Abstract
Background: The epidemiology and prevalence of the Human T-cell leukemia virus type-1 (HTLV-1) infection represent a recommended priority by global health agencies. An in-depth revision to update the status of this infection in countries including those of the Eastern Mediterranean Regional Office (EMRO) of the World Health Organization is hence required. Methods: Ninety-seven studies evaluating the HTLV-1 infection in low- and high-risk populations in EMRO countries were retrieved from the international electronic databases and were used to assess the epidemiological status of the infection in these countries. Results: Most epidemiologic reports were published from Iran, with more than 50% of Iranian prisoners and around 4% of healthy individuals reported to have the infection. In Egypt, a considerable prevalence of the virus spans around 1.11% of blood donors. Foci of HTLV-1 infection are also present in some countries and require a careful epidemiological evaluation. In the other EMRO countries, a lower prevalence that does not exceed 1% was reported. Conclusion: The epidemiology and prevalence of HTLV-1 in the EMRO countries require a tight revision and update. Published studies reveal a scarce distribution of the virus in the African countries of EMRO, while a lower prevalence is denoted in the Asian countries of EMRO, except in Iran, where the prevalence is high.
Keywords: human T-lymphotropic virus 1, Eastern Mediterranean Region, prevalence, epidemiology, Asian countries of EMRO, African countries of EMRO
1. Introduction
Human T-cell leukemia virus (HTLV) types 1 and 2 are the first identified human retroviruses. HTLV-1 was isolated from cultured lymphocytes of a patient with cutaneous lymphoma in 1979 [1], while HTLV-2 was found in a patient with hairy cell leukemia in 1982 [2]. HTLV-1 infects approximately 20 million people worldwide [3]. However, the endemic areas are clustered adjacent to regions where the infection is not common. The highest prevalence of HTLV-1 is reported in different continents; Asia, Japan, and Iran witnessed the highest prevalence of the virus. In Europe, Romania is highly endemic for the virus. The virus is prevalent in Intertropical West and South African countries, South America, and the Caribbean area [4]. In North America and Western Europe, HTLV-1 is predominant in migrants from endemic areas [5,6]. HTLV-1 infection was also reported in Melanesia, some islands in Oceania, and Central Australia [4,7,8].
HTLV-1 can be transmitted vertically from a mother to her child primarily by prolonged breastfeeding [9], through unprotected sexual intercourse mainly from male to female [10], by blood exposure via infected lymphoid cells [11], or by sharing needles between persons who use drugs [12]. HTLV-1 is the etiologic agent of a range of acute, chronic, and inflammatory disorders. Among these, adult T-cell leukemia-lymphoma (ATL) and the HTLV-1-associated myelopathy/tropical spastic paraparesis (HAM/TSP) are significant life-threatening morbidities [13]. In addition, it was demonstrated that the infection is associated with increased odds of developing diseases such as bronchitis, bronchiectasis, eczema, seborrheic dermatitis, and urinary tract infections which adversely affect the quality of life [14]. Moreover, the coinfection of HTLV-1 with other pathogens such as Mycobacterium tuberculosis and human immunodeficiency virus (HIV) was linked with a worse clinical course [15,16]. Likewise, pieces of evidence suggested that HTLV infection has an adverse effect on mortality even regardless of the effect of the increased number of inflammatory conditions [14]. To date, prophylactic measures are still lacking, and treatment strategies combatting this infection are not satisfactory. Moreover, the epidemiology of HTLV-1 remained obscure in certain areas and was underestimated or not updated in various parts of the world. Expanding the epidemiological studies to update the prevalence of HTLV-1 is one of the recent recommended actions by the HTLV-1 task force of the Global Virus Network [3]. The most recent World Health Organization technical guideline on HTLV-1 infection highlighted the same issue. The report emphasizes the need for epidemiological studies especially beyond the endemic areas, as migration contributed to increased detection of the infection [17]. The present review focused on the epidemiological studies on the distribution of HTLV-1 infection over the last two decades, based on the published reports on low-and high-risk populations in countries of the Eastern Mediterranean Regional Office (EMRO) of the World Health Organization.
2. Material and Methods
International electronic databases, including PubMed, Scopus, Web of Science, Index Medicus for the Eastern Mediterranean Region, and the Islamic World Science Citation Index, were searched until August 2021. The search strategy was as follows: (“human T-lymphotropic virus” OR “human T-cell lymphotropic virus”, OR “human T-cell leukemia-lymphoma virus” OR “HTLV”) AND (“Eastern Mediterranean” OR “Middle East” OR “North Africa” OR the names of each of the countries in the region) with no limitation to a specified field. Studies investigating HTLV-1 prevalence among populations at low and high risk of exposure to HTLV-1 were selected. Low-risk populations included healthy people, blood donors, pregnant women, and household-based survey participants. High-risk groups consisted of multi-transfused patients (such as hemodialysis, thalassemia, hemophilia, and malignancies), people who inject drugs (PWID), prisoners, and patients with HIV or sexually-transmitted diseases. The studies were selected based on HTLV-I detection using serological screening tests such as enzyme-linked immunosorbent assay (ELISA) or chemiluminescent immunoassay, with or without confirmation by complementary techniques such as immunoblotting or polymerase chain reaction (PCR).
The Eastern Mediterranean Region (EMR) comprises 15 Asian countries (Afghanistan, Bahrain, Iran, Iraq, Jordan, Kuwait, Lebanon, Oman, Pakistan, Palestine, Qatar, Saudi Arabia, Syria, the United Arab Emirates, and Yemen) and 7 African countries (Djibouti, Egypt, Libya, Morocco, Somalia, Sudan, and Tunisia) with a population of nearly 679 million individuals [18]. Studies published from January 2001 to August 2021 were included. Microsoft Excel (2010) was used to calculate the prevalence rates, and Epi Info 6.04b (CDC, USA) was used to compare the rates among males and females, using the chi-square test in each study. A p-value less than 0.05 was considered statistically significant.
3. Results and Discussion
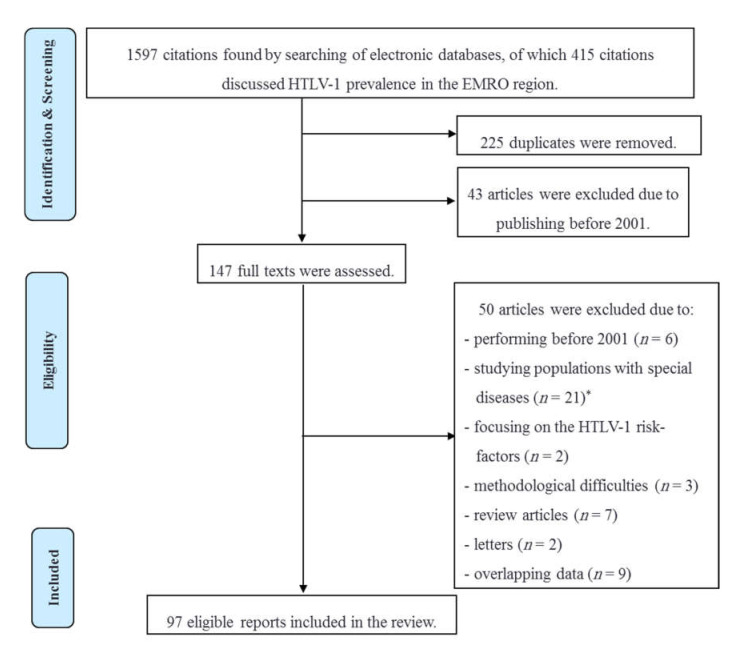
A total number of 1597 citations were identified in the five electronic databases. By screening the titles and abstracts, 190 non-duplicated citations discussing HTLV-1 prevalence among low- and high-risk populations in the EMRO region were identified. Forty-three articles published before 2001 were excluded, and the full texts of 147 remaining documents were reviewed. Forty-one papers were not included in this review. The reasons for excluding showed in Figure 1. Furthermore, nine surveys with the same studied cases, methods, and results were considered as overlapping and thus excluded. Finally, 97 non-overlapping original articles were included. They comprised 71 surveys from Iran; 15 from Saudi Arabia; 2 from Afghanistan, Lebanon, and Qatar; and 1 from Egypt, Iraq, Jordan, Kuwait, and Pakistan.
Figure 1.
Study selection for the review of HTLV-1 infection epidemiology in the countries of the Eastern Mediterranean Regional Office of the World Health Organization. * Patients with dermatological, hematological, rheumatological, or autoimmune disorders; carcinomas; infectious diseases other then HIV/AIDS; chronic diseases such as cardiovascular disorders and diabetes Melitus, etc.
3.1. HTLV-1 Infection in Iran
3.1.1. HTLV-1 Infection in Iranian Low-Risk Population
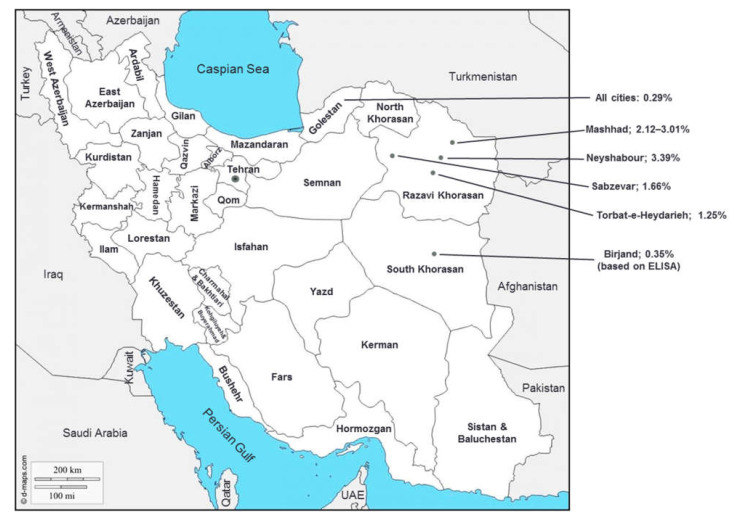
The highest number of published reports on HTLV-1 infection in Southwest Asia was from Iran. However, general population-based reports of HTLV-1 infection were only identified from three among 31 provinces, including Razavi Khorasan, South Khorasan, and Golestan in the north and east parts of the country (Figure 2) [19,20,21,22,23]. Mashhad, the capital of Razavi Khorasan province, and its neighbor city, Neyshabour, in the northeast of Iran, were previously introduced as HTLV-1 endemic districts in Iran [24,25,26]. Later investigations confirmed that these two cities are still endemic regions for the infection. The overall HTLV-1 prevalence was estimated at 2.12% (35/1654, 95% CI: 1.48–2.93%) among the general population of Mashhad [21]. Likewise, the HTLV-1 prevalence reached 7.25% (35/483) of individuals referred to a referral laboratory in Neyshabour and 1.06% (2/189) in screens of subgroups including pregnant women or candidates for a surgical operation in that region [27]. Additionally, many cases with HAM/TSP and ATL were reported in this area [28,29]. Recent investigations revealed an HTLV-1 prevalence of 1.66% (24/1445) and 1.25% (5/400) in healthy populations of Sabzevar and Torbat-e-Heydarieh cities (located in Razavi Khorasan province), respectively [19,22]. Lower rates of HTLV-1 infection were reported among the general population of Birjand city, the capital of South Khorasan province (0.35%, 12/3441, based on ELISA results) and Golestan province (0.29%, 6/2034), respectively (Table 1) [20,23].
Figure 2.
General population-based reports of HTLV-1 infection prevalence in Iran (References [19,20,21,22,23,24,30], source of background map: https://d-maps.com/carte.php?num_car=5494&lang=en, accessed on 12 February 2022).
Table 1.
