Abstract
Objectives:
To examine the association between HIV laws, perceived community stigma, and behaviors and to compare differences between and within Black and White men who have sex with men (MSM).
Design/Methods:
National HIV Behavioral Surveillance conducted interviews and HIV testing with MSM in 23 U.S. cities in 2017 using venue-based sampling methods. We used weighted cross-sectional data to compare MSM living in states with versus without HIV laws using Rao–Scott chi-square tests. We modeled the association between stigma and state HIV laws within racial groups to obtain adjusted prevalence ratios (aPR) and 95% confidence intervals (CIs).
Results:
Among 7392 MSM, 56% lived in a state with HIV laws. In law states, Black MSM were more likely than White MSM to report their community would discriminate against persons with HIV (PWH) (59 versus 34%), not support the rights of PWH (20 versus 9%), not be friends with PWH (19 versus 10%), believe PWH ‘got what they deserved’ (27 versus 16%), and be intolerant of MSM (14 versus 5%). Adjusted for confounders, Black MSM in HIV law states were more likely to think their community would discriminate against PWH (aPR, 1.14; 95% CI, 1.02–1.29; P = 0.02) and be intolerant toward MSM (aPR, 2.02; 95% CI, 1.43–2.86; P < 0.001) than Black MSM in states without such laws.
Conclusions:
HIV laws were related to higher stigma, but only for Black MSM. Future research regarding HIV-related laws should account for racial/ethnic disparities. Modernizing laws can delegitimize stigma and promote focusing on effective HIV prevention strategies.
Keywords: African Americans, HIV, HIV laws, men who have sex with men, policy, stigma, surveillance
Introduction
In the early years of the HIV epidemic, most states enacted HIV laws that criminalized a range of behaviors, including those with negligible risk for transmitting HIV [1]. Fear, homophobia, and lack of knowledge led lawmakers to enact laws intended to punish persons with HIV (PWH), promoting myths of PWH as deceptive and dangerous [2]. HIV stigma [3] and discrimination toward gay, bisexual, or other men who have sex with men (MSM) and PWH persists today. In 2017, 34 states and two territories still had HIV criminalization laws [3]. PWH can still be prosecuted for very low or no-risk behaviors (e.g. spitting, biting, sex while virally suppressed) [3]. Globally, the inappropriate application of HIV criminalization laws is a serious human rights concern [4].
Legal and public health scholars have criticized HIV criminalization laws, which often do not require transmission risk nor account for advances in treatment or prevention [5] (e.g. viral suppression [6] or preexposure prophylaxis [PrEP]) [7]. Second, the laws do not require proving intent, awareness of status, nor actual harm [8], yet prosecution can result in severe penalties, including lengthy sentences [1] and sex-offender registration [3]. Third, the laws discriminate against PWH by prosecuting behavior legal for others [9], which legitimizes stigma [10,11]. Stigma is related to sexual risk behaviors and lower HIV testing [12]. Centers for Disease Control and Prevention (CDC) leaders editorialized, ‘It is time to align with science and consider reforming, rescinding, and revising the application of these laws for the sake of people with HIV and for the public’s health’ [13].
Black MSM experience disparities in HIV [14] and incarceration [15]; therefore, the role of racism needs to be considered in HIV-related laws. Racial disparities illuminate differences in how Black and White MSM are treated. Black persons are disproportionately arrested under HIV laws [16,17]. Between 1988 and 2014, 62% of Black men versus 39% of White men with HIV-related arrests in California were charged [18].
Structural (e.g. legal) and community factors have a larger impact on social norms than individual-level factors [19,20]. HIV laws neither reduce new diagnoses [21] nor curb sexual behaviors [22]. The laws disproportionately target persons who are gay or bisexual [20], sex workers [15], homeless [15], or already incarcerated [21]. Additionally, most people are unaware of their state’s HIV laws [9,13]. As such, these laws might not directly affect personal behaviors [13]. However, HIV laws reflect state values and can be related to community attitudes. Negative attitudes toward PWH may persist in these communities.
The objectives of this analysis were to compare characteristics of MSM living in states with versus without HIV laws and assess the association between living in an HIV law state and perceived community stigma among Black and White MSM.
Methods
Design
The CDC’s National HIV Behavioral Surveillance (NHBS) system collects cross-sectional data on populations at risk for HIV, including MSM, in 23 U.S. cities [23]. NHBS sampling procedures have been published previously [24]. MSM were recruited for interviews and HIV testing using venue-based sampling methods during June–December 2017. All participants provided informed consent.
Measures
HIV law status was defined as the presence of any state law criminalizing HIV-related behaviors as of August 2017 [3]. Figure 1 displays a map of states’ HIV criminalization laws and NHBS project areas.
Fig. 1. Map of state HIV criminalization laws and NHBS cities included in analysis – NHBS, 2017.
