Abstract
Background:
Cervical cancer is the fourth most common cancer among women worldwide. In Indonesia, cervical cancer is the second most frequent disease related to cancer. Based on staging system criteria, clinical findings are the main criteria to determine cervical cancer stage. In the revised version of the Federation of Gynecology and Obstetrics staging system criteria for cervical cancer, radiological examination for pretreatment evaluation in gynecological malignancies has been used in routine modalities. Magnetic resonance imaging (MRI) and ultrasonography (USG) are commonly used in the presurgery determination of tumor size and the follow-up of cervical cancer patients. Tumor size determines cancer stage which influences the treatment and the survival. The equality of diagnostic accuracy was compared for MRI and ultrasound in this study for tumor size evaluation of cervical cancer patients.
Methods:
This was a prospective study including 195 patients with cervical cancer Stage IIIB in Dr. Cipto Mangunkusumo Hospital from 2016 to 2018. The tumor sizes and stages of cervical cancer were assessed on MRI and ultrasound. This study evaluated diagnostic accuracy between MRI and US. The sensitivity and specificity were compared by using McNemar test.
Results:
The result of the study showed that from 195 patients, 76 patients fulfilled the study inclusion criteria. There is a significant difference in assessing tumor size in cervical cancer patients between ultrasound and MRI (mean, 1.72 cm; P < 0.0001). US had 82% sensitivity, 88% specificity, and 82% diagnostic accuracy (P = 0.003, McNemar test).
Conclusion:
Ultrasound examination showed a comparable accuracy to MRI for assessing tumor size in cervical cancer. US is an affordable and feasible diagnostic staging tool with accuracy comparable to MRI.
Keywords: Cervical cancer, imaging modality, magnetic resonance imaging, staging, ultrasonography
INTRODUCTION
Cervical cancer is the fourth most common cancer among women worldwide. In Indonesia, cervical cancer is the second most frequent disease related to cancer. Cervical cancer cases in Indonesia contribute 17.2% of all cancer in women and have caused 8.8% of all cancer-related deaths in Indonesia.[1] Based on the Indonesian Society of Gynecologic Oncology data, cervical cancer cases that are most commonly found in Indonesia are already at an advanced stage, where Stage IIIB holds the highest number compared to other stages.[2] In clinical practice, the severity of cervical cancer is based on staging system that is one of the important prognostic factors in cervical cancer survival rate.[3,4] The International Federation of Gynecology and Obstetrics (FIGO) clinical staging system is the criteria that have been used by gynecologic oncologists to determine the cervical cancer stage based on findings from pelvic examination by a gynecologic oncologist, colposcopy with biopsy, chest radiography, cystoscopy, intravenous excretory urography, barium enema, and sigmoidoscopy. However, in cervical cancer cases to have a more accurate determination of the disease staging, relying only on clinical examination of the characteristics is not enough. The revised 2018 FIGO staging system has included the use of imaging to have more accurate results.[4,5,6] Current studies show improvement in 5 year progression free survival rate in early stages about 80%–100% while at advanced stages have a survival rate with a range of 11%–72%.[7,8] Moreover, an ideal diagnostic test should be Affordable, Sensitive, Specific, User-friendly, Rapid, Equipment-free, and Deliverable to end-users.[9]
Radiological examination for pretreatment evaluation in gynecological malignancies has been used in routine modalities such as magnetic resonance imaging (MRI), positron emission tomography/computed tomography, or ultrasound that could assess tumor size, parametrial involvement, lymph node metastases, adjacent pelvic organ, and pelvic sidewall invasion.[6,10,11] In cervical cancer, the use of MRI makes the requirement for clinical examination under anesthesia, for instance, proctoscopy and cystoscopy are no longer mandatory.[12] On the contrary side, MRI examinations are high priced. It is essential to find inexpensive diagnostic tools comparable to MRI. Ultrasound examination is efficient, easy to prepare, cheaper, and more widely obtainable compared to MRI. Ultrasound is used by physician to visualize the vagina, cervix, rectum wall, parametrium, and bladder.[13,14,15] Transvaginal and transrectal ultrasound's role has been reported in many studies to have a more detailed assessment for cervical cancer staging than transabdominal ultrasound.[10,16,17] In this study, we compared the equality of diagnostic accuracy for transabdominal ultrasound examination to MRI.
METHODS
We conducted a prospective, interdisciplinary, and operator-blinded study at a university teaching hospital, Dr. Cipto Mangunkusumo National Central General Hospital. We conducted multiple researches, and consecutive patients diagnosed with Stage IIIB cervical cancer during the period of November 2016 to September 2018 were enrolled. All cervical cancer patients who were confirmed by biopsy were staged by clinical findings based on FIGO 2018. All patients receiving definitive radiotherapy were part of another study efficacy of biocurcumin as a radiosensitizer, thus they did not receive chemotherapy.
