Abstract
Ovarian endometriosis may increase the risk of malignancy. Several studies have suggested atypical endometriosis as the direct precursor of endometriosis-associated ovarian cancer. We performed an advanced, systematic search of the online medical databases PubMed and Medline. The search revealed n = 40 studies eligible for inclusion in this systematic review. Of these, n = 39 were finally included. The results from included studies are characterized by high heterogeneity, but some consistency has been found for altered expression in phosphoinositide 3-kinase (PI3K)/AKT/mTOR pathway, ARID1a, estrogen and progesterone receptors, transcriptional, nuclear, and growth factors in atypical endometriosis. Although many targets have been proposed as biomarkers for the presence of atypical endometriosis, none of them has such strong evidence to justify their systematic use in clinical practice, and they all need expensive molecular analyses. Further well-designed studies are needed to validate the evidence on available biomarkers and to investigate novel serum markers for atypical endometriosis.
Keywords: endometriosis, atypical, atypical endometriosis, marker, biomarker, atypia
1. Introduction
Endometriosis is a chronic, estrogen-dependent, progressive disease affecting approximately 10% of women of reproductive age [1]. Initially considered a benign disease, endometriosis, and particularly ovarian endometriosis (OMA), may increase the risk of developing malignancy. An association between endometriosis and ovarian cancer was initially proposed in 1925 by Sampson, describing endometrial carcinoma of the ovary arising in endometrial tissue [2]. Then, the transition from endometriosis to ovarian cancer was confirmed in 1953, when Scott wrote about malignant changes in endometriosis and pointed out that benign endometriosis might be observed in proximity to endometriosis-associated ovarian cancer (EAOC) [3].
It has been estimated that 0.5–1% of endometriosis cases are complicated by neoplasia, with a lifetime risk of about 1.9%, but it is relatively increased compared to the general population, having a lifetime risk of approximately 1.4% [4]. In a pooled meta-analysis of 13 case-control studies, the frequency of self-reported endometriosis was significantly higher in the ovarian cancer group (OR 1.46). The OR were significantly increased in the hystotypes: Clear cell ovarian carcinoma (CCC) (OR 3.05), Endometrioid ovarian carcinoma (EnOC) (2.04), and Low-grade serous ovarian carcinoma (OR 2.11) [5].
Several studies have reported that atypical endometriosis (AE) should be considered as the direct precursor of CCC and EnOC, as AE has been identified as contiguous with these tumor histotypes [6,7]. AE refers to two different histologic findings: cellular atypia, also known as cytologic atypia, and architectural atypia, commonly referred to as hyperplasia [8]. The “road” to malignant transformation is not well established, although several pathways leading to AE and finally to EAOC have been suggested: oxidative stress, cytokines, genetic mutations, and hyperestrogenic environment may have a role in the carcinogenesis from benign endometriosis (BE) to cancer. Two potential scenarios for ovarian endometrioma leading to EAOC have been proposed. The one involves extracellular hemoglobin, iron, and heme (from the repeated hemorrhages occurring in endometriosis), causing cellular oxidative damage via increased reactive oxygen species (ROS) with subsequent DNA damage and resulting mutations. The second involves the persistent production of antioxidants, which would favor a tumor-potentiating environment. Most CCC and EnOC are included in Type I ovarian tumors, since they develop from benign extraovarian lesions that implant on the ovary and can subsequently undergo malignant transformation (i.e., in endometriosis they arise within benign ovarian endometriotic cysts). Type I ovarian tumors are clinically indolent and usually present with low-grade carcinoma [9,10]. Indeed, AE and EAOC share common molecular/genetic alterations such as somatic ARID-1A [11,12] and Phosphatase and tensin homolog (PTEN) mutations [13], Phosphatidylinositol-4,5-Bisphosphate 3-Kinase Catalytic Subunit Alpha (PIK3CA) mutations [14], hepatocyte nuclear factor (HNF)-1b up-regulation [15], loss of estrogen receptor (ER) and progesterone receptor (PR) [16], and rarely P53 mutations [17]. These mutations exhibit the continuum of tumor progression between benign cystic neoplasms and the corresponding carcinomas, such as EnOC and CCC, often through precursor lesions, such as AE. These and other targets have been proposed for the early detection of endometriosis-related cancers, but the clinical application of these novel biomarkers may be difficult since they all need molecular analysis. To the best of our knowledge, this is the first study that systematically reviews the current literature focused on AE-associated biomarkers to offer a general view of available data.
2. Materials and Methods
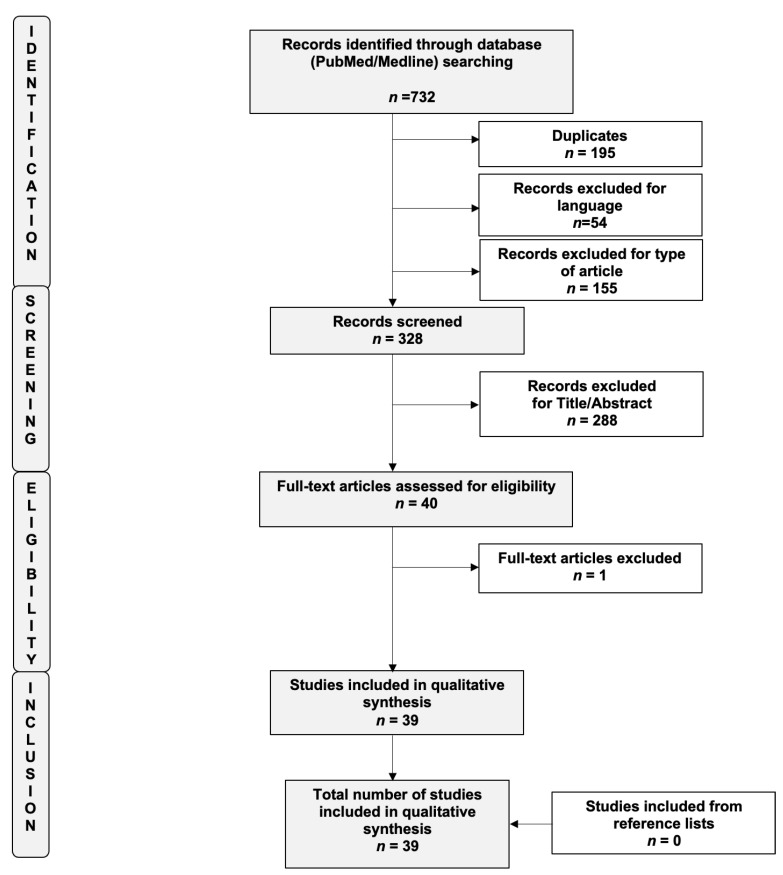
The study was registered “a priori” and accepted for inclusion in the PROSPERO database (ID CRD42021254634). The systematic review was carried out in accordance with the methods proposed by the Preferred Reporting Item for Systematic Reviews and Meta-analysis (PRISMA) guidelines [18]. We performed an advanced, systematic search of the online medical databases PubMed and Medline using the following keywords: “Endometriosis”, “Atypical”, “Atypical endometriosis”, “Marker”, “Biomarker”, and “Atypia”. To optimize the search output, we used specific tools available in each database, such as Medical Subject Headings (MeSH) terms (PubMed/Medline). EndNote software (available online: https://endnote.com, accessed on 1 July 2021) was used to remove duplicate articles. Only full-length manuscripts written in English up to June 2021 were considered. To overcome the low number of published articles, we also decided to include case reports and series in this systematic review of the literature. We checked all citations found in the title and abstract to establish the eligibility of the source and obtained the full text of eligible articles. A flow diagram of the systematic review is shown in Figure 1 (PRISMA template). We also performed a manual scan of the reference lists of the review articles to identify any additional relevant citations. Three review authors (R.V., M.S., and L.B.) independently assessed the risk of bias for each study using the risk-of-bias tool for case–control studies developed by Clarity group [19] according to the following domains: (i) Can we be confident in the assessment of exposure?; (ii) Can we be confident that cases had developed the outcome of interest and controls had not?; (iii) Were the cases properly selected?; (iv) Were the controls properly selected?; (v) Were cases and controls matched according to important prognostic variables or was statistical adjustment carried out for those variables? We graded each potential source of bias as definitely yes (low risk of bias), probably yes (moderate risk of bias), probably no (serious risk of bias), or definitely no (critical, high risk of bias). We summarized the risk of bias judgments across different studies for each of the domains listed. The risks of bias of the included studies are summarized in Supplementary Figure S1.
Figure 1.
Flow diagram of the search strategy, screening, eligibility, and inclusion criteria (PRISMA template).
3. Results
The search revealed n = 40 studies eligible for inclusion in this systematic review. Of these, n = 39 were finally included [11,14,15,17,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54]. A flow diagram of the systematic review is shown in Figure 1 (PRISMA template). The main characteristics of the included studies are summarized in Table 1.
Table 1.
