Abstract
Storage mites (SM) may induce allergic respiratory symptoms in sensitized individuals, in both rural and urban settings. The relationship among specific IgE reactions to determined groups of SM allergens in the coincident asthma pheno-endotypes has not yet been investigated. We aimed to study a Precision Allergy Molecular Diagnosis (PAMD@) model to depict the SM molecular profile in individuals presenting with Type-2 inflammation, in two different (moderate and severe) asthma phenotypes. A customized PAMD@ panel, including SM allergens and their concurrent protein allergenic characterization was investigated. Mite group 2 allergens were most frequently recognized, including Lep d 2 (83.45%), followed by Gly d 2 (69.17%) and Tyr p 2 (47,37%), in 133/164 asthmatic subjects. Blo t 5 and Blo t 21 exhibited significant higher titres in both asthma groups. Although relevant mite group 2 allergens cross-reactivity is suggested, individualized sensitization patterns were relevantly identified. The present PAMD@ panel confirmed the dominance of mite group 2 allergens in moderate-to-severe T2 asthmatics. A broadly heterogeneous molecular repertoire of SM allergens was found in all subjects, regardless of their asthma severity. Blomia tropicalis deserves special attention in certain territories, as diagnostic and/or therapeutic approaches merely based on Pyroglyphidae mites may be insufficient.
Keywords: airborne allergens, allergen exposure, asthma, storage mites, T2 inflammation
1. Introduction
Asthma is a chronic and heterogeneous inflammatory lung disease, in terms of severity, natural history, and treatment responsiveness, reflecting the underlying pathogenic mechanisms and a highly prevalent cause of reduced quality of life in individuals of all ages, turning into a major public health and global economic burden due to both direct and indirect costs [1,2,3]. Asthma management can be individualized, grouping patients according to observable combinations of clinical, biological, and physiological characteristics into distinct pheno-endotypes [4,5], opening up the opportunity for new pathway precision diagnosis and targeted treatments [6,7]. Despite a broad number of distinct cell types that may play a unique role in the immunopathobiology of bronchial asthma, inflammatory cellular profiles of asthma principally fall into a dichotomy of type 2 response (resulting in eosinophilic inflammation) and non-type 2 response (thus, reinforcing non-eosinophilic, pauci-granulocytic inflammation) [8,9]. In addition, the upregulation of type 2 inflammation is characterized by an stimulus at the level of the airway epithelium that results in the production of alarmins -IL-25, IL-33, and thymic stromal lymphopoietin (TSLP) that stimulate the release of IL-4, IL-5, and IL-13, to activate and potentiate the innate and humoral arms of the immune system that lead to the pathogenic airway remodeling in asthma [10,11,12]. In addition, the interaction between the airway epithelium and the inhaled environment is crucial to understanding the pathogenesis of asthma, ever since the early demonstration that type-I hypersensitivity to dust-mite-derived allergens and adjuvants were the origin of the allergenicity of house dust [13]. The distribution of mite species in a geographical area is markedly affected by the local climate conditions, and diverse types of mites dominate in different regions of the world [14]. In this regard, numerous mite species have been described capable of sensitizing and inducing clinical manifestations in humans, in sensitized and genetically predisposed subjects [15,16,17]. Therefore, mites are generally grouped into house dust mites (HDM) belonging to the Pyroglyphidae family and storage mites (SM) (also known as grain mites, flour mites, and/or forage mites), including Acaridae and Glycyphagydae families, related to rural occupational exposure and humid urban dwellings [18,19,20]. The term “domestic mites” refers to mite species present in the indoor environment, causing the development of specific immunoglobulin E (sIgE) antibody responses, encompassing both HDM and SM categories. This is the case for Blomia tropicalis (B. tropicalis), formerly known as an SM, which is nowadays considered a domestic mite, extensively present in homes from tropical and subtropical countries [21,22]. Although several SM allergens have been recently purified, cloned and sequenced, the variations in the biological activity among allergen extracts and manufacturers may restrict the full understanding of the in vivo relevance of the sensitization to these molecules [23,24].
Another issue of concern in the published literature is that SPT reactivity to SM can either represent “true positivity” or “false positivity” due to their taxonomic proximity with HDM [25,26]. In fact, mites of the same family share several proteins with great homology, showing a high cross-reactivity among the Glycyphagydae family and a moderate reactivity between B. tropicalis and Tyrophagus putrescentiae (T. putrescentiae) [27]. To overcome this situation, the current availability of DNA sequences of allergens has allowed the preparation of purified, recombinant allergens and hypoallergenic allergen derivatives, that can be used for Precision Allergy Molecular Diagnosis (PAMD@) to identify the individual molecules, to elucidate between actual poly-sensitization to numerous allergens and cross-reactivity [28]. Despite HDM exposure and sensitization having been previously documented as strong predictors for respiratory disease, there is still limited evidence concerning SM-sIgE responses taking part in the pathogenesis of the T2 inflammation asthma phenotype [29,30,31]. Moreover, data are scarce for subjects simultaneously sensitized to HDM and SM. Here, we investigated a personalized PAMD@ model approach to depict the molecular profiling of different SM families from selected non-occupational moderate and severe asthmatics with the distinct T2-phenotype, subjected to the influence of perennial subtropical weather conditions.
2. Results
2.1. Demographic Characteristics of Patients
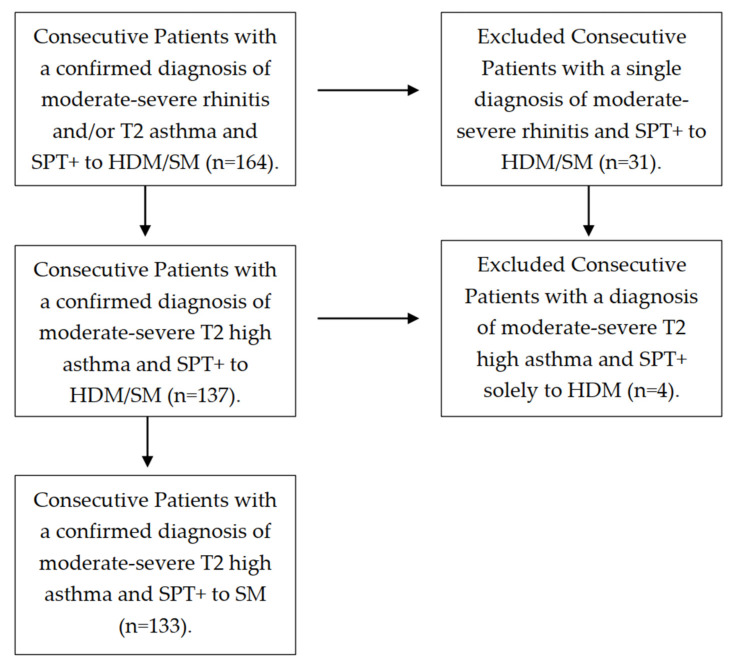
A total of 164 patients were screened, with 133 of them—79 females, 54 males, median age 26.0 years old—finally confirming their eligibility for the study (Figure 1). All subjects who fulfilled the GINA criteria [32] for moderate-to-severe non-occupational T2 persistent asthma showed a positive SPT to any SM. Most of the subjects (109 out of 133 patients, 82.56%) had their asthma onset during childhood or adolescence. All subjects were on regular daily treatment—comprising both mite avoidance measures and medical therapy—according to their asthma stage and severity. Five out sixty-two (8.06%) patients from the severe asthma cohort were on oral steroids upon inclusion in the study. Regarding atopic comorbidities, 121 patients (90.11%) suffered from allergic rhinitis, 32 subjects (24.06%) had atopic dermatitis and 23 (17.29%) had food allergy (seafood, nuts, egg and/or milk) associated. The majority of patients (86.66%) reported a known family history of atopy.
