Abstract
Background
Traditional Chinese medicine (TCM) and Western medicine are available and have a long history in Hong Kong. Little is known on the intention to use TCM in Hong Kong. In this study, the intention to use TCM was examined by the extended theory of planned behavior.
Methods
An online cross-sectional survey was conducted from 15 and 29 November 2021. Respondents’ attitude towards using TCM, intention to use TCM, knowledge, perceived behavioral control, perceived service quality, satisfaction, subjective norms and demographic characteristics were collected from the survey. To examine the conceptual framework in this study, partial least square structural equation model (PLS-SEM) was adopted.
Results
In total, 446 responses (completion rate = 74.3%) were analysed. Attitude towards TCM was the strongest predictor to the intention to use TCM followed by satisfaction and subjective norms. Attitude had a partial mediating effect on the relationship between subjective norms, perceived behavioral control and intention to use TCM. Attitude had a full mediating effect on the relationship between knowledge and intention to use TCM. Satisfaction had a full mediating effect on the relationship between perceived service quality and intention to use TCM.
Conclusions
This is the first study to investigate the predictors of the intention to use TCM in Hong Kong by using TPB. Individuals’ attitude towards TCM has showed stronger effect to the intention to use TCM than other predictors, such as satisfaction, perceived behavioral control and subjective norms. To enhance the intention to use TCM in Hong Kong, key stakeholders, including TCM professional organisations, health professionals and policymakers, should develop a positive attitude towards TCM among Hong Kong population.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12906-022-03598-x.
Keywords: Traditional Chinese medicine, Theory of planned behavior, Attitude
Introduction
Traditional Chinese medicine (TCM) has a long history in China and it has a great potential for health improvement, prevention and treatment. Western medicine is the mainstream medical practice in Hong Kong. Hong Kong was a British colony from 1841 to 1997, before the handover of sovereignty back to China. At the beginning of colonial years, TCM remained popular because of distrusting Western medicine by people [1]. However, the advancement of Western medicine, increased price of TCM and time consuming for the preparation of herbs had caused the decline in popularity of TCM after the Second World War. With proper regulation and registration of TCM, the development of TCM is advancing in the last decades. Both TCM and Western medicine are available and popular medical practice in Hong Kong.
The importance of TCM in primary care has been recognised, with 50–60% of the Hong Kong population consulted TCM practitioner at least once in their lives [2]. There are some evidences showing that TCM can be an effective alternative to Western medicine. TCM, consists of herbal medicine, acupuncture, moxibustion and massage, which have the positive effects on pain management, palliative care and management of rheumatoid arthritis [3–6]. Besides, the use of TCM can alleviate the side effects and optimise the clinical effectiveness of radiotherapy and chemotherapy [7]. For example, radiotherapy and chemotherapy for cancer treatments are commonly causing different side effects like fatigue, vomiting, nausea, hair loss, skin ulcers, etc. [7]. TCM can help relieving the side effects caused by radiation and optimize the clinical effectiveness of radiotherapy and chemotherapy, specifically to guide the tonifying qi and producing blood, to reinforce the spleen and stomach and to eliminate heat produced by blood and toxic substance inside the body [7]. TCM and integrated medicine may improve the quality of care and life of the patients. In Hong Kong, elderly and female are more likely to utilise Chinese medicine primary care and patients using TCM have the aim to manage their chronic diseases [2]. Therefore, the preference of TCM is mainly the management of chronic conditions.
Previous studies have investigated the effectiveness of using TCM on disease management, disease prevention and health maintenance [3–6, 8]. However, to the best knowledge of the researchers, no comprehensive studies have investigated the predictors of the intention to use TCM in Hong Kong. This study aimed to use the extended theory of planned behavior to identify the predictors of the intention to use TCM. The findings of this study could provide new insights for policymakers, practitioners and researchers in promoting TCM to the public. Therefore, the research question for this study was: What factors are predicting the intention to use TCM in Hong Kong?
Literature review
Theory of planned behavior
The Theory of Planned Behavior (TPB) is a well-known model in explaining health-related behavior. TPB has been used in many research, including the evaluation of smoking behavior interventions [9], adoption of social distancing [10], COVID-19 vaccination intention [11] and mobile health service adoption [12], and so TPB is a well-established and validated model. In TPB, behavioral intention, which is affected by subjective norms (perceived expectations from important people on performing the behavior), attitude (personal feelings and beliefs about the behavior) and perceived behavioral control (perceived ability of performing the behavior), is the predictor of actual behavior [13–15].
Subjective norms relates to the likelihood that the important people will agree or disagree of certain behavior and personal motivation to meet their expectations [16]. In some studies, subjective norms has a positive effect to the attitude towards using TCM. Source of TCM information are mostly from family, friends and Chinese medicine practitioner [17]. More than 40% of the medical students in Hong Kong would like to use TCM because of the recommendation from family and friends [18]. Subjective norms significantly predicted attitude towards the use of TCM in China [19]. Additionally, recommendations and referrals from those who are trustworthy could motivate the adults to use acupuncture in Hong Kong [20]. Therefore, the following hypotheses are developed:
H1: Subjective norms is positively related to the attitude towards using TCM.
H2: Subjective norms is positively related to the intention to use TCM.
Perceived behavioral control is about the perceived ability to perform the behavior. The easier to perform the behavior leads to the increase in attitude and intention to perform the behavior. Attitude towards the use of TCM was found to be affected by perceived behavioral control [21]. Some studies have found that perceived behavioral control is one of the predictors of acquiring knowledge intention towards and the use of complementary and alternative medicine [22, 23]. Likewise, perceived behavioral control was found to significantly predict the intention to use TCM in China [24]. Therefore, this study proposes hypothesis 3 and 4 as below:
H3: Perceived behavioral control is positively related to the attitude towards using TCM.
H4: Perceived behavioral control is positively related to the intention to use TCM.
Positive attitude towards behaviors is correlated to the intention to the behaviors. The relationship between the attitude towards behaviors and intention to the behavior was found in many studies using TPB, including wearing PM2.5 mask [25], consumer purchasing behavior for organic food [26], and self-management of stroke [27]. Individual’s attitude towards herbal medicines consumption was correlated with intention of herbal medicine use among pregnant women [28]. Besides, attitude was found to significantly predict the intention to use TCM for health maintenance [24]. Positive attitude about traditional, complementary and alternative medicine had a positive relationship with the willingness to pay for the medicine [29]. The following hypotheses are thus proposed:
H5: Attitude towards using TCM is positively related to the intention to use TCM.
