Abstract
Background
Pharmacists and pharmacy assistants can support consumers by identifying minor ailments and providing evidence-based advice about treatment options. In the Netherlands, advice is based on national minor ailment guidelines and structured WWHAM questions (Who, What, How long, Action, Medication).
Objectives
To study whether pharmacy assistants provide guideline-compliant advice for allergic rhinitis based on WWHAM and condition-specific questions (When and Familiarity) and their association with appropriate self-care advice.
Methods
A retrospective study of the assessments of simulated patient (SP) visits regarding one condition- and two symptom-based cases of allergic rhinitis in Dutch community pharmacies. Pharmacies that participated in 2014, 2016 and 2018 were selected. SPs documented their observations of the problem analysis, dispensing and client interaction on a standardized scoresheet. Dispensing of an oral antihistamine according to the guideline recommendation was considered as the correct outcome. Chi-square tests were used to analyze differences in scores for problem analysis of pharmacies with correct and incorrect advice provision in 2014 and 2018. Predictors for correct outcome were identified by univariate and multivariate logistic regression analysis.
Results
Data from 673 pharmacies were available for all three years. In 2014 and 2018, problems were presented as a symptom (running nose), and 41.2% and 21.1% of pharmacies dispensed an antihistamine. For the condition-based problem (allergy) in 2016, 96.0% of participating pharmacies dispensed an antihistamine. Both in 2014 and 2018, each additional problem analysis question increased the odds ratio of providing correct advice. Questions asked about ‘hay fever symptoms’, ‘medication’, ‘when symptoms occurred’, and ‘familiar symptoms’ were significant predictors of correct advice provision.
Conclusions
Most pharmacies provided appropriate advice for a condition-based request but less than half of them provided appropriate advice for a symptom-based request. More questions asked was associated with an increased chance of providing correct advice. Addition of condition-specific questions may improve the WWHAM-method.
Keywords: Allergic rhinitis, Mystery shopping, Patient simulation, Pharmacy assistant, Self-care, Simulated patient
Highlights
-
•
An increasing number of questions asked increased the chance of providing correct advice
-
•
The question ‘when symptoms occur’ at least doubled the odds ratio of correct advice
-
•
Solving problems presented as conditions was shown to be easier than those presented as symptoms
1. Introduction
The World Health Organisation (WHO) defines self-care as the ability of individuals, families and communities to promote health, prevent disease, maintain health and cope with illness and disability with or without support from a healthcare provider.1 Pharmacists can support self-care for consumers with minor ailments such as allergic rhinitis by identifying conditions and providing evidence-based treatment options.2,3
The prevalence of confirmed allergic rhinitis in adults in Europe ranges from 17% to 28.5%.4 Symptoms include nasal congestion, running nose, sneezing and itching of the nose, palate and/or eyes.4,5 In the Netherlands, the allergic rhinitis self-care guideline as a first choice recommends an oral non-sedative oral antihistamine (e.g., cetirizine or loratadine).6 Nose sprays and eye drops with sodium cromoglycate are available without prescription but not recommended by the guideline. Ocular and nasal azelastine have only recently (2021) been reintroduced as non-prescription medicines after having been available only on prescription for a decade. Contrary to some other countries, in the Netherlands nasal corticosteroids for hay fever treatment are available only on prescription.
In the Netherlands, pharmacy assistants who have completed a three-year vocational program assist the pharmacist by advising consumers on the use of nonprescription medicines to treat minor ailments. Advising on non-prescription medicines and self-care conditions is part of the competence profile of pharmacy assistants, and pharmacy assistants are required to adhere to guidelines and provide their patients with up-to-date evidence-based treatment advice to ensure optimal health outcomes.7 To analyze a patient's problem, pharmacy assistants and pharmacists are trained to ask WWHAM-questions (i.e., ‘Who is it for’, ‘What are the symptoms’,’How long have the symptoms been present’,’Has any Action already been taken’,’Has any other Medication been taken’), according to national self-care guidelines.6 The Allergic rhinitis guideline also recommends to ask the questions ‘when symptoms occur’ and ‘whether symptoms are familiar’: specific allergic rhinitis questions additional to the WWHAM-mnemonic.
Studies in the UK and Australia have shown that a higher number of problem analysis questions resulted in improved outcomes for minor ailment treatment and supply of nonprescription medication.8, 9, 10 A UK study also showed that individual WWHAM questions (e.g. description of symptoms and other medication) were predictors in addition to the total number of questions asked.9 However, other studies in the UK have found that the use of questioning strategies such as WWHAM during problem analysis had limited impact on patient outcomes and that pharmacists were overly reliant on this type of questioning strategy.11,12 These findings suggest that the WWHAM protocol may be important but not always sufficient. Additional questions that may be relevant to a specific minor ailment should be asked; otherwise, crucial information for decision-making can be missed.13 Furthermore, the pharmacy assistant should also accurately collect necessaary information, followed by appropriate problem identification and final advice.14
Dutch pharmacies have the opportunity to assess adherence to national self-care guidelines through simulated patient (SP) visits on a regular basis.15 SPs are specifically trained actors who pretend to be regular consumers visiting the pharmacy for minor ailment advice. Pharmacies can use the results of the regular assessments to improve the quality of consultations on minor ailments.