Ultrasound examination that was performed by a gynecologist was examined in an empty bladder in lithotomy position using a Voluson E8 system (GE Healthcare, Zipf, Austria) equipped with a RAB 4–8 MHz transabdominal probe, and two-dimensional scan settings were used. The sonographer was blinded to the results of the MRI. MRI examinations performed by using an Avanto 1.5T scanner (Siemens Medical Solutions, Munich, Germany) using fast spin-echo sequences with a phased-array surface pelvic coil were done by radiologists who had no access to the results of the MRI.
This study was reviewed and specifically approved by the Institutional Review Board and Ethical Committee Dr. Cipto Mangunkusumo, a national reference and teaching hospital (Research Clearance Certificate Number 499/UN2.F1/ETIK/2015). All patient informed consent was obtained. This study compared the size discrepancy and calculated diagnostic parameters between ultrasound and MRI, as the gold standard. STATA 14.2 software was used for all statistical analyses sensitivity, specificity, positive predictive value (PPV), and negative predictive value. The sensitivity and specificity of ultrasound and MRI were compared by McNemar test.
RESULTS
From 195 patients, 74 patients were excluded because they refuse to join the research, 8 patients died before the research start, and 37 patients have incomplete data. A total of 76 patients, who had biopsy confirmed with Stage IIIB invasive squamous cell carcinoma cervix, were included. The mean age (± standard deviation) of patients at diagnosis was 50.62 ± 8.7 years. Patients’ characteristics are summarized in Table 1. The tumor size was measured using ultrasound and then confirmed with MRI [Figures 1 and 2]. The tumor size measured on ultrasound examination (mean, 5.30 cm3 ± 1.8) was smaller than MRI (mean, 6.6 cm3 ± 1.9; mean difference, 1.3 cm3; P < 0.0001).
Table 1.
Clinical characteristics of cervical cancer patients who underwent disease staging with magnetic resonance imaging and ultrasound examination
| Characteristics | n (%) |
|---|---|
| Age | |
| Mean age±SD (years) | 50.62±8.7 |
| Minimum-maximum (years) | 28-69 |
| Histotype | |
| Squamous cell carcinoma | 76 (100) |
| Tumor volume | |
| Mean | |
| MRI | 6.6±1.9 |
| USG | 5.3±1.8 |
| Median (range) | |
| MRI | 6.7 (2.7-11.4) |
| USG | 5.0 (2.3-11.6) |
| Grade | |
| 1 | 14 (18.4) |
| 2 | 51 (67.1) |
| 3 | 11 (14.5) |
| BMI | |
| Mean±SD | 24.7±3.98 |
| Minimum-maximum | 16-36 |
| Paritas | |
| Median (range) | 3 (0-11) |
| LVSI | |
| Yes | 2 (2.6) |
| No | 74 (97.4) |
BMI: Body mass index, LVSI: Lymphovascular space invasion, SD: Standard deviation, MRI: Magnetic resonance imaging, USG: Ultrasonography
Figure 1.

Ultrasound result of the patient. Solid mass in the cervical area
Figure 2.
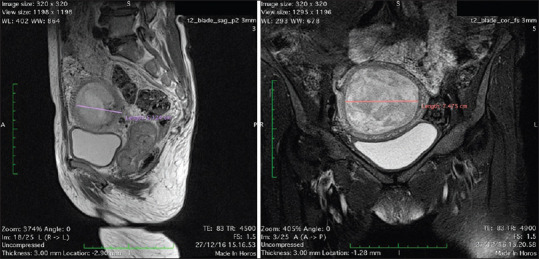
Cervical mass measurement, as shown by the magnetic resonance imaging of the lower abdomen and pelvis
There was a strong correlation between MRI and ultrasound examination (P < 0.0001). A total of 56 patients (73.6%) who were diagnosed with Stage IIIB cervical cancer had tumor size >4 cm based on ultrasound examination [Table 2]. In other words, ultrasound correctly measured tumor size >4 cm in 54 of 56 patients and 2 false-positive diagnoses. At the same time, a total of 20 patients, there were 8 true-positive diagnose and 12 false-positive diagnoses. McNemar's test showed that ultrasound examination had 82% sensitivity and 88% specificity (P = 0.003). We compared MRI and ultrasound examination; the result revealed that the diagnostic accuracy of ultrasound was 82%. The maximum discrepancy in tumor size between MRI and ultrasound examination was 4.9 cm (mean, 1.72 ± 1.07).