Figure 1.
Flow diagram of study selection.
2.2. Total IgE and Blood Eosinophils
A quantitative analysis of serum total IgE was performed in order to evaluate the basal atopic status in the study population. The total IgE showed a median value of 642 IU/mL. The severe asthmatic patients showed a median total IgE value (661 IU/mL) slightly higher than the moderate asthma group (635.5 IU/mL). Blood eosinophils showed a median value of 400 eosinophils/μL, again with a higher significant (p < 0.05) median value (420 eosinophils/μL) in the severe asthma group, with respect to those with the moderate asthma (395 eosinophils/μL) phenotype (Table 1).
Table 1.
Descriptive statistics regarding basal comorbid conditions and associated asthma features in the studied population (n = 133).
| Moderate Asthma | Severe Asthma | |
|---|---|---|
| n = 133 | 71 (53.38%) | 62 (46.62%) |
| Age (y.o.) | 29.59 ± 13.82 | 33.85 ± 16.05 |
| <20 y.o. (n = 41) | 19 ± 7.3 (26.76%) | 16 ± 5.21 (25.8%) |
| >20 y.o. (n = 92) | 52 (73.24%) | 46 (74.2%) |
| Sex (F/M) | 56.33%/43.67% | 61.3%/38.7% |
| BMI | 26.54 ± 5.9 | 28.59 ± 5.4 |
| Allergic Rhinitis | 64 (90.14%) | 55 (88.7%) |
| Atopic Dermatitis * | 17 (23.94%) | 4 (6.45%) |
| Nasal Polyposis * | 2 (2.81%) | 8 (12.9%) |
| Food Allergy | 9 (12.67%) | 3 (4.83%) |
| NSAID sensitivity | 2 (2.81%) | 2 |
| ACT | 18 (16–25) | 14 (9–17) |
| FVC | 3728 (90.1 ± 13.56%) | 3212 (79.0 ± 15.03%) |
| FVC < 20 y.o. | 90.87 ± 15.67% | 81.24 ± 17.22% |
| FEV1 * | 3027 (91.32 ± 15.07%) | 2475 (76.12 ± 17.41%) |
| FEV1 < 20 y.o. | 92.33 ± 18.81% | 81.92 ± 16.33% |
| SPT+HDM/SM | 71 (100%) | 62 (100%) |
| Total IgE (IU/mL) | 635 ± 733 | 661 ± 702 |
| Eosinophils/μL peripheral blood * | 395 ± 225 | 420 ± 259 |
| Asthma Onset at Childhood | 53 (74.6%) | 48 (77.41%) |
| Family History of Atopy | 59 (83.09%) | 51 (82.25%) |
SPT: Skin Prick Test. SM: Storage mites. BMI: Body Mass Index. ACT: Asthma Control Test. FVC: Forced Ventilatory Capacity. FEV1: forced expiratory volume in the first second. Median values and standard error of the median (SEM) are shown. * Indicates statistical significance (p < 0.05).
2.3. Prevalence, Sige Reactivity and Individual Molecular Profile in Serum from SM Asthmatic Subjects
Sensitization to mite extracts by SPT and the prevalence of 133 patients who met the inclusion criteria are summarized in Table 2.
Table 2.
Prevalence of sensitization to mites by Skin Prick Test.
| Skin Prick Test | N (%) |
|---|---|
| Dermatophagoides pteronyssinus | 131 (98.5) |
| Blomia tropicalis | 91 (68.42) |
| Lepidoglyphus destructor | 68 (51.12) |
| Acarus siro | 61 (45.86) |
| Tyrophagus putrescentiae | 46 (34.58) |
| Glycyphagus domesticus | 36 (27.06) |
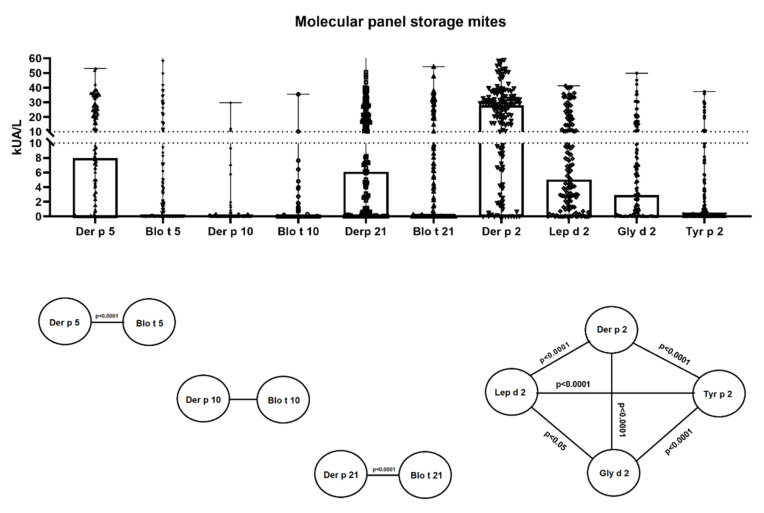
One hundred and twenty-one patients (90.97%) were independently sIgE positive (≥0.35 kUA/L), for either the whole extract of B. tropicalis, L. destructor, A. siro, G. domesticus, and/or T. putrescentiae and/or one of the following individual molecules: Blo t 5, Blo t 10, Blo t 21, Lep d 2, Gly d 2 and/or Tyr p 2. Sensitization to the complete B. tropicalis and L. destructor extract was confirmed in 76 (57.14%) and 62 (46.61%) patients, respectively, followed by a serum sIgE response to the A. siro extract in 57 (42.85%) individuals, T. putrescentiae in 39 cases (29.32%) and G. domesticus in 30 subjects (22.55%). Only 2 subjects out of 133 (1.5%) with a positive sIgE response to SM were not sensitized to sIgE-D. pteronyssinus (whole extract). Considering molecular allergens exclusively, group 2 was most frequently identified, with sIgE positive for Lep d 2 in 111 out of 133 subjects (83.45%), followed by Gly d 2 (69.17%) and Tyr p 2 (47.37%). The mean value of sIgE (kUA/L) against Lep d 2 (10.08), was also significantly (p < 0.05) higher than Gly d 2 (7.82) and Tyr p 2 (3.51). Concerning B. tropicalis major allergens, Blo t 5 (mean sIgE 6.09 kUA/L) was found in 58 asthmatics (43.6%), followed by Blo t 21 (mean sIgE 7.09 kUA/L) in 51 patients (38.34%), while Blo t 10 (mean sIgE 0.63 kUA/L) was limited to 19 subjects (14.28%). Statistical differences (p < 0.001) were found among HDM and SM allergens from groups 2, 5 and 21 (Figure 2).