The aim of this study was to investigate whether pharmacy assistants provide guidance-compliant advice for allergic rhinitis by studying (1)associations between quality of problem analysis (use of WWHAM and condition-specific questions) and guideline recommended advice for symptom-based requests in 2014 and 2018, (2)dispensing of nonprescription medication for a condition-based request in 2016 and (3)general communication skills (conversation skills and consumer interaction).
2. Methods
2.1. Setting
In the Netherlands, from 2014 to 2018 there were 1979 to 1996 community pharmacies.16,17 In 1995, AMP Research and Advice in Healthcare started using SP visits to assess self-care advice in Dutch community pharmacies.15 Pharmacies voluntarily self-subscribe to the assessment program and pay a fee per year. Participating pharmacies are visited 4 times annually by a SP for a condition- or symptom-based self-care request. Subsequently, they receive an extensive report of the assessment results, including a benchmark comparison with the national average, the highest-scoring pharmacy, and comparison with previous results of their pharmacy during the current year.
2.2. Design
This retrospective cross-sectional study examined SP visits for allergic rhinitis at community pharmacies in the Netherlands in 2014, 2016 and 2018. After drafting the research question, the AMP research team developed the scenario through review of guidelines5,18., 19, 20. and literature. A scenario script was developed including starting question, description of the condition, answers to anticipated questions and correct outcome. After discussion of the scenario script with a limited number of SPs, the scenario was tested in 10 pharmacies who did not subscribe to the program, and where needed the scenario script was adjusted. Table 1 shows case descriptions for all study years. Before the assessments in all subscribing pharmacies started, the final version of the scenario script was discussed with all SPs to ensure similar interpretation. In the pharmacy, the SPs asked their starting question when a pharmacy team member (pharmacy assistant or pharmacist) addressed them at the counter.
Table 1.
Case descriptions.
| 2014 | 2016 | 2018 | |
|---|---|---|---|
| Type of case and starting question | Symptom-based: Something for a running nose |
Condition-based: Something for allergy |
Symptom-based: Something for a running nose |
| For Whom (W) | Simulated patient | Simulated patients' husband | Simulated patients' daughter aged 15 years |
| Additional symptoms (W) |
Sneezing Itching of the nose Itching and tearing of the eyes Itching palate Sometimes nasal congestion |
Allergy to cats Mainly sneezing and a running nose, sometimes itching and tearing of the eyes |
Sneezing Itching of the nose Sometimes itching palate, earache, nasal congestion |
| How long (H) | A few weeks | Since babysitting at her daughter's house the day before | Approximately 4 weeks |
| Action taken already (A) | No | No | No |
| Other medication (M) | No | Tamsulosin | No |
| When | More symptoms in the afternoon and in dry weather | In a house with a cat or other pets | Mainly when she's walking the dog and cycling to school, worse in dry weather. She got the dog, a Labradoodle, 6 months earlier. No complaints when playing with the dog |
| Familiar with symptoms | Yes, since relocation to her current house 2 years ago Does not feel like common cold |
Yes, he had something from a pharmacy earlier | No, no previous symptoms Does not feel like common cold |
| Correct advice (guideline) |
Oral cetirizine or loratadine | Oral cetirizine or loratadine | Oral cetirizine or loratadine |
| Incorrect advice | Other antihistamine Ocular sodium cromoglycate Nasal xylometazoline or xylometazoline/ipratropium Other products (nasal saline, herbal product) No product dispensed |
Other antihistamine Ocular sodium cromoglycate Nasal xylometazoline or xylometazoline/ipratropium Other products (nasal saline, herbal product) No product dispensed |
Other antihistamine Ocular sodium cromoglycate Nasal xylometazoline or xylometazoline/ipratropium Other products (nasal saline, herbal product) No product dispensed |
2.3. Data collection
The assessments were performed from 17 April–28 May 2014, 8 March–13 April 2016, and 8 March–11 April 2018, respectively. Only pharmacies that participated in all three assessments were selected to obtain results from comparable populations. The SPs recorded problem analysis questions, consultation characteristics, and general communication characteristics on a standardized data collection form in binary answers (yes or no).,immediately after each visit. Recommended products were bought and noted in the data collection form. The data collection form was based on the Dutch self-care allergic rhinitis guideline and other relevant guidelines.5,20 All pharmacy visits were audio recorded. By default, AMP used these recordings to check the validity of the data collection form.
2.4. Data analysis
The number of participating pharmacies was 823 in 2014, 948 in 2016 and 934 in 2018. The number of pharmacies participating in all 3 years was 673. The results of all of these pharmacies were analyzed. A score of 1 point was allocated to each problem analysis question asked by the pharmacy assistant.9 In 2014 and 2018, a chi-square test was used to analyze individual problem analysis questions for differences between pharmacies that did and did not provide correct advice (p < 0.05). The maximum total score for problem analysis, which consisted of WWHAM and 2 condition specific questions that are mentioned in the guideline, was 7. A chi-square test was used to analyze the total score for problem analysis and the median consultation time for differences between pharmacies that did and did not provide correct advice in 2014 and 2018, as well as between 2014 and 2018 (p < 0.05). Pharmacies with correctly and incorrectly advised medications were counted, and percentages of all pharmacies were calculated. A univariate logistic regression was performed to assess the association between total problem analysis score and correct advice provision in 2014 and 2018 (p < 0.05). A multivariate analysis with all individual questions was performed for 2014 and 2018 to further analyze the contribution of individual problem analysis questions (p < 0.05). For this analysis, specific questions about hay fever and common cold symptoms were used instead of the general question, ‘Do you have any other symptoms?’. For 2014 and 2018, chi-square test was used to analyze differences in the general communication characteristics for pharmacies that did and did not provide correct advice (p < 0.05).
