Abstract
The spread of multidrug-resistant (MDR) Vibrio cholerae necessitates the development of novel prevention and treatment strategies. This study aims to evaluate the in vitro antibacterial activity of green tea polyphenol (−)-epigallocatechin-3-gallate (EGCG) against MDR V. cholerae. First, MIC and MBC values were evaluated by broth microdilution techniques against 45 V. cholerae strains. The checkerboard assay was then used to determine the synergistic effect of EGCG and tetracycline. The pharmaceutical mode of action of EGCG was clarified by time-killing kinetics and membrane disruption assay. Our results revealed that all of the 45 clinical isolates were susceptible to EGCG, with MIC and MBC values in the range of 62.5–250 µg/mL and 125–500 µg/mL, respectively. Furthermore, the combination of EGCG and tetracycline was greater than either treatment alone, with a fractional inhibitory concentration index (FICI) of 0.009 and 0.018 in the O1 and O139 representative serotypes, respectively. Time-killing kinetics analysis suggested that EGCG had bactericidal activity for MDR V. cholerae after exposure to at least 62.5 µg/mL EGCG within 1 h. The mode of action of EGCG might be associated with membrane disrupting permeability, as confirmed by scanning electron microscopy. This is the first indication that EGCG is a viable anti-MDR V. cholerae treatment.
Keywords: antimicrobial activity, EGCG, green tea, MDR, Vibrio cholerae
1. Introduction
Cholera is an acute diarrhoeal infection caused by consuming contaminated food or water containing Vibrio cholerae, a gram-negative bacteria. V. cholerae infection can kill within hours if left untreated, especially with serogroups O1 and O139, which have the potential to cause cholera outbreaks throughout the world [1]. According to the most recent global burden estimate, there are approximately 1.3 to 4.0 million cholera cases per year, with 21,000 to 143,000 deaths worldwide [2]. Despite the availability of a vaccine, 923,037 cases were reported from 31 countries in 2019, with 1911 deaths (a mortality rate of 0.2%) [3]. As a consequence, the World Health Organization (WHO) aims to decrease cholera deaths by 90% by 2030 [4].
The primary treatment for V. cholerae was oral rehydration therapy in combination with antimicrobial agents, such as tetracycline, fluoroquinolones, and azithromycin [5]. Treatment failures have become more common in recent years as a result of the recurrence of antimicrobial-resistant V. cholerae [6,7,8,9,10]. The emergence of drug-resistant V. cholerae is a global health concern because the infections seem to be severe and difficult to treat. Infections with drug-resistant V. cholerae could lead to higher case fatality rates, longer hospitalizations, more secondary infections, and higher health-care costs in various countries, including Thailand [11]. Previously, we reported that 61.5% (48 of 78 isolates) of V. cholerae isolates between 1991 and 2013 were antimicrobial-resistant strains, with 56.3% of them being multidrug resistant (MDR), and conferring resistance to three or more antimicrobial classes [12]. It is important to note that the development of antibiotic resistance outpaces the development of new drugs, resulting in a global problem with long-term negative consequences. Therefore, the finding of alternative anti-Vibrio compounds, particularly those derived from plants, has become critical.
Green tea (Camellia sinensis) is a well-known natural source of polyphenols, including phenolic acids (caffeic acid and gallic acid) and flavonoids. Catechins from green tea belong to the family of flavonoids containing flavan-3-ol units and galloylated catechins. Green tea catechins are characterized by the presence of a benzopyran structure with at least one aromatic ring (Figure S1) [13,14]. Numerous studies have found that drinking green tea provides a wide range of health benefits, including antimicrobial activity against a variety of organisms [15,16,17]. 120 mL of green tea infusion contains approximately 150 mg of catechins, which includes 10–15% (−)-epigallocatechin gallate (EGCG), 6–10% (−)-epigallocatechin (EGC), 2–3% (−)-epicatechin gallate (ECG), and 2% (−)-epicatechin gallate (EC) [18,19]. Green tea consumption has been shown to distribute these compounds and/or their metabolites throughout the body, allowing for not only the treatment of infection, but also its prevention [20]. EGCG is the most effective biological compound for anti-infective properties, i.e., against viruses, bacteria, and fungi [21,22,23]. Green tea catechins exhibit broad antibacterial activity against both gram-positive and gram-negative bacteria through a variety of mechanisms, including the inhibition of cell wall and cell membrane synthesis, protein and nucleic acid synthesis, or the inhibition of metabolic pathways, such as toxins and extracellular matrix virulence factors, oxidative stress, iron chelation, and so on [16,17,24]. For V. cholerae, green tea catechins reveal the inhibition of bacterial growth and/or cholera toxin secretion [25,26]. Moreover, an in vivo study indicated that catechins, especially EGCG at a concentration of 0.5 to 1.0 mg/mL, had anti-cholera activity by inhibiting cholera toxin-induced fluid accumulation in mice and preventing V. cholerae infection in rabbits, using the rabbit ileal loop model [27,28]. However, there have been few reports of data, and the mechanism remains unknown.
As a consequence, we shed light on the potential antimicrobial properties of EGCG against MDR V. cholerae by examining its antimicrobial activity and investigating its synergistic effects with the antibiotic tetracycline. Furthermore, we also assess the pharmacological mode of action of EGCG with respect to the potential disruption of the membrane of the microorganisms and its effect on bacterial morphology, which may be useful in bringing about a new opportunity in complementary and alternative medicine.
2. Results
2.1. EGCG Inhibits Drug Resistant V. cholerae Strains
We investigated the minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) of EGCG on the 45 V. cholerae clinical strains that maintained an antibiotic resistance pattern, such as streptomycin (STM), colistin (COL), nalidixic acid (NAL), sulfamethoxazole (SMX), tetracycline (TET), trimethoprim (TMP), ciprofloxacin (CIP), and azithromycin (AZI). The results, which are expressed as MIC and MBC values in Table 1, showed that all 45 isolates were sensitized to EGCG by expressed MIC values of 62.5 to 250 µg/mL, while MBC values were 125 to 500 µg/mL. The most effective against clinical strains had a MIC of 125 µg/mL (29/45), followed by 62.5 µg/mL (15/45), and 250 µg/mL (1/45), which corresponds to 64.44%, 33.33%, and 2.22%, respectively. Meanwhile, the bactericidal activity of EGCG showed MBC values of 250 µg/mL (29/45), followed by 125 µg/mL (15/45) and 500 µg/mL (1/45), as shown in Table S1. On the other hand, the MIC and MBC values of tetracycline–a positive control antibiotic–for drug-resistant V. cholerae strains were shown to range from 0.48 to 62.5 µg/mL and 0.97 to 125 µg/mL, respectively (Table S2). This suggests that the effects of EGCG on antimicrobial activities vary depending on the V. cholerae clinical strains.
Table 1.