Prevalence of HTLV-1 infection among low-risk population of Iran; 2001–2021.
| Population | Province (City, Direction in Country) |
Study Year | Sample Size | Participants’ Age; Ranges (Mean ± SD) | Male to Female Ratio | Lab Techniques |
Total Prevalence (%) |
Prevalence by Sex (%) | Ref. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Males | Females | p-Value | |||||||||
| General population | Golestan (North) | 2007 | 2034 | (38.7 ± 16.50) | 0.72 | ELISA, WB | 0.29 | 0.35 | 0.25 | 0.49 | [20] |
| Razavi Khorasan (Mashhad, Northeast) | ? | 9274 | ? | 0.67 | ELISA, PCR | 3.01 | 2.34 | 3.46 | 0.002 | [30] | |
| 2009 | 1654 | 1–90 | 0.83 | ELISA, WB, PCR | 2.12 | 1.46 | 2.66 | 0.093 | [21] | ||
| Razavi Khorasan (Neyshabour, Northeast) | 2002 | 1003 | 10–80 (32 ± ?) | 0.68 | ELISA, WB | 3.39 | 2.96 | 3.68 | 0.539 | [24] | |
| Razavi Khorasan (Sabzevar, Northeast) | 2008 | 1445 | 5–88 (36.6 ± 15.6) | 0.46 | ELISA, PCR | 1.66 | 2.42 | 1.31 | 0.128 | [19] | |
| Razavi Khorasan (Torbat-e-Heydarieh, Northeast) | 2011 | 400 | 14–89 (45.0 ± 16.8) | 1.05 | ELISA, PCR | 1.25 | 1.46 | 1.03 | 0.09 | [22] | |
| South Khorasan (East) | 2013–2014 | 3441 | 14–70 (38.7 ± 14.50) | 0.88 | ELISA | 0.35 | 0.25 | 0.44 | 0.34 | [23] | |
| Blood donors | Seven provinces | 2009–2013 | 1,864,489 | 18–65 (34.8 ± 10.4) | 10.32 | ELISA, WB | 0.10 | 0.09 | 0.18 | <0.001 | [31] |
| Razavi Khorasan (Northeast) | 628,667 | ? | ? | ELISA, WB | 0.21 | ? | ? | ? | |||
| West Azerbaijan (Northwest) | 307,422 | ? | ? | ELISA, WB | 0.07 | ? | ? | ? | |||
| North Khorasan (Northeast) | 79,035 | ? | ? | ELISA, WB | 0.06 | ? | ? | ? | |||
| Alborz (Center) | 264,340 | ? | ? | ELISA, WB | 0.06 | ? | ? | ? | |||
| South Khorasan (East) | 72,185 | ? | ? | ELISA, WB | 0.03 | ? | ? | ? | |||
| Gilan (North) | 373,227 | ? | ? | ELISA, WB | 0.02 | ? | ? | ? | |||
| Ardabil (Northwest) | 139,613 | ? | ? | ELISA, WB | 0.01 | ? | ? | ? | |||
| Seven provinces (East, North, Northeast, Northwest, Center)1 | 2010–2018 | 3,622,860 | 18–65 | 18.48 | ELISA, WB | 0.07 | 0.06 | 0.23 | <0.001 | [32] | |
| Bushehr (Southwest) | 2002–2003 | 22,740 | ? | 3.79 | ELISA, WB | 0.01 | 0.02 | 0 | - | [33] | |
| Charmahal and Bakhtiari (Southwest) | 2005–2006 | 800 | ? | ? | ELISA, WB | 0.50 | ? | ? | ? | [34] | |
| Fars (Shiraz) | ? | 500 | ? | 15.97 | ELISA | 0.20 | ? | ? | ? | [35] | |
| Golestan (North) | 2017 | 4226 | males: (37.6 ± 7.9), females: (38.3 ± 8.9) | ELISA, WB, PCR | 0.09 | ? | ? | ? | [36] | ||
| Hormozgan (South) | 2007–2008 | 1100 | ? | ? | ELISA, WB, PCR | 0.18 | ? | ? | ? | [37] | |
| Kermanshah (West) | 2015 | 470 | 10–59 | 9.0 | ELISA, WB | 0 | 0 | 0 | - | [38] | |
| 2011 | 1000 | (43.1 ± 19.8) | 0.71 | ELISA, WB | 0.50 | 0 | 0.86 | 0.079 | [39] | ||
| Mazandaran (Babol, North) | 2015–2016 | 503 | 19–61, males: (40.8 ± 9.8), females: (41.2 ± 11.4) | 24.15 | ELISA, PCR | 0.20 | 0.21 | 0 | - | [40] | |
| Razavi Khorasan (Mashhad, Northeast) | 2001–2002 | 60,892 | ? | ? | ELISA, WB | 0.66 | ? | ? | ? | [12] | |
| 2004–2006 | 232,648 | 18–65 (30 ± ?) | 9.88 | ELISA, WB | 0.45 | 0.42 | 0.76 | <0.001 | [41] | ||
| 2006–2008 | 250,582 | 17–63 (38.3 ± 10.8) | 11.74 | ELISA, WB | 0.40 | 0.36 | 0.88 | <0.001 | [42] | ||
| 2008–2009 | 79,687 | 17–65 | ? | ELISA, WB | 0.38 | ? | ? | ? | [43] | ||
| 2009–2010 | 165,860 | 17–59 (39.9 ± 10.5) | 13.71 | ELISA, WB | 0.26 | 0.23 | 0.70 | <0.001 | [44] | ||
| 2002–2013 | 983,000 | (35 ± 10 to 41 ± 11) | 14.63 | ELISA, WB | 0.30 | 0.28 | 0.48 | <0.001 | [45] | ||
| 2011–2013 | 174,662 | ? | 12.90 | ELISA, WB | 0.19 | 0.16 | 0.56 | <0.001 | [46] | ||
| Razavi Khorasan (Sabzevar, Northeast) | 2009–2012 | 35,067 | 17–59 (38.1 ± 11.8) | 9.06 | ELISA, WB | 0.14 | 0.13 | 0.26 | 0.095 | [47] | |
| South Khorasan (East) | 2005–2015 | 165,267 | males: (29.5 ± ?), females: (32.8 ± ?) | 11.55 | ELISA, WB | 0.03 | 0.03 | 0.02 | 0.038 | [48] | |
| Tehran (North) | ? | 2000 | ? | ? | ELISA, PCR | 0.05 | ? | ? | ? | [49] | |
| West Azerbaijan (Northwest) | 2005 | 2046 | (31.9 ± 10.2) | 14.04 | ELISA, WB | 0.34 | 0.26 | 1.47 | 0.074 | [50] | |
| 2009–2019 | 682,171 | 18–65 | 30.13 | ELISA, WB | 0.05 | 0.05 | 0.14 | <0.001 | [51] | ||
| Corneal donors | Nationwide | 2005–2007 | 5533 | 2–84 | 4.19 | ELISA, WB | 0.67 | 0.58 | 1.03 | 0.105 | [52] |
| Tissue donors | Nationwide | 2002–2007 | 1548 | 0–66 (29.1 ± 11.6) | 3.11 | ELISA | 1.61 | 1.45 | 2.12 | 0.369 | [53] |
| Pregnant women | Razavi Khorasan (Mashhad, Northeast) | 2010–2011 | 407 | (26 ± ?) | ? | ELISA, PCR | 1.47 | ? | ? | ? | [54] |
| People who referred to a medical lab | Razavi Khorasan (Neyshabour, Northeast) | 2009 | 483 | 5–84 (37.4 ± 15.4) | 0.26 | ELISA, WB | 7.25 | 10.31 | 6.49 | 0.196 | [27] |
| 2010–2014 | 8054 | males: (46 ± 3), females: (51 ± 3) | 0.24 | ELISA | 6.56 | 8.31 | 6.13 | 0.002 | [55] | ||
| 2013–2014 | 1169 2 | 2–35, (26.3 ± 5.4) | 0.14 | ELISA | 3.34 | 6.38 | 2.92 | 0.058 | [56] | ||
| 2011–2015 | 5724 3 | 15–40 (28.2 ± 6.0) | ? | ELISA | 2.04 | - | 2.04 | - | [57] | ||
| People who admitted to a referral hospital | Mazandaran (Sari, North) | 2009–2010 | 1200 | 1–76 | 0.55 | ELISA, WB | 0.08 | 0.24 | 0 | - | [58] |
| Razavi Khorasan (Northeast) | 2016–2017 | 758 4 | 0–14 (6.4 ± 1.8) | 1.14 | ELISA, PCR | 1.45 | ? | ? | ? | [59] | |
| Tehran (North) | 2009–2011 | 219 | 13–84 (39.9 ± 16.5) | 0.72 | ELISA | 1.83 | 1.09 | 2.36 | 0.641 | [60] | |
(?) means not reported; (-) means not-applicable; ELISA: Enzyme-linked immunosorbent assay; WB: Western blotting; PCR; polymerase chain reaction. 1 Included Alborz, Ardabil, Gilan, North, South, and Razavi Khorasan, and West Azerbaijan. 2 Children and juveniles (2–35 years old), 3 Young females (15–40 years old), 4 Children (less than 15 years old).
Recent phylogenetic and phylodynamic analysis of the long terminal repeat region of HTLV-1 in blood samples of 100 seropositive individuals from the north and south parts of Iran revealed that Iranian isolates belonged to the globally-distributed HTLV-1 Cosmopolitan subtype A [61]. These results concluded that most infections in Iran presumably occurred following the Mongol attack, before the 15th century, and were further facilitated by the ancient Silk Road linkage starting from China and continuing toward Turkey.
In order to check the published literature related to HTLV-1 infection prevalence among Iranian blood donors, the studies published until August 2011 were previously reviewed, and the prevalence of infection was estimated as low as 0.12% (95% CI: 0.05–0.29%); it ranged from 0.015% in the southwest to 0.38% in the northeast of Iran [62]. A meta-analysis by Azami et al. estimated the prevalence of HTLV-1 infection at 0.20% (95% CI: 0.15–0.26%) based on reviewing 34 studies comprising 3,626,364 blood donors published from 1996 to 2017 [63]. Regular screening of all donated blood units for antibodies against HTLV-1/2 followed by confirmatory tests was introduced in northeastern Iran in 1995 [64] and then extended to some provinces in the north and northwest parts of the country. These tests were performed among first-time and regular blood donors, and as a result, many surveys revealed a gradual decrease in HTLV-1 prevalence among Iranian blood donors from 0.13% in 2009 to 0.03% in 2018 (Table 1) [31,32,63]. A declining trend in the infection rate among blood donors was documented in Razavi Khorasan [41,42,45,47] as well as other provinces of Iran [48,51]. However, over time, no change was observed in the HTLV-1 infection rate among the general population of Razavi Khorasan province [21,26,30]. Statistically significant higher rates of HTLV-1 infection were reported in Iranian females as compared to males [30,31,32,41,42,44,45,46,51]. In that sense, a recent meta-analysis estimated a three-fold higher infection rate among female blood donors as compared to male donors (0.64%, 95% CI: 0.13–3.01% and 0.20%, 95% CI: 0.15–0.27%, respectively) [63]. However, some investigators could not find any differences between both sexes regarding HTLV-1 prevalence in Iran (Table 1); keeping the gender-related infection with this virus a controversial topic requires more epidemiological investigation. Considering a national screening program for mothers to avoid transmission of the virus through breastfeeding could be suggested as a preventive strategy. Furthermore, most of the surveys among the low-risk Iranian population revealed significantly greater rates of HTLV-1 infection among people with an age range between 40 and 60 years old, as compared to younger people in the bracket of 15 to 25 years old [19,20,21,22,24,27,31,32,42,44,45,51,56]. Our previous study among the general population of Mashhad showed an 18-fold higher infection rate among individuals older than 55 years (9.14%, 17/186), compared to people younger than 15 years (0.52%, 2/387). The logistic regression analysis revealed that the participants’ age could significantly affect the risk of infection (Odds ratio = 4.3, 95% CI: 1.5–12.3) [21]. Similarly, Emadi et al. reported an HTLV-1 prevalence in 4 per 100,000 among 263,465 blood donors aged between 18 and 25 years old, while 66 per 100,000 donors of 46 to 65 years old [51]. Conversely, some studies with considerable sample sizes (from 407 to 35,067 individuals) reported no significant relationship between participants’ age and the infection rate [23,36,47,54]. An age- and sex-matched case-control study to assess the HTLV-1 risk factors among “first-time” Iranian blood donors was performed during the period 2011–2012 [65]. The regression analysis revealed that the city of birth, low income, low educational level, history of blood transfusion, and drug abuse were correlated with HTLV-1 infection. In addition, living in the northeastern of Iran [31], being married [21,31,42,48], populated family [27], history of blood transfusion [21,27], hospitalization [21,27], surgery [19,21], wet cupping [21], and imprisonment [19] seemingly correlate with HTLV-1 infection among Iranian population. Moreover, many studies showed that “first-time” blood donors are more likely to be HTLV-1 seropositive than regular donors [31,32,42,47,48,51], which could be because of those who are positive for the infection are not allowed to donate again.