Studies investigating molecular targets associated with atypical endometriosis.
| Authors | Date | Type of Study | Immunohistochemical Analysis | Study Period | AE (n), Mean Age ± ds (yo) |
EAOC (n), Mean Age ± ds (yo) |
Endometrios (n), Mean Age ± ds (yo) |
Results |
|---|---|---|---|---|---|---|---|---|
| Chalas et al. [20] | 1990 | Retrospective Study | Average AgNORs * per nucleus |
NR | 10, NR | 10, NR | 10, NR |
|
| Ogawa et al. [21] | 2000 | Retrospective Study | Ki-67 | 1980–1995 | 29, NR | 30 CCC, 3 EnOC, 4 OSC, 51.4 yo (range, 22–80 years) |
33, NR |
|
| Bayramoglu et al. [22] | 2001 | Retrospective Study | p53 | NR | 7, 34.1 ± NR | 10, NR | 137, 36.1 ± NR |
|
| Nezhat et al. [23] | 2002 | Comparative Study | bcl-2, p53 | NR | -- | 24 EnOC, 19 CCC, 40 OSC; NR | 30; NR |
|
| Del Carmen et al. [24] | 2003 | Retrospective study | VEGF, Ki-67, ER, PR | NR | 17, NR | 8, NR | -- |
|
| Amemiya et al. [25] | 2004 | Case series | K-ras mutation MSI |
1987–1999 | -- | 12 EnOC, 56 ± 7.3 (range 43–68) | -- |
|
| Sáinz de la Cuesta et al. [26] | 2004 | Retrospective study | p53, c-erbB-2, MIB1, and Bcl-2 |
1948–1999 | 6 45.5 yo (range 33–78) |
17 45.5 yo (range 33–78) |
17 45.5 yo (range 33–78) |
|
| Akahane et al. [27] | 2005 | Case Series | ERα, ERβ, PRA, PRB p53, Ki-67, c-erbB-2, EGFR |
1993–2000 | -- | 4 CCC, 56,5 ± 1.11 4 EnOC, 56,8 ± 7.8 |
-- |
Both CCC and EnOC:
|
| Kato N et al. [15] | 2006 | Retrospective Study | HNF-1beta | NR | 4, 32–79 | 30 (17 CCC), 32–79 | 40, NR |
|
| Ali-Fehmi et al. [28] | 2006 | Retrospective Study | LOH and MSI at PTEN (10q23.3) in loci D10S215, D10S608, and D10S541 |
NR | 12, NR | 20, NR 5 CCC 7 EnOC 8 OSC |
23, NR |
|
| Akahane et al. [17] | 2007 | Retrospective Study | p53 | 1993–2002 | -- | 13 CCC, 55 ± NR (range 29–62) 9 EnOC, 51 ± NR (range 42–76) |
7, 34 ± NR (range 30–43) |
|
| Finas et al. [29] |
2008 | Retrospective Study | L1CAM | NR | 14, NR | -- | 17, NR |
|
| Yamamoto et al. [30] | 2008 | Retrospective Study | PDGFR-a, PDGFR-b, PDGF-AB | 1987–2005 | 19, NR | 31 CCC, NR | 17, NR |
|
| Wiegand et al. [11] | 2010 | Case reports of 2 patients | BAF250a | NR | 2 AE contiguous to CCC | 2 CCC | 2 distant endometriosis to CCC |
|
| Yamamoto et al. [31] | 2010 | Retrospective Study | p27Kip1, Skp2, Cks1, cyclin A, and cyclin E, and Ki67 labeling index |
1988–2007 | 15, NR | 23 CCC, NR | 31, NR |
|
| Yamamoto et al. [14] | 2011 | Retrospective Study | PIK3CA | 1986–2007 | 8, NR | 23 CCC, NR | 8, NR |
|
| Kato et al. [32] | 2012 | Retrospective Study | p-mTOR, HIF-1, Glut1 | 1987–2005 | 16, NR | 36 CCC, NR | 21, NR |
|
| Xiao et al. [33] | 2012 | Retrospective study | BAF250a, HNF-1b, ER and PR | 1995–2010 | 13 | 26 CCC | 36 |
|
| Yamamoto et al. [34] | 2012 | Retrospective Study | ARID1A, PIK3CA | 1986–2007 | 22, NR | 28 CCC, NR | 22, NR |
|
| Yamamoto et al. [35] | 2012 | Retrospective Study | MET | 1987–2006 | 10, NR | 5 CCC, NR | 10, NR |
|
| Yamamoto et al. [36] | 2012 | Retrospective study | ACTN4 gene (encoding for Actinin-4) | 1986–2007 | 12 adjacent to tumor, of which:-9 both AE and BE -3 only AE |
16 adjacent to tumor, of -9 both AE and BE which:-7 only BE |
19 CCC |
|
| Lai et al. [37] | 2013 | Retrospective Study | ER, HNF-1 beta, p53, PTEN, BAF250a, COX-2 |
2001–2011 | -- | 79 ((33 EnOC; 40 CCC; 4 OSC; 1 ASC; 1 AS), NR | -- |
|
| Vercellini et al. [38] | 2013 | Retrospective study | IMP3 | 2004-2009 | 9 (35.1 ± 8.1) | NR | 508 |
|
| Lin et al. [39] | 2014 | Retrospective Study | SRAP, ERs | 2003–2012 | 12, 32–62 yo | 12 CCC, 32–62 yo | 24, NR |
|
| Suryawanshi et al. [40] | 2014 | Retrospective Study | Immune gene expression analysis | NR | 15 (48 ± 6.5) | 28 (54.8 yo ± 11.6) | NE: 32 (46.5 yo ± 6) BE:30 (40 yo ± 10) |
|
| Anglesio et al. [41] | 2015 | Whole-genome shotgun sequencing (WGSS) | Overall pattern of somatic mutations within EAOC (CCC and EnOC) | NR | - | 7 CCC | 7 |
|
| Matsumoto et al. [42] | 2015 | Retrospective Study | HIF-1a, iNOS, PIK3CA, pAkt, p65, and HNF-1β, Mutations of the β-Catenin and PIK3CA Genes | 2000–2014 | -- | 28 CCC, 35 EnOC, 54.1 (range 22–28) | -- |
|
| Er et al. [43] | 2016 | Case series | DNA extraction and sequencing | 2006–2012 | -- | 8 CCC 2 EnOC |
-- |
|
| Kato et al. [44] | 2016 | Retrospective Study | BAF250a | 1984–2007 | 38, NR | 38 CCC, NR | 18, NR |
|
| Ma et al. [45] | 2016 | Retrospective Study | PTEN and p53 | 10, NR | 23, NR | 20, NR |
|
|
| Stamp et al. [46] | 2016 | Retrospective study | BAF250a | 2005–2008 | 23 associated with cancer 8 not associated with cancer 45 yo (33–59) |
21 EnOC, 50 yo (30-70) 11 CCC, 57 yo (34–68) 3 mixed |
|
|
| Andersen et al. [47] | 2018 | Retrospective Study | E2sig, ERα, ERβ, PR | NR | 11, 47 (range 34–20) | 19, 57.5 (range 47–77) 5 CCC 14 EnOC |
11, 39 (range 25–74) |
|
| Zhang et al. [48] | 2018 | Retrospective Study | genome-wide transcriptomic profiling | NR | 4, NR | 5 EnOC, NR | 4, NR |
|
| Niguez-Sevilla et al. [49] | 2019 | Prospective Study | Ki-67, BAF250a, COX-2 | 2014–2017 | 23 | 26 | 159 |
|
| Jiao et al. [50] | 2019 | Case Report | CK7, CEA, p16, CA 125, MUC-6, p53, PTEN, ER, PR, CK20, PAX-8, CDX-2 | NR | 46 yo | 1 OMC | NR |
|
| Păvăleanu et al. [51] | 2020 | Retrospective Study | E-cadherin,β-catenin, CK18, Bcl-2/Bax, ER, PR | 2005-2017 | -- | 19 (8 EnOC; 11 non EnOC), 59.10 yo | 31, 36.61 yo |
|
| Penciu et al. [52] | 2020 | Case Series | ER, PR, Ki67, p53, p16, WT1, CD 34, CD10 | 2015–2017 | -- | 2 EnOC, 2 OSC; 30–60 yo | -- |
|
| Lenz et al. [53] | 2021 | Retrospective Study | ER, PR, Ki67, p53 | NR | 5, NR | -- | 40, 33.1 yo (22.0–47.0) |
|
| Shin et al. [54] | 2021 | Case control study | TSPAN1 | NR | 18 (40 ± 6.6) | 7 AdjEm (44.5 ± 11) 17 CCC (43.6 ± 10.6) 12 EnOC (48.5 + 10) |
9 (27.7 ± 5.4) |
|
* p-values statistically significant (p < 0.05). Legend. NR, Not reported; AE, atypical endometriosis; TE, Typical endometriosis; EAOC, endometriosis-associated ovarian cancer; yo, years old; MSI, Microsatellite Instability; ER, Estrogens Receptor; PR, Progesterone receptor; EGFR, Epithelial Growth Factor Receptor; HNF-1beta, hepatocyte nuclear factor-1beta; LOH, Loss of Heterozygosity; PTEN, Phosphatase and tensin homolog; EnOC, ovarian endometrioid carcinoma; CCC, ovarian clear cell carcinoma; CCAF, benign clear-cell adenofibroma; OSC, ovarian serous carcinoma; OMC, ovarian mucinous carcinoma; E2sig, a panel of 236 genes associated with endocrine response, 158 of which showed statistically significant changes in expression between different disease states; FGF18, Fibroblast Growth Factor 18; L1-ICAM, L1, cell adhesion molecule; PDGFR, platelet-derived growth factor receptor; PDGF, platelet-derived growth factor; Cks, cyclin-dependent kinase subunit 1; p-mTOR, phosphorylated mammalian target of rapamycin; ARID1A, AT-rich interactive domain 1;AHIF-1, hypoxia-inducible factor-1; Glut1, glucose transporter 1; COX-2, cyclooxygenase-2; SRAP, steroid receptor RNA activator protein; ASC, adenosquamous carcinoma; AS, adenosarcoma; iNOS, inducible nitric oxide synthase; CEA, Carcinomatous embryonic antigen; CK, Cytokeratin; CA 125, Carbohydrate Antigen 125; MUC-6, Mucine 6; PAX-8, Paired-box gene 8; CDX2, Caudal Type Homeobox 2; Bcl-2, B-cell lymphoma 2; Bcl-2-associated X, BAX; CD, cluster of differentiation; WT1, Wilm’s tumor 1; TSPAN1, Tetraspanin1; AdjEm, adjacent endometriosis to OCCC; NE, normal endometrium; BE, benign endometriosis; C3, C4a, C7, CFD, CFB, CFH, Complement factors 3, 4a, 7, D, B, H;, MASP1, mannose-associated serine protease 1; IHC, immunohistochemistry; BAF250a, Brahma-associated factor (BRG-)associated factor 250a; HNF-1β, hepatocyte nuclear factor 1β; IMP3, insulin-like growth factor II mRNA-binding protein 3; PPV, Positive predictive value; NPV, Negative predictive value; PIK3CA, phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha. * Nucleolar organizer regions (NORs) are loops of DNA, which are associated with nonhistone nucleoproteins, and they can be stained with silver (AgNORs). An increased number of AgNORs per nucleus is observed in many malignancies.