H6. Attitude towards using TCM mediates the relationship between subjective norms and the intention to use TCM.
H7. Attitude towards using TCM mediates the relationship between perceived behavioral control and the intention to use TCM.
Knowledge, attitude and behavioral intention
Individual’s knowledge about the behavior can be one of the predicting factors of attitude towards behavior and behavioral intention. Knowledge is important to provide meaningful and useful information for individuals. Knowledge can be viewed as a distal antecedent of behavior conveyed by attitude [30]. Knowledge is important to the attitudes towards health behaviour under the knowledge-attitude-behaviour model [31]. Patients’ attitude towards using acupuncture had a positive impact on the attitude towards acupuncture, affected by their knowledge [32]. Individual with sufficient knowledge can understand the safety and risk of performing behavior so the level of knowledge may affect the behavioral intention. Abamecha et al. had found that knowledge about cervical cancer was positively associated with intention to use cervical cancer screening [33]. Therefore, the following hypotheses are developed:
H8: The knowledge of TCM is positively related to the attitude towards using TCM.
H9: The knowledge of TCM is positively related to the intention to use TCM.
H10. Attitude towards using TCM mediates the relationship between the knowledge of TCM and the intention to use TCM.
Perceived service quality, satisfaction and behavioral intention
In some studies, customer satisfaction theory was used to predict the relationship of perceived service quality, satisfaction and behavioral intention [34, 35]. Perceived service quality refers to the comparison of prior expectations with perceived performance of a specific service [36, 37]. Satisfaction is interpreted as patient treatment satisfaction, clinical experience and service recommendation [38, 39]. The relationship between perceived service quality, patient satisfaction and behavioral intention was found in many studies [34–37, 40–42]. Therefore, the following hypotheses are developed:
H11: The perceived service quality is positively related to the intention to use TCM.
H12: The perceived service quality is positively related to the satisfaction of using TCM.
H13: The satisfaction of using TCM is positively related to the intention to use TCM.
H14: The satisfaction of using TCM mediates the relationship between the perceived service quality and the intention to use TCM.
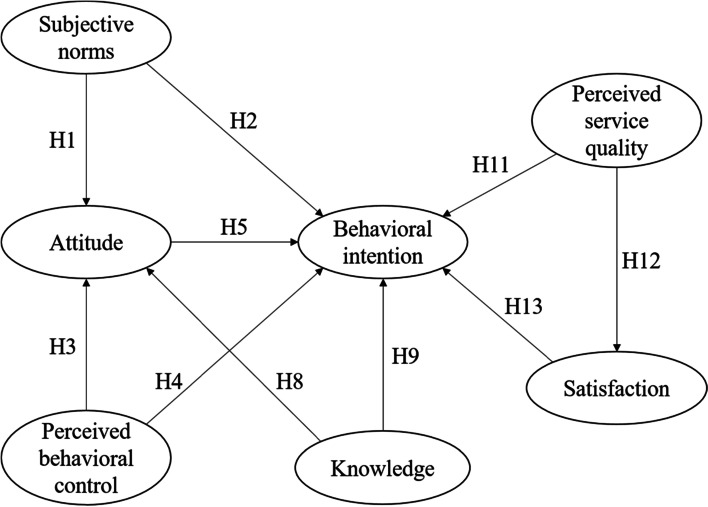
A conceptual model which depicts the relationships between the constructs of TPB, knowledge, satisfaction and perceived service quality of TCM has been developed (Fig. 1).
Fig. 1.
Conceptual model
Methodology
Participants and recruitment procedure
This online cross-sectional survey by a questionnaire was conducted between 15 and 29 November 2021 to address the research question. This study was approved by the Research Committee of College of Professional and Continuing Education, The Hong Kong Polytechnic University. The methodology and results of this study were reported in accordance with the Checklist for Reporting Results of Internet E-Surveys (CHERRIES) [43].
The online questionnaire was initially and purposely sent to participants with varying age and educational level. The link of the survey was posted on social media platforms hosted by the academic institution. Participants were encouraged to forward the questionnaire link to relatives and friends whom they considered suitable. Participants who were literate in Chinese and able to understand the questionnaire; Hong Kong residents aged 18 or above; could access to the internet via smart-phone or computer; consented to participating before they could start the survey; and had used TCM before were included in this study. Interested subjects would read a statement describing the background of the survey, anonymity assurance and participation agreement at the beginning of the survey. Checking the consent box represents that they gave their agreement for study participation. Participation was optional and anonymous. To avoid multiple submissions, the prefix and first three digits of Hong Kong Identity Card (HKID) were collected in the questionnaire. Participants could leave their email address if they were interested to be contacted for survey clarification or join future follow up studies. Identifiers, such as HKID, were removed before data analysis. All decisions were made at subjects’ own discretion. No financial incentives were given after the completion of the questionnaire. The calculation of target sample size should be 10 times the maximum number of measuring items pointing at the construct in the PLS path model [44]. In the present study, there are 33 items measuring seven constructs so the target sample size is 330 (10 × 33).
Measures of questionnaire
The questionnaire consisted of four parts to collect the data regarding the attitude, subjective norms, perceived behavioral control, intention, knowledge, perceived service quality and satisfaction of TCM of respondents. All items in the TPB framework and satisfaction of the use of TCM were measured using the 7-point Likert scale (1 = strongly disagree / Never to 7 = strongly agree / Always). For the perceived service quality, a validated short questionnaire to assess perceived service quality was used [45]. Five items regarding perceived service quality was asked using the 7-point Likert scale (1 = strongly disagree to 7 = strongly agree). The knowledge construct was measured by four questions regarding their self-report knowledge of basic theory, medicine, diagnosis and diet using the 7-point Likert scale (1 = strongly disagree to 7 = strongly agree). The questionnaire items of the seven constructs in this study is shown in Supplementary file 1. Several demographic questions (i.e., age, gender, level of education, economic status, religion, and self-report health status) were also asked in the survey. Respondents were allowed to select more than one religion in the questionnaire.