In terms of clinical findings among HTLV-1 infected individuals in Iran, most studies focused on the neurologic manifestations of the disease. Shoeibi et al. reported that gait disturbances followed by sensory and urinary complaints are the most common manifestation in HAM/TSP patients in Mashhad, Iran. In contrast, other clinical symptoms, including back pain, constipation, and erectile dysfunction, are not commonly reported. The hypertonicity is mainly reported in lower limbs, and most of the patients develop brisk tendon reflexes in all limbs. In terms of sensory findings, foot paresthesia was a common compliment, and impairment of vibration sensation was more prominent in lower limbs [29]. While cranial nerves and cerebellum involvement were reported in HTLV-1 infected patients, this finding was not reported in Iranian HAM/TSP patients [29]. Among Iranian ATLL patients, laboratory findings including leukocytosis, neutropenia, and lymphocytosis were common findings. Moreover, elevated serum alkaline phosphatase and lactate dehydrogenase were reported in 80% and 75% of these patients in Mashhad city [28].
3.1.2. HTLV-1 Infection among High-Risk Iranian Population
HTLV-1 prevalence was also investigated among high-risk Iranian populations, including patients with thalassemia or hemophilia, those undergoing hemodialysis, HIV-positive individuals, PWID, and prisoners. Significant high rates of HTLV-1 infection (3.24%, 95% CI: 2.19–4.78%) were previously estimated among Iranian multi-transfused patients [66]. Currently, the rate of HTLV-1 prevalence varies between 0.18% and 11.28% among thalassemia patients and 0 to 14.49% among the hemodialysis group (Table 2). The highest rates among hemodialysis patients were reported from Razavi Khorasan (5.93%, 8/135 and 14.49%, 20/138) and Charmahal and Bakhtiari provinces (6.54%, 7/107) [67,68,69]. Besides, the highest rates among thalassemia patients were reported from Tehran (6.29%, 11/175 and 11.28%, 29/257) and Charmahal and Bakhtiari provinces (6.80%, 17/250) [49,69,70,71]. Regarding the considerable rate of HTLV-1 infection among patients receiving blood products, more restrictive preventive measures such as screening and leukoreduction programs in blood banks should be considered to reduce the infection transmission through the infected products. Furthermore, considerably high rates of infection were documented in persons experiencing drug dependence and/or HIV-positive individuals in Razavi Khorasan (51.49%, 52/101 and 15%, 3/20, respectively) [12,72], and Khuzestan provinces (16.35%, 17/104) [73]. Rowhani-Rahbar et al. reported a very high rate of HTLV-1 infection (51.49%) among 101 prisoners with a dependence on a substance in the central prison of Mashhad in 2001, especially among subjects who shared their syringes (Odds ratio = 2.5, 95% CI: 1.1–5.7) [12]. Moreover, Khajedaluee et al. reported that HTLV-1 infection occurred in 2% of 1114 inmates of two central prisons in Mashhad in 2008 [74]. Nearly two-fifths of the responders were drug users, and the infection was associated with a history of drug dependence [74]. Reducing HTLV-1 transmission could be improved by avoiding sharing needles or syringes and using sterile devices provided by healthcare systems. Moreover, considering the HTLV-1 infection as a sexually transmitted disease, condom use should be encouraged to prevent sexual transmission from the infected patients, especially those who engage in risky sexual relationships [75].
Table 2.
Prevalence of HTLV-1 infection among high-risk populations of Iran; 2001–2021.
| Population | Province (City, Direction in Country) |
Study Year | Sample Size | Participants’ Age; Ranges (Mean ± SD) | Male to Female Ratio | Lab Techniques |
Prevalence (%) | Ref. |
|---|---|---|---|---|---|---|---|---|
| Hemodialysis patients | Busher (Southwest) | 2003 | 101 | ? | ? | ELISA, WB | 0 | [76] |
| Charmahal and Bakhtiari (Southwest) | 2005 | 107 | 18–90, (65 ± ?) | ? | ELISA, WB | 6.54 | [69] | |
| Hormozgan (South) | 2007–2008 | 40 | ? | ? | ELISA, WB | 0 | [37] | |
| Kurdistan (Sanandaj, West) | 2010 | 65 | (45.1 ± ?) | ? | ELISA, WB | 0 | [77] | |
| Mazandaran (Sari and Ghaemshahr, North) | 2011 | 160 | (59.1 ± 14.7) | 1.0 | ELISA, WB | 0.63 | [78] | |
| Razavi Khorasan (Mashhad, Northeast) | 2009–2010 | 135 | males: (43.5 ± 12.5), females: (50.5 ± 13.2) | 0.99 | ELISA, PCR | 5.93 | [67] | |
| Razavi Khorasan (Neyshabour, Northeast) | 2012 | 138 | 12–84, (53.3 ± 17.9) | 1.23 | ELISA, WB | 14.49 | [68] | |
| South Khorasan (Birjand, East) | 2010 | 41 | (54.9 ± 16.5) | 2.15 | ELISA, WB | 2.44 | [79] | |
| Tehran (North) | ? | 150 | 24–88, (63.6 ± 13.4) | 1.34 | ELISA, WB | 0.67 | [80] | |
| 2016–2017 | 174 | 17–86, (56 ± ?) | 1.32 | ELISA, PCR | 1.15 | [81] | ||
| West Azerbaijan (Urmia, Northwest) | 2006 | 95 | (31.9 ± 10.2) | ? | ELISA, WB | 1.05 | [50] | |
| Thalassemia patients | Busher (Southwest) | 2003 | 455 | ? | ? | ELISA, WB | 3.08 | [76] |
| Charmahal and Bakhtiari (Southwest) | 2005 | 250 | 1–45, (25 ± ?) | ? | ELISA, WB | 6.80 | [69] | |
| Fars (Shiraz, South) | ? | 200 | ? | ? | ELISA | 3.00 | [35] | |
| Golestan (Gorgan, North) | 2004–2005 | 181 | 1–25, (14.1 ± 6.5) | 1.06 | ELISA, WB | 4.42 | [82] | |
| Hormozgan (South) | 2007–2008 | 163 | ? | ? | ELISA, WB, PCR | 3.07 | [37] | |
| Isfahan (Center) | 2007 | 150 | 1–49, (17.7 ± ?) | 1.42 | ELISA, WB | 3.33 | [83] | |
| 2012 | 67 | ? | ? | ELISA, PCR | 1.49 | [84] | ||
| Kermanshah (West) | 2011 | 116 | (16.8 ± 6.6) | 1.23 | ELISA, WB | 3.45 | [39] | |
| Kurdistan (Sanandaj, West) | 2010 | 46 | (13.3 ± ?) | ? | ELISA, WB | 2.17 | [77] | |
| Mazandaran (North) | 2009 | 288 | (21.5 ± 6.6) | 0.91 | ELISA, PCR | 1.39 | [85] | |
| Mazandaran (Tonekabon, North) | 2015 | 80 | ? | ? | ELISA, PCR | 2.50 | [86] | |
| Razavi Khorasan (Mashhad, Northeast) | 2007 | 360 | 1–52, (11.6 ± 0.5) | 1.38 | ELISA | 6.11 | [87] | |
| 2006–2013 | 100 | 5–46, (22.7 ± ?) | 1.38 | ELISA, PCR | 4.00 | [88] | ||
| Tehran (North) | 2003 | 175 | (18.1 ± 1.0) | 1.36 | ELISA, WB | 6.29 | [70] | |
| 2008–2010 | 257 | ? | 0.89 | ELISA, WB | 11.28 | [71] | ||
| ? | 100 | ? | ? | ELISA, PCR | 8.00 | [49] | ||
| Hemophilia patients | Busher (Southwest) | 2003 | 86 | ? | ? | ELISA, WB | 0 | [76] |
| South Khorasan (East) | ? | 80 | (21.3 ± 12.1) | 25.67 | ELISA, WB | 1.25 | [89] | |
| 2010–2012 | 108 | 14–85, (27.7 ± 16.4) | 14.43 | ELISA | 2.78 | [90] | ||
| West Azerbaijan (Northwest) | ? | 50 | (10.3 ± ?) | 6.14 | ELISA, WB | 0 | [91] | |
| Patients with combined factor 5 and 8 deficiency | Razavi Khorasan (Mashhad, Northeast) | 2007 | 24 | 6–61, (26.9 ± 15.1) | 2.0 | ELISA, WB | 0 | [92] |
| HIV-positive patients | Isfahan (Center) | 2010–2011 | 56 | (37.0 ± 8.7) | 5.22 | ELISA | 1.79 | [93] |
| Khuzestan (Ahwaz, Southwest) | 2001–2003 | 104 1 | ? | * | ELISA, WB | 16.35 | [73] | |
| Kurdistan (Sanandaj, West) | 2010 | 130 1 | (27.2 ± ?) | 239.0 | ELISA, WB | 0.77 | [77] | |
| Razavi Khorasan (Mashhad, Northeast) | ? | 20 | 22–50, (36.4 ± 8.6) | 4.0 | ELISA, WB | 15.0 | [72] | |
| Tehran (North) | ? | 100 | ? | ? | ELISA, PCR | 5.00 | [49] | |
| People who inject drugs | Isfahan (Center) | 2007–2008 | 150 2 | (30.7 ± 7.1) | 74.0 | ELISA | 2.67 | [94] |
| Khuzestan (Ahwaz, Southwest) | 2001–2003 | 104 1 | ? | * | ELISA, WB | 16.35 | [73] | |
| Kurdistan (Sanandaj, West) | 2010 | 130 1 | (27.2 ± ?) | 239.0 | ELISA, WB | 0.77 | [77] | |
| 2010 | 110 3 | ? | ? | ELISA, WB | 0.91 | [77] | ||
| Razavi Khorasan (Mashhad, Northeast) | 2001 | 101 4 | (32.8 ± 8.9) | ? | ELISA, WB | 51.49 | [12] | |
| 2007–2008 | 62 5 | (34.3 ± ?) | 30.0 | ELISA | 8.06 | [95] | ||
| Tehran (North) | ? | 180 | 9–67, (36.9 ± 9.2) | ? | ELISA, WB | 0 | [96] | |
| Prisoners | Razavi Khorasan (Northeast) | 2001 | 101 4 | (32.8 ± 8.9) | ? | ELISA, WB | 51.49 | [12] |
| 2008 | 1114 6 | males: (34.4 ± 10.9), females: (40.7 ± 14.2) | 8.13 | ELISA, PCR | 1.97 | [74] | ||
| South Khorasan (Birjand, East) | 2014–2015 | 300 7 | 20–78, (37.4 ± 9.4) | * | ELISA, WB | 0 | [97] |
(?) means not reported; * All cases were male; ELISA: Enzyme-linked immunosorbent assay; WB: Western blotting; PCR; polymerase chain reaction. 1 HIV-positive people who use drugs. 2 Including outpatients and hospitalized people who use drugs. 3 HIV-negative people who use drugs. 4 Imprisoned people who use drugs. 5 Hospitalized people who use drugs. 6 Including people who use drugs and others. 7 Including people who use and/or inject drugs.