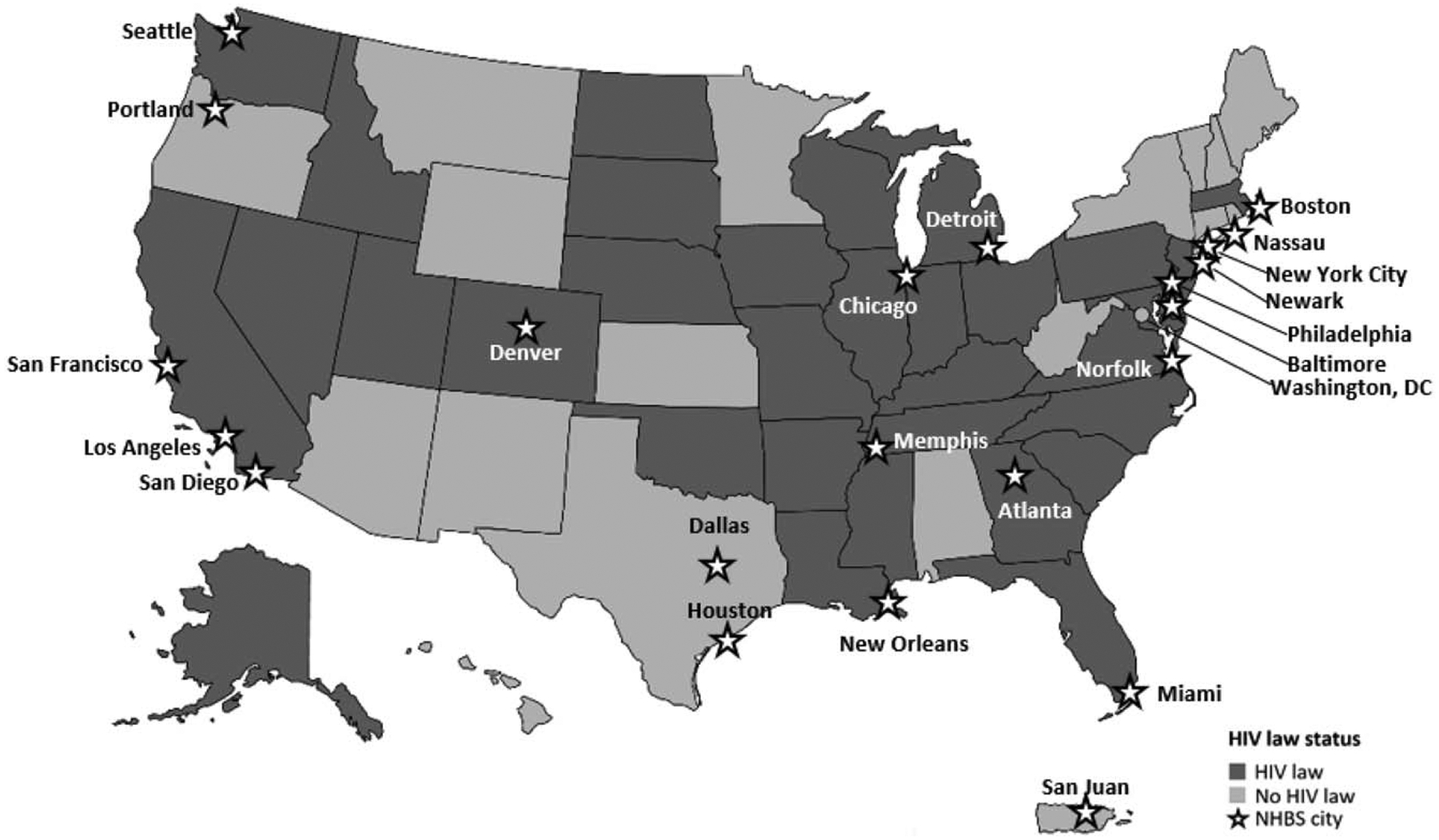
NHBS, National HIV Behavioral Surveillance. Source: Center for HIV Law & Policy, 2017.
Analyses were limited to Black or White MSM. Men were categorized as Black if they reported any Black racial identity. Single-race, multiracial, and Hispanic/Latino Black men reported similar characteristics and stigma. White men were defined as single-race and non-Hispanic to ensure mutual exclusivity.
We used the 2017 U.S. Department of Health and Human Services’ guidelines to define poverty based on participants’ household size and income [25]. Incarceration was defined as having been in jail, prison, or a detention center for >24 h during the previous 12 months.
We measured perceived community stigma (‘stigma’) based on an agreement to the following five statements from 1 (strongly disagree) to 5 (strongly agree): My community would discriminate against PWH, not support the rights of PWH, not be friends with PWH, believe that PWH ‘got what they deserved’, and is intolerant of gay/bisexual men. We combined strongly agree and agree answers and neutral, disagree, and strongly disagree answers. The items are not on a validated scale; we analyzed each question separately. MSM could recall any community that is relevant to them.
We asked if participants perceived same-sex discrimination, defined as verbal discrimination; poorer service; discrimination at work or school; or physical assault during the previous 12 months. We analyzed each question separately.
NHBS conducted rapid and confirmatory HIV testing. Status awareness was defined as concordance between self-reported and actual HIV test. All PrEP variables were limited to HIV-negative MSM: discussed PrEP with a provider or used PrEP in the past 12 months.
We measured condom use with the participant’s last anal sex partner with concordant, discordant, or unknown HIV status. We defined exchange sex as giving or receiving sex for money or drugs with another man during the previous 12 months. The NHBS questionnaire is available online [26].
Analyses
We limited analyses to men who had had sex with another man during the previous 12 months, lived in a participating city, and identified as Black or White. Data were weighted to account for unequal selection probabilities, multiplicity, and nonresponse bias, allowing us to extrapolate to all venue-attending MSM in these cities.
We calculated weighted percentages and 95% confidence intervals (CIs) for all variables. We compared characteristics of MSM living in states with versus without HIV laws using Rao–Scott chi-square tests (P < 0.05). We suppressed variables with an unstable coefficient of variation because of sparse data [coefficient of variation (CV) > 0.30]. We assessed differences in stigma variables by HIV law between Black and White MSM.
We estimated unadjusted and adjusted prevalence ratios (uPR and aPR) using logistic regression models with predicted marginal means to compare stigma within each racial group living in states with versus without HIV criminalization laws. Each stigma variable was a separate outcome. We selected covariates on the basis of literature or a priori interest. We analyzed the association between law and HIV stigma, controlling for age, education, incarceration, community intolerance of MSM, and self-reported HIV status. The model assessing law and intolerance toward MSM controlled for age, education, region, and same-sex discrimination. We conducted all analyses using SAS 9.4 and SUDAAN.
Results
Among 7392 MSM, 56.4% overall, 64.5% of Black MSM, and 48.6% of White MSM lived in a state with HIV criminalization laws (data not shown).
MSM living in HIV law states were more likely than MSM living in states without laws to report poverty, incarceration, or homelessness (Table 1). Compared with MSM living in states without HIV laws, MSM in law states were more likely to have a diagnosed HIV infection (22.5 versus 15.5%; P < 0.001). However, we observed no differences in partner notification, discussing PrEP with providers, PrEP use, condomless anal sex, knowledge of partner’s HIV status, or exchange sex.
Table 1.