MIC and MBC of EGCG for a total of 45 drug resistant V. cholerae strains.
| No. | Strain | Serogroup/Serotype/Serovar | MIC (µg/mL) | MBC (µg/mL) |
|---|---|---|---|---|
| 1 | N16961 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 2 | P33 | V. cholerae O1 El Tor Ogawa | 62.5 | 125 |
| 3 | P34 | V. cholerae O1 El Tor Inaba | 62.5 | 125 |
| 4 | P35 | V. cholerae O1 El Tor Inaba | 62.5 | 125 |
| 5 | P36 | V. cholerae O1 El Tor Ogawa | 62.5 | 125 |
| 6 | P38 | V. cholerae O1 El Tor Inaba | 250 | 500 |
| 7 | P39 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 8 | P41 | V. cholerae O1 El Tor Ogawa | 62.5 | 125 |
| 9 | P42 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 10 | P43 | V. cholerae O1 El Tor Inaba | 62.5 | 125 |
| 11 | P44 | V. cholerae O1 El Tor Inaba | 62.5 | 125 |
| 12 | P45 | V. cholerae O1 El Tor Ogawa | 125 | 250 |
| 13 | P46 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 14 | P47 | V. cholerae O1 El Tor Ogawa | 62.5 | 125 |
| 15 | P48 | V. cholerae O1 El Tor Ogawa | 125 | 250 |
| 16 | 22115 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 17 | 22116 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 18 | 22118 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 19 | 22125 | V. cholerae O1 El Tor Ogawa | 125 | 250 |
| 20 | 22126 | V. cholerae O1 El Tor Ogawa | 125 | 250 |
| 21 | 22127 | V. cholerae O1 El Tor Ogawa | 125 | 250 |
| 22 | 22135 | V. cholerae O139 | 62.5 | 125 |
| 23 | 22136 | V. cholerae O139 | 125 | 250 |
| 24 | 22137 | V. cholerae O139 | 125 | 250 |
| 25 | 22138 | V. cholerae O139 | 125 | 250 |
| 26 | 22144 | V. cholerae non-O1, non-O139 | 125 | 250 |
| 27 | 4053022001 | V. cholerae O1 El Tor Ogawa | 125 | 250 |
| 28 | 4053023816 | V. cholerae O1 El Tor Inaba | 62.5 | 125 |
| 29 | 4053023817 | V. cholerae O1 El Tor Ogawa | 125 | 250 |
| 30 | 4053023818 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 31 | 4053023822 | V. cholerae O1 El Tor Ogawa | 62.5 | 125 |
| 32 | 4053023823 | V. cholerae O1 El Tor Inaba | 62.5 | 125 |
| 33 | 4053023826 | V. cholerae O1 El Tor Inaba | 62.5 | 125 |
| 34 | 4053023828 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 35 | 4053023829 | V. cholerae O1 El Tor Inaba | 62.5 | 125 |
| 36 | 4053023830 | V. cholerae O1 El Tor Ogawa | 125 | 250 |
| 37 | 4053024283 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 38 | 4053024290 | V. cholerae O1 El Tor, Inaba | 125 | 250 |
| 39 | 4053024292 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 40 | 4053024293 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 41 | 4053024294 | V. cholerae O1 El Tor Inaba | 62.5 | 125 |
| 42 | 4053024295 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 43 | 4053024296 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 44 | 4053024297 | V. cholerae O1 El Tor Inaba | 125 | 250 |
| 45 | 4053024299 | V. cholerae O1 El Tor Inaba | 125 | 250 |
Abbreviations: EGCG, (−)-epigallocatechin gallate; MIC, minimum inhibitory concentration; MBC, minimum bactericidal concentration.
Considering MDR V. cholerae as a potential threat to public health, we investigated the synergistic effect of EGCG and tetracycline, the WHO-recommended first-line drug choice for cholera treatment, in the representative MDR strains, P48 V. cholerae O1 El Tor Ogawa, as well as 22,136 V. cholerae O139 strains. It is important to note that the P48 O1 strain is a six-drug resistance strain (AZI, COL, NAL, SMX, TET, and TMP), whereas 22,136 O139 is a three-drug resistance strain (COL, SMX, TMP). Both serogroups were chosen as representative strains for future study because they carried the virulence genes up to 10 genes, i.e., ctxA, ctxB, zot, ace, tcpA, hlyA, rtxA, ompU, toxR, and mshA, which are highest among O1 and O139 strains [29]. Table 2 shows the evaluation of the synergistic effect of EGCG and tetracycline. In both standard and MDR strains, the combination effect on bacterial growth appeared to be greater than treatment alone (MIC 125 µg/mL), where the combination treatment reduced the MIC value to 0.97 µg/mL. It is important to note that the fractional inhibitory concentration index (FICI) is 0.009 for the O1 (P48) and reference strain, and 0.018 for the O139 (22136) strains. These results indicate that combining EGCG with tetracycline might be a more effective treatment for MDR V. cholerae than either treatment alone.
Table 2.
Synergistic effect of EGCG in combination with tetracycline against reference and V. cholerae MDR strains.
| Strain | MIC (µg/mL) of Extracts (a) | FIC (a) | MIC (µg/mL) of Tetracycline (b) | FIC (b) | FICI | Outcome | ||
|---|---|---|---|---|---|---|---|---|
| Alone | Combination | Alone | Combination | |||||
| P48 (O1) | 125.0 | 0.97 | 0.008 | 62.5 | 0.061 | 0.001 | 0.009 | Synergistic |
| 22136 (O139) | 125.0 | 0.97 | 0.008 | 0.78 | 0.008 | 0.01 | 0.018 | Synergistic |
| N16961 (Reference) |
125.0 | 0.97 | 0.008 | 3.91 | 0.004 | 0.001 | 0.009 | Synergistic |
Abbreviations: EGCG, (−)-epigallocatechin gallate; FIC, fractional inhibitory concentration; FICI, fractional inhibitory concentration index; MIC, minimum inhibitory concentration. FIC (a) = MIC of EGCG in the combination/MIC of EGCG alone; FIC (b) = MIC of tetracycline in the combination/MIC of tetracycline alone; FICI = FIC (a) + FIC (b). The values were interpreted as a synergistic effect for FICI ≤ 0.5.
2.2. Analysis of Bacterial Killing Kinetics
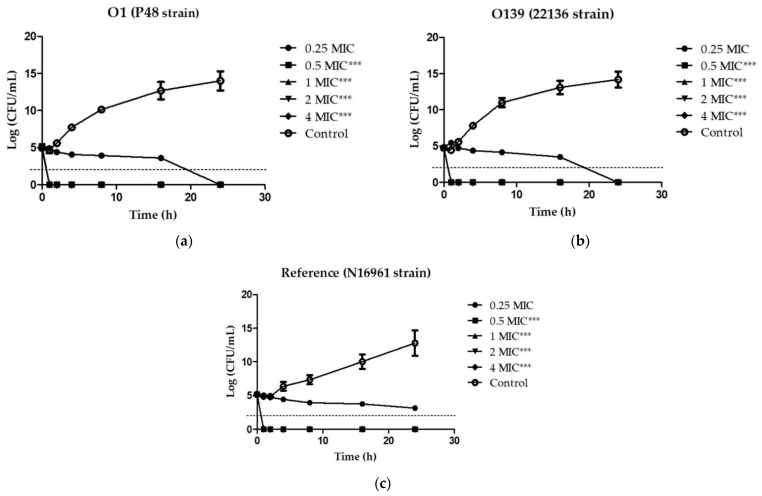
We then investigated the time-kill kinetics of EGCG on the viability of V. cholerae O1 and O139 in order to define the bactericidal level, using a 0.25 to 4-fold MIC treatment. Figure 1 demonstrates the time-killing curve analysis. The kill kinetic profiles of 0.5× MIC (62.5 µg/mL), 1× MIC (125 µg/mL), 2× MIC (250 µg/mL), and 4× MIC (500 µg/mL) of EGCG displayed rapid bactericidal activity in all tested strains, with an approximate colony-forming units (CFU) reduction of 3 log units in viable cell count relative to the initial inoculum at all tested concentrations within 1 h, whereas 0.25× MIC (31.25 µg/mL) demonstrated a time-dependent killing property after EGCG treatment in the O1 and O139 clinical strains. However, no bactericidal effect was observed when the bacterial cultures were treated with 0.25× MIC of EGCG in the reference strain (Figure 1c). In contrast, the bacteria performed exponential growth in the absence of EGCG treatment by increasing to approximately 15 log units within 24 h. As a result, it was clear that EGCG was bacteriostatic against V. cholerae O1 and O139 MDR strains.