To make the paragraph easier to read, the results derived from the various studies will be presented based on the biological role of the investigated molecules. It is interesting to note that all the above-reported data derive from immunohistochemical analysis, since there are no studies that assess hematological or serum biomarkers for atypical endometriosis.
3.1. PI3K/AKT/mTOR Pathway
The phosphatidylinositol 3-kinases (PI3K)/AKT/mTOR pathway is an intracellular signaling pathway that is important in regulating the cell cycle. In many cancers, this pathway is overactive, thus reducing apoptosis and allowing proliferation.
There are many known factors that enhance the PI3K/AKT pathway, including Epidermal growth factor (EGF), Sonic hedgehog (shh), Insulin-like growth factor 1 (IGF-1), and insulin. Both leptin and insulin recruit PI3K signaling for metabolic regulation. The pathway is antagonized by various factors, including PTEN. Moreover, this kinase cascade is highly interconnected with other pathways that regulate cell proliferation, such as the RAS/MAPK/ERK pathway. K-Ras GTPase, which is encoded by the KRAS gene, once activated can upregulate PI3K cell signaling receptors [9].
Five out of 39 studies investigated the correlation between PIK3CA mutations and the presence of AE [14,34,41,42,43]. All of these studies reported concordant mutations in PIK3CA either in cancer or in contiguous AE. PIK3CA is a protein coding gene and, as an integral part of the PI3K pathway, it has long been described as an oncogene. In their retrospective study, Yamamoto et al. [14] found that somatic mutations of the PIK3CA gene were detected in 10/23 (43%) CCC, and in all cases, the type of mutation was H1047R in the kinase domain. The same mutation was retrieved in 6/8 non-atypical endometriotic lesions (75%) and 7/8 atypical endometriotic lesions (88%). These data suggest that mutations of the PIK3CA gene occur in the putative precursor lesions of CCC as very early events in tumorigenesis, probably initiating the malignant transformation of endometriosis in AE, and finally in cancer. The same group of authors showed that somatic mutations of PIK3CA were detected in 17 (40%) tumors, and the majority (71%) of these were ARID1A-deficient carcinomas. All of the 6 PIK3CA-mutation-positive typical endometriosis (TE) were immunohistochemically ARID1A deficient; at the same time, all of the 6 AE harboring PIK3CA mutations were ARID1A deficient [34]. They speculated that the coexistence of the loss of ARID1A expression and PIK3CA mutations suggested a possible cross-talk between the regulation of ARID1A expression and the PI3K signaling pathway during ovarian CCC development.
Confirming their results, Anglesio et al. conducted a whole-genome shotgun sequencing (WGSS) of somatic mutations within 7 cases of CCC. In each specimen, at least one specimen of AE and TE was present for each case. They found that the fraction of detectable somatic mutations that was shared between endometriosis and patient-matched carcinoma ranged from 15 (distant TE) to 98 % (adjacent AE). With the exception of PIK3CA and ARID1A, the constituents of the conserved mutations were generally unique. In cases with somatic ARID1A and/or PIK3CA mutations, they were consistently found to be present across all cancer specimens, as well as any AE or TE from those cases [41]. Matsumoto et al. also found that PIK3CA mutations were observed either in 31.4% of EnOC and 35.7% of CCC, or in five coexisting cases of AE and in 2 cases of non-AE [42]. They also observed that a significantly different expression of Akt, another component of the PI3K pathway, was evident between the two types of EAOC and their coexisting AE and non-AE. Finally, Er et al., after DNA extraction and sequencing of 8 CCC and 2 EnOC, observed that PIK3CA was the most frequent mutation, and it was also observed in concomitant AE in 3/6 cases (50%), even if they reported that only in one case (16%) ARID1A and PIK3CA were both mutated [43]. Only one study assessed the relationship between p-mTOR and the presence of AE [40], showing that the frequency of mTOR immunopositivity was 58% in non-AE, 63% in AE, and 77% in EAOC, with an increasing trend from benign and precursor lesions toward cancer.
Five out of 39 studies reported PTEN mutations associated with AE, with controversial results [28,37,40,45,50]. PTEN acts as a tumor suppressor gene through the action of its phosphatase protein product, which negatively regulates the PI3K/AKT/mTOR pathway.
In their retrospective study, Ali-Fehmi et al. reported that loss of heterozygosity (LOH), microsatellite instability (MSI), and mutations that lead to functional inactivation of PTEN were present either in EAOC, or in endometriosis and AE, suggesting that these genetic alterations may be very early in tumor progression and confirming their precursor status. Moreover, significant differences in LOH were seen between endometriosis (4.3%) and EAOC (23.5%) at D10S608, suggesting that LOH at D105608 may possibly be an important molecular event in the progression of endometriosis to carcinoma [28].
Concomitant PTEN mutations in cancer and coexisting AE were also reported in another retrospective study [37]. Suryawanshi et al. demonstrated that PTEN and K-ras mutations in mice lead to complement upregulation [40]. Gene expression analyses revealed that the complement pathway was most prominently involved in both endometriosis and EAOC. Moreover, from an immune gene expression analysis, they found that AE shared the EAOC pattern. Once again, AE seems to be the precursor of cancer.
In contrast to these findings, Ma [45] and Jiao [50] showed that PTEN expression in cancer was not consistent with its expression in AE. The former in his retrospective study concluded that PTEN and p53 mutation frequency in EAOC were significantly higher compared to AE and endometriosis. The latter, instead, in a case report study, showed a negative immunohistochemical (IHC) PTEN expression both in EAOC and AE. This study is obviously limited by its low population and study design.
Finally, 3 out of 39 studies investigated Kras expression in AE compared to cancer and TE [25,40,48]. Two of them demonstrated that Kras is present either in cancer or in AE and that its expression is related to a higher complement pathway [40] and NFkB signaling activation in AE and EAOC [48]. In contrast to these findings, in a case series study, Amemiya showed that KRAS mutations may be a late event in the malignant transformation to cancer, since they have been observed only in cancer but not in AE or TE [25].
3.2. ARID1a and BAF250
BAF250a, the protein encoded by ARID1A, is one of the accessory subunits of the SWI–SNF complex believed to confer specificity in the regulation of gene expression. In analyzing the correlations between mutations or other aberrations in ARID1A and BAF250a expression in ovarian cancer and contiguous AE, eight studies detected possible correlations [11,33,34,37,43,44,46,49], with a rate of ARID1A mutations and BAF250A loss of expression in AE ranging from 23.8 to 100%. In particular, the study conducted by Wiegand et al. found two patients with ovarian CCC carrying ARID1A mutations in contiguous AE; samples of both the ovarian CCC and AE demonstrated loss of BAF250a expression maintaining his expression in the distant typical endometriotic lesion [11].
Similarly, Yamamoto et al. found that 61% of endometriosis-associated ovarian CCC were ARID1A-deficient. Among them, 86% of TE and 100% of AE were judged as ARID1A deficient [34]. The mutational status in 409 cancer-associated genes of 10 Taiwanese patients with EAOC (8 EnOC; 2 ovarian CCC) showed that ARID1A was mutated in 50% of cases. In their concomitant AE, ARID1A was mutated in 33.3% of cases (2/6) [43].
A retrospective study conducted by Xiao et al. examining molecular alterations found loss of BAF250a expression in about 20% of TE, and a similar pattern of expression in AE (38.5%) and CCC (57.7%) in comparison to papillary serous carcinoma [33].
Lai et al., when comparing the expression of BAF250a among 79 cases of EAOC (40 CCC; 33 EnOC; 4 serous carcinomas; 1 adenosquamous carcinoma, and 1 adenosarcoma), revealed loss of BAF250a in 37 (47%) cases but without statistical significance among different subtypes. Interestingly, all staining results were similar between EAOC and contiguous AE [37].
Kato et al. observed BAF250a deficient expression in 30% (29/97) of ovarian CCC, and among them, they found more frequently the concurrence of endometriosis compared with BAF250a retained cases (p < 0.05). The frequencies of BAF250a deficient expression were 19% (6/31) in TE, 26% (10/38) in AE, 39% (15/38) in synchronous with endometriosis CCC, and 6% (1/18) in solitary endometriosis [44].
A retrospective study conducted by Stamp et al. showed loss of BAF250a expression in 14/35 cancer patients. Among them, AE was present in 10 cases showing BAF250a loss in 60% of cases. None of the 8 cases of AE not associated with cancer had BAF250a loss [46].