Differences in socio-economic, behavioral, and HIV testing and prevention among Black and White men who have sex with men (MSM) living in states with versus without HIV criminalization laws (n = 7392) – NHBS, 2017.
| HIV law statusa | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total (n = 7392) | Law (n = 4931) | No law (n = 2461) | ||||||||
| No. | %b | 95% CI | No. | %b | 95% CI | No. | %b | 95% CI | P-value | |
| Race/ethnicityc | <0.001 | |||||||||
| Black | 3844 | 49.7 | 46.7, 52.6 | 2963 | 56.6 | 52.8, 60.5 | 881 | 40.7 | 36.5, 44.8 | |
| White | 3548 | 50.3 | 47.4, 52.3 | 1968 | 43.4 | 39.5, 47.2 | 1580 | 59.3 | 55.2, 63.5 | |
| Age (years) | 0.33 | |||||||||
| 18–29 | 2860 | 39.8 | 37.5, 42.1 | 1917 | 38.6 | 35.8, 41.5 | 943 | 41.3 | 37.6, 45.1 | |
| 30–39 | 2118 | 28.9 | 27.2, 30.5 | 1388 | 28.6 | 26.5, 30.6 | 730 | 29.2 | 26.5, 31.9 | |
| 40–49 | 1113 | 15.2 | 13.8, 16.6 | 759 | 15.5 | 13.7, 17.3 | 354 | 14.7 | 12.6, 16.8 | |
| 50+ | 1301 | 16.2 | 14.5, 17.8 | 867 | 17.3 | 15.1, 19.4 | 434 | 14.7 | 12.4, 17.1 | |
| Povertyd | <0.001 | |||||||||
| Above poverty level | 5905 | 84.6 | 83.0, 86.3 | 3725 | 80.6 | 78.3, 82.9 | 2180 | 89.9 | 87.8, 91.9 | |
| At or below poverty level | 1424 | 15.3 | 13.8, 17.0 | 1159 | 19.4 | 17.1, 21.7 | 265 | 10.1 | 8.1, 12.2 | |
| Incarceration history | 0.01 | |||||||||
| Never incarcerated | 5636 | 78.9 | 77.3, 80.5 | 3636 | 76.9 | 74.8, 79.0 | 2000 | 81.5 | 79.2, 83.8 | |
| Incarcerated over 12 months ago | 1371 | 16.2 | 14.8, 17.5 | 1000 | 17.4 | 15.7, 19.1 | 371 | 14.5 | 12.4, 16.7 | |
| Incarcerated, past 12 months | 384 | 4.9 | 4.1, 5.8 | 294 | 5.7 | 4.5, 6.8 | 90 | 4.0 | 2.8, 5.2 | |
| Homeless, past 12 months | 0.02 | |||||||||
| No | 6756 | 92.3 | 91.2, 93.3 | 4448 | 91.2 | 89.7, 92.7 | 2308 | 93.7 | 92.3, 95.1 | |
| Yes | 636 | 7.7 | 6.7, 8.8 | 483 | 8.8 | 7.3, 10.3 | 153 | 6.3 | 4.9, 7.7 | |
| Regione | 0.06 | |||||||||
| South | 3035 | 41.1 | 38.1, 44.1 | 2121 | 38.7 | 34.5, 42.8 | 914 | 44.2 | 40.2, 48.3 | |
| Non-South | 4357 | 58.9 | 55.9, 61.9 | 2810 | 61.3 | 57.2, 65.5 | 1547 | 55.8 | 51.7, 59.8 | |
| Ever received an HIV test | 0.22 | |||||||||
| No | 260 | 3.7 | 3.1, 4.4 | 168 | 3.4 | 2.6, 4.2 | 92 | 4.2 | 3.1, 5.3 | |
| Yes | 7125 | 96.3 | 95.6, 96.9 | 4759 | 96.6 | 95.8, 97.4 | 2366 | 95.8 | 94.7, 96.9 | |
| HIV test, past 12 months | <0.001 | |||||||||
| Not tested, HIV-negative | 1344 | 17.1 | 15.6, 18.5 | 840 | 15.1 | 13.4, 16.8 | 504 | 19.5 | 17.1, 22.0 | |
| Not tested, HIV+ over 12 months ago | 1447 | 19.5 | 17.7, 21.3 | 1102 | 22.4 | 19.9, 24.9 | 345 | 15.8 | 13.3, 18.3 | |
| Tested, past 12 months | 4560 | 63.4 | 61.5, 65.4 | 2958 | 62.5 | 59.8, 65.2 | 1602 | 64.7 | 61.7, 67.6 | |
| Awareness of HIV statusf | <0.001 | |||||||||
| Unaware of HIV infection | 291 | 3.2 | 2.5, 3.8 | 239 | 3.6 | 2.8, 4.5 | 52 | 2.6 | 1.7, 3.5 | |
| Aware of HIV infection | 1447 | 19.4 | 17.6, 21.3 | 1108 | 22.5 | 19.9, 25.1 | 339 | 15.5 | 13.0, 18.0 | |
| HIV-negative | 5002 | 69.6 | 67.5, 71.6 | 3141 | 66.3 | 63.6, 69.0 | 1861 | 73.8 | 70.7, 76.8 | |
| Talked to a counselor about HIV prevention, past 12 months | 0.38 | |||||||||
| No | 5074 | 71.2 | 69.3, 73.1 | 3257 | 70.4 | 68.0, 72.9 | 1817 | 72.2 | 69.3, 75.1 | |
| Yes | 2318 | 28.8 | 26.9, 30.7 | 1674 | 30.0 | 27.1, 32.0 | 644 | 27.9 | 25.0, 30.7 | |
| Visited a provider, past 12 months | 0.6 | |||||||||
| No | 918 | 12.7 | 11.4, 13.9 | 613 | 13.0 | 11.4, 14.6 | 305 | 12.3 | 10.3, 14.3 | |
| Yes | 6472 | 87.3 | 86.1, 88.6 | 4316 | 87.0 | 85.4, 88.6 | 2156 | 87.7 | 85.7, 89.7 | |
| Participant was asked to give partner names after HIV+ test for notification | 0.23 | |||||||||
| No | 488 | 34.6 | 30.5, 38.8 | 352 | 36.5 | 31.1, 41.8 | 136 | 31.4 | 25.0, 37.8 | |
| Yes | 1019 | 65.4 | 61.3, 69.5 | 791 | 63.5 | 58.2, 68.9 | 228 | 68.6 | 62.2, 75.0 | |
| Participant gave partner names for notification (HIV+ only) | 0.68 | |||||||||
| No | 648 | 45.9 | 41.6, 50.2 | 462 | 46.6 | 41.0, 52.2 | 186 | 44.7 | 38.3, 51.1 | |
| Yes | 856 | 54.1 | 49.8, 58.4 | 679 | 53.4 | 47.8, 59.1 | 177 | 55.3 | 48.9, 61.7 | |
| Discussed PrEP with a provider, past 12 months (HIV-negative only) | 0.62 | |||||||||
| No | 2970 | 57.0 | 54.7, 59.4 | 1904 | 57.6 | 54.5, 60.7 | 1066 | 56.4 | 52.8, 59.9 | |