Figure 2.
Specific IgE serodominance in a comprehensive panel of molecular allergens to Dermatophagoides pteronyssinus, Blomia tropicalis, Lepidoglyphus destructor, Glyciphagus domesticus and Tyrophagus putrescentiae in 133 asthmatic subjects. Statistical differences (p < 0.001) among mite allergens from groups 2, 5 and 21 are shown.
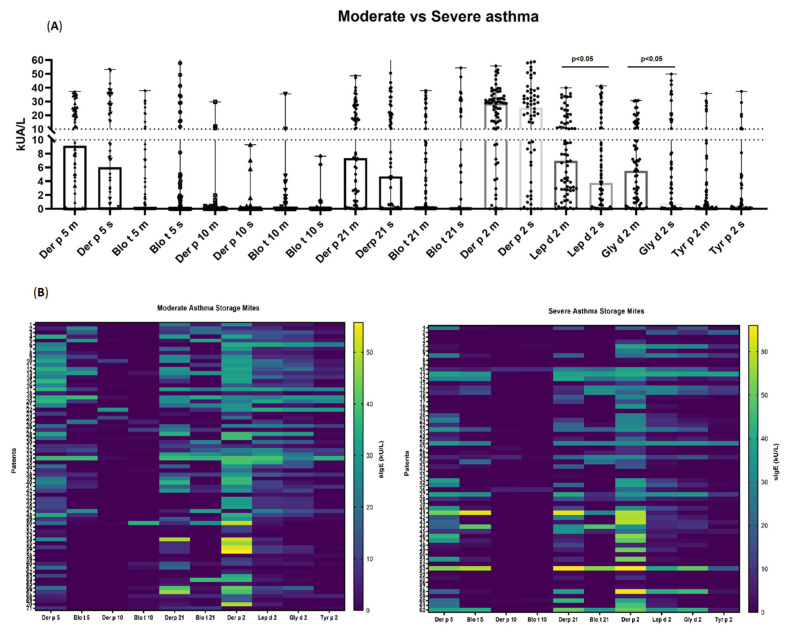
2.4. Relation of Sige-Sensitization Profile and Severity of Asthma
Specific IgE (kUA/L) to the whole extract of B. tropicalis was higher in the moderate asthma group (22.21 ± 7.35) compared to the severe phenotype (16.87 ± 9.22). In contrast, severe asthmatics showed slightly higher mean sIgE to complete G. domesticus, A. siro and T. putrescentiae extracts, compared to moderate asthmatics. With respect to individual molecules, non-significant (p = 0.48), higher sIgE titres were found for Blo t 5 in the severe asthma group (7.42 ± 5.67), compared to the milder (4.77 ± 3.86) asthma patients. Higher quantitative differences (p < 0.05) were only found for Lep d 2 and Gly d 2 in the moderate asthmatics, with no further variations in the rest of the investigated molecules (i.e., Tyr p 2, Blo t 10 and Blo t 21), as displayed in Figure 3.
Figure 3.
Sensitization profile to specific IgE (sIgE) (A) and heatmap (B) to a comprehensive panel of molecular allergens of Dermatophagoides pteronyssinus, Blomia tropicalis, Lepidoglyphus destructor, Glyciphagus domesticus and Tyrophagus putrescentiae in 133 moderate (m) to severe (s) asthmatic patients. Broadly different patterns of sIgE were identified in both groups of asthmatics.
2.5. Molecular Sensitization Profiles and Aggregation into Mite Allergen Homologous Proteins
Lep d 2 exhibited the most prevalent individual SM allergen in 17 out of 21 (77.77%) different depicted SM profiles, followed by Gly d 2 (59.25%), Blo t 5 (48.14%), Bl t 21 (44.44%), Tyr p 2 (37.03) and Blo t 10 (37.03%). Nineteen patients (14.28%) showed a monomolecular sIgE response to either Lep d 2 (11.27%), Gly d 2 (1.5%), Blo t 5 (0.75%) or Blo t 10 (0.75%). Meanwhile, no subjects were found to be solely sensitized to Blo t 21. In contrast, despite 14 subjects (10.52%) having a positive sIgE response to the crude extract of SM, no detection to any of the 6 individual available SM molecular allergens was found. Considering the principle of homologous groups among D. pteronyssinus and SM, the repertoire of recognized molecules (sIgE against groups 2, 5, 10 and 21) was markedly complex, including 41 distinct profiles in 133 subjects (Table 3), with 8 specific molecules (Der p 2, Lep d 2, Gly d 2, Tyr p 2, Der p 5, Blo t 5, Der p 21, and Blo t 21), most frequently (15.03%) identified in both groups of asthmatics. Further, 6 out 133 patients (4.51%) were sensitized to either Lep d 2, Gly d 2 and/or Tyr p 2, but not to Der p 2. In addition, nine patients (6.76%) showed a positive sIgE response to Blo t 10 but not to Der p 10, while eight subjects (6.01%) were selectively sensitized to Blo t 5 and not to Der p 5, and five individuals (3.75%) were sensitized to Blo t 21 but not to Der p 21.
Table 3.
Specific IgE profiles aggregated into mite homologous group allergens 2, 5, 10 and 21 between D. pteronyssinus and storage mites in 133 subjects tested with microarray. Profiles are ordered by the increasing number of recognized molecules.