3.2. HTLV-2 Infection in Iran
Screening 1654 serum samples from the general population of Mashhad did not demonstrate any HTLV-2 positive cases [98]. This was asserted by the results of nested PCR using specific external and internal primers to detect HTLV-2 provirus in 50 Iranian HTLV-1-positive blood donors, who showed sero-indeterminate results in the Western blotting test. Ten cases with positive PCR results for HTLV-1 were identified, while all samples were negative for HTLV-2 [99]. On the other hand, there is no evidence regarding HTLV-2 infection incidence among the high-risk Iranian population. However, the prevalence of this infection was considerably high among PWID in western countries [100].
3.3. HTLV-1 Infection in EMRO Countries except for Iran
3.3.1. HTLV-1 Infection in Asian Countries of EMRO
In countries of Southwest Asia other than Iran, HTLV-1 infection seems non-endemic (Table 3). In a survey among the general population of five provinces in Afghanistan, anti-HTLV-1 antibodies were detected in 0.64% of 466 participants using ELISA. However, no complimentary test was further performed to confirm these results [101]. The highest infection rate (1.59%, 2/126) was observed among people older than 45 years, but the rate was associated with neither the participants’ gender nor the geographical region. Another survey conducted in four cities of Afghanistan showed no evidence of HTLV-1 seropositivity in 80 hemophilia screened patients [102].
Table 3.
Prevalence of HTLV-1 infection low- and high-risk populations of countries in the Eastern Mediterranean Regional Office of WHO (except Iran); 2001–2021.
| Population | Country (Province, City) | Study Year | Sample Size | Participants’ Age; Ranges (Mean ± SD) | Male to Female Ratio | Lab Techniques | Prevalence (%) | Ref. |
|---|---|---|---|---|---|---|---|---|
| General population | Afghanistan (5 provinces) 1 | 2015 | 466 | 25–70, (38.9 ± 12.0) | 0.98 | CMIA | 0.64 | [101] |
| Blood donors | Egypt (Cairo) | 2005–2006 | 90 | 18–47, (29.3 ± 6.5) | 6.50 | ELISA, PCR | 1.11 | [103] |
| Iraq (7 provinces) 2 | 2015 | 15,239 | 20–57, (36 ± ?) | ? | ELISA, CMIA | 0.26 | [104] | |
| Jordan (Amman) | 2009–2013 | 62,933 | 18–60 | ? | ELISA | 0 | [105] | |
| Kuwait (Nationwide) | 2002 | 12,798 | males: 20–56, (35 ± ?), females: 24–50, (30 ± ?) | ? | ELISA, CMIA | 0.01 | [106] | |
| Lebanon (Beirut) | 2000–2002 | 500 | (38.7 ± ?) | 3.17 | ELISA | 0 | [107] | |
| Lebanon (Nationwide) | 2001–2002 | 3529 | (30.0 ± 8.9) | 22.80 | ELISA, WB, PCR | 0.06 (WB), 0.03 (PCR) | [108] | |
| Qatar (Nationwide) | 1991–2003 | 124,266 | ? | ? | ELISA, WB | 0.0002 | [109] | |
| Qatar (Doha) | 2013–2017 | 190,509 | ? | 10.03 | CMIA, LIA | 0.18 | [110] | |
| Pakistan (Rawalpindi) | 2013 | 2100 | 18–60, (29.0 ± 9.3) | 62.64 | CMIA, LIA, PCR | 0.19 | [111] | |
| Saudi Arabia (Al-Khobar) | 1995–2001 | 23,493 | (33.8 ± ?) | ? | ELISA, WB | 0.05 | [112] | |
| Saudi Arabia (Dammam) | 1998–2001 | 13,443 | ? | ? | ELISA, WB | 0.06 | [113] | |
| Saudi Arabia (Riyadh) | 1999–2001 | 24,654 | ? | ? | ELISA, WB | 0.004 | [114] | |
| Saudi Arabia (Riyadh) | 2000–2002 | 24,173 | (33.8 ± ?) | 108.38 | ELISA, LIA | 0 | [115] | |
| Saudi Arabia (Al-Hasa) | 1997–2003 | 47,426 | 18–55 | ? | ELISA, WB | 0.01 | [116] | |
| Saudi Arabia (Jeddah) | ? | 30,000 | ? | ? | ELISA, WB | 0 | [117] | |
| 2006–2015 | 107,419 | ? | ? | CMIA, WB | 0 | [118] | ||
| Saudi Arabia (Al-Baha) | 2009–2011 | 2807 | 16–66 | * | ELISA | 0.04 | [119] | |
| Saudi Arabia (Aseer) | 2012 | 4432 | 18–60, (30 ± ?) | * | ELISA | 0 | [120] | |
| Saudi Arabia (Aseer) | 2012–2013 | 7267 | 18–60 | 278.50 | ELISA | 0 | [121] | |
| Saudi Arabia (Qassim/Unaizah) | 2013–2016 | 9460 | 18–48, (31.4 ± 8.7) | 26.82 | ELISA, PCR | 0.10 | [122] | |
| Saudi Arabia (Hail) | 2016 | 361 | <20 to >50 | ? | ELISA | 2.22 | [123] | |
| Saudi Arabia (Majmaah) | 2015–2017 | 3028 | 18–61 | 44.6 | ELISA | 0.20 | [124] | |
| Saudi Arabia (Buraidah) | 2017–2018 | 4590 | 16–65 | 4.88 | ELISA | 0 | [125] | |
| Saudi Arabia (Najran) | ? | 953 | ? | 237.25 | ELISA | 0 | [126] | |
| Hemophilia patients | Afghanistan (four cities) 3 | 2017 | 80 | 2–38, (13.7 ± 9.8) | ? | ELISA | 0 | [102] |
| Lebanon (Beirut) | 2000–2002 | 30 | (37.4 ± ?) | * | ELISA | 0 | [107] | |
| Malignancy patients with multiply transfusions | Lebanon (Beirut) | 2000–2002 | 65 | (30.5 ± ?) | 1.32 | ELISA | 0 | [107] |
| People who inject drugs | Lebanon (Beirut) | 2000–2002 | 40 | (50.3 ± ?) | 3.0 | ELISA | 0 | [107] |
(?) means not reported; * All cases were male; CMIA: Chemiluminescent microparticle immunoassay; ELISA: Enzyme-linked immunosorbent assay; LIA: Line Immunoassay; WB: Western blotting; PCR; polymerase chain reaction. 1 Including Nangarhar, Herat, Mazar-e Sharif, Kandahar, and Kabul. 2 Including Baghdad, Karbala, Al-Qadisiyyah, Al-Najaf, Al-Muthanna, Al-Basrah, and Wasit. 3 Including Kabul, Herat, Mazar-i-Sharif, and Jalal Abad.
In a cross-sectional survey performed in Qatar, 0.18% of nearly 200,000 blood samples donated from 2013 to 2017 showed HTLV-1/2 seroreactivity in enzyme-linked and line immunoassays, and the trend for this infection was increasing from 0.08% to 0.23% [110]. Likewise, Ibrahim et al. demonstrated a rate of 0.26% (39/15239) HTLV-1/2 seropositivity among samples collected in Iraqi blood banks using enzyme-linked and chemiluminescent immunoassays [104]. No or meager seroprevalence rates of HTLV-1 infection were reported in blood donors from Jordan [105], Kuwait [106], Lebanon [107,108], Pakistan [111], and different parts of Saudi Arabia [109,114,115,116,117,118,120,122,124,125]. In Lebanon, no HTLV-1 positive cases were found initially among blood donors and even in high-risk groups such as PWID, hemophilia patients, or those with malignancy who received multiply blood transfusions [107]. Bitar et al. later reported two cases of acute ATL diagnosed in Lebanon, one from the Lebanese origin and the second from the Romanian origin. In both patients, Western blotting confirmed HTLV-1 seropositivity, and the HTLV-I oncoprotein Tax expression was documented in the leukemic cells [127]. Upon screening of Lebanese patient family members, seven direct family members were HTLV-I positive, and four were regular blood donors [127].
HTLV-1 infection rates were associated with the nationality of participants in most Arab countries. In Saudi Arabia, slightly higher infection rates were reported among non-Saudi blood donors (0.074–0.113%) as compared to Saudi donors (0.046–0.055%) [112,113]. Nevertheless, other studies showed a decreasing trend in HTLV-1 prevalence among blood donors of Saudi Arabia [113,116]. Similarly, the infection rate among 81,699 non-Qatari (including Arab and non-Arab) blood donation volunteers was 0.03%, but only one positive case was identified among 42,567 Qatari national donors (0.002%) [109]. Conversely, one of 8561 Kuwaiti blood donors was HTLV seropositive, and no positive HTLV cases were detected among 4237 non-Kuwaiti Arab donors [106].
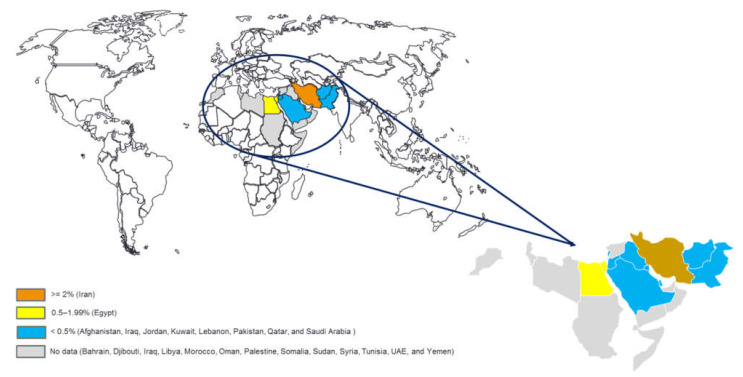
Not a single report documented the prevalence of HTLV-1 infection in other Asian countries, including Bahrain, Oman, Palestine, Syria, United Arab Emirates, and Yemen of EMRO (Figure 3). However, sporadic cases were reported in Arab populations residing in other countries. Fawzi et al. reported one person with HTLV-1 among 1929 Syrian blood donors who resided in Qatar but did not find any seropositive cases among donors who originated from Jordan, Palestine, and Yemen [109]. Similarly, Bazarbachi et al. diagnosed four HTLV-1 positive ATL patients among Iraqi patients who sought medical care in Lebanon (manuscript in preparation). Although no formal epidemiological study was conducted in Iraq, epidemiological foci of HTLV-1 infection seemingly exist. Therefore, a tight screening to evaluate the incidence, prevalence, and burden of this viral infection is required in the Iraqi population.
Figure 3.
Map of the geographical distribution of HTLV-1 infection in countries of the Eastern Mediterranean Regional Office of the World Health Organization (drawn based on the epidemiological reports in the general population or blood donors included in this review).
As with Iran, the limited genotype data indicated that the most frequent subtype of HTLV-1 is the “transcontinental” subgroup of cosmopolitan (A) subtype over the EMRO region [4].