A Spanish prospective study conducted by Niguez-Sevilla et al. analyzing 185 patients with endometriosis reported AE in 23 cases (12.43%), of which 14 (60.86%) had endometriosis alone and the other 9 (39.13%) had EAOC. They found a higher loss of BAF250a expression in the AE versus TE group (23.8% vs. 3%) (p = 0.004) [49].
3.3. Estrogen Receptors and Progesterone Receptors
Since estrogen and progesterone receptors are expressed in endometriotic tissue, the loss of their expression in EAOC may be part of carcinogenesis and indicative of cell dedifferentiation. Ten studies assessed the expression of hormonal receptors in AE, with controversial results [24,27,33,37,39,47,50,51,52,53]. Five showed a significant ER and/or PR loss of expression in AE and EAOC.
A reduction in the expression of hormone receptors from endometriosis to AE has been described by Lenz et al., suggesting their role in diagnosing AE. The authors found a decrease in ER (on average 56%) and PR (less than 1%) expression in atypical ovarian endometriosis compared to lymph node endometriosis and deep infiltrating endometriosis [53].
The analysis conducted by Xiao et al. detected the expression of ER in only 7.7% (2/26) of ovarian CCC and 91.8% (22/24) of papillary serous carcinoma cases, while PR expression was not significantly different between them. Fifty percent of CCC (13/26) showed concomitant AE with a loss of ER and PR expression. In particular, both AE and adjacent CCC had a similar profile, with a loss of ER (84.6% vs. 92.3%) and PR (76.9% vs. 84.6%) expression. The concurrent rate of loss of BAF250a expression, HNF-1b upregulation, and loss of ER expression was not observed in any TE, was increased to 23.1% in AE, and was further increased to 42.3% in CCC [33].
The retrospective study conducted by Lin et al. in 12 patients with CCC showed how the positive ratio of ERb expression gradually reduced from ovarian endometriosis (83.3%) to AE (33.3%) to cancer (0%) with minimal changes of ERa expression during the process. Conversely, the poorest intense expression of steroid receptor RNA activator protein (SRAP) was detected in the cells of endometriosis, gradually increasing in the process of malignant transformation, with the most intense expression in cancer [39].
Concordant with these findings, the study conducted by Andersen et al. on 19 EAOC (5 CCC; 14 EnOC) found decreased ERα and PR protein levels from benign endometriosis to EAOC while ERβ expression increased incrementally from benign endometriosis to EAOC [47].
A case report of a poorly differentiated mucinous carcinoma with signet ring cells and concurrent endometriotic cyst with atypical features showed that the tumor cells were negative for estrogen and progesterone receptors upon immunohistochemistry [50].
On the contrary, as demonstrated by other studies, estrogens appear to be a mitogen for endometriosis, and estrogen-receptor positivity is observed in EnOC. However, CCC does not present estrogen receptor positive expression in tumor tissue. Del Carmen et al. found that 23% of EAOC and 100% of AE tissue blocks, respectively, exhibited positive staining for ER (p < 0.05), while 35% of EAOC and 100% of AE samples showed positive staining for PR (p < 0.05) [24]. A case series evaluating the expression of steroid hormone receptors in the pathological progression from endometriosis to AE to CCC showed a gradual reduction in ERa and PRA expression. In the oncogenesis of EnOC from TE to AE and finally to cancer, a gradual increase in ER alpha was observed [27]. Lai et al. evaluated 79 cases of EAOC (40 CCC; 33 EnOC; four serous carcinomas; one adenosquamous carcinoma; one adenosarcoma). The analysis resulted in positive staining for ER more often in EnOC (30/33, 91%) than in CCC (3/40, 8%) and serous carcinomas (0/4, 0%) supporting the suggestion that estrogen-dependent ovarian cancer arising from endometriosis is more associated with EnOC than CCC. All staining results were similar between AE and contiguous EAOC [37]. Finally, two Romanian studies reported different results concerning hormone receptor expression in AE and EAOC [51,52]. In fact, Păvăleanu et al. showed negative ER immunoexpression in 29.03% cases of endometriotic areas, while PR revealed a negative score in 38.70% of cases. The authors also identified a particular immunoexpression pattern of ER and PR in the stromal cells (32.25% of cases had positive ER immunoreaction, while 35.48% of cases were PR positive). With regards to EAOC, ER immunoexpression had a negative score of 21.05% of cases, while PR immunoexpression revealed a negative score in 47.36% of cases, with a stromal expression for both ER and PR significantly higher in EAOC when compared to endometriosis [51]. Higher values of ER expression in endometriosis associated with high-grade serous ovarian cancer than in TE/AE associated with EnOC were found by Penciu et al. Moreover, higher values of ER expression were also recorded in ovarian cancer than in endometriotic foci [52].
3.4. Transcriptional and Nuclear Factors
Seventeen out of 39 studies [15,17,21,22,23,24,26,27,31,32,33,37,42,45,50,52,53] have investigated the expression of some transcriptional and nuclear factors involved in cancer development, aiming to point out any similarities between AE and ovarian tumors.
Among them, ten studies (six retrospective studies, two case series, one case report, and one comparative study) have analyzed the expression of p53, a tumor suppressor gene. However, the results were not concordant. Lenz et al. [53] found higher and stronger p53 alterations in AE compared to benign ovarian endometriosis. Nezhat et al. observed positive p53 staining in cancers and in benign ovarian endometriosis next to the tumor [23]. Similar results were obtained from the retrospective study of Saìnz de la Cuesta, where more than 50% of cancer and AE had p53 overexpression, with an increasing trend going from benign endometriosis to cancer [26]. The same findings were reported in the case series of Akahane et al., the case report of Jiao et al., and the retrospective study of Ma et al. [27,45,50]. In contrast, Bayramoglu et al. found p53 alterations in neither AE nor in 17 out of 20 cancer tissues analyzed [22]. In another retrospective study, only 13% of cancers stained positive for p53. All staining results were similar between AE and contiguous EAOC [37]. The same results were obtained from Akahane et al. [17] since only 8/26 cancer tissue analyzed had p53 mutations. Moreover, no p53 alterations were found neither in endometriosis nor in AE tissue coexisting with cancer. Penciu et al. [52] observed p53 alterations only in two cases of ovarian serous carcinoma. They did not find the same results in EnOC and corresponding AE. Seven studies analyzed ki-67 which represents an excellent marker to determine the growth fraction of a given cell population, particularly used to assess cancer growth. Akahane, Ogawa, and Yamamoto found a mean Ki67 labeling index increased from endometriosis through AE to cancer [17,21,31], while Del Carmen, Penciu, and Lenz did not observe any significant findings [24,52,53]. Another tumor suppressor protein that has been investigated is p16, a protein that slows cell division by slowing the progression of the cell cycle from the G1 phase to the S phase. Tumor cells were positive for p16 only in the case report of Yurong Jiao [50] and in two cases of ovarian serous cancer in the case series of Penciu [52]. In both studies, AE had a different pathway from cancer, not exhibiting p16 at immunohistochemical analysis. Among the transcription factors, hepatocyte nuclear factor-1 beta (HNF1-B), a protein that binds to specific regions of DNA and regulates the activity of other genes, has been analyzed in 3 out of 39 studies, with concordant HNF-1b expression between AE and EAOC. In particular, 30% of cancer cases showed positive staining for HNF-1 beta, with similar staining results in adjacent AE [37]. In another study, all CCC cases demonstrated strong nuclear immunostaining for HNF-1Beta, while benign endometriotic cysts were negative. 4 cases of AE showed nuclear staining for HNF-1beta in the atypical endometriotic epithelium [15]. In another study, it was found that AE and CCC had a similar profile with HNF-1beta up-regulation (53.8% vs. 92.3%) [33]. Another transcription factor investigated is hypoxia-inducible factors (HIFs), which respond to a decrease in available oxygen in the cellular environment. Kato and colleagues found an increasing trend in HIF immunopositivity from TE (5%) to AE (37%) and then to cancer (95%) [32]. However, HIF expression could differ according to cancer histotype: significant differences in the expression of HIF-1α were evident between the two types of EAOC (CCC and EnOC) and their coexisting AE and non-AE [42].
3.5. Growth Factors and Their Receptors
Among the growth factor receptors, platelet-derived growth factor-A (PDGF) and its receptor-a/b (PDGFR-a/b) showed increased positivity in accordance with higher cytologic atypia in the putative precursors: 71, 47, and 59% in the 17 TE, 84, 73, and 84% in the 19 AE and 97, 97, and 100% in the 31 CCC. Positivity for PDGF-B decreased in accordance with increased atypia in endometriosis coexisting with CCC: 35% in TE, 11% in AE, and 5% in coexisting carcinomas [38]. In addition, the vascular endothelial growth factor (VEGF) stained positively in 94.1% EAOC compared with only 12.5% of the AE [32]. Akahane et al. [35] found an increased Receptor tyrosine-protein kinase 2 expression (c-erbB-2) in CCC and EnOC, first observed in AE, but Saìnz de la Cuesta et al. [34] did not observe any differences in (erbB-2) between cancer and AE because it was never expressed.