| Yes | 2028 | 43.0 | 40.6, 45.3 | 1234 | 42.4 | 39.3, 45.5 | 794 | 43.6 | 40.0, 47.2 | |
| Used PrEP, past 12 months (HIV-negative only) | 0.52 | |||||||||
| No | 3709 | 72.9 | 70.6, 75.2 | 2346 | 72.1 | 69.3, 75.0 | 1363 | 73.7 | 70.0, 77.4 | |
| Yes | 1289 | 27.1 | 24.8, 29.4 | 792 | 27.9 | 25.1, 30.7 | 497 | 26.3 | 22.6, 30.0 | |
| Knew last sex partner’s HIV status, past 12 months | 0.38 | |||||||||
| No | 2351 | 32.0 | 30.2, 33.7 | 1543 | 31.3 | 29.0, 33.5 | 808 | 32.8 | 30.1, 35.6 | |
| Yes | 4997 | 68.0 | 66.3, 69.8 | 3353 | 68.7 | 66.5, 71.0 | 1644 | 67.2 | 64.4, 70.0 | |
| Anal sex with last partner, past 12 months | 0.20 | |||||||||
| Used condoms, concordant partner | 6137 | 82.9 | 81.5, 84.4 | 4106 | 84.0 | 82.2, 85.7 | 2031 | 81.6 | 79.3, 84.0 | |
| Condomless sex, discordant partner | 386 | 5.7 | 4.7, 6.6 | 263 | 5.6 | 4.5, 6.8 | 123 | 5.7 | 4.2, 7.2 | |
| Condomless sex, unknown HIV status partner | 831 | 11.4 | 10.2, 12.6 | 532 | 10.4 | 8.9, 12.0 | 299 | 12.7 | 10.7, 14.6 | |
| Exchange sex, past 12 monthsg | 0.06 | |||||||||
| No | 6655 | 91.4 | 90.3, 92.5 | 4370 | 90.5 | 89.0, 91.9 | 2285 | 92.7 | 91.0, 94.4 | |
| Yes | 2458 | 8.6 | 7.5, 9.7 | 558 | 9.5 | 8.1, 11.0 | 173 | 7.3 | 5.6, 9.0 | |
CI, confidence interval; MSM, men who have sex with men; NHBS, National HIV Behavioral Surveillance; PrEP, preexposure prophylaxis.
State had any HIV criminalization law as of August 2017 according to the Center for HIV Law & Policy.
Column percentages are weighted; not all percentages sum to 100 due to missing or suppressed values; values suppressed if the coefficient of variance was >0.30.
Black people may identify as Hispanic/Latino ethnicity or other races; White people are single-race, non-Hispanic.
Poverty defined by 2017 DHHS federal poverty guidelines: https://www.federalregister.gov/documents/2017/01/31/2017-02076/annual-update-of-the-hhs-poverty-guidelines.
Southern states: AL, AR, DE, DC, FL, GA, KY, LA, MD, MS, NC, OK, SC, TN, TX, VA, WV.
Columns do not sum to 100% because invalid test results were not reported.
Gave or receive sex in exchange for drugs/money with another man in the past 12 months.
We observed racial differences in community stigma between MSM in states with versus without HIV laws (Table 2). Black MSM reported higher community stigma regardless of law status. In HIV law states, Black MSM were more likely than White MSM to say their community discriminates against PWH (58.5 versus 34.3%; P < 0.001), does not support the rights of PWH (19.7 versus 9.3%; P < 0.001), would not be friends with PWH (18.5 versus 9.8%; P < 0.001), believes that PWH ‘got what they deserved’ (27.0 versus 15.7%; P < 0.001), and is intolerant toward MSM (13.8 versus 4.9%; P < 0.001). In HIV law states, Black MSM were less likely than White MSM to experience perceived discrimination during the previous 12 months (37.0 versus 41.6%; P = 0.03); we observed no racial differences in discrimination towards MSM in states without laws.
Table 2.
Differences in community stigma, same-sex discrimination, and incarceration history between MSM living in states with versus without HIV laws, stratified by race/ethnicity (n = 7392) – NHBS, 2017.
| Law | No law | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Black (n = 2963) | White (n = 1968) | Black (n = 881) | White (n = 1580) | |||||||||||
| No. | %b | 95% CI | No. | %b | 95% CI | P-value | No. | %b | 95% CI | No. | %b | 95% CI | P-value | |
| Most people in my community…. | ||||||||||||||
| …would discriminate against PWH | <0.001 | 0.001 | ||||||||||||
| Disagree/neutral | 1126 | 41.5 | 38.3, 44.7 | 1125 | 65.7 | 62.3, 69.1 | 426 | 48.8 | 44.0, 53.6 | 882 | 58.3 | 54.4, 62.1 | ||
| Agree | 1822 | 58.5 | 55.3, 61.7 | 687 | 34.3 | 30.9, 37.7 | 454 | 51.2 | 46.4, 56.0 | 560 | 41.7 | 37.9, 45.6 | ||
| …would not support rights of PWH | <0.001 | 0.04 | ||||||||||||
| Disagree/neutral | 2260 | 80.3 | 78.1, 82.5 | 1740 | 90.7 | 88.4, 92.9 | 726 | 84.3 | 80.7, 87.9 | 1415 | 88.8 | 86.2, 91.3 | ||
| Agree | 691 | 19.7 | 17.5, 21.9 | 219 | 9.3 | 7.1, 11.6 | 154 | 15.7 | 12.1, 19.3 | 162 | 11.2 | 8.7, 13.8 | ||
| …would not be friends with PWH | <0.001 | 0.11 | ||||||||||||