Data analysis
To examine the conceptual framework in this study, the partial least squares structural equation model (PLS-SEM) was adopted. The reflective measurement model and structural model were examined with the SmartPLS 3.0 statistical software. The reliability and validity of the measurement instrument were verified. To evaluate the reliability of this study, value of Cronbach’s alpha and composite reliability greater than 0.7 is considered to be reliable [44]. The convergent validity is considered good if the outer loadings of the measurement items are greater than 0.6 and the Average Variance Extracted (AVE) of each construct greater than 0.5 [44, 46]. To evaluate discriminant validity, both Fornell Larcker criterion and heterotrait-monotrait (HTMT) ratio were assessed.
Results
Participant characteristics
There were 446 valid responses (n = 446/600, completeness rate: 74.3%). Table 1 shows the demographic characteristics of the participants. 38.6% of the respondents were aged 18 to 25 and 60.3% of the respondents were female. Most of the participants (85.2%) had attained a post-secondary educational level or above. Nearly half and one third of the participants had rated their health status as fair and good respectively.
Table 1.
Demographic characteristics
| Variables | Number of respondents | Percentage |
|---|---|---|
| Age | ||
| 18–25 | 172 | 38.6 |
| 26–35 | 51 | 11.4 |
| 36–45 | 55 | 12.3 |
| 46–55 | 47 | 10.5 |
| 56–65 | 72 | 16.1 |
| 66–75 | 45 | 10.1 |
| 76 or above | 4 | 0.9 |
| Gender | ||
| Male | 177 | 39.7 |
| Female | 269 | 60.3 |
| Educational level | ||
| Primary of below | 3 | 0.7 |
| Secondary | 63 | 14.1 |
| Post-secondary | 169 | 37.9 |
| Degree | 113 | 25.3 |
| Postgraduate or above | 98 | 22.0 |
| Religion | ||
| Christianity | 98 | 22.0 |
| Catholic | 22 | 4.9 |
| Buddhism | 49 | 11.0 |
| Taoism | 11 | 2.5 |
| Confucianism | 2 | 0.4 |
| No religion | 271 | 60.8 |
| Employment status | ||
| Student | 168 | 37.7 |
| Employed | 170 | 38.1 |
| Self-employed | 21 | 4.7 |
| Unemployed | 8 | 1.8 |
| Retired | 79 | 17.7 |
| Monthly income (HK$) | ||
| ≤ 4000 | 171 | 38.3 |
| 4001–16,000 | 55 | 12.3 |
| 16,000 – 28,000 | 81 | 18.2 |
| > 28,000 | 139 | 31.2 |
| Health status | ||
| Poor | 46 | 10.3 |
| Fair | 214 | 48.0 |
| Good | 145 | 32.5 |
| Very good | 33 | 7.4 |
| Excellent | 8 | 1.8 |
Measurement model
The reliability of the model is presented in Table 2. The variance inflation factor (VIF) level of each item was lower than 5, indicating no critical levels of collinearity [44]. All items had outer loadings of greater than 0.6, except one item of attitude construct and one item of perceived service quality. Hence, these two items were deleted. The composite reliability and Cronbach’s alpha were higher than the threshold value of 0.7, indicating a satisfactory internal consistency reliability. The AVE of all constructs were above 0.5, suggesting that the constructs had good convergent validity [44]. The results of the assessment of discriminant validity are presented in Table 3. The discriminant validity in this study was supported. With adequate reliability, convergent validity and sufficient discriminant validity, it was possible to move forward to assess the structure model.
Table 2.
Loadings, Cronbach’s alpha, average variance extracted (AVE), and construct reliability (CR) of the measurement model
| Constructs | Items | Mean | SD | VIF | Loadings | AVE | Composite reliability | Cronbach’s alpha |
|---|---|---|---|---|---|---|---|---|
| Attitude (ATT) | 0.695 | 0.919 | 0.888 | |||||
| A1 | I extremely trust traditional Chinese medicine (TCM) | 5.50 | 1.070 | 2.856 | 0.883 | |||
| A2 | I am very concerned about TCM | 4.89 | 1.333 | 2.000 | 0.801 | |||
| A3 | I’d very much like to accept TCM theory | 5.56 | 1.149 | 2.997 | 0.887 | |||
| A4 | I think TCM is effective | 5.77 | 0.953 | 2.586 | 0.861 | |||
| A5 | I think TCM is safe | 5.62 | 0.959 | 1.618 | 0.725 | |||
| Behavioral intention (BI) | 0.820 | 0.948 | 0.926 | |||||
| BI1 | I would like to use TCM in the future | 5.51 | 1.149 | 2.210 | 0.847 | |||
| BI2 | I would recommend relatives, friends and colleagues to choose TCM | 5.39 | 1.171 | 4.071 | 0.926 | |||
| BI3 | I would say positive things about TCM to others | 5.55 | 1.116 | 4.034 | 0.922 | |||
| BI4 | I would encourage others to use TCM | 5.36 | 1.208 | 4.336 | 0.925 | |||
| Knowledge (K) | 0.798 | 0.940 | 0.916 | |||||
| K1 | I know the basic theory of TCM | 4.38 | 1.426 | 2.940 | 0.909 | |||
| K2 | I know the medicine of TCM | 3.98 | 1.410 | 2.973 | 0.891 | |||
| K3 | I know the diagnosis of TCM | 4.00 | 1.452 | 3.058 | 0.893 | |||
| K4 | I know the diet of TCM | 4.46 | 1.437 | 2.624 | 0.880 | |||
| Perceived behavioral control (PBC) | 0.512 | 0.839 | 0.765 | |||||
| PBC1 | I have time to receive TCM services | 5.29 | 1.157 | 1.508 | 0.745 | |||
| PBC2 | I am economically capable to receive TCM services | 5.42 | 1.158 | 1.644 | 0.681 | |||
| PBC3 | I have the ability to decide whether to choose TCM | 5.93 | 0.913 | 1.508 | 0.664 | |||
| PBC4 | I can share my knowledge and experience of TCM with others | 5.22 | 1.306 | 1.525 | 0.766 | |||
| PBC5 | I can overcome my difficulty in choosing TCM | 5.18 | 1.233 | 1.407 | 0.716 | |||
| Perceived service quality (PSQ) | 0.704 | 0.922 | 0.894 | |||||
| PSQ1 | The TCM services provide their service at the time they promise to do so | 5.22 | 1.090 | 1.792 | 0.746 | |||
| PSQ2 | Personnel of the TCM services react promptly to my requests | 5.12 | 1.087 | 2.342 | 0.845 | |||
| PSQ3 | Personnel of the TCM services are polite | 5.47 | 1.048 | 2.738 | 0.862 | |||
| PSQ4 | Personnel of the TCM services give me personal attention | 5.27 | 1.116 | 3.639 | 0.872 | |||
| PSQ5 | Personnel of the TCM services communicate carefully with me | 5.45 | 1.026 | 2.969 | 0.863 | |||
| Satisfaction (SAT) | 0.847 | 0.957 | 0.940 | |||||
| S1 | My chief complaints can be addressed after receiving TCM | 5.23 | 1.130 | 3.907 | 0.916 | |||
| S2 | I feel better after receiving TCM | 5.43 | 1.093 | 4.493 | 0.934 | |||
| S3 | TCM can fulfill my expectation of treatment | 5.27 | 1.142 | 3.870 | 0.924 | |||
| S4 | I am satisfied with the last curative effect | 5.18 | 1.191 | 3.359 | 0.907 | |||
| Subjective norms (SN) | 0.690 | 0.899 | 0.852 | |||||
| SN1 | My family and friends support me to choose TCM | 5.40 | 1.084 | 1.898 | 0.842 | |||
| SN2 | My family and friends think I should choose TCM | 4.83 | 1.094 | 2.136 | 0.825 | |||
| SN3 | My family and friends will choose TCM | 5.10 | 1.123 | 2.176 | 0.831 | |||
| SN4 | My family and friends choose TCM, I would make the same choice | 4.97 | 1.260 | 1.721 | 0.824 | |||
Table 3.