3.6. Others
Other molecular markers have been investigated in a solitary or a few studies. The results from these studies can be reviewed in Table 1. Among these, the most frequently assessed was Bcl-2 (B-cell lymphoma 2). It is encoded in humans by the BCL2 gene and is the founding member of the Bcl-2 family of regulator proteins that regulate cell death (apoptosis) by either inhibiting (anti-apoptotic) or inducing (pro-apoptotic) apoptosis. Three out of 39 studies assessed the correlation between Bcl-2 immunohistochemical expression and AE [23,26,51]. Two of them found that a higher Bcl-2 rate in endometriosis had a statistically significant association with more aggressive tumor behavior, starting from TE toward AE and finally cancers (both CCC and EnOC histotypes) [23,51]. On the contrary, Sainz de la Cuesta and coworkers did not find any significant difference in Bcl-2 expression either in EAOC or in AE compared to TE [26].
4. Discussion
Atypical endometriosis has been observed in 12–35% of ovarian endometriosis, and it is estimated that around 60% to 80% of all EAOC occur in the presence of AE, often found in direct continuity with the tumor [55]. Evidence suggests that AE could be a transitioning entity from benign lesions to malignant variants. The pre-malignant, “atypical” lesions, are defined by several histologic criteria, including large nuclei with moderate to marked pleomorphism, increased nuclear-to-cytoplasmic ratio, cellular crowding, stratification, or tufting [55,56]. It has been reported that AE actually refers to two different histologic findings: cellular atypia, also known as cytologic atypia, and architectural atypia, commonly referred to as hyperplasia. The diagnosis of endometriosis with architectural atypia is important because patients with hyperplasia-type endometriosis may be at a higher risk of developing EAOC [49]. This variability in the incidence of the disease may be due to a difficult histological diagnosis, which is still far from being standardized among medical centers worldwide. Moreover, the new conceptualization of the histological pattern, and the differences that emerged in prognostic significance between cytological AE and hyperplastic AE should strongly encourage a revision of this classification in order to better understand which type of AE is actually to define a “high-risk” disease. Reflections can be made on the meaning of a “preneoplastic lesion”: determining whether the mere presence of endometrium at ectopic sites should be considered “per se” a premalignant condition seems crucial and constitutes the conceptual base of any strategy aimed at reducing EAOC mortality. Lesions are defined as “precancerous” based on definite epidemiologic, morphologic, molecular, and biologic criteria that imply the acquisition of genetic, karyotypic, structural, or functional changes in a cluster of cells that differentiate them from the surrounding normal tissue [57]. In other words, premalignant lesions such as AE should reflect an intermediate stage along the pathway leading to cancer. When enough genetic changes have occurred, modifications in appearance and function are observed but not yet associated with typical malignant behavior. In recent years, the literature has focused on the relationship between endometriosis and ovarian cancer. Indeed, sequencing and immunohistochemical studies have revealed that mutations found in endometriosis-associated cancers are found in adjacent endometriosis, supporting the theory of a clonal relationship between benign and malignant counterparts and confirming that the cancers have arisen from the endometriotic lesions probably through an “intermediate” premalignant step. In addition, gene encoding b-catenin (CTNNB1) mutations in 16–53.3%, PTEN mutations in 14–20%, and ARID1A mutations in 30–55% of cases were found in EnOC. PIK3CA mutations in 20–40% and ARID1A mutations in 46–57% of cases are found in ovarian CCC [58].
This systematic review has been conducted with the aim of identifying all biomarkers associated with AE in order to have a “pre-histological” diagnosis of this premalignant entity. Unfortunately, in regards to the results of our systematic review, none of the above discussed biomarkers has such strong evidence that could justify their systematic clinical use in the management of endometriosis and AE. The most frequently detected mutations in AE are ARID1A, genes involved in PI3K pathway (i.e., PIK3CA), genes encoding for ER and PR, KRAS, and PTEN. Interestingly, somatic driven mutations in KRAS, PTEN, PIK3CA and ARID1A have been also observed in more than 26% of cases of deep infiltrating endometriosis lesions, which are associated with virtually no risk of malignant transformation [59]. Therefore, a specific role seems to be played by the ovarian microenvironment in increasing the risk of malignant derailment [60]. Karnezis concurs that the ovarian microenvironment seems to be essential for the malignant transformation of endometriosis because many endometriotic lesions are located outside the ovary, including the pelvic peritoneum, but carcinomas at such sites are rare [61]. Indeed, it was proposed for the endometrioma’s neoplastic transformation as a hypothetical model called the “two-hits” hypothesis [9]. Reactive oxygen species due to free heme and catalytic iron contained in the trapped blood in endometriomas may lead to increased oxidative stress and DNA damage in the epithelial layer of endometriomas. This may result in mutations and epigenetic changes, including mutations in the tumor suppressor gene ARID1A leading to AE. Possible second-hit mutations, as well as activation of the PI3K-AKT-mTOR pathway allow the mutated cell to escape apoptosis caused by increased oxidative stress. The accumulation of oncogenic mutations in AE may ultimately lead to the development of endometriosis-associated ovarian CCC and endometrioid carcinomas. ARID1A loss and activation of PI3K/AKT functionally cooperate in ovarian carcinogenesis and suggest that ARID1A-loss occurs early and that it may be “addicted” to PI3K/AKT oncogenic signaling [9]. In line with this hypothesis and with the reduction of the hormone dependency of CCC, oxidative stress has been shown to act as a physiological regulator of estrogen receptors. Contrary to CCC, EnOC is generally estrogen sensitive and associated with hormonal risk factors. ERa has been shown to represent an independent prognostic marker for EnOC, while nuclear ERa is barely detectable in CCC [62]. Inactivating ARID1A mutations are the most common molecular genetic alteration reported thus far in CCC and EnOC, but a higher frequency of ARID1A mutations has been detected in CCC (46–57%) compared with EnOC (30%). The fact that no differences in clinical behavior were observed comparing BAF250a-positive versus BAF250a-negative cancers may be the basis for supporting the idea of a marker for genomic instability without driving the phenotype: BAF250a appears to be an early event in most of these cases [46,63]. Based on results from the systematic review, there is a remarkable association between BAF250a loss in cases of AE and TE contiguous to BAF250a-deficient EAOC with a higher frequency of inactivating ARID1A mutations detected in CCC compared to EnOC [11,33,34,37,43,44,46,49]. Concordantly with these findings, also PI3K/Akt/mTOR molecular pathway seems to be altered in AE and in EAOC in all of the studies included, with a similar pattern between the two diseases [25,28,31,32,34,37,40,42,43,45,48,50]. Since ovarian cancer is considered a hormone-responsive cancer, its correlation to PR and ER immunoexpression has a major importance in clinic-pathological manifestations of ovarian carcinoma, including those associated with endometriosis [64,65]. Actions of estradiol are mediated by two isoforms of ERs (ERa and ERb) that differ in their tissue distributions, their ligand-binding specificity, and affinity: ERa has been shown to represent an independent prognostic marker for EnOC, while nuclear ERa was poorly detectable in CCC [62,66]. Since progesterone is modulated by the expression of both isoforms of the specific receptor (PR-A and PR-B), it is involved in the pathogenesis of endometriosis and EAOC [65]. Thus, from the results of the systematic review, it seems that alteration of steroid receptor immune expression is correlated to ovarian endometriosis and endometriosis-related carcinogenesis in a hormone-dependent manner with regards to EnOC and in a hormone-independent way concerning CCC.
Associated AE lesions seem to have the same biological expression as their adjacent Cancer histotypes [15,67,68,69,70,71,72,73,74,75]. Moreover, ER and PR expression seems to be higher in AE as compared to EAOC, and lower when compared to endometriosis. The gradual loss of ER and PR expression from endometriosis to EAOC carcinogenesis suggests that hormone receptor staining may be proposed as a marker for premalignant or malignant lesions in endometriosis. A reduced HNF 1-beta expression in AE as compared to EAOC, and in particular to CCC, and a higher HNF-1 beta expression in AE as compared to TE has also been reported in our systematic review [15,33,37]. The main limit to the use of these molecular markers proposed for the early detection of endometriosis-preneoplastic lesions is that their clinical application may be difficult since they all need expensive molecular analyses. Moreover, strong evidence supporting their systematic use in clinical practice is still lacking. The presence of a serum non-invasive marker for the presence of AE could be more effective and easy to use. Inflammatory parameters, such as the neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR), have been found altered in the peripheral blood in patients with endometriosis, thus suggesting that systemic perturbations may contribute to the pathogenetic process of the disease [76]. NLR and PLR have also gained more and more space in the diagnostic and prognostic management of ovarian carcinoma [77]. Indeed, systemic inflammation contributes to cancer initiation and progression by promoting cell proliferation, angiogenesis, and gene repair [78]. To the best of our knowledge, there are no studies in the literature evaluating the possible role of NLR and PLR in predicting AE and its risk of malignant transformation. This is even more important if we think that, according to the literature, women with endometriosis had a tripled and doubled risk for CCC and EnOC subtypes, and a more frequent localized form of the disease when cancer arises in endometriosis [79]. Even if cancer arising in endometriosis seems to be characterized by a better prognosis, the early detection of preneoplastic lesions could really impact the quality of life of women with endometriosis. Our study has some limitations: (1) The non-homogeneous definition of AE in the studies included in the systematic review; (2) Heterogeneity between studies (i.e., study design) included in the systematic review; and (3) Low number of studies included in the systematic review. These limitations suggest that the results should be interpreted with caution until validated by future research projects providing more detailed, well-designed, and standardized data collection.