3.3.2. HTLV-1 Infection in African Countries of EMRO
Only one epidemiologic survey in Egypt was conducted and reported one HTLV-1-positive case among 90 Egyptian blood donors during 2005–2006 (Table 3). Unfortunately, not a single epidemiological study from Djibouti, Libya, Morocco, Somalia, Sudan, and Tunisia was identified over the last two decades, leaving a gap in our knowledge on the status of HTLV-1 infection in these EMRO countries (Figure 3). However, it is noteworthy to mention that there are some reports regarding the infected individuals who originated from Somalia [109], Sudan [109], and morocco [128], which highlight the need for more epidemiological studies in this part of the EMRO countries.
3.4. Study Limitations
In the present study, we skimmed the known literature to evaluate the epidemiological status of HTLV-1 infection in the countries of the EMRO region. We relied on the scientific reports indexed in specific electronic databases. We also tried to include common international and regional databanks. Therefore, some reports about the prevalence of HLTV-1 infection may be lacking. These include indexed reports in other sources or data not included in any database but presented in conference proceedings, dissertations, organizational reports, and magazines. Reports considering HAM or ATL published from the EMRO region were also excluded.
Moreover, the heterogeneous studied population of the surveys included in the present review may make the comparison of the results difficult. In addition, confirmatory laboratory tests were not performed in some studies or were not the same across all the studies. The present review included the studies with even small sample sizes to cover the entire EMRO population as possible.
4. Conclusions
The epidemiologic data on HTLV-1 infection in most parts of the Eastern Mediterranean region are limited or lacking. The available published literature reveals that the prevalence of HTLV-1 infection in part of the Eastern Mediterranean region, except Iran, is low. The evidence on HTLV-1 prevalence in the African part of EMRO is scarce, and the epidemiological data in endemic regions are not updated. A more systematic and more frequent analysis of the status of HTLV-1 infection in EMRO countries is required, especially in countries such as Iraq and Morocco, where the HTLV-1 infection was identified and reflected the presence of foci in these countries. Finally, the longstanding infection control strategies, including the HTLV-1 screening of blood donors in most endemic regions, requires future validation by complementary techniques, such as PCR, to increase the specificity of the infection diagnosis.
Author Contributions
Conceptualization, M.R.H.-M. and A.B.; methodology, M.R.H.-M. and R.J.E.; writing—original draft preparation, M.R.H.-M., R.J.E. and H.E.H.; writing—review and editing, M.R.H.-M., R.J.E., H.E.H. and A.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Poiesz B.J., Ruscetti F.W., Gazdar A.F., Bunn P.A., Minna J.D., Gallo R.C. Detection and isolation of type C retrovirus particles from fresh and cultured lymphocytes of a patient with cutaneous T-cell lymphoma. Proc. Natl. Acad. Sci. USA. 1980;77:7415–7419. doi: 10.1073/pnas.77.12.7415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalyanaraman V.S., Sarngadharan M.G., Robert-Guroff M., Miyoshi I., Blayney D., Golde D., Gallo R.C. A new subtype of human t-cell leukemia virus (HTLV-II) associated with a t-cell variant of hairy cell leukemia. Science. 1982;218:571–573. doi: 10.1126/science.6981847. [DOI] [PubMed] [Google Scholar]
- 3.Willems L., Hasegawa H., Accolla R., Bangham C., Bazarbachi A., Bertazzoni U., Carneiro-Proietti A.B.D.F., Cheng H., Chieco-Bianchi L., Ciminale V., et al. Reducing the global burden of HTLV-1 infection: An agenda for research and action. Antivir. Res. 2016;137:41–48. doi: 10.1016/j.antiviral.2016.10.015. [DOI] [PubMed] [Google Scholar]
- 4.Gessain A., Cassar O. Epidemiological Aspects and World Distribution of HTLV-1 Infection. Front. Microbiol. 2012;3:388. doi: 10.3389/fmicb.2012.00388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Catovsky D., Greaves M.F., Rose M., Galton D.A., Goolden A.W., McCluskey D.R., White J.M., Lampert I., Bourikas G., Ireland R., et al. Adult T-cell lymphoma-leukaemia in Blacks from the West Indies. Lancet. 1982;1:639–643. doi: 10.1016/S0140-6736(82)92200-0. [DOI] [PubMed] [Google Scholar]
- 6.Harrington W.J., Jr., Ucar A., Gill P., Snodgrass S., Sheremata W., Cabral L., Rabin M., Byrne G.E., Jr., Berger J., Voight W., et al. Clinical spectrum of HTLV-I in south Florida. J. Acquir. Immune Defic. Syndr. Hum. Retrovirology. 1995;8:466–473. doi: 10.1097/00042560-199504120-00006. [DOI] [PubMed] [Google Scholar]
- 7.Afonso P.V., Cassar O., Gessain A. Molecular epidemiology, genetic variability and evolution of HTLV-1 with special emphasis on African genotypes. Retrovirology. 2019;16:39. doi: 10.1186/s12977-019-0504-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cassar O., Einsiedel L., Afonso P.V., Gessain A. Human T-cell lymphotropic virus type 1 subtype c molecular variants among indigenous Australians: New insights into the molecular epidemiology of HTLV-1 in Australo-melanesia. PLoS Neglected Trop. Dis. 2013;7:e2418. doi: 10.1371/journal.pntd.0002418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Percher F., Jeannin P., Martin-Latil S., Gessain A., Afonso P.V., Vidy-Roche A., Ceccaldi P.-E. Mother-to-Child Transmission of HTLV-1 Epidemiological Aspects, Mechanisms and Determinants of Mother-to-Child Transmission. Viruses. 2016;8:40. doi: 10.3390/v8020040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roucoux D.F., Wang B., Smith D., Nass C.C., Smith J., Hutching S.T., Newman B., Lee T., Chafets D.M., Murphy E.L., et al. A prospective study of sexual transmission of human T lymphotropic virus (HTLV)–I and HTLV-II. J. Infect. Dis. 2005;191:1490–1497. doi: 10.1086/429410. [DOI] [PubMed] [Google Scholar]
- 11.Murphy E. Infection with human T-lymphotropic virus types-1 and -2 (HTLV-1 and -2): Implications for blood transfusion safety. Transfus. Clin. Biol. 2016;23:13–19. doi: 10.1016/j.tracli.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rowhani-Rahbar A., Tabatabee-Yazdi A., Panahi M. Prevalence of common blood-borne infections among imprisoned injection drug users in Mashhad, North-East of Iran. Arch. Iran. Med. 2004;7:190–194. [Google Scholar]
- 13.Proietti F.A., Carneiro-Proietti AB F., Catalan-Soares B.C., Murphy E.L. Global epidemiology of HTLV-I infection and associated diseases. Oncogene. 2005;24:6058–6068. doi: 10.1038/sj.onc.1208968. [DOI] [PubMed] [Google Scholar]
- 14.Schierhout G., McGregor S., Gessain A., Einsiedel L., Martinello M., Kaldor J. Association between HTLV-1 infection and adverse health outcomes: A systematic review and meta-analysis of epidemiological studies. Lancet Infect. Dis. 2019;20:133–143. doi: 10.1016/S1473-3099(19)30402-5. [DOI] [PubMed] [Google Scholar]
- 15.Keikha M., Karbalaei M. Overview on coinfection of HTLV-1 and tuberculosis: Mini-review. J. Clin. Tuberc. Other Mycobact. Dis. 2021;23:100224. doi: 10.1016/j.jctube.2021.100224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Page J.B., Lai S.H., Chitwood D.D., Klimas N.G., Smith P.C., Fletcher M.A. HTLV-I/II seropositivity and death from AIDS among HIV-1 seropositive intravenous drug users. Lancet. 1990;335:1439–1441. doi: 10.1016/0140-6736(90)91456-K. [DOI] [PubMed] [Google Scholar]
- 17.World Health Organization . Human T-Lymphotropic Virus Type 1: Technical Report. World Health Organization; Geneva, Switzerland: 2021. [Google Scholar]
- 18.World Health Organization Regional Office for the Eastern Mediterranean. [(accessed on 15 May 2021)]. Available online: http://www.emro.who.int/countries.html.
- 19.Azarpazhooh M.R., Hasanpour K., Ghanbari M., Rezaee S.R., Mashkani B., Hedayati-Moghaddam M.R., Valizadeh N., Hosseini R.F., Foroghipoor M., Soltanifar A., et al. Human T-lymphotropic virus type 1 prevalence in northeastern Iran, Sabzevar: An epidemiologic-based study and phylogenetic analysis. AIDS Res. Hum. Retrovir. 2012;28:1095–1101. doi: 10.1089/aid.2011.0248. [DOI] [PubMed] [Google Scholar]
- 20.Kalavi K., Moradi A., Tabarraei A. Population-based Seroprevalence of HTLV-I Infection in Golestan Province, South East of Caspian Sea, Iran. Iran J. Basic Med. Sci. 2013;16:225–228. [PMC free article] [PubMed] [Google Scholar]
- 21.Rafatpanah H., Hedayati-Moghaddam M.R., Fathimoghadam F., Bidkhori H.R., Shamsian S.K., Ahmadi S., Sohgandi L., Azarpazhooh M.R., Rezaee S.A., Farid R., et al. High prevalence of HTLV-I infection in Mashhad, Northeast Iran: A population-based seroepidemiology survey. J. Clin. Virol. 2011;52:172–176. doi: 10.1016/j.jcv.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 22.Rafatpanah H., Torkamani M., Valizadeh N., Vakili R., Meshkani B., Khademi H., Gerayli S., Mozhgani S.H.R., Rezaee S.A. Prevalence and phylogenetic analysis of HTLV-1 in a segregated population in Iran. J. Med. Virol. 2016;88:1247–1253. doi: 10.1002/jmv.24448. [DOI] [PubMed] [Google Scholar]
- 23.Yousefi M., Sharifzadeh G.R., Ebrahimzadeh A., Azarkar Z., Namaei M.H., Azarkar G., Ghezeldasht S.A., Rezaee R., Zare N.V., Mosavat A., et al. Prevalence and Associated Risk Factors of HTLV-1 and Co-infections of Blood-Borne Viruses in Birjand, Iran’s Eastern Border. Arch. Iran. Med. 2020;23:672–677. doi: 10.34172/aim.2020.85. [DOI] [PubMed] [Google Scholar]