Construct correlations, square roots of AVE (in italic) and HTMT values
| ATT | BI | K | PBC | PSQ | SAT | SN | |
|---|---|---|---|---|---|---|---|
| ATT | 0.837 | 0.851 | 0.451 | 0.702 | 0.535 | 0.725 | 0.713 |
| BI | 0.775 | 0.906 | 0.428 | 0.744 | 0.578 | 0.720 | 0.727 |
| K | 0.413 | 0.399 | 0.894 | 0.477 | 0.402 | 0.367 | 0.462 |
| PBC | 0.599 | 0.645 | 0.433 | 0.718 | 0.610 | 0.593 | 0.687 |
| PSQ | 0.475 | 0.526 | 0.366 | 0.514 | 0.840 | 0.535 | 0.558 |
| SAT | 0.663 | 0.673 | 0.344 | 0.514 | 0.492 | 0.920 | 0.567 |
| SN | 0.632 | 0.657 | 0.408 | 0.578 | 0.490 | 0.514 | 0.830 |
ATT Attitude, BI Behavioral intention, K Knowledge, PBC Perceived behavioral control, PSQ Perceived service quality, SAT Satisfaction, SN Subjective norms
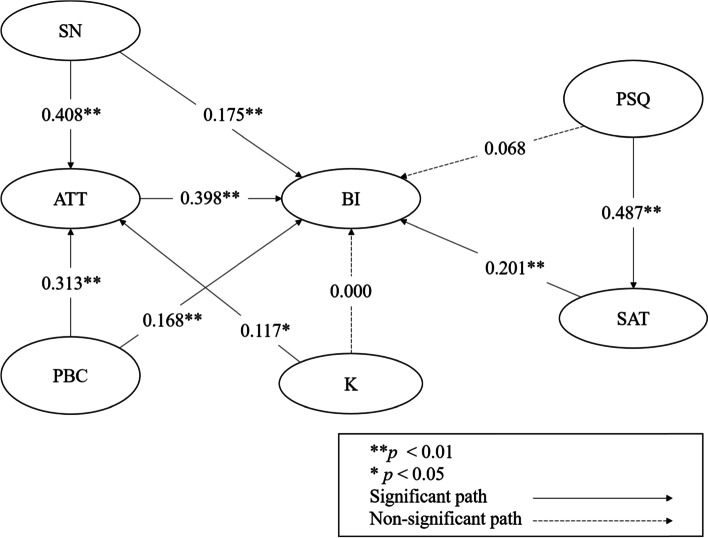
Structural model
The results of the direct effects of structural model are shown in Table 4. These results supported the hypotheses H1, H3 and H8, indicating that the subjective norms (β = 0.408; p < 0.01), perceived behavioral control (β = 0.313; p < 0.01) and knowledge of TCM (β = 0.117; p < 0.05) are positively related to the attitude towards using TCM but the result exhibited weak effect sizes on knowledge. The results showed that subjective norms (β = 0.175; p < 0.01), perceived behavioral control (β = 0.168; p < 0.01), attitude (β = 0.398; p < 0.01) and satisfaction (β = 0.201; p < 0.01) have significantly positive effects on the intention to use TCM. However, there was a non-significant relationship between knowledge and behavioral intention of using TCM (β = 0.000; p > 0.05) and perceived service quality and behavioral intention of using TCM (β = 0.068; p > 0.05). H12 stated that the perceived service quality was positively related to the satisfaction and the results provided statistical support for this hypothesis (β = 0.487; p < 0.01). The results of structural model are shown in Fig. 2. The mediation model results are shown in Table 5. All meditation hypotheses were supported. Attitude had a partial mediating effect on the relationship between subjective norms, perceived behavioral control and intention to use TCM. Attitude had a full mediating effect on the relationship between knowledge and intention to use TCM. Satisfaction had a full mediating effect on the relationship between perceived service quality and intention to use TCM.
Table 4.