| n = 133 | % | Number of Molecules | Der p 2 | Lep d 2 | Gly d 2 | Tyr p 2 | Der p 5 | Blo t 5 | Der p 10 | Blo t 10 | Der p 21 | Blo t 21 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4 | 3.00 | 0 | ||||||||||
| 4 | 3.00 | 1 | * | |||||||||
| 1 | 0.75 | 1 | * | |||||||||
| 1 | 0.75 | 1 | * | |||||||||
| 2 | 1.50 | 2 | * | * | ||||||||
| 1 | 0.75 | 2 | * | * | ||||||||
| 2 | 1.50 | 2 | * | * | ||||||||
| 1 | 0.75 | 2 | * | * | ||||||||
| 3 | 0.75 | 3 | * | * | * | |||||||
| 2 | 1.50 | 3 | * | * | * | |||||||
| 1 | 0.75 | 3 | * | * | * | |||||||
| 1 | 0.75 | 3 | * | * | * | |||||||
| 1 | 0.75 | 3 | * | * | * | |||||||
| 2 | 1.50 | 3 | * | * | * | |||||||
| 1 | 0.75 | 3 | * | * | * | |||||||
| 1 | 0.75 | 3 | * | * | * | |||||||
| 3 | 2.25 | 4 | * | * | * | * | ||||||
| 1 | 0.75 | 4 | * | * | * | * | ||||||
| 1 | 0.75 | 4 | * | * | * | * | ||||||
| 1 | 0.75 | 4 | * | * | * | * | ||||||
| 6 | 4.51 | 4 | * | * | * | * | ||||||
| 2 | 1.50 | 4 | * | * | * | * | ||||||
| 3 | 2.25 | 4 | * | * | * | * | ||||||
| 2 | 1.50 | 4 | * | * | * | * | ||||||
| 1 | 0.75 | 4 | * | * | * | * | ||||||
| 1 | 0.75 | 4 | * | * | * | * | ||||||
| 3 | 2.25 | 5 | * | * | * | * | * | |||||
| 3 | 2.25 | 5 | * | * | * | * | * | |||||
| 2 | 1.50 | 5 | * | * | * | * | * | |||||
| 1 | 0.75 | 5 | * | * | * | * | * | |||||
| 1 | 0.75 | 5 | * | * | * | * | * | |||||
| 1 | 0.75 | 5 | * | * | * | * | * | |||||
| 1 | 0.75 | 5 | * | * | * | * | * | |||||
| 1 | 0.75 | 5 | * | * | * | * | * | |||||
| 9 | 6.76 | 6 | * | * | * | * | * | * | ||||
| 7 | 5.26 | 6 | * | * | * | * | * | * | ||||
| 2 | 1.50 | 6 | * | * | * | * | * | * | ||||
| 1 | 0.75 | 6 | * | * | * | * | * | * | ||||
| 1 | 0.75 | 6 | * | * | * | * | * | * | ||||
| 1 | 0.75 | 6 | * | * | * | * | * | * | ||||
| 1 | 0.75 | 6 | * | * | * | * | * | * | ||||
| 1 | 0.75 | 6 | * | * | * | * | * | * | ||||
| 1 | 0.75 | 6 | * | * | * | * | * | * | ||||
| 1 | 0.75 | 6 | * | * | * | * | * | * | ||||
| 8 | 6.01 | 7 | * | * | * | * | * | * | * | |||
| 5 | 3.75 | 7 | * | * | * | * | * | * | * | |||
| 1 | 0.75 | 7 | * | * | * | * | * | * | * | |||
| 1 | 0.75 | 7 | * | * | * | * | * | * | * | |||
| 1 | 0.75 | 7 | * | * | * | * | * | * | * | |||
| 1 | 0.75 | 7 | * | * | * | * | * | * | * | |||
| 1 | 0.75 | 7 | * | * | * | * | * | * | * | |||
| 1 | 0.75 | 7 | * | * | * | * | * | * | * | |||
| 20 | 15.03 | 8 | * | * | * | * | * | * | * | * | ||
| 1 | 0.75 | 8 | * | * | * | * | * | * | * | * | ||
| 3 | 2.25 | 9 | * | * | * | * | * | * | * | * | * | |
| 2 | 1.50 | 9 | * | * | * | * | * | * | * | * | * | |
| 1 | 0.75 | 10 | * | * | * | * | * | * | * | * | * | * |
Asterisk (*) indicates specific IgE sensitization to a single mite molecular allergen.
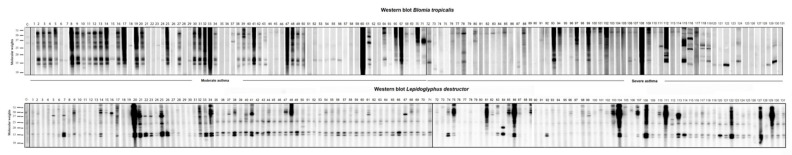
2.6. SDS PAGE and IgE Western Blot
Western blot of selected patients with a sensitization to B. tropicalis and L. destructor showed different patterns of sensitization (Figure 4). A marked IgE-binding intensity was found around 13, 14, 17, 30, 35, 50 and 55 kDa for B. tropicalis in the majority of subjects, and around 14–16 kDa for patients with moderate asthma with a more complex repertoire, including 14–16, 25, 40 and 50 kDa for L. destructor in those with the severe asthma presentation.
Figure 4.
IgE Western blot of selected patients for Blomia tropicalis and Lepidoglyphus destructor allergenic extract. A marked IgE-binding intensity was found around 13, 14, 17, 30, 35, 50 and 55 kDa for Blomia tropicalis in the majority of subjects, and around 14–16 kDa mainly for patients with mild–moderate asthma and a more heterogenous repertoire including 14–16, 25, 40 and 50 kDa for Lepidoglyphus destructor in severe asthmatics.
3. Discussion
Unique attributes of mites have allowed them to colonize the indoor environment, producing an unparalleled diversity of allergens and adjuvants, perfectly complemented to elicit both innate and adaptive immune reactions [33]. In fact, despite SM having been traditionally related to occupational disease, attention has been focused on their clinical relevance in the adult general population and children in non-occupational environments, from temperate regions of the world [34,35,36]. Conforming to our previous observations, describing the clinical role of SM in different atopic conditions, most of the screened SM patients (98.5%) were simultaneously sensitized to HDM [37,38]. Studies of cross-reactivity among non-pyroglyphid mites have been carried out, with conflicting results, showing a limited cross-reactivity among Gly d 2, Lep d 2, and Tyr p 2 [39]. The 14-kDa mite group 2 allergen—belonging to the NPC2 (NPC intracellular cholesterol transporter 2, Niemann-Pick proteins type C2) family—was identified in more than 83% of the current cohort, with Lep d 2 as the most frequently SM-depicted allergen, closely followed by Gly d 2 and Tyr p 2, to a lesser extent [40]. In line with previous reports [41], indicating an important IgE cross-reactivity among Lep d 2, Gly d 2 and Tyr p 2, and a partial cross-reactivity between T. putrescentiae and G. domesticus/L. destructor, we found that more than 50% of the individuals were all concomitantly sensitized to these three molecules, regardless of the asthma severity.
It is noteworthy that, despite Gly d 2 sharing a high (79%) sequence homology with Lep d 2 [42], only 31.98% of individuals presented a selective response to Lep d 2 and Gly d 2, followed by Gly d 2 and Tyr p 2 (3.36%) and Lep d 2 and Tyr p 2 (1.68%). Further, in accordance with reports from Southern Spain, nearly all patients (>98%) with a positive response to Gly d 2 were also sensitized to Lep d 2, whereas this mite has been detected in only 2.6% of the patients’ house dust samples [43,44]. Interestingly, both Lep d 2 and Gly d 2 may be speculated as potential biomarkers in milder forms of asthma presentations, as significant differences were only found in the moderate asthmatics against the severe asthma group. In respect of group 2 allergen interactions, above 90% of the screened subjects showed a sIgE response to Der p 2, and more than half of them were concurrently sensitized to Lep d 2, Gly d 2 and Tyr p 2. In agreement with the low (45%) sequence homology described for group 2 proteins between D. pteronyssinus and SM [45,46], only 16.52% of subjects were sensitized to Der p 2 and Lep d 2, with even lower ratios between Der p 2 and Gly d 2 (1.65%) and Der p 2 and Tyr p 2 (0.82%).
Molecular sensitization to B. tropicalis was broadly present in the selected cohort (63.02%), supporting a pivotal role for Blo t 5, not only in respiratory allergies, but also in the severity of the underlying disease [47,48]. These findings may be of interest, as murine models of CD4 T-cell epitopes for Blo t 5 could be therapeutically employed to suppress the inflammatory response in the allergic airway, regardless of the inferred gravity of symptoms [49].