5. Conclusions
Atypical endometriosis can be a transitioning entity from endometriosis to endometriosis-associated ovarian cancers. In our systematic review, we found 39 studies assessing numerous molecular targets of AE, such as immunohistochemical expression of BAF250, PIK3CA, PTEN, HNF-1beta, ER, and PR. Unfortunately, these molecular biomarkers of AE require expensive molecular analysis, histological examination is always needed, and none of them has such strong evidence to justify their systematic use in the management of the neoplastic risk of endometriosis. Further studies are needed to validate evidence on available biomarkers for the presence of AE, which is a high oncologic risk condition. Moreover, the introduction of novel serum biomarkers could be useful for the non-invasive diagnosis of AE.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms23084425/s1.
Author Contributions
Conceptualization, L.B., M.S. and R.V.; Methodology, G.M. and N.S.; Software, N.S.; Validation, S.F., M.C. and G.M.; Formal Analysis, N.S.; Investigation, R.V., M.S., L.B., C.D. and N.S.; Resources, R.V., M.S., L.B., C.D. and N.S.; Data Curation, N.S., J.O. and C.D.; Writing—Original Draft Preparation, L.B., M.S., R.V., N.S., C.D. and I.T.; Writing—Review & Editing, S.F., J.O. and G.M.; Visualization, M.C., S.F., J.O., I.T. and G.M.; Supervision, M.C., S.F. and G.M.; Project Administration, M.C., S.F. and G.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (Comitato Etico Ospedale San Raffaele; No. 01END, approved 12 April 2012).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Parazzini F., Esposito G., Tozzi L., Noli S., Bianchi S. Epidemiology of endometriosis and its comorbidities. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017;209:3–7. doi: 10.1016/j.ejogrb.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 2.Sampson J.A. Endometrial carcinoma of the ovary, arising in endometrial tissue in that organ. Arch. Surg. 1925;10:1–72. doi: 10.1001/archsurg.1925.01120100007001. [DOI] [Google Scholar]
- 3.Scott R.B. Malignant changes in endometriosis. Obstet. Gynecol. 1953;2:283–289. [PubMed] [Google Scholar]
- 4.Matias-Guiu X., Stewart C.J. Endometriosis-associated ovarian neoplasia. Pathology. 2018;50:190–204. doi: 10.1016/j.pathol.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 5.Pearce C.L., Templeman C., Rossing M.A., Lee A., Near A.M., Webb P.M., Nagle C.M., A Doherty J., Cushing-Haugen K.L., Wicklund K.G., et al. Association between endometriosis and risk of histological subtypes of ovarian cancer: A pooled analysis of case–control studies. Lancet Oncol. 2012;13:385–394. doi: 10.1016/S1470-2045(11)70404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anglesio M.S., Yong P. Endometriosis-associated Ovarian Cancers. Clin. Obstet. Gynecol. 2017;60:711–727. doi: 10.1097/GRF.0000000000000320. [DOI] [PubMed] [Google Scholar]
- 7.Wilbur M.A., Shih I.-M., Segars J.H., Fader A.N. Cancer Implications for Patients with Endometriosis. Semin. Reprod. Med. 2017;35:110–116. doi: 10.1055/s-0036-1597120. [DOI] [PubMed] [Google Scholar]
- 8.Mikami Y. Endometriosis-related ovarian neoplasms: Pathogenesis and histopathologic features. Diagn. Histopathol. 2014;20:357–363. doi: 10.1016/j.mpdhp.2014.07.002. [DOI] [Google Scholar]
- 9.Králíčková M., Laganà A.S., Ghezzi F., Vetvicka V. Endometriosis and risk of ovarian cancer: What do we know? Arch. Gynecol. Obstet. 2020;301:1–10. doi: 10.1007/s00404-019-05358-8. [DOI] [PubMed] [Google Scholar]
- 10.Vetvicka V., Fiala L., Garzon S., Buzzaccarini G., Terzic M., Laganà A.S. Endometriosis and gynaecological cancers: Molecular insights behind a complex machinery. Prz. Menopauzalny. 2021;20:201–206. doi: 10.5114/pm.2021.111276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiegand K.C., Shah S.P., Al-Agha O.M., Zhao Y., Tse K., Zeng T., Senz J., McConechy M.K., Anglesio M.S., Kalloger S.E., et al. ARID1AMutations in Endometriosis-Associated Ovarian Carcinomas. N. Engl. J. Med. 2010;363:1532–1543. doi: 10.1056/NEJMoa1008433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wiegand K.C., Lee A., Al-Agha O.M., Chow C., E Kalloger S., Scott D.W., Steidl C., Wiseman S.M., Gascoyne R.D., Gilks B., et al. Loss of BAF250a (ARID1A) is frequent in high-grade endometrial carcinomas. J. Pathol. 2011;224:328–333. doi: 10.1002/path.2911. [DOI] [PubMed] [Google Scholar]
- 13.Sato N., Tsunoda H., Nishida M., Morishita Y., Takimoto Y., Kubo T., Noguchi M. Loss of het- erozygosity on 10q23.3 and mutation of the tumor suppressor gene PTEN in benign endo- metrial cyst of the ovary: Possible sequence progression from benign endometrial cyst to endometrioid carcinoma and clear cell carcinoma of the ovary. Cancer Res. 2000;60:7052–7056. [PubMed] [Google Scholar]
- 14.Yamamoto S., Tsuda H., Takano M., Iwaya K., Tamai S., Matsubara O. PIK3CA mutation is an early event in the development of endometriosis-associated ovarian clear cell adenocarcinoma. J. Pathol. 2011;225:189–194. doi: 10.1002/path.2940. [DOI] [PubMed] [Google Scholar]
- 15.Kato N., Sasou S.-I., Motoyama T. Expression of hepatocyte nuclear factor-1beta (HNF-1beta) in clear cell tumors and endometriosis of the ovary. Mod. Pathol. 2005;19:83–89. doi: 10.1038/modpathol.3800492. [DOI] [PubMed] [Google Scholar]
- 16.Fujimura M., Hidaka T., Kataoka K., Yamakawa Y., Akada S., Teranishi A., Saito S. Absence of Estrogen Receptor-α Expression in Human Ovarian Clear Cell Adenocarcinoma Compared with Ovarian Serous, Endometrioid, and Mucinous Adenocarcinoma. Am. J. Surg. Pathol. 2001;25:667–672. doi: 10.1097/00000478-200105000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Akahane T., Sekizawa A., Purwosunu Y., Nagatsuka M., Okai T. The Role of p53 Mutation in the Carcinomas Arising from Endometriosis. Int. J. Gynecol. Pathol. 2007;26:345–351. doi: 10.1097/pgp.0b013e31802b41a8. [DOI] [PubMed] [Google Scholar]
- 18.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021;372:71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.EFSA Scientific Committee. Benford D., Halldorsson T., Jeger M.J., Knutsen H.K., More S., Naegeli H., Noteborn H., Ockleford C., Ricci A., et al. The principles and methods behind EFSA’s Guidance on Uncertainty Analysis in Scientific Assessment. EFSA J. 2018;16:e05122. doi: 10.2903/j.efsa.2018.5122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chalas E., ChumasS J., Barbieri R., Mann W.J. Nucleolar organizer regions in endometriosis, atypical endometriosis, and clear cell and endometrioid carcinomas. Gynecol. Oncol. 1990;40:260–263. doi: 10.1016/0090-8258(90)90288-V. [DOI] [PubMed] [Google Scholar]
- 21.Ogawa S., Kaku T., Amada S., Kobayashi H., Hirakawa T., Ariyoshi K., Kamura T., Nakano H. Ovarian Endometriosis Associated with Ovarian Carcinoma: A Clinicopathological and Immunohistochemical Study. Gynecol. Oncol. 2000;77:298–304. doi: 10.1006/gyno.2000.5765. [DOI] [PubMed] [Google Scholar]
- 22.Bayramođlu H., Duzcan E. Atypical epithelial changes and mutant p53 gene expression in ovarian endometriosis. Pathol. Oncol. Res. 2001;7:33–38. doi: 10.1007/BF03032602. [DOI] [PubMed] [Google Scholar]
- 23.Nezhat F., Cohen C., Rahaman J., Gretz H., Cole P., Kalir T. Comparative immunohistochemical studies ofbcl-2 and p53 proteins in benign and malignant ovarian endometriotic cysts. Cancer. 2002;94:2935–2940. doi: 10.1002/cncr.10566. [DOI] [PubMed] [Google Scholar]
- 24.Del Carmen M.G., Sehdev A.E.S., Fader A.N., Zahurak M.L., Richardson M., Fruehauf J.P., Montz F.J., Bristow R.E. Endometriosis-associated ovarian carcinoma: Differential expression of vascular endothelial growth factor and estrogen/progesterone receptors. Cancer. 2003;98:1658–1663. doi: 10.1002/cncr.11714. [DOI] [PubMed] [Google Scholar]
- 25.Amemiya S., Sekizawa A., Otsuka J., Tachikawa T., Saito H., Okai T. Malignant transformation of endometriosis and genetic alterations of K-ras and microsatellite instability. Int. J. Gynecol. Obstet. 2004;86:371–376. doi: 10.1016/j.ijgo.2004.04.036. [DOI] [PubMed] [Google Scholar]
- 26.de la Cuesta R.S., Izquierdo M., Cañamero M., Granizo J.J., Manzarbeitia F. Increased prevalence of p53 overexpression from typical endometriosis to atypical endometriosis and ovarian cancer associated with endometriosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2004;113:87–93. doi: 10.1016/S0301-2115(03)00367-1. [DOI] [PubMed] [Google Scholar]
