Abstract
We report a rare case of midgut malrotation and volvulus with “whirlpool sign” in a new-born infant. The “whirlpool sign” is an imaging characteristic of midgut volvulus and has a high predicting value for volvulus. Malrotation or malrotation with volvulus can be effectively diagnosed based on these characteristics. Ultrasound diagnosis has the advantage of no radiation exposure. Color Doppler documenting the reversal or aberrant superior mesenteric vein/superior mesenteric artery axis is not only predictive but also diagnostic of malrotation of gut. The rapid and accurate diagnosis of volvulus by ultrasound helps to establish the diagnosis of malrotation in time and thus allows for urgent surgical intervention to avoid bowel necrosis.
Keywords: Color Doppler, computed tomography, corkscrew sign, intestinal malrotation, midgut volvulus, superior mesenteric artery, superior mesenteric vein, ultrasound, upper gastrointestinal, whirlpool sign
INTRODUCTION
Midgut malrotation and volvulus are rare in infants and difficult to diagnose preoperatively. Ultrasound diagnosis has the advantage of no radiation exposure. Color Doppler documenting the reversal or aberrant the superior mesenteric vein/superior mesenteric artery (SMV/SMA) axis is not only predictive but also diagnostic of malrotation of gut. Abdominal sonography demonstrated wrapping of the SMV and bowel loops around the SMA (“whirlpool sign”). An upper gastrointestinal (UGI) series showed a corkscrew appearance of the duodenum, consistent with malrotation, and midgut volvulus. The diagnosis of midgut volvulus and mesenteric malrotation was made. The patient underwent successful midgut reduction surgery smoothly.
CASE REPORT
A 5-day-old female new-born was transferred from the Sijhih Branch to the Cathay General Hospital due to abdominal distension and biliary vomiting. After admission, she first corrected the dehydration caused by vomiting and the problem of electrolyte imbalance. An abdominal X-ray revealed a mild stomach distension and bowel dilatation over the left lower quadrant area. Laboratory tests revealed nonspecific findings. Ultrasound showing the relationship between the SMV and the SMA is reversed. The SMV is located at the left front of the SMA [Figure 1a]. An image examination of the UGI showed a corkscrew sign in the duodenum, indicating a spiral curve formed by midgut volvulus, similar to “apple-peel/twisted ribbon” [Figure 1b].
Figure 1.
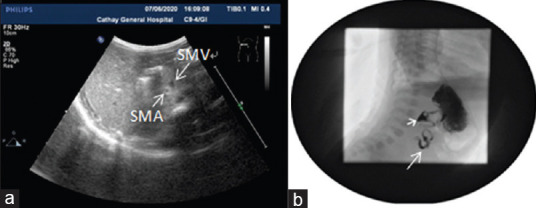
(a) Ultrasound image showing the reverse positional relationship between the superior mesenteric vein and superior mesenteric artery. The superior mesenteric vein is located at the left front of the superior mesenteric artery. (b) Upper gastrointestinal imaging examination showing the corkscrew sign in the duodenum, indicating a spiral curve similar to “apple-peel/twisted ribbon” formed due to midgut volvulus
The ultrasound image of the mid-section of the upper abdomen showed concentric circular masses [Figure 2a and b]. Color Doppler ultrasound demonstrated a typical whirlpool signs [Figure 3a and b]. The diagnosis of malrotation and midgut volvulus is established.
Figure 2.
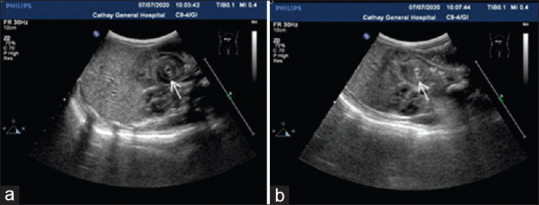
(a and b) Ultrasound image of the mid-section of the upper abdomen showing concentric circular masses
Figure 3.
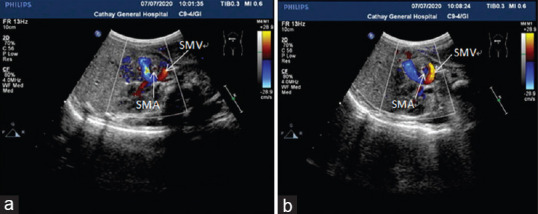
(a and b) Whirlpool signs visualized on color Doppler ultrasound: the small intestine and mesenteric are wrapped around the superior mesenteric artery to form a clockwise whirlpool
After detailed communication with family members, the baby underwent a midgut reduction operation, resetting the original small intestine to relieve the obstruction and restore the intestinal patency. No persistent vomiting occurred after the operation. The new-born was fed on the 3rd day after the surgery and was discharged 6 days later.
DISCUSSION
Congenital intestinal malrotation is due to the obstruction of intestinal rotation during embryonic development, that is, malrotation of the SMA as the axis, which causes the position of the intestine to change and the incomplete mesenteric attachment, complicated by intestinal obstruction or intestine volvulus.
The early embryonic intestine is a straight tube with a common mesentery. During the 4th to 6th week of pregnancy, the midgut develops faster and cannot be accommodated in the slower growing abdominal cavity. Most of the midgut protrudes into the yolk sac through the umbilical ring. A physiological umbilical hernia is formed. At the 6th to 10th week of the embryo, the abdominal cavity develops faster, the volume increases, and the midgut returns to the abdominal cavity with the SMA as the axis, rotating 270° counterclockwise. The duodenum-jejunal curve turns from right to left, from the back of the SMA to the left, forming the suspensory ligament of the duodenum. The ileocolonic junction turns from left to right in front of the SMA to the right upper abdomen, and then gradually descends to the right iliac. After the normal rotation is completed, the transverse colon is located in front of the SMA, the ascending colon and descending colon are attached to the posterior abdominal wall by the mesentery of the colon, and the small bowel mesentery is obliquely from the upper left abdomen to the lower right abdomen and is attached to the posterior wall of the abdomen, namely duodenum-jejunum junction. The junction is anchored to the SMA at the Treitz ligament, and the cecum is attached to the lower right abdominal wall. These two anchor points lay a solid foundation for the small bowel mesentery.[1]
Clinical symptoms pay attention to the presence or absence of bile from vomit
Most neonatal patients with intestinal malrotation will normally passage meconium within 24 h after birth. The condition of breastfeeding is good at the beginning, and then, a large amount of biliary vomiting suddenly appears on the 3rd to 5th day. Due to the different degree of duodenal compression, it can manifest as partial or complete obstruction. In partial obstruction, the patient will vomit intermittently. The vomit contains bile, and the abdomen is not distended. When the obstruction is complete, biliary vomiting will continue and frequent, accompanied by dehydration, weight loss, and constipation. If it is complicated by midgut volvulus, the symptoms will be more serious and finally may cause small bowel necrosis, perforation, peritonitis, shock, and other symptoms.
Due to different pathological variations, patients with neonatal intestinal malrotation have clinical manifestations of various degrees of intestinal obstruction. Some patients have intermittent bile-containing vomiting, eating intolerance, and often relieve themselves. This has been repeated. There are also a small number of patients who are asymptomatic after birth, and suddenly experience intestinal volvulus and severe abdominal pain, frequent vomiting, and constipation. In other words, the appearance of intestinal volvulus is like twisting a towel with your hands. If the torsion is not serious, the patient may feel pain, vomiting, and be fine after a short rest. This situation is less likely to cause small intestinal necrosis. It is very tight, blood circulation stops causing intestinal necrosis, which may cause peritonitis, or even sepsis, which is life-threatening. This is a surgical emergency and requires immediate surgical exploration.
