects with a History of Suicide Attempts. J. Nerv. Ment. Dis. 1995;183:664–666. doi: 10.1097/00005053-199510000-00010. [DOI] [PubMed] [Google Scholar]
- 34.Rodriguez-Srednicki O. Childhood Sexual Abuse, Dissociation, and Adult Self-Destructive Behavior. J. Child Sex. Abus. 2002;10:75–89. doi: 10.1300/J070v10n03_05. [DOI] [PubMed] [Google Scholar]
- 35.Zoroglu S.S., Tuzun U., Sar V., Tutkun H., Savaçs H.A., Ozturk M., Alyanak B., Kora M.E. Suicide Attempt and Self-Mutilation among Turkish High School Students in Relation with Abuse, Neglect and Dissociation. Psychiatry Clin. Neurosci. 2003;57:119–126. doi: 10.1046/j.1440-1819.2003.01088.x. [DOI] [PubMed] [Google Scholar]
- 36.Tamar-Gurol D., Sar V., Karadag F., Evren C., Karagoz M. Childhood Emotional Abuse, Dissociation, and Suicidality among Patients with Drug Dependency in Turkey. Psychiatry Clin. Neurosci. 2008;62:540–547. doi: 10.1111/j.1440-1819.2008.01847.x. [DOI] [PubMed] [Google Scholar]
- 37.Swannell S., Martin G., Page A., Hasking P., Hazell P., Taylor A., Protani M. Child Maltreatment, Subsequent Non-suicidal Self-Injury and the Mediating Roles of Dissociation, Alexithymia and Self-Blame. Child Abus. Negl. 2012;36:572–584. doi: 10.1016/j.chiabu.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 38.Bertule M., Sebre S.B., Kolesovs A. Childhood Abuse Experiences, Depression and Dissociation Symptoms in Relation to Suicide Attempts and Suicidal Ideation. J. Trauma Dissociation. 2021;22:598–614. doi: 10.1080/15299732.2020.1869652. [DOI] [PubMed] [Google Scholar]
- 39.Haatainen K.M., Tanskanen A., Kylmä J., Honkalampi K., Koivumaa-Honkanen H., Hintikka J., Antikainen R., Viinamäki H. Gender Differences in the Association of Adult Hopelessness with Adverse Childhood Experiences. Soc. Psychiatry Psychiatr. Epidemiol. 2003;38:12–17. doi: 10.1007/s00127-003-0598-3. [DOI] [PubMed] [Google Scholar]
- 40.Brenner L.A., Forster J.E., Hoffberg A.S., Matarazzo B.B., Hostetter T.A., Signoracci G., Simpson G.K. Window to Hope: A Randomized Controlled Trial of a Psychological Intervention for the Treatment of Hopelessness among Veterans with Moderate to Severe Traumatic Brain Injury. J. Head Trauma Rehabil. 2018;33:E64–E73. doi: 10.1097/HTR.0000000000000351. [DOI] [PubMed] [Google Scholar]
- 41.Erbuto D., Innamorati M., Lamis D.A., Berardelli I., Forte A., De Pisa E., Migliorati M., Serafini G., Gonda X., Rihmer Z., et al. Mediators in the Association Between Affective Temperaments and Suicide Risk among Psychiatric Inpatients. Psychiatry. 2018;81:240–257. doi: 10.1080/00332747.2018.1480251. [DOI] [PubMed] [Google Scholar]
- 42.Janiri D., De Rossi P., Kotzalidis G.D., Girardi P., Koukopoulos A.E., Reginaldi D., Dotto F., Manfredi G., Jollant F., Gorwood P., et al. Psychopathological Characteristics and Adverse Childhood Events Are Differentially Associated with Suicidal Ideation and Suicidal Acts in Mood Disorders. Eur. Psychiatry. 2018;53:31–36. doi: 10.1016/j.eurpsy.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 43.Gibb B.E., Alloy L.B., Abramson L.Y., Rose D.T., Whitehouse W.G., Hogan M.E. Childhood Maltreatment and College Students’ Current Suicidal Ideation: A Test of the Hopelessness Theory. Suicide Life-Threat. Behav. 2001;31:405–415. doi: 10.1521/suli.31.4.405.22042. [DOI] [PubMed] [Google Scholar]