Results of the direct effects of structural model
| Hypothesis | Path relations | β | t values | p-values | Decision |
|---|---|---|---|---|---|
| H1 | SN ➔ ATT | 0.408 | 9.226 | < 0.01 | Supported |
| H2 | SN ➔ BI | 0.175 | 4.128 | < 0.01 | Supported |
| H3 | PBC ➔ ATT | 0.313 | 6.360 | < 0.01 | Supported |
| H4 | PBC ➔ BI | 0.168 | 4.132 | < 0.01 | Supported |
| H5 | ATT ➔ BI | 0.398 | 7.718 | < 0.01 | Supported |
| H8 | K ➔ ATT | 0.117 | 2.249 | < 0.05 | Supported |
| H9 | K ➔ BI | 0.000 | 0.004 | 0.997 | Not supported |
| H11 | PSQ ➔ BI | 0.068 | 1.705 | 0.088 | Not supported |
| H12 | PSQ ➔ SAT | 0.487 | 9.379 | < 0.01 | Supported |
| H13 | SAT ➔ BI | 0.201 | 4.146 | < 0.01 | Supported |
ATT Attitude, BI Behavioral intention, K Knowledge, PBC Perceived behavioral control, PSQ Perceived service quality, SAT Satisfaction, SN Subjective norms
Fig. 2.
Results of structural model. ATT: Attitude; BI: Behavioral intention; K: Knowledge; PBC: Perceived behavioral control; PSQ: Perceived service quality; SAT: Satisfaction; SN: Subjective norms
Table 5.
Results of the mediating effects of structural model
| Hypothesis | Path relations | Indirect effect | t values | p-values | Result |
|---|---|---|---|---|---|
| H6 | SN ➔ ATT ➔ BI | 0.162 | 5.919 | < 0.01 | Partial mediating effect |
| H7 | PBC ➔ ATT ➔ BI | 0.125 | 5.085 | < 0.01 | Partial mediating effect |
| H10 | K ➔ ATT ➔ BI | 0.046 | 2.147 | < 0.05 | Full mediating effect |
| H14 | PSQ ➔ SAT ➔ BI | 0.098 | 4.065 | < 0.01 | Full mediating effect |
ATT Attitude, BI Behavioral intention, K Knowledge, PBC Perceived behavioral control, PSQ Perceived service quality, SAT Satisfaction, SN Subjective norms
Discussion
The study sought to assess and examine the relationships among attitude towards TCM, intention to use TCM, knowledge, perceived behavioral control, perceived service quality, satisfaction and subjective norms. The conceptual model was established based on the TPB by integrating customer satisfaction theory and knowledge-attitude-behaviour theory. The present study showed that the attitude towards TCM was significantly influenced by subjective norms, perceived behavioral control and knowledge. For example, advice and referrals by friends and health professionals would motivate individuals to use acupuncture [20]. Additionally, perceived behavioral control was positively related to attitude. Affordability and accessibility have been found to be the reason of using herbs among diabetes patients [47]. Moreover, this study showed that knowledge was positively related to the attitude towards TCM. Such positive correlation towards CAM has been found among health professionals and patients [48, 49]. Nevertheless, another study has not found a significant positive relationship between knowledge and attitude [50]. Further study to examine the knowledge and attitude relationship is needed.
The behavioral intention to use TCM was significantly affected by subjective norms, perceived behavioral control, attitude and satisfaction. This is consistent with the study by McIntyre et al. which demonstrated attitude, subjective norms and perceived behavioral control were significantly predicted the intention to use herbal medicines to manage anxiety symptoms, but strong association between perceived behavioral control and intention to use herbal medicines were found [51]. Nevertheless, a meta-analysis has concluded that attitude towards the behavior is the most important predictor of health behavior intention [52]. Furthermore, satisfaction was one of the predictors to the intention to use TCM. This finding is in line with that of another study which found that satisfaction with treatment was one of the reasons to use acupuncture [20]. The effectiveness of the treatment has influenced the compliance of participating in acupuncture trial [53]. Satisfying with the treatment may cause the users to continue the use of TCM. Our findings also provided empirical support for the mediating role of attitude towards TCM in TPB. Higher levels of subjective norms and perceived behavioral control increased the intention to use TCM directly but also increased individuals’ attitude, which in turn led to intention to use TCM. Therefore, some of subjective norms and perceived behavioral control’s effect on intention to use TCM was explained by attitude.
Contrary to the expectations, knowledge and perceived service quality did not have a significant direct influence on the intention to use TCM. Research has demonstrated that there is no association between patients’ familiarity with and willingness to pay for TCM services [54]. However, lack of knowledge with TCM is one of the concerns about undesirable effects among cancer patients [55]. Therefore, lack of knowledge about TCM may decrease patients’ intention to use TCM. Previous study has also found cancer patients’ willingness to use TCM for rehabilitation is positively correlated with their educational level [56], but another study has found no relationship between educational level and intention to use TCM [24]. Nevertheless, our findings provided empirical support for the mediating role of attitude in the knowledge and intention to use TCM relationship. The results indicated that knowledge affected attitude, and attitude in turn led to intention to use TCM. On the other hand, the result of this study could not find statistically significant direct effect between perceived service quality and intention to use TCM. Unlike a previous study that had demonstrated perceived service quality has a positive effect on repurchasing and sharing of TCM [57]. The mediating role of satisfaction in the relationship between perceived service quality and intention to use TCM was found in the present study. Thus, perceived service quality leads to satisfaction, and satisfaction in turn leads to intention to use TCM.
Practical implication
Predicting the intention to use TCM may facilitate the promotion of TCM in Hong Kong. This study has concluded that attitude towards TCM has the strongest effect on the intention to use TCM, while satisfaction to the TCM is the second predictor to the intention of using TCM. The findings may assist key stakeholders, including TCM profession and related organisations, health professionals and policymakers, to develop policies and community strategies for promoting positive attitude towards TCM and enhancing service quality. Besides, subjective norms and perceived behavioral control could influence individuals’ attitude towards TCM, and lead to positive intention to TCM. To promote the use of TCM in Hong Kong, the development of evidence-based TCM is important. Evidence-based TCM allows both practitioners and patients to understand the effectiveness of TCM and more widely accept, recognise and apply TCM [58]. The integration of TCM and Western medicine may facilitate the promotion of TCM in Hong Kong. Public-private partnership on the use of TCM can foster the integration of TCM and Western medicine. Additionally, building the reputation of the TCM practitioners may enhance the intention to use TCM. TCM practitioners need to take this into account that the quality of treatment is vital for TCM users to have revisit intention to use TCM.
Research implication
The present study offers theoretical contributions to researchers because it is the first study using the extended theory of planned behavior to examine predictors of intention to use TCM. The findings of this study could enhance researchers’ understanding on how TCM users’ intention to use TCM was influenced by different factors. The results may provide insights for researchers to conduct future research on exploring the in-depth views on the intention to use TCM among TCM users in Hong Kong.
