Abstract
Autoimmune glial fibrillary acidic protein (GFAP) astrocytopathy (GFAP-A) is a type of autoimmune corticosteroid-responsive meningoencephalitis that occurs with or without myelitis. Movement disorders have been reported in GFAP-A patients but have not been characterized. In this study, we examined the characteristics of movement disorders in GFAP-A patients. We retrospectively reviewed clinical data from 87 consecutive patients with GFAP-A attending Gifu University Hospital in Japan. We compared the demographics, clinical features, cerebrospinal fluid characteristics, and neuroimaging findings from patients with and without movement disorders. Seventy-four patients (85%) had movement disorders, including ataxia (49%), tremor (45%), myoclonus (37%), dyskinesia (2%), opsoclonus (2%), rigidity (2%), myokymia (1%), and choreoathetosis (1%). GFAP-A patients with movement disorders were significantly older than those without. Movement disorders are therefore common in GFAP-A patients, and the main types of movement disorders observed in this population were ataxia, tremor, and myoclonus. These abnormal movements can serve as clinical features that facilitate the early diagnosis of GFAP-A. Elderly GFAP-A patients are more likely to have movement disorder complications than younger patients.
Keywords: astrocytopathy, ataxia, glial fibrillary acidic protein (GFAP), movement disorder, myoclonus, tremor
1. Introduction
Autoimmune glial fibrillary acidic protein (GFAP) astrocytopathy (GFAP-A) is a type of autoimmune corticosteroid-responsive meningoencephalitis that occurs with or without myelitis [1,2]. The detection of immunoglobulin G (IgG) against GFAP (GFAP-IgG) in cerebrospinal fluid (CSF) is a biomarker of GFAP-A. GFAP-A was first described in 16 patients [1], and since then, it has been documented in several countries, including the USA, China, Italy, the UK, France, and Japan [3,4,5,6,7,8]. Patients generally present with headache and fever, followed by disturbed consciousness and signs of meningeal irritation [2,8]. Blurred vision related to optic disc edema has also been observed [2]. Some GFAP-A patients have a neoplasm such as ovarian teratoma [2,9]. Brain linear perivascular radial gadolinium enhancement (LPRGE) patterns, an imaging hallmark of GFAP-A, are noted in about half of all patients [2,7,8]. A neuropathological study reported inflammatory infiltrates, including T, B, and plasma cells surrounding blood vessels [4]. Although the pathophysiological mechanisms of GFAP-A have not yet been elucidated, GFAP-specific CD8+ T cells are likely effectors of this disorder [4,10,11]. GFAP-A is usually corticosteroid-responsive in the acute stage [2,7,8]. However, some patients are prone to relapse or even death [12]. Early diagnosis and initiation of corticosteroid therapies are important for patient prognoses [13].
Previous reports have addressed the movement disorders associated with GFAP-A [14,15,16]. However, most reports are case reports or studies with small sample populations. Therefore, the characteristics of movement disorders in GFAP-A patients remain to be elucidated. Here, we describe the characteristics of movement disorders in GFAP-A patients and consider clinical features that may facilitate the early diagnosis of this condition.
2. Patients and Methods
2.1. Patients
We enrolled 492 Japanese patients with inflammatory central nervous system diseases to examine CSF GFAP-IgG in this population. Of the participants, 277 had been admitted to Gifu University Hospital between May 2002 and December 2021. The other 215 participants submitted CSF samples for GFAP-IgG evaluation to Gifu University Graduate School of Medicine between January 2019 and December 2021. We retrospectively reviewed the clinical data from all patients with CSF GFAP-IgG. Clinical information was available via the clinical records of Gifu University Hospital and from communication with referring physicians. The referring neurologists were asked to note the presence and type of movement disorder during the clinical course. Written informed consent was obtained from all patients before the investigation commenced. This study was approved by the institutional review board of Gifu University Graduate School of Medicine, Gifu, Japan (Protocol 27-43).
2.2. Measurement of CSF GFAP-IgG
GFAP-IgG was detected in CSF samples via a transfected cell-based assay and a tissue-based immunofluorescence assay, according to a previous report [2,8].
2.3. Statistical Analysis
Data are reported as the median and range, or the number and percentage. Data analysis was performed using statistical software (Excel-Toukei 2012, Social Survey Research Information; Tokyo, Japan). The Shapiro–Wilk test determined that the data were nonparametrically distributed; therefore, differences in statistical significance between patient groups were calculated using the Mann–Whitney U Test for continuous variables and Fisher’s exact test for categorical variables, as appropriate. A p-value ≤ 0.05 was considered statistically significant.
3. Results
3.1. Demographics, Clinical Features, CSF Characteristics, and Neuroimaging in Autoimmune GFAP-A Patients
Both the transfected cell-based assay and the tissue-based immunofluorescence assay revealed GFAP-IgG in CSF samples from 109 of the 492 patients tested. Among these 109 GFAP-A patients, 22 were excluded because sufficient clinical data were not available. Thus, we evaluated clinical information from 87 GFAP-A patients. The demographics, clinical features, CSF characteristics, and neuroimaging findings from the 87 GFAP-A patients are shown in Table 1. The median age of the 87 patients was 51 years (range: 5–83), and 56 (64%) were male. Fourteen patients (16%) had tumors: ovarian teratoma in five patients, breast cancer in three patients, and one patient each for pituitary adenoma, acoustic tumor, thyroid follicular adenoma, hepatic teratoma, colon cancer, and rectum cancer. Two patients had autoimmune diseases: one had atopic dermatitis and the other had rheumatoid arthritis. The median period from onset to admission was 12 days (range: 1–1054).