- 27.Akahane T., Sekizawa A., Okuda T., Kushima M., Saito H., Okai T. Disappearance of Steroid Hormone Dependency During Malignant Transformation of Ovarian Clear Cell Cancer. Int. J. Gynecol. Pathol. 2005;24:369–376. doi: 10.1097/01.pgp.0000165173.90339.a2. [DOI] [PubMed] [Google Scholar]
- 28.Ali-Fehmi R., Khalifeh I., Bandyopadhyay S., Lawrence W.D., Silva E., Liao D., Sarkar F.H., Munkarah A.R. Patterns of Loss of Heterozygosity at 10q23.3 and Microsatellite Instability in Endometriosis, Atypical Endometriosis, and Ovarian Carcinoma Arising in Association with Endometriosis. Int. J. Gynecol. Pathol. 2006;25:223–229. doi: 10.1097/01.pgp.0000192274.44061.36. [DOI] [PubMed] [Google Scholar]
- 29.Finas D., Huszar M., Agic A., Dogan S., Kiefel H., Riedle S., Gast D., Marcovich R., Noack F., Altevogt P., et al. L1 cell adhesion molecule (L1CAM) as a pathogenetic factor in endometriosis. Hum. Reprod. 2008;23:1053–1062. doi: 10.1093/humrep/den044. [DOI] [PubMed] [Google Scholar]
- 30.Yamamoto S., Tsuda H., Takano M., Kita T., Kudoh K., Furuya K., Tamai S., Matsubara O. Expression of platelet-derived growth factors and their receptors in ovarian clear-cell carcinoma and its putative precursors. Mod. Pathol. 2007;21:115–124. doi: 10.1038/modpathol.3800984. [DOI] [PubMed] [Google Scholar]
- 31.Yamamoto S., Tsuda H., Miyai K., Takano M., Tamai S., Matsubara O. Cumulative alterations of p27Kip1-related cell-cycle regulators in the development of endometriosis-associated ovarian clear cell adenocarcinoma. Histopathology. 2010;56:740–749. doi: 10.1111/j.1365-2559.2010.03551.x. [DOI] [PubMed] [Google Scholar]
- 32.Kato M., Yamamoto S., Takano M., Matsubara O., Furuya K. Aberrant Expression of the Mammalian Target of Rapamycin, Hypoxia-inducible Factor-1α, and Glucose Transporter 1 in the Development of Ovarian Clear-cell Adenocarcinoma. Int. J. Gynecol. Pathol. 2012;31:254–263. doi: 10.1097/PGP.0b013e318237d66c. [DOI] [PubMed] [Google Scholar]
- 33.Xiao W., Awadallah A., Xin W. Loss of ARID1A/BAF250a expression in ovarian endometriosis and clear cell carcinoma. Int. J. Clin. Exp. Pathol. 2012;5:642–650. [PMC free article] [PubMed] [Google Scholar]
- 34.Yamamoto S., Tsuda H., Takano M., Tamai S., Matsubara O. Loss of ARID1A protein expression occurs as an early event in ovarian clear-cell carcinoma development and frequently coexists with PIK3CA mutations. Mod. Pathol. 2011;25:615–624. doi: 10.1038/modpathol.2011.189. [DOI] [PubMed] [Google Scholar]
- 35.Yamamoto S., Tsuda H., Miyai K., Takano M., Tamai S., Matsubara O. Accumulative copy number increase of MET drives tumor development and histological progression in a subset of ovarian clear-cell adenocarcinomas. Mod. Pathol. 2011;25:122–130. doi: 10.1038/modpathol.2011.143. [DOI] [PubMed] [Google Scholar]
- 36.Yamamoto S., Tsuda H., Honda K., Takano M., Tamai S., Imoto I., Inazawa J., Yamada T., Matsubara O. ACTN4 gene amplification and actinin-4 protein overexpression drive tumour development and histological progression in a high-grade subset of ovarian clear-cell adenocarcinomas. Histopathology. 2012;60:1073–1083. doi: 10.1111/j.1365-2559.2011.04163.x. [DOI] [PubMed] [Google Scholar]
- 37.Lai C.-R., Hsu C.-Y., Chen Y.-J., Yen M.-S., Chao K.-C., Li A.F.-Y. Ovarian cancers arising from endometriosis: A microenvironmental biomarker study including ER, HNF1ß, p53, PTEN, BAF250a, and COX-2. J. Chin. Med. Assoc. 2013;76:629–634. doi: 10.1016/j.jcma.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 38.Vercellini P., Cribiù F.M., Del Gobbo A., Carcangiu M.L., Somigliana E., Bòsari S. The oncofetal protein IMP3: A novel biomarker and triage tool for premalignant atypical endometriotic lesions. Fertil. Steril. 2013;99:1974–1979. doi: 10.1016/j.fertnstert.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 39.Lin K., Zhan H., Ma J., Xu K., Wu R., Zhou C., Lin J. Increased steroid receptor RNA activator protein (SRAP) accompanied by decreased estrogen receptor-beta (ER-β) levels during the malignant transformation of endometriosis associated ovarian clear cell carcinoma. Acta Histochem. 2014;116:878–882. doi: 10.1016/j.acthis.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 40.Suryawanshi S., Huang X., Elishaev E., Budiu R.A., Zhang L., Kim S., Donnellan N., Mantia-Smaldone G., Ma T., Tseng G., et al. Complement Pathway Is Frequently Altered in Endometriosis and Endometriosis-Associated Ovarian Cancer. Clin. Cancer Res. 2014;20:6163–6174. doi: 10.1158/1078-0432.CCR-14-1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Anglesio M.S., Bashashati A., Wang Y.K., Senz J., Ha G., Yang W., Aniba M.R., Prentice L.M., Farahani H., Chang H.L., et al. Multifocal endometriotic lesions associated with cancer are clonal and carry a high mutation burden. J. Pathol. 2015;236:201–209. doi: 10.1002/path.4516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matsumoto T., Yamazaki M., Takahashi H., Kajita S., Suzuki E., Tsuruta T., Saegusa M. Distinct β-Catenin and PIK3CA Mutation Profiles in Endometriosis-Associated Ovarian Endometrioid and Clear Cell Carcinomas. Am. J. Clin. Pathol. 2015;144:452–463. doi: 10.1309/AJCPZ5T2POOFMQVN. [DOI] [PubMed] [Google Scholar]
- 43.Er T.-K., Su Y.-F., Wu C.-C., Chen C.-C., Wang J., Hsieh T.-H., Herreros-Villanueva M., Chen W.-T., Chen Y.-T., Liu T.-C., et al. Targeted next-generation sequencing for molecular diagnosis of endometriosis-associated ovarian cancer. J. Mol. Med. 2016;94:835–847. doi: 10.1007/s00109-016-1395-2. [DOI] [PubMed] [Google Scholar]
- 44.Kato M., Takano M., Miyamoto M., Sasaki N., Goto T., Suzuki A., Hirata J., Sasa H., Tsuda H., Furuya K. Effect of ARID1A/BAF250a expression on carcinogenesis and clinicopathological factors in pure-type clear cell adenocarcinoma of the ovary. Mol. Clin. Oncol. 2016;5:395–401. doi: 10.3892/mco.2016.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ma X., Hui Y., Lin L., Wu Y., Zhang X., Qin X. Possible relevance of tumor-related genes mutation to malignant transformation of endometriosis. Eur. J. Gynaecol. Oncol. 2016;37:89–94. [PubMed] [Google Scholar]
- 46.Stamp J.P., Gilks C.B., Wesseling M., Eshragh S., Ceballos K., Anglesio M.S., Kwon J.S., Tone A., Huntsman D.G., Carey M.S. BAF250a Expression in Atypical Endometriosis and Endometriosis-Associated Ovarian Cancer. Int. J. Gynecol. Cancer. 2016;26:825–832. doi: 10.1097/IGC.0000000000000698. [DOI] [PubMed] [Google Scholar]
- 47.Andersen C.L., Boisen M.M., Sikora M.J., Ma T., Tseng G., Suryawanshi S., Vlad A., Elishaev E., Edwards R.P., Oesterreich S. The Evolution of Estrogen Receptor Signaling in the Progression of Endometriosis to Endometriosis-Associated Ovarian Cancer. Horm. Cancer. 2018;9:399–407. doi: 10.1007/s12672-018-0350-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhang C., Wang X., Anaya Y., Parodi L., Cheng L., Anderson M.L., Hawkins S.M. Distinct molecular pathways in ovarian endometrioid adenocarcinoma with concurrent endometriosis. Int. J. Cancer. 2018;143:2505–2515. doi: 10.1002/ijc.31768. [DOI] [PubMed] [Google Scholar]
- 49.Sevilla I., Linde F.M., Sánchez M.D.P.M., Arense J.J., Torroba A., Díaz A.N., Ferrer M.L.S. Prognostic importance of atypical endometriosis with architectural hyperplasia versus cytologic atypia in endometriosis-associated ovarian cancer. J. Gynecol. Oncol. 2019;30:e63. doi: 10.3802/jgo.2019.30.e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jiao Y., Lu B. Poorly differentiated mucinous carcinoma with signet ring cells in an ovarian endometriotic cyst: A case report. Diagn. Pathol. 2019;14:73. doi: 10.1186/s13000-019-0850-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Păvăleanu I., Lozneanu L., Balan R.A., Giuşcă S.E., Avădănei E.-R., Căruntu I.-D., Amălinei C. Insights into molecular pathways of endometriosis and endometriosis-related ovarian carcinoma. Rom. J. Morphol. Embryol. 2021;61:739–749. doi: 10.47162/RJME.61.3.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Penciu R.-C., Postolache I., Steriu L., Izvoranu S., Tica A.-A., Mocanu I.-D., Sârbu V., Deacu M., Tica I., Bălţătescu G.-I., et al. Is there a relationship in-between ovarian endometriosis and ovarian cancer? Immunohistochemical profile of four cases with coexisting ovarian endometriosis and cancer. Rom. J. Morphol. Embryol. 2020;61:157–165. doi: 10.47162/RJME.61.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lenz J., Chvatal R., Fiala L., Konecna P., Lenz D. Comparative immunohistochemical study of deep infiltrating endometriosis, lymph node endometriosis and atypical ovarian endometriosis including description of a perineural invasion. Biomed. Pap. Med. Fac. Univ. Palacky Olomouc. Czech Repub. 2021;165:69–79. doi: 10.5507/bp.2020.006. [DOI] [PubMed] [Google Scholar]
