INTRODUCTION
Acromegaly is characterized by slowly progressive somatic abnormal hyperplasia caused by overproduction of growth hormone and insulin-like growth factor 1, and is frequently associated with pituitary adenomas.1 This disorder commonly results in mandibular hyperplasia and orofacial deformities requiring surgical correction. Here, we describe a novel use of virtual surgical planning in reduction mandibuloplasty for correction of mandibular hyperplasia secondary to acromegaly.
CASE
A 25-year-old woman presented to our clinic with mandibular hyperplasia secondary to a growth-hormone secreting pituitary adenoma, consistent with facial manifestations of acromegaly. This had been treated with a combination of prior surgical resection and lanreotide. Interestingly, she presented with normal occlusion, and reported this to be at her premorbid baseline. After clearance by endocrinology, a surgical plan was developed for a reduction genioplasty and mandibuloplasty to reduce her lower facial proportions without altering her current normal occlusion.
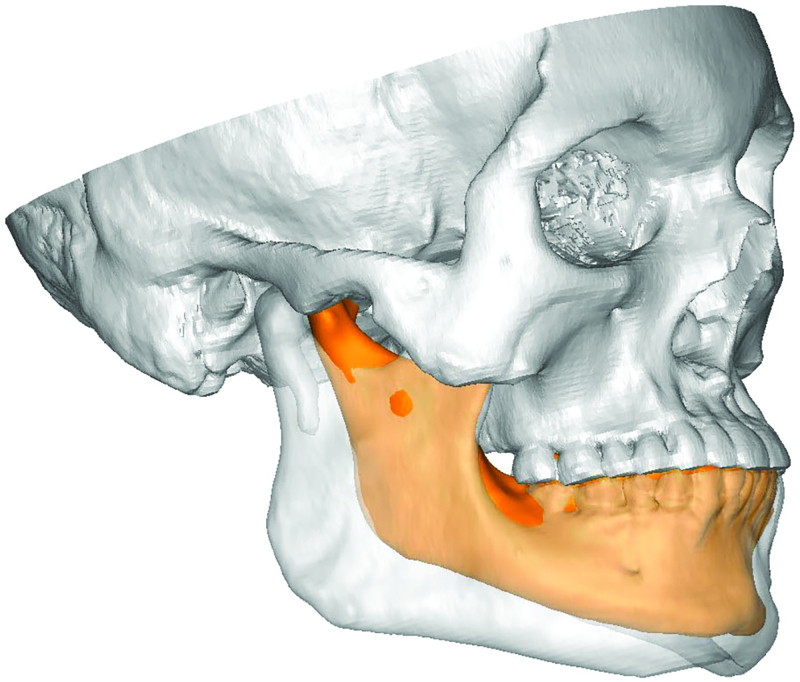
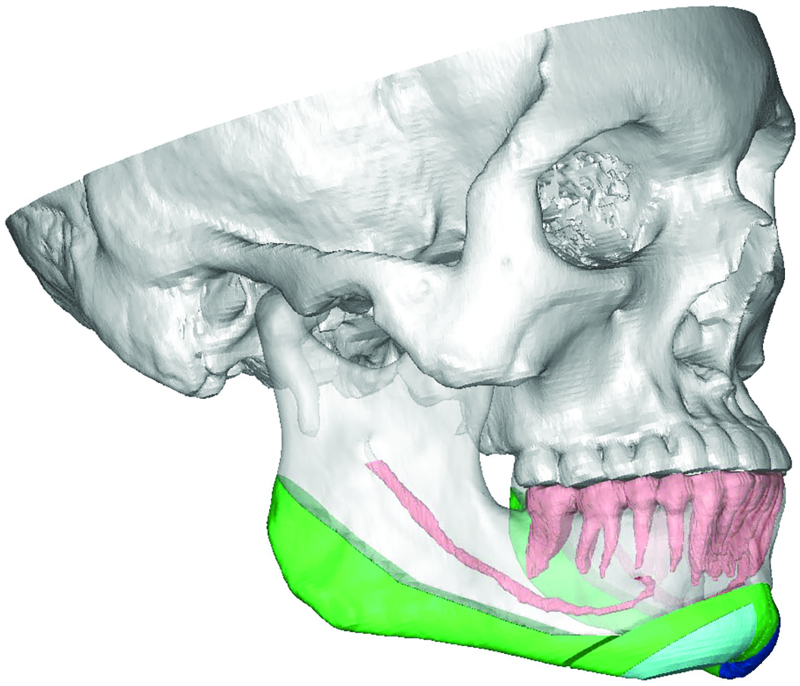
To facilitate intraoperative bone resection, virtual surgical planning (3D systems, Littleton, Colo.) was used to develop prefabricated cutting guides for reduction genioplasty, and ostectomy of the inferior border and gonial angles of the mandible. The planned degree of bone resection was facilitated during a planning session by overlay of the patient’s CT scan images with a “generic” female mandible model (Figs. 1, 2).