All statistical analyses were performed using Statistical Package for the Social Sciences, IBM SPSS statistics for Windows, version 26.0.
2.5. Ethics
All data were anonymous and could not be traced back to the participating pharmacies. Use of routinely collected and anonymous observational data is not subject to the Medical Research Involving Human Subjects Act (WMO) in the Netherlands. Therefore, the study protocol did not need to be submitted for review by a medical ethics committee. All pharmacists participating in the assessment program have provided written consent to AMP to use the assessment data for research.
3. Results
3.1. Basic characteristics
A total of 673 pharmacies participated in all three years of data collection. Table 2 shows the basic characteristics of the consultations in these pharmacies. In the 2014 and 2018 symptom-based scenarios, the median consultation time in pharmacies that provided correct advice was significantly higher than in pharmacies that provided incorrect advice (p < 0.05); in the 2016 condition-based scenario, the difference in consultation time between correct and incorrect advice provision was not significant. In 2018, the consultation time was significantly higher than in 2014 for all pharmacies, including those that provided correct advice and those that provided incorrect advice (p < 0.05).
Table 2.
Consultation characteristics of community pharmacies (n = 673).
| 2014 | 2016 | 2018 | |
|---|---|---|---|
| Median waiting time before consultation, minutes (min–max) | 1.0 (0–29) | 2.0 (0–25) | 2.0 (0–26) |
| Median consultation time, minutes (min–max) | 3.0 (1–19) | 3.0 (1−20) | 4.0 (1–34) |
| in pharmacies that provided correct advice | 4.0 (1–19) | 3.0 (1–20) | 7.0 (1–34) |
| in pharmacies that provided incorrect advice | 2.0 (1−13) | 4.0 (1−10) | 3.0 (1–15) |
| Separate self-care counter: n (%) | 57 (8.5%) | 43 (6.4%) | 51 (7.6%) |
| Self-care advisor's job title visible on name plate: n (%) |
80 (11.9%) | 89 (13.2%) | 109 (16.2%) |
| Consultation with a colleague: n (%) | 85 (12.6%) | 71 (10.5%) | 137 (20.4%) |
| -consultation with a pharmacist: n (%) | 3 (0.5%) | 13 (1.9%) | 18 (2.7%) |
| Sufficient attention to privacy: n (%) | 433 (64.3%) | 470 (69.8%) | 406 (60.3%) |
| Queuing system in waiting area: n (%) | 113 (16.8%) | 138 (20.5%) | 140 (20.8%) |
3.2. Symptom-based scenarios (2014 and 2018)
Of all pharmacies, 10.8% (n = 73) provided correct advice in both 2014 and 2018, and 48.4% (n = 326) provided incorrect advice in both years. Only 10.4% (n = 70) of all pharmacies that had provided incorrect advice in 2014, then provided correct advice in 2018. In 2014 and 2018, pharmacies that provided correct advice had significantly higher scores for all individual WWHAM problem analysis questions, as well as the condition specific questions regarding ‘when symptoms occurred’ and ‘familiarity with symptoms’, than pharmacies that provided incorrect advice (p < 0.05; see Table 3).
Table 3.
Numbers (and percentages) of pharmacies that provided correct and incorrect advice and had a positive score on individual problem analysis questions.
| Year | 2014 |
2016 |
2018 |
|||
|---|---|---|---|---|---|---|
| Correct advice | Incorrect advice | Correct advice | Incorrect advice | Correct advice | Incorrect advice | |
| Number of pharmacies | 277 | 396 | 646 | 27 | 143 | 530 |
| WWHAM questions | ||||||
| Who (W) | 149 (53.8%)⁎ | 160 (40.4%)⁎ | 454 (70.3%) | 17 (63.0%) | 139 (97.2%)⁎⁎ | 430 (81.1%)⁎⁎ |
| Symptoms, in general (W) | 277 (100.0%)⁎ | 239 (60.4%)⁎ | 577 (89.3%) | 26 (96.3%) | 143 100.0%)⁎⁎ | 389 (73.4%)⁎⁎ |
| Hay feverª | 248 (89.5%)⁎ | 116 (29.3%)⁎ | NA | NA | 124 (86.7%)⁎⁎ | 198 (37.6%)⁎⁎ |
| Common coldᵇ | 114 (41.2%) | 126 (31.8%) | NA | NA | 76 (53.1%)⁎⁎ | 207 (39.1%)⁎⁎ |
| Both | 109 (39.4%)⁎ | 63 (15.9%)⁎ | NA | NA | 72 (50.3%)⁎⁎ | 110 (20.8%)⁎⁎ |
| How long symptoms present (H) | 177 (63.9%) ⁎ | 121 (30.6%)⁎ | 153 (23.7%) | 9 (33.3%) | 111 (77.6%)⁎⁎ | 230 (43.4%)⁎⁎ |
| Action taken (A) | 155 (56.0%) ⁎ | 134 (33.8%)⁎ | 464 (71.8%) | 14 (51.9%) | 106 (74.1%)⁎⁎ | 257 (48.5%)⁎⁎ |
| Other medication (M) | 213 (76.9%) ⁎ | 151 (38.1%)⁎ | 460 (71.2%) | 23 (85.2%) | 121 (84.6%)⁎⁎ | 222 (41.9%)⁎⁎ |
| Additional questions | ||||||
| When symptoms occur | 109 (39.4%) ⁎ | 47 (11.9%)⁎ | 167 (25.9%) | 14 (14.8%) | 92 (64.3%)⁎⁎ | 92 (17.4%)⁎⁎ |
| Familiar symptoms | 160 (61.0%) ⁎ | 83 (21.0%)⁎ | 209 (32.4%) | 1 (3.7%) | 103 (72.0%)⁎⁎ | 137 (25.8%)⁎⁎ |
ª itching nose, sneezing, running nose, itching and tearing eyes, itching palate.