Figure 1.
Effect of EGCG on the viability of V. cholerae. Time-kill kinetics of V. cholerae O1 (a), O139 (b) and reference strain (c) at concentrations of 0.25× to 4× MIC against V. cholerae were investigated over a 24 h incubation period at 37 °C. The MIC for EGCG were 125 µg/mL for all strains. MHB was used as the control instead of compound. Samples were taken at 1, 2, 4, 8, 16, and 24 h, to determine viable bacterial numbers. The bactericidal level is indicated by the dashed lines. Significant differences compared to untreated controls at 1 h are indicated by asterisks: *** p < 0.001.
2.3. EGCG Disrupts V. cholerae Membrane Permeability
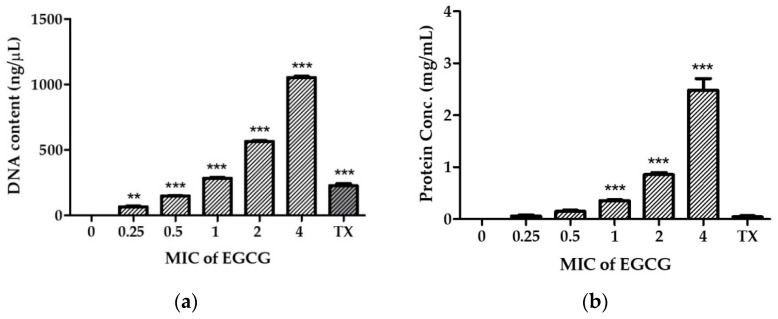
To investigate the mechanism of EGCG on the damaged bacterial cell membrane of the V. cholerae reference strain, an effective drug permeability barrier of the gram-negative cell wall, we measured nucleotide and protein leakage, N-phenyl-1-naphthylamine (NPN) uptake, and Rhodamine 123 (Rh123) incorporation, as shown in Figure 2. Bacterial cells were treated with EGCG at various concentrations of 0.25× to 4× MIC (31.25 µg/mL to 500 µg/mL) for 1 h.
Figure 2.
Effect of EGCG on membrane permeability. V. cholerae N16961 was treated with EGCG at concentrations of 0.25× MIC to 4× MIC for 2 h at 37 °C. Intracellular leakage of nucleotides (a) and proteins (b) were measured, and 0.1% Triton X-100 (TX) was used as a positive control. The outer membrane disruption and membrane potential dissipation were investigated in terms of the Relative Fluorescence Intensity (RFI) percentages of NPN (c) and Rh123 (d). Significant differences compared to untreated controls are indicated by asterisks: * p < 0.05, ** p < 0.01, *** p < 0.001.
The leakage of genetic materials, i.e., DNA, and the amount of protein passing through the bacterial membrane was used to reveal the action of EGCG on the integrity of the membrane. The disruption of the membrane was determined by measuring the cell constituents released; this was done by assessing the absorbance in the supernatant of the bacterial culture treated with EGCG. The results, summarized as the DNA content and protein concentration (Figure 2a,b, respectively), indicated that the released cell constituents increased significantly, in an EGCG concentration-dependent manner.
The outer membrane permeabilization of V. cholerae was determined using the NPN uptake assay, where NPN is a neutral hydrophobic fluorescent probe. NPN cannot normally insert into intact bacteria membranes; however, when EGCG disrupts the outer membrane, it gains access to lipid layers in the outer membrane and/or the cytoplasmic membrane, increasing the intensity of its fluorescence emission. As shown in Figure 2c, EGCG slightly permeabilized the outer membrane in a dose-dependent manner, as indicated by an increase in NPN fluorescence. It is important to note that 0.5 mg/mL of EGCG (4× MIC) showed a significant permeabilized cell membrane, equivalent to the positive control Triton X-100. Moreover, we also investigated transmembrane potential activity by staining with Rh123. Considering that Rh123 uptake is proportional to the membrane potential, the results show that EGCG strongly reduces the transmembrane potential in a dose-dependent manner (Figure 2d).
These findings suggest that EGCG may interfere with membrane potential activity, resulting in increased membrane permeability, which causes intracellular ingredient leakage and cell death.
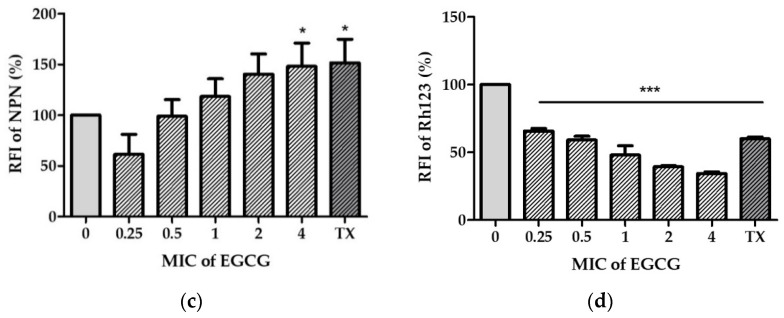
2.4. EGCG Altered the Morphological Characterization of V. cholerae
Finally, SEM was used to compare the morphological changes in the appearance of cells with and without 0.5 mg/mL of EGCG exposure. Figure 3 shows SEM images of bacterial cells at ×10,000 and ×20,000 magnifications. The untreated control bacteria had a smooth, compact surface with an intact cell membrane and no surface ruptures (Figure 3a,b). In contrast, after 2 h of exposure to EGCG, the cell was found to be severely disrupted, with membrane corrugations due to withering, wrinkling, and damage, as indicated by the arrow in Figure 3d. Thus, EGCG treatment of bacterial cells typically interferes with the integrity of the cell membranes, resulting in morphological changes that allow for intracellular material leakage, cell membrane shrinkage, and ultimately, cell death.
Figure 3.
Effect of EGCG on bacterial cell morphology. V. cholerae N16961 was treated for 2 h at 37 °C with EGCG 0.5 mg/mL. Scanning electron microscopy (SEM) images at ×10,000 and ×20,000 magnifications were demonstrated: (a,b) are the controls, (c,d) are the effective treatments. The cell membrane disruption is represented by the arrow.
3. Discussion
According to the WHO report, antimicrobial resistance is one of the top 10 global public health threats facing humanity. This resistance is due to the misuse and overuse of drugs, which has resulted in the decreased efficacy of antibiotics [30]. Anti-cholera medications are some of the drugs affected. As a consequence, alternative therapeutic approaches are in high demand. EGCG and green tea catechins have been shown to have a variety of pharmacologically beneficial effects on humans.