Table 2.
Performance between ultrasound examination and gold standard magnetic resonance imaging in measuring cervical cancer lesions
| Ultrasound measurement (cm) | MRI measurement (cm) | Total | Sensitivity (82%) Specificity (80%) |
|
|---|---|---|---|---|
|
| ||||
| >4 | ≤4 | |||
| >4 | 54 | 2 | 56 | PPV (96%) NPV (40%) |
| ≤4 | 12 | 8 | 20 | Conformity MRI versus USG Mean±SD (1.72±1.07) Minimum-maximum (0-4.9) |
| Total | 66 | 10 | 76 | |
P=0.003, McNemar test. PPV: Positive predictive value, NPV: Negative predictive value, SD: Standard deviation, MRI: Magnetic resonance imaging, USG: Ultrasonography
DISCUSSION
This study showed that the sensitivity and specificity of the ultrasound examination in diagnosing Stage IIIB cervical cancer by comparison to MRI were 82% and 88%, respectively [Table 2]. Furthermore, ultrasound can identify roughly 96% of the actual Stage IIIB cervical cancer PPV.
An accurate diagnostic test is essential to ensure a reliable diagnosis of carcinoma to choose the best treatment strategy and monitor significant improvements.[18,19] Precise tumor size is required for a more accurate stage. Tumor size was an independent prognostic factor regarding recurrent disease and overall survival.[18]
An ideal diagnostic test would be sensitive, noninvasive, inflict no side effect, widely accessible, and also affordable.[14] Complementing clinical assessment for more accurate staging, imaging is needed to provide information about other relevant prognostic factors.[10] MRI is a gold standard measurement and is superior to an ultrasound examination,[20] but the disadvantages are more expensive, the difficulty of availability, and ineligible for renal failure in using contrast medium and metal implants like pacemakers.[20,21]
Because most of the cervical cancer cases are diagnosed in low-resource settings where modern imaging is not accessible, the choice of imaging is also modified.[11] Compared with MRI, ultrasound examination offers several advantages such as noninvasive, rapid, widely available, inexpensive, and patients and user-friendly, but on the contrary side, it is user dependent.[20]
The principal findings of this study revealed that ultrasound examination is a feasible diagnostic tool in assessing tumor size in cervical cancer patients. There was a statistically significant difference in assessing tumor size between ultrasound and MRI. Even so, the tumor size measured on ultrasound examination was smaller than MRI.
Our study had some strengths. First, this study conducted a prospective design. Second, the radiologist who performed all measurements was blinded to ultrasound results. Third, all measurements in this study were in line with standardized protocols in our country, and would be easily implemented at each center. The constraint of this study had a relatively small sample size. The tumor size that bigger than the cervix could be caused by the invasion of the mass to the parametrium, so the size measured was the combination of cervical and parametrium, but the jurisdiction of the tumor size measurement was given solely to the radiologist. The diagnosis of advanced-stage cervical cancer was not supported by pathologic confirmation because the patients did not undergo surgery.
CONCLUSION
Ultrasound examination showed a comparable accuracy to MRI for assessing tumor size in cervical cancer. Ultrasonography is an affordable and feasible diagnostic staging tool with accuracy comparable to MRI.
Data availability
None.
Financial support and sponsorship
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.WHO. Indonesia fact sheets. Int Agency Res Cancer Globocan. 2019;256:2018–9. [Google Scholar]
- 2.INASGO. Indonesian Society of Gynecologic Oncology National Data. [Last accessed on 2020 Jun 22]. Available from: http://www.inasgo.org/fusionchart/APP/Staging_cervix_bar.asp .
- 3.Carneiro SR, Fagundes MA, do Rosário PJ, Neves LM, Souza GD, Pinheiro MD. Five-year survival and associated factors in women treated for cervical cancer at a reference hospital in the Brazilian Amazon. PLoS One. 2017;12:e0187579. doi: 10.1371/journal.pone.0187579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R. Cancer of the cervix uteri. Int J Gynecol Obstet. 2018;143:22–36. doi: 10.1002/ijgo.12611. [DOI] [PubMed] [Google Scholar]
- 5.Pecorelli S. Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet. 2009;105:103–4. doi: 10.1016/j.ijgo.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 6.Rizzo S, Calareso G, de Maria F, Zanagnolo V, Lazzari R, Cecconi A, et al. Gynecologic tumors: How to communicate imaging results to the surgeon. Cancer Imaging. 2013;13:611–25. doi: 10.1102/1470-7330.2013.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matsuo K, Machida H, Mandelbaum RS, Konishi I, Mikami M. Validation of the 2018 FIGO cervical cancer staging system. Gynecol Oncol. 2019;152:87–93. doi: 10.1016/j.ygyno.2018.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grigsby PW, Massad LS, Mutch DG, Powell MA, Thaker PH, McCourt C, et al. FIGO 2018 staging criteria for cervical cancer: Impact on stage migration and survival. Gynecol Oncol. 2020;157:639–43. doi: 10.1016/j.ygyno.2020.03.027. [DOI] [PubMed] [Google Scholar]
- 9.Kosack CS, Page AL, Klatser PR. A guide to aid the selection of diagnostic tests. Bull World Health Organ. 2017;95:639–45. doi: 10.2471/BLT.16.187468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miccò M, Sala E, Lakhman Y, Hricak H, Vargas HA. Role of imaging in the pretreatment evaluation of common gynecological cancers. Womens Health (Lond) 2014;10:299–321. doi: 10.2217/whe.14.19. [DOI] [PubMed] [Google Scholar]
- 11.Lee SI, Atri M. 2018 FIGO staging system for uterine cervical cancer: Enter cross-sectional imaging. Radiology. 2019;292:15–24. doi: 10.1148/radiol.2019190088. [DOI] [PubMed] [Google Scholar]
- 12.Freeman SJ, Aly AM, Kataoka MY, Addley HC, Reinhold C, Sala E. The revised FIGO staging system for uterine malignancies: Implications for MR imaging. Radiographics. 2012;32:1805–27. doi: 10.1148/rg.326125519. [DOI] [PubMed] [Google Scholar]
- 13.Testa AC, Ludovisi M, Manfredi R, Zannoni G, Gui B, Basso D, et al. Transvaginal ultrasonography and magnetic resonance imaging for assessment of presence, size and extent of invasive cervical cancer. Ultrasound Obstet Gynecol. 2009;34:335–44. doi: 10.1002/uog.7325. [DOI] [PubMed] [Google Scholar]
- 14.Epstein E, Testa A, Gaurilcikas A, Di Legge A, Ameye L, Atstupenaite V, et al. Early-stage cervical cancer: Tumor delineation by magnetic resonance imaging and ultrasound – A European multicenter trial. Gynecol Oncol. 2013;128:449–53. doi: 10.1016/j.ygyno.2012.09.025. [DOI] [PubMed] [Google Scholar]
- 15.Sozzi G, Berretta R, Fiengo S, Ferreri M, Giallombardo V, Finazzo F, et al. Integrated pre-surgical diagnostic algorithm to define extent of disease in cervical cancer. Int J Gynecol Cancer. 2020;30:16–20. doi: 10.1136/ijgc-2019-000665. [DOI] [PubMed] [Google Scholar]
- 16.Fischerova D. Ultrasound scanning of the pelvis and abdomen for staging of gynecological tumors: A review. Ultrasound Obstet Gynecol. 2011;38:246–66. doi: 10.1002/uog.10054. [DOI] [PubMed] [Google Scholar]
- 17.Ordeanu C, Pop DC, Badea R, Csutak C, Todor N, Ordeanu C, et al. Local experience in cervical cancer imaging: Comparison in tumour assessment between TRUS and MRI. Reports Pract Oncol Radiother. 2015;20:223–30. doi: 10.1016/j.rpor.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kyung MS, Kim HB, Seoung JY, Choi IY, Joo YS, Lee MY, et al. Tumor size and lymph node status determined by imaging are reliable factors for predicting advanced cervical cancer prognosis. Oncol Lett. 2015;9:2218–24. doi: 10.3892/ol.2015.3015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Horn LC, Bilek K, Fischer U, Einenkel J, Hentschel B. A cut-off value of 2 cm in tumor size is of prognostic value in surgically treated FIGO stage IB cervical cancer. Gynecol Oncol. 2014;134:42–6. doi: 10.1016/j.ygyno.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 20.Moloney F, Ryan D, Twomey M, Hewitt M, Barry J. Comparison of MRI and high-resolution transvaginal sonography for the local staging of cervical cancer. J Clin Ultrasound. 2016;44:78–84. doi: 10.1002/jcu.22288. [DOI] [PubMed] [Google Scholar]
- 21.Taydas O, Durhan G, Akpinar MG, Basaran Demirkazik F. Comparison of MRI and US in tumor size evaluation of breast cancer patients receiving neoadjuvant chemotherapy. Eur J Breast Heal. 2019;15:119–24. doi: 10.5152/ejbh.2019.4547. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
None.