ᵇ stuffy nose, mucus appearance, sore throat, earache, elevated body temperature, fever or general malaise.
statistical significance of difference between groups with and without correct advice in 2014, tested by chi-square (p < 0.05).
statistical significance of difference between groups with and without correct advice in 2018, tested by chi-square (p < 0.05).
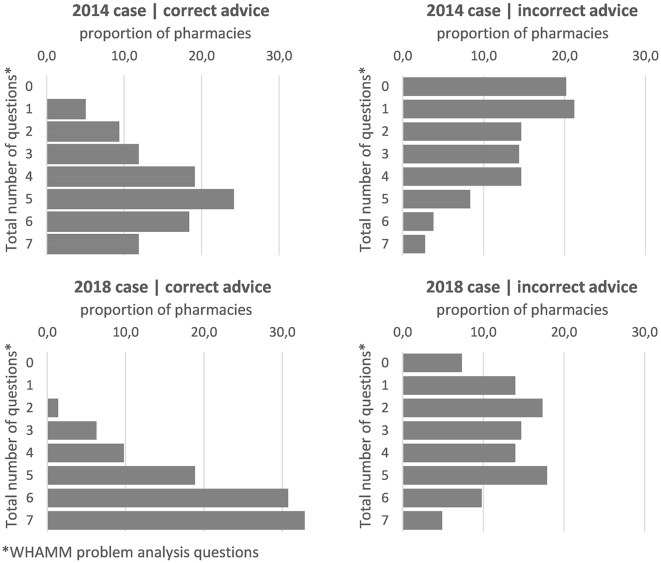
Fig. 1 shows the total number of problem analysis questions asked at pharmacies in 2014 and 2018, including pharmacies that provided correct and incorrect advice. In both years, the total number of questions asked in pharmacies that provided correct advice was significantly higher than that of pharmacies that provided incorrect advice (p < 0.05). In 2018, the total number of questions asked in pharmacies that provided correct advice was significantly higher than in 2014 (p < 0.05). The total number of questions asked in pharmacies that provided incorrect advice in 2018 was also significantly higher than in 2014 (p < 0.05). Both in 2014 and 2018, each additional problem analysis question significantly increased the odds ratio for providing correct advice, in 2014 with 1.8 (95% CI 1.7–2.0) and in 2018 with 2.3 (95% CI 1.9–2.6, see Table 4). Table 4 also shows the individual problem analysis questions that significantly increased the odds ratio of correct advice provision in 2014 and 2018. Asking about ‘when symptoms occur’ increased the odds ratio with 1.9 and 4.0 in 2014 and 2018 respectively; asking about ‘familiarity with symptoms’ increased the odds ratio with 2.4 and 2.6 in 2014 and 2018 respectively.
Fig. 1.
Percentages of pharmacies with correct and incorrect advice provision in 2014 and 2018 for total number of problem analysis questions (WWHAM plus condition-specific questions).
Table 4.
Association between problem analysis questions and correct advice provision in 2014 and 2018.
| Problem analysis questions | Year | OR (95% CI) |
|---|---|---|
| All questions | 2014 2018 |
1.8 (1.7–2.0) 2.3 (1.9–2.6) |
| Hay fever symptoms | 2014 2018 |
2.8 (2.2–3.6) 1.5 (1.3–2.0) |
| Other medication | 2014 2018 |
2.4 (1.6–3.6) 3.9 (2.3–6.7) |
| When symptoms occur | 2014 2018 |
1.9 (1.2–3.0) 4.0 (2.5–6.3) |
| Familiarity with symptoms | 2014 2018 |
2.4 (1.6–3.0) 2.6 (1.6–4.2) |
Table 5 shows the products (correct or incorrect according to the guideline) that were dispensed by pharmacies in each study year. The median number of problem analysis questions asked by pharmacy assistants who dispensed xylometazoline or xylometazoline/ipratropium in 2014 and 2018 was 1.5 and 2.0 respectively.
Table 5.