Here, our results strongly indicate that EGCG has anti-cholera properties in the MDR V. cholerae strains, similar to a previous report where the phytochemical phenolic compounds derived from Piper betle leaf extract (Piper betle L.), i.e., piperidine, chlorogenic acid and eugenyl acetate, were all shown to be equally effective against MDR strains of V. cholerae [31,32,33]. Moreover, natural compounds had antimicrobial activity against V. cholerae, including procyanidins from Guazuma (Guazuma ulmifolia) [34], gallate analogues from Daio (Rhei rhizoma) [35], apelphenon from apple (Malus spp.) [36], procyanidins from hop (Humulus lupulus) [37], oil (diallyl sulphides) from elephant garlic (Allium ampleloprasum) [38], and capsaicin from red chili (Capsicum annum) [39,40]. Carvacrol, a major essential oil fraction of oregano (Origanum vulgare), inhibited the virulence of V. cholerae by inhibiting mucin penetration, adhesion, and the expression of virulence-associated genes (tcpA, ctxB, hlyA and toxT), resulting in reduced fluid accumulation [41]. On the other hand, cranberry (Vaccinium macrocarpon) extract inhibited V. cholerae biofilm formation, possibly by modulating the cyclic dimeric guanosine monophosphate (c-di-GMP) level [42]. Furthermore, methanolic extracts of basil (Ocimum basilicum L.), nopal cactus (Opuntia ficus-indica var. Villanueva L.), sweet acacia (Acacia farnesiana L.), and white sagebrush (Artemisia ludoviciana Nutt.) were found to be the most active against V. cholerae via cell membrane disruption [43]. Although several studies have reported anti-cholera infection with natural product extracts, as mentioned above, to the best of our knowledge, this is the first report of antibacterial activity of EGCG against MDR V. cholerae strains. According to our findings, EGCG has a synergistic effect with tetracycline. EGCG has long been recognized as a potentially synergistic compound with antibiotics in MDR bacterial clinical strains, such as Mycobacterium smegmatis [44], methicillin-resistant Staphylococcus aureus (MRSA) [45,46], Escherichia coli [47], and Acinetobacter baumannii [48].
The modes of action of EGCG and green tea catechins against gram-positive and gram-negative antibacterial activity are classified as follows: (1) inhibition of virulence factors (toxins and extracellular matrix); (2) disruption of cell walls and membranes; (3) inhibition of intracellular enzymes; (4) oxidative stress; (5) DNA damage; and (6) iron chelation [24,49]. The mechanism of action of EGCG is associated with membrane disruption in bacteria cells, such as binding to the bacterial cell membrane, damaging the bacterial cell membrane, inhibiting the ability of bacteria to bind to host cells, inhibiting the ability of bacteria to form biofilms, disrupting bacterial quorum sensing, and interfering with bacterial membrane transporters [20]. However, the mechanism of antibacterial action of EGCG in V. cholerae has not yet been reported. Many virulent factors are involved in V. cholerae infection, including cholera toxin (haemolysins), toxin coregulated plus (TCP), adhesin factor (ACF), hemagglutination-protease (hap, mucinase), neuramindase, siderophores, and outer membrane proteins, and lipopolysaccharides [50]. Therefore, the modes of action and target sites of EGCG might vary considerably. During bacterial infection, the outer membrane prevents the entry of noxious compounds into the cell, helping them recognize the host and facilitate colonization. This prompted us to speculate that EGCG may influence bacterial membrane permeabilization. As expected, EGCG disrupts the integrity of V. cholerae cell membranes by causing intracellular material leakage of both protein and nucleotide, resulting in cell membrane shrinkage and morphological changes that allow for cell death.
However, for future studies, we need to investigate the other modes of action of EGCG, such as virulence gene expression inhibition, as well as the efficacy, safety in animal models and finally, in clinical trials.
4. Materials and Methods
4.1. Chemicals
EGCG, with more than 98% purity, was kindly provided by Prof. Masami Suganuma at Saitama University (Saitama, Japan). It was extracted from Japanese green tea leaves (Camellia sinensis L., O. Kuntze, Theaceae) that were cultured at the Saitama Prefectural Tea Institute in Saitama Prefecture, Japan, as described previously [19,51]. Mueller Hinton Broth (MHB) and Muller Hinton Agar (MHA) were purchased from HiMedia (Mumbai, Maharashtra, India). Rh123, Triton X-100, Glutaraldehyde, and Osmium tetroxide (OsO4) were obtained from Sigma Aldrich (St Louis, MO, USA). Resazurin AR (ALPHA CHEMIKA, Mumbai, Maharashtra, India), Tetracycline hydrochloride (PanReac AppliChem, Barcelona, Spain), NPN (TCI, Tokyo, Japan), Bio-Rad DC Protein Assay kit, and bovine serum albumin (BSA) (Bio-Rad Laboratories, Hercules, CA, USA) were used for the experiments.
4.2. Bacterial Strains
A total of 45 clinical strains of V. cholerae were isolated from stools and rectal swabs, including serogroups O1 and O139, and non-O1/non-O139 strains, originating from Thailand (1983 to 2013). The antimicrobial resistance patterns were characterized in a previous study [12]. V. cholerae N16961 was used as a standard reference strain.
4.3. Determination of the MIC and the MBC
The MIC values were determined using a 96-well microtiter plate, according to the Clinical and Laboratory Standards Institute (CLSI) guidelines [52], with slight modification, as described in the previous study [53,54]. EGCG was freshly prepared in phosphate buffered saline (PBS) and ethanol at a final concentration of 20%, which was then delicately diluted by using two-fold serial dilution from a concentration of 4.0 mg/mL to 1.95 µg/mL in MHB with 1% NaCl. All wells were inoculated with V. cholerae at a final volume of 100 µL of bacterial inoculum (5 × 105 CFU/mL). After incubation for 24 h at 37 °C, 1 mg/mL resazurin was added to all wells (10 µL per well), and incubation then continued for a further 4 h for observation of colour change. The wells with no colour change were appraised as being above the MIC value [55]. On the other hand, the MBC was determined by dropping 10 µL from the wells with concentrations higher than the MIC value directly onto MHA plates and incubating at 37 °C for 24 h. The MBC value was determined when there was no colony growth. Tetracycline, the first line treatment for cholera disease, was used as a positive control [43,56], and media solution was used as a negative control.
4.4. Antimicrobial Synergy Testing
The checkerboard assay, which is a two-dimensional array of serial concentrations of test compounds, as previously described [57], was used to determine the potential synergistic activity of EGCG and tetracycline on V. cholerae N16961, and also on P48 and 22136, a reference and tetracycline-resistant strain of O1 and O139, respectively. EGCG and tetracycline were prepared in 96-well microtiter plates using two-fold serial dilution based on the MIC of each substance. A final bacterial suspension at 5 × 105 CFU/mL was added to each well. After incubation for 24 h at 37 °C, the synergistic MIC was determined. The observed MIC values were used to calculate the fractional inhibitory concentration (FIC) index; this index allows evaluation of the combined effects of an antibiotic and a compound according to the following formula:
| FIC (a) = MIC of EGCG in the combination/MIC of EGCG alone; | (1) |
| FIC (b) = MIC of tetracycline in the combination/MIC of tetracycline alone; | (2) |
| FIC index = FIC (a) + FIC (b) | (3) |
These values were interpreted as follows: for FIC index ≤ 0.5, a synergistic effect; for FIC index > 0.5 and ≤ 4, an additive effect; and for FIC index > 4, an antagonistic effect [58,59].
