Abstract
The contributory roles of vitamin D in ocular and visual health have long been discussed, with numerous studies pointing to the adverse effects of vitamin D deficiency. In this paper, we provide a systematic review of recent findings on the association between vitamin D and different ocular diseases, including myopia, age-related macular degeneration (AMD), glaucoma, diabetic retinopathy (DR), dry eye syndrome (DES), thyroid eye disease (TED), uveitis, retinoblastoma (RB), cataract, and others, from epidemiological, clinical and basic studies, and briefly discuss vitamin D metabolism in the eye. We searched two research databases for articles examining the association between vitamin D deficiency and different ocular diseases. One hundred and sixty-two studies were found. There is evidence on the association between vitamin D and myopia, AMD, DR, and DES. Overall, 17 out of 27 studies reported an association between vitamin D and AMD, while 48 out of 54 studies reported that vitamin D was associated with DR, and 25 out of 27 studies reported an association between vitamin D and DES. However, the available evidence for the association with other ocular diseases, such as glaucoma, TED, and RB, remains limited.
Keywords: vitamin D, ocular disease, vitamin D receptor, myopia, age-related macular degeneration, glaucoma, dry eye syndrome, thyroid eye disease, uveitis, retinoblastoma
1. Introduction
Vitamin D has diverse functions in maintaining human health, including regulating gene expression, immune system, inflammation, cell proliferation and differentiation, apoptosis, and angiogenesis [1,2]. Vitamin D3, or cholecalciferol, is produced from its precursor, 7-dehydrocholesterol, in the epidermal layer of skin under exposure to sunlight, or is obtained from the diet. It is metabolized in the liver and kidneys to its biologically active forms, 25-hydroxyvitamin D (25(OH)D3) and 1,25-dihydroxyvitamin D (1,25(OH)2D3), respectively. The latter is also known as potent steroid hormone calcitriol. Reduced sun exposure will lead to vitamin D deficiency [3,4]. Low vitamin D levels have been associated with many diseases, including cardiovascular diseases [5,6], hypertension [7], diabetes mellitus [8,9], and cancers [10].
The vitamin D status of an individual is usually determined by serum 25(OH)D3 instead of 1,25(OH)2D3 because of its longer circulating half-life and higher concentration in circulation [11]. Besides, 1,25(OH)2D3 levels are affected by calcium levels [12,13]. Even though a range of thresholds is used between various scientific societies, having blood levels lower than 12 ng/mL of 25(OH)D3 represents deficiency, 12–20 ng/mL represents insufficiency, 20–100 ng/mL represents sufficiency, and >100 ng/mL indicates a risk of toxicity [14].
2. Metabolism of Vitamin D
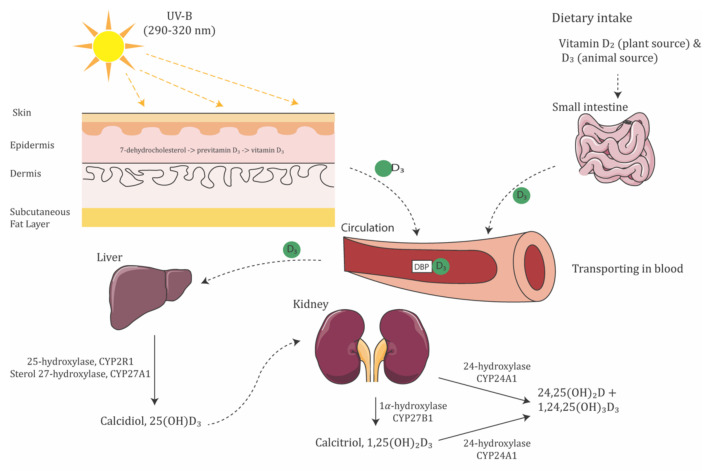
Vitamin D is synthesized and activated in three steps (Figure 1). Cholecalciferol (vitamin D3) and ergocalciferol (vitamin D2) are the two major biologically inert precursors of vitamin D. For the former, 7-dehydrocholesterol in the skin produces previtamin D3 under exposure to ultraviolet B radiation (UVB, λ = 290–315 nm), which then thermally isomerizes to Vitamin D3 in the skin; in contrast, vitamin D2 is derived from plants and obtained from the diet. After its production, vitamin D3 attaches to vitamin D-binding protein (DBP) in the liver, where it is activated to produce 25(OH)D3, the primary circulating form of vitamin D, by 25-hydroxylases, CYP2R1 and CYP27A1. Then, 25(OH)D3 is converted to 1,25(OH)2D3, the active form of vitamin D, by 1α-hydroxylase, CYP27B1. In contrast, vitamin D2 is derived from plants and obtained from the diet. CYP27A1 does not hydroxylate vitamin D2 at the 25 positions. Lastly, vitamin D metabolite levels are downregulated by CYP24A1, which catalyzes the 24-hydroxylation of both 25(OH)D3 and 1,25(OH)2D3 [15]. The genetic variation in the metabolic enzyme would affect the regulation of vitamin D levels.
Figure 1.
Schematic illustration of vitamin D synthesis pathway. Moreover, 7-dehydrocholesterol in the epidermis layer of skin absorbs UV-B radiation and is converted to pre-vitamin D3. Vitamin D3, by either the isomerization of pre-vitamin D3 in the epidermal basal layers or intestinal absorption from the diet, binds to vitamin D-binding protein (DBP) in the bloodstream, transported to the liver. Vitamin D3 is hydroxylated by 25-hydroxylase or sterol 27-hydroxylase. The resultant calcidiol (25(OH)D3) is 1α-hydroxylated in the kidney by 1α-hydroxylase, yielding biologically active vitamin D (1,25(OH)2D3).
Moreover, 1,25(OH)2D3 can penetrate the cell membranes, either as a free molecule or in DBP-1,25(OH)2D3 complexes. It then binds to the vitamin D receptor (VDR), facilitating the interaction of VDR with the retinoic X receptor (RXR) [16]. This VDR-RXR heterodimer binds to both positive and negative vitamin D response elements in target genes, influencing gene transcription [17]. Hence, the presence of VDR suggests the local activity of vitamin D [18]. In particular, VDR has been detected in different parts of the eye, including the epithelium and endothelium of the cornea, lens, ciliary body, retinal ganglion cells (RGCs), inner nuclear layer, photoreceptors, and retinal pigment epithelium (RPE) [19,20]. Genetic alternations of the VDR gene could lead to defects in gene function, calcium metabolism, cell proliferation, and immune function. DBP is mainly responsible for the transportation of vitamin D and its metabolites.
Levels of active vitamin D in the body are regulated by the enzymes 25-hydroxylase, 1α-hydroxylase, and 24-hydroxylase [15]. In a recent study, the 25(OH)D3 and 1,25(OH)2D3 generating enzymes 25-hydroxylase (CYP2R1 and CYP27A1) and 1α-hydroxylase (CYP27B1), as well as the deactivating enzyme 24-hydroxylase (CYP24A1), were found to be strongly localized at the complementary regions of the ciliary body, RPE, neural retina, corneal epithelium and endothelium, and scleral fibroblast, suggesting that vitamin D in the eye is locally produced, activated, and regulated [21,22]. Moreover, vitamin D-dependent calcium binding protein calbindin, a vitamin D metabolizing protein, was shown to be expressed throughout the human retina [23]. Some of the cohort studies reported the correlation of metabolic enzymes in ocular diseases. In diabetic patients, retinal CYP27B1 was found to correlate strongly with VEGF-A in the eyes [24]. In a cohort of patients with Vogt-Koyanagi-Harada disease, a non-synonymous variant of CYP2R1 was found in 17 of 39 patients, suggesting that the variant in CYP2R1 may play a role in VKH pathogenesis [25].
Some of the vitamin D regulating proteins, such as ferredoxin reductase participating in the activation of vitamin D in the kidney, are metalloproteins. Vitamin D is able to interact with the matrix metalloproteinase. Metal deficiency may affect ocular condition. However, only one study found significantly lower serum calcium levels in blepharospasm patients, but no significant difference in magnesium, phosphorus, or vitamin D [26].
Therefore, the potential of vitamin D to regulate various processes of potential relevance to ocular diseases has been acknowledged. Studies investigating the roles of vitamin D in ocular tissues and ocular disease pathogenic pathways have been carried out and will continue to contribute towards our understanding of ocular disease mechanisms and help establish effective intervention.
3. Vitamin D and Ocular Diseases
The potential effect of vitamin D deficiency on human health is a big concern. Recently, especially over the past few years, since the last published review articles related to vitamin D and ocular diseases, more and more studies investigating the relationship between serum vitamin D level and ocular diseases were published, including some prospective studies examining this relationship and therapeutic effects of vitamin D. Currently, review articles related to vitamin D and ocular disease are available [18,20]. To update this and reach a comprehensive understanding, hence, we performed a systematic review here to summarize the evidence revealing the association between vitamin D and ocular diseases.
3.1. Method of Literature Search
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines [27]. The protocol is described as follows.
3.1.1. Search Strategy
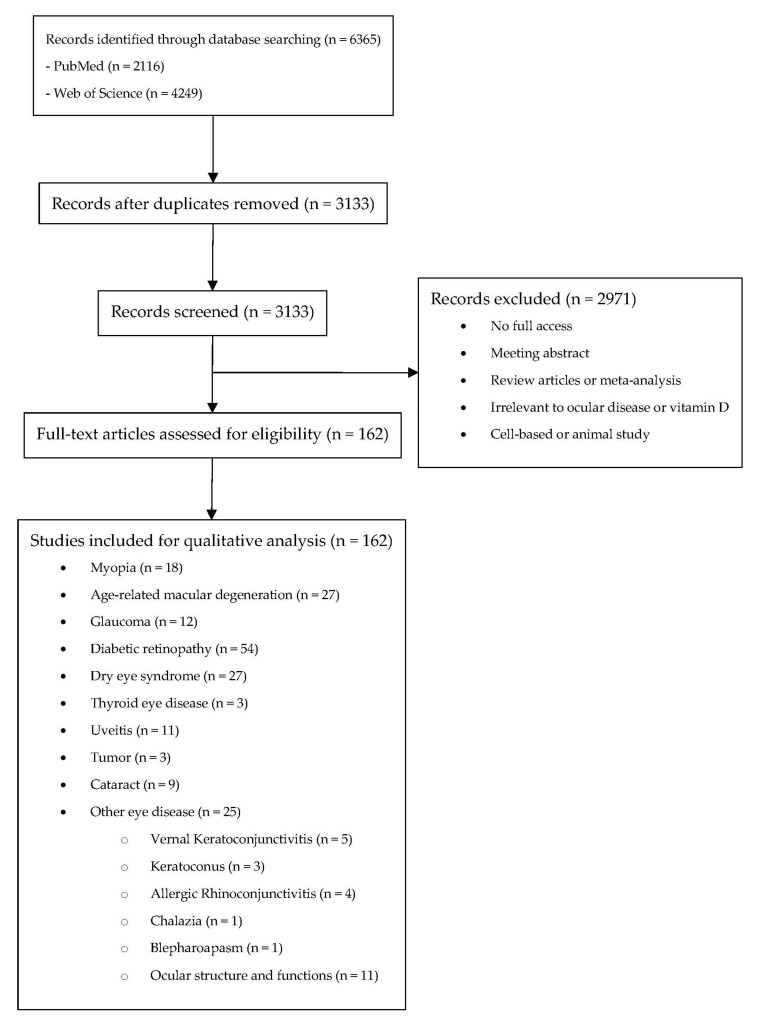
A systematic search on PubMed (Available online: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?DB5pubmed, accessed on 18 March 2022) and Web of Science (Available online: https://www.webofscience.com/wos/woscc/basic-search, accessed on 18 March 2022) with coverage up to 18 March 2022 was conducted initially using the following keywords: vitamin D in combinations with eye (PubMED: 544; WOS: 1909), eye disease (PubMed: 824; WOS: 854), ocular (PubMed: 183; WOS: 534), cataract (PubMed: 158; WOS: 355), lens opacity (PubMed: 118; WOS: 51), glaucoma (PubMed: 51; WOS: 151), intraocular pressure (PubMed: 24; WOS: 68), maculopathy (PubMed: 85; WOS: 97), diabetic retinopathy (PubMed: 126; WOS: 228), hypertensive retinopathy (PubMed: 2; WOS: 2), retinal arterial occlusion (PubMed: 0; WOS: 0), retinal venous occlusion (PubMed: 1; WOS:0). The search results from both databases were exported and imported in Covidence, which is a software for literature screening in systematic reviews. Among these 6813 results, the system detects that 3533 results were duplicated. They have been removed prior to the screening of the articles (Figure 2).
Figure 2.
Systematic review flow diagram.
3.1.2. Inclusion and Exclusion Criteria
The inclusion criteria for studies were: (1) written in English; (2) evaluating the association between blood vitamin D and different ocular diseases in a randomized controlled trial, prospective study, cross-sectional study, or case-control study. After a review of abstracts, relevant articles were retrieved and reviewed. Bibliographies of these articles provided further references. All retrieved records were reviewed by two independent reviewers (HNC and XL). Uncertainties were resolved via discussion with another reviewer (XJZ).
3.1.3. Risk of Bias Assessment
Included interventional studies (both randomized controlled trials and clinical controlled trials) were assessed for quality according to the RoB tool for randomized trials from the Effective Practice and Organisation of Care (EPOC) Group. The assessment for the clinical controlled trial was assessed according to the suggestion from previous literature that both “random sequence generation” and “allocation concealment” were scored as “high risk”, while grading the remaining items as RCT [28]. We further modified the RoB tool by allocating 1 point to “low risk”, 0.5 point to “unclear risk” and 0 points to “high risk”. There are a total of 9 items to be assessed using the RoB tool, and hence, the total number of points for the RoB tool is 9 points, while those cohort, case-control, cross-sectional studies were assessed for quality according to the LEGEND (Let Evidence Guide Every New Decision) System designed for Cincinnati Children’s Hospital [29].
3.2. Myopia
Myopia is an important public health problem worldwide [30]. The etiology of myopia is complex, with both genetic and environmental risk factors [31,32,33,34]. Epidemiologic evidence indicates that time spent outdoors is a protective factor against myopia development [34,35,36,37,38], yet the underlying mechanism is unclear. Since the main source of vitamin D is sunlight exposure, vitamin D is linked to myopia, hypothesizing that a vitamin D pathway may mediate the protective effect of time spent outdoors on myopia. Evidence from studies on the relationship of vitamin D and myopia is summarized in Table 1.
Table 1.
Summary of studies related to myopia included.
| First Author | Years | Country | Study Design | Sample Size | Main Finding | Rate # |
|---|---|---|---|---|---|---|
| Jin A. Choi [39] | 2014 | South Korea | Cross-sectional study | 2038 subjects | Individuals with higher concentrations of serum 25(OH)D had lower prevalences of myopia after adjustment for confounding factors (p < 0.001). In multiple linear regression analyses, spherical equivalent was significantly associated with serum 25(OH)D concentration after adjustment for confounding factors (p = 0.002). | 4a |
| Jeremy A. Guggenheim [40] | 2014 | UK | Prospective observational study | 3677 subjects | Total vitamin D and D3 were biomarkers for time spent outdoors, however there was no evidence they were independently associated with future myopia. | 3a |
| Donald O. Mutti [41] | 2011 | United States | Cross-sectional study | 32 subjects | Adjusted for differences in the intake of dietary variables, myopes appear to have lower average blood levels of vitamin D than non-myopes. | 4b |
| J. Willem L. Tideman [42] | 2016 | Netherlands | Cross-sectional study | 2666 subjects | Serum levels of 25(OH)D3 were inversely related to AL, and that low levels increased the risk of myopia. This relationship may be independent from time spent outdoors. | 4a |
| Seyhan Yazar [43] | 2014 | Australia | Cross-sectional study | 946 subjects | Myopic participants had significantly lower 25(OH)D3 concentrations. The prevalence of myopia was significantly higher in individuals with vitamin D deficiency compared to the individuals with sufficient levels. | 4a |
| Jin-woo Kwon [44] | 2017 | South Korea | Cross-sectional study | 15,126 subjects | Low serum 25(OH)D3 levels and shorter daily sun exposure time may be independently associated with a high prevalence of myopia in Korean adults. These data suggest a direct role for vitamin D in the development of myopia. | 4a |
| Katie M. Williams [45] | 2016 | Europe including Norway, Estonia, United Kingdom, France, Italy, Greece, and Spain | Cross-sectional study | 3168 subjects | No independent associations between myopia and serum vitamin D3 concentrations nor variants in genes associated with vitamin D metabolism were found. No convincing evidence for a direct role of vitamin D in myopia risk. | 4a |
| Ina Olmer Specht [46] | 2020 | Denmark | Case-control study | 457 myopic subjects and 1280 emmetropic subjects | No increased odds of myopia in relation to low neonatal 25(OH)D3 levels, and no seasonal variation in myopia risk. | 4a |
| Byung J Jung [47] | 2020 | South Korea | Cross-sectional study | 25,199 subjects | Serum 25(OH)D3 level was inversely associated with myopia in Korean adults. | 4a |
| Hung-Da Chou [48] | 2021 | China | Prospective, cross-sectional study | 99 Preterm children | Among preterm children with or without ROP, more time spent outdoors was associated with lower odds of myopia. The serum 25(OH)D3 concentration was not associated with myopia, but a high proportion of the participants had insufficient levels. | 4a |
| Gareth Lingham [49] | 2021 | Australia | Multi-generation, longitudinal cohort study | 1260 subjects | Myopia in young adulthood was most strongly associated with recent 25(OH)D3 concentrations, a marker of time spent outdoors. | 3a |
| Sang Beom Han [50] | 2019 | South Korea | Cross-sectional study | 3398 subjects | Lower serum 25(OH)D3 concentration (<9 ng/mL) was associated with increased prevalence of both myopia and high myopia. Serum 25(OH)D3 concentration of ≥9 ng/ml was significantly associated with decreased prevalence of high myopia in participants with near work of ≥3 h/day, although the effect was not significant in myopia and low myopia. | 4a |
| Fan Gao [51] | 2021 | China | Cross-sectional study | 186 subjects | Children with a higher level of serum 25(OH)D3 have a lower prevalence of moderate to high myopia. | 4a |
| Gareth Lingham [52] | 2019 | Australia | Cross-sectional study | 4112 subjects | Vitamin D levels are unrelated to myopia risk in adults. | 4a |
| Ho Sik Hwang [53] | 2018 | South Korea | Cross-sectional study | 11,703 subjects | Serum 25(OH)D3 level (OR, 0.97 per 1 ng/mL) showed protective effect against high myopia | 4a |
| Harb Elise N [54] | 2021 | United States | Cross-sectional study | 4838 subjects | There is nonsignificant correlation between serum vitamin D levels and spherical equivalent refractive errors | 4a |
| Didik Wahyudi [55] | 2020 | Indonesia | Non-randomised pre-post study | 80 subjects | Vitamin D supplementation and sunlight exposure could increase serum 25-hydroxyvitamin D, decrease myopia, and inhibit the progression of myopia. | 8/12* |
| Xiaoman Li [56] | 2022 | China | Cross-sectional study | 294 lowland area children and 89 highland area children | There is no association between serum 25(OH)D concentration and myopia in the 6–14 years old Chinese children. | 4a |
* NIH quality assessment tool for before-after (Pre-Post) study with no control group; # LEGEND for case-control, cohort, and cross-sectional studies, rating of the studies follow the guidelines from LEGEND.
As demonstrated in Table 1, the association between vitamin D and myopia is controversial in cross-sectional studies. Many studies suggest that the serum 25(OH)D3 level shows an inverse association with myopia and may have a protective effect on myopia [39,41,42,43,44,47,50,51,53,55]. However, several case-control studies from Australia [52], Denmark [46], and the US [54] found that the risks of myopia are not related to their neonatal vitamin D levels.
Nevertheless, it is important to distinguish the causation between vitamin D and myopia. A large longitudinal cohort study found that 25(OH)D3 levels correlated with self-reported time spent outdoors; however, no evidence suggested that the participants’ serum vitamin D levels were independently associated with myopia [40]. Another study of preterm children also suggested that more time spent outdoors was associated with a lower risk of myopia, despite serum 25(OH)D3 concentrations not being shown to relate to myopia [48]. However, an Australian perspective study showed that, in young adults, myopia was most strongly associated with recent 25(OH)D3 concentrations, which is a marker of time spent outdoors [49].
Our meta-analysis found that the risk of myopia is inversely associated with blood 25(OH)D3 concentration after adjusting for sunlight exposure or time spent outdoors. However, this relationship was not significant among individuals under 18 years of age [57]. Polymorphisms in the vitamin D pathway genes may affect the development of myopia. One study reported the association of VDR polymorphisms, rs2853559, with myopia [58]. However, the results of other studies suggested that the true contribution of the vitamin D pathway to myopia could be negligible [42,45,59]. Our meta-analysis suggested that polymorphisms in the VDR gene are not associated with myopia [57]. On the other hand, animal studies proved that violet light (VL, λ = 360–400 nm) can suppress myopia progression, whereas no therapeutic effects were observed with UVB radiation (λ = 290–315 nm) [60], suggesting that UVB exposure and its dependent vitamin D synthetic pathway may not have a protective effect on myopia progression.
In conclusion, from the literature evidence, we know that, although blood 25(OH)D3 concentration is inversely associated with the risk of myopia, it seems unlikely that vitamin D has a direct protective effect on myopia progression. Instead, vitamin D levels may only serve as a biomarker for outdoor exposure.
3.3. Age-Related Macular Degeneration
As a chronic, progressive, degenerative disease, age-related macular degeneration (AMD) is a major cause of central blindness among people aged 60 years or over worldwide [61,62]. Oxidation, inflammation, and angiogenesis contribute to the pathogenesis of AMD, resulting in the dysfunction of RPE [63], Bruch’s membrane, and choriocapillaries [64]. In an aging retina, the complement cascade [65,66] and the tissue resident macrophage (retinal microglia) activation pathway [67] ultimately cause protein damage and aggregation, and degeneration of the RPE [68]. Angiogenesis, often caused by oxidative stress and inflammatory reactions, plays a major role in the development and progression of exudative AMD, potentially leading to severe and permanent visual impairment.
The results of studies on cell lines and animal models have shown that vitamin D can protect cells or reduce oxidative stress [69,70,71]. Vitamin D has an anti-inflammatory role in chronic inflammatory diseases by decreasing the proliferation of T-cells and the production of pro-inflammatory agents [72,73]. On the other hand, vitamin D exerted an inhibitory effect on the angiogenesis signaling pathway [74,75], which may play a protective role in exudative AMD development and/or progression. Morrison et al. studied the variants in the vitamin D catabolizing enzyme, CYP24A1, and reported that variants (rs1570669, rs1570670, rs2274130, rs2296239, and rs4809957) were associated with reduced risk for AMD [76].
Table 2 summarized the studies on vitamin D and AMD. Case-control studies with small sample sizes suggest that AMD patients always have relatively low levels of serum vitamin D [77,78,79,80,81,82,83,84,85,86,87], except in a Iranian study, which did not find any significant correlation between serum vitamin D level and AMD [79]. However, this association seems to change in cross-sectional studies with larger sample sizes. Population-based studies held in France [88], the United States [89,90], and Israel [91] did not support a specific role for vitamin D in AMD, but vitamin D may work in some specific populations. An analysis of a sample of 1313 US participants indicated that high serum 25(OH)D3 concentrations may protect against early AMD in women less than 75 years old [92], while another US study supported the fact that levels of serum vitamin D were inversely associated with early AMD but not advanced AMD [93]. A Korean study had 17,045 participants and found that a high level of vitamin D was inversely associated with late AMD in men but not women [94]. Vitamin D deficiency in the European population was found to be associated with nvAMD, but the adjusted OR was small, and cannot exclude residual confounding [95].
Table 2.
Summary of studies related to age-related macular degeneration included.
| First Author | Years | Country | Study-Design | Sample Size | Main Finding | Rate # |
|---|---|---|---|---|---|---|
| Audrey Cougnard-Grégoire [88] | 2018 | South Korea | Case-control study | 32 Early AMD, 30 late AMD, and 34 normal controls | Serum vitamin D deficiency increases the risk of early AMD with borderline significance [odds ratio (OR) = 3.59; 95% confidence interval (95% CI) 0.95–13.58; p = 0.060], while significantly associated with a higher risk of late AMD (OR = 3.61; 95%CI 1.04–12.51; p = 0.043). In 2 subgroups of late AMD, serum vitamin D deficiency only increase the risk of patients with subretinal fibrosis (OR = 7.54; 95% CI 1.34–42.51), but not. However, there was no significant association between serum vitamin D deficiency and late AMD without subretinal fibrosis (OR = 1.89; 95% CI 0.40–8.92). | 4a |
| Shelley Day [89] | 2017 | Europe (Norway, Estonia, UK, France, Italy, Greece, Spain) | Cross-sectional study | 2209 Early AMD, 150 late AMD and 104 nvAMD | No linear association was found with 25(OH)D and early or late AMD or nvAMD. Deficient status was associated with nvAMD (adjusted OR, 1.27; 95% confidence interval, 1.1–1.45; p < 0.0001), but no association between insufficient or deficient status with early or late AMD. | 4b |
| S Golan [91] | 2015 | United States | Cross-sectional study | 913 subjects | For women with vitamin D deficient (<12 ng/mL), there were 6.7-fold increased odds of AMD (95% CI, 1.6–28.2). | 4b |
| Alix Graffe [78] | 2019 | United States | Prospective study | 1225 subjects | High 25(OH)D3 concentrations, approximately >70 nM, may be associated with decreased odds of incident early AMD. | 4b |
| Rezvan Hashemi [79] | 2017 | United States | Cross-sectional study | 9734 subjects | The adjusted OR (95% CIs) for early AMD among those with adequate (=75 nmol/L) compared to deficient (<30 nmol/L) vitamin D status was 0.94 (0.59–1.50), p-trend = 0.86. Vitamin D status was not associated with early AMD in this cohort sample. | 4b |
| Sujit Itty [96] | 2011 | United States | Cross-sectional study | 1313 subjects | Serum 25(OH)D was associated with decreased odds of early AMD in women younger than 75 years and increased odds in women aged 75 years or older (OR for quintile 5 vs. 1, 0.52; 95% CI, 0.29–0.91; p for trend = 0.02 and OR, 1.76; 95% CI, 0.77–4.13; p for trend = 0.05, respectively). High serum 25(OH)D3 concentrations may protect against early AMD in women younger than 75 years. | 4a |
| Emrah Kan [80] | 2011 | United States | Cross-sectional study | 100 subjects (50 pairs of siblings) | Comparing among affected and unaffected siblings, serum 25(OH)D levels were not statistically different (p = 0.22). Although evaluation of serum 25(OH)D3 was higher in unaffected individuals than in their affected siblings, but the finding did not reach statistical significance. | 4a |
| Eun Chul Kim [94] | 2007 | United States | Cross-sectional study | 7752 subjects | Levels of serum vitamin D were inversely associated with early AMD but not advanced AMD. The odds ratio (OR) and 95% confidence interval (CI) for early AMD among participants in the highest vs. lowest quintile of serum vitamin D was 0.64 (95% CI, 0.5–0.8; p trend <0.001). | 4a |
| Kyoung Lae Kim [81] | 2013 | Denmark | Cross-sectional study | 178 subjects | Across different AMD stages by CARMS, the plasema 25(OH)D levels were comparable. In CARMS 5, the presence of subretinal fibrosis was associated with significantly lower concentrations of 25-hydroxyvitamin D as compared to the absence of subretinal fibrosis (47.2 versus 75.6 nmol/L, p < 0.001). Patients in CARMS 5 with subretinal fibrosis were more likely to have insufficient levels of 25-hydroxyvitamin D compared to patients without subretinal fibrosis (p = 0.006) | 4a |
| Gareth J.McKay [95] | 2020 | United States | RCT | 25,871 subjects | Neither vitamin D3 nor marine ω-3 fatty acid supplementation had a significant overall effect on AMD incidence or progression. | 4a |
| Amy E. Millen [92] | 2017 | France | Prospective cohort study | 2146 subjects | Compared with the highest and lowest quintile of dietary vitamin D intake after adjustment for other confounding facters, there was a lower risk of progression to late AMD and NV (for late AMD: hazard ratio [HR]: 0.60; 95% confidence interval [CI]: 0.43–0.83; p trend = 0.0007; for NV: HR: 0.59; 95% CI: 0.39–0.89; p trend = 0.005) but not GA (HR: 0.83; 95% CI: 0.53–1.30; p trend = 0.35). When supplement use was considered, the effect was in the protective direction but was not significant. A diet rich in vitamin D may prevent or delay progression to advanced AMD, especially nvAMD. | 4a |
| Amy E. Millen [87] | 2016 | Japan | Case-control study | 161 Neovascular AMD patients and 369 healthy controls | Logistic regression analysis demonstrated that low intakes of vitamin D was associated with neovascular AMD (Trend p = 0.002 for vitamin D). High dietary intake of vitamin D is associated with a reduced risk of AMD. | 3a |
| Amy E. Millen [90] | 2011 | France | Cross-sectional study | 311 subjects | Low serum 25OHD concentrations were associated with poorer vision acuity. | 4a |
| Amy E. Millen [97,98] | 2021 | Turkey | Retrospective study | 114 ARMD and 102 healthy controls | The age-related macular degeneration group had significantly lower vitamin D levels than the control group (p > 0.001). Significantly decreased levels of 25(OH) vitamin D in advanced-stage age-related macular degeneration suggest a significant correlation existing between vitamin D deficiency and age-related macular degeneration development | 4a |
| Margaux A. Morrison [76] | 2020 | Egypt | Cross-sectional study | 222 Primary osteoarthritis patients (46 with AMD, 176 without AMD) | Less vitamin D intake were significantly associated with AMD occurrence in primary osteoarthritis patients. | 4b |
| Niyati Parekh [93] | 2019 | Italy | RCT | 30 Intermediate AMD | In intermediate AMD, Macuprev® supplementation (contained vitamin D3 800 IU) increases the function of the macular pre-ganglionic elements, with no associated retinal and choroidal ultra-structural changes. | 4a |
| Amardeep Singh [82] | 2011 | United States | Case series | 184 Caucasian male twin pairs | Higher dietary intake of vitamin D was present in the twins with less severe AMD (p = 0.01) and smaller drusen size (p = 0.05) compared with co-twins, adjusted for smoking and age | 4b |
| William G. Christen [99] | 2015 | France | Cross-sectional study | 91 subjects | Patients with vitamin D deficiency (n = 11) had a reduced mean GCC thickness compared to those without vitamin D deficiency (72.1 ± 7.4 μm versus 77.5 ± 7.5 μm, p = 0.028) | 9/9 * (RoB) |
| Bénédicte M. J. Merle [100] | 2022 | Spain | Cross-sectional study | 93 AMD patients and 93 healthy controls | The AMD patients had statistically significant lower 25 (OH)D levels than healthy controls but the median 25(OH)D levels in different stages and subtypes (early, intermediate, advance atrophic and advanced neovascular) were not statistically significant. | 3a |
| Aya Aoki [101] | 2018 | South Korea | Case-control study | 32 Early AMD, 30 late AMD, and 34 normal controls | Serum vitamin D deficiency increase the risk of early AMD with borderline significance [odds ratio (OR) = 3.59; 95% confidence interval (95% CI) 0.95–13.58; p = 0.060], while significantly associated with a higher risk of late AMD (OR = 3.61; 95%CI 1.04–12.51; p = 0.043). In 2 subgroups of late AMD, serum vitamin D deficiency only increase the risk of patients with subretinal fibrosis (OR = 7.54; 95% CI 1.34–42.51), but not. However, there was no significant association between serum vitamin D deficiency and late AMD without subretinal fibrosis (OR = 1.89; 95% CI 0.40–8.92). | 4a |
| Olivier Beauchet [102] | 2017 | Europe (Norway, Estonia, UK, France, Italy, Greece, Spain) | Cross-sectional study | 2209 Early AMD, 150 late AMD and 104 nvAMD | No linear association was found with 25(OH)D and early or late AMD or nvAMD. Deficient status was associated with nvAMD (adjusted OR, 1.27; 95% confidence interval, 1.1–1.45; p < 0.0001), but no association between insufficient or deficient status with early or late AMD. | 3a |
| Naciye Kabataş [83] | 2015 | United States | Cross-sectional study | 913 subjects | For women with vitamin D deficient (<12 ng/mL), there was 6.7-fold increased odds of AMD (95% CI, 1.6–28.2). | 4a |
| Marwa Yahia Mahgoub [86] | 2019 | United States | Prospective study | 1225 subjects | High 25(OH)D3 concentrations, approximately >70 nM, may be associated with decreased odds of incident early AMD. | 4a |
| Mariacristina Parravano [103] | 2017 | United States | Cross-sectional study | 9734 subjects | The adjusted OR (95% CIs) for early AMD among those with adequate (=75 nmol/L) compared to deficient (<30 nmol/L) vitamin D status was 0.94 (0.59–1.50), p-trend = 0.86. Vitamin D status was not associated with early AMD in this cohort sample. | 8/9 * (RoB) |
| Johanna M Seddon [84] | 2011 | United States | Cross-sectional study | 1313 subjects | Serum 25(OH)D was associated with decreased odds of early AMD in women younger than 75 years and increased odds in women aged 75 years or older (OR for quintile 5 vs. 1, 0.52; 95% CI, 0.29–0.91; p for trend = 0.02 and OR, 1.76; 95% CI, 0.77–4.13; p for trend = 0.05, respectively). High serum 25(OH)D3 concentrations may protect against early AMD in women younger than 75 years. | 4a |
| Mathieu Uro [85] | 2011 | United States | Cross-sectional study | 100 subjects (50 pairs of siblings) | Comparing among affected and unaffected siblings, serum 25(OH)D levels were not statistically different (p = 0.22). Although evaluation of serum 25(OH)D3 was higher in unaffected individuals than in their affected siblings, but the finding did not reach statistical significance. | 3a |
| Perez Serena [104] | 2007 | United States | Cross-sectional study | 7752 subjects | Levels of serum vitamin D were inversely associated with early AMD but not advanced AMD. The odds ratio (OR) and 95% confidence interval (CI) for early AMD among participants in the highest vs. lowest quintile of serum vitamin D was 0.64 (95% CI, 0.5–0.8; p trend <0.001). | 3a |
nvAMD = nonvascular AMD; * The Effective Practice and Organisation of Care (EPOC) RoB Tool for randomized trials; # LEGEND for case-control, cohort, and cross-sectional studies, rating of the studies follow the guidelines from LEGEND.
Prospective studies, however, have not found a consistent association between vitamin D and the risk of developing AMD. In a large prospective cohort study of 2146 participants with a mean follow-up time of over 9 years, high dietary intake of vitamin D was significantly associated with a 40% lower risk of progression to advanced AMD [99]. However, recently, a nationwide, placebo-controlled, randomized clinical trial found that supplementing vitamin D had no significant overall effect on AMD incidence or progression in healthy people [98]. For this trial, 25,871 participants with a median age of 67.1 years were divided into four groups, receiving vitamin D supplements (2000 IU/day), ω-3 fatty acids (1 g/day), a combination of both, and placebo, respectively. After a median follow-up period of 5.3 years, no significant differences were found in the incidence or progression of AMD when compared with baseline [98]. This study suffered from a lack of stratification by clinical manifestations of AMD, a relatively short follow-up period for chronic disease, and a reliance on self-reported AMD diagnosis, leading to inconsistencies with the previous two studies [98,104].
In summary, cross-sectional studies suggest that vitamin D may have a protective effect on AMD formation, but this effect is small or may only work in a specific population. Furthermore, evidence from prospective cohort studies showed that continuously supplementing vitamin D may not reduce the risks of AMD over a period of several years.
3.4. Glaucoma
A leading cause of irreversible blindness, glaucoma is a group of optic neuropathies involving the death of retinal ganglion cells (RGCs) and the loss of their axons [105,106]. Two cross-sectional studies in South Korea reported that vitamin D deficiency is associated with glaucoma [107,108]. Similarly, a Chinese study found that the vitamin D deficiency, along with the presence of the BsmI ‘B’ allele and TaqI ‘t’ allele of the VDR gene, are relevant risk factors for glaucoma development [109]. Other studies in France [110], Croatia [111], the United States [112,113], and Turkey [114] have demonstrated that glaucoma patients have lower serum vitamin D levels compared to normal controls. However, another Turkish case-control study found no statistically significant difference in serum vitamin D levels between glaucoma patients and control subjects [115]. Similarly, a recent large-sample study in the United States showed that dietary intake, supplements, and serum levels of vitamin D are not significantly related to the risk of glaucoma [116]. Notably, ethnicity may contribute to the pathogenesis of glaucoma, giving rise to different conclusions among these studies [117]. Most of the literature reported the association between vitamin D and glaucoma and that a lower vitamin D concentration was found in glaucoma patients when compared with the control group [108,109,110,111,114], however, there were no findings on the association between vitamin D and the severity. Increases in vitamin D were associated with lower risks of having glaucoma (fourth quintile versus first quintile, OR 0.713, 95% confidence interval, 0.520 to 0.979) [108]. Only a limited study reported no statistically significant difference between the glaucoma group and the control group [108]; significantly lower vitamin D can only be found in advanced glaucoma patients [112] (Table 3).
Table 3.
Summary of studies related to glaucoma included.
| First Author | Years | Country | Study-Design | Sample Size | Main Finding | Rate # |
|---|---|---|---|---|---|---|
| Einar Andreas Krefting [118] | 2013 | Norway | 1.Nested case-control; 2. randomized controlled intervention trial | 1. 87 low serum vitamin D3 group and 42 healthy controls (high serum vitamin D3 group 2. 39 vitamin D and 39 placebo |
Intraocular pressure in the 87 participants with low serum 25(OH)D levels (mean 40.1 ± 12.9 nm) did not differ from IOP in the 42 participants with high serum 25(OH)D levels (mean 85.1 ± 14.0 nm) (15.9 ± 3.3 mmHg versus 15.6 ± 3.1 mmHg, p = 0.56, independent t-test). No associations between serum 25(OH)D3 levels and IOP, and administration of vitamin D3 to participants with low levels of 25(OH)D3 did not affect IOP. | 9/9 * (RoB) |
| Tae Keun Yoo [107] | 2014 | South Korea | Cross-sectional | 290 POAG, 410 Glaucoma suspects and 5394 healthy controls | A reverse J-shaped association between 25(OH)D3 levels and the risk of OAG, with significantly elevated risk at lower 25(OH)D3. | 4a |
| Aurélien Goncalves [110] | 2015 | France | Case-control | 99 Severe POAG, 51 moderate POAG, and 164 healthy controls | Decreased serum 25OHD concentration was associated with POAG. There was no 25OHD difference between moderate and severe POAG. | 4a |
| Hyun Tae Kim [108] | 2016 | South Korea | Retrospective cross-sectional study | 1627 Glaucoma and 12,1704 healthy controls | In the multivariable-adjusted logistic analysis, the odds ratio of glaucoma in the fourth quintile was significantly lower than that of the first quintile in females (odds ratio, 0.713; 95% confidence interval, 0.520 to 0.979). Lower 25(OH)D level was significantly associated with an elevated risk of glaucoma in females compared with higher 25(OH)D level. | 4a |
| Yingjuan Lv [109] | 2016 | China | Hospital-based and case-control study | 71 POAG and healthy controls | The serum levels of 1 a, 25-Dihydroxyvitamin D3 in age-matched controls was significantly higher than the levels in POAG patients. (p < 0.001). Vitamin D deficiency and the presence of the BsmI ‘B’ allele and the TaqI ‘t’ allele are relevant risk factors in the development of glaucoma. | 2a |
| Željka Vuković Arar [111] | 2016 | Croatia | Case-control | 20 POAG and 20 healthy controls | Serum vitamin D level was statistically significantly lower in glaucoma patients as compared with control group. No statistically significant difference in the IOP values between glaucoma patients and control subjects. | 2a |
| Radha Ayyagari [112] | 2019 | United States | Case-control | 357 POAG and 178 healthy controls | Patients with advanced glaucoma had lower serum levels of vitamin D compared with early glaucoma and normal subjects.The mean (95% confidence interval [C]) levels of vitamin D of the subjects in the control (8.02 ± 6.19 pg/mL) and early phenotype (7.56 ± 5.74 pg/mL) groups were significantly or marginally significantly different from the levels observed in subjects with the advanced phenotype (6.35 ± 4.76 pg/mL; p = 0.0117 and 0.0543, respectively). | 2a |
| Seyhan Dikci [115] | 2019 | Turkey | Prospective, cross-sectional study | 31 PEX glaucoma, 34 PEX syndrome and 43 healthy controls | No statistically significant difference between the PEX syndrome/glaucoma, and control group in terms of serum vitamin D levels, serum vitamin D levels were lower in PEX syndrome and glaucoma group than control group. | 3b |
| K.Atalay [114] | 2019 | Turkey | Prospective, cross-sectional study | 29 XFG, 77 POAG and 33 healthy control | Mean vitamin D levels show a significant difference between the control group and POAG (p = 0.015) | 3a |
| Yongwun Cho [119] | 2021 | South Korea | Case-control | 25 OAG and 90 health controls | Patients with OAG had significantly lower 25(OH)D concentrations in aqueous humor than control patients | 4a |
| Timur Ekiz [113] | 2016 | United States | Case-control | 23 PEX glaucoma and 46 healthy controls | Although patients with ocular pseudoexfoliation have low bone mineral density and 25(OH)D, bone mineral density and 25(OH)D do not appear to be linked to ocular pseudoexfoliation syndrome in our study population. | 2b |
| Tolga Kocaturk [120] | 2019 | Turkey | Cross-sectional | 120 subjects | The IOPg values were higher in cases of vitamin D deficiency. Corneal biomechanical differences in patients with lack of vitamin D were not statistically significant. | 3b |
* The Effective Practice and Organisation of Care (EPOC) RoB Tool for randomized trials; # LEGEND for case-control, cohort, and cross-sectional studies, rating of the studies follow the guidelines from LEGEND.
High intraocular pressure (IOP) is an important risk factor for glaucoma. In an animal study on non-human primates, vitamin D treatment modulated the expression of IOP–regulating genes, with IOP falling in a dose-dependent manner [121]. However, a human study found no association between serum 25(OH)D3 levels and IOP, nor significant changes in participants’ IOP levels after receiving 6 months of oral vitamin D supplements (20,000 IU twice weekly) compared to the placebo group [118]. This contradiction may be due to the oral intake of vitamin D, which may lower the availability of vitamin D in the eye. Patients with glaucoma were found to have lower 25(OH)D concentrations in aqueous humor [119], and the IOP values were higher in cases of vitamin D deficiency [120]. Further studies are required to determine if vitamin D can be a potential intervention for glaucoma, especially through testing different supplement approaches.
Some studies have identified vitamin D as an independent risk factor for glaucoma; however, the role that vitamin D plays in relation to glaucoma remains uncertain. Apart from the elevated IOP pathway, vitamin D may participate in the oxidative stress pathway due to its anti-oxidation and anti-inflammatory abilities. In an in vivo study, 1,25(OH)2D3 ameliorated the effects of oxidative stress from hydrogen peroxide-induced toxicity in human RPE cells through antioxidant signaling pathways, leading to lower levels of reactive oxygen species (ROS), cytokines, and vascular endothelial growth factor (VEGF) [122]. Another study demonstrated that vitamin D significantly altered the inflammatory-related genes in glaucoma, suppressing the expression of the angiotensin I–converting enzyme (ACE), carbonic anhydrase (CA), and Ras homologue gene family member A (RhoA), while significantly increasing the expression of the cytokine A20 precursor (CCL20) in the small intestines of rats [123]. ACE inhibitors are neuroprotective for cultured retinal neurons and can lower IOP in humans [124,125], while CA inhibitors can lower IOP and increase blood flow in the retinal vasculature and optic nerve [126]. The suppression of RhoA through subsequent vitamin D treatment can reduce aqueous outflow resistance and enhance fluid outflow [127,128]. Lastly, CCL2, an intraocular pressure responsive cytokine, possesses a potential role in intraocular pressure regulation [129].
In summary, all reported studies are cross-sectional studies (case-control studies and population surveys) and suggested the protective associations of vitamin D on glaucoma. Future studies should employ randomized clinical trial designs to investigate the causal relationship between glaucoma and low vitamin D levels or calcitriol deficiency.
3.5. Diabetic Retinopathy
Because of its ability to inhibit neovascularization, vitamin D has been studied in the development of diabetic retinopathy (DR). Many observational studies have examined the relationship between vitamin D levels and the prevalence or severity of DR, with most identifying an inverse association with both type 1 and 2 diabetes [130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165]. However, a Chinese study has reported a lack of association between vitamin D deficiency and DR after adjusting for all potential covariates, such as demographics, physical measurements, laboratory measurements, related complications, comorbidities, and medications [166]. Another Indian study suggested a possible association of vitamin D deficiency with type 2 diabetes, but not specifically with DR [167]. As demonstrated in Table 4, in general, some of the studies reported an inverse correlation between the serum vitamin D and severity of retinopathy [130,132,133,134,135,136,137,138,139,152,157,168,169]; similar findings were also reported, for example, the co-existence of low vitamin D and microvascular complications [131] or the association between the severity of DR and the prevalence of vitamin D deficiency [133,161,165] (Table 4); while some studies reported either no association or no significant difference between DR patients and healthy controls [170,171,172,173]. The agreement of the association between vitamin D deficiency and neuropathy is lower when compared with retinopathy. While some studies report that the risk for having diabetic neuropathy is higher in those with vitamin D deficiency [134,137], there is limited research on contrasting findings [174]. Further investigations are warranted.
Table 4.
Summary of studies related to diabetic retinopathy included.
| First Author | Years | Country | Study-Design | Sample Size | Main Finding | Rate # |
|---|---|---|---|---|---|---|
| HülyaAksoy [130] | 2000 | Turkey | Cross-sectional study | 20 DM without DR patients, 15 DM with BDR patients, 14 pre-DM with PDR patients, 17 DM with PDR patients and 20 healthy controls | There was an inverse relationship between the severity of the retinopathy, neovascularization, and serum 1,25(OH)2D3 concentrations, being the lowest in PDR and the highest in diabetic patients without retinopathy patients. Mean 1,25(OH)2D3 concentrations fell with increasing severity of diabetic retinopathy. Only mean 1,25(OH)2D3 concentrations were not significantly different between NDR and BDR, pre-PDR and PDR (p > 0.05). Mean 1,25(OH)2D3 concentrations were significantly different among the other groups (p < 0.05). | 3a |
| Atsushi Suzuki [131] | 2006 | Japan | Descriptive study | 581 T2DM patients and 51 healthy controls | Serum concentration of 25(OH)D3 were associated with HbAlc (p = 0.013). Microvascular complications and insulin treatment in T2DM patients are associated with the co-existence of hypovitaminosis D although serum creatinine levels were below 2.0 mg/dl. | 4a |
| Harleen Kaur [132] | 2011 | Australia | Cross-sectional study | 517 T1DM patients | Vitamin D deficiency is associated with an increased prevalence of retinopathy in young people with T1DM. In logistic regression, retinopathy was associated with VDD (odds ratio 2.12 [95% CI 1.03–4.33]), diabetes duration (1.13, 1.05–1.23), and HbA1c (1.24, 1.02–1.50). | 4a |
| Christel Joergensen [175] | 2011 | Denmark | Prospective observational study | 227 T1DM patients | In patients with type 1 diabetes, severe vitamin D deficiency independently predicts all-cause mortality (unadjusted HR 2.0 [0.9–4.4], p = 0.1 and HR 2.7 [1.1–6.7], p = 0.03, respectively) but not development of microvascular complications in the eye (HR 1.1 [0.7–1.7], p = 0.8) and kidney (unadjusted HR 1.1 [0.5–2.4], p = 0.8 and HR 1.3 [0.3–5.4], p = 0.7, respectively). | 3a |
| Patricia A. Patrick [133] | 2012 | United States | Cross-sectional study | 1790 subjects | There is an association between severity of diabetic retinopathy and prevalence of vitamin D deficiency (β = 1.3, p = 0.01, unadjusted; and β = 1.2, p = 0.01, adjusted for age and obesity status given their clinical significance). However, regression analysis of these data did not demonstrate a statistically significant relationship between the 2 variables (β = −0.04, p = 0.07, unadjusted; and β = −0.03, p = 0.13, adjusted). The findings were inconclusive about the existence of a relationship between retinopathy severity and serum 25(OH)D3 concentration. | 3a |
| John F Payne [176] | 2012 | Georgia | Cross-sectional study | 221 subjects (17 No diabetes or ocular diseases; 51 No diabetes with ocular disease; 41 No BDR; 40 NPDR; 42 PDR) | Patients with diabetes had lower 25(OH)D levels than did those without diabetes (22.9 ng/mL versus 30.3 ng/mL, respectively; p < 0.001). Patients with diabetes, especially those with PDR, have lower 25(OH)D levels than those without diabetes. The mean 25(OH)D levels, stratified by group, were as follows: no diabetes or ocular disease = 31.9 ng/mL; no diabetes with ocular disease = 28.8 ng/mL; no background diabetic retinopathy = 24.3 ng/mL; nonproliferative diabetic retinopathy = 23.6 ng/mL; and PDR = 21.1 ng/mL | 3a |
| Rania NAM Reheem [168] | 2013 | Egypt | Cross-sectional study | 200 DM patients with suspected DR (43 T1DM; 157 T2DM) | Low levels of vitamin D might be a risk marker of development or progression of diabetic retinopathy. Mean serum concentration of 1, 25 dihydroxy vitamin D 3 (1,25(OH)2D3) was significantly lower in diabetic patients with retinopathy than those with no retinopathy (NR) (51.4 ± 16.64 vs. 70.7 ± 15.56 pmol/L, p < 0.001). There was a significant negative correlation between the mean level of 1, 25(OH)2D3 and the degree of severity of retinopathy (p < 0.001). It might be advisable that detailed ophthalmologic examination is needed for diabetics whose serum 1, 25(OH)2D3 concentrations gradually decreased. The measurement of serum 1, 25(OH)2D3 concentrations could become a useful biochemical means to predict the severity of DR in patients with diabetes mellitus | 3a |
| Hala Ahmadieh [134] | 2013 | Lebanon | Cross-sectional study | 136 T2DM and 74 controls | Low serum 25(OH)D3 level was an independent predictor for diabetic neuropathy (OR 4.5 [95% CI 1.6–12]) and diabetic retinopathy (OR 2.8 [95% CI 2.1–8.0]) in patients with T2DM for vitamin D < 20 versus vitamin D ≥ 20 ng/mL after adjustment for HbA1c, age, smoking, BMI and disease duration. | 4a |
| Myra Poon [177] | 2013 | Australia | Cross-sectional study | 481 DM | VDD was associated with a two-fold increased risk of DR. VDD is not associated with changes in retinal vascular geometric measures, suggesting an earlier role in the time course of DR pathogenesis. | 4a |
| Jimmy D. Alele [170] | 2013 | United States | Cross-sectional study | 936 T2DM patients | Vitamin D status had no significant impact on the incidence of vascular events in a cohort of high-risk veterans with diabetes. No differences in the odds associated with retinopathy or renal disease onset or progression in the lowest versus highest vitamin D quartile were observed. | 4b |
| NaokiShimo [135] | 2014 | Japan | Cross-sectional study | 75 T1DM patients (21 with VDD; 54 without VDD) | Vitamin D deficiency was significantly associated with retinopathy in young Japanese T1DM patients. In a multivariate regression analysis, duration of diabetes (adjusted OR; 1.14, 95% CI; 1.02–1.27, p = 0.02) and VDD (adjusted OR; 3.45, 95% CI; 1.11–10.6, p = 0.03) were independent determinants of DR. | 4a |
| R He [136] | 2014 | China | Cross-sectional study | 625 T2DM with no DR patients, 562 T2DM with non-sight-threatening DR patients and 333 T2DM with sight-threatening DR patients | Vitamin D deficiency is an independent risk factor for diabetic retinopathy (OR 1.93) and sight-threatening diabetic retinopathy (OR 2.42) (both p < 0.01). The prevalence of sight-threatening diabetic retinopathy doubles when the serum 25(OH)D3 level is <15.57 ng/mL (odds ratio 2.38, p < 0.01). | 4a |
| Sarita Bajaj [137] | 2014 | India | Observational caase-control study | 158 T2DM patients and 130 healthy controls | Vitamin D deficiency was found to be significantly associated with neuropathy (χ2 = 5.39, df = 1, p = 0.020), retinopathy (χ2 = 6.6, df = 1, p = 0.010), and nephropathy (χ2 = 10. 52, df = 1, p = 0.001). | 2a |
| Donghyun Jee [169] | 2014 | South Korea | Cross-sectional study | 18,363 subjects | There was an inverse relationships of blood 25-hydroxyvitamin D levels with any DR and proliferative DR but only in men. After adjusting for potential confounders, including age, sex, diabetes duration, hemoglobin A1c levels, and hypertension, the odds ratios (OR) for any DR and proliferative DR among men decreased significantly in the highest blood 25-hydroxyvitamin D level quintile relative to the lowest quintile (OR, 0.37; 95% confidence interval [CI], 0.18–0.76; p for trend =0.004 and OR, 0.15; 95% CI, 0.03–0.83; p for trend = 0.043). | 4a |
| Giacomo Zoppini [138] | 2015 | Italy | Cross-sectional study | 715 T2DM patients | There is an inverse and independent relationship between circulating 25(OH)D3 levels and the prevalence of microvascular complications in patients with T2DM. Serum 25(OH)D levels decreased significantly in relation to the severity of either retinopathy or nephropathy or both. In multivariate logistic regression analysis, lower 25(OH)D levels were independently associated with the presence of microvascular complications (considered as a composite end point; OR 0.758; 95% CI 0.607 to 0.947, p = 0.015). | 4a |
| Markus Herrmann [139] | 2015 | Australia, New Zealand, and Finland | Multinational, double-blind, placebo-controlled trial | 9795 T2DM patients | Low blood 25(OH)D3 concentrations are associated with an increased risk of macrovascular and microvascular disease events in T2DM. A 50 nmol/L difference in blood 25OH-D concentration was associated with a 23% (p = 0.007) change in risk of macrovascular complications. | 4a |
| G Bhanuprakash Reddy [167] | 2015 | India | Cross-sectional case-control study | 82 T2DM with DR patients and 99 healthy controls | There is a possible association between vitamin D deficiency and type 2 diabetes, but not specifically with retinopathy. | 3a |
| Celil Alper Usluogullari [140] | 2015 | Turkey | Cross-sectional study | 557 T2DM patients (299 DPN, 223 DN and 235 DR) and 112 healthy controls | Vitamin D deficiency is associated with microvascular complications in DM patients. After adjustment, the 25 (OH) D level was confirmed to be an independent protective factor for DPN (odds ratio [OR]: 0.968, p = 0.004]) and DN (OR: 0.962, p = 0.006). The prevalence of DPN and DN increased significantly as the serum 25 (OH) D levels decreased. | 4a |
| Nuria Alcubierre [154] | 2015 | Spain | Case-Control study | 139 DR patients and 144 NDR patients | Patients with more advanced stages of retinopathy (grades 2–4) had lower concentrations of 25(OH)D and were more frequently vitamin D deficient as compared with patients not carrying this eye complication. The multivariate analyses showed that there was a significant association of retinopathy and 25(OH)D, even when considering other variables associated with this variable which were consistent when analyzing both the concentrations of 25(OH)D and the presence of vitamin D deficiency, as defined by a 25(OH)D <15 ng/mL (values 0.04 and 0.009, respectively.) | 2a |
| Shokoufeh Bonakdaran [174] | 2015 | Iran | Cross-sectional study | 235 T2DM patients (153 NDR, 64 NPDR and 18 PDR) | This study did not find any association between diabetic retinopathy and its severity and vitamin D insufficiency. Vitamin D insufficiency is not related to risk factors of diabetic retinopathy. 25(OH)D level was not significant different between NDR, NPDR and PDR groups. Correlation between 25 (OH) D level and other known risk factors of diabetic retinopathy was not significant. | 3b |
| Lian Engelen [155] | 2015 | 16 European countries | Prospective cohort study | 532 T1DM patients | In individuals with type 1 diabetes, both higher 25(OH)D2 and 25(OH)D3 are associated with a lower prevalence of macroalbuminuria, but not of retinopathy and CVD. | 3b |
| Adem Gungor [156] | 2015 | Turkey | Prospective study | 50 VDD with DR patients and 50 VDD without DR patients | The results indicate that vitamin D functions as a neuroprotective component for optic nerves. Low serum 25(OH)D concentrations contribute to RNLF thinning in early-stage DR patients with VDD. The mean RNFL thickness of group 1 was significantly reduced compared to that of group 2 (p < 0.001). A significant relationship between the mean RNFL thickness and serum 25(OH)D concentrations was observed in group 1 (p < 0.001). | 3a |
| Amy E Millen [178] | 2016 | United States | Population-based prospective study | 1305 DM patients | 25(OH)D3 concentrations ≥75 nmol/L were associated with lower odds of any retinopathy assessed 3 years later. ORs (95 % CIs) for retinopathy, adjusted for race and duration, were 0.77 (0.45–1.32), 0.64 (0.37–1.10), and 0.39 (0.20–0.75), p for trend = 0.001, for participants with 25(OH)D of 30–<50, 50–<75, and ≥75 nmol/L, respectively. Further adjustment for hypertension minimally influenced results (data not show), but adjustment for HBA1c attenuated the OR among those with 25(OH)D ≥75 (0.47 [0.23–0.96], p for trend = 0.030). | 3a |
| Uazman Alam [171] | 2016 | UK | Prospective observational follow-up study | 657 DM patients (257 NDR, 243 BDR, 135 PPDR and 22 PDR) | This study has found no association between serum 25(OH)D and the presence and severity of diabetic retinopathy or maculopathy. There was no correlation of DR with 25(OH)D (OR 1.00 (95% CI 0.98–1.02), = NS), gender, or ethnicity. | 3b |
| Chan-Hee Jung [179] | 2016 | South Korea | Cross-sectional study | 257 T2DM patients (men: 21 deficient, 60 insufficient and 30 sufficient; women: 63 deficient, 72 insufficient and 11 sufficient) | Serum 25(OH)D level < 10 ng/mL is independently associated with increased DPN in male patients and increased DN in female patients with T2DM. For men, the prevalence of DPN was significantly higher in vitamin D deficient patients than those with insufficient or sufficient vitamin D (38%, 11.7%, and 10%, respectively; p = 0.005). The prevalence of DR and DN was not different according to the vitamin status. For women, the prevalence of DN was significantly higher in patients with vitamin D deficiency than in the other 2 vitamin D status (40%, 20.6%, and 0%, for vitamin D-deficient, vitamin D-insufficient, and vitamin D-sufficient groups, respectively; p = 0.007) and the prevalence of DPN and DR was not different among 3 status. | 4a |
| Xianglong Yi [180] | 2016 | China | Case-control study | 22 PDR patients, 29 NPDR patients and 24 healthy controls | There is a potential protective effect of 1,25(OH)2 D3 in DR, whereas supplementation with 1,25(OH)2 D3 might be an effective strategy for preventing the development of DR | 2a |
| M Long [141] | 2017 | United States | Retrospective cross-sectional study | 842 DR patients, 301 mild NPR patients, 195 severe NPR patients and 106 PDR | Vitamin D deficiency associated with severe DR in patients with well controlled glycasemia. After adjusting gender, ethnicity and duration of diabetes, the interaction of HbA1 with vitamin D deficiency significantly affected retinopathy severity (p = 0.029). | 4b |
| Banu Boyuk [157] | 2017 | Turkey | Cross-sectional case-control study | 206 T2DM patients and 34 healthy controls | There is an inverse relationship between the circulating 25(OH) D level and the prevalence of retinopathy and neuropathy in T2DM patients. The level of serum 25-hydroxyvitamin D (25(OH) D) was significantly lower in the T2DM patients (11.16 ± 3.99 ng/mL vs. 15.58 ± 3.16 ng/mL; p < 0.05). Serum 25(OH) D levels weresignificantly lower in the presence of retinopathy and neuropathy (p < 0.05 for both), but no significant association between Vitamin D level and microalbuminuria was found. | 3b |
| Anurag Chaurasia [158] | 2017 | India | Case-control study | 120 DM patients (40 No BDR, 42 mild-mod NPDR and 38 sev–v.serv NPDR and PDR) and 100 NDM patients (58 no DM and ocular diseases and 42 no DM with ocular diseases) | Diabetic subjects, especially those with NPDR (severe and very severe grade) and PDR have lower Vitamin D levels than those without diabetes. Subjects with vitamin D insufficiency are at risk of having retinopathy 9.75 times that of vitamin D sufficient subjects (Odds Ratio 9.75; 95% C.I. 1.96 to 48.46). The mean vitamin D level in Diabetics (20.7 ± 6.91 ng/mL) is significantly less than that in non-diabetics (27.51 ± 5.53 ng/mL) (p < 0.0001). Also, diabetics have significantly higher proportion of subjects with vitamin D insufficiency (91.3%) as compared to Non-Diabetics (68%). | 4a |
| Beteal Ashinne [142] | 2018 | India | Retrospective study | 3054 T2DM patients | Lower serum 25(OH)D3 was associated with increased severity of DR and the presence of vitamin D deficiency was associated with a two-fold increased risk for PDR. A statistically significant difference in the serum vitamin D means of these categorizations: no DR (13.7 ± 2.1 ng/mL), non-sight threatening DR (12.8 ± 2.1 ng/mL), sight threatening DR (11.1 ± 2.2 ng/mL), (p < 0.001). | 4a |
| Abdulbari Bener [143] | 2018 | Turkey | Cross-sectional study | 638 DM patients | Vitamin D deficiency is considered as a risk factor for DR and hearing loss among diabetic patients. | |
| Krishnamoorthy Ezhilarasi [181] | 2018 | India | Case-control study | 200 T2DM patients, 216 T2DM with microvascular complications, 198 T2DM with macrovascular complications and 252 controls with nomal glucose tolerance | VDR (rs1544410) SNP was found to be associated with decreased serum (25[OH]D) levels in both micro-macrovascular complications of T2DM among South Indian Population. | 4a |
| Josef Richter [159] | 2018 | Czech Republic | Clinic Controlled Trial | 52 DR patients (Vitamin D and Beta-glucan supplement, Vitamin D and placebo supplement and vitamin D supplement only) | Significant vitamin D deficits were found in all cases, even after three months of supplementation with vitamin D. | 7/9 * (RoB) |
| Martina Závorková [182] | 2018 | Czech Republic | Clinic Controlled Trial | 54 DR patients (beta-glucan and vitamin D supplement, vitamin D and placebo supplement, vitamin D supplement only, no supplementation | Glucan and vitamin D supplementation strongly influence lipid metabolism and have positive effects on human health. | 7/9 * (RoB) |
| Gauhar Nadri [144] | 2019 | India | Cross-sectional study | 24 DM without DR patients, 24 DM with NPDR patients and 24 DM with PDR patients | Serum vitamin D levels of ≤ 18.6 ng/mL serve as sensitive and specific indicator for proliferative disease, among patients of DR. Univariate ordinal logistic regression analysis found vitamin D as a significant predictor of severity of diabetic retinopathy {OR (95% CI) = 1.11 (1.06–1.16) (p < 0.01 or p < 0.001)}. ROC curve analysis demonstrated vitamin D cut off value of 18.6 ng/mL to be significantly associated with NPDR and PDR | 4a |
| Jing Yuan [145] | 2019 | China | Cross-sectional study | 889 T2DM patients | Vitamin D deficiency is significantly associated with risk of PDR. The odd ratio in VDD individuals was significantly increased (1.84, 95% CI 1.18–2.86) for DR, 1.60 (95% CI 1.06–2.42) for PDR, compared with those in vitamin D sufficient individuals, adjusted by age, sex, blood pressure, kidney function, diabetic duration, and HbA1c. | 4a |
| Heng Wan [146] | 2019 | China | Cross-sectional study | 4767 DM patients | Lower serum 25(OH)D3 concentration is significantly associated with higher prevalence of DR in middle-aged and elderly diabetic adults. Compared with the first 25(OH)D quartile (relatively lower concentraion), participants in the fourth quartile (relatively higher concentration) had a lower prevalence of high ACR (OR 0.77, 95% CI 0.61, 0.96) (p for trend <0.01). For DR, the OR of DR for the fourth 25(OH)D quartile when compared with the first quartile was 0.62 (95% CI: 0.47, 0.82; p for trend <0.01). | 4a |
| Abdulhalim Senyigit [160] | 2019 | Turkey | Cross-sectional study | 163 T2DM patients and 40 controls | Low serum 25-OHD levels were found to be associated with the development of diabetes and complications. Serum 25(OH)D levels in all patients were significantly lower than the control group (p < 0.05). Levels of 25(OH)D for those with complications were lower than that without complications. (p values for nephropahty and retinopathy groups were <0.001 while that for neuropahty was <0.01). Low serum 25-OHD levels may be a consequence of even worse metabolic control of diabetes. | 3a |
| Abdulla Almoosa [161] | 2019 | Bahrain | Prospective observational study | 300 T2DM patients (150 NDR, 99 NPDR and 51 PDR) | VDD was commonly found in type II DM patients. Lower serum 25(OH)D levels were associated with more severe DR. | 3b |
| Mehrdad Afarid [148] | 2020 | Iran | Cross-sectional study | 21 DM with NPR patients, 9 DM with PDR patients and 30 DM with no DR patients | Patients with DR had lower levels of serum vitamin D compared with those without retinopathy, especially those with severe NPDR and PDR | 3a |
| Amy E. Millen [178] | 2020 | Portugal | Retrospective observational study | 182 T1DM patients | Lower levels of vitamin D were associated with an increased prevalence of diabetic retinopathy in patients with T1DM, after adjusting for possible confounders. The lower circulating 25(OH)D levels were significantly associated with greater prevalence of DR after adjusting for confounders (OR = 0.94; 95% CI 0.90–0.99, p = 0.023). | 4a |
| Lina H. M. Ahmed [150] | 2020 | Qatar | Case-control study | 274 T2DM patients and 222 healthy controls | Vitamin D3 was associated with diabetic retinopathy whilst vitamin D2 was not. | 2a |
| Lina H. M. Ahmed [162] | 2021 | Qatar | Cross-sectional study | 460 T2DM patients and 290 healthy controls | Vitamin D3 metabolites were associated with diabetic retinopathy, whereas total vitamin D levels were not, suggesting that endogenous vitamin D(3) metabolites are a better measure of diabetic microvascular complications. The lower 1,25(OH)2D3 levels were associated with diabetic retinopathy (p = 0.006) hypertension and dyslipidemia (both p = 0.01) and CAD (p = 0.012); while no association between either total 1,25(OH)2D or 1,25(OH)2D3 levels with diabetic neuropathy, PAD or CAD. | 3a |
| Alexandra E. Butler [147] | 2020 | Qatar | Cross-sectional study | 460 T2DM patients and 290 healthy controls | Lower 25(OH)D(3) was associated with retinopathy (p < 0.03) and dyslipidemia (p < 0.04), but not neuropathy or vascular complications | 3a |
| Ying Xiao [166] | 2020 | China | Cross-sectional study | 4284 T2DM patients | In unadjusted analyses, DR was associated with VDD status (PR: 1.147; 95% CI: 1.025–1.283), the associate retained after adjusted with age and sex and other demographic and physical measurements. However, the significance diminished after adjusting all confounders (PR: 1.093; 95% CI: 0.983–1.215). | 4a |
| Gauhar Nadri [163] | 2021 | India | Cross-sectional study | 66 T2DM patients (22 No DR, 22 NPDR and 22 PDR) and 22 controls | Low serum vitamin D levels correlate with increased severity of DR. | 4a |
| Li Lu [151] | 2021 | China | Retrospective study | 55 PDR patients, 25 non-diabetic patients with idiopathic macular hole patients and 10 NDR patients | In ROC-curve analyses, both serum and vitreous 25(OH)D showed discriminatory ability in predicting DR (NPDR and PDR) and PDR. In DR prediction, they obtained the same area under curve (AUC) of 0.77. Serum 25 (OH) D has a better predictive value (AUC: 0.77) than serum 25 (OH) D (AUC: 0.66) in PDR prediction. | 4a |
| Wei-Jing Zhao [152] | 2021 | China | Cross-sectional study | 815 T2DM patients | Vitamin D deficiency is independently associated with higher risk of diabetic peripheral neuropathy and DR, but not diabetic retinopathy, in T2DM patients. Univariate analysis showed that the 25 (OH) D was significantly correlated with DPN (odds ratio [OR]: 0.969, 95% confidence interval [CI]: 0.950–0.989, p = 0.003) and DN (OR: 0.950, 95% CI: 0.928–0.973, p < 0.001), but not with DR (OR: 1.014, 95% CI: 0.994–1.034, p = 0.165). Multiple logistic regression analysis after adjustment showed that the 25 (OH) D level was an independent protective factor for DPN and DN. | 4a |
| Xin Zhao [153] | 2021 | China | Retrospective study | 636 T2DM patients (466 NDR, 120 BDR and 50 PDR) | A close association was observed between 25(OH)D3 level and DR in the elderly male patients and postmenopausal women with T2DM. There was a significant difference was observed among the three groups in men and women (men: χ2 = 7:75, p < 0.05; women: χ2 = 7:75, p < 0.05) | 4a |
| Mehmet Balbaba [172] | 2021 | Turkey | Prospective study | 20 T2DM-DR patients, 20 T2DM-NDR patients and 20 healthy controls | Vitamin D levels were similar between diabetic patients with and without DR and healthy control subjects | 3b |
| Saeed Karimi [183] | 2021 | Iran | Prospective comparative case series study | 71 diabetic macular edema patients | In diabetic macular edema patients with vitamin D deficiency, vitamin D supplement therapy had some beneficial effects on central macular thickness reduction following three injections of intravitreal bevacizumab; nevertheless, these effects were not statistically significant | 8/9 * (RoB) |
| Elise Girard [173] | 2021 | French Guiana | Cross-sectional study | 361 DM patients | There was no significant difference between type of diabetes and VD deficiency. There was no significant relation between nephropathy and vitamin D deficiency even after adjustment with confounders. Patients with diabetic retinopathy had significantly greater median vitamin D concentrations than those without retinopathy (respectively, 31 ng/mL (interquartile range (IQR) = 23–34) vs. 26 ng/mL (IQR = 23–32), p = 0.03). | 4a |
| José M. Castillo-Otí [164] | 2021 | Spain | Case-Control study | 385 T2DM patients (30 with DR, 335 without DR) | Levels of 25(OH)D and treatment of diabetes were significantly associated with DR after adjusting for other risk factors. Patients with both 25(OH)D and 1,25(OH)2D less than or equal to 16 ng/mL and 29 pg/mL respectively had a greated risk of DR (OR 5.21, 95% CI: 1.76, 15.42; p = 0.003). | 4a |
| Martina Tomić [165] | 2021 | Croatia | Cross-sectional study | 94 T2DM patients (69 without DR and 25 with NPDR) | Hypovitaminosis D is often in T2DM, especially in those with proliferative DR. | 3b |
Diabetic retinopathy (DR), background diabetic retinopathy (BDR), non-proliferative retinopathy (NPR), preproliferative diabetic retinopathy (pre-PDR), proliferative diabetic retinopathy (PDR), Diabetes mellitus (DM), Type 1 diabetes mellitus (T1DM), type 2 diabetes mellitus (T2DM), diabetic kidney disease (DKD); * The Effective Practice and Organisation of Care (EPOC) RoB Tool for randomized trials; # LEGEND for case-control, cohort, and cross-sectional studies, rating of the studies follow the guidelines from LEGEND.
Besides cross-sectional studies, a population-based prospective study also showed that a high level of vitamin D was associated with a lower risk of DR after 3 years [178]. A double-blind, placebo-controlled trial found that low blood 25(OH)D3 levels were associated with an increased risk of macrovascular and microvascular disease events among type 2 diabetics [139].
DR is a serious microvascular complication of diabetes. The characteristics of early DR include the loss of pericytes from retinal capillaries, the appearance of acellular capillaries and microaneurysms, and the breakdown of the blood-retinal barrier. In the proliferative phase of DR, neovascularization in the retina may occur, which significantly increases the probability of vision loss [184,185]. Potential mechanisms that explain how vitamin D can prevent DR include insulin resistance, immune regulation, anti-inflammation, and anti-angiogenesis. Animal studies have shown that vitamin D is important for insulin synthesis and can improve the body’s sensitivity to insulin, reducing the risk of insulin resistance [186,187]. Other studies have found that vitamin D treatment decreased the retinal expression of VEGF and the transforming growth factor TGF-β1 in rats [188], which may have protective effects on the retina. VDR has also been implicated in the pathogenesis of DR [189]. A meta-analysis of seven studies evaluating the association of the VDR gene polymorphisms with DR found that the FokI polymorphism of the VDR gene has a significant association with DR susceptibility [190]. Apart from the VDR polymorphism, other studies have proposed different protective mechanisms of vitamin D on DR, including protecting the vasculature [191,192,193], reducing oxidative stress [194,195], modulating inflammation and immune responses [180,196,197,198], inhibiting the renin-angiotensin aldosterone system [199,200], reducing the effects of advanced glycation end products [201,202], reducing endoplasmic reticulum stress [203,204], regulating endothelial cells apoptosis [205], and regulating diabetic leukostasis [206]. Further studies are needed to determine the exact mechanisms of vitamin D on DR.
In summary, even though there are no consistent associations between vitamin D level and DR in observational studies, more than 30 reports suggested an inverse relationship. The same conclusion is made in perspective studies, although the causal relationship has not been identified. Further studies should investigate whether vitamin D supplementation can reduce the risk of DR.
3.6. Dry Eye Syndrome
Dry eye syndrome (DES), or dry eye disease [207], is a common eye disease affecting about 12% of the world’s population; prevalence was lowest in North America (4.6%) and highest in Africa (47.9%) [208]. Many factors are related to DES, including hormonal alterations, environmental changes, and aging [209]. DES is accompanied by the inflammation of the ocular surface, which may cause visual disturbances, tear film instability, and potential damage [210]. Whereas an increasing number of studies have shown that a relationship exists between vitamin D and DES, their findings remained controversial. Some cross-sectional studies suggested an inverse correlation between vitamin D levels and ocular surface disease index (OSDI) scores or DES incidence [211,212,213,214,215,216,217,218,219,220,221,222,223,224,225,226], while three others have not reached a significant conclusion [227,228,229,230], as demonstrated in Table 5.
Table 5.
Summary of studies related to dry eye syndrome included.
| First Author | Years | Country | Study-Design | Sample Size | Main Finding | Rate # |
|---|---|---|---|---|---|---|
| B Bang [211] | 1999 | Denmark | Case-control study | 41 Primary SS patients and 596 healthy controls | Vitamin D metabolism may be involved in the pathogenesis of primary SS. | 7/9 * (RoB) |
| Anat Galor [212] | 2014 | United States | Cross-sectional study | 247 subjects | Higher vitamin D levels had a favorable but small effect on DES symptoms. Higher vitamin D levels were significantly associated with lower DES symptoms (−1.24 decrease for every 10-U increase in vitamin D, p = 0.01). | 2b |
| B E Kurtul [213] | 2015 | Turkey | Case-control study | 34 Vitamin D deficiency patients and 21 healthy controls | Vitamin D deficiency decreases the TBUT and Schirmer test values and may be associated with dry-eye symptoms in non-SS. The TBUT scores and Schirmer-1 test values of study group were significantly lower than that of the control group (p = 0.01 and 0.007, respectively). | 3a |
| Pelin Yildirim [214] | 2015 | Turkey | Case-control study | 50 Premenopausal women with vitamin D deficiency and 48 healthy controls | Dry eye and impaired tear function in patients with vitamin D deficiency may indicate a protective role of vitamin D in the development of dry eye. There were significant differences between the vitamin D deficiency group and control group for the frequencies of the patients with dry eye (p-value for the results of Schirmer’s test, TBUT and OSDI were 0.001, 0.001 and 0.003 respectively). | 3a |
| Donghyun Jee [227] | 2016 | South Korea | Cross-sectional study | 1679 DES patients and 14,717 No DES patients | The present study does not support an association between serum 25-hydroxyvitamin D levels and DES. | 2a |
| Ki Won Jin [215] | 2016 | South Korea | Retrospective observational study | 79 DES patients | TBUT and secretion were correlated with serum vitamin D levels. Tear break-up time (TBUT) and tear secretion were shorter in the vitamin D-deficient group compared to the sufficient group (p = 0.022 and p = 0.004). Vitamin D status may be an important factor for dry eye syndrome. | 4a |
| Sam Young Yoon [216] | 2016 | South Korea | Cross-sectional study | 1822 DES patients and 15,720 healthy controls | Low serum 25(OH)D3 levels and inadequate sunlight exposure are associated with DES in Korean adults. Inadequate sunlight exposure time (odds ratio [OR], 1.554; 95% confidence interval [CI], 1.307–1.848), low serum 25(OH)D level (OR, 1.158; 95% CI, 1.026–1.308) and indoor occupation (OR, 1.578; 95% CI, 1.389–1.814) were the risk factors for DES. Sufficient sunlight exposure or vitamin D supplementation may be useful in DES treatment. | 8/9 * (RoB) |
| Rohit Shetty [217] | 2016 | India | Cross-sectional study | 52 evaporative dry eye patients and 43 healthy controls | In the evaporative dry eye cohort, there were strong inverse correlation between the vitamin D levels and OSDI scores (total and discomfort- and vision-related subscales) but not total corneal DC density, DCs without dendritic process, or subbasal nerve plexus features. | 2b |
| Rohit Shetty [218] | 2016 | India | Cross-sectional study | 19 Mild dry eye signs with exaggerated symptoms patients and 19 healthy controls | Decreased serum vitamin D was associated with exaggerated symptoms in dry eye patients with mild dry eye signs. An inverse correlation (r = −0.569; p = 0.0110) was observed between serum vitamin D levels and OSDI score in the patient cohort. Tukey’s multiple comparisons test showed a significant difference between the OSDI score of patients with serum vitamin D less than or equal to 10 ng/mL and greater than 20 ng/mL. | 7/9 * (RoB) |
| Seok Hyun Bae [219] | 2016 | South Korea | Retrospective observational study | 105 DES refractory to conventional treatment and vitamin D deficiency patients | Vitamin D supplementation is effective and useful in the treatment of patients with DES refractory to conventional treatment and with vitamin D deficiency. The TBUT in males was increased after 2 weeks compared to pre–treatment and in female it was increased after 2 and 6 weeks compared to pre-treatment (p = 0.041, <0.001 and <0.001, respectively, paired t-test). OSDI score in men was lower at 6 weeks compared to pre-treatment and in women it was lower at 10 weeks compared to pre-treatment (p = 0.033 and 0.012, respectively, paired t-test). | 3a |
| Min Ji Kim [228] | 2017 | South Korea | Cross-sectional study | 1428 DES patients and 7921 healthy controls | Severe vitamin D deficiency was associated with dry eye in an unadjusted model (p = 0.01), but the association was not statistically significant after adjustment (p = 0.49, Vit D insufficiency; p = 0.33, VDD; p = 0.18, sever VDD). OR was 1.24 (95% CI, 0.66 to 2.41) for vitamin D insufficiency, 1.30 (95% CI, 0.75 to 2.25) for vitamin D deficiency, and 1.42 (95% CI, 0.83 to 2.41) for severe vitamin D deficiency after adjusting confounders. | 4a |
| Da-Hye Jeon [229] | 2017 | South Korea | Cross-sectional study | 393 DES patients and 347 healthy controls | Serum vitamin D levels are not associated with DES after adjusting confounders. Higher serum vitamin D levels were associated with a non-significantly reduced risk of DED in the crude analysis (odds ratio [OR], 0.991; 95% confidence interval [CI], 0.971 to 1.011) and in the adjusted analysis (OR, 0.988; 95% CI, 0.966 to 1.010). | 8/9 * (RoB) |
| Yi-Fang Meng [220] | 2017 | China | Case-control study | 70 DES patients and 70 healthy controls | A significant association between serum 25(OH)D level and DES incidence was detected. In Pearson correlation analysis, serum 25(OH)D level was associated with increased Schimer test I (r = 0.8248, p < 0.001). In addition, there was an inverse correlation between serum 25(OH)D and ODSI scores (r = −0.3348, p = 0.005) and TBUT (r = −0.6806, p < 0.001). | 4a |
| Reiko Arita [231] | 2017 | Japan | Clinical trial | 8 MGD patients and 6 healthy controls | Topical eyelid application of an analog of the active form of vitamin D3 was found to be safe as well as to improve the condition of patients with obstructive meibomian gland dysfunction. | 7/9 * (RoB) |
| Muhammed Kizilgul [232] | 2017 | United States | Clinical trial | 44 DES patients | As a consequence of the presence of VDR and 1α-hydroxylase in different parts of the eye, vitamin D replacement improves tear hyperosmolarity that is considered to be induced by ocular surface inflammation. The change of TFO was negatively correlated with the change of 25(OH)D3 before and after replacement in patients with dry eye disease (r = −0.390, p = 0.049). | 2b |
| Chih-Huang Yang [233] | 2017 | Australia | Case-control study | 29 DES patients and 29 healthy controls | Low vitamin D levels (<50 nmol/l) were associated with dry eye symptoms in older individuals but not those diagnosed with dry eye. Vitamin D supplement increased the vitamin D levels, and improved dry eye symptoms, the tear quality and ocular surface conditions. | 3a |
| Goktug Demirci [221] | 2018 | Turkey | Cross-sectional observational study | 30 Vitamin D deficiency patients and 30 healthy controls | Vitamin D deficiency is associated with tear hyperosmolarity and tear film dysfunction. The Schirmer I test values and TBUT measurements for VDD were significantly lower compared with controls (p < 0.001). Patients with vitamin D deficiency may be prone to dry eye. | 3a |
| Pooja Khamar [222] | 2019 | India | Cross-sectional study | 47 evaporative dry eye patients and 33 healthy controls | Significantly lower vitamin D was observed in DED patients (p < 0.05). These dysregulated tear factors showed significant associations with DED signs and symptoms. | 2a |
| Hwang Jin Sun [234] | 2019 | South Korea | Case-control study | 116 DED patients (52 VDD and 64 non-VDD) | The OSDI score was decreased in the IM group (intramascular supplementation of vitamin D for 2 weeks) after cholecalciferol supplementation compared with pretreatment, whereas that in the none group and oral group was not different between after cholecalciferol supplementation and pretreatment. The effect of topical carbomer-based lipid–containing artificial tears and hyaluronate was dependent on serum 25HD levels. | 4a |
| Jee Hye Lee [223] | 2020 | South Korea | Retrospective study | 74 Primary SS patients | Serum 25(OH)D3 level might be associated with dry eye severity in primary SS. Among dry eye parameters, the corneal staining score, conjunctival staining score, Schirmer I value, and TBUT were statistically worse in the serum 25(OH)D3 deficiency group compared with the normal group (p < 0.05). The conjunctival staining score showed a significant difference between the deficiency group and insufficiency group (p < 0.05). | 8/9 * (RoB) |
| Palak Watts [235] | 2020 | India | Prospective study | 90 DED with deficient serum 25(OH)D3 levels patients | Vitamin D supplementation leads to earlier and significant improvement in TBUT, Schirmer’s, and OSDI score in patients with vitamin D deficient DED. | 2b |
| Seyhan Dikci [226] | 2020 | Turkey | Case-control study | 36 Vitamin D deficiency patients and 27 healthy controls | Vitamin D deficiency may lead to dry eye causing conjunctival squamous metaplasia and loss of goblet cells on the ocular surface. Serum vitamin D levels had moderate negative correlation with CIC results (r = −0.595; p < 0.001), and mild positive correlation with TBUT scores (r = 0.384, p = 0.002). There was no correlation between serum vitamin D levels and Schirmer II test and OSDI scores (r = 0.169, p = 0.185, r = 0.163, p = 0.202, respectively). No correlation was found between age and Schirmer’s II, TBUT, OSDI scores, and CIC results. | 7/9 * (RoB) |
| Emine Esra Karaca [236] | 2020 | Turkey | Clinical controlled trial | 40 Vitamin D deficiency patients | Vitamin D replacement appears to improve ocular surface in individuals with vitamin D deficiency. | 3a |
| Aksoy Aydemir, Gozde [225] | 2021 | Turkey | Prospective cross-sectional study | 90 Pediatric patients with type 1 diabetes mellitus patients and 80 healthy controls | The tear measurements of the pediatric type 1 diabetes mellitus were lower than those in the healthy pediatric control group. The accompanying VDD made this situation more pronounced. The correlations between the vitamin D level and the Schirmer test, OSDI score, CSS, TF–BUT measurements, TMA, and TMH values were examined in T1DM group and control groups. Although there was a significant correlation in all measurements in T1DM group, there was no correlation in control groups. | 4a |
| Shima Fukuoka [224] | 2021 | Japan | Cross-sectional study | 300 subjects | High intake of total fat, SFAs, oleic acid, and vitamin D may be inversely associated with the prevalence of MGD in Japanese individuals. Vitamin D intake in the MGD group was significantly lower than that in the non-MGD group (p = 0.039). Multivariate adjusted odds ratios (95% confidence intervals) between extreme quintiles of intake of vitamin D for MGD prevalence was 0.38 (0.17–0.87). | 8/9 * (RoB) |
| Alireza Eslampoor [237] | 2022 | Iran | RCT | 100 dry eye disease patients with concurrent vitamin D deficiency | Vitamin D supplementation as an adjuvant to routine dry eye treatment improves ocular surface hemostasis parameters, results in better tear stability and a more improved tear osmolarity in patients with vitamin D deficiency. | 4a |
| Jain Nikita [238] | 2022 | India | Hospital-based cross-sectional | 60 VDD patients and 60 normal levels subjects | A significant difference in the mean values of Schirmer I and Schirmer I test (with anesthesia) (p < 0.001) was seen between the case and control groups. A significant difference in the mean values of TFBUT (p < 0.001) and OSDI scores (p < 0.01) was also seen between the two groups. | 7/9 * (RoB) |
Sjögren’s syndrome (SS), Dry eye syndrome (DES), Tear film break-up time (TBUT), Ocular surface disease index (OSDI); * The Effective Practice and Organisation of Care (EPOC) RoB Tool for randomized trials; # LEGEND for case-control, cohort, and cross-sectional studies, rating of the studies follow the guidelines from LEGEND.
Several clinical trials investigated the treatment effects of vitamin D supplementation on DES symptoms, as demonstrated. Some of them only involved DES patients [232,236,237], while four other studies set healthy controls [219,231,233,235]. All these studies concluded that vitamin D can improve the DES symptoms of tear quality and ocular surface conditions. However, these studies may suffer from a small sample size or lack of a placebo-control group. Further well-design clinical trials with more samples are required to better understand the relationship between vitamin D and DES.
The key mechanism of vitamin D on DES may involve its antioxidation, anti-inflammatory, and immune-regulatory effects [239,240,241]. Vitamin D deficiency may cause the inflammation of the ocular surface and ultimately DES [233]. Conversely, vitamin D may relieve DES through inhibiting the interleukin-6 (IL-6) inhibitor [233], the key mediator of localized inflammation [242]. Moreover, vitamin D can suppress the release of inflammatory cytokines and stimulate the release of antioxidant cytokines in tears. Lastly, vitamin D can improve corneal epithelial barrier functions [233], which may improve ocular conditions. Apart from the role of vitamin D in the pathogenesis of DES, a study reported that the expression of VDR and CYP27B1 (vitamin D metabolism enzyme) was significantly decreased in DED patients, suggesting the possible involvement of the vitamin D regulatory enzyme in protecting the human eye from dry eye [243]. A study on SNPs of the VDR gene Apa-1, Bsm-1, Fok-1 and Taq-1, reported the association of Apa-1 and Taq-1 with the risk of DES [244].
In conclusion, the exact mechanisms of vitamin D on DES are unclear, but evidence from cross-sectional studies seems to suggest that vitamin D has a protective effect against DES. Limit evidence from clinical trials also suggests that vitamin D supplementation could help to improve DES symptoms, but a further placebo RCT is needed to verify this treatment effect.
3.7. Thyroid Eye Diseases
Thyroid eye disease (TED), also known as Graves’ ophthalmopathy (GO), is an autoimmune inflammatory disorder. Few studies have examined the relationship between vitamin D and TED (Table 6). A pilot study in Texas, United States found prevalence rates of 20% and 31% for vitamin D deficiency and insufficiency among TED patients, respectively [245]. Another retrospective case-control study comparing vitamin D levels between Graves’ disease patients and TED patients found that low serum vitamin D was associated with TED [246]. Assessing and supplementing vitamin D levels may be an important addition to the early management strategies of GD patients. Since vitamin D can regulate immune responses and reduce inflammation, there is a definite need to further evaluate the role of vitamin D deficiency in TED patients. The current evidence for TED suggests that vitamin D would be associated with TED, however, the evidence is limited. It is worthwhile to further investigate the effect of vitamin D on TED.
Table 6.
Summary of studies related to thyroid eye disease included.
| First Author | Years | Country | Study-Design | Sample Size | Main Finding | Rate # |
|---|---|---|---|---|---|---|
| Ama Sadaka [245] | 2019 | United States | Retrospective study | 35 TED patients | 20% and 31% prevalence of vitamin D deficiency and insufficiency were found in TED, respectively. | 4a |
| Curtis J Heisel [246] | 2020 | United States | Retrospective case-control study | 89 TED patients (TED), 89 GD patients without TED (GD), and 2 healthy control groups matched 4:1 to the cases; 356 healthy control patients matched to the TED group (HC TED), and 356 HC patients matched to the GD (HC GD) | Low serum vitamin D is associated with TED diagnosis. Assessing and supplementing vitamin D levels may be an important addition to the early management of GD patients. | 4a |
| Tereza Planck [247] | 2018 | Sweden | Cross sectional study | Epidemiological part—292 GD patients and 2305 healthy controls Clinical part—219 GD patients Relapse analysis after antithyroid drug treatment part —100 GD patients Genetic part—708 GD patients with (n = 245) or without (n = 459) ophthalmopathy and 1178 sex-matched controls |
Patients with GD had lower vitamin D levels compared to the general population; however, the vitamin D levels did not affect the laboratory or clinical parameters of GD. SNPs in the VDR influenced the risk of GD through mechanisms other than reducing the vitamin D levels. | 4a |
Thyroid eye disease (TED), Graves’ disease (GD); # LEGEND for case-control, cohort, and cross-sectional studies, rating of the studies follow the guidelines from LEGEND.
3.8. Uveitis
Uveitis is the inflammation of the uvea driven by the T-cells [248]. It can be described as a failure of the ocular immune system, with the disease resulting from inflammation and tissue destruction. Since vitamin D can inhibit inflammation, influence T-cell responses, and regulate the immune system, it is necessary to examine its involvement in the development of uveitis. In an experimental autoimmune uveitis model, the oral administration of calcitriol was found to prevent and reverse the progression of uveitis by reducing the immunological response [249].
Although in a population-based study, none of the 25 uveitis patients were found to have vitamin D deficiency [250], two large retrospective case-control studies in the United States found an association of lower vitamin D levels with uveitis and scleritis, respectively [251,252]. Other case-control studies have been conducted on patients with specific types of uveitis, such as anterior uveitis (AAU) or non-infectious anterior uveitis [253,254,255], Vogt-Koyanagi-Harada (VKH) disease [256], sarcoidosis-associated uveitis [257], and juvenile idiopathic arthritis (JIA)-associated uveitis [258] (Table 7). All these studies suggested that the vitamin D deficiency is associated with uveitis development. A recent prospective case-control study consistently reported the association of vitamin D levels with active and inactive non-infectious uveitis patients. Vitamin D levels are related to uveitis severity [259].
Table 7.
Summary of studies related to uveitis included.
| First Author | Years | Country | Study-Design | Sample Size | Main Finding | Rate # |
|---|---|---|---|---|---|---|
| Stephanie M. Llop [251] | 2018 | United States | Retrospective case-control study | 333 Uveitis patients, 103 scleritis patients and 329 controls | Hypovitaminosis D was associated with increased risk of ocular inflammation | 4a |
| Lindsay A Grotting [255] | 2017 | United States | Retrospective case-control study | 100 Noninfectious anterior uveitis patients and 100 healthy controls | Lower vitamin D levels are associated with an increased risk of noninfectious anterior uveitis. | 4a |
| Xianglong Yi [256] | 2011 | China | Case-control study | 8 active VKH patients, 7 inactive VKH patients and 8 healthy controls | These findings suggest that decreased expression of 1,25(OH)2D3 may be involved in the development of VKH disease. 1,25(OH)2D3 may be potentially used in the treatment of this disease. | 4b |
| Zeynep Dadaci [254] | 2016 | Turkey | Case-control study | 20 acute anterior uveitis patients and 20 healthy controls | Significantly low serum levels of vitamin D was found in patients with acute anterior uveitis, which suggest that vitamin D deficiency may play a role in the pathogenesis of anterior uveitis. | 4a |
| TC Mitulescu [253] | 2016 | Romania | Case-control study | 11 AS with AAU patients, 23 AS patients without AAU patients and 18 healthy controls | Altered levels of Vit D affect the balance between LL-37, IL-8 and Serum Amyloid A, suggesting an association with AAU, an extra-articular manifestation of AS. | 4b |
| Lucia Sobrin [252] | 2018 | United States | Retrospective case-control study | 558 noninfectious uveitis patients and 2790 healthy controls | Hypovitaminosis D may be a risk factor for noninfectious uveitis. | 4a |
| Zelia K. Chiu [259] | 2020 | Australia | Prospective case-control study | 74 active and 77 inactive noninfectious uveitis patients and 594 local general population controls | Participants with active uveitis showed significantly lower serum 25(OH)D3 levels than inactive uveitis patients and local population-based estimates. Vitamin D supplementation was found to be associated with decreased uveitis activity, as was sun exposure in those with vitamin D deficiency. | 4a |
| Ma’an Abdullah Al-Barry [25] | 2016 | Arabia | Cross-sectional study | 39 VKH patients and 50 healthy controls | low vitamin D levels might play a role in VKH pathogenesis and mutations in genes involved in vitamin D anabolism and catabolism might be of importance in VKH pathobiology. | 3b |
| Julien Rohmer [257] | 2020 | France | Retrospective study | 59 Uveitis patients | The measurement of serum 25(OH)D3 and 1,25(OH)2D3 levels is a useful tool in the etiological workup of patients with unexplained uveitis, since a high 1,25(OH)2D3/25(OH)D3 ratio is suggestive of ocular sarcoidosis. | 4a |
| Claudia Sengler [258] | 2018 | Germany | Prospective observational, controlled multicenter study | 360 juvenile idiopathic arthritis (JIA) patients and 360 healthy controls | 25(OH)D3 deficiency was common and associated with higher disease activity and risk of developing JIA-associated uveitis. | 3a |
| Marta Mora Gonzalez [250] | 2018 | United States | Cross-sectional population-based study | 25 uveitis patients and unknown number of non-uveitis controls | None of the 25 patients were found to have serum vitamin D values indicative of deficiency (less than or equal to 30 nmol/L). | 3b |
Vogt-Koyanagi-Harada (VKH), ankylosing spondylitis (AS), acute anterior uveitis (AAU); # LEGEND for case-control, cohort, and cross-sectional studies, rating of the studies follow the guidelines from LEGEND.
There are reported associations between VDR polymorphisms and uveitis. Single-nucleotide polymorphisms (SNPs) of the CYP2R1, CYP27B1, CYP24A1 and DHCR7 genes are linked with lower circulating vitamin D levels [260,261,262,263]. A study in a Chinese cohort found that the frequencies of the genotype TT and T allele of DHCR7 rs12785878 were both significantly higher among ocular Behçet disease (BD) patients compared with healthy controls; however, similar associations were not found for the VKH, AAU with ankylosing spondylitis (AS), or pediatric uveitis [263]. Another cross-sectional study found that gene variants involved in vitamin D anabolism and catabolism may be important for VKH pathology [25].
In summary, much evidence has shown that the onset and activity of uveitis are associated with vitamin D level, but most of the above studies were observational and did not provide evidence for causality. In the future, randomized-controlled studies are required to evaluate whether vitamin D can be an option for treating uveitis.
3.9. Retinoblastoma
Vitamin D has antineoplastic functions against many types of cancers through influencing cell differentiation, apoptosis regulation, anti-angiogenesis, and cell cycle arrest in various tumors [20]. Animal studies suggested that vitamin D analogues inhibited retinoblastoma (RB) tumor growth in athymic mice by increasing apoptosis, which is associated with the upregulation of both the p53 and p21 proteins [264,265]. However, due to the extremely low incidence rate of RB, few clinical studies have been conducted regarding the effect of vitamin D on RB. Two recent studies in Mexico found that sun exposure in early childhood protects against RB and may decrease the degree of intraocular spread in children with bilateral RB [266,267] (Table 8). However, RB is a childhood cancer, which usually presents at the age of 1 to 2 for bilateral and unilateral RB. Further studies are needed to confirm and understand the association between vitamin D levels and RB.
Table 8.
Summary of studies related to tumor included.
| First Author | Years | Country | Study-Design | Sample Size | Main Finding | Rate # |
|---|---|---|---|---|---|---|
| Fabiola Mejía-Rodríguez [266] | 2021 | Mexico | Case-control study | 126 Sporadic RB patients and 102 healthy controls | Latitude and the number of days exposed to the spring–summer season during 6 to 11.9 months of life were negatively associated with sporadic retinoblastoma in children who had exclusive maternal lactation. | 4a |
| Manuela Orjuela-Grimm [267] | 2021 | Mexico | Case-control study | 259 Unilateral RB patients, 120 bilateral RB and 132 healthy controls | Sun exposure in early childhood is protective for retinoblastoma and may decrease degree of intraocular spread in children with bilateral RB. | 4a |
| Schundeln Michael M [268] | 2015 | Germany | Cross-sectional study | 14 Unilateral RB patients and 19 bilateral RB | 51.7% of RB patients and 13.7% of RB patients were vitamin D deficient and severe vitamin D deficient, respectively. | 3b |
Retinoblastoma (RB); # LEGEND for case-control, cohort, and cross-sectional studies, rating of the studies follow the guidelines from LEGEND.
3.10. Cataract
For the past 20 years, the prevalence of cataracts has declined due to the advancement of surgical technology. However, in middle-income and low-income countries, cataract is still the most common cause of visual loss, accounting for 50% blindness [269]. Cataract is caused by losing lens transparency when the lens becomes opaque [269]. Epidemiology studies have shown that ultraviolet radiation is an important factor in increasing the risk of cataract [270,271,272]. Since the natural source of vitamin D is sunlight exposure, vitamin D may be involved in the pathophysiology of cataract. The opacity of the lens is a result of oxidative stress [273]. Since vitamin D can protect cells or reduce oxidative stress [69,70,71], it can be protective against cataract and play a role in lens metabolism.
There are studies attempting to reveal the association between vitamin D and cataract (Table 9). A large cross-sectional study in South Korea, with 16,086 participants aged 40 years or older, revealed that serum 25(OH)D levels were inversely associated with the risk of nuclear cataract [274]. Similarly, another South Korean study on 18,804 subjects also found that cataract risk decreased in men with higher serum 25-hydroxyvitamin D levels compared with those with lower serum 25(OH)D levels, but this association is not significant in women [275]. Other studies in Egypt [276], Turkey [277,278], and the UK [279] also showed that cataract patients often have a low level of serum vitamin D. However, one study [280] reported that serum 25(OH)D levels were not related to nuclear opacities.
Table 9.
Summary of studies related to cataract included.
| First Author | Years | Country | Study-Design | Sample Size | Main Finding | Rate # |
|---|---|---|---|---|---|---|
| Aidenloo Naser Samadi [280] | 2021 | Iran | Cross-sectional study | 216 nuclear cataract patients, 336 cortical cataract patients, 140 posterior sub-capsular cataract patients, 549 mixed cataract patients and 200 normal controls | Serum 25(OH)D3 levels were inversely associated with the risk of nuclear cataract and cortical cataract and not associated with posterior sub-capsular cataract or mixed cataract in women. No association between vitamin D and cataractogenesis in men. | 4a |
| Donghyun Jee [281] | 2015 | South Korea | Population-based cross-sectional study | 18,804 participants (7993 age-related cataracts, 1332 with a history of cataract surgery and 9479 no cataract participants) | Men with higher serum 25(OH)D3 levels have a lower risk for the age-related cataract; while no association were found in women. | 4a |
| Sangshin Park [274] | 2016 | South Korea | Cross-sectional study | 16,086 participants (cortical, 1562; nuclear, 4116; anterior subcapsular, 174; posterior subcapsular, 87; mixed, 1013; Q1, 3215; Q2, 3214; Q3, 3217; Q4, 3226; and Q5, 3214) | Serum 25(OH)D3 levels were inversely associated with the risk of nuclear cataract. | 4a |
| Caglar Okem [278] | 2021 | Turkey | Sectional case-control study | 37 cataract patients and 53 healthy controls | Vitamin D deficiency as associated with early age-related cataract. | 4a |
| Prethy Rao [280,282] | 2015 | United States | Cross-sectional study | 1278 participants (nuclear cataract, 516; Q1, 256; Q2, 257; Q3, 254; Q4, 256; and Q5, 255) | No significant association between serum 25(OH)D3 levels and nuclear cataract. | 4a |
| Craig J Brown [279] | 2015 | United States | Cross-sectional | 175 cataract patients | Vitamin D deficiency was associated with posterior subcapsular cataract. | 4b |
| K Atalay [277] | 2020 | Turkey | Hospital-based cross-sectional study | 26 posterior subcapsular cataract patients and 53 age-related cataract without posterior subcapsular cataract patients | Patients with age-related cataract without posterior subcapsular component showed statistically significantly lower vitamin D level than 20 ng/mL (vitamin D insufficiency level). | 4b |
| Min-Chul Cho [283] | 2020 | South Korea | Prospective study | 87 senile cataract patients and 49 diabetic cataract patients | Higher 25(OH)D3 levels in aqueous humor was associated with diabetic cataract. | 3a |
| Marwa Mahmoud Abdellan [276] | 2019 | Egypt | Case-control study | 325 cataract patients and 385 healthy controls | Vitamin D deficiency may have a role in age-related cataract patients. | 4a |
# LEGEND for case-control, cohort, and cross-sectional studies, rating of the studies follow the guidelines from LEGEND.
In summary, all the current studies are cross-sectional or retrospective in design, so the causal relationship between vitamin D and cataract needs to be proved by further large-prospective cohort or RCT. Cataract is essentially a treatable disease. Future study design should aim to find out whether vitamin D supplementation could protect elders against cataract development.
3.11. Other Ocular Diseases
Apart from the diseases described earlier, some studies reported on the association of vitamin D with curable or rare ocular diseases (Table 10). Vernal keratoconjunctivitis patients were found to be at a significantly lower level of serum vitamin D in case-control studies held in Turkey [284,285], Italy [286], and Iran [287]. Deficiency of vitamin D is also more frequently found in patients with keratoconus [288,289,290], retinal venous occlusions [291,292], and optic neuritis [293,294,295]. However, in children with allergic conjunctivitis, the results were contradictory: two studies [296,297] found significantly higher vitamin D levels in patients, while the other studies reported complete opposite conclusion [298,299].
Table 10.
Summary of studies related to other ocular diseases included.
| First Author | Years | Country | Disease | Study-Design | Sample Size | Main Finding | Rate # |
|---|---|---|---|---|---|---|---|
| Gonul Karatas Durusoy [284] | 2020 | Turkey | VKC | Case-control study | 46 VKC patients and 40 healthy controls | Children with VKC has a lower serum 25(OH)D3 levels when compared with healthy controls. | 4b |
| Anna Maria Zicari [286] | 2016 | Italy | VKC | Prospective | 47 VKC patients and 63 healthy controls | Children with VKC has a lower serum 25(OH)D3 levels when compared with healthy controls. And the vitamin D level was significantly correlated with the severity. | 3b |
| Banu Bozkurt [285] | 2016 | Turkey | VKC | Case-control study | 29 VKC patients and 62 healthy controls | Serum 25(OH)D3 levels in VKC children was significantly lower than those healthy control. 48.3% of VKC children and 22.6% healthy children were found to have severe vitamin D deficiency. | 4b |
| Rana Sorkhabi [287] | 2021 | Iran | VKC | Case-control study | 39 VKC patients and 32 healthy controls | Serum 25(OH)D3 levels in VKC patients were significantly lower than healthy controls. A statically insignificant reverse correlation of the serum vitamin D levels and the severity were found. | 4a |
| Daniele Giovanni Ghiglioni [313] | 2019 | Italy | VKC | Prospective | 71 VKC patients (mixed, 46; tarsal, 19; and limbal, 6) | There was a significant different in serum 25(OH)D3 levels in children with limbal VKC and tarsal VKC. The ocular treatment with immunomodulator eye drops allow the improvement in serum 25(OH)D3 levels. | 3b |
| Mehmet Gökhan Aslan [288] | 2021 | Italy | KCN | Case-control study | 28 progressive KCN patients, 27 nonprogressive KCN patients and 30 healthy controls | Serum 25(OH)D3 levels in KCN were significantly lower than healthy controls. Decreased vitamin D levels significantly increased nonprogressive KCN and progressive KCN probability 1.23 and 1.29 times, respectively. | 4a |
| Serkan Akkaya [289] | 2020 | Turkey | KCN | Case-control study | 100 KCN patients and 100 healthy controls | Serum 25(OH)D3 levels were significantly lower in KCN group than healthy control group, but no significant difference in the distribution of vitamin D levels among KCN groups of different severity. | 4a |
| Siamak Zarei-Ghanavati [290] | 2020 | Iran | KCN | Cross-sectional | 100 KCN patients and 100 healthy controls | A lower serum 25(OH)D3 level was found in the KCN group compared to the control group, but insignificant differences were found among different KCN stage groups. | 4a |
| Sevil Bilir Goksugur [296] | 2015 | Turkey | ARC | Case-control study | 22 ARC patients and 31 healthy controls | Serum 25(OH)D3 levels were associated with ARC in children. | 4a |
| Alper Yenign [298] | 2015 | Turkey | ARC | Prospective cross-sectional study | 42 ARC patients and 35 healthy controls | Plasma 25(OH)D3 levels in ARC patients were significantly lower than the control group. | 4a |
| Zeynep Dadaci [299] | 2014 | Turkey | Seasonal ARC | Case-control study | 49 seasonal ARC patients and 44 healthy controls | Plasma 25(OH)D3 levels of seasonal ARC were significantly lower than control group. | 4a |
| Farhan Khashim Alswailmi [297] | 2021 | Saudi Arabi | Seasonal ARC | Cross-sectional case-control study | 26 seasonal ARC patients and 26 healthy controls | Mean vitamin D level was significantly higher in seasonal ARC patients. Higher serum vitamin D levels may be linked with seasonal ARC. | 4b |
| Lin Chen [314] | 2014 | China | Chalazia | Prospective case-control study | 88 chalazia patients and 72 healthy controls | No significant differences in vitamin D3 | 4b |
| Kubra Serefoglu Cabuk [26] | 2020 | Turkey | Blepharospasm | Prospective case-control study | 50 Blepharospasm patients and 22 healthy controls | Serum 25(OH)D3 levels were moderately negatively correlated with Blepharospasm severity (Jankovic severity score). | 4b |
| Emrah Utku Kabatas [315] | 2017 | Turkey | Retinopathy | Prospective | 97 premature infants patients | Serum 25(OH)D3 levels were significantly lower in infants with retinopathy of prematurity than those without retinopathy of prematurity. | 3a |
| Sedat Arikan [300] | 2020 | Turkey | Spatial contrast | Prospective | 41 VDD patients and 30 without VDD controls | Vitamin D deficiency cause a decrease in contrast sensitivity function. | 3a |
| Emrah Ozturk [301] | 2020 | Turkey | Contrast sensitivity | Prospective | 42 VDD patients and 34 normal levels control | VDD had negative effects on contrast sensitivity function and also caused thickness difference in certain segments of retinal layers. | 3a |
| Aydemir Gozde Aksoy [302] | 2022 | Turkey | Choroidal thickness | Case-control study | 46 DM with VDD patients, 42 DM with normal vitamin D level patients, and 73 healthy controls | No difference in retinal nerve fibre layer (RNFL) between three groups. VDD has no effect on the RNFL. However, a positive correlation existed between the macular choroidal thickness (CT) and the vitamin D levels in DM patients with VDD. | 4a |
| Esra Vural [303] | 2020 | Turkey | Choroidal thickness | Prospective case-control study | 30 VDD patients and 30 normal level controls | A positive correlation was found between vitamin D levels and subfoveal choroidal thickness and inferior and nasal peripapillary choroidal thickness in all participants. | 4a |
| Hasan Oncul [304] | 2020 | Turkey | Choroidal thickness | Prospective case-control study | 65 VDD patients and 60 normal level controls | VDD patients have a thinner choroid and the choroidal thickness increased after vitamin D replacement therapy. | 4a |
| Cem Cankaya [305] | 2018 | United States | Corneal endothelial | Case-control study | 58 VDD patients and 40 normal level controls | The mean corneal endothelial cell density and mean hexagonal cell ratio in VDD patients were lower than healthy controls. The mean coefficient of variation in VDD patients were higher than healthy controls. VDD may affect the corneal endothelial layer. | 4a |
| Alix Graffe [306] | 2014 | France | Macular thickness | Cross-sectional | 62 patients (17 and 45 with vitamin D insufficiency and sufficiency, respectively) | Vitamin D insufficiency was associated with reduced macular thickness with no patent macular dysfunction. | 4a |
| Unal Mutlu [316] | 2016 | Netherlands | Retinal microvascular | Prospective population-based study | 5675 subjects (sample) and 2973 subjects (subsample) | Individuals with lower vitamin D levels were more likely to have retinopathy. Lower vitamin D levels were associated with wider venular calibers. | 3a |
| Hatice Daldal [317] | 2021 | Turkey | Ocular findings | Prospective | 98 patients (41, 45 and 12 were vitamin D severe deficient, deficient and insufficient, respectively) | Vitamin D may be related to thinning in macular and nasal of RNFL. | 3a |
| Karabulut Mujdat [318] | 2022 | Turkey | Retinal microvascularity | Case-control study | 98 VDD patients and 96 healthy controls | There was a strong negative correlation between the serum vitamin D level and vessel density in the whole image, parafoveal, and perifoveal regions of the deep capillary plexus in the study group (Spearman’s rho = −0.71, p = 0.043; Spearman’s rho = −0.79, p = 0.011; and Spearman’s rho = −0.74, p = 0.032; respectively). | 4a |
VKC: vernal keratoconjunctivitis; KCN: keratoconus; ARC: allergic rhinoconjunctivitis; VDD: vitamin D deficiency; # LEGEND for case-control, cohort, and cross-sectional studies, rating of the studies follow the guidelines from LEGEND.
It is notable that vitamin D is associated with most ocular diseases, from anterior segment to retina. One possible explanation is that vitamin D or its metabolite plays a role in maintaining the stability of ocular metabolism and structure. Higher 25(OH)D levels in aqueous humor may have an influence on ocular disease [119,283]. The change of ocular structure and function, including spatial contrast [300], contrast sensitivity [301], choroidal thickness [302,303,304], corneal endothelial [305], and macular thickness [306], may be affected by serum levels of vitamin D. On the other hand, this association is not a causality. Vitamin D may work as a marker of health status. People with poor health or low vision will have little outdoor activities and consequentially less exposure to sunlight. Some studies found a positive association or no association between vitamin D levels and pterygium [275,307,308,309,310]. Outdoor occupation is a major risk factor for the development of pterygium [311,312].
4. Perspective
In this systematic review, we summarize the evidence of vitamin D’s effect on different ocular diseases. However, there are significant limitations in many studies, and the interpretation of results should be within these limitations.
First, the definition of vitamin D deficiency is not consistent in different studies, which affects the objective comparison of results from different studies. Until 1998, vitamin D deficiency was defined as a blood level of 25(OH)D, which represents a total concentration of both 25-hydroxyvitamin D2 and 25-hydroxyvitamin D3 of less than 10 ng/mL (25 nmol/L). However, this definition was redefined in 1998 as a blood level of 25(OH)D < 20 ng/mL (50 nmol/L). One reason for the change in the involvement of PTH: adults may require a serum 25(OH)D of at least 50 nmol/L to achieve optimum PTH levels [319]. Moreover, some studies use quintiles or quartiles to perform data analysis. We suggest that future studies should use the common classification to analyze serum vitamin D levels.
Second, vitamin D levels are related to different socioeconomic, lifestyle, and dietary factors. These factors are very important when considering the onset or development of ocular diseases. Future studies should determine these factors and consider them as confounders in statistical analysis.
Finally, few studies provided causal evidence on whether supplementing vitamin D can reduce the prevalence of ocular diseases. Currently, available evidence is insufficient to confirm how vitamin D works in ocular diseases. Moreover, investigations of those metabolic enzymes are also important to understand why significantly low vitamin D is found in patients with ocular diseases. In summary, among all ocular diseases, the association between vitamin D and AMD was unclear, while clinical trials in DES or DR required bigger sample sizes in different ethnic populations. Other ocular diseases such as cataract, myopia, and uveitis, no RCTs or perspective cohorts have been reported, so their associations with vitamin D are still unclear.
5. Vitamin D and Eye Care
Vitamin D can be a potential intervention for different ocular diseases. Although findings for certain ocular diseases are inconsistent, they can still serve as references for further studies that examine the therapeutic effects of vitamin D on ocular diseases, considering that vitamin D deficiency is a common health issue worldwide, and vitamin D has wide safety doses and rare side effects. Even though more evidence from the randomized controlled trial is needed to confirm the effect of vitamin D on various ocular diseases, it is recommended to maintain blood 25(OH)D3 at a desirable level (25–50 nmol/L) by spending a short period of time outdoors, baring skin to the sun, and boosting vitamin D intake by a daily supplement of 400–800 international units (10 to 20 μg).
The human body can also obtain vitamin D naturally from sunlight exposure, however, both extended exposure to unprotected sunshine, which also increases the risk for cataracts, and AMD and completely avoiding sunlight by applying UV B sunscreen should be avoided. Several factors affect vitamin D production, and a more efficient production of vitamin D can be achieved when someone is closer to the equator, has a lighter skin color, and/or exposes larger surfaces of skin during summer midday without sunscreen. Generally, 5–30 min of sun exposure on the unprotected face, arms, legs, or back between 10 a.m. and 3 p.m. twice to three times a week is enough for sufficient vitamin D. Even though vitamin D can be beneficial to our ocular health, long term prolonged sun exposure is also associated with corneal sunburn, tissue growths on sclera, cataracts, and macular degeneration, and wearing hats, and sunglasses are recommended to protect the eyes from UV damage.
6. Conclusions
Various epidemiological and clinical studies have demonstrated a connection between vitamin D deficiency and ocular diseases, such as myopia, age-related macular degeneration, glaucoma, diabetic retinopathy, dry eye syndrome, thyroid eye disease, uveitis, retinoblastoma, and cataract, among others. While vitamin D is associated with potential pathways related to these respective diseases, their pathogeneses are complicated, and current understandings of the underlying mechanisms remain limited. Vitamin D not only affects mineral metabolism homeostasis, but also possesses antioxidation and anti-inflammatory properties. It also plays a role in anti-angiogenesis, modulating cell cycle including cell proliferation, differentiation, and apoptosis. VDR and vitamin D regulatory enzymes are present in ocular tissues, and studies have demonstrated that ocular tissues can activate and regulate vitamin D, suggesting the importance of vitamin D in maintaining ocular health.
Author Contributions
Conceptualization, H.-N.C., X.-J.Z., J.C.Y., C.-P.P.; methodology, H.-N.C. and X.-J.Z.; validation, H.-N.C., X.-J.Z. and X.-T.L.; formal analysis, H.-N.C., X.-J.Z. and X.-T.L.; investigation, H.-N.C. and X.-J.Z.; writing—original draft preparation, H.-N.C., X.-J.Z., X.-T.L. and C.H.-T.B.; writing—review and editing, Y.-M.W., P.I., W.-K.C., L.-J.C., C.C.T., J.C.Y. and C.-P.P.; supervision, J.C.Y. and C.-P.P. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported in part by the General Research Fund (GRF), Research Grants Council, Hong Kong (14111515 and 14103419 [JCY]); Collaborative Research Fund (C7149-20G [JCY]); Health and Medical Research Fund (HMRF), Hong Kong (5160836, [LJC] and 07180826 [XJZ]), and the Direct Grants of the Chinese University of Hong Kong, (4054193 [LJC] and 4054121 & 4054199 [JCY] and 4054634 [XJZ]), the Innovation and Technology Fund (7010590 [JCY]), the UBS Optimus Foundation Grant 8984 (JCY); the Centaline Myopia Fund [JCY]; the CUHK Jockey Club Children’s Eye Care Programme; and the CUHK Jockey Club Myopia Prevention Programme.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Plum L.A., DeLuca H.F. Vitamin D, disease and therapeutic opportunities. Nat. Rev. Drug Discov. 2010;9:941–955. doi: 10.1038/nrd3318. [DOI] [PubMed] [Google Scholar]
- 2.Zmijewski M.A. Vitamin D and Human Health. Int. J. Mol. Sci. 2019;20:10145. doi: 10.3390/ijms20010145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang R., Naughton D.P. Vitamin D in health and disease: Current perspectives. Nutr. J. 2010;9:65. doi: 10.1186/1475-2891-9-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Ishaq R.K., Kubatka P., Brozmanova M., Gazdikova K., Caprnda M., Büsselberg D. Health implication of vitamin D on the cardiovascular and the renal system. Arch. Physiol. Biochem. 2021;127:195–209. doi: 10.1080/13813455.2019.1628064. [DOI] [PubMed] [Google Scholar]
- 5.Rai V., Agrawal D.K. Role of Vitamin D in Cardiovascular Diseases. Endocrinol. Metab. Clin. N. Am. 2017;46:1039–1059. doi: 10.1016/j.ecl.2017.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang T.J., Pencina M.J., Booth S.L., Jacques P.F., Ingelsson E., Lanier K., Benjamin E.J., D’Agostino R.B., Wolf M., Vasan R.S. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117:503–511. doi: 10.1161/CIRCULATIONAHA.107.706127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adamczak M., Surma S., Więcek A. Vitamin D and Arterial Hypertension: Facts and Myths. Curr. Hypertens. Rep. 2020;22:57. doi: 10.1007/s11906-020-01059-9. [DOI] [PubMed] [Google Scholar]
- 8.Seshadri K.G., Tamilselvan B., Rajendran A. Role of Vitamin D in Diabetes. J. Endocrinol. Metab. 2011;1:47–56. doi: 10.4021/jem23w. [DOI] [Google Scholar]
- 9.Jani R., Mhaskar K., Tsiampalis T., Kassaw N.A., González M.Á.M., Panagiotakos D.B. Circulating 25-hydroxy-vitamin D and the risk of cardiovascular diseases. Systematic review and meta-analysis of prospective cohort studies. Nutr. Metab. Cardiovasc. Dis. 2021;31:3282–3304. doi: 10.1016/j.numecd.2021.09.003. [DOI] [PubMed] [Google Scholar]
- 10.Jeon S.M., Shin E.A. Exploring vitamin D metabolism and function in cancer. Exp. Mol. Med. 2018;50:1–14. doi: 10.1038/s12276-018-0038-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Holick M.F., Binkley N.C., Bischoff-Ferrari H.A., Gordon C.M., Hanley D.A., Heaney R.P., Murad M.H., Weaver C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011;96:1911–1930. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 12.Brown E.M., Gamba G., Riccardi D., Lombardi M., Butters R., Kifor O., Sun A., Hediger M.A., Lytton J., Hebert S.C. Cloning and characterization of an extracellular Ca(2+)–sensing receptor from bovine parathyroid. Nature. 1993;366:575–580. doi: 10.1038/366575a0. [DOI] [PubMed] [Google Scholar]
- 13.Holick M.F. Vitamin D status: Measurement, interpretation, and clinical application. Ann. Epidemiol. 2009;19:73–78. doi: 10.1016/j.annepidem.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dominguez L.J., Farruggia M., Veronese N., Barbagallo M. Vitamin D Sources, Metabolism, and Deficiency: Available Compounds and Guidelines for Its Treatment. Metabolites. 2021;11:255. doi: 10.3390/metabo11040255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bikle D.D. Vitamin D Metabolism, Mechanism of Action, and Clinical Applications. Chem. Biol. 2014;21:319–329. doi: 10.1016/j.chembiol.2013.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zmijewski M.A., Carlberg C. Vitamin D receptor(s): In the nucleus but also at membranes? Exp. Dermatol. 2020;29:876–884. doi: 10.1111/exd.14147. [DOI] [PubMed] [Google Scholar]
- 17.Kim S., Shevde N.K., Pike J.W. 1,25-Dihydroxyvitamin D3 stimulates cyclic vitamin D receptor/retinoid X receptor DNA–binding, co-activator recruitment, and histone acetylation in intact osteoblasts. J. Bone Miner. Res. 2005;20:305–317. doi: 10.1359/JBMR.041112. [DOI] [PubMed] [Google Scholar]
- 18.Skowron K., Pawlicka I., Gil K. The role of vitamin D in the pathogenesis of ocular diseases. Folia Med. Cracov. 2018;58:103–118. doi: 10.24425/fmc.2018.124662. [DOI] [PubMed] [Google Scholar]
- 19.Jamali N., Wang S., Darjatmoko S.R., Sorenson C.M., Sheibani N. Vitamin D receptor expression is essential during retinal vascular development and attenuation of neovascularization by 1, 25(OH)2D3. PLoS ONE. 2017;12:e0190131. doi: 10.1371/journal.pone.0190131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reins R.Y., McDermott A.M. Vitamin D: Implications for ocular disease and therapeutic potential. Exp. Eye Res. 2015;134:101–110. doi: 10.1016/j.exer.2015.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alsalem J.A., Patel D., Susarla R., Coca-Prados M., Bland R., Walker E.A., Rauz S., Wallace G.R. Characterization of vitamin D production by human ocular barrier cells. Investig. Ophthalmol. Vis. Sci. 2014;55:2140–2147. doi: 10.1167/iovs.13-13019. [DOI] [PubMed] [Google Scholar]
- 22.Yin Z., Pintea V., Lin Y., Hammock B.D., Watsky M.A. Vitamin D enhances corneal epithelial barrier function. Investig. Ophthalmol. Vis. Sci. 2011;52:7359–7364. doi: 10.1167/iovs.11-7605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Verstappen A., Parmentier M., Chirnoaga M., Lawson D.E., Pasteels J.L., Pochet R. Vitamin D–dependent calcium binding protein immunoreactivity in human retina. Ophthalmic Res. 1986;18:209–214. doi: 10.1159/000265436. [DOI] [PubMed] [Google Scholar]
- 24.Rullo J., Pennimpede T., Mehraban Far P., Strube Y.N., Irrcher I., Urton T., Bona M., Gonder T., Campbell R.J., Ten Hove M., et al. Intraocular calcidiol: Uncovering a role for vitamin D in the eye. J. Steroid Biochem. Mol. Biol. 2020;197:105536. doi: 10.1016/j.jsbmb.2019.105536. [DOI] [PubMed] [Google Scholar]
- 25.Al-Barry M.A., Albalawi A.M., Sayf M.A., Badawi A., Afzal S., Latif M., Samman M.I., Basit S. Sequence analysis of four vitamin D family genes (VDR, CYP24A1, CYP27B1 and CYP2R1) in Vogt-Koyanagi-Harada (VKH) patients: Identification of a potentially pathogenic variant in CYP2R1. BMC Ophthalmol. 2016;16:172. doi: 10.1186/s12886-016-0354-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Serefoglu Cabuk K., Tunc U., Ozturk Karabulut G., Fazil K., Karaagac Gunaydin Z., Asik Nacaroglu S., Taskapili M. Serum calcium, magnesium, phosphorus, and vitamin D in benign essential blepharospasm. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020;258:1293–1297. doi: 10.1007/s00417-020-04650-7. [DOI] [PubMed] [Google Scholar]
- 27.Moher D., Liberati A., Tetzlaff J., Altman D.G., The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta–Analyses: The PRISMA Statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ma L.-L., Wang Y.-Y., Yang Z.-H., Huang D., Weng H., Zeng X.-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020;7:7. doi: 10.1186/s40779-020-00238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clark E., Burkett K., Stanko-Lopp D. Let Evidence Guide Every New Decision (LEGEND): An evidence evaluation system for point-of-care clinicians and guideline development teams. J. Eval. Clin. Pract. 2009;15:1054–1060. doi: 10.1111/j.1365-2753.2009.01314.x. [DOI] [PubMed] [Google Scholar]
- 30.Dolgin E. The myopia boom. Nature. 2015;519:276–278. doi: 10.1038/519276a. [DOI] [PubMed] [Google Scholar]
- 31.Zadnik K., Satariano W.A., Mutti D.O., Sholtz R.I., Adams A.J. The effect of parental history of myopia on children’s eye size. JAMA. 1994;271:1323–1327. doi: 10.1001/jama.1994.03510410035029. [DOI] [PubMed] [Google Scholar]
- 32.Lam D.S., Fan D.S., Lam R.F., Rao S.K., Chong K.S., Lau J.T., Lai R.Y., Cheung E.Y. The effect of parental history of myopia on children’s eye size and growth: Results of a longitudinal study. Investig. Ophthalmol. Vis. Sci. 2008;49:873–876. doi: 10.1167/iovs.06-1097. [DOI] [PubMed] [Google Scholar]
- 33.Fan Q., Verhoeven V.J., Wojciechowski R., Barathi V.A., Hysi P.G., Guggenheim J.A., Hohn R., Vitart V., Khawaja A.P., Yamashiro K., et al. Meta–analysis of gene–environment–wide association scans accounting for education level identifies additional loci for refractive error. Nat. Commun. 2016;7:11008. doi: 10.1038/ncomms11008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rose K.A., Morgan I.G., Ip J., Kifley A., Huynh S., Smith W., Mitchell P. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology. 2008;115:1279–1285. doi: 10.1016/j.ophtha.2007.12.019. [DOI] [PubMed] [Google Scholar]
- 35.Dirani M., Tong L., Gazzard G., Zhang X., Chia A., Young T.L., Rose K.A., Mitchell P., Saw S.M. Outdoor activity and myopia in Singapore teenage children. Br. J. Ophthalmol. 2009;93:997–1000. doi: 10.1136/bjo.2008.150979. [DOI] [PubMed] [Google Scholar]
- 36.Jones L.A., Sinnott L.T., Mutti D.O., Mitchell G.L., Moeschberger M.L., Zadnik K. Parental history of myopia, sports and outdoor activities, and future myopia. Investig. Ophthalmol. Vis. Sci. 2007;48:3524–3532. doi: 10.1167/iovs.06-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Low W., Dirani M., Gazzard G., Chan Y.H., Zhou H.J., Selvaraj P., Au Eong K.G., Young T.L., Mitchell P., Wong T.Y., et al. Family history, near work, outdoor activity, and myopia in Singapore Chinese preschool children. Br. J. Ophthalmol. 2010;94:1012–1016. doi: 10.1136/bjo.2009.173187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.He M., Xiang F., Zeng Y., Mai J., Chen Q., Zhang J., Smith W., Rose K., Morgan I.G. Effect of Time Spent Outdoors at School on the Development of Myopia Among Children in China: A Randomized Clinical Trial. JAMA. 2015;314:1142–1148. doi: 10.1001/jama.2015.10803. [DOI] [PubMed] [Google Scholar]
- 39.Choi J.A., Han K., Park Y.M., La T.Y. Low serum 25-hydroxyvitamin D is associated with myopia in Korean adolescents. Investig. Ophthalmol. Vis. Sci. 2014;55:2041–2047. doi: 10.1167/iovs.13-12853. [DOI] [PubMed] [Google Scholar]
- 40.Guggenheim J.A., Williams C., Northstone K., Howe L.D., Tilling K., St. Pourcain B., McMahon G., Lawlor D.A. Does vitamin D mediate the protective effects of time outdoors on myopia? Findings from a prospective birth cohort. Investig. Ophthalmol. Vis. Sci. 2014;55:8550–8558. doi: 10.1167/iovs.14-15839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mutti D.O., Marks A.R. Blood levels of vitamin D in teens and young adults with myopia. Optom. Vis. Sci. 2011;88:377–382. doi: 10.1097/OPX.0b013e31820b0385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tideman J.W., Polling J.R., Voortman T., Jaddoe V.W., Uitterlinden A.G., Hofman A., Vingerling J.R., Franco O.H., Klaver C.C. Low serum vitamin D is associated with axial length and risk of myopia in young children. Eur. J. Epidemiol. 2016;31:491–499. doi: 10.1007/s10654-016-0128-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yazar S., Hewitt A.W., Black L.J., McKnight C.M., Mountain J.A., Sherwin J.C., Oddy W.H., Coroneo M.T., Lucas R.M., Mackey D.A. Myopia is associated with lower vitamin D status in young adults. Investig. Ophthalmol. Vis. Sci. 2014;55:4552–4559. doi: 10.1167/iovs.14-14589. [DOI] [PubMed] [Google Scholar]
- 44.Kwon J.W., Choi J.A., La T.Y., Epidemiologic Survey Committee of the Korean Ophthalmological Society Serum 25-hydroxyvitamin D level is associated with myopia in the Korea national health and nutrition examination survey. Medicine. 2016;95:5012. doi: 10.1097/MD.0000000000005012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Williams K.M., Bentham G.C., Young I.S., McGinty A., McKay G.J., Hogg R., Hammond C.J., Chakravarthy U., Rahu M., Seland J., et al. Association Between Myopia, Ultraviolet B Radiation Exposure, Serum Vitamin D Concentrations, and Genetic Polymorphisms in Vitamin D Metabolic Pathways in a Multicountry European Study. JAMA Ophthalmol. 2017;135:47–53. doi: 10.1001/jamaophthalmol.2016.4752. [DOI] [PubMed] [Google Scholar]
- 46.Specht I.O., Jacobsen N., Frederiksen P., Heitmann B.L. Neonatal vitamin D status and myopia in young adult men. Acta Ophthalmol. 2020;98:500–505. doi: 10.1111/aos.14349. [DOI] [PubMed] [Google Scholar]
- 47.Jung B.J., Jee D. Association between serum 25-hydroxyvitamin D levels and myopia in general Korean adults. Indian J. Ophthalmol. 2020;68:15–22. doi: 10.4103/ijo.IJO_760_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chou H.D., Yao T.C., Huang Y.S., Huang C.Y., Yang M.L., Sun M.H., Chen H.C., Liu C.H., Chu S.M., Hsu J.F., et al. Myopia in school-aged children with preterm birth: The roles of time spent outdoors and serum vitamin D. Br. J. Ophthalmol. 2021;105:468–472. doi: 10.1136/bjophthalmol-2019-315663. [DOI] [PubMed] [Google Scholar]
- 49.Lingham G., Mackey D.A., Zhu K., Lucas R.M., Black L.J., Oddy W.H., Holt P., Walsh J.P., Sanfilippo P.G., Chan She Ping-Delfos W., et al. Time spent outdoors through childhood and adolescence–assessed by 25-hydroxyvitamin D concentration–and risk of myopia at 20 years. Acta Ophthalmol. 2021;99:679–687. doi: 10.1111/aos.14709. [DOI] [PubMed] [Google Scholar]
- 50.Han S.B., Jang J., Yang H.K., Hwang J.M., Park S.K. Prevalence and risk factors of myopia in adult Korean population: Korea national health and nutrition examination survey 2013–2014 (KNHANES VI) PLoS ONE. 2019;14:e0211204. doi: 10.1371/journal.pone.0211204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gao F., Li P., Liu Y.Q., Chen Y. Association study of the serum 25(OH)D concentration and myopia in Chinese children. Medicine. 2021;100:e26570. doi: 10.1097/MD.0000000000026570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lingham G., Yazar S., Lucas R.M., Walsh J.P., Zhu K., Hunter M., Lim E.M., Cooke B.R., Mackey D.A. Low 25-Hydroxyvitamin D Concentration Is Not Associated With Refractive Error in Middle-Aged and Older Western Australian Adults. Transl. Vis. Sci. Technol. 2019;8:13. doi: 10.1167/tvst.8.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hwang H.S., Chun M.Y., Kim J.S., Oh B., Yoo S.H., Cho B.J. Risk Factors for High Myopia in Koreans: The Korea National Health and Nutrition Examination Survey. Curr. Eye Res. 2018;43:1052–1060. doi: 10.1080/02713683.2018.1472286. [DOI] [PubMed] [Google Scholar]
- 54.Harb E.N., Wildsoet C.F. Nutritional Factors and Myopia: An Analysis of National Health and Nutrition Examination Survey Data. Optom. Vis. Sci. 2021;98:458–468. doi: 10.1097/OPX.0000000000001694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wahyudi D., Reiki W., Hardhono. Suhartono The Effect of Vitamin-D and Sunlight to Progressive Myopia in Students with Glasses Correction. Pak. J. Med. Health Sci. 2020;14:1588–1591. [Google Scholar]
- 56.Li X., Lin H., Jiang L., Chen X., Chen J., Lu F. Low Serum Vitamin D Is Not Correlated with Myopia in Chinese Children and Adolescents. Front. Med. 2022;9:809787. doi: 10.3389/fmed.2022.809787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tang S.M., Lau T., Rong S.S., Yazar S., Chen L.J., Mackey D.A., Lucas R.M., Pang C.P., Yam J.C. Vitamin D and its pathway genes in myopia: Systematic review and meta-analysis. Br. J. Ophthalmol. 2019;103:8–17. doi: 10.1136/bjophthalmol-2018-312159. [DOI] [PubMed] [Google Scholar]
- 58.Mutti D.O., Cooper M.E., Dragan E., Jones-Jordan L.A., Bailey M.D., Marazita M.L., Murray J.C., Zadnik K., Group C.S. Vitamin D receptor (VDR) and group–specific component (GC, vitamin D–binding protein) polymorphisms in myopia. Investig. Ophthalmol. Vis. Sci. 2011;52:3818–3824. doi: 10.1167/iovs.10-6534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cuellar-Partida G., Williams K.M., Yazar S., Guggenheim J.A., Hewitt A.W., Williams C., Wang J.J., Kho P.F., Saw S.M., Cheng C.Y., et al. Genetically low vitamin D concentrations and myopic refractive error: A Mendelian randomization study. Int. J. Epidemiol. 2017;46:1882–1890. doi: 10.1093/ije/dyx068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Torii H., Kurihara T., Seko Y., Negishi K., Ohnuma K., Inaba T., Kawashima M., Jiang X., Kondo S., Miyauchi M., et al. Violet Light Exposure Can Be a Preventive Strategy Against Myopia Progression. eBioMedicine. 2017;15:210–219. doi: 10.1016/j.ebiom.2016.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ramin S., Soheilian M., Habibi G., Ghazavi R., Gharebaghi R., Heidary F. Age-Related Macular Degeneration: A Scientometric Analysis. Med. Hypothesis Discov. Innov. Ophthalmol. 2015;4:39–49. [PMC free article] [PubMed] [Google Scholar]
- 62.Apte R.S. Age-Related Macular Degeneration. N. Engl. J. Med. 2021;385:539–547. doi: 10.1056/NEJMcp2102061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Coppé A.M., Ripandelli G., Parisi V., Varano M., Stirpe M. Prevalence of asymptomatic macular holes in highly myopic eyes. Ophthalmology. 2005;112:2103–2109. doi: 10.1016/j.ophtha.2005.06.028. [DOI] [PubMed] [Google Scholar]
- 64.Yonekawa Y., Miller J.W., Kim I.K. Age-Related Macular Degeneration: Advances in Management and Diagnosis. J. Clin. Med. 2015;4:343–359. doi: 10.3390/jcm4020343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Khandhadia S., Cipriani V., Yates J.R., Lotery A.J. Age-related macular degeneration and the complement system. Immunobiology. 2012;217:127–146. doi: 10.1016/j.imbio.2011.07.019. [DOI] [PubMed] [Google Scholar]
- 66.Park Y.G., Park Y.S., Kim I.B. Complement System and Potential Therapeutics in Age-Related Macular Degeneration. Int. J. Mol. Sci. 2021;22:36851. doi: 10.3390/ijms22136851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Chen M., Muckersie E., Forrester J.V., Xu H. Immune activation in retinal aging: A gene expression study. Investig. Ophthalmol. Vis. Sci. 2010;51:5888–5896. doi: 10.1167/iovs.09-5103. [DOI] [PubMed] [Google Scholar]
- 68.Layana A.G., Minnella A.M., Garhofer G., Aslam T., Holz F.G., Leys A., Silva R., Delcourt C., Souied E., Seddon J.M. Vitamin D and Age-Related Macular Degeneration. Nutrients. 2017;9:1120. doi: 10.3390/nu9101120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Peng X., Vaishnav A., Murillo G., Alimirah F., Torres K.E., Mehta R.G. Protection against cellular stress by 25-hydroxyvitamin D3 in breast epithelial cells. J. Cell. Biochem. 2010;110:1324–1333. doi: 10.1002/jcb.22646. [DOI] [PubMed] [Google Scholar]
- 70.Diker-Cohen T., Koren R., Ravid A. Programmed cell death of stressed keratinocytes and its inhibition by vitamin D: The role of death and survival signaling pathways. Apoptosis. 2006;11:519–534. doi: 10.1007/s10495-006-5115-1. [DOI] [PubMed] [Google Scholar]
- 71.Tohari A.M., Zhou X., Shu X. Protection against oxidative stress by vitamin D in cone cells. Cell Biochem. Funct. 2016;34:82–94. doi: 10.1002/cbf.3167. [DOI] [PubMed] [Google Scholar]
- 72.Schleithoff S.S., Zittermann A., Tenderich G., Berthold H.K., Stehle P., Koerfer R. Vitamin D supplementation improves cytokine profiles in patients with congestive heart failure: A double–blind, randomized, placebo-controlled trial. Am. J. Clin. Nutr. 2006;83:754–759. doi: 10.1093/ajcn/83.4.754. [DOI] [PubMed] [Google Scholar]
- 73.Hewison M. Vitamin D and the immune system: New perspectives on an old theme. Rheum. Dis. Clin. N. Am. 2012;38:125–139. doi: 10.1016/j.rdc.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 74.Mantell D.J., Owens P.E., Bundred N.J., Mawer E.B., Canfield A.E. 1 alpha,25-dihydroxyvitamin D(3) inhibits angiogenesis in vitro and in vivo. Circ. Res. 2000;87:214–220. doi: 10.1161/01.RES.87.3.214. [DOI] [PubMed] [Google Scholar]
- 75.Albert D.M., Scheef E.A., Wang S., Mehraein F., Darjatmoko S.R., Sorenson C.M., Sheibani N. Calcitriol is a potent inhibitor of retinal neovascularization. Investig. Ophthalmol. Vis. Sci. 2007;48:2327–2334. doi: 10.1167/iovs.06-1210. [DOI] [PubMed] [Google Scholar]
- 76.Morrison M.A., Silveira A.C., Huynh N., Jun G., Smith S.E., Zacharaki F., Sato H., Loomis S., Andreoli M.T., Adams S.M., et al. Systems biology–based analysis implicates a novel role for vitamin D metabolism in the pathogenesis of age-related macular degeneration. Hum. Genom. 2011;5:538–568. doi: 10.1186/1479-7364-5-6-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Song W.S., Yoon W.T., Kim Y.K., Park S.P. Analysis of 25-Hydroxy Vitamin D in the Aqueous Humor of Age-related Macular Degeneration Patients. J. Korean Ophthalmol. Soc. 2018;59:1024–1029. doi: 10.3341/jkos.2018.59.11.1024. [DOI] [Google Scholar]
- 78.Graffe A., Milea D., Annweiler C., Beauchet O., Mauget-Faysse M., Beauchet O., Kodjikian L., Milea D. Association between hypovitaminosis D and late stages of age-related macular degeneration: A case-control study. J. Am. Geriatr. Soc. 2012;60:1367–1369. doi: 10.1111/j.1532-5415.2012.04015.x. [DOI] [PubMed] [Google Scholar]
- 79.Hashemi R., Bandarian M., Abedi-Taleb E., Khojasteh H., Khedmat L., Asadollahi E., Beytollahi M., Jelodar A.M. The association between blood vitamins D and E with age-related macular degeneration: A pilot study. Interv. Med. Appl. Sci. 2018;10:127–132. doi: 10.1556/1646.10.2018.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kan E., Kan E.K., Yucel O.E. The Possible Link Between Vitamin D Levels and Exudative Age-related Macular Degeneration. Oman. Med. J. 2020;35:e83. doi: 10.5001/omj.2020.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kim K.L., Park S.P. Association between serum vitamin D deficiency and age-related macular degeneration in Koreans: Clinical case-control pilot study. Medicine. 2018;97:e11908. doi: 10.1097/MD.0000000000011908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Singh A., Falk M.K., Subhi Y., Sorensen T.L. The association between plasma 25-hydroxyvitamin D and subgroups in age-related macular degeneration: A cross-sectional study. PLoS ONE. 2013;8:e70948. doi: 10.1371/journal.pone.0070948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kabatas N., Dogan A.S., Yilmaz M., Kabatas E.U., Bicer T., Caliskan S., Celikay O., Ucar F., Gurdal C. Association between age-related macular degeneration and 25(OH) vitamin D levels in the Turkish population. Arq. Bras. Oftalmol. 2022;85:7–12. doi: 10.5935/0004-2749.20220002. [DOI] [PubMed] [Google Scholar]
- 84.Seddon J.M., Reynolds R., Shah H.R., Rosner B. Smoking, dietary betaine, methionine, and vitamin D in monozygotic twins with discordant macular degeneration: Epigenetic implications. Ophthalmology. 2011;118:1386–1394. doi: 10.1016/j.ophtha.2010.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Uro M., Beauchet O., Cherif M., Graffe A., Milea D., Annweiler C. Age-Related Vitamin D Deficiency Is Associated with Reduced Macular Ganglion Cell Complex: A Cross-Sectional High–Definition Optical Coherence Tomography Study. PLoS ONE. 2015;10:e0130879. doi: 10.1371/journal.pone.0130879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mahgoub M.Y., Abou Ghanima A.T., Elmohamady M.N., Abdul Basset S. Age-Related Macular Degeneration in Primary Osteoarthritis Egyptian Patients. Open Access Rheumatol. 2020;12:35–40. doi: 10.2147/OARRR.S244838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Millen A.E., Nie J., Mares J.A., Lutsey P.L., LaMonte M.J., Meuer S.M., Sahli M.W., Andrews C.A., Klein B.E.K., Klein R. Serum 25-Hydroxyvitamin D Concentrations and Incidence of Age-Related Macular Degeneration: The Atherosclerosis Risk in Communities Study. Investig. Ophthalmol. Vis. Sci. 2019;60:1362–1371. doi: 10.1167/iovs.18-25945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cougnard-Gregoire A., Merle B.M., Korobelnik J.F., Rougier M.B., Delyfer M.N., Feart C., Le Goff M., Dartigues J.F., Barberger-Gateau P., Delcourt C. Vitamin D Deficiency in Community–Dwelling Elderly Is Not Associated with Age-Related Macular Degeneration. J. Nutr. 2015;145:1865–1872. doi: 10.3945/jn.115.214387. [DOI] [PubMed] [Google Scholar]
- 89.Day S., Acquah K., Platt A., Lee P.P., Mruthyunjaya P., Sloan F.A. Association of vitamin D deficiency and age-related macular degeneration in medicare beneficiaries. Arch. Ophthalmol. 2012;130:1070–1071. doi: 10.1001/archophthalmol.2012.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Millen A.E., Nie J., Sahli M.W., Mares J.A., Meyers K.J., Klein B.E.K., LaMonte M.J., Lutsey P.L., Andrews C.A., Klein R. Vitamin D Status and Prevalent Early Age-Related Macular Degeneration in African Americans and Caucasians: The Atherosclerosis Risk in Communities (ARIC) Study. J. Nutr. Health Aging. 2017;21:772–780. doi: 10.1007/s12603-016-0827-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Golan S., Shalev V., Treister G., Chodick G., Loewenstein A. Reconsidering the connection between vitamin D levels and age-related macular degeneration. Eye. 2011;25:1122–1129. doi: 10.1038/eye.2011.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Millen A.E., Meyers K.J., Liu Z., Engelman C.D., Wallace R.B., LeBlanc E.S., Tinker L.F., Iyengar S.K., Robinson J.G., Sarto G.E., et al. Association between vitamin D status and age-related macular degeneration by genetic risk. JAMA Ophthalmol. 2015;133:1171–1179. doi: 10.1001/jamaophthalmol.2015.2715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Parekh N., Chappell R.J., Millen A.E., Albert D.M., Mares J.A. Association between vitamin D and age-related macular degeneration in the Third National Health and Nutrition Examination Survey, 1988 through 1994. Arch. Ophthalmol. 2007;125:661–669. doi: 10.1001/archopht.125.5.661. [DOI] [PubMed] [Google Scholar]
- 94.Kim E.C., Han K., Jee D. Inverse relationship between high blood 25-hydroxyvitamin D and late stage of age-related macular degeneration in a representative Korean population. Investig. Ophthalmol. Vis. Sci. 2014;55:4823–4831. doi: 10.1167/iovs.14-14763. [DOI] [PubMed] [Google Scholar]
- 95.McKay G.J., Young I.S., McGinty A., Bentham G.C., Chakravarthy U., Rahu M., Seland J., Soubrane G., Tomazzoli L., Topouzis F., et al. Associations between Serum Vitamin D and Genetic Variants in Vitamin D Pathways and Age-Related Macular Degeneration in the European Eye Study. Ophthalmology. 2017;124:90–96. doi: 10.1016/j.ophtha.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 96.Itty S., Day S., Lyles K.W., Stinnett S.S., Vajzovic L.M., Mruthyunjaya P. Vitamin D deficiency in neovascular versus nonneovascular age-related macular degeneration. Retina. 2014;34:1779–1786. doi: 10.1097/IAE.0000000000000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Millen A.E., Voland R., Sondel S.A., Parekh N., Horst R.L., Wallace R.B., Hageman G.S., Chappell R., Blodi B.A., Klein M.L., et al. Vitamin D status and early age-related macular degeneration in postmenopausal women. Arch. Ophthalmol. 2011;129:481–489. doi: 10.1001/archophthalmol.2011.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Christen W.G., Cook N.R., Manson J.E., Buring J.E., Chasman D.I., Lee I.M., Bubes V., Li C., Haubourg M., Schaumberg D.A., et al. Effect of Vitamin D and omega–3 Fatty Acid Supplementation on Risk of Age-Related Macular Degeneration: An Ancillary Study of the VITAL Randomized Clinical Trial. JAMA Ophthalmol. 2020;138:1280–1289. doi: 10.1001/jamaophthalmol.2020.4409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Merle B.M.J., Silver R.E., Rosner B., Seddon J.M. Associations Between Vitamin D Intake and Progression to Incident Advanced Age-Related Macular Degeneration. Investig. Ophthalmol. Vis. Sci. 2017;58:4569–4578. doi: 10.1167/iovs.17-21673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Aoki A., Inoue M., Nguyen E., Obata R., Kadonosono K., Shinkai S., Hashimoto H., Sasaki S., Yanagi Y. Dietary n-3 Fatty Acid, alpha-Tocopherol, Zinc, vitamin D, vitamin C, and beta-carotene are Associated with Age-Related Macular Degeneration in Japan. Sci. Rep. 2016;6:20723. doi: 10.1038/srep20723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Beauchet O., Milea D., Graffe A., Fantino B., Annweiler C. Association between serum 25-hydroxyvitamin D concentrations and vision: A cross-sectional population-based study of older adults. J. Am. Geriatr. Soc. 2011;59:568–570. doi: 10.1111/j.1532-5415.2010.03299.x. [DOI] [PubMed] [Google Scholar]
- 102.Parravano M., Tedeschi M., Manca D., Costanzo E., Di Renzo A., Giorno P., Barbano L., Ziccardi L., Varano M., Parisi V. Effects of Macuprev((R)) Supplementation in Age-Related Macular Degeneration: A Double-Blind Randomized Morpho–Functional Study Along 6 Months of Follow-Up. Adv. Ther. 2019;36:2493–2505. doi: 10.1007/s12325-019-01016-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pérez Serena A., Martínez Betancourt D.P., González del Valle F., Ruiz-Moreno J.M. Serum 25-hydroxy vitamin D levels in age-related macular degeneration. Int. J. Retin. Vitr. 2022;8:17. doi: 10.1186/s40942-022-00368-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jacob J., Mangelschots E., Michez M., Sanak S.N., Leys A. Cross-Sectional Study on Vitamin D, Zinc Oxide and Fatty Acid Status in a Population with a Moderate to High Risk of AMD Identified by the STARS((R)) Questionnaire. Ophthalmol. Ther. 2021;10:299–311. doi: 10.1007/s40123-021-00335-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Resnikoff S., Pascolini D., Etya’ale D., Kocur I., Pararajasegaram R., Pokharel G.P., Mariotti S.P. Global data on visual impairment in the year 2002. Bull. World Health Organ. 2004;82:844–851. [PMC free article] [PubMed] [Google Scholar]
- 106.Mantravadi A.V., Vadhar N. Glaucoma. Prim. Care. 2015;42:437–449. doi: 10.1016/j.pop.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 107.Yoo T.K., Oh E., Hong S. Is vitamin D status associated with open–angle glaucoma? A cross-sectional study from South Korea. Public Health Nutr. 2014;17:833–843. doi: 10.1017/S1368980013003492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kim H.T., Kim J.M., Kim J.H., Lee M.Y., Won Y.S., Lee J.Y., Park K.H. The Relationship between Vitamin D and Glaucoma: A Kangbuk Samsung Health Study. Korean J. Ophthalmol. 2016;30:426–433. doi: 10.3341/kjo.2016.30.6.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lv Y., Yao Q., Ma W., Liu H., Ji J., Li X. Associations of vitamin D deficiency and vitamin D receptor (Cdx-2, Fok I, Bsm I and Taq I) polymorphisms with the risk of primary open–angle glaucoma. BMC Ophthalmol. 2016;16:116. doi: 10.1186/s12886-016-0289-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Goncalves A., Milea D., Gohier P., Jallet G., Leruez S., Baskaran M., Aung T., Annweiler C. Serum vitamin D status is associated with the presence but not the severity of primary open angle glaucoma. Maturitas. 2015;81:470–474. doi: 10.1016/j.maturitas.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 111.Vukovic Arar Z., Knezevic Pravecek M., Miskic B., Vatavuk Z., Vukovic Rodriguez J., Sekelj S. Association Between Serum Vitamin D Level and Glaucoma in Women. Acta Clin. Croat. 2016;55:203–208. doi: 10.20471/acc.2016.55.02.04. [DOI] [PubMed] [Google Scholar]
- 112.Ayyagari R., Chen Y.I., Zangwill L.M., Holman M., Dirkes K., Hai Y., Arzumanyan Z., Slight R., Hammel N., Girkin C.A., et al. Association of severity of primary open–angle glaucoma with serum vitamin D levels in patients of African descent. Mol. Vis. 2019;25:438–445. [PMC free article] [PubMed] [Google Scholar]
- 113.Ekiz T., Helvaci S. Bone Mineral Density and 25-Hydroxyvitamin D Levels in Patients with Ocular Pseudoexfoliation Syndrome: A Case-Control Study. J. Clin. Densitom. 2016;19:419–422. doi: 10.1016/j.jocd.2016.03.011. [DOI] [PubMed] [Google Scholar]
- 114.Atalay K., Savur F.G., Kirgiz A., Kaldirim H.E., Zengi O. Serum levels of thyroid hormone, vitamin D, vitamin B12, folic acid, C–reactive protein, and hemoglobin in Pseudoexfoliation and primary open angle Glaucoma. J. Fr. Ophtalmol. 2019;42:730–738. doi: 10.1016/j.jfo.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 115.Dikci S., Ozturk E., Firat P.G., Yilmaz T., Taskapan M.C., Yologlu S. The Association of Serum Vitamin D Levels with Pseudoexfoliation Glaucoma/Syndrome. Endocr. Metab. Immune Disord. Drug Targets. 2019;19:166–170. doi: 10.2174/1871530319666181128105911. [DOI] [PubMed] [Google Scholar]
- 116.Carbone L.D., Johnson K., Larson J.C., Thomas F., Wactawski-Wende J., Bollinger K., Chen Z., Watsky M. Association of vitamin D with incident glaucoma: Findings from the Women’s Health Initiative. J. Investig. Med. 2021;69:843–850. doi: 10.1136/jim-2020-001645. [DOI] [PubMed] [Google Scholar]
- 117.Rudnicka A.R., Mt-Isa S., Owen C.G., Cook D.G., Ashby D. Variations in primary open–angle glaucoma prevalence by age, gender, and race: A Bayesian meta-analysis. Investig. Ophthalmol. Vis. Sci. 2006;47:4254–4261. doi: 10.1167/iovs.06-0299. [DOI] [PubMed] [Google Scholar]
- 118.Krefting E.A., Jorde R., Christoffersen T., Grimnes G. Vitamin D and intraocular pressure—Results from a case-control and an intervention study. Acta Ophthalmol. 2014;92:345–349. doi: 10.1111/aos.12125. [DOI] [PubMed] [Google Scholar]
- 119.Cho Y., Yun S.P., Yoo W.S., Kim R.B., Cho M.C., Kim S.J. Reduced 25-hydroxyvitamin D concentration in the aqueous humor of cataract patients with open–angle glaucoma. Sci. Rep. 2021;11:18785. doi: 10.1038/s41598-021-98342-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kocaturk T., Bekmez S., Unubol M. Effects of vitamin D deficiency on intraocular pressure values obtained by ocular response analyzer. Int. Ophthalmol. 2020;40:697–701. doi: 10.1007/s10792-019-01230-5. [DOI] [PubMed] [Google Scholar]
- 121.Kutuzova G.D., Gabelt B.T., Kiland J.A., Hennes-Beann E.A., Kaufman P.L., DeLuca H.F. 1alpha,25-Dihydroxyvitamin D(3) and its analog, 2-methylene-19-nor-(20S)-1alpha,25-dihydroxyvitamin D(3) (2MD), suppress intraocular pressure in non-human primates. Arch. Biochem. Biophys. 2012;518:53–60. doi: 10.1016/j.abb.2011.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Tohari A.M., Alhasani R.H., Biswas L., Patnaik S.R., Reilly J., Zeng Z., Shu X. Vitamin D Attenuates Oxidative Damage and Inflammation in Retinal Pigment Epithelial Cells. Antioxidants. 2019;8:341. doi: 10.3390/antiox8090341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kutuzova G.D., Deluca H.F. Gene expression profiles in rat intestine identify pathways for 1,25-dihydroxyvitamin D(3) stimulated calcium absorption and clarify its immunomodulatory properties. Arch. Biochem. Biophys. 2004;432:152–166. doi: 10.1016/j.abb.2004.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hirooka K., Shiraga F. Potential role for angiotensin–converting enzyme inhibitors in the treatment of glaucoma. Clin. Ophthalmol. 2007;1:217–223. [PMC free article] [PubMed] [Google Scholar]
- 125.Constad W.H., Fiore P., Samson C., Cinotti A.A. Use of an angiotensin converting enzyme inhibitor in ocular hypertension and primary open–angle glaucoma. Am. J. Ophthalmol. 1988;105:674–677. doi: 10.1016/0002-9394(88)90063-3. [DOI] [PubMed] [Google Scholar]
- 126.Harris A., Arend O., Kagemann L., Garrett M., Chung H.S., Martin B. Dorzolamide, visual function and ocular hemodynamics in normal–tension glaucoma. J. Ocul. Pharmacol. Ther. 1999;15:189–197. doi: 10.1089/jop.1999.15.189. [DOI] [PubMed] [Google Scholar]
- 127.Faralli J.A., Schwinn M.K., Gonzalez J.M., Jr., Filla M.S., Peters D.M. Functional properties of fibronectin in the trabecular meshwork. Exp. Eye Res. 2009;88:689–693. doi: 10.1016/j.exer.2008.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Tian B., