Abstract
Objectives:
qigong, a traditional Chinese mind–body exercise, has been shown to improve balance and gait in several neurological conditions; however, community-delivered qigong has never been assessed for people with multiple sclerosis (MS). The authors assessed the feasibility of community qigong classes for people with MS and explored outcomes of balance, gait, and quality of life (QOL).
Design:
Twenty adults with MS were randomly assigned to 10 weeks of community qigong classes or wait-list control.
Settings/Location:
Portland, Oregon.
Subjects:
People with MS.
Intervention:
Community qigong classes.
Outcome measures:
Feasibility criteria included recruitment, retention, adherence, and ability to participate in qigong movements. Secondary outcome measures included physical tests of mobility, gait, and balance and participant-reported mobility, depression, anxiety, fatigue, and QOL.
Results:
Recruitment of eligible and interested people with MS was feasible. Retention in the trial was 60%. Completers attended a mean of 7 of 10 classes. All completers participated with no or minor modifications to qigong movements. Exploratory within-group analyses showed trends toward improved mental health, QOL, and reduced fatigue and depression. Several participants spontaneously reported improved energy, flexibility, sleep, and mobility.
Conclusions:
Community qigong may be a feasible form of exercise for people with MS. To improve retention and capture potential effects of qigong on physical function and quality of life, future studies might consider pragmatic trials with tiered level classes, simpler forms of qigong, and/or refined inclusion criteria (CTR#: NCT04585659).
Keywords: qigong, gait, multiple sclerosis, pragmatic design
Introduction
Multiple sclerosis (MS) is a chronic, progressive autoimmune disorder affecting the central nervous system.1 Neuronal damage results from demyelination and axonal loss, manifesting in cognitive, psycho-emotional, and physical symptoms, including fatigue, muscle weakness and spasticity, gait dysfunction, memory loss, anxiety, and depression.2 Up to 80% of people with MS experience walking impairment during the course of their disease.3 Problems with balance and gait are associated with increased risk of falls and injuries, impaired activities of daily living, and lower quality of life.4–6 Conventional treatments for walking impairment include medication (e.g., dalfampridine) and rehabilitation.3,7 Less than 50% of people with MS respond to medications for gait, speed, and endurance.8 Physical therapy and multidisciplinary rehabilitation have been found to have moderate impact.9 Community-based exercise programs may offer additional support for people with MS.
qigong is an ancient Chinese mind–body exercise involving physical movements, breathwork, and cognitive activities (e.g., visualization, body awareness, and meditation). qigong may benefit people with MS by combining gentle physical exercise and stretching with mindful movement and meditation. Moderate-intensity exercise has been shown to improve mobility, balance, fatigue, mood, and quality of life (QOL) for people with MS.10–15 Meditation and guided imagery have also shown benefits in mood, fatigue, and QOL for people with MS.16–18 Although the mechanisms of action remain unclear, some research suggests qigong functions similarly to other mind–body practices by promoting parasympathetic dominance of the autonomic nervous system, reducing gene expression of inflammatory cytokines, and improving metabolic and immune function and telomere maintenance.19 These benefits may be especially helpful to people for MS by improving mood, reducing inflammation, and increasing balance, strength, flexibility, and cognitive function.
Previous research has shown qigong to improve balance and gait in neurological conditions, including Parkinson's disease and fibromyalgia.20–22 qigong has also been shown to benefit fatigue and depression, common MS symptoms.21,23 The authors are aware of only one pilot study involving one-on-one qigong for 16 people with secondary progressive MS.24 Statistically significant improvements in depression and balance were observed after six sessions. However, small sample size, loss to follow-up, and nonvalidated questionnaires limited interpretation of the findings.
Based on promising results in other neurological conditions, the authors aimed to determine the feasibility of assessing qigong for MS, applying a randomized trial design with validated questions to assess outcomes. Because qigong is commonly taught in community classes, the primary objective of this study was to assess the feasibility of conducting research to evaluate community-delivered qigong classes for people with MS.
Materials and Methods
Study design
In this unmasked, parallel group, randomized clinical trial of qigong versus wait-list control for people with MS (n = 20), the authors employed a pragmatic design where participants attended weekly, pre-existing, public qigong classes for 10 weeks. Benefits of this design include the ability for participants to select a preferred instructor and qigong style, and class times and locations that fit their schedule. Feasibility criteria included a priori targets for recruitment, retention, adherence, and ability to participate in classes. The authors also explored preliminary effects of qigong on balance, gait, fatigue, and QOL.
Adults, aged 18 years and older, were recruited from the Portland Metropolitan Area. Inclusion criteria included self-reported diagnosis of MS (any type), demonstrated ability to walk 50 feet without assistance, and stable on disease-modifying or balance medications 3 months before baseline. Candidates who were pregnant or nursing; participated in qigong, Tai Chi, or yoga (>1 month) within 6 months before baseline; or had an MS relapse within 30 days before baseline were excluded. The authors confirmed that participants did not practice yoga, Tai Chi, or other qigong during the observation period, through check-in phone calls at weeks 1, 2, and 7 of the 10-week study. The study was conducted from January 2017 to March 2018. The study protocol was approved by the National University of Natural Medicine IRB and registered with ClinicalTrials.gov (CTR#: NCT04585659).