Numbers (percentages) of all pharmacies for dispensed products in 2014, 2016 and 2018.
| Year | 2014 | 2016 | 2018 |
|---|---|---|---|
| Number of pharmacies | 673 | 673 | 673 |
| Products dispensed | |||
| Correct advice | |||
| Antihistamine | 277 (41.2%) | 646 (96.0%) | 143 (21.2%) |
| (cetirizine or loratadine) | |||
| Incorrect advice | |||
| Sodium cromoglycate | 72 (10.7%) | 17 (2.5%) | 72 (10.7%) |
| Xylometazoline | 98 (14.6%) | 0 (0.0%) | 183 (27.2%) |
| Xylometazoline/ipratropium | 192 (28.5%) | 1 (0.1%) | 126 (18.7%) |
| Other products (saline, herbal) | 8 (1.1%) | 3 (0.4%) | 42 (6.2%) |
| No products dispensed | 26 (3.9%) | 6 (0.9%) | 107 (15.9%) |
3.3. Condition-based scenario (2016)
Table 3 shows that scores for individual problem analysis questions did not differ significantly for pharmacies that provided correct or incorrect advice. Questions about for whom the medication was meant for, action already taken and other medication used were asked by approximately 70% of pharmacy assistants. In the condition-based scenario 96.0% of all pharmacies advised an oral antihistamine according to the guideline, 2.5% advised sodium cromoglycate and almost 1% did not advise any product.
3.4. General communication skills
Table 6 shows that almost all pharmacies consistently scored high on general communication skills and most SPs were content on being served. Both in 2014 and 2018, sufficient consulting time, contentment, repeating of agreements or actions, explicitly asking if everything was clear, and offering the possibility to contact the pharmacy for questions or persistent complaints were significantly higher for pharmacies that provided correct advice than for pharmacies that provided incorrect advice. For 2014, also appropriate ending of the conversation was significantly higher for pharmacies that provided correct advice.
Table 6.
Percentages (numbers) of pharmacies for positive scores on general communication characteristics, stratified for correct and incorrect advice.
| Year | 2014 |
2016 |
2018 |
|||
|---|---|---|---|---|---|---|
| Correct advice | Incorrect advice | Correct advice | Incorrect advice | Correct advice | Incorrect advice | |
| Number of pharmacies | 277 | 396 | 646 | 27 | 143 | 530 |
| Friendly greeting | 98.9 (274) | 99.2 (393) | 99.4 (642) | 96.3 (26) | 100.0(143) | 99.6 (528) |
| Eye contact | 100.0 (277) | 99.2 (393) | 99.4 (642) | 92.6 (25) | 99.3 (42) | 99.4 (527) |
| Sufficient consulting time | 99,6 (276)⁎ | 89,1 (353)⁎ | 97,8 (632) | 96,3 (26) | 100,0 (143)⁎⁎ | 95,5 (506)⁎⁎ |
| Appropriate talking volume | 98,2 (272) | 97,5 (386) | 96,3 (622) | 92,6 (25) | 97,9 (140) | 97,2 (515) |
| Without interruption from others | 97,8 (271) | 98,2 (389) | 98,5 (636) | 100,0 (27) | 97,2 (139) | 98,3 (521) |
| Appropriate language | 99,6 (276) | 100,0 (396) | 100,0 (646) | 100,0 (27) | 99,3 (142) | 99,6 (528) |
| Calm and clear voice | 100,0 (277) | 99.2 (393) | 98,5 (636) | 100,0 (27) | 98.6 (141) | 99.2 (526) |
| Confident appearance | 96,8 (268) | 94.7 (375) | 98,9 (639) | 96,3 (26) | 97.0 (140) | 96.8 (513) |
| Appropriate ending of the conversation | 98,2 (272)⁎ | 91.2 (361)⁎ | 93,8 (606) | 96,3 (26) | 100.0 (143) | 98.9 (524) |
| SP content on being served | 98,9 274)⁎ | 82.3 (326)⁎ | 99,1 (640) | 85,2 (23) | 100.0 (143)⁎⁎ | 91.3 (484)⁎⁎ |
| Assistant repeats agreements or actions | 66,4 (184)⁎ | 37.1 (147)⁎ | 36,2 (234) | 51,9 (14) | 80.4 (115)⁎⁎ | 47.0 (249)⁎⁎ |
| Assistant explicitly asks if everything is clear/understood | 65,3 (181)⁎ | 42.2 (168)⁎ | 58,7 (379) | 55,6 (15) | 44.1 (63)⁎⁎ | 14.0 (74)⁎⁎ |
| Assistant mentions possibility to call or visit the pharmacy for questions or persistent complaints | 25,3 (70)⁎ | 7.6 (30)⁎ | 23,1 (149) | 25,9 (7) | 50.3 (72)⁎⁎ | 13.6 (72)⁎⁎ |
statistical significance tested by Chi-Square test, difference significant if p < 0.05.
statistical significance tested by Chi-Square test, difference significant if p < 0.05.
4. Discussion
Almost all pharmacies provided appropriate advice for a condition-based request (allergy) but less than half of all pharmacies gave appropriate advice for a symptom-based request (a running nose). In 2014 and 2018, the total number of questions and specific questions regarding the nature of the condition (e.g., asking about hay fever symptoms, other medications, when symptoms occurred and familiarity with symptoms) was associated with an odds ratio of 1.5–4.0 for providing correct advice. Most pharmacies scored consistently high on general communication skills like talking volume, appropriate language and eye contact. Pharmacy assistants that were insecure mostly consulted a colleague for advice; the percentage in 2018 being almost twice as high as in 2014 and 2016. Pharmacists were consulted by a very low percentage of pharmacy assistants.
The problem analysis questions were not consistently asked in pharmacies in 2014 or 2018. Within pharmacies, the probability of providing correct advice likely depended on the competency of the individual pharmacy assistant who provided the advice. The education level of pharmacy assistants in practice varies from a basic three-year vocational training to completed accredited (self-)care modules in addition to this basic training. In the Netherlands, the pharmacy technician position was added to the pharmacy workforce in 2004. To become a pharmacy technician, experienced pharmacy assistants must complete three additional years of training at the level of higher professional education, which includes theoretical courses and workplace learning.21 An estimated 20–25% of the 2000 community pharmacies in the Netherlands employ a pharmacy technician.
