Abstract
People in need of care, chronic or acute, often present problematic food intake and special nutritional needs. Integrated, person-centred and pro-active food and nutritional care delivery has been proven effective for people in health care. However, skills mismatches have been reported in different professions involved, which also applies to the role of chefs in healthcare. The EU funded project NECTAR aims at closing this gap by creating a new job profile, called Chef Gastro-Engineering (CGE). The current publication summarizes the status quo in hospitals and gives a perspective on the future role of chefs in integrated healthcare delivery.
Keywords: integrated health care systems, chef, vocational education and training (VET), interprofessional, food, nutrition, malnutrition
Context and aim
Change of appetite, decreased food intake, unintended weight loss and psychological stress are all considered independent risk factors as well as symptoms of malnutrition [1]. If not managed adequately, malnutrition leads to multiple negative health outcomes and a significant economic burden [2,3,4]. According to a recent meta-analysis [5], the prevalence of malnutrition is higher in hospitals (28%) than residential care (18%) and community setting (8,5%). Although it represents a common condition, malnutrition may remain unrecognized for a long period of time. Especially hospitalized elderly patients are not always concerned about decreased food intake or fully realize their nutritional status and loss of body weight [6]. Moreover, reduced food intake during hospitalization is associated with variables related to both patients’ condition (e.g. clinical, physical) and factors related to the quality of hospital food itself [7].
The present paper reflects the role of chefs in the integrated food and nutrition care team in hospitals. Special attention is drawn on political frameworks underlining new perspectives and needs in the field of healthcare provision and the education of professionals involved in the care pathway. Therefore, this paper highlights an innovative approach to food and nutrition care provision including a new professional profile of chefs in healthcare.
Current situation of interprofessional nutrition care in hospitals
Delivering adequate nutritional care for a large group of people characterized by complex care needs requires audited standards, education and training for smooth communication between care professions, but also coordination and integration between different stakeholders working in an institution and outside. This is based on dimensions that reflect the culinary (primary food care) and the mixed culinary-clinical (collaboration primary food care/secondary nutritional care) of interventions [8]. Currently, effective food and nutritional care in hospitals includes nurses screening patients on admission, monitoring them and ensuring food intake, dieticians or registered nurses, depending on the care setting, assessing nutritional needs and communicating individual goals to medical doctors. However, there are still gaps in the care pathway like lack of nursing time, knowledge of balanced diets and constituent food groups, inadequate communication, trust, quality of food and beverages, and respect within care teams [9]. Additionally, the personal tastiness of meals and eating and chewing abilities are often neglected, stretching the importance of the chef in a care team. This opens a bigger picture of effective food and nutrition care delivery in health care, chefs becoming a potential part of an integrated food and nutrition care delivery model [10].
This horizontal integration between professionals and care sections of institutions allows person-centred and proactive care delivery especially for those most vulnerable, who are in need for tailored food and nutrition care approaches. Although modern European society has created many services to support vulnerable populations [11], these services are divided into organizational clusters, managed, and delivered in an uncoordinated and isolated manner without considering the chef’s perspective.
European educational frameworks and political strategies fostering the integrated care model
The World Health Organization recently published two strategies promoting interprofessional care approach where health workers work together across organizational boundaries [12,13]. Interprofessional teamwork differs from the multidisciplinary approach, aligning and integrating skills of different professions on a shared competence base, making all members of the team equally important for success of care provision [14]. This improves care for an ageing population [15,16] and addresses specific food needs of persons and/or malnutrition [17]. However, this requires adequately trained staff and clear skills distribution of care professions to assure successful collaboration and favourable outcomes.
Although the European Skills, Competences, Qualifications and Occupations inventory describes occupational profiles, skills, competencies and qualifications of nutritional healthcare workers [18,19,20,21,22], the healthcare workers report shows a high rate of skills mismatches because of increased demand of more complex and changing working environments due to reforms of healthcare systems toward more integrated and personalised care [23]. This also includes the role of chefs in healthcare and may be observed in all EU member states (MSs). Chefs in healthcare should be considered as part of an integrated food and nutritional care team as they address food preferences, organoleptic food qualities, alter recipes and menus and encourage food consumption and calorie intake [24,25].