Randomization
After participants attended a baseline visit to provide written informed consent, confirm eligibility, and provide baseline measures, they were randomly assigned to a qigong group (QG) or wait-list control group (CG). A randomization scheme (block size = four) was pre-established by the statistician at the start of the study using SPSS software. A university staff member, who was not part of the study, maintained the randomization key, ensuring that research investigators were blinded to group allocation. At the end of the baseline visit, the study investigator received the group assignment for the participant through e-mail. Researchers and study participants were not blinded when administering surveys and physical tests at the second and third study visits.
Intervention
The QG attended 60- to 90-min community qigong classes weekly for 10 weeks and were asked to practice at least 10 min daily. At baseline, participants selected from a list of community qigong classes that included class times and locations, a description of the qigong style, and a brief biography of the instructor. Class instructors were preselected and required to have at least 5 years of teaching experience (including teaching people with limited mobility); teach weekly qigong classes open to any level; and offer movement modifications and seated options. The qigong styles available to participants were (1) dayan (wild goose) qigong, which included warm-up stretches, self-massage, and a 64-movement form; (2) jin jing gong (tendon and channel) qigong, which included shaking the body to warm up and a 5- to 12-movement form; (3) huo long jing (fire dragon meridian) qigong, which also included shaking warm-ups and a set of 7 movements; and (4) wu xing (5 element) qigong, which included stretching exercises and a 5-movement form. Classes involving any external martial arts or fighting component were excluded. Participants could switch classes once after their first class, if desired. The authors contacted participants after classes 1, 2, and 7 to ensure they felt comfortable and safe in class and to screen for adverse events (AEs). Final outcomes were measured after 10 weeks of qigong.
Control
The CG was advised to refrain from qigong, Tai Chi, or yoga during the 10-week parallel phase of the trial. Maintenance of pretrial exercise and other self-care was encouraged. Participants provided outcome measures at the second study visit (week 11), at which time they could opt to begin qigong classes for 10 weeks. Those who joined the qigong intervention (CGQ) were asked to attend a third study visit to provide outcome measures.
Outcome measures
Primary: feasibility
Feasibility was defined a priori and included the ability to recruit and enroll 20 participants in 8 months; participate in the community classes overall; retain 80% enrollment in the trial; and maintain 70% attendance in the qigong classes and practice at home 2 days/week. The ability to participate was based on participants' subjective report: full participation, partial, a little, or none. Participants unable to physically perform movements were encouraged to visualize them. To assess perceived challenges and benefits of the qigong intervention, any participant who attended at least one qigong class from both the QG and CGQ was asked to complete an exit survey at the end of their observed time in the study.
Secondary: clinical measures for MS
The authors assessed mobility, gait, and balance with the timed 25-foot walk test (T25FW),25,26 timed up and go test (TUG),27 and four square step test (FSST).28 The T25FW reliably measures walking ability for people with MS,25 with high test–retest reliability (intraclass correlation coefficient [ICC] of 0.99).26 The TUG tests muscle function and mobility, predicts safe walking ability, and correlates with other mobility tests (r = 0.81 correlation with the Berg Balance Scale, r = −0.61 for gait speed).27 The FSST is a validated measure of multidirectional mobility for MS, with high inter-rater (ICC = 0.99) and retest (ICC = 0.98) reliability.28