| Disagree/neutral | 2262 | 81.5 | 79.0, 84.0 | 1756 | 90.2 | 88.0, 92.4 | 746 | 86.1 | 82.7, 89.5 | 1443 | 89.6 | 86.9, 92.3 | ||
| Agree | 689 | 18.5 | 16.0, 21.0 | 205 | 9.8 | 7.6, 12.0 | 133 | 13.9 | 10.5, 17.3 | 134 | 10.4 | 7.7, 13.1 | ||
| …believe PWH ‘got what they deserved’ | <0.001 | 0.001 | ||||||||||||
| Disagree/neutral | 2030 | 73.1 | 70.2, 75.9 | 1640 | 84.3 | 81.8, 86.8 | 680 | 78.4 | 74.7, 82.1 | 1380 | 86.5 | 84.1, 88.9 | ||
| Agree | 923 | 27.0 | 24.1, 29.8 | 321 | 15.7 | 13.2, 18.2 | 198 | 21.6 | 17.9, 25.3 | 199 | 13.5 | 11.1, 15.9 | ||
| …are intolerant towards gay/bisexual men | <0.001 | 0.004 | ||||||||||||
| Disagree/neutral | 2427 | 86.2 | 84.0, 88.3 | 1848 | 95.1 | 93.6, 96.6 | 801 | 93.3 | 91.2, 95.4 | 1529 | 96.7 | 95.5, 98.0 | ||
| Agree | 531 | 13.8 | 11.7, 16.0 | 119 | 4.9 | 3.4, 6.4 | 78 | 6.7 | 4.6, 8.8 | 50 | 3.3 | 2.0, 4.5 | ||
| Same-sex discrimination, past 12 months | 0.03 | 0.95 | ||||||||||||
| Any discriminationc | ||||||||||||||
| No | 1677 | 63.0 | 60.0, 66.1 | 1076 | 58.4 | 55.1, 61.6 | 527 | 61.6 | 56.9, 66.2 | 914 | 61.4 | 57.9, 64.8 | ||
| Yes | 1278 | 37.0 | 33.9, 40.0 | 889 | 41.6 | 38.4, 44.9 | 347 | 38.6 | 35.2, 42.1 | 662 | 38.6 | 35.2, 42.1 | ||
| Verbal discrimination | 0.002 | 0.31 | ||||||||||||
| No | 1998 | 72.5 | 69.6, 75.4 | 1227 | 65.8 | 62.7, 69.0 | 626 | 70.9 | 66.8, 75.1 | 1032 | 68.3 | 65.0, 71.7 | ||
| Yes | 964 | 27.5 | 24.6, 30.4 | 740 | 34.2 | 31.0, 37.3 | 255 | 29.1 | 24.9, 33.2 | 546 | 31.7 | 2.3, 35.0 | ||
| Poor service at restaurants, stores, etc. | 0.96 | 0.19 | ||||||||||||
| No | 2472 | 85.8 | 83.8, 87.9 | 1661 | 85.7 | 83.3, 88.2 | 730 | 86.9 | 84.0, 89.8 | 1388 | 89.3 | 87.1, 91.5 | ||
| Yes | 482 | 14.2 | 12.1, 16.2 | 302 | 14.3 | 11.8, 16.7 | 147 | 13.1 | 10.2, 16.0 | 187 | 10.7 | 8.5, 12.9 | ||
| Discrimination at work/school | 0.001 | 0.20 | ||||||||||||
| No | 2377 | 82.2 | 79.7, 84.7 | 1701 | 88.1 | 85.8, 90.4 | 738 | 86.1 | 82.9, 89.4 | 1397 | 88.7 | 86.2, 91.3 | ||
| Yes | 583 | 17.8 | 15.3, 20.3 | 258 | 11.9 | 9.6, 14.2 | 136 | 13.9 | 10.6, 17.1 | 181 | 11.3 | 8.7, 13.8 | ||
| Discrimination at healthcare settings | 0.33 | . | ||||||||||||
| No | 2877 | 98.2 | 97.3, 99.0 | 1904 | 97.5 | 96.5, 98.5 | . | . | . | . | . | . | ||
| Yes | 78 | 1.8 | 1.0, 2.7 | 57 | 2.5 | 1.5, 3.5 | . | . | . | . | . | . | ||
| Physically assaulted, past 12 months | 0.20 | 0.06 | ||||||||||||
| No | 2665 | 92.6 | 90.8, 94.4 | 1821 | 94.1 | 92.6, 95.6 | 809 | 92.7 | 90.4, 95.1 | 1488 | 95.1 | 93.7, 96.6 | ||
| Yes | 296 | 7.4 | 5.6, 9.2 | 147 | 5.9 | 4.4, 7.4 | 71 | 7.3 | 4.9, 9.6 | 91 | 4.9 | 3.4, 6.3 | ||
| Disclosed same-sex attraction to all groups | <0.001 | <0.001 | ||||||||||||
| No | 1215 | 42.1 | 38.8, 45.4 | 631 | 33.0 | 29.5, 36.4 | 363 | 42.6 | 37.6, 47.7 | 450 | 27.3 | 23.6, 30.9 | ||
| Yes | 1734 | 57.9 | 54.6, 61.2 | 1329 | 67.0 | 63.6, 70.5 | 515 | 57.4 | 52.3, 62.4 | 1124 | 72.7 | 69.1, 76.4 | ||
| Incarceration history* | <0.001 | <0.001 | ||||||||||||
| Never incarcerated | 2019 | 71.7 | 68.8, 74.6 | 1617 | 83.7 | 81.3, 86.2 | 651 | 75.0 | 71.1, 78.9 | 1349 | 85.9 | 83.0, 88.8 | ||
| Incarcerated over 12 months ago | 715 | 20.7 | 18.4, 23.0 | 285 | 13.1 | 11.0, 15.2 | 176 | 19.2 | 15.4, 23.0 | 195 | 11.4 | 8.7, 14.1 | ||
| Incarcerated past 12 months | 229 | 7.6 | 5.9, 9.3 | 65 | 3.2 | 1.8, 4.5 | 54 | 5.8 | 3.8, 7.9 | 36 | 2.7 | 1.3, 4.2 | ||
CI, confidence interval; MSM, mMen who have sex with men; NHBS, National HIV Behavioral Surveillance; PWH, people with HIV.
State had any HIV criminalization law as of August 2017 according to the Center for HIV Law & Policy.
Column percentages are weighted to account for sampling biases, nonresponse, and multiplicity and may not sum to 100% due to rounding. The sampling design and weighting methods allow inference to all venue-attending men who have sex with men living in cities.
In the past 12 months, experienced name calling/insults, received poor service, was treated unfairly at work/school, received worse healthcare, or were physically attacked because someone knew or assumed they were attracted to men.
Disclosed same-sex attraction to family, friends, healthcare provider, and women sex partners (if applicable).
Because stigma and HIV laws disproportionately affect Black men, we assessed models comparing community stigma between Black MSM in law versus no-law states (Table 3). Black MSM in states with HIV laws were more likely than Black MSM in states without HIV laws to think their community is intolerant of MSM (aPR, 2.02; 95% CI, 1.43–2.86) and would discriminate against PWH (aPR, 1.14; 95% CI, 1.02–1.29). In a similar analysis for White MSM, White MSM in HIV law states were less likely to think their community would discriminate against PWH (aPR, 0.82; 95% CI, 0.72–0.94) than White MSM in no-law states, but otherwise reported no differences in stigma.
Table 3.
Within-racial group comparison of stigma between MSM living in states with versus without HIV lawsa (n = 7392) – NHBS, 2017.
| Outcome | Black MSM (n = 3844) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Law (n = 2963) | No law (n = 881) | |||||||||||
| No. | %b | 95% CI | No. | %b | 95% CI | uPR | 95% CI | P-value | aPR | 95% CI | P-value | |
| My community… | ||||||||||||
| …would discriminate against people with HIV | 1822 | 58.5 | 55.3, 61.7 | 454 | 51.2 | 46.4, 56.0 | 1.14 | 1.02, 1.27 | 0.01 | 1.14c | 1.02, 1.29 | 0.02 |
| …would not support people with HIV’s rights to live and work wherever they want | 691 | 19.7 | 17.5, 21.9 | 154 | 15.7 | 12.1, 19.3 | 1.25 | 0.97, 1.62 | 0.08 | 1.13c | 0.86, 1.47 | 0.37 |
| …would not be friends with people with HIV | 689 | 18.5 | 16.0, 21.0 | 133 | 13.9 | 10.5, 17.3 | 1.33 | 1.00, 1.76 | 0.04 | 1.16c | 0.86, 1.58 | 0.33 |
| …believes people with HIV ‘got what they deserved’ | 923 | 27.0 | 24.1, 29.8 | 198 | 21.6 | 17.9, 25.3 | 1.25 | 1.03, 1.52 | 0.02 | 1.19c | 0.96, 1.47 | 0.10 |
| …is intolerant of gay/bisexual men | 531 | 13.8 | 11.7, 16.0 | 78 | 6.7 | 4.6, 8.8 | 2.06 | 1.45, 2.91 | <0.001 | 2.02d | 1.43, 2.86 | <0.001 |
| Outcome | White MSM (n = 3548) | |||||||||||
| Law (n = 1968) | No law (n = 1580) | |||||||||||
| No. | %b | 95% CI | No. | %b | 95% CI | uPR | 95% CI | P-value | aPR | 95% CI | P-value | |
| My community… | ||||||||||||
| …would discriminate against people with HIV | 687 | 34.3 | 30.9, 37.7 | 560 | 41.7 | 37.9, 45.6 | 0.83 | 0.72, 0.95 | <0.01 | 0.82 | 0.72, 0.94 | <0.001 |
| …would not support people with HIV’s rights to live and work wherever they want | 219 | 9.3 | 7.1, 11.6 | 162 | 11.2 | 8.7, 13.8 | 0.83 | 0.60, 1.16 | 0.28 | 0.79 | 0.56, 1.11 | 0.17 |
| …would not be friends with people with HIV | 205 | 9.8 | 7.6, 12.0 | 134 | 10.4 | 7.7, 13.1 | 0.95 | 0.68, 1.33 | 0.75 | 0.9 | 0.64, 1.27 | 0.17 |
| …believes people with HIV ‘got what they deserved’ | 321 | 15.7 | 13.2, 18.2 | 199 | 13.5 | 11.1, 15.9 | 1.16 | 0.91, 1.48 | 0.22 | 1.12 | 0.87, 1.45 | 0.37 |
| …is intolerant of gay/bisexual men | 119 | 4.9 | 3.4, 6.4 | 50 | 3.3 | 2.0, 4.5 | 1.50 | 0.91, 2.45 | 0.11 | 1.55 | 0.94, 2.56 | 0.08 |
aPR, adjusted prevalence ratio; CI, confidence interval; NHBS, National HIV Behavioral Surveillance; uPR, unadjusted prevalence ratio.
State had any HIV criminalization law as of August 2017 according to the Center for HIV Law & Policy.
Column percentages are weighted to account for sampling biases, nonresponse, and multiplicity and may not sum to 100% due to rounding. The sampling design and weighting methods allow inference to all venue-attending men who have sex with men living in cities.
Models adjusted for age, education, incarceration history, community intolerance of gay/bisexual men, and self-reported HIV status.
Model adjusted for age, education, region, and personally experienced discrimination for being gay/bisexual in the past 12 months.
Discussion
Black MSM living in states with versus without HIV criminalization laws were more likely to think their community discriminates against PWH and is intolerant of MSM. For White MSM, HIV laws and stigma were mostly unrelated. These opposing results highlight how differently Black and White MSM experience stigma, discrimination, and HIV laws in their communities.
MSM in HIV law states were more likely to report characteristics associated with HIV-related arrests (e.g. poverty [10], homelessness [17], incarceration [21]). Our results support previous findings that HIV laws were unrelated to most individual behaviors [8]. We found no differences in knowledge of partner’s status, provider visits, partner notification, condom use, exchange sex, PrEP discussion with providers, or PrEP use, indicating that these laws have limited impact on behaviors.
Black MSM experience greater levels of social and political marginalization than White MSM or heterosexual Black men [27]. Intersectional dynamics of racism and homophobia contribute to HIV stigma [28,29]. For example, HIV laws were associated with higher perceived community stigma for Black MSM but not White MSM. Although our analysis was exploratory, this finding might be attributable to these laws historically and disproportionately targeting Black men and higher prevalence of community stigma in Black men’s communities.
Overall, community stigma was higher for Black MSM than for White MSM, regardless of state laws. This finding is consistent with other studies that found elevated levels of HIV stigma among Black communities [30]. Unmeasured factors likely contributed to community stigma, including internalized homophobia [31,32], religious communities that do not support homosexuality [33], and medical mistrust [34].
Homophobia is related to sexual risk behaviors [33] and social isolation [35]. Two times as many Black MSM in states with HIV laws said their communities were intolerant of MSM than Black MSM in no-law states and approximately four times as many as White MSM in no-law states. This concurs with a study reporting that HIV laws were related to structural stigma against MSM [36]. However, our findings that White MSM in HIV law states were more likely to experience perceived same-sex discrimination than Black MSM align with the literature [37,38].
The unequal application of HIV laws has further implications for Black communities, contributing to inequitable incarceration [11] and loss of voting rights and employment opportunities, which systemically limits Black persons’ political and economic power [39]. Future HIV law studies should account for how differently Black persons are affected and stratify results by race. Promoting social acceptance of PWH and homosexuality in the context of stigmatizing laws is needed [33].
Limitations
Our analysis has at least four limitations. First, NHBS is not generalizable to all MSM. Second, stigma cannot fully be attributed to HIV laws because of unmeasured factors, including local policies and unawareness of HIV–related laws. Due to the cross-sectional design and ecological analysis, we do not infer causality. Although we considered as many factors as possible, there is potential for ecologic fallacy. Third, the community stigma questions were developed specifically for NHBS and are not intended to scale together. Fourth, self-report data are subject to recall and social desirability biases.
Conclusions
HIV criminalization laws, a relic of the years before modern HIV treatment and prevention, are related to higher community HIV stigma, but only for Black MSM. States may consider modernizing HIV laws [10], focusing on effective HIV prevention efforts (e.g. treatment-as-prevention, PrEP). Stigma undermines these efforts [35]. Indeed, since 2014, five states have modernized their HIV laws [40]. Punishment is not an effective public health strategy [10]; modernizing these laws can help delegitimize HIV stigma and build a stigma-free future [13].
Acknowledgements
We thank National HIV Behavioral Surveillance participants, data management contractors, the CDC behavioral surveillance team, C. Kay Smith for technical editing, and the NHBS Study Group: Atlanta, GA: Pascale Wortley, Jeff Todd, David Melton; Baltimore, MD: Colin Flynn, Danielle German; Boston, MA: Monina Klevens, Rose Doherty, Conall O’Cleirigh; Chicago, IL: Stephanie Masiello Schuette, David Kern, Antonio D. Jimenez; Dallas, TX: Jonathon Poe, Margaret Vaaler, Jie Deng; Denver, CO: Alia Al-Tayyib, Melanie Mattson; Detroit, MI: Vivian Griffin, Emily Higgins, Mary-Grace Brandt; Houston, TX: Salma Khuwaja, Zaida Lopez, Paige Padgett; Los Angeles, CA: Ekow Kwa Sey, Yingbo Ma; Memphis, TN: Shanell L. McGoy, Meredith Brantley, Randi Rosack; Miami, FL: Emma Spencer, Willie Nixon, David Forrest; Nassau-Suffolk, NY: Bridget Anderson, Ashley Tate, Meaghan Abrego; New Orleans, LA: William T. Robinson, Narquis Barak, Jeremy M. Beckford; New York City, NY: Sarah Braunstein, Alexis Rivera, Sidney Carrillo Newark, NJ: Barbara Bolden, Afework Wogayehu, Henry Godette; Philadelphia, PA: Kathleen A. Brady, Chrysanthus Nnumolu, Jennifer Shinefeld; Portland, OR: Sean Schafer, E. Roberto Orellana, Amisha Bhattari; San Diego, CA: Anna Flynn, Rosalinda Cano; San Francisco, CA: H. Fisher Raymond, Theresa Ick; San Juan, PR: Sandra Miranda De León,Yadira Rolón-Colón; Seattle, WA: Tom Jaenicke, Sara Glick; Virginia Beach, VA: Celestine Buyu, Toyah Reid, Karen Diepstra; Washington, DC: Jenevieve Opoku, Irene Kuo; CDC: Monica Adams, Christine Agnew Brune, Qian An, Alexandra Balaji, Dita Broz, Janet Burnett, Johanna Chapin-Bardales, Melissa Cribbin, YenTyng Chen, Paul Denning, Katherine Doyle, Teresa Finlayson, Senad Handanagic, Brooke Hoots, Wade Ivy, Kathryn Lee, Rashunda Lewis, Lina Nerlander, Evelyn Olansky, Gabriela Paz-Bailey, Taylor Robbins, Catlainn Sionean, Amanda Smith, Anna Teplinskaya, Lindsay Trujillo, Cyprian Wejnert, Akilah Wise, Mingjing Xia.
Sources of funding:
Funding for the National HIV Behavioral Surveillance system is provided by the Centers for Disease Control and Prevention. This research was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the US Department of Energy and CDC.
Footnotes
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lehman JS, Carr MH, Nichol AJ, Ruisanchez A, Knight DW, Langford AE, et al. Prevalence and public health implications of state laws that criminalize potential HIV exposure in the United States. AIDS Behav 2014; 18:997–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mayer KH, Sohn A, Kippax S, Bras M. Addressing HIV criminalization: Science confronts ignorance and bias. J Int AIDS Soc 2018; 21:e25163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Center for HIV Law and Policy. State-by-state chart of HIV specific laws and prosecutorial tools. Available at: http://www.hivlawandpolicy.org/sites/default/files/State-by-State%20Chart%20of%20HIV-Specific%20Statutes%20and%20Prosecutorial%20Tools.%20%28final%208%2023%2017%29.pdf. [Accessed 24 March 2021]
- 4.UNAIDS. Criminalization HIV transmission. Available at: https://www.unaids.org/en/keywords/criminalization-hiv-transmission. [Accessed 24 March 2021]
- 5.American Academy of HIV Medicine. HIV criminalization. Available at: https://aahivm.org/hiv-criminalization/. [Accessed 24 March 2021]
- 6.Centers for Disease Control and Prevention. Treatment as prevention. Available at: https://www.cdc.gov/hiv/risk/art/index.html. [Accessed 24 March 2021]
- 7.Centers for Disease Control and Prevention. PrEP. Available at: https://www.cdc.gov/hiv/basics/prep.html. [Accessed 24 March 2021]
- 8.Yang YT, Underhill K. Rethinking criminalization of HIV exposure – lessons from California’s new legislation. N Engl J Med 2018; 378:1174–1175. [DOI] [PubMed] [Google Scholar]
- 9.Burris S, Cameron E. The case against criminalization of HIV transmission. JAMA 2008; 300:578–581. [DOI] [PubMed] [Google Scholar]
- 10.Hoppe T Punishing disease: HIV and the criminalization of sickness. Berkeley, CA: University of California Press; 2017. [Google Scholar]
- 11.Sykes BL, Hoppe TA, Maziarka KD. Cruel intentions? HIV prevalence and criminalization during an age of mass incarceration, U S 1999 to 2012 Medicine (Baltimore) 2016; 95:e3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Balaji ABB, Bowlers KE, Hess KL, Smith JC, Paz-Bailey G, NHBS Study Group. Association between enacted stigma and HIV-related risk behavior among MSM, National HIV Behavioral Surveillance System, 2011. AIDS Behav 2017; 21:227–237. [DOI] [PubMed] [Google Scholar]