4.5. Time-Kill Kinetics Assay
The killing kinetics of EGCG at 0.25×, 0.5×, 1×, 2× and 4× MIC values were determined using the method described previously [60,61,62], with slight modifications. Different concentrations of EGCG were added to each final volume of 100 μL with 1 × 105 CFU/mL of V. cholerae N16961 (reference), P48 (O1), and 22136 (O139) stains grown in MHB containing 1% NaCl and kept at 37 °C. Bacterial growth was monitored over a time-course of 24 h (0, 1, 2, 4, 8, 16, 24 h). A sample without the compound served as a growth control. To evaluate the survival of pandemic strains during the observation period, aliquots of serial dilutions of the bacterial suspensions were determined by a spread plate technique on MHA with 1% NaCl, and the plates were incubated at 37 °C for 24 h to evaluate the viable bacterial colony counts. Data were analysed as killing curves by plotting the log10 CFU/mL versus time (h), and the change in bacterial concentration was determined. The viable bacterial cell count for the time-kill end point determination, i.e., the bactericidal activity, is defined as a reduction of ≥3 log10 CFU/mL relative to the initial inoculum, whereas bacteriostatic activity corresponds to <3 log10 CFU/mL decrease relative to the initial inoculum [63].
4.6. Outer Membrane Permeabilization Analysis
4.6.1. Determination of Nucleotide and Protein Leakage
The integrity of the cell membrane can be monitored by the release of cytoplasmic constituents of the cell, using the method described by Lou and others [64], with some modifications. In brief, the V. cholerae N16961 cells were cultured overnight at 37 °C. The cells were washed and resuspended at a concentration of 1 × 107 CFU/mL in PBS, pH 7.2. One millilitre of these suspensions was then incubated with EGCG at concentrations of 0.25×, 0.5×, 1×, 2× and 4× MIC at 37 °C for 1 h. After centrifugation, the supernatant samples were immediately filtered through a 0.2 μm organic membrane. To determine the amounts of DNA released from the cytoplasm, the supernatant was used to measure the optical density at 260 nm using a NANO-400A Micro Spectrophotometer (Hangzhou Allsheng Instruments Co.,Ltd. Hangzhou, China). Cell integrity was further examined by determining the release of proteins into the supernatant. The Bradford dye-binding reagent of the Bio-Rad DC Protein Assay kit (Bio-Rad Laboratories, Inc., Hercules, CA, USA) was used to determine the protein amount by measuring the optical density (OD) of the resulting solution at 750 nm within 5 min. The protein quantity of each sample was determined from the equation of the best-fit linear regression obtained from the BSA standard curve. Triton X-100 (0.1%; v/v) was used as a positive control, while PBS inoculated with the same inoculum was used as a negative control.
4.6.2. Determination of Outer Membrane Disruption
The effect of EGCG on the bacterial outer membrane permeability was determined using an NPN uptake assay [65,66]. Briefly, V. cholerae N16961 cells were treated with an appropriate concentration of EGCG at a final volume of 1 mL for 2 h at 37 °C. Then, cell suspensions were washed and resuspended in 0.5% NaCl for 1 mL. The NPN solution in ethanol (100 mM) was added to 200 µL of cells to give a final concentration of 0.75 mM. The background fluorescence was recorded for subtraction using the Cytation 5 Cell Imaging Multi-Mode Reader (BioTek Instruments, Winooski, VT, USA) with an excitation wavelength of 350 nm and an emission wavelength of 420 nm at room temperature. As the outer membrane permeability increased due to the addition of EGCG, NPN incorporated into the membrane resulted in an increase in fluorescence. Triton X-100 (0.1%; v/v) was used as a positive control. The fluorescence intensity was calculated using the equation:
| Relative fluorescence intensity (%) = F1/F0 × 100, |
where F0 is the fluorescence intensity of untreated cells and F1 is the fluorescence intensity of EGCG-treated cells.
4.6.3. Determination of Cell Membrane Potential
Changes in membrane polarity caused by EGCG were measured through the incorporation of Rh123 [67,68,69]. V. cholerae cells were treatment with EGCG at concentrations of 0.25×, 0.5×, 1×, 2×, and 4× MIC at 37 °C for 2 h. The cell suspension was then mixed with a freshly-prepared Rh123 solution (final Rh123 concentration, 5 µg/mL), kept at 37 °C for 10 min, and centrifuged at 1500 rpm for 10 min. Then, cell pellets were diluted in 0.5% NaCl and the fluorescence signal measured at the excitation and emission wavelengths of 480 and 530 nm, respectively. The fluorescence intensity was calculated using the equation mentioned above.
4.7. Scanning Electron Microscopy (SEM) Analysis
V. cholerae N16961 was treated with EGCG at a concentration of 4× MIC at 37 °C for 2 h. The appropriate treatment was harvested by centrifugation at 5000 rpm for 5 min, washed with PBS, dropped onto a filter membrane of 0.2 µm, and air dried. The samples were fixed using 2.5% (v/v) glutaraldehyde in PBS at 4 °C overnight. Thereafter, bacterial cells were washed with 0.1 M PO4 buffer and re-fixed with 1% OsO4 for 1 h. After dehydration with a graded ethanol series (50%, 70%, 90%, and 100%) for 10 min each, the bacterial samples were transferred to absolute ethanol for 20 min. After drying by critical-point drying (CPD), the bacterial sample was then mounted and coated with gold before examination by SEM (JSM 5910 LV, Oxford Instrument, CA, USA) [65].
4.8. Statistical Analysis
Values were presented as the mean ± standard deviation (SD) of three independent experiments. The significance of differences between average values of different experimental treatments and controls was assessed by ANOVA, considering that statistical significance was set at a p value less than 0.05. When ANOVA revealed significant differences among treatments, post hoc tests were carried out with Dunnett’s Multiple Comparison Test from GraphPad Prism 5.01 (GraphPad Software, Inc., Scotts Valley, La Jolla, CA, USA).
5. Conclusions
The findings of the present study highlight the promising role of EGCG as a natural anti-cholera compound against MDR V. cholerae. All of the 45 clinical isolates were responsive to EGCG, with MIC and MBC values ranging from 62.5–250 µg/mL and 125–500 µg/mL, respectively. The combination of EGCG and tetracycline was more effective than either treatment alone, with FICIs of 0.009 and 0.018 in O1 and O139 highly drug-resistant representative strains, respectively. According to time-killing kinetics analysis, EGCG had bactericidal activity for MDR V. cholerae after 1 h of exposure to at least 62.5 µg/mL EGCG, which is associated with membrane disrupting. As an outcome, EGCG could be promoted as a potential alternative therapeutic agent for MDR V. cholerae infections.
Acknowledgments
We are sincerely grateful to Masami Suganuma at the Graduate School of Science and Engineering, Saitama University in Japan and Supaporn Lamlertthon at the School of Medical Science, Naresuan University, Thailand, for their stimulating discussions. We also thank Chatchaya Sumana from the University of Phayao for her technical assistance. We thank Emma Taylor, PhD, from the PRS Group for editing a draft of this manuscript.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics11040518/s1, Figure S1: Chemical structures and classifications of tea polyphenols; Table S1: The susceptibility of a total of 45 V. cholerae clinical strains to EGCG (µg/mL); Table S2: MIC and MBC of tetracycline for a total of 45 clinical strains of drug-resistant V. cholerae strains.