Fig. 1.
Virtual surgical planning was used to assist in planning ostectomies of the lower mandible for correction of mandibular hyperplasia secondary to acromegaly. Preoperative mandible (gray) interposed with a “generic” female mandible (orange).
Fig. 2.
Planned bone for resection is shown in green, and repositioned bone is shown in blue after T-shaped ostectomy to reduce the chin.
An intraoral approach was used for reduction genioplasty and mandibuloplasty, with a technique similar to that used for feminizing mandibuloplasty.5 Osseous genioplasty was performed with a T-shaped excision of the bone to allow for reduction of chin dimensions in both horizontal and vertical vectors, with reduction amounts of 12.0 mm and 7.2 mm, respectively. Rigid titanium osteosynthesis of the remaining chin segments was performed. Ostectomy of the inferior border of the mandible was continued posteriorly and included the gonial angles to further reduce mandibular proportions. A surgical drain was placed for 24 hours. Routine postoperative oral hygiene and antibiotic prophylaxis was instituted, and the patient recovered uneventfully. A postoperative CT scan demonstrated effective mandibular reduction with contours approximating those of the “generic” female mandible used for surgical planning. (See figure, Supplemental Digital Content 1, which shows a postoperative CT scan demonstrating reduced mandible proportions, mirroring those of the “generic” female mandible used for surgical planning. http://links.lww.com/PRSGO/B949.)
DISCUSSION
Acromegaly results in overgrowth of skeletal and soft tissues, with typical enlargement of the mandible being seen. The most prominent facial manifestation of acromegaly is mandibular prognathism due to excessive jaw overgrowth, and the ramus is more often affected than the body of the mandible.2,3 Patients with acromegaly typically exhibit enlargement of all parts of the neurocranium and orofacial bones, though often sparing the maxilla, and common manifestations include dental malocclusion. This often warrants orthognathic surgery for correction of associated orofacial deformities. “Horseshoe horizontal osteotomy” has also been utilized to reduce the vertical dimension of the body of the mandible.4
Interestingly, in our case, the lower facial enlargement was associated with normal occlusion, and a plan for lower mandible reduction was implemented. We found the use of virtual surgical planning in planning the appropriate osteotomies to be a useful tool in determining the degree of bone resection to mirror a “generic” female mandible proportion with a pleasing end result.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online 22 April 2022.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Holdaway IM, Rajasoorya C. Epidemiology of acromegaly. Pituitary 1999;2:29–41. [DOI] [PubMed] [Google Scholar]
- 2.Dostálová S, Sonka K, Smahel Z, et al. Cephalometric assessment of cranial abnormalities in patients with acromegaly. J Craniomaxillofac Surg. 2003;31:80–87. [DOI] [PubMed] [Google Scholar]
- 3.Chung KC, Buchman SR, Aly HM, et al. Use of modern craniofacial techniques for comprehensive reconstruction of the acromegalic face. Ann Plast Surg. 1996;36:403–8; discussion 408. [DOI] [PubMed] [Google Scholar]
- 4.Converse JM, Baker DC. Surgical correction of the facial deformities of acromegaly. Ann Plast Surg. 1978;1:612–616. [DOI] [PubMed] [Google Scholar]
- 5.Becking AG, Tuinzing DB, Hage JJ, et al. Transgender feminization of the facial skeleton. Clin Plast Surg. 2007;34:557–564. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.