- 13.Mermin J, Valentine SS, McCray E. HIV criminalisation laws and ending the US HIV epidemic. Lancet HIV 2021; 8:e4–e6. [DOI] [PubMed] [Google Scholar]
- 14.McCree DH, Williams AM, Chesson HW, Beer L, Jeffries WL, Lemons A, et al. Changes in disparities in estimated HIV incidence rates among Black, Hispanic/Latino, and White men who have sex with men (MSM) in the United States, 2010–2015. J Acquir Immune Defic Syndr 2019; 81:57–62. [DOI] [PubMed] [Google Scholar]
- 15.English D, Carter JA, Bowleg L, Malebranche DJ, Talan AJ, Rendina HJ. Intersectional social control: the roles of incarceration and police discrimination in psychological and HIV-related outcomes for Black sexual minority men. Soc Sci Med 2020; 258:113121 doi: 10.1016/j.socscimed.2020.113121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harsono D, Galletly CL, O’Keefe E, Lazzarini Z. Criminalization of HIV exposure: a review of empirical studies in the United States. AIDS Behav 2017; 21:27–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cann D, Harrison SE, Qiao S. Historical and current trends in HIV criminalization in South Carolina: implications for the southern HIV epidemic. AIDS Behav 2019; 23 (Suppl 3):233–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hasenbush A, Miyashita A, Wilson B. HIV criminalization in California. Available at: https://williamsinstitute.law.ucla.edu/wp-content/uploads/HIV-Criminalization-CA-Dec-2015.pdf. [Accessed: 24 March 2021]
- 19.Krieger N. Epidemiology and the people’s health: theory and context. New York, NY: Oxford University Press; 2011. [Google Scholar]
- 20.Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health 2013; 13:482 doi: 10.1186/1471-2458-13-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sweeney P, Gray SC, Purcell DW, Sewell J, Babu AS, Tarver BA, et al. Association of HIV diagnosis rates and laws criminalizing HIV exposure in the United States. AIDS 2017; 31:1483–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Burris S, Beletsky L, Burleson JA, Case P, Lazzarini Z. Do criminal laws influence HIV risk behavior? An empirical trial. Arizona State Law J 2007; 39:1–53. [Google Scholar]
- 23.Paz-Bailey G, Raymond HF, Lansky A, Mermin J. Using the National HIV Behavioral Surveillance system to inform HIV prevention efforts in the United States. AIDS Behav 2014; 18 (Suppl 3):S233–236. [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance, 23 U.S. cities, 2017. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-special-report-number-22.pdf. [Accessed 24 March 2021]
- 25.Department of Health and Human Services. Annual update of the HHS poverty guidelines. 2017. Available at: https://www.federalregister.gov/documents/2017/01/31/2017-02076/annual-update-of-the-hhs-poverty-guidelines. [Accessed 24 March 2021]
- 26.National HIV Behavioral Surveillance. NHBS round 5 CAPI reference questionnaire. Available at: https://www.cdc.gov/hiv/pdf/statistics/systems/nhbs/NHBS_CRQ_R5_HET5.pdf. [Accessed 24 March 2021]
- 27.Bowleg L. Once you’ve blended the cake, you can’t take the parts back to the main ingredients’: Black gay and bisexual men’s descriptions and experiences of intersectionality. Sex Roles 2012; 68:754–767. [Google Scholar]
- 28.Quinn K, Bowleg L, Dickson-Gomez J. The fear of being Black plus the fear of being gay: the effects of intersectional stigma on PrEP use among young Black gay, bisexual, and other men who have sex with men. Soc Sci Med 2019; 232:86–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev 1991; 43:1241–1299. [Google Scholar]
- 30.Jeffries WL, Townsend ES, Gelaude DJ, Torrone EA, Gasiorowicz M, Bertolli J. HIV stigma experienced by young men who have sex with men (MSM) living with HIV infection. AIDS Educ Prev 2015; 27:58–71. [DOI] [PubMed] [Google Scholar]
- 31.Jeffries WL, Gelaude DJ, Torrone EA, Gasiorowicz M, Oster AM, Spikes PS, et al. Unhealthy environments, unhealthy consequences: experienced homonegativity and HIV infection risk among young men who have sex with men. Glob Public Health 2017; 12:116–129. [DOI] [PubMed] [Google Scholar]
- 32.Glick SN, Golden MR. Persistence of racial differences in attitudes toward homosexuality in the United States. J Acquir Immune Defic Syndr 2010; 55:516–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jeffries WL, Marks G, Lauby J, Murrill CS, Millett GA. Homophobia is associated with sexual behavior that increases risk of acquiring and transmitting HIV infection among black men who have sex with men. AIDS Behav 2013; 17:1442–1453. [DOI] [PubMed] [Google Scholar]
- 34.Malebranche DJ, Peterson JL, Fullilove RE, Stackhouse RW. Race and sexual identity: perceptions about medical culture and healthcare among Black men who have sex with men. J Natl Med Assoc 2004; 96:97–107. [PMC free article] [PubMed] [Google Scholar]
- 35.Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, et al. HIV among Black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav 2014; 18:10–25. [DOI] [PubMed] [Google Scholar]
- 36.Tran NK, Hatzenbuehler ML, Goldstein ND. Potential relationship between HIV criminalization and structural stigma related to sexual orientation in the United States. J Acquir Immune Defic Syndr 2019; 80:e106–e108. [DOI] [PubMed] [Google Scholar]
- 37.Whiteman A, Baugher A, Sionean C, NHBS Study Group. Assessing self-reported discrimination among men who have sex with men (MSM). AIDS 2021; 35:141–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baugher AR, Beer L, Fagan JL, Mattson CL, Shouse RL, Medical Monitoring Project. Discrimination in healthcare settings among adults with recent HIV diagnoses. AIDS Care 2019; 31:1077–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brewer RA, Magnus M, Kuo I, Wang L, Liu TY, Mayer KH. Exploring the relationship between incarceration and HIV among black men who have sex with men in the United States. J Acquir Immune Defic Syndr 2014; 65:218–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. HIV and STD criminal laws. Available at: https://www.cdc.gov/hiv/policies/law/states/exposure.html. [Accessed 12 February 2021]