Table 1.
Demographics, clinical features, cerebrospinal fluid characteristics, and neuroimaging findings from 87 GFAP-A patients.
| Variables | Patients (%) | Median (Range) |
|---|---|---|
| Demographics | ||
| Age (N = 87) | 51 (5–83) | |
| Male | 56/87 (64) | |
| Concomitant tumor | 14/87 (16) | |
| Concomitant autoimmune disease | 2/87 (2) | |
| Period from onset to admission (days) (N = 85) | 12 (1–1054) | |
| Clinical findings | ||
| Movement disorder | 74/87 (85) | |
| Urinary dysfunction | 67/87 (77) | |
| Altered consciousness | 66/87 (76) | |
| Nuchal rigidity and/or Kernig’s sign | 56/87 (64) | |
| Fever | 54/85 (64) | |
| Hyperreflexia | 50/86 (58) | |
| Headache | 43/85 (51) | |
| Cognitive dysfunction | 42/87 (48) | |
| Psychosis | 37/87 (43) | |
| Papillary edema | 17/48 (43) | |
| Weakness | 32/87 (37) | |
| Sensory disturbance | 24/87 (28) | |
| Respiratory failure | 19/86 (22) | |
| Convulsion | 17/87 (20) | |
| Cerebrospinal fluid findings | ||
| Cell counts (cells/μL) (N = 86) | 79 (4–472) | |
| Protein concentrations (mg/dL) (N = 86) | 146 (30–320) | |
| Oligoclonal IgG bands | 43/61 (70) | |
| Coexisting neural autoantibodies | ||
| Anti-MOG antibodies | 2/57 (4) | |
| Anti-GAD antibodies | 2/8 (25) | |
| Anti-NMDAR antibodies | 2/42 (5) | |
| Anti-AQP4 antibodies | 0/66 (0) | |
| Brain MRI findings | ||
| T2/FLAIR hyperintensity lesions | 76/86 (88) | |
| Hyperintensities in white matter | 49/84 (58) | |
| Hyperintensities in basal ganglia | 36/84 (43) | |
| Hyperintensities in cerebellum | 5/84 (6) | |
| Gadolinium enhancement lesions | 53/78 (68) | |
| LPRGE patterns | 42/78 (54) | |
| Spinal cord MRI findings | ||
| Intramedullary T2 hyperintensity lesions | 29/71 (41) | |
| Gadolinium enhancement lesions | 24/51 (47) | |
| Intramedullary enhancement lesions | 12/51 (24) | |
| Meningeal enhancement lesions | 13/51 (25) | |
| Therapies | ||
| Corticosteroid therapies | 85/87 (98) | |
| Period from onset to steroid initiation (day) (N = 83) | 24 (7–1084) | |
AQP4: aquaporin 4, FLAIR: fluid-attenuated inversion recovery, GAD: glutamic acid decarboxylase, GFAP-A: autoimmune glial fibrillar acidic protein astrocytopathy, IgG: immunoglobulin G, LPRGE: linear perivascular radial gadolinium enhancement, MOG: myelin oligodendrocyte glycoprotein, MRI: magnetic resonance imaging. NMDA: N-methyl-D-aspartate.
Seventy-four of the 87 GFAP-A patients (85%) had a movement disorder, and this was the most common clinical finding in this patient group. The other common clinical findings were urinary dysfunction (67/87 (77%)), altered consciousness (66/87 (76%)), nuchal rigidity and/or Kernig’s sign (56/87 (64%)), fever (54/85 (64%)), and hyperreflexia (50/86 (58%)). The least common clinical findings were respiratory failure (19/86 (22%)) and convulsion (17/87 (20%)).
The CSF examination showed mononuclear cell-predominant pleocytosis and elevated protein concentrations in almost all of the patients. The median cell count was 79 cells/μL (range: 4–472), and the median protein concentration was 146 mg/dL (range: 30–320). Forty-three out of 61patients (70%) had oligoclonal IgG bands.
Coexisting neuronal autoantibodies were anti-N-methyl-D-aspartate (NMDAR) (2/42 (5%)), anti-myelin oligodendrocyte glycoprotein (MOG) (2/57 (4%)), and anti-glutamic acid decarboxylase (GAD) antibodies (2/8 (25%)). None of the 66 patients had anti-aquaporin 4 (AQP4) antibodies.
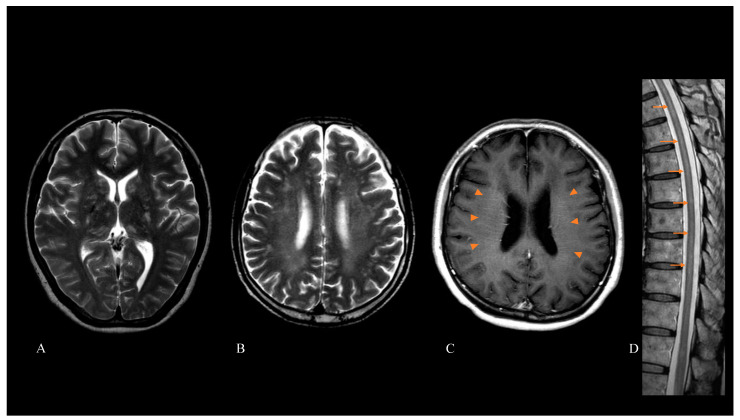
Brain magnetic resonance imaging (MRI) revealed that 76 out of 86 patients (88%) had abnormal hyperintensity lesions on T2-weighted and fluid-attenuated inversion recovery (FLAIR) images. The hyperintensity lesions were in white matter (49/84 (58%)), the basal ganglia (36/84 (43%)), and cerebellum (5/84 (6%)). When we conducted gadolinium-enhanced brain MRI, 53 out of 78 patients (68%) had abnormal enhancement lesions. Forty-two out of 78 patients (54%) had LPRGE patterns in the cerebral white matter. Twenty-nine out of 71 patients (41%) who underwent spinal cord MRI showed intramedullary hyperintensity lesions on T2-weighted images. Twenty-four out of 51 patients (47%) who underwent enhanced spinal cord MRI had abnormal enhancement lesions. These were intramedullary lesions (12/51 (24%)) and meningeal lesions (13/51 (25%)). Images of brain and spinal cord MRI of representative patients are shown in Figure 1.