- 24.Farid Hoseini R., Parizadeh M., Ghafari J., Miri S., Nasirian A., Rafatpanah H. Seroepidemiology of HTLV-1 infection in Neyshabour. Med. J. Mashad Univ. Med. Sci. 2005;47:417–424. (In Persian) [Google Scholar]
- 25.Rezvan H., Ahmadi J., Farhadi M. A cluster of HTLV1 infection in northeastern of Iran. Transfus. Today. 1996;27:8–9. [Google Scholar]
- 26.Safai B., Huang J.-L., Boeri E., Farid R., Raafat J., Schutzer P., Ahkami R., Franchini G. Prevalence of HTLV Type I Infection in Iran: A Serological and Genetic Study. AIDS Res. Hum. Retrovir. 1996;12:1185–1190. doi: 10.1089/aid.1996.12.1185. [DOI] [PubMed] [Google Scholar]
- 27.Hedayati-Moghaddam M.R., Fathimoghadam F., Eftekharzadeh Mashhadi I., Soghandi L., Bidkhori H.R. Epidemiology of HTLV-1 in Neyshabour, Northeast of Iran. Iran. Red Crescent Med. J. 2011;13:424–427. [PMC free article] [PubMed] [Google Scholar]
- 28.Keramati M.R., Sadeghian M.H., Ayatollahi H. Clinical and laboratory features in adult T-cell leukemia/lymphoma in Khorasan, Iran. Leuk. Lymphoma. 2010;51:727–729. doi: 10.3109/10428191003611436. [DOI] [PubMed] [Google Scholar]
- 29.Shoeibi A., Rafatpanah H., Azarpazhooh A., Mokhber N., Hedayati-Moghaddam M.R., Amiri A., Hashemi P., Foroghipour M., Hoseini R.F., Bazarbachi A., et al. Clinical features of HTLV-1-associated myelopathy/tropical spastic paraparesis (HAM/TSP) in northeast Iran. Acta Neurol. Belg. 2013;113:427–433. doi: 10.1007/s13760-013-0194-6. [DOI] [PubMed] [Google Scholar]
- 30.Darroudi S., Abolbashari S., Ahangari N., Tayefi M., Khashyarmanesh Z., Zamani P., Haghighi H.M., Mohammadpour A.H., Tavalaei S., Esmaily H., et al. Association Between Trace Element Status and Depression in HTLV-1-Infected Patients: A Retrospective Cohort Study. Biol. Trace Element Res. 2019;191:75–80. doi: 10.1007/s12011-018-1613-6. [DOI] [PubMed] [Google Scholar]
- 31.Karimi G., Zadsar M., Pourfathollah A.A. Seroprevalence and geographical distribution of human T-lymphotropic virus type 1 among volunteer blood donors in endemic areas of Iran. Virol. J. 2017;14:14. doi: 10.1186/s12985-017-0693-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Omidkhoda A., Razi B., Arabkhazaeli A., Kafi-Abad S.A. Trends and epidemiological analysis of hepatitis B virus, hepatitis C virus, human immunodeficiency virus, and human T-cell lymphotropic virus among Iranian blood donors: Strategies for improving blood safety. BMC Infect. Dis. 2020;20:736. doi: 10.1186/s12879-020-05405-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poukarim M.R., Khamisipour G., Zandi K., Roustaee M.H. Prevalence of anti-HTLV-I & anti- HTLV-II antibodies in blood donors in Bushehr province. Iran South Med. J. 2004;6:161–164. (In Persian) [Google Scholar]
- 34.Karimi A., Nafici M., Imani R. Comparison of human T-cell leukemia virus type-1 [HTLV-1]seroprevalence in high risk patients [thalassemia and hemodialysis]and healthy individuals from charmahal-Bakhtiari province, Iran. KMJ-Kuwait Med. J. 2007;39:259–261. [Google Scholar]
- 35.Arjmandi F., Shahriari M., Sadeghi Hasanabadi A. A comparitive study of the prevalence of HTLV–I infection in luekemia/ non–hodgkins lymphoma patients, thalassemic patients and blood donors. J. Shahid Sadoughi Univ. Med. Sci. 2003;10:25–29. [Google Scholar]
- 36.Habibabadi H.M., Parsania M., Pourfathollah A.A., Bahrami A., Sharifi Z. Prevalence and phylogenetic analysis of HTLV-1 in blood donors in Golestan Province, in the Northeast of Iran. J. Virol. Methods. 2021;290:114073. doi: 10.1016/j.jviromet.2021.114073. [DOI] [PubMed] [Google Scholar]
- 37.Abedi F., Yavarian M., Shakibzadeh A., Khalvati B., Asadi A. A pilot Seroepidemiologic study of HTLV in thalassemia, hemophilia, and hemodialysed patients in Hormozgan. Hormozgan Med. J. 2009;13:e88635. [Google Scholar]
- 38.Zalei B., Pourmand D., Rahmani Y., Bilvaye S. Investigating the prevalence of HTLV and HCV infection in blood donors (for the first time) in blood transfusion organization of Kermanshah, Iran. Ann. Clin. Anal. Med. 2017;8:509–512. doi: 10.4328/jcam.5540. [DOI] [Google Scholar]
- 39.Ghadiri K., Hashemian A., Rezaei M., Payandeh M., Zare M.E. Serologic prevalence of human T-lymphotropic virus (HTLV) among major thalassemic patients in Kermanshah 2010. Int. J. Hematol.-Oncol. Stem Cell Res. 2011;5:14–17. [Google Scholar]
- 40.Yahyapour Y., Aghajanipour K., Mir S.M., Khademian A., Sadeghi F. Human T- Lymphotropic Virus Type 1 in Blood Donors from Babol County Blood Transfusion Center: A Pilot Study From Northern Iran. Jundishapur J. Microbiol. 2017;10:e13757. doi: 10.5812/jjm.13757. [DOI] [Google Scholar]
- 41.Tarhini M., Kchour G., Zanjani D.S., Rafatpanah H., Otrock Z.K., Bazarbachi A., Farid R. Declining tendency of human T-cell leukaemia virus type I carrier rates among blood donors in Mashhad, Iran. Pathology. 2009;41:498–499. doi: 10.1080/00313020903041010. [DOI] [PubMed] [Google Scholar]
- 42.Hatami H., Karimi G., Safabakhsh H.R. Seroepidemiologic prevalence of HTLV in voluntary blood donors in Mashhad. Sci. J. Iran. Blood Transfus. Organ. 2012;9:149–159. [Google Scholar]
- 43.Sayadpour Zanjani D., Shahabi M., Talaei N., Afzalaghaee M., Tehranian F., Bazargani R. Molecular Analysis of Human T Cell Lymphotropic Virus Type 1 and 2 (HTLV-1/2) Seroindeterminate Blood Donors from Northeast Iran: Evidence of Proviral tax, env, and gag Sequences. AIDS Res. Hum. Retrovir. 2011;27:131–135. doi: 10.1089/aid.2010.0017. [DOI] [PubMed] [Google Scholar]
- 44.Safabakhsh H.r., Karimi G., Hatami H. The prevalence of HTLV-1 infection in blood donation volunteers in Mashhad. J. Sch. Public Health Inst. Public Health Res. 2014;11:85–94. [Google Scholar]
- 45.Tabriznia Tabrizi S., Gholampour M., Zarmehri A.M., Sadeghian M.H., Keramati M.R. The frequency and risk factors of human T-cell lymphotropic virus type I among blood donors in Khorasan-e Razavi, Iran, from 2002 to 2013. Niger. Med. J. Niger. Med. Assoc. 2020;61:151–155. doi: 10.4103/nmj.nmj_127_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Safabakhsh H., Jalalian M., Karimi G. Seroepidemiology of human T-Cell lymphotropic virus Type-1 (HTLV1) in mashhad. Glob. J. Health Sci. 2014;6:99–104. doi: 10.5539/gjhs.v6n5p99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maghsudlu M., Safabakhsh H., Jamili P. Seroepidemiology of human T-cell lymphotropic virus type-I in blood donors of Northeastern Iran, Sabzevar. Asian J. Transfus. Sci. 2015;9:203–206. doi: 10.4103/0973-6247.154255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ferdowsi S., Najafzadeh M., Ameli M.R., Sajjadi S.M. Evaluating the Frequency of Human T-Lymphotropic Virus Type 1 Infection in Iranian Population. Iran. J. Blood Cancer. 2019;11:47–50. [Google Scholar]
- 49.Pirayeshfard L., Sharifi Z., Amini-Kafiabad S., Sadaghiani N.H. Phylogenetic analysis of HTLV-1 in Iranian blood donors, HIV-1 positive patients and patients with beta thalassemia. J. Med. Virol. 2018;90:1398–1405. doi: 10.1002/jmv.25192. [DOI] [PubMed] [Google Scholar]
- 50.Rostamzadeh Khameneh Z., Baradaran M., Sepehrvand N. Survey of the seroprovalence of HTLV I/II in hemodialysis patients and blood donors in Urmia. Saudi J. Kidney Dis. Transplant. Off. Publ. Saudi Cent. Organ Transplant. Saudi Arab. 2008;19:838–841. [PubMed] [Google Scholar]
- 51.Emadi B., Rezaieh M.G., Sedighi M. Seroprevalence and trends of transfusion transmissible infections among retrospective blood donors in Western Azerbaijan Regional Blood Transfusion Center, Iran: A ten-years evaluation. Transfus. Apher. Sci. Off. J. World Apher. Assoc. Off. J. Eur. Soc. Haemapheresis. 2021;60:103132. doi: 10.1016/j.transci.2021.103132. [DOI] [PubMed] [Google Scholar]
- 52.Rezaei Kanavi M., Javadi M., Nazparvar B., Bayat Makoo K. Seropositivity for human T-cell lymphotropic virus [HTL V] in donors at the eye bank of I.R. Iran. Bina J. Ohthalmol. 2008;14:40–43. [Google Scholar]
- 53.Arjmand B., Aghayan S.H., Goodarzi P., Farzanehkhah M., Mortazavi S.M., Nicknam M.H., Jafarian A., Arjmand F., Far S.J. Seroprevalence of human T lymphtropic virus (HTLV) among tissue donors in Iranian tissue bank. Cell Tissue Bank. 2008;10:247–252. doi: 10.1007/s10561-008-9117-9. [DOI] [PubMed] [Google Scholar]
- 54.Hamedi A., Akhlaghi F., Meshkat Z., Sezavar M., Nomani H. The Prevalence of Human T-Cell lymphotropic Virus Type 1 in Pregnant Women and Their Newborns. ISRN Obstet. Gynecol. 2012;2012:975135. doi: 10.5402/2012/975135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Salehi M., Mostafavi S.K.S., Ghasemian A., Gholami M., Kazemi-Vardanjani A., Rahimi M.K. Seroepidemiology of HTLV-1 and HTLV-2 Infection in Neyshabur City, North-Eastern Iran, during 2010–2014. Iran. Biomed. J. 2017;21:57–60. doi: 10.18869/acadpub.ibj.21.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Salehi M., Mobini M. The seroepidemiological of Human T-lymphotropic virus on children, teenage and juveniles in Nyshabor city. Iran. J. Med. Microbiol. 2015;9:31–35. [Google Scholar]
- 57.Mobini M., Salehi M. Prevalence of Human T-cell Leukemia Virus Antibodies among Young Females Attending a Large Medical Diagnostic Laboratory in Neyshabour, Northeast of Iran, During 2011 to 2015. Arch. Clin. Infect. Dis. 2018;13:e62305. doi: 10.5812/archcid.62305. [DOI] [Google Scholar]
- 58.Ghaffari J., Naghshvar F., Nazari Z., Farid R. Seroprevalence of human T-cell lymphotropic virus type 1 infection (HTLV1) in different patients in the north of Iran. Afr. J. Biotechnol. 2011;10:10752–10755. doi: 10.5897/AJB11.177. [DOI] [Google Scholar]