- 44.Abramson L.Y., Alloy L.B., Hogan M.E., Whitehouse W.G., Gibb B.E., Hankin B.L., Cornette M.M. The Hopelessness Theory of Suicidality. In: Joiner T.E., Rudd M.D., editors. Suicide Science: Expanding Boundaries. Kluwer Academic/Plenum Publishers; New York, NY, USA: 2000. pp. 17–32. [Google Scholar]
- 45.Meadows L.A., Kaslow N.J. Hopelessness as Mediator of the Link between Reports of a History of Child Maltreatment and Suicidality in African American Women. Cognit. Ther. Res. 2008;26:657–674. doi: 10.1023/A:1020361311046. [DOI] [Google Scholar]
- 46.First M.B., Williams J.B.W., Karg R.S., Spitzer R.L. Structured Clinical Interview for DSM-5 Disorders, Clinician Version (SCID-5-CV) American Psychiatric Association; Arlington, VA, USA: 2016. [Google Scholar]
- 47.Silverman M.M., Berman A.L., Sanddal N.D., O’carroll P.W., Joiner T.E. Rebuilding the tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors. Part 1: Background, rationale, and methodology. Suicide Life-Threat Behav. 2007;37:248–263. doi: 10.1521/suli.2007.37.3.248. [DOI] [PubMed] [Google Scholar]
- 48.Silverman M.M., Berman A.L., Sanddal N.D., O’carroll P.W., Joiner T.E. Rebuilding the tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors. Part 2: Suicide-related ideations, communications, and behaviors. Suicide Life-Threat Behav. 2007;37:264–277. doi: 10.1521/suli.2007.37.3.264. [DOI] [PubMed] [Google Scholar]
- 49.Posner K., Brent D., Lucas C., Gould M., Stanley B., Brown G., Fisher P., Zelazny J., Burke A., Oquendo M., et al. Columbia-Suicide Severity Rating Scale (C-SSRS) Columbia University Medical Center; New York, NY, USA: 2008. p. 10. [Google Scholar]
- 50.Posner K., Brown G.K., Stanley B., Brent D.A., Yershova K.V., Oquendo M.A., Currier G.W., Melvin G.A., Greenhill L., Shen S., et al. The Columbia-Suicide Severity Rating Scale: Initial Validity and Internal Consistency Findings from Three Multisite Studies with Adolescents and Adults. Am. J. Psychiatry. 2011;168:1266–1277. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bernstein D.P., Fink L., Handelsman L., Foote J., Lovejoy M., Wenzel K., Sapareto E., Ruggiero J. Initial Reliability and Validity of a New Retrospective Measure of Child Abuse and Neglect. Am. J. Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 52.Bernstein D.P., Fink L.A. CTQ: Childhood Trauma Questionnaire: A retrospective Self-Report. Psychological Corp.; San Antonio, TX, USA: 1998. [Google Scholar]
- 53.Beck A.T., Steer R.A. Manual for the Beck Hopelessness Scale. 2nd ed. Psychological Corp; San Antonio, TX, USA: 1993. [Google Scholar]
- 54.Pompili M., Iliceto P., Lester D., Innamorati M., Girardi P., Tatarelli R. BHS Beck Hopelessness Scale: Manuale. Giunti O.S. Organizzazioni Speciali; Firenze, Italy: 2008. [Google Scholar]
- 55.Innamorati M., Lester D., Balsamo M., Erbuto D., Ricci F., Amore M., Girardi P., Pompili M. Factor validity of the Beck Hopelessness Scale in Italian medical patients. J. Psychopathol. Behav. Assess. 2014;36:300–307. doi: 10.1007/s10862-013-9380-3. [DOI] [Google Scholar]