Limitations
There are several limitations. First, the data collection was conducted online and promoted through social media, and so younger and educated individuals might be overrepresented in this study. This might lead to selection bias and neglect the participation of older individuals who had limited Internet access. Hence, paper-based surveys in the community and structured interviews would be performed to draw a concrete conclusion about the predictors of the intention to use TCM among Hong Kong population. Second, the recruitment criteria of participants, who had used TCM before, might lead to selection bias. Both TCM users and nonusers would be recruited in further research studies. Third, reliance on the self-report of the questionnaires might cause a measurement bias. Future research using qualitative study to investigate the predictors of the intention of using TCM is recommended. Finally, perceived needs to use TCM is also important in determining the intention to use TCM, but this topic was not included in the questionnaire. Further research should include the construct measuring individual perceived needs to use TCM.
Conclusions
TCM has a long history in Hong Kong and is used by many people in the community. To our knowledge, this is the first study to investigate the predictors of the intention to use TCM in Hong Kong by using TPB. Individuals’ attitude towards TCM has been shown to have stronger effect on the intention to use TCM than other predictors, such as satisfaction, perceived behavioral control and subjective norms. Moreover, the indirect effect of the relationship of subjective norms, perceived behavioral control, knowledge, perceived service quality and intention to use TCM are supported in this study. To enhance the intention to use TCM in Hong Kong, key stakeholders should develop a positive attitude towards TCM in the population. In addition, it is suggested that researchers should explore the in-depth views on the intention to use TCM in future studies.
Supplementary Information
Additional file 1. Supplementary file 1.
Acknowledgements
Not applicable.
Abbreviations
- ATT
Attitude
- AVE
Average variance extracted
- BI
Behavioral intention
- HTMT
Heterotrait-monotrait
- K
Knowledge
- PBC
Perceived behavioral control
- PSQ
Perceived service quality
- SAT
Satisfaction
- SN
Subjective norms
- TCM
Traditional Chinese medicine
Authors’ contributions
TN designed the study, performed the data analysis and contributed in drafting the manuscript; HY, MFL and BF reviewed and edited the manuscript. All authors reviewed and approved the final version of manuscript.
Funding
The work described in this paper was fully supported by a grant from the Research Grants Council of the Hong Kong Special Administrative Region, China (Project Reference No.: UGC/IDS24/18).
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Research Committee of College of Professional and Continuing Education, The Hong Kong Polytechnic University (Ref No. RC/ETH/H/0025). Detailed participant information sheet was provided and informed consent was obtained from all participants prior to participating in the study. All methods were performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest in this work.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chan-Yeung MMW. A Medical history of Hong Kong: 1942–2015. The Chinese University of Hong Kong Press; 2019. [Google Scholar]
- 2.Wong W, Lam CLK, Bian XZ, Zhang ZJ, Ng ST, Tung S. Morbidity pattern of traditional Chinese medicine primary care in the Hong Kong population. Sci Rep. 2017;7:7513. doi: 10.1038/s41598-017-07538-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tang JL, Liu BY, Ma KW. Traditional Chinese medicine. Lancet. 2008;372(9654):1938–1940. doi: 10.1016/S0140-6736(08)61354-9. [DOI] [PubMed] [Google Scholar]
- 4.Chung VC, Wu X, Hui EP, Ziea ET, Ng BF, Ho RS, Tsoi KK, Wong SY, Wu JC. Effectiveness of Chinese herbal medicine for cancer palliative care: overview of systematic reviews with meta-analyses. Sci Rep. 2015;5:18111. doi: 10.1038/srep18111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mayrink WC, Garcia JBS, dos Santos AM, Nunes JKVRS, Mendonça THN. Effectiveness of acupuncture as auxiliary treatment for chronic headache. J Acupunct Meridian Stud. 2018;11(5):296–302. doi: 10.1016/j.jams.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 6.Zhang P, Li J, Han Y, Yu XW, Qin L. Traditional Chinese medicine in the treatment of rheumatoid arthritis: a general review. Rheumatol Int. 2010;30(6):713–718. doi: 10.1007/s00296-010-1370-0. [DOI] [PubMed] [Google Scholar]
- 7.Liu J, Wang S, Zhang Y, Fan HT, Lin HS. Traditional Chinese medicine and cancer: history, present situation, and development. Thorac Cancer. 2015;6(5):561–569. doi: 10.1111/1759-7714.12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li L, Yao H, Wang J, Li Y, Wang Q. The role of Chinese medicine in health maintenance and disease prevention: application of constitution theory. Am J Chinese Med. 2019;47(3):495–506. doi: 10.1142/S0192415X19500253. [DOI] [PubMed] [Google Scholar]
- 9.Cameron D, Epton T, Norman P, Sheeran P, Harris PR, Webb TL, et al. A theory-based online health behaviour intervention for new university students (U@ Uni: LifeGuide): results from a repeat randomized controlled trial. Trials. 2015;16(1):1–15. doi: 10.1186/s13063-015-1092-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Das AK, Abdul Kader Jilani MM, Uddin MS, Uddin MA, Ghosh AK. Fighting ahead: adoption of social distancing in COVID-19 outbreak through the lens of theory of planned behavior. J Hum Behav Soc. 2021;31(1–4):373–393. doi: 10.1080/10911359.2020.1833804. [DOI] [Google Scholar]
- 11.Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. 2021;21(1):1–13. doi: 10.1186/s12889-021-10816-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang X, Liu S, Wang L, Zhang Y, Wang J. Mobile health service adoption in China: integration of theory of planned behavior, protection motivation theory and personal health differences. Online Inf Rev. 2020;44(1):1–23. doi: 10.1108/OIR-11-2016-0339. [DOI] [Google Scholar]
- 13.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- 14.Hagger MS, Chan DK, Protogerou C, Chatzisarantis NL. Using meta-analytic path analysis to test theoretical predictions in health behavior: An illustration based on meta-analyses of the theory of planned behavior. Prev Med. 2016;89:154–161. doi: 10.1016/j.ypmed.2016.05.020. [DOI] [PubMed] [Google Scholar]
- 15.Meng B, Cui M. The role of co-creation experience in forming tourists' revisit intention to home-based accommodation: extending the theory of planned behavior. Tour Manag Perspect. 2020;33:100581. doi: 10.1016/j.tmp.2019.100581. [DOI] [Google Scholar]