Figure 1.
Brain and spinal cord magnetic resonance imaging (MRI) of patients with autoimmune glial fibrillary acidic protein (GFAP) astrocytopathy. Abnormal hyperintensity lesions on T2-weighted imaging were observed in the basal ganglia, thalamus (A), and cerebral white matter (B). Gadolinium-enhanced brain MRI showed a linear perivascular radial enhancement pattern (arrowheads) (C). Spinal cord MRI showed longitudinally extensive T2-hyperintensity lesions (arrow) (D).
Eighty-five out of the 87 patients (98%) were treated with corticosteroids. The median period from symptom onset to the initiation of corticosteroids was 24 days (range: 7–1084).
3.2. Types and Frequencies of Movement Disorders in GFAP-A Patients
The types and frequencies of movement disorders in GFAP-A patients are shown in Table 2. The most frequently observed movement disorder was ataxia (truncal and/or limb ataxia), and it was found in 43/87 patients (49%). The second most frequent movement disorder was tremor, observed in 39/87 patients (45%). Tremor was postural and/or an action tremor. The part of the body most affected by tremor was the upper limbs. Tremor in 21/39 patients (54%) was confirmed within 28 days. The third most frequent movement disorder was myoclonus, observed in 32/87 patients (37%). The parts of the body most affected by myoclonus were the upper and lower limbs. Myoclonus in 17/32 patients (53%) was confirmed within 28 days.
Table 2.
Types and frequencies of movement disorders in GFAP-A patients.
| Movement Disorders | Patients (%) |
|---|---|
| Ataxia | 43/87 (49) |
| Tremor | 39/87 (45) |
| Myoclonus | 32/87 (37) |
| Dyskinesia | 2/87 (2) |
| Opsoclonus | 2/87 (2) |
| Rigidity | 2/87 (2) |
| Myokymia | 1/87 (1) |
| Choreoathetosis | 1/87 (1) |
GFAP-A: autoimmune glial fibrillar acidic protein astrocytopathy.
The least common movement disorders were dyskinesia, opsoclonus, rigidity, myokymia, and choreoathetosis (Table 2).
3.3. Characteristics of GFAP-A Patients with Movement Disorders
To examine the characteristics of the GFAP-A patients with movement disorders, we compared the demographics, clinical features, CSF characteristics, and neuroimaging findings from patients with and without movement disorders (Table 3). GFAP-A patients with movement disorders (median age, 54 years; range: 5–83 years) were significantly older than those without (median age, 30 years; range: 17–76 years) (p = 0.005). There were no significant differences in the other demographics between the two patient groups. There were also no significant differences between the two patient groups in terms of clinical findings, CSF characteristics, and neuroimaging findings. We examined the association between age and movement disorders using multivariable logistic regression analysis to control for the potentially confounding effects of gender and concomitant tumor. Older age was associated with movement disorders in GFAP-A (OR 1.052, CI: 1.011–1.094, p = 0.013).
Table 3.
Demographics, clinical features, cerebrospinal fluid characteristics, and neuroimaging findings according to the presence or absence of movement disorders in GFAP-A patients.