Standardization of health workers’ professional profiles, adaption of professionals’ training and alignment of professional inputs along persons’ journeys through healthcare systems are needed to address the interprofessional care delivery demanded in those policy documents.
Throughout Europe, tools allow quality cross-national control of Vocational Education and Training (VET), support national MS in implementing health workforce training on national level [26] and are the strategic framework for European cooperation in education and training [27]. EU frameworks like the European Quality Framework (EQF) or the European Quality Assurance in Vocational Education and Training [28,29] build the ground to go beyond the current service delivery and allow future developments in health workforce development.
Integrated food and nutrition care in institutions
Integration of healthcare improves patient experiences and serves better outcomes of care delivery and effective healthcare systems [30,31]. One challenge is the highly context-sensitivity and the myriad among care providers, that integrated care is a “processual concept” only, rather than a consistent and designated model [31,32,33].
To overcome these barriers, Valentijn et al. have developed a comprehensive conceptual framework for integrated care. Figure 1 visualises this model, high-lightening the future role of chefs in integrated food and nutritional care team [34]. In practice, integrated care ideally permeates the clinical level, which puts focus on the person on a micro level, up to the professional level that enables coordination of services among different care professions [35]. For a horizontal integration of chefs, clear definitions of roles, responsibilities and principles are needed. Organizational integration facilitates integration of chefs in healthcare systems through inter-organizational relationships (e.g. educational institutions, workplaces, cooperation). System integration, on macro level, defines structures, policies, and governance of different care institutions (e.g. access to healthcare system, financial status of countries, legal structure).
Figure 1.
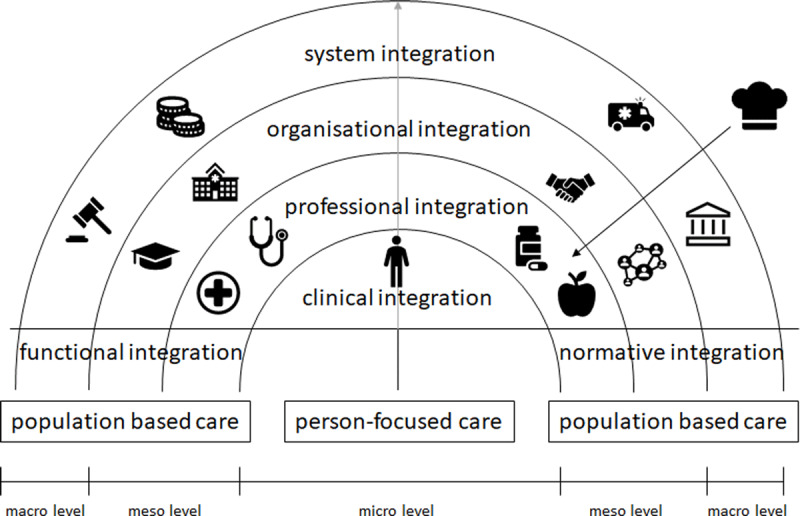
Adaption of Conceptual Framework of Integrated Care considering Chefs.
Legend: Figure 1 shows conceptual framework for integrated care by Valentijn et al., 2013 (32) modified to show the role of the chef/cook in an integrated nutritional care team.
This framework distinguishes functional from normative integration. Functional integration answers the question “who does what” and covers the tasks, activities, competencies, processes and tools necessary to provide coordinated care, while normative integration involves the context of care in terms of norms and values that guide care provision and daily demand [34]. In order to provide a key characteristic of integrated care, not only formal integration of structures and organizations need to be considered, but also an interdisciplinary way of working beyond professional silos [36,37].
As may be seen from Figure 1, the rainbow model is very useful to reflect all dimensions of involvement of chefs in healthcare, from community to institutionalized care provision. To illustrate possible practice-based dimensions of this innovative approach to integrated food and nutrition care delivery, authors have collected hands-on duties for chefs possibly included in the future professional profile (Table 1).
Table 1.