In 2014, 20% of pharmacy assistants asked no questions at all; this share was 7% in 2018. Possibly, feedback from earlier assessments may have led to more questions being asked. On the other hand, in 2018 there was no increase in the percentage of pharmacies that provided correct advice. In 2014 and 2018, pharmacy assistants in most pharmacies asked about symptoms in general. Also in 2014 and 2018, the majority of pharmacies that provided correct advice specifically asked about symptoms of hay fever; this share was significantly higher than that of pharmacies that provided incorrect advice. Itching symptoms distinguish hay fever from a common nose cold. Asking questions about these symptoms of hay fever at the beginning of a consultation should increase the odds ratio of identifying the correct condition and reduce clinical consultation time.13 Asking about ‘when symptoms occur ‘and about ‘familiarity of symptoms' significantly increased the odds of correct advice provision as well. Condition specific questions may be added to the WWHAM-method to encourage pharmacy assistants to ask these questions.
In 2014 and 2018, pharmacies that provided incorrect advice frequently asked about symptoms of hay fever but in these pharmacies the condition specific questions did not lead them to provide correct advice. A reason might be that counselling follows a process of collection of relevant information, correct problem identification and adequate problem solving and advice.14 This process can be supported by the WWHAM plus condition specific questions, but this may not be sufficient and additional skills may be needed.
Pharmacies use reports from SP visits as feedback to improve their counselling on minor ailments. Previous studies using SPs mostly included a limited number of pharmacies in a designated area.7,22, 23, 24 This study analyzed data from a high number of pharmacies all over the country which offers insight into the quality of self-care advice on a national level. Each individual pharmacy SP visit provided a snapshot of a counselling situation; however, because of the large number of snapshots over time an overall picture of the counselling and advice quality during subsequent years could be collected. Earlier research of AMP self-care scenarios in 2016 and 2017 (4 cases in each year) also found that problem analysis questions were not consistently asked in Dutch pharmacies.25 Pharmacy assistants' relatively low adherence to counselling guidelines may reflect the low priority of advice for minor ailments in Dutch pharmacies; pharmaceutical care generally focusses on prescription related medication issues (e.g., dispensing information, drug shortages, and medication review).26 It is the pharmacist's responsibility to ensure that pharmacy assistants are competent self-care advisors. This competence requires active knowledge of minor ailments and accurate appraisal of answers, on which items the pharmacy support workforce should be trained.
In the 2016 condition-based scenario, nearly all pharmacy assistants dispensed an appropriate product when the SP asked for something to treat an allergy, which suggests that they were aware of the guideline recommendation for allergic rhinitis. However, in the 2014 and 2018 symptom-based scenarios, less than 50% of pharmacies dispensed an appropriate product according to the guideline. In 2014 and 2018, xylometazoline was dispensed by more than 40% of all pharmacies, likely because pharmacy assistants asked a low number of questions (median: 1.5 and 2.0, respectively) and concluded that the symptoms were caused by a common cold. The timing of SP visits may have been a factor that contributed to the assumption of a common cold.27 These differences in performance are compliant with an overview of the simulated patient method which stated that scenario variation was shown to affect performance, including whether it relates to a direct product, a condition- or symptom-based request.28
In 2016, the median consultation time among pharmacies that provided correct advice was about 25% lower than that of pharmacies that provided correct advice in 2014. Contrary to 2014, in 2016 allergic rhinitis did not need to be established because the SP presented with an allergy and a much lower median consultation time was expected. In 2016, only the WWHAM questions for whom the product was meant for, use of other medication and the condition specific question about the kind of allergy were relevant for correct advice provision. The higher than expected consultation time in 2016 may be caused by pharmacy assistants failing to distinguish between essential and non-essential questions. Notably, there was a wide range of consultation times in all years, including for pharmacies that provided correct and incorrect advice. If the right questions are asked and answers are interpreted appropriately, providing correct advice may not take a long time. However, training is necessary to acquire this competency.
4.1. Strengths and limitations
A strength of this study lies in the relatively large number of pharmacies included. The 673 participating pharmacies account for more than one-third of the total number of pharmacies in the Netherlands.26 Moreover, the percentage of chain owned pharmacies in this study was 23% in 2016, whereas the national percentage of chain owned pharmacies in 2016 was 30%.26 Therefore, the results are likely representative of all community pharmacies in the Netherlands. An additional strength is that pharmacy staff were not aware of when they were being assessed, the identity of the SP or the self-care case that was being assessed.
A potential limitation is that the included pharmacies participated in the AMP program more than once, which suggests that participating pharmacies may be more focused on long-term development of self-care advice than other pharmacies. Therefore, the findings may skew toward an overestimation of the quality of pharmacies. However, in all study years one of the largest health care insurance companies offered the 50% highest scoring pharmacies that participated in the program a higher dispensing fee. For pharmacists, this may have been the incentive to subscribe to the program.
Only limited percentages of pharmacy assistants consulted a colleague or pharmacist. There may have been instances that the SP interacted with a pharmacist and not a pharmacy assistant. However, a complete account of the number of staff members that referred to a pharmacist could not be determined, as not all staff wear a pharmacy name plate.