Ultrasonic diagnosis of intestinal malrotation is the main cross section of the upper abdomen. The positional relationship of the SMA is used to determine whether there is malrotation. Normally, the relationship between the SMA and the vein is approximately parallel. Once the relationship between the SMV and the SMA is reversed, that is, SMV is located on the front left of the SMA, rather than the ventral and right sides, that is, malrotation of the intestine.[2] The ultrasound image of the mid-section of the upper abdomen shows concentric circular masses. If the malrotation causes small bowel volvulus, it is called the “whirlpool sign”, color Doppler ultrasound can see the whirlpool sign: Which is a clockwise whirlpool formed by the small intestine and mesenteric surrounding the SMA.[3]
The symptoms in infants and children are sometimes atypical, so X-ray examinations are often required, including UGI series study. Older babies and children can swallow a small amount of diluted barium for the examination when incomplete duodenal obstruction occurs. Imaging examination, typical malrotation of the intestine can reveal that the duodenum does not cross the midline, and the small intestine is only present on the right side of the abdomen. The so-called corkscrew sign means that the distal end of the duodenum and the proximal end of the jejunum do not cross the midline, but pass from below.[4] These loops are easily twisted on the shorter mesentery, thus forming a classic midgut volvulus. Appearance of the corkscrew is not easy to diagnose in patients with atypical and partial bowel rotation. Abdominal computed tomography (CT) and angiography can show all these anatomical abnormalities, but the costs and radiation exposure associated with CT limit its use as an early imaging test to diagnose intestinal malrotation.[5]
Asymptomatic patients should not be operated on and remain to be observed. If the patient has obvious symptoms of intestinal obstruction, it means midgut volvulus, and midgut reduction surgery should be actively performed as soon as possible to relieve the obstruction and restore the intestinal patency. If there is intestinal necrosis, intestinal resection and anastomosis were performed.[6]
Surgery for simple intestinal malrotation is very effective. If the patient has intestinal volvulus without intestinal necrosis, symptoms such as chronic abdominal pain, digestive and absorption dysfunction, anemia, and malnutrition may remain after the operation. As for patients with intestinal volvulus necrosis and extensive resection of the small intestine, short bowel syndrome will appear after the operation, which requires long-term parenteral nutrition to maintain life.[7] Some cases can be gradually improved by transitioning to oral elemental diet, but some cases require short bowel correction surgery, which requires a more expensive price premature babies, other severe malformations, and extensive bowel necrosis are the main causes of death of this disease. The key to reduce the mortality rate lies in the early diagnosis and correct operation.
CONCLUSION
Ultrasonography has been introduced as an alternative method for the diagnosis of malrotation, with an emphasis on the relationship of the SMV and SMA and the so-called “whirlpool sign” in cases of volvulus. The sonographic whirlpool sign is a valid and highly sensitive sign for the diagnosis of midgut volvulus secondary to malrotation. The whirlpool sign is valuable for the preoperative diagnosis of mesenteric vessel malrotation and midgut volvulus.
Declaration of patient consent
The authors certify that they have obtained appropriate the legal guardian consent form. In the form, the legal guardian have given the consent for the patient's images and other clinical information to be reported in the journal. The legal guardian understands that the name and initial will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Larsen W. Edinburgh: Churchill Livingstone; 1998. Essentials of Human Embryology; pp. 160–71. [Google Scholar]
- 2.Zhang W, Sun H, Luo F. The efficiency of sonography in diagnosing volvulus in neonates with suspected intestinal malrotation. Medicine (Baltimore) 2017;96:e8287. doi: 10.1097/MD.0000000000008287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Garel J, Daneman A, Rialon K, Zani A, Fecteau A, Piero A. The role of sonography for depiction of a whirlpool sign unrelated to midgut malrotation in neonates. Pediatr Radiol. 2020;50:46–56. doi: 10.1007/s00247-019-04508-z. [DOI] [PubMed] [Google Scholar]
- 4.Ortiz-Neira CL. The corkscrew sign: Midgut volvulus Radiology. 2007;242:315–6. doi: 10.1148/radiol.2421040730. [DOI] [PubMed] [Google Scholar]
- 5.Garcia AM, Asad I, Tessaro MO, Sivitz A, Osborn K, Shaahinfar A, et al. A multi-institutional case series with review of point-of-care ultrasound to diagnose malrotation and midgut volvulus in the pediatric emergency department. Pediatr Emerg Care. 2019;35:443–7. doi: 10.1097/PEC.0000000000001737. [DOI] [PubMed] [Google Scholar]
- 6.Millar AJ, Rode H, Cywes S. Malrotation and volvulus in infancy and childhood. Semin Pediatr Surg. 2003;12:229–36. doi: 10.1053/j.sempedsurg.2003.08.003. [DOI] [PubMed] [Google Scholar]
- 7.Nehra D, Goldstein AM. Intestinal malrotation: Varied clinical presentation from infancy through adulthood. Surgery. 2011;149:386–93. doi: 10.1016/j.surg.2010.07.004. [DOI] [PubMed] [Google Scholar]