- 59.Ghodsi A., Jamehdar S.A., Hamedi A.K. Frequency of HTLV-1 Antibody in Children of 6 Months to 14 Years old Hospitalized in the Pediatric Ward of Imam Reza Hospital, Mashhad, Iran. Int. J. Pediatrics-Mashhad. 2021;9:12975–12980. doi: 10.22038/IJP.2020.54237.4289. [DOI] [Google Scholar]
- 60.Tahaei S.M.E., Mohebbi S.R., Fatemi S.R., Azimzadeh P., Mirsattari D., Sanati A., Sharifian A. Evaluation of antibody frequency against HBV, HCV and HTLV-1. Gastroenterol. Hepatol. Bed Bench. 2012;5:161–165. [PMC free article] [PubMed] [Google Scholar]
- 61.Razavi Pashabayg C., Momenifar N., Malekpour S.A., Sadeghi M., Foroushani A.R., Rafatpanah H., Valizadeh N., Sabet F., Jazayeri S.M., Keyvani H., et al. Phylogenetic and phylodynamic study of Human T-cell lymphotropic virus Type 1 (HTLV-1) in Iran. Infect. Genet. Evol. 2020;85:104426. doi: 10.1016/j.meegid.2020.104426. [DOI] [PubMed] [Google Scholar]
- 62.Hedayati-Moghaddam M.R. A Systematic Review for Estimation of HTLV-I Infection in the Blood Donors of Iran. Iran. J. Basic Med. Sci. 2013;16:196–201. doi: 10.22038/IJBMS.2013.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Azami M., Badfar G., Esmaeli E., Moslemirad M., Rahmati S. Epidemiology of human T-lymphotropic virus type 1 among blood donors and general population in Iran: A meta-analysis. Futur. Virol. 2018;13:585–599. doi: 10.2217/fvl-2018-0015. [DOI] [Google Scholar]
- 64.Rezvan H., Abolghassemi H., Kafiabad S.A. Transfusion-transmitted infections among multitransfused patients in Iran: A review. Transfus. Med. 2007;17:425–433. doi: 10.1111/j.1365-3148.2007.00794.x. [DOI] [PubMed] [Google Scholar]
- 65.Hedayati-Moghaddam M.R., Tehranian F., Bayati M. Human T-Lymphotropic Virus Type I (HTLV-1) Infection among Iranian Blood Donors: First Case-Control Study on the Risk Factors. Viruses. 2015;7:5736–5745. doi: 10.3390/v7112904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Dayyani M., Hedayati-Moghaddam M.R., Amini A.R. HTLV-1 infection as a serious health issue among iranian multi-transfused patients: Evidence from a systematic review and meta-analysis. Iran. J. Blood Cancer. 2015;7:85–94. [Google Scholar]
- 67.Ahmadi Ghezeldasht S., Hassannia T., Rafatpanah H., Hekmat R., Valizadeh N., Mobarhan M.G., Rezaee S.A. Oncogenic Virus Infections in the General Population and End-stage Renal Disease Patients with Special Emphasis on Kaposi’s Sarcoma Associated Herpes Virus (KSHV) in Northeast of Iran. Jundishapur J. Microbiol. 2015;8:e14920. doi: 10.5812/jjm.14920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hedayati-Moghaddam M.R., Fathimoghadam F., Soghandi L., Darrudi A. High Prevalence of HTLV-1 Infection Among Hemodialysis Patients in Neyshabur, Northeast of Iran. Int. J. Infect. 2019;6:e85164. doi: 10.5812/iji.85164. [DOI] [Google Scholar]
- 69.Karimi A., Nafisi M. Seroprevalence of Human T-Cell Leukemia Virus Type-1 (HTLV-1) in High Risk Patients. J. Res. Health Sci. 2006;6:44–47. [Google Scholar]
- 70.Anaraki Mohammadi G., Sadeghipour A.R., Vossough P., Nour Mohammadi I., Mirnateghi A.M. Assessment of the Prevalence of Human T-Lymphotropic Virus type 1 among Thalassemic Patients with Frequent Blood Transfusion in Tehran in 2003. Razi J. Med. Sci. 2005;12:19–24. [Google Scholar]
- 71.Keshvari M., Hajibeigi B., Azarkeivan A., Keyvani H., Behnava B., Hosseini S.Y.S., Sharafi H., Alavian S.M. Seroepidemiology of human T-cell lymphotropic virus among Iranian adult thalassemic patients. Transfus. Med. 2014;24:227–232. doi: 10.1111/tme.12133. [DOI] [PubMed] [Google Scholar]
- 72.Abbasnia S., Hassannia T., Ariaee N., Sabet F., Pashabayg K.R., Keyvani H., Sarv-Ghad M.R., Ziaeemehr A., Fakor F., Valizadeh N. Immunovirological Assessment of HIV-Infected Patients and Phylogenetic Analysis of the Virus in Northeast of Iran. Jundishapur J. Microbiol. 2021;14:e112123. doi: 10.5812/jjm.112123. [DOI] [Google Scholar]
- 73.Alavi S.M., Etemadi A. HIV/HBV, HIV/HCV and HIV/HTLV-1 Co infection among injecting drug user patients hospitalized at the infectious disease ward of a training hospital in Iran. Pak. J. Med. Sci. 2007;23:510–513. [Google Scholar]
- 74.Khajedaluee M., Babaei A., Vakili R., Valizade N., Shandiz F.H., Alavian S.M., Nozadi M.S., Jazayeri S.M., Hassannia T. Sero-Prevalence of Bloodborne Tumor Viruses (HCV, HBV, HTLV-I and KSHV Infections) and Related Risk Factors among Prisoners in Razavi Khorasan Province, Iran, in 2008. Hepat. Mon. 2016;16:e31541. doi: 10.5812/hepatmon.31541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Centers for Disease Control and Prevention and the U.S.P.H.S. Working Group. Guidelines for counseling persons infected with human T-lymphotropic virus type I (HTLV-I) and type II (HTLV-II) Ann. Intern. Med. 1993;118:448–454. doi: 10.7326/0003-4819-118-6-199303150-00009. [DOI] [PubMed] [Google Scholar]
- 76.Pourkarim M., Khamisipour G., Hajiani G., Tahmasebi R., Ardeshirdavani N. Seroepidemiological investigation of HTLV I, II infection among Busherian multi-transfused patients in 2003. Sci. J. Iran. Blood Transfus. Organ. 2005;2:99–104. [Google Scholar]
- 77.Ardalan N., Abdi M., Zarif B.R., Amini A., Meamari F., Haydari E., Ahmadi A. Prevalence of human T-lymphotropic virus types I & II among high risk groups in Sanandaj in 2010. Sci. J. Kurd. Univ. Med. Sci. 2013;18:51–57. [Google Scholar]
- 78.Ghaffari J., Ebrahimi M., Makhlough A., Mohammadjafari H., Nazari Z. Seroepidemiology of human T-cell lymphotropic virus 1 infection in hemodialysis patients: Should we be concerned about it? Iran. J. Kidney Dis. 2013;7:187–190. [PubMed] [Google Scholar]
- 79.Ziaee M., Azizee R., Namaei M.H., Masood Z., Roghiya A., Hasan N. Prevalence of HCV infection in hemodialysis patients of South Khorasan in comparison with HBV, HDV, HTLV I/II, And HIV infection. Bangladesh J. Med. Sci. 2013;13:36–39. doi: 10.3329/bjms.v13i1.13903. [DOI] [Google Scholar]
- 80.Yazdani R., Dadmanesh M., Ghorban K. First Report of the Prevalence of Human T-Lymphotropic Virus Type 1 (HTLV-1) for Hemodialysis Patients in Tehran. Arch. Clin. Infect. Dis. 2018;13:e65512. doi: 10.5812/archcid.65512. [DOI] [Google Scholar]
- 81.Hatatian F., Babakhani F., Gudarzi H., Momenifar N., Norouzi M., Shafieifar M., Kakavandi E., Sadeghi A., Sharbatdar-Alaei H., Farahmand M., et al. Relative Frequency of Blood-Borne Viruses in Hemodialysis-Dependent and Kidney Transplant Recipients in Iran. Iran. J. Public Health. 2020;49:2136–2143. doi: 10.18502/ijph.v49i11.4731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Moradi A., Mansurian A., Ahmadi A., Ghaemi E.A., Kalavi K., Marjani A., Moghaddam E.S. Prevalence of HTLV-1 Antibody among Major Thalassemic Patients in Gorgan (South East of Caspian Sea) J. Appl. Sci. 2008;8:391–393. doi: 10.3923/jas.2008.391.393. [DOI] [Google Scholar]
- 83.Mortezaie Z., Bouzari M., Roghanian R. Evaluating the frequency of HTLV-I/Π infection among blood donors, major thalassemic patients and individuals infected with hepatitis B and C viruses in Isfahan, Iran. Iran. J. Blood Cancer. 2012;4:75–80. [Google Scholar]
- 84.Mahzounieh M., Ghorani M., Karimi A., Pourgheysari B., Nikoozad R. Prevalence of Human T-Lymphotropic Virus Types I and II in Patients with Hematological Disorders in Isfahan, Iran. Jundishapur J. Microbiol. 2015;8:e17201. doi: 10.5812/jjm.8(5)2015.17201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ghaffari J., Kowsarian M., Mahdavi M., Shahi K.V., Rafatpanah H., Tafreshian A. Prevalence of HTLV-I Infection in Patients with Thalassemia Major in Mazandaran, North of Iran. Jundishapur J. Microbiol. 2012;6:57–60. doi: 10.5812/jjm.4702. [DOI] [Google Scholar]
- 86.Hamidi S., Bashizadeh-Fakhar H., Nazemi A. Identification of Human T-Cell Lymphotropic Virus Type 1 Pro-Invasion in Patients with β-Thalassemia Major Using TaqMan Real-Time PCR in Tonekabon, Iran. Zahedan J. Res. Med. Sci. 2018;20:e59961. doi: 10.5812/zjrms.59961. [DOI] [Google Scholar]
- 87.Mansouritorghabeh H., Badiei Z. Transfusion-Transmitted Viruses in Individuals with β Thalassemia Major at Northeastern Iran, a Retrospective Sero-Epidemiological Survey. Iran. J. Blood Cancer. 2008;1:1–4. [Google Scholar]
- 88.Abedi F., Mozhgani S.-H., Rahimzadegan M., Gudarzi H., Valizadeh N., Rezaee S.A. Prevalence and phylogenic study of human T-lymphotropic virus 1 in patients with thalassemia in the northeast of Iran. Futur. Virol. 2017;12:253–258. doi: 10.2217/fvl-2016-0107. [DOI] [Google Scholar]
- 89.Ziaee M., Zarban A., Malekinejad P., Akhbary H. Evaluation of HGV viremia prevalence and its co-infection with HBV, HCV, HIV and HTLV-1 in hemophilic patients of southern Khorassan, Iran. Hepat. Mon. 2007;7:11–14. [Google Scholar]
- 90.Ziaee M., Namaei M.H., Azarkar G. The prevalence of HTLV-1 and its Co-Infection with HCV, HBV and HIV in Hemophilic patients. Pak. J. Med. Sci. 2015;31:1246–1249. doi: 10.12669/pjms.315.7888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Rostamzadeh Z., Valizadeh N., Mohammadian M. Prevalence of Seropositivity for Human T lymphocytes Virus in Patients with Hereditary Bleeding Diseases in Population of West Azerbaijan. Int. J. Med. Lab. 2016;3:159–162. [Google Scholar]
- 92.Mansouritorghabeh H., Farid Hosseini R., Pourfath Elah A.A., Behjati A.A. Serological markers of blood borne viruses among persons with combined factor V & VIII deficiency. Hepat. Mon. 2008;8:221–224. [Google Scholar]
- 93.Meidani M., Ahmadi N., Jamali B., Askarian Z. Relative frequency of Human T-cell Lymphotropic Virus I/II in HIV/AIDS patients. Adv. Biomed. Res. 2014;3:8. doi: 10.4103/2277-9175.124635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Meidani M., Farzaneh S., Baferani A., Zade A. [Seroprevalence of HTLV1, 2 virus among injection drug addicts in Isfahan, 2007–2008] J. Shaheed Sadoughi Univ. Med. Sci. 2009;17:286–290. [Google Scholar]