This study compared the symptom-based scenarios in 2014 and 2018 despite differences in the scenarios, for example, the SP's age and familiarity with symptoms. Overall the 2018 scenario may have been more difficult than the 2014 scenario which may have contributed to the lower scores for correct advice provision. Also, the pharmacy assistants that approached the SP in 2014 and 2018 may have been different persons. This may as well have resulted in different scores for correct advice provision.
4.2. Implications for practice
The study findings indicate that pharmacists should ensure that their pharmacy assistants have active knowledge of minor ailments and are able to accurately appraise the answers they receive (e.g., through training) and should work to implement a pharmacy-wide self-care counselling policy to reduce the variety of advice given by different team members. Team discussions of the results of SP visits may be an adequate instrument to achieve these goals. With their team they can also discuss the recommendations of the guideline including condition-specific questions, instead of solely focusing on the WWHAM-mnemonic. Implementation of these measures may lead to the provision of consistent evidence-based advice, possibly with a reduction in consultation time. Pharmacists can also discuss with their team the point at which pharmacy assistants should consult them for self-care questions regarding allergic rhinitis. Management of allergic rhinitis is a complex process that requires a coordinated effort from consumers, patients and healthcare providers, including pharmacists and pharmacy assistants.29 A self-care counselling policy may benefit from the input of local GPs, based on a recent study finding that approximately 15–40% of people with allergic rhinitis also suffer from asthma and 80–90% of asthmatic patients also suffer from allergic rhinitis.30 Agreements can be made with GPs regarding referral of pharmacy clients to the GP practice.
5. Conclusions
The study findings indicate that a more detailed problem analysis by a pharmacy assistant is associated with an increase of the odds ratio of providing correct advice for a minor ailment. In 2014 and 2018, condition specific questions were also associated with an increase of the odds ratio of providing correct advice. In 2016, nearly all pharmacies dispensed an antihistamine for allergy when the patient specifically stated that they had an allergy. In 2014 and 2018, only half of the questions that predicted correct advice provision were part of the WWHAM mnemonic. Therefore, adding condition-specific problem analysis questions to the WWHAM mnemonic may be considered alongside educating the pharmacy team in active knowledge and accurate appraisal of answers to questions asked. Most pharmacies scored consistently high on conversation characteristics like talking volume, appropriate language and eye contact.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
The data used in this research are available on request, subject to AMP approval.
Declaration of Competing Interest
None.
Acknowledgements
The authors thank AMP pharmacist Hetty Prins and AMP researcher Martijn Hendrix for providing the data for this study, as well as Valerie Kleuver for her work on this study in the context of her master's research.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rcsop.2021.100086.
Appendix A. Supplementary data
Supplementary material
References
- 1.WHO . World Health Organisation; 2021. Self-care interventions for health.https://www.who.int/health-topics/self-care#tab=tab_1 Accessed 15 april 2021. [PubMed] [Google Scholar]
- 2.FIP . FIP; 2017. Pharmacy as a gateway to care.https://www.fip.org/files/fip/publications/2017-04-Pharmacy-Gateway-Care.pdf Accessed 15 April 2021. [Google Scholar]
- 3.FIP, GSCF Joint statement of policy on responsible and effective self-care. Int Pharmaceut Federat Global Self Care Federat. 2019:4. https://www.fip.org/files/content/publications/2019/FIP-GSCF-Responsible-and-effective-self-care.pdf Accessed 15 April 2021. [Google Scholar]
- 4.Brozek J.L., Bousquet J., Agache I., et al. Allergic rhinitis and its impact on asthma (ARIA) guidelines-2016 revision. J Allergy Clin Immunol. 2017;140(4):950–958. doi: 10.1016/j.jaci.2017.03.050. [DOI] [PubMed] [Google Scholar]
- 5.Aalberse J., Fokkens W., Lucassen P., et al. NHG; Utrecht: 2018. NHG standaard allergische en niet-allergische rhinitis. NHG standaarden.https://richtlijnen.nhg.org/standaarden/allergische-en-niet-allergische-rinitis Accessed 30 March 2021. [Google Scholar]
- 6.Geneesmiddel Informatie Centrum . Standaarden voor zelfzorg. 10 ed. KNMP; Den Haag: 2021. Standaarden voor zelfzorg. [Google Scholar]
- 7.Collins J.C., Schneider C.R., Naughtin C.L., Wilson F., Neto A.C.D., Moles R.J. Mystery shopping and coaching as a form of audit and feedback to improve community pharmacy management of non-prescription medicine requests: an intervention study. BMJ Open. 2017;7(12):8. doi: 10.1136/bmjopen-2017-019462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schneider C.R., Everett A.W., Geelhoed E., Kendall P.A., Clifford R.M. Measuring the assessment and counseling provided with the supply of nonprescription asthma reliever medication: a simulated patient study. Ann Pharmacother. 2009;43(9):1512–1518. doi: 10.1345/aph.1M086. [DOI] [PubMed] [Google Scholar]
- 9.Watson M.C., Bond C.M., Grimshaw J.M., Johnston M. Factors predicting the guideline compliant supply (or nonsupply) of non-prescription medicines in the community pharmacy setting. Qual Saf Health Care. 2006;15(1):53–57. doi: 10.1136/qshc.2005.014720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schneider C.R., Everett A.W., Geelhoed E., et al. Provision of primary care to patients with chronic cough in the community pharmacy setting. Ann Pharmacother. 2011;45(3):402–408. doi: 10.1345/aph.1P514. [DOI] [PubMed] [Google Scholar]
- 11.Rutter P. Role of community pharmacists in patients’ self-care and self-medication. Integr Pharm Res Pract. 2015;4:57–65. doi: 10.2147/iprp.S70403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akhtar S., Rutter P. Pharmacists thought processes in making a differential diagnosis using a gastro-intestinal case vignette. Res Soc Adm Pharm. 2015;11(3):472–479. doi: 10.1016/j.sapharm.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Rutter P. Elsevier; 2017. Community Pharmacy, Symptoms, Diagnosis and Treatment. [Google Scholar]
- 14.Schneider C.R., Gudka S., Fleischer L., Clifford R.M. The use of a written assessment checklist for the provision of emergency contraception via community pharmacies: a simulated patient study. Pharm Pract. 2013;11(3):127–131. doi: 10.4321/s1886-36552013000300001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.AMP Apotheken Monitoring Program: Onderzoek en advies in de zorg. https://www.ampnet.nl/ Accessed 26 March 2021.