Author Contributions
Conceptualization, A.R., A.S. and A.K.; methodology, A.S., A.K., A.D., A.Y., G.P.-I., S.S., O.S. and A.R.; software, A.R.; validation, A.R., A.S. and A.K.; formal analysis, A.R., A.S. and A.K.; investigation, A.R.; resources, A.R., A.S., A.K., A.Y. and O.S.; data curation, A.R., A.S. and A.K.; writing—original draft preparation, A.R.; writing—review and editing, A.R., A.S., A.K. and O.S.; visualization, A.R., A.S. and A.K.; supervision, A.R.; project administration, A.R., S.S. and A.D.; funding acquisition, A.R., S.S. and A.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the School of Medical Sciences (grant no. 621003), Unit of Excellence in Research and Product Development of Coffee (grant no. UoE64002), and Unit of Excellence on Clinical Outcomes Research and IntegratioN (UNICORN) [grant no. FF65-UoE005], University of Phayao, Thailand.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hu D., Liu B., Feng L., Ding P., Guo X., Wang M., Cao B., Reeves P.R., Wang L. Origins of the current seventh cholera pandemic. Proc. Natl. Acad. Sci. USA. 2016;113:E7730. doi: 10.1073/pnas.1608732113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ali M., Nelson A.R., Lopez A.L., Sack D.A. Updated global burden of cholera in endemic countries. PLoS Negl. Trop. Dis. 2015;9:e0003832. doi: 10.1371/journal.pntd.0003832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO . Cholera Annual Report 2019 Weekly Epidemiological Record. WHO; Genewa, Switzerland: 2020. pp. 441–448. [Google Scholar]
- 4.WHO Cholera Fact Sheet. [(accessed on 4 January 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/cholera.
- 5.Saha D., Karim M.M., Khan W.A., Ahmed S., Salam M.A., Bennish M.L. Single-dose azithromycin for the treatment of cholera in adults. N. Engl. J. Med. 2006;354:2452–2462. doi: 10.1056/NEJMoa054493. [DOI] [PubMed] [Google Scholar]
- 6.Das B., Verma J., Kumar P., Ghosh A., Ramamurthy T. Antibiotic resistance in Vibrio cholerae: Understanding the ecology of resistance genes and mechanisms. Vaccine. 2020;38:A83–A92. doi: 10.1016/j.vaccine.2019.06.031. [DOI] [PubMed] [Google Scholar]
- 7.Verma J., Bag S., Saha B., Kumar P., Ghosh T.S., Dayal M., Senapati T., Mehra S., Dey P., Desigamani A., et al. Genomic plasticity associated with antimicrobial resistance in Vibrio cholerae. Proc. Natl. Acad. Sci. USA. 2019;116:6226–6231. doi: 10.1073/pnas.1900141116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rivard N., Colwell R.R., Burrus V., Castanheira M. Antibiotic Resistance in Vibrio cholerae: Mechanistic Insights from IncC Plasmid-Mediated Dissemination of a Novel Family of Genomic Islands Inserted at trmE. mSphere. 2020;5:e00748-20. doi: 10.1128/mSphere.00748-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shankar U., Jain N., Majee P., Kodgire P., Sharma T.K., Kumar A. Exploring Computational and Biophysical Tools to Study the Presence of G-Quadruplex Structures: A Promising Therapeutic Solution for Drug-Resistant Vibrio cholerae. Front. Genet. 2020;11:935. doi: 10.3389/fgene.2020.00935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De R. Mobile Genetic Elements of Vibrio cholerae and the Evolution of Its Antimicrobial Resistance. Front. Trop. Dis. 2021;2:691604. doi: 10.3389/fitd.2021.691604. [DOI] [Google Scholar]
- 11.Sjölund-Karlsson M., Reimer A., Folster J.P., Walker M., Dahourou G.A., Batra D.G., Martin I., Joyce K., Parsons M.B., Boncy J., et al. Drug-resistance mechanisms in Vibrio cholerae O1 outbreak strain, Haiti, 2010. Emerg. Infect. Dis. 2011;17:2151–2154. doi: 10.3201/eid1711.110720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siriphap A., Leekitcharoenphon P., Kaas R.S., Theethakaew C., Aarestrup F.M., Sutheinkul O., Hendriksen R.S. Characterization and Genetic Variation of Vibrio cholerae Isolated from Clinical and Environmental Sources in Thailand. PLoS ONE. 2017;12:e0169324. doi: 10.1371/journal.pone.0169324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taylor P.W., Hamilton-Miller J.M., Stapleton P.D. Antimicrobial properties of green tea catechins. Food Sci. Technol. Bull. 2005;2:71–81. doi: 10.1616/1476-2137.14184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Daglia M. Polyphenols as antimicrobial agents. Curr. Opin. Biotechnol. 2012;23:174–181. doi: 10.1016/j.copbio.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 15.Chacko S.M., Thambi P.T., Kuttan R., Nishigaki I. Beneficial effects of green tea: A literature review. Chin. Med. 2010;5:13. doi: 10.1186/1749-8546-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reygaert W.C. The antimicrobial possibilities of green tea. Front. Microbiol. 2014;5:434. doi: 10.3389/fmicb.2014.00434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu M., Brown A.C. Applications of Catechins in the Treatment of Bacterial Infections. Pathogens. 2021;10:546. doi: 10.3390/pathogens10050546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fujiki H., Suganuma M., Imai K., Nakachi K. Green tea: Cancer preventive beverage and/or drug. Cancer Lett. 2002;188:9–13. doi: 10.1016/S0304-3835(02)00379-8. [DOI] [PubMed] [Google Scholar]
- 19.Rawangkan A., Wongsirisin P., Namiki K., Iida K., Kobayashi Y., Shimizu Y., Fujiki H., Suganuma M. Green Tea Catechin Is an Alternative Immune Checkpoint Inhibitor that Inhibits PD-L1 Expression and Lung Tumor Growth. Molecules. 2018;23:2071. doi: 10.3390/molecules23082071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reygaert W.C. Green Tea Catechins: Their Use in Treating and Preventing Infectious Diseases. BioMed Res. Int. 2018;2018:9105261. doi: 10.1155/2018/9105261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steinmann J., Buer J., Pietschmann T., Steinmann E. Anti-infective properties of epigallocatechin-3-gallate (EGCG), a component of green tea. Br. J. Pharmacol. 2013;168:1059–1073. doi: 10.1111/bph.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hengge R. Targeting Bacterial Biofilms by the Green Tea Polyphenol EGCG. Molecules. 2019;24:2403. doi: 10.3390/molecules24132403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rawangkan A., Kengkla K., Kanchanasurakit S., Duangjai A., Saokaew S. Anti-Influenza with Green Tea Catechins: A Systematic Review and Meta-Analysis. Molecules. 2021;26:4014. doi: 10.3390/molecules26134014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Renzetti A., Betts J.W., Fukumoto K., Rutherford R.N. Antibacterial green tea catechins from a molecular perspective: Mechanisms of action and structure-activity relationships. Food Funct. 2020;11:9370–9396. doi: 10.1039/D0FO02054K. [DOI] [PubMed] [Google Scholar]
- 25.Toda M., Okubo S., Ikigai H., Shimamura T. Antibacterial and anti-hemolysin activities of tea catechins and their structural relatives. Nihon Saikingaku Zasshi. 1990;45:561–566. doi: 10.3412/jsb.45.561. [DOI] [PubMed] [Google Scholar]
- 26.Aldhaher Z. Evaluation of Antibacterial Activity of Aqueous Extracts of Pomegranate Peels, Green Tea Leaves and Bay Leaves against Vibrio cholera. Iraqi J. Vet. Med. 2018;37:90–95. doi: 10.30539/iraqijvm.v37i1.338. [DOI] [Google Scholar]
- 27.Toda M., Okubo S., Ikigai H., Suzuki T., Suzuki Y., Hara Y., Shimamura T. The protective activity of tea catechins against experimental infection by Vibrio cholerae O1. Microbiol. Immunol. 1992;36:999–1001. doi: 10.1111/j.1348-0421.1992.tb02103.x. [DOI] [PubMed] [Google Scholar]
- 28.Bandyopadhyay D., Dutta P., Dastidar S., Chatterjee T. In vitro and in vivo antidiarrhoeal activity of epigallocatechin 3-gallate: A major catechin isolated from indian green tea. Orient. Pharm. Exp. Med. 2008;8:171–177. doi: 10.3742/OPEM.2008.8.2.171. [DOI] [Google Scholar]
- 29.Sarwar S., Chakraborti S., Bera S., Sheikh I.A., Hoque K.M., Chakrabarti P. The antimicrobial activity of ZnO nanoparticles against Vibrio cholerae: Variation in response depends on biotype. Nanomed. Nanotechnol. Biol. Med. 2016;12:1499–1509. doi: 10.1016/j.nano.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 30.WHO Antimicrobial Resistance. [(accessed on 12 January 2022)]. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance.