| Variables | With MDs | Without MDs | p | ||
|---|---|---|---|---|---|
| Patients (%) | Median (Range) | Patients (%) | Median (Range) | ||
| Demographics | |||||
| Age | 54 (5–83), N = 74 | 30 (17–76), N = 13 | 0.005 | ||
| Male | 50/74 (68) | 6/13 (46) | 0.208 | ||
| Concomitant tumor | 11/74 (15) | 3/12 (25) | 0.400 | ||
| Concomitant autoimmune disease | 2/74 (3) | 0/13 (0) | 1.000 | ||
| Period from onset to admission (days) | 12 (1–1054), N = 74 | 8 (1–39), N = 13 | 0.139 | ||
| Clinical features | |||||
| Urinary disturbance | 59/74 (80) | 8/13 (62) | 0.165 | ||
| Altered consciousness | 55/74 (74) | 11/13 (85) | 0.726 | ||
| Nuchal rigidity and/or Kernig’s sign | 46/74 (62) | 10/13 (77) | 0.364 | ||
| Fever | 44/72 (61) | 10/13 (77) | 0.358 | ||
| Hyperreflexia | 43/73 (59) | 7/13 (54) | 0.768 | ||
| Cognitive disfunction | 37/74 (50) | 5/13 (38) | 0.553 | ||
| Headache | 34/72 (47) | 9/13 (69) | 0.228 | ||
| Psychosis | 31/74 (42) | 6/13 (46) | 0.771 | ||
| Papillary edema | 16/35 (46) | 1/5 (20) | 0.373 | ||
| Weakness | 28/74 (38) | 4/13 (31) | 0.760 | ||
| Sensory disturbance | 22/74 (30) | 2/13 (15) | 0.501 | ||
| Respiratory failure | 14/73 (19) | 5/13 (38) | 0.150 | ||
| Convulsion | 14/74 (19) | 3/10 (30) | 0.712 | ||
| Cerebrospinal fluid | |||||
| Cell counts (cells/μL) | 79 (4–378), N = 73 | 74 (10–472), N = 13 | 0.109 | ||
| Protein concentrations (mg/dL) | 136 (54–320), N = 73 | 156 (30–241), N = 13 | 0.376 | ||
| Oligoclonal IgG bands | 39/56 (70) | 4/5 (80) | 1.000 | ||
| Coexisting neural autoantibodies | |||||
| Anti-MOG antibodies | 2/50 (4) | 0/7 (0) | 1.000 | ||
| Anti-GAD antibodies | 1/7 (14) | 1/1 (100) | 0.250 | ||
| Anti-NMDAR antibodies | 2/38 (5) | 0/4 (0) | 1.000 | ||
| Brain MRI | |||||
| T2/FLAIR hyperintensity lesions | 64/73 (88) | 12/13 (92) | 1.000 | ||
| Hyperintensities in white matter | 43/71 (61) | 6/13 (46) | 0.371 | ||
| Hyperintensities in basal ganglia | 27/71 (38) | 9/13 (70) | 0.065 | ||
| Hyperintensities in cerebellum | 4/71 (6) | 1/13 (8) | 0.578 | ||
| Gadolinium enhancement lesions | 47/67 (70) | 6/11 (55) | 0.316 | ||
| LPRGE | 36/67 (54) | 6/11 (55) | 1.000 | ||
| Spinal cord MRI | |||||
| Intramedullary T2 hyperintensity lesions | 25/60 (42) | 4/11 (36) | 1.000 | ||
| Gadolinium enhancement lesions | 21/44 (48) | 3/7 (45) | 1.000 | ||
| Intramedullary enhancement lesions | 11/44 (25) | 1/7 (14) | 1.000 | ||
| Meningeal enhancement lesions | 11/44 (25) | 2/7 (29) | 1.000 | ||
| Therapies | |||||
| Corticosteroid therapies | 72/74 (97) | 13/13 (100) | 1.000 | ||
| Period from onset to steroid initiation (days) | 25 (7–1084), N = 70 | 14 (8–60), N = 13 | 0.136 | ||
FLAIR: fluid-attenuated inversion recovery, GAD: glutamic acid decarboxylase, GFAP-A: autoimmune glial fibrillar acidic protein astrocytopathy, IgG: immunoglobulin G, LPRGE: linear perivascular radial gadolinium enhancement, MDs: movement disorders, MOG: myelin oligodendrocyte glycoprotein, MRI: magnetic resonance imaging. NMDA: N-methyl-D-aspartate.
3.4. Literature Review of Movement Disorders in GFAP-A Patients
In the previous literature, we found that 37 of 79 papers (47%) described movement disorders in GFAP-A patients (Table 4) [1,2,3,4,5,6,8,9,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41]. In these reports, the most frequently described movement disorders were ataxia (23/79 (29%)), followed by tremor (22/79 (28%)), myoclonus (12/79 (15%)), and dyskinesia (6/79 (8%)). The least common movement disorders were hyperekplexia (3/79 (4%)), dystonia (2/79 (3%)), parkinsonism (2/79 (3%)), chorea (1/79 (1%)), axial stiffness (1/79 (1%)), grimacing (1/79 (1%)), oral movements (1/79 (1%)), catatonia (1/79 (1%)), and oculogyric crises (1/79 (1%)).
Table 4.
Previous data on the presence of movement disorders in autoimmune GFAP astrocytopathy patients.
| Movement Disorders | Number of Reports | References |
|---|---|---|
| Ataxia | 23 | [1,2,3,4,5,8,9,13,15,16,17,19,22,23,24,25,26,27,32,36,38,40,41] |
| Tremor | 22 | [1,2,6,8,13,14,20,21,24,26,27,28,29,30,31,33,34,35,36,37,38,39] |
| Myoclonus | 12 | [6,8,13,14,15,16,25,32,33,35,36,37] |
| Dyskinesia | 6 | [4,5,6,17,23,41] |
| Hyperekplexia | 3 | [6,32,35] |
| Dystonia | 2 | [6,23] |
| Parkinsonism | 2 | [6,14] |
| Chorea | 1 | [13] |
| Axial stiffness | 1 | [35] |
| Grimacing | 1 | [18] |
| Oral movements | 1 | [18] |
| Catatonia | 1 | [18] |
| Oculogyric crises | 1 | [35] |
GFAP: glial fibrillary acidic protein.
4. Discussion
In this study, we clarified the characteristics of movement disorders in individuals with autoimmune GFAP-A. The novel findings of this study are as follows. (1) Movement disorders are common neurological findings in GFAP-A patients. (2) The major types of movement disorders in this population were ataxia, tremor, and myoclonus. (3) GFAP-A patients with movement disorders were significantly older than those without.
The present study demonstrated that movement disorders are common in GFAP-A patients. In the previous literature, the most frequently described movement disorders were ataxia, followed by tremor and myoclonus. These three movement disorders were also common in our study population. Among patients with tremor and myoclonus, these symptoms were confirmed in about half of the patients within 28 days. These abnormal movements may thus be neurological findings characteristic of GFAP-A and can act as clinical features that would facilitate early diagnosis.
The pathophysiology of movement disorders in GFAP-A patients is unclear. GFAP is expressed exclusively in astrocytes, including Bergmann glia in the cerebellum. Extensive inflammatory lesions can occur in the central nervous system of GFAP-A patients [1,2,8]. The observed movement disorders might have been complicated by various central nervous system lesions. Although abnormal intensities in the cerebellum on brain MRI are rare, ataxia in the GFAP-A patients might have been caused by cerebellar dysfunction [2,8]. Ataxia was usually mild and was observed in the early phase. Most patients had both limb and truncal ataxia. Although it improved after immunotherapy, truncal ataxia persisted in some patients. Tremor was predominantly postural and/or an action tremor in the upper limbs. A surface electromyogram from one patient showed an 11–12 Hz tremor, indicating an essential tremor. Structural changes in cerebellar Purkinje cells and neighboring neuronal populations have been observed in post-mortem studies of essential tremor, and GABAergic dysfunction and dysregulation of the cerebellar-thalamic-cortical circuitry have been documented [42,43,44]. Tremor may also be associated with impairment of the cerebellar pathways. Myoclonus in this population was usually non-segmental multifocal myoclonus in the upper and lower limbs. A previous report described a GFAP-A patient with multifocal myoclonus in whom hypermetabolism of the spinal cord was associated with areas of cortical hyper- and hypometabolism in 18F-fluorodeoxyglucose positron emission tomography imaging [25].
Dyskinesia, observed in this study, has previously been reported [4,5,6,17,23,41]. One of two patients with dyskinesia had an N-methyl-D-aspartate receptor (NMDAR)-IgG and ovarian teratoma. GFAP-IgG was sometimes accompanied by anti-neuronal antibodies, including NMDAR-IgG [2,3,13]. Dyskinesia is a common manifestation of NMDAR encephalitis [45,46]. If a GFAP-A patient is a young woman presenting with dyskinesia, examinations for NMDAR-IgG and ovarian teratoma should be performed because their presence is important for determining the treatment strategy.
In this study, two patients with no medical history of Parkinson’s disease or Parkinson-related disorders presented with rigidity in their upper limbs. The rigidity of one of these two patients was bilateral cogwheel rigidity dominant in the right upper limb. This patient also presented with bilateral hand postural tremor. The rigidity in these two patients improved after corticosteroid therapy. Brain MRI showed abnormal hyperintensity lesions, including in the cerebral white matter in both patients, and in the basal ganglia and the brainstem in one patient. Two reports have described parkinsonism in GFAP-A [6,14]. Tomczak et al. reported a case of GFAP-A with reversible parkinsonism, including rigidity, right hand action tremor, and bradykinesia [14]. This patient’s brain MRI showed nonspecific white matter changes and attenuated nigrosomes on susceptibility-weighted images. Although the pathophysiology of parkinsonism is unknown, GFAP-A patients may present with reversible parkinsonism.
We compared the demographics, clinical features, CSF characteristics, and neuroimaging findings from patients with and without movement disorders. The age of the GFAP-A patients with movement disorders was significantly higher than that of the GFAP-A patients without movement disorders. This result is important because movement disorders are common neurological features in elderly patients with neurodegenerative or cognitive disorders. GFAP-A should be differentiated in elderly patients with sudden-onset movement disorders.
The main limitations of this study are as follows: (i) the number of GFAP-A patients was small, (ii) the clinical information was based solely on the recall of the referring neurologist, (iii) the movement disorders were not evaluated by movement disorder experts, and (iv) the possibility of movement disorders becoming apparent during the clinical course cannot be ruled out in GFAP-A patients without movement disorders. To further examine the presence of movement disorders in GFAP-A patients, it will be necessary for movement disorder experts to prospectively observe clinical symptoms in a large group of GFAP-A patients.
5. Conclusions
Movement disorders are a common neurological feature of GFAP-A. Ataxia, tremor, and myoclonus are the major movement disorders found in GFAP-A patients, and these may be clinical features that can facilitate early diagnosis. GFAP-A should be differentiated in elderly patients who present with sudden-onset movement disorders.
Acknowledgments
We gratefully acknowledge Eri Sakai and Saori Yamauchi (Department of Neurology, Gifu University Graduate School of Medicine) for their technical assistance.
Author Contributions
Conceptualization, A.K.; methodology, A.K.; formal analysis, A.K.; investigation, A.K. and A.T.; data curation, A.K. and A.T.; writing—original draft preparation, A.K.; writing—review and editing, A.T. and T.S.; supervision, T.S.; project administration, A.K.; funding acquisition, A.K. and T.S. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by JSPS KAKENHI (JP21K07457).
Institutional Review Board Statement
We examined CSF GFAP-IgG under a study approved by the Institutional Review Board of Gifu University Graduate School of Medicine, Gifu, Japan (27-43).
Informed Consent Statement
Written informed consent was obtained from all patients for the use of CSF samples.