- 16.SFK . Data en Feiten. SFK; Den Haag: 2015. Data en Feiten 2015.https://www.sfk.nl/publicaties/data-en-feiten/data-en-feiten-2015 Accessed 23 August 2021. [Google Scholar]
- 17.SFK . Data en Feiten. SFK; Den Haag: 2019. Data en Feiten 2019.https://www.sfk.nl/publicaties/data-en-feiten/data-en-feiten-2019 Accessed 23 August 2021. [Google Scholar]
- 18.Geneesmiddel Informatie Centrum . KNMP; Den Haag: 2014. Standaarden voor zelfzorg. 7 ed. Standaarden voor zelfzorg. [Google Scholar]
- 19.Geneesmiddel Informatie Centrum . Standaarden voor zelfzorg. 8 ed. KNMP; Den Haag: 2017. Standaarden voor zelfzorg. [Google Scholar]
- 20.KNMP . KNMP; Den Haag: 2018. Richtlijn ter hand stellen.https://www.knmp.nl/praktijkvoering/richtlijnen/knmp-richtlijnen-farmaceutische-zorg/knmp-richtlijn-ter-hand-stellen Accessed 23 August 2021. [Google Scholar]
- 21.Koehler T.C., Bok H., Westerman M., Jaarsma D. Developing a competency framework for pharmacy technicians: perspectives from the field. Res Soc Adm Pharm. 2019;15(5):514–520. doi: 10.1016/j.sapharm.2018.06.017. [DOI] [PubMed] [Google Scholar]
- 22.Schneider C.R., Everett A.W., Geelhoed E., et al. Provision of primary care to patients with chronic cough in the community pharmacy setting. Ann Pharmacother. 2011;45(3):402–408. doi: 10.1345/aph.1P514. [DOI] [PubMed] [Google Scholar]
- 23.Collins J.C., Schneider C.R., Faraj R., Wilson F., Neto A.C.D., Moles R.J. Management of common ailments requiring referral in the pharmacy: a mystery shopping intervention study. Int J Clin Pharm. 2017;39(4):697–703. doi: 10.1007/s11096-017-0505-8. [DOI] [PubMed] [Google Scholar]
- 24.Collins J.C., Schneider C.R., Moles R.J. Emergency contraception supply in Australian pharmacies after the introduction of ulipristal acetate: a mystery shopping mixed-methods study. Contraception. 2018;98(3):243–246. doi: 10.1016/j.contraception.2018.04.020. [DOI] [PubMed] [Google Scholar]
- 25.Blom L. Assistenten stellen niet alle relevante WHAM-vragen Pharmaceutisch Weekblad. 2017. https://www.pw.nl/achtergrond/2017/assistenten-stellen-niet-alle-relevante-wham-vragen Accessed 5 April 2021.
- 26.SFK . Dutch foundation for pharmaceutical statistics; Den Haag: 2017. Facts and figures 2017.https://www.sfk.nl/english/foundation-for-pharmaceutical-statistics Accessed 12 August 2021. [Google Scholar]
- 27.D’Amato G., Chong-Neto H.J., Ortega O.P.M., et al. The effects of climate change on respiratory allergy and asthma induced by pollen and mold allergens. Allergy. 2020;75(9):2219–2228. doi: 10.1111/all.14476. [DOI] [PubMed] [Google Scholar]
- 28.Collins J.C., Chong W.W., de Almeida Neto A.C., Moles R.J., Schneider C.R. The simulated patient method: design and application in health services research. Res Soc Adm Pharm. 2021 doi: 10.1016/j.sapharm.2021.04.021. [DOI] [PubMed] [Google Scholar]
- 29.Lourenco O., Bosnic-Anticevich S., Costa E., et al. Managing allergic rhinitis in the pharmacy: an ARIA guide for implementation in practice. Pharmacy. 2020;8(2):14. doi: 10.3390/pharmacy8020085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leynaert B., Neukirch C., Liard R., Bousquet J., Neukirch F. Quality of life in allergic rhinitis and asthma - a population-based study of young adults. Am J Respir Crit Care Med. 2000;162(4):1391–1396. doi: 10.1164/ajrccm.162.4.9912033. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
The data used in this research are available on request, subject to AMP approval.