- 56.Beck A.T., Brown G., Berchick R.J., Stewart B.L., Steer R.A. Relationship between Hopelessness and Ultimate Suicide: A Replication with Psychiatric Outpatients. Am. J. Psychiatry. 1990;147:190–195. doi: 10.1176/foc.4.2.291. [DOI] [PubMed] [Google Scholar]
- 57.Granö N., Oksanen J., Kallionpää S., Roine M. Specificity and Sensitivity of the Beck Hopelessness Scale for Suicidal Ideation among Adolescents Entering Early Intervention Service. Nord. J. Psychiatry. 2017;71:72–76. doi: 10.1080/08039488.2016.1227370. [DOI] [PubMed] [Google Scholar]
- 58.McMillan D., Gilbody S., Beresford E., Neilly L. Can we predict suicide and non-fatal self- harm with the Beck Hopelessness Scale? A meta-analysis. Psychol. Med. 2007;37:769–778. doi: 10.1017/S0033291706009664. [DOI] [PubMed] [Google Scholar]
- 59.Bernstein E.M., Putnam F.W. Development, Reliability, and Validity of a Dissociation Scale. J. Nerv. Ment. Dis. 1986;174:727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- 60.Carlson E.B., Putnam F.W. An Update on the Dissociative Experiences Scale. Dissociation. 1993;6:16–27. [Google Scholar]
- 61.Mazzotti E., Farina B., Imperatori C., Mansutti F., Prunetti E., Speranza A.M., Barbaranelli C. Is the Dissociative Experiences Scale able to identify detachment and compartmentalization symptoms? Factor structure of the Dissociative Experiences Scale in a large sample of psychiatric and nonpsychiatric subjects. Neuropsychiatr. Dis. Treat. 2016;12:1295–1302. doi: 10.2147/NDT.S105110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Muthén L.K., Muthén B. Mplus. The Comprehensive Modelling Program for Applied Researchers: User’s Guide. 5th ed. Muthén & Muthén; Los Angeles, CA, USA: 2018. [Google Scholar]
- 63.Kline R.B. Principles and Practice of Structural Equation Modeling. 2nd ed. Guilford; New York, NY, USA: 2005. [Google Scholar]
- 64.Hart S.N., Brassard M.R., Karlson H.C. Psychological Maltreatment. In: Brier J., Berliner L., Bulkley J.A., Jenny C., Raid T., editors. The APSAC Handbook on Child Maltreatment. Sage Publications; Thousand Oaks, CA, USA: 1996. pp. 72–89. [Google Scholar]
- 65.Lin L., Du Q.Q., Hu N.B., Jia G.Z., Wang P.Y. Study on the Correlation between Childhood Neglect and Coping Styles of Middle School Students. Chin. J. Child Health Care. 2012;20:890–892. [Google Scholar]
- 66.Liu J., Fang Y., Gong J., Cui X., Meng T., Xiao B., He Y., Shen Y., Luo X. Associations between Suicidal Behavior and Childhood Abuse and Neglect: A Meta-Analysis. J. Affect. Disord. 2017;220:147–155. doi: 10.1016/j.jad.2017.03.060. [DOI] [PubMed] [Google Scholar]
- 67.McGee R.A., Wolfe D.A., Wilson S.K. Multiple Maltreatment Experiences and Adolescent Behavior Problems: Adolescents’ Perspectives. Dev. Psychopathol. 1997;9:131–149. doi: 10.1017/S0954579497001107. [DOI] [PubMed] [Google Scholar]
- 68.Martins-Monteverde C.M.S., Baes C.V.W., Reisdorfer E., Padovan T., Tofoli S.M.D.C., Juruena M.F. Relationship between Depression and Subtypes of Early Life Stress in Adult Psychiatric Patients. Front. Psychiatry. 2019;10:19. doi: 10.3389/fpsyt.2019.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Abramson L.Y., Metalsky G.I., Alloy L.B. Hopelessness Depression: A Theory-Based Subtype of Depression. Psychol. Rev. 1989;96:358. doi: 10.1037/0033-295X.96.2.358. [DOI] [Google Scholar]