Additional validated self-report questionnaires were used to measure physical and psychological well-being. The MS Impact Scale (MSIS-29) has high internal consistency (Cronbach's α ≥0.91) and test–retest reliability (ICC ≥0.87).29 The MS Walking Scale (MSWS) has good test–retest reproducibility (ICC ≥0.78) and high internal reliability (Cronbach's α ≥0.94).30 The Modified Fatigue Impact Scale (MFIS-5) has high internal consistency (Cronbach's α of 0.80).31 Patient-Reported Outcomes Measurement Information System (PROMIS) measures included global health (v1.1) and computer-adaptive tests for physical function (v1.2), fatigue (v1.0), anxiety (v1.0), and depression (v1.0).32
Data analyses
The primary objective of this trial was feasibility, with a focus on methodology and intervention appropriateness. Descriptive statistics were calculated for feasibility outcomes. A sample size calculation was not included based on CONSORT guidelines for pilot and feasibility studies.33 For secondary outcomes, the authors present means and standard deviations for the QG and CG at baseline and follow-up and mean pre-post change with confidence intervals (95% CIs) within each group. The authors also present means and standard deviations of pre- and post-qigong measures for all participants who completed qigong (QG+CGQ) and 95% CIs for mean pre-post change. Because this was a feasibility study, the authors did not conduct an inferential analysis on secondary outcomes.33 Analyses were conducted in R (version 3.3.3).34
Results
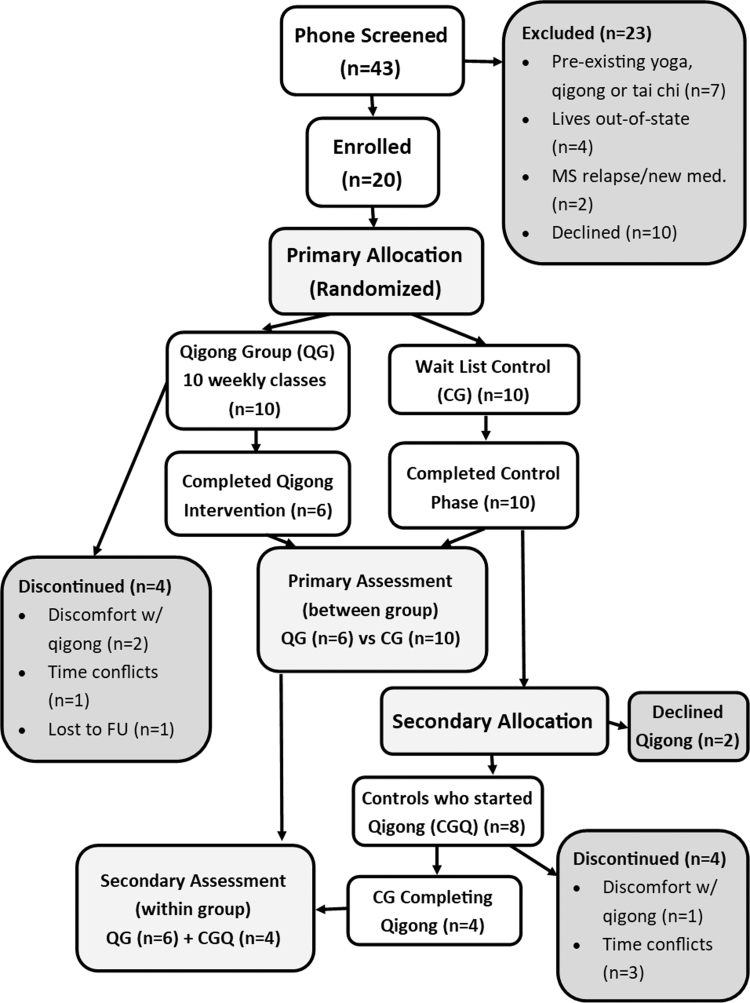
The authors screened 43 people; 23 were excluded or declined to participate and 20 were randomized (Fig. 1). Participants ranged in age from 30 to 71 years (average 44 ± 9.8 years; Table 1). The female:male ratio was 3:1; the majority (90%) had relapsing MS. Time since diagnosis ranged from <1 to 24 years (mean 9.9 ± 6.9 years).
FIG. 1.
Flow chart of enrollment and randomization to qigong and wait-list control groups and secondary allocation of wait-list control to qigong intervention.
Table 1.
Baseline Demographic and Clinical Characteristics of Study Participants
| Overall (n = 20) | qigong (n = 10) | Control (n = 10) | |
|---|---|---|---|
| Age in years, mean (SD) | 44 (9.8) | 42 (8.9) | 46 (10.6) |
| Sex | |||
| Female | 15 | 7 | 8 |
| Male | 4 | 2 | 2 |
| Decline to state | 1 | 1 | 0 |
| Education | |||
| High school graduate | 1 | 0 | 1 |
| Some college | 4 | 3 | 1 |
| College graduate | 8 | 4 | 4 |
| Postgraduate | 7 | 3 | 4 |
| Race/ethnicity | |||
| Caucasian | 18 | 8 | 10 |
| Hispanic/Latino | 2 | 2 | 0 |
| Type of MS | |||
| Relapsing remitting | 18 | 9 | 9 |
| Secondary progressive | 1 | 1 | 0 |
| Unknown | 1 | 0 | 1 |
| Years since MS diagnosis, mean (SD) | 9.9 (6.9) | 12.1 (6.9) | 7.7 (6.4) |
| Currently taking disease-modifying therapiesa | 10 | 4 | 6 |
| Currently taking balance medication | 0 | 0 | 0 |
| Severity of MS disability | |||
| Noneb | 3 | 1 | 2 |
| Mildc | 9 | 3 | 5 |
| Moderated | 8 | 6 | 3 |
| Activity level | |||
| Vigorous exercise ≥weekly | 12 | 5 | 7 |
| Moderate exercise ≥weekly | 19 | 9 | 10 |
| Prior experience with qigong, Tai Chi, other martial arts, or yoga | 13 | 5 | 8 |
Disease-modifying therapies (medications) included rebif (1), copaxone (1), tecfidera (4), tysabri (1), extavia (1), and rituxan (2).
No or minimal MS symptoms, no limitations in walking ability, and no limitations in daily activities.
Noticeable MS symptoms, but no limitations in walking ability or daily activities, and can walk at least one block without support.
Many MS symptoms that affect daily activities, but can walk at least one block without support.
MS, multiple sclerosis.
Of the 10 QG participants, 4 discontinued: 2 reported discomfort with qigong, 1 had scheduling conflicts, and 1 gave no reason (Fig. 1). All 10 in the CG were retained at the 11-week follow-up; 1 person was unable to complete physical assessments due to relapse, but completed required questionnaires. Eight CG participants opted to continue with the 10-week qigong intervention. Of these, four withdrew: one reported discomfort with qigong movements and three reported scheduling conflicts (Fig. 1).