Data Availability Statement
All data reported within the article are anonymized and available upon request from the qualified investigators.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fang B., McKeon A., Hinson S.R., Kryzer T.J., Pittock S.J., Aksamit A.J., Lennon V.A. Autoimmune glial fibrillary acidic protein astrocytopathy: A novel meningoencephalomyelitis. JAMA Neurol. 2016;73:1297–1307. doi: 10.1001/jamaneurol.2016.2549. [DOI] [PubMed] [Google Scholar]
- 2.Flanagan E.P., Hinson S.R., Lennon V.A., Fang B., Aksamit A.J., Morris P.P., Basal E., Honorat J.A., Alfugham N.B., Linnoila J.J., et al. Glial fibrillary acidic protein immunoglobulin G as biomarker of autoimmune astrocytopathy: Analysis of 102 patients. Ann. Neurol. 2017;81:298–309. doi: 10.1002/ana.24881. [DOI] [PubMed] [Google Scholar]
- 3.Dubey D., Hinson S.R., Jolliffe E.A., Zekeridou A., Flanagan E.P., Pittock S.J., Basal E., Drubach D.A., Lachance D.H., Lennon V.A., et al. Autoimmune GFAP astrocytopathy: Prospective evaluation of 90 patients in 1 year. J. Neuroimmunol. 2018;321:157–163. doi: 10.1016/j.jneuroim.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 4.Long Y., Liang J., Xu H., Huang Q., Yang J., Gao C., Qiu W., Lin S., Chen X. Autoimmune glial fibrillary acidic protein astrocytopathy in Chinese patients: A retrospective study. Eur. J. Neurol. 2018;25:477–483. doi: 10.1111/ene.13531. [DOI] [PubMed] [Google Scholar]
- 5.Iorio R., Damato V., Evoli A., Gessi M., Gaudino S., Di Lazzaro V., Spagni G., Sluijs J.A., Hol E.M. Clinical and immunological characteristics of the spectrum of GFAP autoimmunity: A case series of 22 patients. J. Neurol. Neurosurg. Psychiatry. 2018;89:138–146. doi: 10.1136/jnnp-2017-316583. [DOI] [PubMed] [Google Scholar]
- 6.Dumonceau A.G., Ameli R., Rogemond V., Ruiz A., Joubert B., Muñiz-Castrillo S., Vogrig A., Picard G., Ambati A., Benaiteau M., et al. Glial fibrillary acidic protein autoimmunity: A French cohort study. Neurology. 2022;98:e653–e668. doi: 10.1212/WNL.0000000000013087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zarkali A., Cousins O., Athauda D., Moses S., Moran N., Harikrishnan S. Glial fibrillary acidic protein antibody-positive meningoencephalomyelitis. Pract. Neurol. 2018;18:315–319. doi: 10.1136/practneurol-2017-001863. [DOI] [PubMed] [Google Scholar]
- 8.Kimura A., Takekoshi A., Yoshikura N., Hayashi Y., Shimohata T. Clinical characteristics of autoimmune GFAP astrocytopathy. J. Neuroimmunol. 2019;332:91–98. doi: 10.1016/j.jneuroim.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 9.Martin A.L., Jolliffe E., Hertweck S.P. Ovarian teratoma associated with coexisting anti-N-methyl-D-aspartate receptor and glial fibrillary acidic protein autoimmune meningoencephalitis in an adolescent girl: A case report. J. Pediatr. Adolesc. Gynecol. 2018;31:321–324. doi: 10.1016/j.jpag.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 10.Shu Y., Long Y., Chang Y., Li R., Sun X., Wang Y., Huang Y., Li J., Chen J., Yang Y., et al. Brain immunohistopathology in a patient with autoimmune glial fibrillary acidic protein astrocytopathy. Neuroimmunomodulation. 2018;25:1–6. doi: 10.1159/000488879. [DOI] [PubMed] [Google Scholar]
- 11.Yuan Z., Li H., Huang L., Fu C., Chen Y., Zhi C., Qiu W., Long Y. CD8+ T-cell predominance in autoimmune glial fibrillary acidic protein astrocytopathy. Eur. J. Neurol. 2021;28:2121–2125. doi: 10.1111/ene.14778. [DOI] [PubMed] [Google Scholar]
- 12.Yang X., Liang J., Huang Q., Xu H., Gao C., Long Y., Xiao X. Treatment of autoimmune glial fibrillary acidic protein astrocytopathy: Follow-up in 7 cases. Neuroimmunomodulation. 2017;24:113–119. doi: 10.1159/000479948. [DOI] [PubMed] [Google Scholar]
- 13.Kunchok A., Zekeridou A., McKeon A. Autoimmune glial fibrillary acidic protein astrocytopathy. Curr. Opin. Neurol. 2019;32:452–458. doi: 10.1097/WCO.0000000000000676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tomczak A., Su E., Tugizova M., Carlson A.M., Kipp L.B., Feng H., Han M.H. A case of GFAP-astroglial autoimmunity presenting with reversible Parkinsonism. Mult. Scler. Relat. Disord. 2019;39:101900. doi: 10.1016/j.msard.2019.101900. [DOI] [PubMed] [Google Scholar]
- 15.Novo A.C., Venegas Pérez B. Autoimmune glial fibrillary acidic protein astrocytopathy presented as ataxia, myoclonus and bulbar syndrome: A case report and review of the literature. BMJ Neurol. Open. 2021;3:e000142. doi: 10.1136/bmjno-2021-000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asan L., Klebe S., Kleinschnitz C., Stettner M., Köhrmann M. Anti-GFAP-antibody positive postinfectious acute cerebellar ataxia and myoclonus after COVID-19: A case report. Ther. Adv. Neurol. Disord. 2021;14:17562864211062824. doi: 10.1177/17562864211062824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang X., Xu H., Ding M., Huang Q., Chen B., Yang H., Liu T., Long Y., Gao C. Overlapping autoimmune syndromes in patients with glial fibrillary acidic protein antibodies. Front. Neurol. 2018;9:251. doi: 10.3389/fneur.2018.00251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Theroux L.M., Goodkin H.P., Heinan K.C., Quigg M., Brenton J.N. Extreme delta brush and distinctive imaging in a pediatric patient with autoimmune GFAP astrocytopathy. Mult. Scler. Relat. Disord. 2018;26:121–123. doi: 10.1016/j.msard.2018.09.015. [DOI] [PubMed] [Google Scholar]
- 19.Luessi F., Engel S., Spreer A., Bittner S., Zipp F. GFAPα IgG-associated encephalitis upon daclizumab treatment of MS. Neurol. Neuroimmunol. Neuroinflamm. 2018;5:e481. doi: 10.1212/NXI.0000000000000481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sechi E., Morris P.P., McKeon A., Pittock S.J., Hinson S.R., Weinshenker B.G., Aksamit A.J., Krecke K.N., Kaufmann T.J., Jolliffe E.A., et al. Glial fibrillary acidic protein IgG related myelitis: Characterisation and comparison with aquaporin-4-IgG myelitis. J. Neurol. Neurosurg. Psychiatry. 2019;90:488–490. doi: 10.1136/jnnp-2018-318004. [DOI] [PubMed] [Google Scholar]
- 21.Tokimura R., Matsuda N., Kobayashi S., Kimura A., Kanai K. Abnormal evoked potentials in autoimmune glial fibrillary acidic protein astrocytopathy. eNeurologicalSci. 2020;18:100229. doi: 10.1016/j.ensci.2020.100229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lin H., Huang Y., Zeng H., Wang M., Guan S., Chen G., Guan H. Overlapping clinical syndromes in patients with glial fibrillary acidic protein IgG. Neuroimmunomodulation. 2020;27:69–74. doi: 10.1159/000505730. [DOI] [PubMed] [Google Scholar]
- 23.Oger V., Bost C., Salah L., Yazbeck E., Maurey H., Bellesme C., Sevin C., Adamsbaum C., Chrétien P., Benaiteau M., et al. Mild encephalitis/encephalopathy with reversible splenial lesion syndrome: An unusual presentation of anti-GFAP astrocytopathy. Eur. J. Paediatr. Neurol. 2020;26:89–91. doi: 10.1016/j.ejpn.2020.03.002. [DOI] [PubMed] [Google Scholar]
- 24.Natori T., Shindo K., Okumura A., Kimura A., Takiyama Y. A treatable case of autoimmune GFAP astrocytopathy presenting chronic progressive impairment. Neurol. Sci. 2020;41:2999–3002. doi: 10.1007/s10072-020-04454-x. [DOI] [PubMed] [Google Scholar]
- 25.Rosales J.J., Toledano C., Riverol M., Arbizu J. [18F]-FDG PET imaging in autoimmune GFAP meningoencephalomyelitis. Eur. J. Nucl. Med. Mol. Imaging. 2021;48:947–948. doi: 10.1007/s00259-020-05001-8. [DOI] [PubMed] [Google Scholar]
- 26.Xu L., Xian W., Li J., Yao X., Long Y. Purkinje cell (PC) antibody positivity in a patient with autoimmune glial fibrillary acidic protein (GFAP) astrocytopathy. Int. J. Neurosci. 2020:1–9. doi: 10.1080/00207454.2020.1860965. [DOI] [PubMed] [Google Scholar]
- 27.Osakada Y., Omote Y., Ikegami K., Tadokoro K., Sato K., Hishikawa N., Takemoto M., Ohta Y., Yamashita T., Kimura A., et al. A case of autoimmune GFAP astrocytopathy with profound weight loss and increased uptake in the spinal cord on 18F-FDG PET. Neurol. Clin. Neurosci. 2021;9:95–97. doi: 10.1111/ncn3.12441. [DOI] [Google Scholar]
- 28.Wang H., Chin J.H., Fang B.Y., Chen X., Zhao A.L., Ren H.T., Guan H.Z. Autoimmune glial fibrillary acidic protein astrocytopathy manifesting as subacute meningoencephalitis with descending myelitis: A case report. BMC Neurol. 2020;20:443. doi: 10.1186/s12883-020-02021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang H., Bai K., Fu Y., Lu S., Ran Y., Dang H., Li J. Glial fibrillary acidic protein astrocytopathy in pediatric patients: A retrospective study. Front. Pediatr. 2021;8:626564. doi: 10.3389/fped.2020.626564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nakamura S., Fujioka T., Kawashima S., Kawaguchi T., Mizuno M., Omura M., Okita K., Kimura A., Shimohata T., Matsukawa N. Self-remitting elevation of adenosine deaminase levels in the cerebrospinal fluid with autoimmune glial fibrillary acidic protein astrocytopathy: A case report and review of the literature. Intern. Med. 2021;60:3031–3036. doi: 10.2169/internalmedicine.6457-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heide E.S., Chaudhari A., Pirverdian A., Lai S., Courtney A. Failure of IVIG in steroid-responsive autoimmune glial fibrillary acidic protein astrocytopathy: A case report. Mult. Scler. Relat. Disord. 2021;51:102933. doi: 10.1016/j.msard.2021.102933. [DOI] [PubMed] [Google Scholar]