- 31.Barh D., Barve N., Gupta K., Chandra S., Jain N., Tiwari S., Leon-Sicairos N., Canizalez-Roman A., dos Santos A.R., Hassan S.S., et al. Exoproteome and secretome derived broad spectrum novel drug and vaccine candidates in Vibrio cholerae targeted by Piper betel derived compounds. PLoS ONE. 2013;8:e52773. doi: 10.1371/journal.pone.0052773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tiwari S., Barh D., Imchen M., Rao E., Kumavath R.K., Seenivasan S.P., Jaiswal A.K., Jamal S.B., Kumar V., Ghosh P., et al. Acetate Kinase (AcK) is Essential for Microbial Growth and Betel-derived Compounds Potentially Target AcK, PhoP and MDR Proteins in M. tuberculosis, V. cholerae and Pathogenic, E. coli: An in silico and in vitro Study. Curr. Top. Med. Chem. 2018;18:2731–2740. doi: 10.2174/1568026619666190121105851. [DOI] [PubMed] [Google Scholar]
- 33.Acosta-Smith E., Leon-Sicairos N., Tiwari S., Flores-Villaseñor H., Canizalez-Roman A., Kumavath R., Ghosh P., Azevedo V., Barh D. Piper betel Compounds Piperidine, Eugenyl Acetate, and Chlorogenic Acid Are Broad-Spectrum Anti-Vibrio Compounds that Are Also Effective on MDR Strains of the Pathogen. Pathogens. 2019;8:64. doi: 10.3390/pathogens8020064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hör M., Rimpler H., Heinrich M. Inhibition of intestinal chloride secretion by proanthocyanidins from Guazuma ulmifolia. Planta Med. 1995;61:208–212. doi: 10.1055/s-2006-958057. [DOI] [PubMed] [Google Scholar]
- 35.Oi H., Matsuura D., Miyake M., Ueno M., Takai I., Yamamoto T., Kubo M., Moss J., Noda M. Identification in traditional herbal medications and confirmation by synthesis of factors that inhibit cholera toxin-induced fluid accumulation. Proc. Natl. Acad. Sci. USA. 2002;99:3042–3046. doi: 10.1073/pnas.052709499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saito T., Miyake M., Toba M., Okamatsu H., Shimizu S., Noda M. Inhibition by apple polyphenols of ADP-ribosyltransferase activity of cholera toxin and toxin-induced fluid accumulation in mice. Microbiol. Immunol. 2002;46:249–255. doi: 10.1111/j.1348-0421.2002.tb02693.x. [DOI] [PubMed] [Google Scholar]
- 37.Morinaga N., Iwamaru Y., Yahiro K., Tagashira M., Moss J., Noda M. Differential activities of plant polyphenols on the binding and internalization of cholera toxin in vero cells. J. Biol. Chem. 2005;280:23303–23309. doi: 10.1074/jbc.M502093200. [DOI] [PubMed] [Google Scholar]
- 38.Rattanachaikunsopon P., Phumkhachorn P. Antimicrobial activity of elephant garlic oil against Vibrio cholerae in vitro and in a food model. Biosci. Biotechnol. Biochem. 2009;73:1623–1627. doi: 10.1271/bbb.90128. [DOI] [PubMed] [Google Scholar]
- 39.Yamasaki S., Asakura M., Neogi S.B., Hinenoya A., Iwaoka E., Aoki S. Inhibition of virulence potential of Vibrio cholerae by natural compounds. Indian J. Med. Res. 2011;133:232–239. [PMC free article] [PubMed] [Google Scholar]
- 40.Chatterjee S., Asakura M., Chowdhury N., Neogi S.B., Sugimoto N., Haldar S., Awasthi S.P., Hinenoya A., Aoki S., Yamasaki S. Capsaicin, a potential inhibitor of cholera toxin production in Vibrio cholerae. FEMS Microbiol. Lett. 2010;306:54–60. doi: 10.1111/j.1574-6968.2010.01931.x. [DOI] [PubMed] [Google Scholar]
- 41.Das S., Chourashi R., Mukherjee P., Kundu S., Koley H., Dutta M., Mukhopadhyay A.K., Okamoto K., Chatterjee N.S. Inhibition of growth and virulence of Vibrio cholerae by carvacrol, an essential oil component of Origanum spp. J. Appl. Microbiol. 2021;131:1147–1161. doi: 10.1111/jam.15022. [DOI] [PubMed] [Google Scholar]
- 42.Pederson D.B., Dong Y., Blue L.B., Smith S.V., Cao M. Water-soluble cranberry extract inhibits Vibrio cholerae biofilm formation possibly through modulating the second messenger 3’,5’—Cyclic diguanylate level. PLoS ONE. 2018;13:e0207056. doi: 10.1371/journal.pone.0207056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sanchez E., García S., Heredia N. Extracts of Edible and Medicinal Plants Damage Membranes of Vibrio cholerae. Appl. Environ. Microbiol. 2010;76:6888–6894. doi: 10.1128/AEM.03052-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yussof A., Habiba U., Liaw D., Chu T., Lee L. Epigallocatechin Gallate-Stearate Enhances the Efficacy of Antibiotics. Open J. Med. Microbiol. 2019;9:77–94. doi: 10.4236/ojmm.2019.93009. [DOI] [Google Scholar]
- 45.Zhao W.-H., Hu Z.-Q., Okubo S., Hara Y., Shimamura T. Mechanism of Synergy between Epigallocatechin Gallate and β-Lactams against Methicillin-Resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2001;45:1737–1742. doi: 10.1128/AAC.45.6.1737-1742.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aboulmagd E., Al-Mohammed H., Al-Badry S. Synergism and postantibiotic effect of green tea extract and imipenem against methicillin-resistant Staphylococcus aureus. Microbiol. J. 2011;1:89–96. doi: 10.3923/mj.2011.89.96. [DOI] [Google Scholar]
- 47.Parvez M.A.K., Saha K., Rahman J., Munmun R.A., Rahman M.A., Dey S.K., Rahman M.S., Islam S., Shariare M.H. Antibacterial activities of green tea crude extracts and synergistic effects of epigallocatechingallate (EGCG) with gentamicin against MDR pathogens. Heliyon. 2019;5:e02126. doi: 10.1016/j.heliyon.2019.e02126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lee S., Razqan G.S., Kwon D.H. Antibacterial activity of epigallocatechin-3-gallate (EGCG) and its synergism with β-lactam antibiotics sensitizing carbapenem-associated multidrug resistant clinical isolates of Acinetobacter baumannii. Phytomedicine. 2017;24:49–55. doi: 10.1016/j.phymed.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 49.Zhang Q., Zhang J.I.N., Zhang J., Xu D.U.O., Li Y., Liu Y., Zhang X.I.N., Zhang R., Wu Z., Weng P. Antimicrobial Effect of Tea Polyphenols against Foodborne Pathogens: A Review. J. Food Prot. 2021;84:1801–1808. doi: 10.4315/JFP-21-043. [DOI] [PubMed] [Google Scholar]