- 16.Lino S, Marshak HH, Herring RP, Belliard JC, Hilliard C, Campbell D, Montgomery S. Using the theory of planned behavior to explore attitudes and beliefs about dietary supplements among HIV-positive black women. Complement Ther Med. 2014;22(2):400–408. doi: 10.1016/j.ctim.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Lam CS, Koon HK, Chung VCH, Cheung YT. A public survey of traditional, complementary and integrative medicine use during the COVID-19 outbreak in Hong Kong. PLoS One. 2021;16(7):e0253890. doi: 10.1371/journal.pone.0253890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hon KLE, Leung TF, Tse HM, Lam LN, Tam KC, Chu KM, et al. A survey of attitudes to traditional Chinese medicine among Chinese medical students. Am J Chinese Med. 2005;33(02):269–279. doi: 10.1142/S0192415X05002904. [DOI] [PubMed] [Google Scholar]
- 19.Wang M, Duan LS. 2016 International Conference on Management Science and Engineering (ICMSE) IEEE; 2016. To cure, to relieve, or to comfort? An exploration of the predictors of TCM usage intention among Chinese youth; pp. 1608–1615. [Google Scholar]
- 20.Chan K, Siu JYM, Fung TK. Perception of acupuncture among users and nonusers: a qualitative study. Health Mark Q. 2016;33(1):78–93. doi: 10.1080/07359683.2016.1132051. [DOI] [PubMed] [Google Scholar]
- 21.Xia Y, Chang JH, Miao HZ, Wang D. Impact of the COVID-19 pandemic on intention to use traditional Chinese medicine: a cross-sectional study based on the theory of planned behavior. J Integr Med. 2021;19(3):219–225. doi: 10.1016/j.joim.2021.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tarhan N, Arslan M, Şar S. A structural equation model for pharmacy students’ acquiring knowledge-based behavior towards complementary and alternative medicine. Eur J Integr Med. 2017;16:54–60. doi: 10.1016/j.eujim.2017.10.007. [DOI] [Google Scholar]
- 23.Ben Natan M, Perelman M, Ben-Naftali G. Factors related to the intention of Israelis to use complementary and alternative medicine. J Holist Nurs. 2016;34(4):361–368. doi: 10.1177/0898010115619088. [DOI] [PubMed] [Google Scholar]
- 24.Mou Y. Predicting the use of traditional Chinese medicine health maintenance approach from cultural and spiritual perspectives. J Relig Health. 2017;56(3):971–985. doi: 10.1007/s10943-016-0299-3. [DOI] [PubMed] [Google Scholar]
- 25.Yang Q, Wu S. How social media exposure to health information influences Chinese people’s health protective behavior during air pollution: a theory of planned behavior perspective. Health Commun. 2021;36(3):324–333. doi: 10.1080/10410236.2019.1692486. [DOI] [PubMed] [Google Scholar]
- 26.Dorce LC, da Silva MC, Mauad JRC, de Faria Domingues CH, Borges JAR. Extending the theory of planned behavior to understand consumer purchase behavior for organic vegetables in Brazil: the role of perceived health benefits, perceived sustainability benefits and perceived price. Food Qual Prefer. 2021;91:104191. doi: 10.1016/j.foodqual.2021.104191. [DOI] [Google Scholar]
- 27.Li Y, Zhang S, Song J, Tuo M, Sun C, Yang F. Effects of self-management intervention programs based on the health belief model and planned behavior theory on self-management behavior and quality of life in middle-aged stroke patients. Evid Based Complement Altern Med. 2021;2021:8911143. doi: 10.1155/2021/8911143. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 28.Karimian Z, Sadat Z, Afshar B, Hasani M, Araban M, Kafaei-Atrian M. Predictors of self-medication with herbal remedies during pregnancy based on the theory of planned behavior in Kashan. Iran BMC Complement Altern Med. 2021;21(1):1–7. doi: 10.1186/s12906-021-03353-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koh MZY, Goh YN. Willingness to pay for traditional, complementary and alternative medicine (TCAM) among Malaysian adults. Int J Pharm Healthc Mark. 2021;15(2):312–330. doi: 10.1108/IJPHM-09-2019-0066. [DOI] [Google Scholar]
- 30.Kaiser FG, Fuhrer U. Ecological behavior's dependency on different forms of knowledge. Appl Psychol. 2003;52(4):598–613. doi: 10.1111/1464-0597.00153. [DOI] [Google Scholar]
- 31.Liu L, Liu YP, Wang J, An LW, Jiao JM. Use of a knowledge-attitude-behaviour education programme for Chinese adults undergoing maintenance haemodialysis: randomized controlled trial. Int J Med Res. 2016;44(3):557–568. doi: 10.1177/0300060515604980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang F, Zheng M, Zhu J, Xu WH, Wu WZ, Zou R, et al. Patients’ attitudes to the perioperative application of acupuncture: a Chinese survey. Eur J Integr Med. 2017;9:131–140. doi: 10.1016/j.eujim.2016.12.006. [DOI] [Google Scholar]
- 33.Abamecha F, Tena A, Kiros G. Psychographic predictors of intention to use cervical cancer screening services among women attending maternal and child health services in southern Ethiopia: the theory of planned behavior (TPB) perspective. BMC Public Health. 2019;19(1):1–9. doi: 10.1186/s12889-019-6745-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Oña R, Machado JL, de Oña J. Perceived service quality, customer satisfaction, and behavioral intentions: structural equation model for the metro of Seville. Spain Transp Res Rec. 2015;2538(1):76–85. doi: 10.3141/2538-09. [DOI] [Google Scholar]
- 35.Fu X, Juan Z. Understanding public transit use behavior: integration of the theory of planned behavior and the customer satisfaction theory. Transportation. 2017;44(5):1021–1042. doi: 10.1007/s11116-016-9692-8. [DOI] [Google Scholar]
- 36.Agyapong A, Afi JD, Kwateng KO. Examining the effect of perceived service quality of health care delivery in Ghana on behavioural intentions of patients: the mediating role of customer satisfaction. Int J Healthc Manag. 2018;11(4):276–288. doi: 10.1080/20479700.2017.1326703. [DOI] [Google Scholar]
- 37.Kim CE, Shin JS, Lee J, Lee YJ, Kim MR, Choi A, et al. Quality of medical service, patient satisfaction and loyalty with a focus on interpersonal-based medical service encounters and treatment effectiveness: a cross-sectional multicenter study of complementary and alternative medicine (CAM) hospitals. BMC Complement Altern Med. 2017;17(1):1–12. doi: 10.1186/s12906-017-1691-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liang H, Xue Y, Zhang ZR. Patient satisfaction in China: a national survey of inpatients and outpatients. BMJ Open. 2021;11(9):e049570. doi: 10.1136/bmjopen-2021-049570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Y, Fang J, Gao W, Han Y, Zhang R, He L, Liu B. Treatment satisfaction in Chinese medicine outpatient care: a comparison of patients’ and doctors’ views. BMC Complement Altern Med. 2019;19(1):1–11. doi: 10.1186/s12906-019-2729-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cronin JJ, Jr, Brady MK, Hult GTM. Assessing the effects of quality, value, and customer satisfaction on consumer behavioral intentions in service environments. J Retail. 2000;76(2):193–218. doi: 10.1016/S0022-4359(00)00028-2. [DOI] [Google Scholar]
- 41.Li SJ, Huang YY, Yang MM. How satisfaction modifies the strength of the influence of perceived service quality on behavioral intentions. Leadersh Health Serv. 2011;24(2):91–105. doi: 10.1108/17511871111125675. [DOI] [Google Scholar]
- 42.Polas MRH, Raju V, Hossen SM, Karim AM, Tabash MI. Customer's revisit intention: empirical evidence on gen-Z from Bangladesh towards halal restaurants. J Public Aff. 2020:e2572. 10.1002/pa.2572.