- 32.Toledano-Illán C., Esparragosa Vázquez I., Zelaya Huerta M.V., Rosales Castillo J.J., Paternain Nuin A., Arbizu Lostao J., García de Eulate M.R., Riverol Fernández M. Autoimmune glial fibrillary acidic protein astrocytopathy: Case report of a treatable cause of rapidly progressive dementia. J. Neurol. 2021;268:2256–2258. doi: 10.1007/s00415-021-10484-y. [DOI] [PubMed] [Google Scholar]
- 33.Adachi H., Shiomi Y., Kimura A., Shimohata T., Yoneda Y., Kageyama Y. A case of autoimmune glial fibrillary acidic protein (GFAP) astrocytopathy. Rinsho. Shinkeigaku. 2021;61:401–404. doi: 10.5692/clinicalneurol.cn-001575. [DOI] [PubMed] [Google Scholar]
- 34.Tewkesbury G., Song J.W., Perrone C.M. Magnetic resonance imaging of autoimmune GFAP astrocytopathy. Ann. Neurol. 2021;90:691–692. doi: 10.1002/ana.26195. [DOI] [PubMed] [Google Scholar]
- 35.Equiza J., Rodríguez-Antigüedad J., Campo-Caballero D., Iruzubieta P., Prada Á., Roncancio A., Fernández E., Ganzarain Oyarbide M., Arruti M., Urtasun M.A., et al. Autoimmune GFAP astrocytopathy presenting with remarkable CNS hyperexcitability and oculogyric crises. J. Neuroimmunol. 2021;359:577695. doi: 10.1016/j.jneuroim.2021.577695. [DOI] [PubMed] [Google Scholar]
- 36.Xiao J., Chen X., Shang K., Tang Y., Chen M., Deng G., Qin C., Tian D.S. Clinical, neuroradiological, diagnostic and prognostic profile of autoimmune glial fibrillary acidic protein astrocytopathy: A pooled analysis of 324 cases from published data and a single-center retrospective study. J. Neuroimmunol. 2021;360:577718. doi: 10.1016/j.jneuroim.2021.577718. [DOI] [PubMed] [Google Scholar]
- 37.Yamakawa M., Hogan K.O., Leever J., Jassam Y.N. Autopsy Case of Meningoencephalomyelitis Associated With Glial Fibrillary Acidic Protein Antibody. Neurol. Neuroimmunol. Neuroinflamm. 2021;8:e1081. doi: 10.1212/NXI.0000000000001081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kimura A., Kato S., Takekoshi A., Yoshikura N., Yanagida N., Kitaguchi H., Akiyama D., Shimizu H., Kakita A., Shimohata T. Autoimmune glial fibrillary acidic protein astrocytopathy resembling isolated central nervous system lymphomatoid granulomatosis. J. Neuroimmunol. 2021;361:577748. doi: 10.1016/j.jneuroim.2021.577748. [DOI] [PubMed] [Google Scholar]
- 39.Mirian A., Sharma M., Budhram A. Linear radial brainstem enhancement in autoimmune glial fibrillary acidic protein astrocytopathy. JAMA Neurol. 2021;79:82–83. doi: 10.1001/jamaneurol.2021.4054. [DOI] [PubMed] [Google Scholar]
- 40.Héraud C., Capet N., Levraut M., Hattenberger R., Bourg V., Thomas P., Mondot L., Lebrun-Frenay C. Glial fibrillary acidic protein (GFAP) astrocytopathy presenting as mild encephalopathy with reversible splenium lesion. Neurol. Ther. 2021 doi: 10.1007/s40120-021-00302-y. Online ahead of print . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fang H., Hu W., Jiang Z., Yang H., Liao H., Yang L., Wu L. Autoimmune glial fibrillary acidic protein astrocytopathy in children: A retrospective analysis of 35 cases. Front. Immunol. 2021;12:761354. doi: 10.3389/fimmu.2021.761354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Louis E.D., Faust P.L., Vonsattel J.P., Honig L.S., Rajput A., Robinson C.A., Rajput A., Pahwa R., Lyons K.E., Ross G.W., et al. Neuropathological changes in essential tremor: 33 cases compared with 21 controls. Brain. 2007;130:3297–3307. doi: 10.1093/brain/awm266. [DOI] [PubMed] [Google Scholar]
- 43.Louis E.D. Essential tremor: Evolving clinicopathological concepts in an era of intensive post-mortem enquiry. Lancet Neurol. 2010;9:613–622. doi: 10.1016/S1474-4422(10)70090-9. [DOI] [PubMed] [Google Scholar]
- 44.Welton T., Cardoso F., Carr J.A., Chan L.L., Deuschl G., Jankovic J., Tan E.K. Essential tremor. Nat. Rev. Dis. Primers. 2021;7:83. doi: 10.1038/s41572-021-00314-w. [DOI] [PubMed] [Google Scholar]
- 45.Panzer J., Dalmau J. Movement disorders in paraneoplastic and autoimmune disease. Curr. Opin. Neurol. 2011;24:346–353. doi: 10.1097/WCO.0b013e328347b307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dalmau J., Armangué T., Planagumà J., Radosevic M., Mannara F., Leypoldt F., Geis C., Lancaster E., Titulaer M.J., Rosenfeld M.R., et al. An update on anti-NMDA receptor encephalitis for neurologists and psychiatrists: Mechanisms and models. Lancet Neurol. 2019;18:1045–1057. doi: 10.1016/S1474-4422(19)30244-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data reported within the article are anonymized and available upon request from the qualified investigators.