- 50.Kishore R.S., Meena K.S., Ramesh C. Post-Genomic Approaches in Drug and Vaccine Development. River Publishers; Gistrup, Denmark: 2015. 13 Inhibition of virulence potential of Vibrio cholerae by herbal compounds; pp. 347–374. [Google Scholar]
- 51.Namiki K., Wongsirisin P., Yokoyama S., Sato M., Rawangkan A., Sakai R., Iida K., Suganuma M. (−)-Epigallocatechin gallate inhibits stemness and tumourigenicity stimulated by AXL receptor tyrosine kinase in human lung cancer cells. Sci. Rep. 2020;10:2444. doi: 10.1038/s41598-020-59281-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Performance Standards for Antimicrobial Susceptibility Testing. Twenty-Fifth Informational Supplement. Clinical and Laboratory Standards Institute (CLSI); Wayne, PA, USA: 2015. [Google Scholar]
- 53.Qaiyumi S. Antimicrobial Susceptibility Testing Protocols. Taylor & Francis; Boca Raton, FL, USA: 2007. Macro-and microdilution methods of antimicrobial susceptibility testing; pp. 75–79. [Google Scholar]
- 54.Balouiri M., Sadiki M., Ibnsouda S.K. Methods for in vitro evaluating antimicrobial activity: A review. J. Pharm. Anal. 2016;6:71–79. doi: 10.1016/j.jpha.2015.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Elshikh M., Ahmed S., Funston S., Dunlop P., McGaw M., Marchant R., Banat I.M. Resazurin-based 96-well plate microdilution method for the determination of minimum inhibitory concentration of biosurfactants. Biotechnol. Lett. 2016;38:1015–1019. doi: 10.1007/s10529-016-2079-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ahmadi M.H. Global status of tetracycline resistance among clinical isolates of Vibrio cholerae: A systematic review and meta-analysis. Antimicrob. Resist. Infect. Control. 2021;10:115. doi: 10.1186/s13756-021-00985-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Magi G., Marini E., Facinelli B. Antimicrobial activity of essential oils and carvacrol, and synergy of carvacrol and erythromycin, against clinical, erythromycin-resistant Group A Streptococci. Front. Microbiol. 2015;6:165. doi: 10.3389/fmicb.2015.00165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Odds F.C. Synergy, antagonism, and what the chequerboard puts between them. J. Antimicrob. Chemother. 2003;52:1. doi: 10.1093/jac/dkg301. [DOI] [PubMed] [Google Scholar]
- 59.Zimmermann S., Klinger-Strobel M., Bohnert J.A., Wendler S., Rödel J., Pletz M.W., Löffler B., Tuchscherr L. Clinically Approved Drugs Inhibit the Staphylococcus aureus Multidrug NorA Efflux Pump and Reduce Biofilm Formation. Front. Microbiol. 2019;10:2762. doi: 10.3389/fmicb.2019.02762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Foerster S., Unemo M., Hathaway L.J., Low N., Althaus C.L. Time-kill curve analysis and pharmacodynamic modelling for in vitro evaluation of antimicrobials against Neisseria gonorrhoeae. BMC Microbiol. 2016;16:214. doi: 10.1186/s12866-016-0838-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Soudeiha M.A.H., Dahdouh E.A., Azar E., Sarkis D.K., Daoud Z. In vitro Evaluation of the Colistin-Carbapenem Combination in Clinical Isolates of A. baumannii Using the Checkerboard, Etest, and Time-Kill Curve Techniques. Front. Cell. Infect. Microbiol. 2017;7:209. doi: 10.3389/fcimb.2017.00209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sateriale D., Facchiano S., Colicchio R., Pagliuca C., Varricchio E., Paolucci M., Volpe M.G., Salvatore P., Pagliarulo C. In vitro Synergy of Polyphenolic Extracts from Honey, Myrtle and Pomegranate against Oral Pathogens, S. mutans and R. dentocariosa. Front. Microbiol. 2020;11:1465. doi: 10.3389/fmicb.2020.01465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Petersen P.J., Jones C.H., Bradford P.A. In vitro antibacterial activities of tigecycline and comparative agents by time-kill kinetic studies in fresh Mueller-Hinton broth. Diagn. Microbiol. Infect. Dis. 2007;59:347–349. doi: 10.1016/j.diagmicrobio.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 64.Lou Z., Wang H., Zhu S., Ma C., Wang Z. Antibacterial activity and mechanism of action of chlorogenic acid. J. Food Sci. 2011;76:M398–M403. doi: 10.1111/j.1750-3841.2011.02213.x. [DOI] [PubMed] [Google Scholar]
- 65.Lv Y., Wang J., Gao H., Wang Z., Dong N., Ma Q., Shan A. Antimicrobial Properties and Membrane-Active Mechanism of a Potential α-Helical Antimicrobial Derived from Cathelicidin PMAP-36. PLoS ONE. 2014;9:e86364. doi: 10.1371/journal.pone.0086364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wang J., Chou S., Xu L., Zhu X., Dong N., Shan A., Chen Z. High specific selectivity and Membrane-Active Mechanism of the synthetic centrosymmetric α-helical peptides with Gly-Gly pairs. Sci. Rep. 2015;5:15963. doi: 10.1038/srep15963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Darzynkiewicz Z., Staiano-Coico L., Melamed M.R. Increased mitochondrial uptake of rhodamine 123 during lymphocyte stimulation. Proc. Natl. Acad. Sci. USA. 1981;78:2383. doi: 10.1073/pnas.78.4.2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Matsuyama T. Staining of living bacteria with rhodamine 123. FEMS Microbiol. Lett. 1984;21:153–157. doi: 10.1111/j.1574-6968.1984.tb00202.x. [DOI] [Google Scholar]
- 69.Leal A.M., de Queiroz J.D., de Medeiros S.R., Lima T.K., Agnez-Lima L.F. Violacein induces cell death by triggering mitochondrial membrane hyperpolarization in vitro. BMC Microbiol. 2015;15:115. doi: 10.1186/s12866-015-0452-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.