Considering the homology between group 5 and 21 allergens, above 71% subjects showed sIgE to Der p 5 or Der p 21. Despite low cross-reactivity having been only addressed between group 5 allergens [50], similar ratios were found for patients concomitantly sensitized to Der p 5 and Blo t 5 (50%), and/or Der p 21 and Blo t 21 (46.31%).
Group 10 tropomyosins are noted for their conserved amino acid sequences, being almost identical to other arthropod tropomyosins and, thus, being involved in cross-reactivity mechanisms [51]. In the present study, not only was Blo t 10 more frequently identified than Der p 10, but also selective Blo t 10 responses were detected. Notably, although 10 asthmatic patients were associated with a confirmed—double-blind placebo-controlled challenge (DBPCC) according to their previous medical records—seafood allergy diagnosis, Blo t 10 and Der p 10 were only identified in three and two subjects, respectively.
Despite different patterns of sensitization to B. tropicalis having been outlined, the additional quantification of potentially relevant allergens from B. tropicalis is not commercially available at present. This is the case for Blo t 4, described as a local serodominant allergen, showing an unusually higher frequency than Blo t 5, in areas from China and Spain [52,53]. Further, recent progress in the immuno-characterization of B. tropicalis, has elegantly evidenced that Blo t 2 is a clinically relevant allergen, with unique IgE epitopes, compared to the major group 2 allergens from Dermatophagoides spp. [54].
Although the concept of homologous groups could serve as a dynamic tool in the regulation of allergen products, our findings do not support a reduction in the study panel of mite allergens, as mites other than Pyroglyphidae are frequently present in significant amounts in tropical and subtropical dust samples, from both rural and urban environments [55,56]. The current study showed several restrictions, as 14 subjects (10.52%) with a positive sIgE response to the raw extract of SM (with 3 and 2 out of those 14 patients showing a positive SPT to G. domesticus and A. siro, respectively) could not be identified through the proposed molecular panel, and also, a limited number of patients was studied, making these findings challenging to match with other SM-sensitive asthma cohorts, exposed to different mite populations.
4. Materials and Methods
4.1. Subjects
We consecutively recruited patients with a clinical diagnosis of moderate-to-severe persistent rhinitis and/or non-occupational asthma with the mixed T2 endotype (i.e., eosinophilic, high total IgE and sIgE to airborne allergens) according to the 2020 GINA Guidelines [32] from the Severe Asthma Unit and the Outpatient Allergy Clinic at Hospital Universitario de Canarias (Tenerife, Spain), serving an area of 368,000 inhabitants under subtropical climate conditions, and mites as the most frequently found respiratory allergen [57]. Asthma severity and staging were also clinically evaluated according to the aforementioned specific Guidelines [32].
Included subjects needed to achieve the subsequent clinical standards: persistent non-occupational respiratory symptoms with recurrent exacerbations, improvement in symptoms at altitudes (>1500 m) and increase in symptoms with household dust and indoor activities. The following clinical data were collected from the patients’ medical records: forced expiratory volume in the first second (FEV1), rhinitis and conjunctivitis diagnosis, treatments, a validated Asthma Control Test (ACT), and skin prick test (SPT) results. Only subjects with an immediate positive SPT to any SM extract were included. Blood samples were obtained from all participating individuals, identified with a code label, stored at −40 °C and thawed immediately prior to the in vitro assay. Patients under treatment with allergen immunotherapy or monoclonal antibodies (biologics) were excluded. Pregnant and breast-feeding women were also excluded. The investigation was approved by the local Ethical Committee of our institution and informed consent was signed by all subjects and parents/guardians for those participants <18 y.o.
4.2. Skin Prick Test
Percutaneous testing was carried out according to European standards [58], enclosing a diagnostic panel (Diater, Madrid, Spain) with standardized (Dermatophagoides pteronyssinus (D. pteronyssinus), B. tropicalis, Lepidoglyphus destructor (L. destructor), and T. putrescentiae) and non-standarized (Glycyphagus domesticus (G. domesticus) and Acarus siro (A. siro)) mite extracts. Histamine (10 mg/mL) and saline were used as positive and negative controls as usual. Antihistamines were withdrawn a week before the SPT, and wheal diameters were immediately measured after 20 min with those diameters greater than 3 mm considered as positive.
4.3. Mite Allergenic Extracts
Proteins from mite bodies of D. pteronyssinus, B. tropicalis, and L. destructor were extracted in phosphate-buffered saline buffer (PBS), 0.01 M, pH 7.4, for 2 h at 5 ± 3 °C. Both protein solutions were clarified by filtration and centrifugation (1 h at 16,000× g). Afterwards, the isolated supernatants were ultrafiltered against highly purified water (Ph. Eur. specification), sterile filtered, frozen and lyophilized.
4.4. SDS PAGE and IgE Western Blot
Proteins from B. tropicalis, and L. destructor extracts were analyzed by sodium dodecylsulfate polyacrylamide gel electrophoresis (SDS-PAGE), according to Laemmli [59] in 15% polyacrylamide gels under reducing conditions. Proteins were visualized by Coomassie Brilliant Blue R-250 staining and transferred to polyvinylidene difluoride (PVDF, Trans-blot turbo TM. BIORAD, Hercules, CA, USA). The binding of IgE antibody to allergens was analyzed by Western blot using individual patients’ sera and anti-human IgE peroxidase conjugate (Southern Biotech, Birmingham, AL, USA). Chemiluminescence detection reagents (Western lightning® Plus-ECL. Perkin Elmer. Waltham, MA, USA) were added following the manufacturer’s instructions. IgE-binding bands were identified using the BioRad Diversity database program.
4.5. Blood Eosinophils and Serological Analysis
Peripheral blood eosinophils were determined and expressed as eosinophils/μL. Total IgE levels, sIgE to B. tropicalis, L. destructor, A. siro, G. domesticus, T. putrescentiae and D. pteronyssinus (whole extract), and sIgE to Der p 2, Der p 5, Der p 10, Der p 21, Blo t 5, Blo t 10, Blo t 21, Lep d 2, Gly d 2, Tyr p 2 were measured (ALEX MacroArray Diagnostics, Vienna, Austria) according to the manufacturer´s instructions. In brief, ALEX is a multiplex array containing 282 reagents (157 whole allergens and 125 molecular components). The different allergens and components are coupled onto polystyrene nano-beads, and then the allergen beads are deposited on a nitrocellulose membrane, as formerly published [60]. Total IgE levels were expressed in international units per unit volume (IU/mL), sIgE levels were expressed in kUA/L. Values ≥ 0.35 kUA/L were considered positive.
4.6. Statistical Analysis
Demographic features were summarized by medians and standard deviations for continuous variables and percentages for categorical variables. To compare differences analysis of variance, Kruskal–Wallis, Mann–Whitney U and Chi-square tests are required for parametric continuous, nonparametric continuous, and categorical variables respectively. A P value of less than 0.05 was considered statistically significant. All statistical data were analyzed using GraphPad Prism version 8.0.0 for Windows, GraphPad Software, La Jolla, CA, USA.