Examples for possible real-life Integration of Chefs in Healthcare.
|
| ||||
|---|---|---|---|---|
| LEVEL OF EFFECTIVE INTEGRATED FOOD AND NUTRITION CARE | CLINICAL INTEGRATION | PROFESSIONAL INTEGRATION | ORGANIZATIONAL INTEGRATION | SYSTEM INTEGRATION |
|
| ||||
| Person-centered care | Chefs carrying out taste steering assessments with patients on taste disturbances and create solutions for taste deterioration; Chefs talking with patients about their satisfaction with intervention outcomes in cooperation with other health professionals |
Chefs attending interprofessional team meetings and discussing treatment options with other professions in the nutritional care team | Chefs working together with educational institutions to educate chefs about nutrition and health Chefs working on promotion of workplace health, offering healthy cooking classes for employees |
Chefs advocating for a high quality cooking process to improve the nutritional value of meals for patients with needs |
|
| ||||
| Population-based care | Chefs creating cooking books for adapting meals and recipes for people with specific nutritional needs | Chefs cooperating with dieticians in developing baseline menus for people with specific needs | Chefs working together with insurance companies to promote cooking classes as social prescribing | Chefs working together with their professional association in order to promote healthy meals for the population and nutritional education for chefs |
|
| ||||
Legend: Table 1 illustrates practice-based examples, how chefs will be integrated in food and nutrition care delivery in healthcare through their new occupational profile developed during the ongoing EU-funded project “Nectar” (Grant agreement number 621707). As may be seen from the table, chefs’ involvement includes functional as well as normative aspects of integration. The profile developed will be based on learning outcomes during the training process, which include a comprehensive set of knowledge, skills and attitudes enabling chefs to become an integral part of the care team.
Discussion and reflection
The future needs and perspectives outlined in this paper are targeted by the project NECTAR: aN Eu Curriculum for chef gasTro-engineering in primAry food caRe (http://www.nectar-project.eu). Funded by the EU Erasmus+ program, NECTAR targets skills panorama for chefs in healthcare. All standards outlined in this publication will be addressed and included into the new job profile of CGEs to allow a functional integration.
One strength of NECTAR is the participation of European stakeholders, defining the new job profile, competence list and learning outcomes for CGEs. The project has been designed on a co-creation design-approach for sustainable service innovation and value creation during change management [38]. During the development of the profile and competencies, all partners from different professional sectors in food and healthcare contribute content according to relatively strict submission requirements, so that contributions may be categorized as having fixed contribution and aligned in structured methodology [39].
Another strength is the implementation of training programs arising from the desktop work done during the project. Underpinned by a strong evaluation framework, which will allow direct comparison of program designs through Europe, all educational pilots will address the same European framework, but are offered from cooking school to university level.
One of the challenges of NECTAR is the different EQF entry levels of chefs after their basic qualification across Europe. The project has designed tools to address these differences and to allow scaling-up of the project results in every EU MS.
Drawbacks of the project are that the new curriculum and program delivered will not allow to measure impact on healthcare quality already during the project phase and that the impact of functional integration on organisational structures and on system level is not measurable.
Conclusion
Evidence-based research points out that food and nutrition should become a cornerstone in future institutional healthcare delivery [40]. Although the EU has various frameworks and strategies for quality assurance, transferability and transparency for VET for professionals involved into that new care model [27,28,29,41], there is a skill gap for chefs in healthcare. Therefore, a high-standard workforce education is needed for chefs, which addresses the demand of the labour market.
The project presented in this publication gives a key perspective and solution to this challenge. Closing skills gaps for chefs in healthcare will allow a functional integration of chefs in the care team and will contribute to promote tasty, healthy and safe food compositions adapted for healthcare, not only at the national health and policy level but also at regional, institutional and individual level. Results gathered during the project are scale-able due to the project design and will push Europe and its MSs at the forefront of change management towards integrated interprofessional healthcare delivery.
Competing Interests
The authors have no competing interests to declare.
References
- 1.NutritionDay worldwide. How to recognize malnutrition? n. d. Available from: https://www.nutritionday.org/en/patients-relatives/patients-relatives/how-to-recognize-malnutrition/index.html.