Eight of the QG participants selected the wild goose (dayan) form and two selected the tendon and channel (iin iing) form. For the CGQ, seven selected the dayan classes and one joined the jin jing class.
Primary outcome measures: feasibility
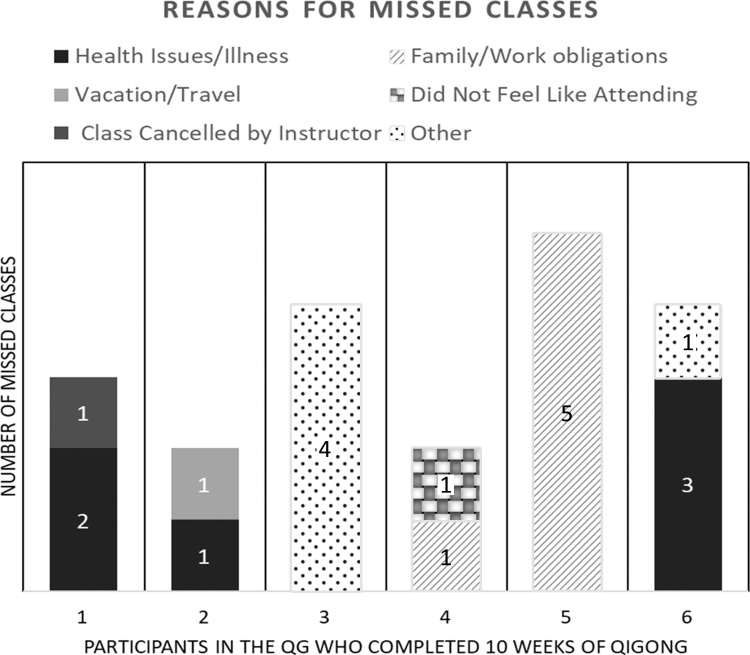
Twenty participants were recruited in 9 months. Retention in the QG was 60% (n = 6) and 100% (n = 10) for the CG. Participants who completed the qigong intervention (n = 6) attended a mean of 7 (±1.27) of 10 weeks of classes and practiced at home for at least 5 min an average of 4 (±1.58) days per week. Fifty percent (3 of 6 participants) in the QG attended 70% or more classes and 100% attended 50% or more classes. The proportions were the same when including the CGQ participants who completed qigong. Reasons for missing classes included health issues/illness, vacation/travel, family/work obligations, not feeling like attending, and one class cancellation (Fig. 2). Among the four CG participants who dropped out, three attended only the first class before discontinuing and one attended at least the first two classes, but was lost to follow-up with total class attendance not accurately captured.
FIG. 2.
Reasons for missed classes among participants who were randomized to the qigong group in the parallel phase and completed the 10-week intervention. Each bar represents an individual participant. Reasons for missed classes: • Health Issues/Illness (black) • Vacation/Travel (light gray) • Class Canceled by Instructor (dark gray) • Family/Work Obligations (lines) • Did Not Feel Like Attending (checkered) • Other (dotted).
Of the 20 participants enrolled, 15 completed the exit survey: 6 QG participants who completed the intervention and 1 who withdrew; and 4 CGQ participants who completed the intervention and 4 who withdrew (Supplementary Table S1). Fifty percent reported that they could fully participate in classes and 50% reported participation with some modification (≤25%) of movements. Most (79%) reported feeling comfortable in class with people who did not have MS.
Secondary outcome measures
The authors observed little difference in physical function and QOL measures between groups (Table 2). Results of exploratory pre-post analyses (within-group change) for completers (QG+CGQ) are presented in Table 3. Mean PROMIS mental health scores improved ∼3 points (2.92, 95% CI: 0.17–5.67, Table 3). Both MFIS and the PROMIS fatigue subscale suggested reduced fatigue (−13 points, 95% CI: −26.51 to 0.51, and −4.56 points, 95% CI: −10.13 to 1.01, respectively), following the qigong intervention (Table 3).
Table 2.