5. Conclusions
The present study is, to our knowledge, the first to investigate a real-life molecular response to a comprehensive panel of SM allergens in our territory, displaying a widely heterogeneous repertoire in more than 89% of the T2 asthma subjects. Although the analysis of PAMD@ revealed the dominance of mite group 2 allergens, and part of the detected IgE signals suggest determined cross-reactivity, the depiction of individual sensitization patterns should be carefully evaluated for precise diagnosis and targeted AIT. Similarly, SM distinctly demands specific attention in certain regions, as current diagnostic and therapeutic tools based on Dermatophagoides allergens may lead to under-diagnosis or inaccurate treatment. In addition, the regular follow-up of SM sensitization could potentially be a non-invasive marker of epithelial barrier dysfunction in asthma, and to monitor other affected tissues [61]. The proposed PAMD@ panel approach ought to be included to provide a more precise diagnosis, particularly in populations with concomitant HDM and SM exposure, thus, expanding the intricacy of the molecular picture in this asthma phenotype. Furthermore, our results confirm that molecular diagnosis is a sensitive and highly specific tool to determine SM allergen exposure in certain territories.
Acknowledgments
The authors acknowledge Peter Forstenlechner and Martina Aumayr at Macro Array Diagnostics, Vienna, Austria, for their technical support during the current investigation.
Author Contributions
Conceptualization, R.G.-P., P.P.-G. and F.P.; methodology, R.G.-P., P.P.-G. and F.P.; software, F.P., M.C.; validation and formal analysis, I.S.-M., F.P., M.C.; investigation, I.S.-M., R.G.-P., P.P.-G. and F.P.; resources, I.S.-M., F.P., F.P., M.C.; data curation, R.G.-P., P.P.-G. and F.P.; writing—original draft preparation, R.G.-P. and P.P.-G.; writing—review and editing, R.G.-P., P.P.-G., F.P. and M.C.; project administration R.G.-P., P.P.-G. and I.S.-M.; funding acquisition R.G.-P., P.P.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Fundación Canaria Instituto de Investigación Sanitaria de Canarias (FIISC), Servicio Canario de Salud, grant number OA17/042.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Ethics Committee of CEIC Hospital Universitario de Canarias, Tenerife, Spain with the reference number P.I.-2017/72 on 30 October 2017.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from Servicio Canario de Salud but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with the permission of Servicio Canario de Salud.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dharmage S.C., Perret J.L., Custovic A. Epidemiology of Asthma in Children and Adults. Front. Pediatr. 2019;7:246. doi: 10.3389/fped.2019.00246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ellwood P., Asher M.I., Billo N.E., Bissell K., Chiang C.-Y., Ellwood E.M., El-Sony A., García-Marcos L., Mallol J., Marks G., et al. The Global Asthma Network rationale and methods for Phase I global surveillance: Prevalence, severity, management and risk factors. Eur. Respir. J. 2017;49:1601605. doi: 10.1183/13993003.01605-2016. [DOI] [PubMed] [Google Scholar]
- 3.Pawankar R. Allergic diseases and asthma: A global public health concern and a call to action. World Allergy Organ. J. 2014;7:1–3. doi: 10.1186/1939-4551-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agache I., Akdis C.A. Endotypes of allergic diseases and asthma: An important step in building blocks for the future of precision medicine. Allergol. Int. 2016;65:243–252. doi: 10.1016/j.alit.2016.04.011. [DOI] [PubMed] [Google Scholar]
- 5.Kuruvilla M.E., Lee F.E.-H., Lee G.B. Understanding Asthma Phenotypes, Endotypes, and Mechanisms of Disease. Clin. Rev. Allergy Immunol. 2019;56:219–233. doi: 10.1007/s12016-018-8712-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robinson D., Humbert M., Buhl R., Cruz A.A., Inoue H., Korom S., Hanania N.A., Nair P. Revisiting Type 2-high and Type 2-low airway inflam-mation in asthma: Current knowledge and therapeutic implications. Clin. Exp. Allergy. 2017;47:161–175. doi: 10.1111/cea.12880. [DOI] [PubMed] [Google Scholar]
- 7.Fajt M.L., Wenzel S.E. Asthma phenotypes and the use of biologic medications in asthma and allergic disease: The next steps toward personalized care. J. Allergy Clin. Immunol. 2015;135:299–310. doi: 10.1016/j.jaci.2014.12.1871. [DOI] [PubMed] [Google Scholar]
- 8.Lambrecht B.N., Hammad H. The immunology of asthma. Nat. Immunol. 2015;16:45–56. doi: 10.1038/ni.3049. [DOI] [PubMed] [Google Scholar]
- 9.Jeong J.S., Kim S.R., Cho S.H., Lee Y.C. A Novel Insight on Endotyping Heterogeneous Severe Asthma Based on Endoplasmic Reticulum Stress: Beyond the “Type 2/Non-Type 2 Dichotomy”. Int. J. Mol. Sci. 2019;20:713. doi: 10.3390/ijms20030713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Woodruff P.G., Modrek B., Choy D., Jia G., Abbas A.R., Ellwanger A., Arron J., Koth L.L., Fahy J.V. T-helper Type 2–driven Inflammation Defines Major Subphenotypes of Asthma. Am. J. Respir. Crit. Care Med. 2009;180:388–395. doi: 10.1164/rccm.200903-0392OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trivedi M., Denton E. Asthma in Children and Adults-What Are the Differences and What Can They Tell us About Asthma? Front. Pediatr. 2019;25:256. doi: 10.3389/fped.2019.00256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mitchell P.D., O’Byrne P.M. Epithelial-Derived Cytokines in Asthma. Chest. 2017;151:1338–1344. doi: 10.1016/j.chest.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 13.Korsgaard J. House-dust mites and asthma. A review on house-dust mites as a domestic risk factor for mite asthma. Allergy. 1998;53((Suppl. 48)):77–83. doi: 10.1111/j.1398-9995.1998.tb05003.x. [DOI] [PubMed] [Google Scholar]
- 14.Li L., Qian J., Zhou Y., Cui Y. Domestic mite-induced allergy: Causes, diagnosis, and future prospects. Int. J. Immunopathol. Pharmacol. 2018;32:2058738418804095. doi: 10.1177/2058738418804095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller J.D. The Role of Dust Mites in Allergy. Clin. Rev. Allergy Immunol. 2019;57:312–329. doi: 10.1007/s12016-018-8693-0. [DOI] [PubMed] [Google Scholar]
- 16.Fernández-Caldas E., Puerta L., Caraballo L. Mites and allergy. In: Bergmann K., Ring J., editors. History of Allergy, Chem Immunol Allergy. Volume 100. Karger; Basel, Switzerland: 2014. pp. 234–242. [DOI] [PubMed] [Google Scholar]