- 2.Kang MC, Kim JH, Ryu SW, Moon JY, Park JH, Park JK, et al. Prevalence of Malnutrition in Hospitalized Patients: a Multicenter Cross-sectional Study. J Korean Med Sci. 2018; 33(2): e10. DOI: 10.3346/jkms.2018.33.e10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ruiz AJ, Buitrago G, Rodriguez N, Gomez G, Sulo S, Gomez C, et al. Clinical and economic outcomes associated with malnutrition in hospitalized patients. Clin Nutr. 2019; 38(3): 1310–6. DOI: 10.1016/j.clnu.2018.05.016 [DOI] [PubMed] [Google Scholar]
- 4.Barker LA, Gout BS, Crowe TC. Hospital malnutrition: prevalence, identification and impact on patients and the healthcare system. Int J Environ Res Public Health. 2011; 8(2): 514–27. DOI: 10.3390/ijerph8020514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leij-Halfwerk S, Verwijs MH, van Houdt S, Borkent JW, Guaitoli PR, Pelgrim T, et al. Prevalence of protein-energy malnutrition risk in European older adults in community, residential and hospital settings, according to 22 malnutrition screening tools validated for use in adults ≥65 years: A systematic review and meta-analysis. Maturitas. 2019; 126: 80–9. DOI: 10.1016/j.maturitas.2019.05.006 [DOI] [PubMed] [Google Scholar]
- 6.Lueg G, Wirth R, Kwiatkowski J, Rosler A, Jager M, Gehrke I, et al. Low Self-Perception of Malnutrition in Older Hospitalized Patients. Clin Interv Aging. 2020; 15: 2219–26. DOI: 10.2147/CIA.S278578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kontogianni MD, Poulia KA, Bersimis F, Sulz I, Schindler K, Hiesmayr M, et al. Exploring factors influencing dietary intake during hospitalization: Results from analyzing nutritionDay’s database (2006–2013). Clin Nutr ESPEN. 2020; 38: 263–70. DOI: 10.1016/j.clnesp.2020.04.001 [DOI] [PubMed] [Google Scholar]
- 8.BAPEN. British Association for Parental and Enteral Nutrition. Organisation of Food and Nutritional Support in Hospitals; 2007. [Google Scholar]
- 9.All Answers Ltd. Importance of Nutrition in Patient Care; November 2020. Available from: https://nursinganswers.net/essays/identify-the-importance-of-nutrition-in-patient-care-health-essay.php?vref=1.
- 10.Nichani S, Fitterman N, Lukela M, Crocker J, the Society of Hospital Medicine. 3.23 Team Approach and Multidisciplinary Care. J Hosp Med. 2017; 12(4). DOI: 10.12788/jhm.2998 [DOI] [Google Scholar]
- 11.Rigby M, Koch S, Keeling D, Hill P. Developing a New Understanding of Enabling Health and Wellbeing in Europe - Harmonising Health and Social Care Delivery and Informatics Support to Ensure Holistic Care. France: European Science Foundation; 2013. [Google Scholar]
- 12.World Health Organization. WHO global strategy on integrated people-centred health services 2016–2026. Executive Summary; July 2015. [Google Scholar]
- 13.World Health Organization Secretariat. Framework on integrated, people-centred health services. Report by the Secretariat. Assembly S-NWH; April 2016. [Google Scholar]
- 14.World Health Organization. Framework for Action on Interprofessional Education & Collaborative Practice. Health HPNNMHRf; 2010. [PubMed] [Google Scholar]
- 15.World Health Organization. Global strategy on human resources for health: Workforce 2030. Switzerland; 2016. [Google Scholar]
- 16.Lindner S, Kubitschke L, Lionis C, Anastasaki M, Kirchmayer U, Giacomini S, et al. Can Integrated Care Help in Meeting the Challenges Posed on Our Health Care Systems by COVID-19? Some Preliminary Lessons Learned from the European VIGOUR Project. Int J Integr Care. 2020; 20(4): 4. DOI: 10.5334/ijic.5596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. Strengthening Nutrition Action. A resource guide for countries based on the policy recommendations of the Second International Conference on Nutrition (ICN2). Rome; 2018. [Google Scholar]
- 18.European Commission. Skills Panorama. Health associate professionals; n. d. Available from: https://skillspanorama.cedefop.europa.eu/en/dashboard/browse-occupation?occupation=3.32&country=#7.
- 19.European Commission. ESCO. Medical doctors; n. d. Available from: http://data.europa.eu/esco/isco/C221.