- 54.Shin H.Y., Yang W., Chay D.B., Lee E.J., Chung J.Y., Kim H.S., Kim J.H. Tetraspanin 1 promotes endometriosis leading to ovarian clear cell carcinoma. Mol. Oncol. 2020;15:987–1004. doi: 10.1002/1878-0261.12884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Varma R., Rollason T., Gupta J.K., Maher E.R. Endometriosis and the neoplastic process. Reproduction. 2004;127:293–304. doi: 10.1530/rep.1.00020. [DOI] [PubMed] [Google Scholar]
- 56.Fukunaga M., Nomura K., Ishikawa E., Ushigome S. Ovarian atypical endometriosis: Its close association with malignant epithelial tumours. Histopathology. 1997;30:249–255. doi: 10.1046/j.1365-2559.1997.d01-592.x. [DOI] [PubMed] [Google Scholar]
- 57.Berman J.J., Albores-Saavedra J., Bostwick D., DeLellis R., Eble J., Hamilton S.R., Hruban R.H., Mutter G.L., Page D., Rohan T., et al. Precancer: A conceptual working definition: Results of a Consensus Conference. Cancer Detect. Prev. 2006;30:387–394. doi: 10.1016/j.cdp.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 58.Mikhaleva L.M., Davydov A., Patsap O.I., Mikhaylenko E.V., Nikolenko V., Neganova M.E., Klochkov S., Somasundaram S., Kirkland C.E., Aliev G. Malignant Transformation and Associated Biomarkers of Ovarian Endometriosis: A Narrative Review. Adv. Ther. 2020;37:2580–2603. doi: 10.1007/s12325-020-01363-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Anglesio M.S., Papadopoulos N., Ayhan A., Nazeran T.M., Noë M., Horlings H.M., Lum A., Jones S., Senz J., Seckin T., et al. Cancer-Associated Mutations in Endometriosis without Cancer. N. Engl. J. Med. 2017;376:1835–1848. doi: 10.1056/NEJMoa1614814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cochrane D.R., Tessier-Cloutier B., Lawrence K.M., Nazeran T., Karnezis A.N., Salamanca C., Cheng A.S., McAlpine J.N., Hoang L.N., Gilks C.B., et al. Clear cell and endometrioid carcinomas: Are their differences attributable to distinct cells of 772 origin? J. Pathol. 2017;243:26–36. doi: 10.1002/path.4934. [DOI] [PubMed] [Google Scholar]
- 61.Karnezis A.N., Cho K., Gilks C.B., Pearce C.L., Huntsman D.G. The disparate origins of ovarian cancers: Pathogenesis and prevention strategies. Nat. Cancer. 2016;17:65–74. doi: 10.1038/nrc.2016.113. [DOI] [PubMed] [Google Scholar]
- 62.Sieh W., Köbel M., A Longacre T., Bowtell D.D., Defazio A., Goodman M.T., Høgdall E., Deen S., Wentzensen N., Moysich K.B., et al. Hormone-receptor expression and ovarian cancer survival: An Ovarian Tumor Tissue Analysis consortium study. Lancet Oncol. 2013;14:853–862. doi: 10.1016/S1470-2045(13)70253-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lowery W.J., Schildkraut J.M., Akushevich L., Bentley R., Marks J.R., Huntsman D., Berchuck A. Loss of ARID1A-Associated Protein Expression is a Frequent Event in Clear Cell and Endometrioid Ovarian Cancers. Int. J. Gynecol. Cancer. 2012;22:9–14. doi: 10.1097/IGC.0b013e318231f140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tkalia I.G., I Vorobyova L., Svintsitsky V.S., Nespryadko S.V., Goncharuk I.V., Lukyanova N.Y., Chekhun V.F. Clinical significance of hormonal receptor status of malignant ovarian tumors. Exp. Oncol. 2014;36:125–133. [PubMed] [Google Scholar]
- 65.Chen S., Dai X., Gao Y., Shen F., Ding J., Chen Q. The positivity of estrogen receptor and progesterone receptor may not be associated with metastasis and recurrence in epithelial ovarian cancer. Sci. Rep. 2017;7:16922. doi: 10.1038/s41598-017-17265-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chan K.K.L., Siu M.K.Y., Jiang Y.X., Wang J.J., Wang Y., Leung T.H.Y., Liu S.S., Cheung A.N.Y., Ngan H.Y.S. Differential expression of estrogen receptor subtypes and variants in ovarian cancer: Effects on cell invasion, proliferation and prognosis. BMC Cancer. 2017;17:606. doi: 10.1186/s12885-017-3601-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jiang X., Morland S.J., Hitchcock A., Thomas E.J., Campbell I.G. Allelo- typing of endometriosis with adjacent ovarian carcinoma reveals evidence of a common lineage. Cancer Res. 1998;58:1707–1712. [PubMed] [Google Scholar]
- 68.Guan B., Rahmanto Y.S., Wu R.-C., Wang Y., Wang Z., Wang T.-L., Shih I.-M. Roles of Deletion of Arid1a, a Tumor Suppressor, in Mouse Ovarian Tumorigenesis. JNCI J. Natl. Cancer Inst. 2014;106:dju146. doi: 10.1093/jnci/dju146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ghai V., Jan H., Shakir F., Haines P., Kent A. Diagnostic delay for superficial and deep endometriosis in the United Kingdom. J. Obstet. Gynaecol. 2020;40:83–89. doi: 10.1080/01443615.2019.1603217. [DOI] [PubMed] [Google Scholar]
- 70.Hudson Q.J., Ashjaei K., Perricos A., Kuessel L., Husslein H., Wenzl R., Yotova I. Endometriosis Patients Show an Increased M2 Response in the Peritoneal CD14+low/CD68+low Macrophage Subpopulation Coupled with an Increase in the T-helper 2 and T-regulatory Cells. Reprod. Sci. 2020;27:1920–1931. doi: 10.1007/s43032-020-00211-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Seckin B., Ates M.C., Kirbas A., Yesilyurt H. Usefulness of hematological parameters for differential diagnosis of endometriomas in adolescents/young adults and older women. Int. J. Adolesc. Med. Health. 2018;33 doi: 10.1515/ijamh-2018-0078. [DOI] [PubMed] [Google Scholar]
- 72.Králíčková M., Vetvicka V., Fiala L., Laganà A.S., Garzon S. The Search for Biomarkers in Endometriosis: A Long and Windy Road. Reprod. Sci. 2021:1–7. doi: 10.1007/s43032-021-00668-2. [DOI] [PubMed] [Google Scholar]
- 73.Vanhie A., Dorien O., Peterse D., Beckers A., Cuéllar A., Fassbender A., Meuleman C., Mestdagh P., D’Hooghe T. Plasma miRNAs as biomarkers for endometriosis. Hum. Reprod. 2019;34:1650–1660. doi: 10.1093/humrep/dez116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.ETIC Endometriosis Treatment Italian Club. Alio L., Angioni S., Arena S., Bartiromo L., Bergamini V., Berlanda N., Bonin C., Busacca M., Candiani M., et al. When more is not better: 10 ’don’ts’ in endometriosis management. An ETIC* position statement. Hum. Reprod. Open. 2019;2019:hoz009. doi: 10.1093/hropen/hoz009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jing X., Li C., Sun J., Peng J., Dou Y., Xu X., Ma C., Dong Z., Liu Y., Zhang H., et al. Systemic Inflammatory Response Markers Associated with Infertility and Endometrioma or Uterine Leiomyoma in Endometriosis. Ther. Clin. Risk Manag. 2020;16:403–412. doi: 10.2147/TCRM.S232849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ottolina J., Bartiromo L., Dolci C., Salmeri N., Schimberni M., Villanacci R., Viganò P., Candiani M. Assessment of Coagulation Parameters in Women Affected by Endometriosis: Validation Study and Systematic Review of the Literature. Diagnostics. 2020;10:567. doi: 10.3390/diagnostics10080567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhao Z., Zhao X., Lu J., Xue J., Liu P., Mao H. Prognostic roles of neutrophil to lymphocyte ratio and platelet to lymphocyte ratio in ovarian cancer: A meta-analysis of retrospective studies. Arch. Gynecol. Obstet. 2018;297:849–857. doi: 10.1007/s00404-018-4678-8. [DOI] [PubMed] [Google Scholar]
- 78.Hainaut P., Plymoth A. Targeting the hallmarks of can-cer: Towards a rational approach to next-generation cancer therapy. Curr Opin Oncol. 2013;25:50–51. doi: 10.1097/CCO.0b013e32835b651e. [DOI] [PubMed] [Google Scholar]
- 79.Kim H.S., Kim T.H., Chung H.H., Song Y.S. Risk and prognosis of ovarian cancer in women with endometriosis: A meta-analysis. Br. J. Cancer. 2014;110:1878–1890. doi: 10.1038/bjc.2014.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author.