- 17.Andiappan A.K., Puan K.J., Lee B., Nardin A., Poidinger M., Connolly J., Chew F.T., Wang D.Y., Rotzschke O. Allergic airway diseases in a tropical urban envi-ronment are driven by dominant mono-specific sensitization against house dust mites. Allergy. 2014;69:501–509. doi: 10.1111/all.12364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Müsken H., Franz J.T., Wahl R., Paap A., Cromwell O., Masuch G., Bergmann K.C. Sensitization to different mite species in German farm-ers: Clinical aspects. J. Investig. Allergol. Clin. Immunol. 2000;10:346–351. [PubMed] [Google Scholar]
- 19.Sánchez-Borges M., Fernandez-Caldas E., Thomas W.R., Chapman M.D., Lee B.W., Caraballo L., Acevedo N., Chew F.T., Ansotegui I.J., Behrooz L., et al. International consensus (ICON) on: Clinical consequences of mite hypersensitivity, a global problem. World Allergy Organ. J. 2017;10:14. doi: 10.1186/s40413-017-0145-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang C., Li J., Lai X., Zheng Y., Gjesing B., Spangfort M.D., Zhong N. House dust mite and storage mite IgE reactivity in allergic patients from Guangzhou, China. Asian Pac. J. Allergy Immunol. 2012;30:294–300. [PubMed] [Google Scholar]
- 21.Juliá-Serdá G., Cabrera-Navarro P., Acosta-Fernández O., Martín-Pérez P., García-Bello M.A., Antó-Boqué J. Prevalence of sen-sitization to Blomia tropicalis among young adults in a temperate climate. J. Asthma. 2012;49:349–354. doi: 10.3109/02770903.2012.672611. [DOI] [PubMed] [Google Scholar]
- 22.González-Pérez R., Pineda F., Poza-Guedes P., Castillo M., Matheu V., Sánchez-Machín I. Molecular Allergen Profiling of Dual Mite Sensitization in Severe Allergic Rhinitis. J. Investig. Allergy Clin. Immunol. 2020;30:421–429. doi: 10.18176/jiaci.0439. [DOI] [PubMed] [Google Scholar]
- 23.Esch R.E., Codina R. Fungal raw materials used to produce allergen extracts. Ann. Allergy Asthma Immunol. 2017;118:399–405. doi: 10.1016/j.anai.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 24.González-Pérez R., Poza-Guedes P., del Pino Y.B., Matheu V., Sánchez-Machín I. Evaluation of major mite allergens from European standardized commercial extracts for in vivo diagnosis: Addressing the need for precision medicine. Clin. Transl. Allergy. 2019;9:14. doi: 10.1186/s13601-019-0254-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vidal C., Boquete O., Gude F., Rey J., Meijide L.M., Fernandez-Merino M.C., Gonzalez-Quintela A. High prevalence of storage mite sensitization in a general adult population. Allergy. 2004;59:401–405. doi: 10.1111/j.1398-9995.2003.00430.x. [DOI] [PubMed] [Google Scholar]
- 26.Warner A., Boström S., Möller C., Kjellman N. Mite fauna in the home and sensitivity to house-dust and storage mites. Allergy. 1999;54:681–690. doi: 10.1034/j.1398-9995.1999.00850.x. [DOI] [PubMed] [Google Scholar]
- 27.Marques M., Rezende I., Cunha I., Gouveia J., Dos Santos F.R., Falcao I., Cunha L., Falcao H. Allergic sensitization to storage dust mites: A prospective study of patients with respiratory allergy. Eur. Ann. Allergy Clin. Immunol. 2022;54:43–47. doi: 10.23822/EurAnnACI.1764-1489.178. [DOI] [PubMed] [Google Scholar]
- 28.Valenta R., Lidholm J., Niederberger V., Hayek B., Kraft D., Gronlund H. The recombinant allergen-based concept of compo-nent-resolved diagnostics and immunotherapy (CRD and CRIT) Clin. Exp. Allergy. 1999;29:896–904. doi: 10.1046/j.1365-2222.1999.00653.x. [DOI] [PubMed] [Google Scholar]
- 29.Soto-Quiros M., Avila L., Platts-Mills T.A., Hunt J.F., Erdman D.D., Carper H., Murphy D.D., Odio S., James H.R., Patrie J.T., et al. High titers of IgE antibody to dust mite allergen and risk for wheezing among asthmatic children infected with rhinovirus. J. Allergy Clin. Immunol. 2012;129:1499–1505.e5. doi: 10.1016/j.jaci.2012.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Alba J., Raemdonck K., Dekkak A., Collins M., Wong S., Nials A.T., Knowles R.G., Belvisi M.G., Birrell M.A. House dust mite induces direct airway inflammation in vivo: Implications for future disease therapy? Eur. Respir. J. 2010;35:1377–1387. doi: 10.1183/09031936.00022908. [DOI] [PubMed] [Google Scholar]
- 31.Minami T., Fukutomi Y., Lidholm J., Yasueda H., Saito A., Sekiya K., Tsuburai T., Maeda Y., Mori A., Taniguchi M., et al. IgE Abs to Der p 1 and Der p 2 as diagnostic markers of house dust mite allergy as defined by a bronchoprovocation test. Allergol. Int. 2015;64:90–95. doi: 10.1016/j.alit.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 32. [(accessed on 15 December 2021)]. Available online: https://ginasthma.org/gina-reports/
- 33.Cao H., Liu Z. Clinical significance of dust mite allergens. Mol. Biol. Rep. 2020;47:6239–6246. doi: 10.1007/s11033-020-05613-1. [DOI] [PubMed] [Google Scholar]
- 34.Spiewak R., Gòra A., Dutkiewicz J. Work-related skin symptoms and type I allergy among eastern-Polish farmers growing hops and other crops. Ann. Agric. Environ. Med. 2001;8:51–56. [PubMed] [Google Scholar]
- 35.Jõgi N.O., Olsen R.K., Svanes C., Gislason D., Gislason T., Schlunssen V., Sigsgaard T., Sundbom F., Storaas T., Bertelsen R.J. Prevalence of allergic sensitization to storage mites in Northern Europe. Clin. Exp. Allergy. 2020;50:372–382. doi: 10.1111/cea.13536. [DOI] [PubMed] [Google Scholar]
- 36.Boquete M., Carballada F., Armisen M., Nieto A., Martin S., Polo F., Carreira J. Factors influencing the clinical picture and the differ-ential sensitization to house dust mites and storage mites. J. Investig. Allergol. Clin. Immunol. 2000;10:229–234. [PubMed] [Google Scholar]
- 37.Sanchez-Machín I., Poza R.G.-P., Iglesias-Souto J., Iraola V., Matheu V. Asthma and rhinitis by storage mites. Allergy. 2011;66:1615–1616. doi: 10.1111/j.1398-9995.2011.02687.x. [DOI] [PubMed] [Google Scholar]
- 38.Iglesias-Souto J., Sánchez-Machín I., Iraola V., Poza P., González R., Matheu V. Oral mite anaphylaxis by Thyreophagus ento-mophagus in a child: A case report. Clin. Mol. Allergy. 2009;7:10. doi: 10.1186/1476-7961-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Van der Heide S., Niemeijer N.R., Hovenga H., de Monchy J.G., Dubois A.E., Kauffman H.F. Prevalence of sensitization to the storage mites Acarus siro, Tyrophagus putrescentiae, and Lepidoglyphus destructor in allergic patients with different degrees of sensitization to the house-dust mite Dermatophagoides pteronyssinus. Allergy. 1998;53:426–430. doi: 10.1111/j.1398-9995.1998.tb03917.x. [DOI] [PubMed] [Google Scholar]