- 20.European Commission. ESCO. dietitian; n. d. Available from: http://data.europa.eu/esco/occupation/8a53f8d3-d995-4c7b-a70d-d79f76bdcb3f.
- 21.European Commission. ESCO. Nursing professionals; n. d. Available from: http://data.europa.eu/esco/isco/C2221.
- 22.European Commission. ESCO. Diet cook; n. d. Available from: http://data.europa.eu/esco/occupation/9ab80ce6-504f-474f-bb91-98163e9d45fd.
- 23.OECD Health Division Team. Feasibility Study on Health Workforce Skills Assessment; Supporting health workers achieve personcentred care. February 2018. [Google Scholar]
- 24.Tsui EK, Morillo A. How cooks navigate nutrition, hunger and care in public-sector foodservice settings. Public Health Nutr. 2016; 19(5): 946–54. DOI: 10.1017/S1368980015002086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Obbagy JE, Condrasky MD, Roe LS, Sharp JL, Rolls BJ. Chefs’ opinions about reducing the calorie content of menu items in restaurants. Obesity (Silver Spring). 2011; 19(2): 332–7. DOI: 10.1038/oby.2010.188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.European Commission. Education and Training. About education and training in the EU; n. d. Available from: https://ec.europa.eu/education/education-in-the-eu/about-education-and-training-in-the-eu_en.
- 27.European Commission. Education and Training. European policy cooperation (ET 2020 framework); n. d. Available from: https://ec.europa.eu/education/policies/european-policy-cooperation/et2020-framework_en.
- 28.European Commission. Employment, Social Affairs & Inclusion. EQAVET – European Quality Assurance in Vocational Education and Training; n. d. Available from: https://ec.europa.eu/social/main.jsp?catId=1536&langId=en.
- 29.Europass European Union. The European Qualifications Framework (EQF); n. d. Available from: https://europa.eu/europass/en/european-qualifications-framework-eqf.
- 30.World Health Organization. Integrated care models: an overview. Working document; October 2016. [Google Scholar]
- 31.Zonneveld N, Driessen N, Stüssgen RAJ, Minkman MMN. Values of Integrated Care: A Systematic Review. Int J Integr Care. 2018; 18(4): 9. DOI: 10.5334/ijic.4172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MacAdam M. Frameworks of Integrated Care for the Elderly: A Systematic Review. Canadian Policy Research Networks Inc.; April 2008. [Google Scholar]
- 33.Goodwin N. Taking integrated care forward: the need for shared values. International journal of integrated care. 2013; 13: e026–e. DOI: 10.5334/ijic.1180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valentijn PP, Schepman SM, Opheij W, Bruijnzeels MA. Understanding integrated care: a comprehensive conceptual framework based on the integrative functions of primary care. Int J Integr Care. 2013; 13: e010. DOI: 10.5334/ijic.886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nightingale J. Nutrition support teams: how they work, are set up and maintained. Frontline Gastroenterol. 2010; 1(3): 171–7. DOI: 10.1136/fg.2009.000224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization. World report on Ageing and Health. Luxembourg; 2015. [Google Scholar]
- 37.Minkman MMN. Longing for Integrated Care: The Importance of Effective Governance. Int J Integr Care. 2017; 17(4): 10. DOI: 10.5334/ijic.3510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chathoth P, Altinay L, Harrington RJ, Okumus F, Chan ESW. Co-production versus co-creation: A process based continuum in the hotel service context. International Journal of Hospitality Management. 2013; 32: 11–20. DOI: 10.1016/j.ijhm.2012.03.009 [DOI] [Google Scholar]
- 39.Ohern MS, Rindfleisch A. Customer Co-Creation. In: Malhotra NK, (ed.), Review of Marketing Research. Review of Marketing Research. Emerald Group Publishing Limited. 2010; 6: 84–106. DOI: 10.1108/S1548-6435(2009)0000006008 [DOI] [Google Scholar]
- 40.World Health Organization. Nutrition in universal health coverage; October 2019. [Google Scholar]
- 41.European Commission. Get to know ESCO; n. d. Available from: https://ec.europa.eu/esco/portal/home?resetLanguage=true&newLanguage=en.