- 70.Freyd J.J. Betrayal Trauma: Traumatic Amnesia as an Adaptive Response to Childhood Abuse. Ethics Behav. 1994;4:307–329. doi: 10.1207/s15327019eb0404_1. [DOI] [Google Scholar]
- 71.Brown J., Cohen P., Johnson J.G., Smailes E.M. Childhood Abuse and Neglect: Specificity of Effects on Adolescent and Young Adult Depression and Suicidality. J. Am. Acad. Child Adolesc. Psychiatry. 1999;38:1490–1496. doi: 10.1097/00004583-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 72.Eisenberg M.E., Ackard D.M., Resnick M.D. Protective Factors and Suicide Risk in Adolescents with a History of Sexual Abuse. J. Pediatr. 2007;151:482–487. doi: 10.1016/j.jpeds.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 73.Bahk Y.C., Jang S.K., Choi K.H., Lee S.H. The Relationship between Childhood Trauma and Suicidal Ideation: Role of Maltreatment and Potential Mediators. Psychiatry Investig. 2017;14:37–43. doi: 10.4306/pi.2017.14.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hailes H.P., Yu R., Danese A., Fazel S. Long-Term Outcomes of Childhood Sexual Abuse: An Umbrella Review. Lancet Psychiatry. 2019;6:830–839. doi: 10.1016/S2215-0366(19)30286-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Alloy L.B., Abramson L.Y., Smith J.M., Gibb B.E., Neeren A.M. Role of Parenting and Maltreatment Histories in Unipolar and Bipolar Mood Disorders: Mediation by Cognitive Vulnerability to Depression. Clin. Child Fam. Psychol. Rev. 2006;9:23–64. doi: 10.1007/s10567-006-0002-4. [DOI] [PubMed] [Google Scholar]
- 76.Teicher M.H., Andersen S.L., Polcari A., Anderson C.M., Navalta C.P., Kim D.M. The Neurobiological Consequences of Early Stress and Childhood Maltreatment. Neurosci. Biobehav. Rev. 2003;27:33–44. doi: 10.1016/S0149-7634(03)00007-1. [DOI] [PubMed] [Google Scholar]
- 77.Demirkol M.E., Uğur K., Tamam L. The Mediating Effects of Psychache and Dissociation in the Relationship between Childhood Trauma and Suicide Attempts. Anadolu. Psikiyatri. Derg. 2020;21:453–460. doi: 10.5455/apd.82990. [DOI] [Google Scholar]
- 78.Savitz J.B., van der Merwe L., Stein D.J., Solms M., Ramesar R.S. Neuropsychological Task Performance in Bipolar Spectrum Illness: Genetics, Alcohol Abuse, Medication and Childhood Trauma. Bipolar Disord. 2008;10:79–94. doi: 10.1111/j.1399-5618.2008.00591.x. [DOI] [PubMed] [Google Scholar]
- 79.McLaughlin K.A., Colich N.L., Rodman A.M., Weissman D.G. Mechanisms Linking Childhood Trauma Exposure and Psychopathology: A Transdiagnostic Model of Risk and Resilience. BMC Med. 2020;18:96. doi: 10.1186/s12916-020-01561-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jaworska-Andryszewska P., Rybakowski J.K. Childhood Trauma in Mood Disorders: Neurobiological Mechanisms and Implications for Treatment. Pharmacol. Rep. 2019;71:112–120. doi: 10.1016/j.pharep.2018.10.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request due to restrictions, e.g., privacy or ethical. The data presented in this study are available on request from the corresponding author.