- 40.Derewenda U., Li J., Dauter Z., Mueller G., Rule G., Benjamin D. The Crystal Structure of a Major Dust Mite Allergen Der p 2, and its Biological Implications. J. Mol. Biol. 2002;318:189–197. doi: 10.1016/S0022-2836(02)00027-X. [DOI] [PubMed] [Google Scholar]
- 41.Johansson E., Schmidt M., Johansson S.G., Machado L., Olsson S., van Hage-Hamsten M. Allergenic crossreactivity between Lepidoglyphus destructor and Blomia tropicalis. Clin. Exp. Allergy. 1997;27:691–709. doi: 10.1111/j.1365-2222.1997.tb01198.x. [DOI] [PubMed] [Google Scholar]
- 42.Gafvelin G., Johansson E., Lundin A., Smith A.M., Chapman M.D., Benjamin D.C., Derewenda U., van Hage-Hamsten M. Cross-reactivity studies of a new group 2 allergen from the dust mite Glycyphagus domesticus, Gly d 2, and group 2 allergens from Dermatophagoides pteronyssinus, Lepidoglyphus destructor, and Tyrophagus putrescentiae with recombinant allergens. J. Allergy Clin. Immunol. 2001;107:511–518. doi: 10.1067/mai.2001.112264. [DOI] [PubMed] [Google Scholar]
- 43.Arias-Irigoyen J., Lombardero M., Arteaga C., Carpizo J.A., Barber D. Limited IgE cross-reactivity between Dermatophagoides pteronyssinus and Glycyphagus domesticus in patients naturally exposed to both mite species. J. Allergy Clin. Immunol. 2007;120:98–104. doi: 10.1016/j.jaci.2007.02.028. [DOI] [PubMed] [Google Scholar]
- 44.Iraola Calvo V., Fernández-Caldas E. Mapa Acarológico de España. Laboratorios Leti; Barcelona, Spain: 2009. [Google Scholar]
- 45.Iraola V., Carnes J. Molecular and Biochemical Properties of Storage Mites (Except Blomia species) Protein Pept. Lett. 2007;14:954–959. doi: 10.2174/092986607782541033. [DOI] [PubMed] [Google Scholar]
- 46.Morales M., Iraola V., Leonor J.R., Bartra J., Rodríguez F., Boquete M., Huertas Á.J., Paniagua M.J., Pinto H., Carnés J. Different sensitization to storage mites depending on the co-exposure to house dust mites. Ann. Allergy Asthma. Immunol. 2015;114:36–42.e1. doi: 10.1016/j.anai.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 47.Arruda L.K., Vailes L.D., Platts-Mills T.A., Fernandez-Caldas E., Montealegre F., Lin K.L., Chua K.Y., Rizzo M.C., Naspitz C.K., Chapman M. Sensitization to Blomia tropicalis in patients with asthma and identification of allergen Blo t 5. Am. J. Respir. Crit. Care Med. 1997;155:343–350. doi: 10.1164/ajrccm.155.1.9001334. [DOI] [PubMed] [Google Scholar]
- 48.Manolio T.A., Barnes K.C., Naidu R.P., Levett P.N., Beaty T.H., Wilson A.F. Correlates of sensitization to Blomia tropicalis and Dermatophagoides pteronyssinus in asthma in Barbados. Int. Arch. Allergy Immunol. 2003;131:119–126. doi: 10.1159/000070927. [DOI] [PubMed] [Google Scholar]
- 49.Wong K.H., Zhou Q., Prabhu N., Furuhashi K., Chua Y.L., Grotenbreg G.M., Kemeny D.M. Blomia tropicalis allergen 5 (Blo t 5) T-cell epitopes and their ability to suppress the allergic immune response. Immunology. 2017;152:344–355. doi: 10.1111/imm.12772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tan K.W., Ong T.C., Gao Y.F., Tiong Y.S., Wong K.N., Chew F.T., Mok Y.K. NMR Structure and IgE Epitopes of Blo t 21, a Major Dust Mite Allergen from Blomia tropicalis. J. Biol. Chem. 2012;287:34776–34785. doi: 10.1074/jbc.M112.348730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Thomas W.R. Hierarchy and molecular properties of house dust mite allergens. Allergol. Int. 2015;64:304–311. doi: 10.1016/j.alit.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 52.Cheong N., Ramos J.D.A., Tang C.Y., Chng H.H., Yao R., Liang Z., Lee B.W., Chua K.Y. Mite Amylase from Blomia tropicalis (Blo t 4): Differential Allergenicity Linked to Geographical Regions. Int. Arch. Allergy Immunol. 2009;149:25–32. doi: 10.1159/000176303. [DOI] [PubMed] [Google Scholar]
- 53.Gonzalez-Perez R., Pineda F., Poza-Guedes P., Matheu V., Sanchez-Machin I. Minor Allergens in Moderate Severe Allergic Rhi-nitis: Group 4 Mite Amylasa (Blo t4) and Geographical Variations. J. Allergy Clin. Immunol. 2018;141:AB286. doi: 10.1016/j.jaci.2017.12.911. [DOI] [Google Scholar]
- 54.Reginald K., Pang S.L., Chew F.T. Blo t 2: Group 2 allergen from the dust mite Blomia tropicalis. Sci. Rep. 2019;9:12239. doi: 10.1038/s41598-019-48688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lorenz A., Lüttkopf D., May S., Scheurer S., Vieths S. The Principle of Homologous Groups in Regulatory Affairs of Allergen Products—A Proposal. Int. Arch. Allergy Immunol. 2009;148:1–17. doi: 10.1159/000151243. [DOI] [PubMed] [Google Scholar]
- 56.Eder K., Markmann S., Gellrich D., Mann S.L., Högerle C., Gröger M. Does the principle of homologous groups allow a reduction of allergens in the skin prick test panel? Eur. Arch. Otorhinolaryngol. 2021;278:117–125. doi: 10.1007/s00405-020-06264-5. [DOI] [PubMed] [Google Scholar]
- 57.Poza Guedes P., Sánchez Machín I., Matheu V., Iraola V., González Pérez R. Role of Predatory Mites in Persistent Nonoccupa-tional Allergic Rhinitis. Can. Respir. J. 2016;2016:5782317. doi: 10.1155/2016/5782317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Heinzerling L., Mari A., Bergmann K.C., Bresciani M., Burbach G., Darsow U., Durham S., Fokkens W., Gjomarkaj M., Haahtela T., et al. The skin prick test—European standards. Clin. Transl. Allergy. 2013;3:3. doi: 10.1186/2045-7022-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Laemmli U.K. Cleavage of Structural Proteins during the Assembly of the Head of Bacteriophage T4. Nature. 1970;227:680–685. doi: 10.1038/227680a0. [DOI] [PubMed] [Google Scholar]
- 60.Bojcukova J., Vlas T., Forstenlechner P., Panzner P. Comparison of two multiplex arrays in the diagnostics of allergy. Clin. Transl. Allergy. 2019;9:31. doi: 10.1186/s13601-019-0270-y. [DOI] [Google Scholar]
- 61.Akdis C.A. Does the epithelial barrier hypothesis explain the increase in allergy, autoimmunity and other chronic conditions? Nat. Rev. Immunol. 2021;21:739–751. doi: 10.1038/s41577-021-00538-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from Servicio Canario de Salud but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with the permission of Servicio Canario de Salud.