- 43.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES) J Medical Internet Res. 2004;6(3):e132. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hair JF, Hult GTM, Ringle C, Sarstedt M. A primer on partial least squares structural equation modeling (PLS-SEM) (2nd ed) Sage Publications; 2016. [Google Scholar]
- 45.Konerding U, Bowen T, Elkhuizen SG, Faubel R, Forte P, Karampli E, et al. Development of a universal short patient satisfaction questionnaire on the basis of SERVQUAL: psychometric analyses with data of diabetes and stroke patients from six different European countries. PLoS One. 2019;14(10):e0197924. doi: 10.1371/journal.pone.0197924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jordan EJ, Spencer DM, Prayag G. Tourism impacts, emotions and stress. Ann Tour Res. 2019;75:213–226. doi: 10.1016/j.annals.2019.01.011. [DOI] [Google Scholar]
- 47.Kamel FO, Magadmi RM, Hagras MM, Magadmi B, AlAhmad RA. Knowledge, attitude, and beliefs toward traditional herbal medicine use among diabetics in Jeddah Saudi Arabia. Complement Ther Clin Pract. 2017;29:207–212. doi: 10.1016/j.ctcp.2017.10.007. [DOI] [PubMed] [Google Scholar]
- 48.Shorofi SA, Arbon P. Complementary and alternative medicine (CAM) among hospitalised patients: an Australian study. Complement Ther Clin Pract. 2010;16(2):86–91. doi: 10.1016/j.ctcp.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 49.Shorofi SA, Arbon P. Complementary and alternative medicine (CAM) among Australian hospital-based nurses: knowledge, attitude, personal and professional use, reasons for use, CAM referrals, and socio-demographic predictors of CAM users. Complement Ther Clin Pract. 2017;27:37–45. doi: 10.1016/j.ctcp.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 50.Ng TKC, Lo MF, Fong BYF. Knowledge, attitude, utilisation and satisfaction of traditional Chinese medicine in Hong Kong. Int J Pharm Healthc Mark. 2021. 10.1108/IJPHM-08-2020-0068.
- 51.McIntyre E, Saliba AJ, Wiener KK, Bishop FL. Predicting the intention to use herbal medicines for anxiety symptoms: a model of health behaviour. J Ment Health. 2017;28(6):589–596. doi: 10.1080/09638237.2017.1417553. [DOI] [PubMed] [Google Scholar]
- 52.McEachan RRC, Conner M, Taylor NJ, Lawton RJ. Prospective prediction of health-related behaviours with the theory of planned behaviour: a meta-analysis. Health Psychol Rev. 2011;5(2):97–144. doi: 10.1080/17437199.2010.521684. [DOI] [Google Scholar]
- 53.Cao HJ, Li X, Li XL, Ward L, Xie ZG, Hu H, et al. Factors influencing participant compliance in acupuncture trials: An in-depth interview study. PLoS One. 2020;15(4):e0231780. doi: 10.1371/journal.pone.0231780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Meng F, Ji Z, Song F, Bai T, Fan X, Wang D. Patients’ familiarity with, trust in and willingness to pay for traditional Chinese medicine in Chinese community health care centres. Eur J Integr Med. 2020;36:101118. doi: 10.1016/j.eujim.2020.101118. [DOI] [Google Scholar]
- 55.Chan HY, Chui YY, Chan CW, Cheng KK, Shiu AT, So WK, et al. Exploring the influence of traditional Chinese medicine on self-care among Chinese cancer patients. Eur J Oncol Nurs. 2014;18(5):445–451. doi: 10.1016/j.ejon.2014.05.005. [DOI] [PubMed] [Google Scholar]
- 56.Yu HY, Wang XQ, Zhang Y, Liu J, Lin HS. Application status of Chinese medicine on Cancer rehabilitation: a preliminary questionnaire survey. Chin J Integr Med. 2020;26(12):890–896. doi: 10.1007/s11655-020-3280-7. [DOI] [PubMed] [Google Scholar]
- 57.Li H, Wang L, Xia X, Liu H. Perceived service quality’s effect on patient loyalty through patient attitude within the context of traditional Chinese medicine. J Comb Optim. 2020;42:1030–1041. doi: 10.1007/s10878-019-00520-z. [DOI] [Google Scholar]
- 58.Chen YL, Zhao C, Zhang L, Li B, Wu CH, Mu W, et al. Toward evidence-based Chinese medicine: status quo, opportunities and challenges. Chin J Integr Med. 2018;24(3):163–170. doi: 10.1007/s11655-017-2795-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplementary file 1.
Data Availability Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.