- 95.Tavanaee Sani A., Khaleghinia M. Epidemiologic evaluation and some species in injection drug users that admitted in infectious department of Imam Reza hospital [2007–2009] J. Med. Counc. Iran. 2012;30:155–161. [Google Scholar]
- 96.Ramezani A., Aghakhani A., Banifazl M., Boland-Ghamat Z., Foroughi M., Gachkar L., Khadem-Sadegh A., Mohraz M. Frequency of human T-Cell lymphotropic virus (HTLV) type 1 and 2 infection in HIV infected patients. Iran. J. Pathol. 2012;7:9–13. [Google Scholar]
- 97.Abedi F., Saeedi E., Sharifzadeh G.R., Ziaee M. Comparing the Prevalence of HTLV-1 and Its Risk Factors in Prisoners with Intravenous and Non-Intravenous Drug Use in Birjand. Mod. Care J. 2019;16:e95601. doi: 10.5812/modernc.95601. [DOI] [Google Scholar]
- 98.Rafatpanah H., Hedayati-Moghaddam M.R., Fathimoghadam F., Bidkhori H.R., Shamsian S.K., Ahmadi S., Sohgandi L., Azarpazhooh M.R., Rezaee S.A., Farid R., et al. Prevalence of human T-cell lymphotropic virus type 2 infection in general population of Mashhad, Iran. J. Isfahan Med. Sch. 2015;32:2260–2267. [Google Scholar]
- 99.Rafatpanah H., Fathimoghadam F., Shahabi M., Eftekharzadeh I., Hedayati-Moghaddam M., Valizadeh N., Tadayon M., Shamsian S.A., Bidkhori H., Miri R., et al. No Evidence of HTLV-II Infection Among Immonoblot Indeterminate Samples Using Nested PCR in Mashhad, Northeast of Iran. Iran J. Basic Med. Sci. 2013;16:229–234. [PMC free article] [PubMed] [Google Scholar]
- 100.Lowis G. Epidemiologic Features of HTLV-II Serologic and Molecular Evidence. Ann. Epidemiol. 2002;12:46–66. doi: 10.1016/S1047-2797(01)00231-9. [DOI] [PubMed] [Google Scholar]
- 101.Husseini A.A., Saeed K.M.I., Yurdcu E., Sertoz R., Bozdayi A.M. Epidemiology of blood-borne viral infections in Afghanistan. Arch. Virol. 2019;164:2083–2090. doi: 10.1007/s00705-019-04285-y. [DOI] [PubMed] [Google Scholar]
- 102.Mousavi S.H., Khairkhah N., Bahri T.D., Anvar A., Saraji A.A., Behnava B., Alavian S.M., Namvar A. First Report of Prevalence of Blood-Borne Viruses (HBV, HCV, HIV, HTLV-1 and Parvovirus B19) Among Hemophilia Patients in Afghanistan. Sci. Rep. 2019;9:7259. doi: 10.1038/s41598-019-43541-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zaki S.M., Darwish M.M., Mahmoud M.H. Sporadic carriers of human T-cell lymphotropic virus type 1 among blood donors in Egypt. Egypt. J. Med. Lab. Sci. 2007;16:77–87. [Google Scholar]
- 104.Ibrahim A.I., Al-Musawi Y.A., Abdullah A.I. Seroprevalence of HTLV-type-1 and type-2 among Blood Donors in Some Iraqi Provinces. Indian J. Forensic Med. Toxicol. 2020;14:2179–2184. doi: 10.37506/ijfmt.v14i4.11874. [DOI] [Google Scholar]
- 105.Souan L., Tout F., Siag M., Sughayer M.A. Seroprevalence rates of transfusion-transmitted infections among blood donors in Jordan. J. Infect. Dev. Ctries. 2016;10:377–383. doi: 10.3855/jidc.8160. [DOI] [PubMed] [Google Scholar]
- 106.Ameen R., Sanad N., Al-Shemmari S., Siddique I., Chowdhury R.I., Al-Hamdan S., Al-Bashir A. Prevalence of viral markers among first-time Arab blood donors in Kuwait. Transfusion. 2005;45:1973–1980. doi: 10.1111/j.1537-2995.2005.00635.x. [DOI] [PubMed] [Google Scholar]
- 107.Ramia S., Klayme S., Naman R. Infection with hepatitis B and C viruses and human retroviruses (HTLV-I and HIV) among high-risk Lebanese patients. Ann. Trop. Med. Parasitol. 2003;97:187–192. doi: 10.1179/000349803235001363. [DOI] [PubMed] [Google Scholar]
- 108.Tamim H., Musharrafieh U., Ramia S., Almawi W.Y., Al-Jisr T., Ayoub T., Nabulsi-Majzoub M., Kazma H., Baz E.K. Is seroprevalence of HTLV-I/II among blood donors in Lebanon relevant? Am. J. Infect. Control. 2004;32:220–223. doi: 10.1016/j.ajic.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 109.Fawzi Z.O., Al Malki A., Al Mutawa H. Prevalence of Human T-Lymphotropic Virus (HTLV) Antibodies Among the Donor Population in the State of Qatar. Qatar Med. J. 2006;2006:9. doi: 10.5339/qmj.2006.2.9. [DOI] [Google Scholar]
- 110.Aabdien M., Selim N., Himatt S., Hmissi S., Merenkov Z., AlKubaisi N., Abdel-Rahman M., Abdelmola A., Khelfa S., Farag E., et al. Prevalence and trends of transfusion transmissible infections among blood donors in the State of Qatar, 2013–2017. BMC Infect. Dis. 2020;20:617. doi: 10.1186/s12879-020-05344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Niazi S.K., Bhatti F.A., Salamat N. Seroprevalence of Human T-Cell Lymphotropic Virus-1/2 in Blood Donors in Northern Pakistan: Implications for Blood Donor Screening. J. Coll. Physicians Surg. Pak. JCPSP. 2015;25:874–877. [PubMed] [Google Scholar]
- 112.Taha M.A., Bashawri L.A., Ahmed M.S., Ahmed M.A. Prevalence of antibodies to human T-lymphotropic viruses types I and II among healthy blood donors. Saudi Med. J. 2003;24:637–640. [PubMed] [Google Scholar]
- 113.Fawaz N., Tamim H., Almawi W. Low prevalence of antibodies to human T-lymphotropic virus-I/II among blood donors in Eastern Saudi Arabia. Am. J. Infect. Control. 2005;33:189–191. doi: 10.1016/j.ajic.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 114.Balkhy H.H., Memish Z.A., Abed E., Qasem L., Bin Amer A., Masoud S., Hajeer A.H. Saudi national guard donor screening for human T cell lymphotropic virus I/II: Time to use molecular biology techniques. Mil. Med. 2004;169:251–253. doi: 10.7205/MILMED.169.3.251. [DOI] [PubMed] [Google Scholar]
- 115.El-Hazmi M. Prevalence of HBV, HCV, HIV-1, 2 and HTLV-I/II infections among blood donors in a teaching hospital in the Central region of Saudi Arabia. Saudi Med. J. 2004;25:26–33. [PubMed] [Google Scholar]
- 116.Ul-Hassan Z., Al-Bahrani A.T., Panhotra B.R. Prevalence of human T-lymphotropic virus type I and type II antibody among blood donors in Eastern Saudi Arabia. Saudi Med. J. 2004;25:1419–1422. [PubMed] [Google Scholar]
- 117.Kawashti M.I., Hindawi S.I., Damanhouri G.A., Rowehy N.G., Bawazeer M.M., Alshawa M. Serologial screening of human T cell lymphotropic virus I and II (HTLV I/II) in blood banks by immunoblotting and enzyme-immuno assays: To demand or to defeat? Egypt. J. Immunol. 2005;12:137–142. [PubMed] [Google Scholar]
- 118.Hindawi S., Badawi M., Fouda F., Mallah B., Rajab H., Madani T.A. Testing for HTLV 1 and HTLV 2 among blood donors in Western Saudi Arabia: Prevalence and cost considerations. Transfus. Med. 2018;28:60–64. doi: 10.1111/tme.12440. [DOI] [PubMed] [Google Scholar]
- 119.Almutairi H.H., AlAhmari M.M., Al-Zahran B.H., Abbas I.S., Al Ghamdi J.S., Raja’a Y.A., Sallam T.A. Prevalence of serological markers and nucleic acid for blood-borne viral infections in blood donors in Al-Baha, Saudi Arabia. J. Infect. Dev. Ctries. 2016;10:619–625. doi: 10.3855/jidc.6666. [DOI] [PubMed] [Google Scholar]
- 120.AlShehri A. Human T Lymphotropic Virus-I (HTLV-I), the Causative Agent of Acute T-Cell Leukaemia/Lymphoma, Is Absent among Blood Donors in Aseer Region, Saudi Arabia. J. King Abdulaziz Univ. Sci. 2014;26:35–52. doi: 10.4197/Sci.26-1.3. [DOI] [Google Scholar]
- 121.Kilany M., Bin Dajem S.M., Ibrahim Y.M., Alshehri A., Aljeamelani A.A., Ibrahim E.H. Seroprevalence of Anti-Treponemapallidum Antibodies (Syphilis) In Blood Donors in the Southern Area of Saudi Arabia. Res. J. Pharm. Biol. Chem. Sci. 2015;6:549–556. [Google Scholar]
- 122.Almaiman A.A., Almaiman S.H. Evaluation of Blood Donors and Transfusion Transmitted Infections and their Association with ABO and Rh Blood Groups in Unaizah, Saudi Arabia: A Retrospective Study. Int. J. Med. Res. Health Sci. 2018;7:143–150. [Google Scholar]
- 123.Sarah Y.A.E.G.A., Sabry A.E.G.A.E.H.E.S., Maryam A.A.-S. Seropositivity of TTIs among blood donors in Hail, Saudi Arabia, from 2014 to 2015. Asian Pac. J. Trop. Dis. 2016;6:141–146. doi: 10.1016/S2222-1808(15)61000-3. [DOI] [Google Scholar]
- 124.Alaidarous M., Choudhary R.K., Waly M.I., Mir S., Bin Dukhyil A., Banawas S.S., Alshehri B.M. The prevalence of transfusion-transmitted infections and nucleic acid testing among blood donors in Majmaah, Saudi Arabia. J. Infect. Public Health. 2018;11:702–706. doi: 10.1016/j.jiph.2018.04.008. [DOI] [PubMed] [Google Scholar]
- 125.Alabdulmonem W., Shariq A., Alqossayir F., AbaAlkhail F.M., Al-Musallam A.Y., Alzaaqi F.O., Aloqla A.A., Alodhaylah S.A., Alsugayyir A.H., Aldoubiab R.K., et al. Sero-prevalence ABO and Rh blood groups and their associated Transfusion-Transmissible Infections among Blood Donors in the Central Region of Saudi Arabia. J. Infect. Public Health. 2020;13:299–305. doi: 10.1016/j.jiph.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 126.Alshehri O.M., Nahari M.H., Hassan E.E., Alqahtani M.F., Awaji T.H. Prevalence of ABO, Rh and KELL Blood Group Types and Transfusion- Transmissible Infections (TTI) among Blood Donors in Najran City, Saudi Arabia. Biomed. Pharmacol. J. 2021;14:1065–1076. doi: 10.13005/bpj/2210. [DOI] [Google Scholar]
- 127.Bitar N., El Hajj H., Houmani Z., Sabbah A., Otrock Z.K., Mahfouz R., Zaatari G., Bazarbachi A. Adult T-cell leukemia/lymphoma in the Middle East: First report of two cases from Lebanon. Transfusion. 2009;49:1859–1864. doi: 10.1111/j.1537-2995.2009.02223.x. [DOI] [PubMed] [Google Scholar]
- 128.Cassar O., Desrames A., Marçais A., Gout O., Taylor G.P., Hermine O., Soriano V., De Mendoza C., Dehan O., Le Mener M., et al. Multiple recombinant events in human T-cell Leukemia virus Type 1: Complete sequences of recombinant African strains. Emerg. Microbes Infect. 2020;9:913–923. doi: 10.1080/22221751.2020.1752117. [DOI] [PMC free article] [PubMed] [Google Scholar]