Mean Change in Exploratory Outcome Measures for Participants Who Completed 10 Weekly qigong Classes or Wait-List Control
| Control (n = 10) qigong (n = 6) | Baseline mean (SD) | Follow-up mean (SD) | Change mean (95% CI) |
|---|---|---|---|
| T25FW | |||
| Controla | 5.13 (1.10) | 5.16 (1.10) | 0.03 (−0.23 to 0.29) |
| qigong | 5.23 (0.97) | 5.72 (1.16) | 0.49 (0.13 to 0.85) |
| TUG | |||
| Controla | 7.95 (1.35) | 7.66 (1.13) | −0.29 (−0.71 to 0.12) |
| qigong | 7.72 (1.93) | 8.13 (2.34) | 0.41 (−0.48 to 1.30) |
| FSST | |||
| Controla | 9.75 (2.39) | 9.22 (1.53) | −0.52 (−1.45 to 0.40) |
| qigong | 10.22 (1.73) | 9.62 (1.56) | −0.59 (−1.26 to 0.07) |
| MFIS | |||
| Control | 45.0 (23.57) | 41.5 (26.15) | −3.50 (−11.05 to 4.05) |
| qigong | 60.83 (18.00) | 48.33 (18.07) | −12.50 (−34.70 to 9.70) |
| MSIS-29 | |||
| Control | 42.69 (15.60) | 42.21 (15.99) | −0.48 (−3.51 to 2.54) |
| qigong | 44.02 (10.00) | 47.36 (13.58) | 3.33 (−11.45 to 18.12) |
| MSWS12 | |||
| Control | 36.17 (14.61) | 38.17 (18.14) | 2.0 (−3.70 to 7.70) |
| qigong | 49.44 (19.99) | 54.16 (25.47) | 4.7 (−9.59 to 19.04) |
| PROMIS | |||
| Global health (mental) | |||
| Control | 43.48 (6.65) | 45.49 (7.16) | 2.01 (−1.97 to 5.99) |
| qigong | 43.60 (8.93) | 47.87 (10.11) | 4.27 (−0.12 to 8.64) |
| Global health (physical) | |||
| Control | 45.85 (7.26) | 46.76 (8.19) | 0.91 (−1.37 to 3.19) |
| qigong | 41.55 (7.45) | 41.93 (3.19) | 0.38 (−6.37 to 7.14) |
| Anxiety | |||
| Control | 59.01 (8.31) | 57.29 (5.91) | −1.72 (−4.41 to 0.97) |
| qigong | 57.27 (3.76) | 57.03 (8.02) | −0.23 (−9.05 to 8.58) |
| Depression | |||
| Control | 54.42 (9.02) | 52.93 (7.14) | −1.49 (−4.56 to 1.58) |
| qigong | 54.58 (5.72) | 53.32 (5.58) | −1.27 (−6.23 to 3.70) |
| Fatigue | |||
| Control | 54.66 (10.48) | 58.15 (10.47) | 3.49 (0.17 to 6.81) |
| qigong | 59.85 (6.49) | 59.22 (5.39) | −0.63 (−6.35 to 5.08) |
| Physical function | |||
| Control | 44.98 (6.94) | 44.44 (5.10) | −0.54 (−2.19 to 1.11) |
| qigong | 43.95 (6.59) | 41.38 (7.75) | −2.56 (−6.98 to 1.85) |
n = 9 for T25FW, TUG, and FSST in the control group, as one participant was unable to complete the physical tests due to exacerbation of MS symptoms.
CI, confidence interval; FSST, four square step test (measured in sec); MFIS, Modified Fatigue Impact Scale; MSIS-29, Multiple Sclerosis Impact Scale; MSWS12, Multiple Sclerosis Walking Scale; PROMIS, Patient-Reported Outcomes Measurement Information System; T25FW, timed 25-foot walk test (measured in sec); TUG, timed up and go test (measured in sec).
Table 3.
Mean Change in Exploratory Outcome Measures for all Participants Who Completed 10 Weeks of qigong (n = 10)
| Pre-qigong mean (SD) | Post-qigong mean (SD) | Mean change (95% CI) | |
|---|---|---|---|
| T25FW | 4.97 (0.85) | 5.28 (1.06) | 0.31 (0.04 to 0.58) |
| TUG | 7.42 (1.54) | 7.54 (1.98) | 0.12 (−0.52 to 0.72) |
| FSST | 9.38 (1.71) | 8.95 (1.54) | −0.42 (−0.89 to 0.04) |
| MFIS | 53.50 (21.86) | 40.50 (18.02) | −13.00 (−26.51 to 0.51) |
| MSIS-29 | 43.10 (12.58) | 40.90 (13.37) | −2.21 (−12.89 to 8.48) |
| MSWS12 | 43.67 (17.70) | 43.33 (23.77) | −0.33 (−9.43 to 8.76) |
| PROMIS | |||
| Global health (mental) | 46.22 (8.77) | 49.14 (8.84) | 2.92 (0.17 to 5.67) |
| Global health (physical) | 43.72 (6.92) | 45.96 (6.10) | 2.24 (−1.79 to 6.26) |
| Anxiety | 58.14 (5.18) | 57.07 (6.25) | −1.07 (−6.05 to 3.91) |
| Depression | 53.54 (7.43) | 50.62 (6.34) | −2.92 (−6.83 to 0.99) |
| Fatigue | 59.72 (6.93) | 55.16 (7.88) | −4.56 (−10.13 to 1.01) |
| Physical function | 43.96 (5.56) | 44.23 (7.52) | 0.27 (−3.55 to 4.09) |
CI, confidence interval; FSST, four square step test; MFIS, Modified Fatigue Impact Scale; MSIS-29, Multiple Sclerosis Impact Scale; MSWS12, Multiple Sclerosis Walking Scale; PROMIS, Patient-Reported Outcomes Measurement Information System; T25FW, timed 25-foot walk test; TUG, timed up and go test.
Adverse events
Three AEs possibly related to qigong were reported. One involved lower back pain that interfered with usual activities. The onset did not coincide with a qigong class, but qigong stretching may have aggravated the pain. Another involved increased leg spasticity after discontinuing daily stretching during the qigong intervention. The third case involved mild back pain at the onset of qigong that resolved after a week. No serious AEs were reported.
Discussion
The authors found community qigong classes feasible for some people with MS with high physical function. Recruitment goals were achieved in roughly the expected time frame. Participants experienced minimal burden taking surveys and physical tests. Adherence met the authors' expectations, with well-attended classes and regular home practice. Participants mentioned day, time, and location as important factors in selecting a class, preferring mid-to-late morning and weekends for those with weekday jobs.
Attrition was higher than expected, although within the range observed in Tai Chi for MS studies (5.3%–43%).35 Psychological discomfort with qigong was given as one reason for attrition. Some qigong forms involve shaking and vocalizations and two participants dropped out because they felt uncomfortable with this. Mills and Allen similarly reported minor attrition due to dislike of exercises.36 Another participant dropped out, in part, because he felt self-conscious modifying movements when others were not. One participant reported feeling intimidated by joining a pre-existing class with more experienced students who did not have MS.
Another reason given for attrition was difficulty committing to classes and home practice. Committing to regular movement classes and home practice can be difficult, especially for those with chronic illness.37–40 For people with MS, committing to regular qigong may be challenging due to the unpredictability of MS symptoms, including fatigue and physical disability.41
qigong classes may have been too advanced or complex for some participants.42 Mills recommends gentle meditative styles of qigong for people with MS.42 In this study, the jin jing and huo long jing forms were more rigorous, while the dayan form was gentle, but complex. The qigong style should be considered to enhance retention in future studies.
Trends in improvements in global mental health and reduced fatigue from exploratory within-group analyses warrant additional research. In addition, all participants who completed the intervention qualitatively reported positive benefits from qigong, including improved energy, mood, flexibility, sleep, and mobility, on the exit survey.
Participants who reported AEs possibly related to qigong, including back pain and leg spasticity, had prior histories of these symptoms that may have been exacerbated by certain qigong movements. Wayne et al. found that the most common complaints in Tai Chi studies for any patient group were musculoskeletal aches and pain, particularly knee, ankle, and back pain, although most studies failed to report AEs.43 Ensuring that people with MS receive support with modifications is an important consideration before enrolling in a qigong class. Future studies should consider modification of any movement that may exacerbate MS symptoms.
A strength of this study was the pragmatic design, which enabled assessment of qigong in a real-world setting. qigong involves a complex set of physical, cognitive, and psycho-social elements, including the environment, instructor, and group setting.44 Pragmatic designs encapsulate these factors and may better reflect actual adherence and health outcomes.45 One pragmatic Tai Chi study of women with osteopenia reported adherence attributed to support and encouragement from experienced students, community-building opportunities, and ability to continue classes after study termination.46 The participants reported being motivated to attend class, in part, because they liked the support of the instructor and fellow students. If qigong is deemed feasible and effective in people with MS, future studies might assess the specific impact of such factors on health outcomes.
Limitations
This study was limited by a small sample size and attrition. The intervention included multiple qigong styles and the small sample size also precluded the authors' ability to assess the impact of this heterogeneity on health outcomes. Neither participants nor outcome assessors were blinded. Participants who discontinued could have had negative outcomes that were uncaptured, which may have overestimated qigong effects in the within-group analysis. Within-group improvements may reflect a regression to the mean or spontaneous improvement rather than an effect from qigong. Participants had high physical function, which may have reduced the capacity to detect improvements in physical measures. Since most participants were non-Hispanic white, the authors were not able to assess interest in qigong among other racial/ethnic groups.
Future directions
Retention was the greatest challenge in this study. Future studies should consider tailoring classes for beginners, offering a range of classes for different abilities, or having MS-specific classes. Seated forms may also accommodate people with greater levels of disability and would be more inclusive of the greater MS community. Additional research into appropriate forms of qigong for MS based on therapeutic principles and empirical findings is warranted.47 Litrownik et al. recommend protocol validity testing for Tai Chi interventions, such as the use of patient focus groups, a Delphi process to gain expert recommendations and feedback, and pilot testing.47 Observing effects of qigong on physical outcomes may require longer duration or higher dose interventions. Future studies might include an expanded qualitative component to better identify appropriate qigong styles, movements, dosage, frequency, duration, and mode of delivery that provide the greatest benefit for people with MS. Future studies might also consider the use of an active comparator, such as another form of exercise or educational component, rather than a wait-list control, to better control for nonspecific effects of attending qigong classes, such as attention from an instructor or time spent engaged in a group activity.
Conclusions
This pragmatic feasibility study provides a greater understanding of how people with MS experience community qigong classes. Community qigong may be feasible for people with MS with high physical function and may offer health benefits. Pooled pre- and post-qigong comparisons showed trends in improvement in global mental health, fatigue, and depression. Future studies of qigong tailored for beginners and modified for people with MS are warranted to explore the potential benefits of qigong for these outcomes.
Supplementary Material
Acknowledgments
The authors thank the study participants and qigong instructors.
Author Disclosure Statement
L.B. has received payment for teaching qigong since 2005, but was not an instructor in this trial. The other authors declare no conflicts of interest.
Funding Information
This work was supported by the National Center for Complementary and Integrative Health of the National Institutes of Health (grant number K23AT008211 to AS). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Supplementary Material
References
- 1. National MS Society. What is Multiple Sclerosis?: National MS Society. Available at: https://www.nationalmssociety.org/What-is-MS/Definition-of-MS Accessed March 7, 2021.
- 2. National MS Society. Symptoms: National MS Society. Available at: https://www.nationalmssociety.org/Symptoms-Diagnosis/MS-Symptoms Accessed March 7, 2021.
- 3. Ben-Zacharia AB. Therapeutics for multiple sclerosis symptoms. Mt Sinai J Med A J Transl Pers Med 2011;78:176–191. [DOI] [PubMed] [Google Scholar]
- 4. Nilsagård Y, Gunn H, Freeman J, et al. Falls in people with MS—an individual data meta-analysis from studies from Australia, Sweden, United Kingdom and the United States. Mult Scler J 2015;21:92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Peterson EW, Cho CC, von Koch L, Finlayson ML. Injurious falls among middle aged and older adults with multiple sclerosis. Arch Phys Med Rehabil 2008;89:1031–1037. [DOI] [PubMed] [Google Scholar]
- 6. Peterson EW, Cho CC, Finlayson ML. Fear of falling and associated activity curtailment among middle aged and older adults with multiple sclerosis. Mult Scler J 2007;13:1168–1175. [DOI] [PubMed] [Google Scholar]
- 7. Goodman AD, Brown TR, Krupp LB, et al. Sustained-release oral fampridine in multiple sclerosis: A randomised, double-blind, controlled trial. Lancet 2009;373:732–738. [DOI] [PubMed] [Google Scholar]
- 8. Behm K, Morgan P. The effect of symptom-controlling medication on gait outcomes in people with multiple sclerosis: A systematic review. Disabil Rehabil 2018;40:1733–1744. [DOI] [PubMed] [Google Scholar]
- 9. Amatya B, Khan F, Galea M. Rehabilitation for people with multiple sclerosis: An overview of Cochrane Reviews. Cochrane Database Syst Rev 2019;1:CD012732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Latimer-Cheung AE, Pilutti LA, Hicks AL, et al. Effects of exercise training on fitness, mobility, fatigue, and health-related quality of life among adults with multiple sclerosis: A systematic review to inform guideline development. Arch Phys Med Rehabil 2013;94:1800–1828.e3. [DOI] [PubMed] [Google Scholar]
- 11. Ensari I, Motl RW, Pilutti LA. Exercise training improves depressive symptoms in people with multiple sclerosis: Results of a meta-analysis. J Psychosom Res 2014;76:465–471. [DOI] [PubMed] [Google Scholar]
- 12. Asano M, Finlayson ML. Meta-analysis of three different types of fatigue management interventions for people with multiple sclerosis: Exercise, education, and medication. Mult Scler Int 2014;2014:798285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Carter AM, Daley AJ, Kesterton SW, et al. Pragmatic exercise intervention in people with mild to moderate multiple sclerosis: A randomised controlled feasibility study. Contemp Clin Trials 2013;35:40–47. [DOI] [PubMed] [Google Scholar]
- 14. Marck CH, Hadgkiss EJ, Weiland TJ, et al. Physical activity and associated levels of disability and quality of life in people with multiple sclerosis: A large international survey. BMC Neurol 2014;14:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mayo NE, Bayley M, Duquette P, et al. The role of exercise in modifying outcomes for people with multiple sclerosis: A randomized trial. BMC Neurol 2013;13:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Crescentini C, Matiz A, Cimenti M, et al. Effect of mindfulness meditation on personality and psychological well-being in patients with multiple sclerosis. Int J MS Care 2018;20:101–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Carletto S, Tesio V, Borghi M, et al. The effectiveness of a body-affective mindfulness intervention for multiple sclerosis patients with depressive symptoms: A randomized controlled clinical trial. Front Psychol 2017;8:2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Levin AB, Hadgkiss EJ, Weiland TJ, Jelinek GA. Meditation as an adjunct to the management of multiple sclerosis. Neurol Res Int 2014;2014:704691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yeung A, Chan JSM, Cheung JC, Zou L. Qigong and Tai-Chi for mood regulation. Focus (Madison) 2018;16:40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schmitz-Hübsch T, Pyfer D, Kielwein K, et al. Qigong exercise for the symptoms of Parkinson's disease: A randomized, controlled pilot study. Mov Disord 2006;21:543–548. [DOI] [PubMed] [Google Scholar]
- 21. Song R, Grabowska W, Park M, et al. The impact of Tai Chi and Qigong mind-body exercises on motor and non-motor function and quality of life in Parkinson's disease: A systematic review and meta-analysis. Parkinsonism Relat Disord 2017;41:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sawynok J, Lynch M, Marcon D. Extension trial of qigong for fibromyalgia: A quantitative and qualitative study. Evid Based Complement Alternat Med 2013;2013:726062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Chan JSM, Ho RTH, Wang C-W, et al. Effects of qigong exercise on fatigue, anxiety, and depressive symptoms of patients with chronic fatigue syndrome-like illness: A randomized controlled trial. Evid Based Complement Alternat Med 2013;2013:485341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mills N, Allen J, Carey-Morgan S. Does Tai Chi/Qi Gong help patients with multiple sclerosis? J Bodyw Mov Ther 2000;4:39–48. [Google Scholar]
- 25. Motl RW, Cohen JA, Benedict R, et al. Validity of the timed 25-foot walk as an ambulatory performance outcome measure for multiple sclerosis. Mult Scler J 2017;23:704–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Learmonth YC, Dlugonski DD, Pilutti LA, et al. The reliability, precision and clinically meaningful change of walking assessments in multiple sclerosis. Mult Scler 2013;19:1784–1791. [DOI] [PubMed] [Google Scholar]
- 27. Podsiadlo D, Richardson S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 1991;39:142–148. [DOI] [PubMed] [Google Scholar]
- 28. Dite W, Temple VA. A clinical test of stepping and change of direction to identify multiple falling older adults. Arch Phys Med Rehabil 2002;83:1566–1571. [DOI] [PubMed] [Google Scholar]
- 29. Hobart J, Lamping D, Fitzpatrick R, et al. The Multiple Sclerosis Impact Scale (MSIS-29): A new patient-based outcome measure. Brain 2001;124:962–973. [DOI] [PubMed] [Google Scholar]
- 30. Hobart JC, Riazi A, Lamping DL, et al. Measuring the impact of MS on walking ability: The 12-Item MS Walking Scale (MSWS-12). Neurology 2003;60:31–36. [DOI] [PubMed] [Google Scholar]
- 31. D'Souza E. Modified Fatigue Impact Scale -5-item version (MFIS-5). Occup Med (Lond) 2016;66:256–257. [DOI] [PubMed] [Google Scholar]
- 32. Intro to PROMIS. Available at: https://www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis Accessed April 9, 2020.
- 33. Eldridge SM, Chan CL, Campbell MJ, et al. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 2016;355. DOI: 10.1136/bmj.i5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. R Core Team. R: The R Project for Statistical Computing. R Foundation for Statistical Computing website. Available at: https://www.r-project.org/ Accessed March 7, 2021.
- 35. Taylor E, Taylor-Piliae RE. The effects of Tai Chi on physical and psychosocial function among persons with multiple sclerosis: A systematic review. Complement Ther Med 2017;31:100–108. [DOI] [PubMed] [Google Scholar]
- 36. Mills N, Allen J. Mindfulness of movement as a coping strategy in a Pilot Study. Gen Hosp Psychiatry 2000;22:425–431. [DOI] [PubMed] [Google Scholar]
- 37. Kolt GS, McEvoy JF. Adherence to rehabilitation in patients with low back pain. Man Ther 2003;8:110–116. [DOI] [PubMed] [Google Scholar]
- 38. Jordan JL, Holden MA, Mason EE, Foster NE. Interventions to improve adherence to exercise for chronic musculoskeletal pain in adults. Cochrane Database Syst Rev 2010. [Epub ahead of print]; DOI: 10.1002/14651858.CD005956.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Forechi L, Mill JG, Griep RH, et al. Adherence to physical activity in adults with chronic diseases: ELSA-Brasil. Rev Saude Publica 2018;52:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hawley-Hague H, Horne M, Skelton DA, Todd C. Older adults' uptake and adherence to exercise classes: Instructors' perspectives. J Aging Phys Act 2016;24:119–128. [DOI] [PubMed] [Google Scholar]
- 41. Gilbertson RM, Klatt MD. Mindfulness in motion for people with multiple sclerosis: A feasibility study. Int J MS Care 2017;19:225–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mills N. Qigong for Multiple Sclerosis. London: Singing Dragon, 2010. [Google Scholar]
- 43. Wayne PM, Berkowitz DL, Litrownik DE, et al. What do we really know about the safety of tai chi?: A systematic review of adverse event reports in randomized trials. Arch Phys Med Rehabil 2014;95:2470–2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wayne PM, Buring JE, Davis RB, et al. Tai Chi for osteopenic women: Design and rationale of a pragmatic randomized controlled trial. BMC Musculoskelet Disord 2010;11:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wayne PM, Kiel DP, Buring JE, et al. Impact of Tai Chi exercise on multiple fracture-related risk factors in post-menopausal osteopenic women: A pilot pragmatic, randomized trial. BMC Complement Altern Med 2012;12:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Fischer M, Fugate-Woods N, Wayne PM. Use of pragmatic community-based interventions to enhance recruitment and adherence in a randomized trial of Tai Chi for women with osteopenia. Menopause 2014;21:1181–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Litrownik D, Gilliam E, Berkowitz D, et al. Reporting of protocol rationale and content validity in randomized clinical trials of T'ai Chi: A systematic evaluation. J Altern Complement Med 2019;25:370–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.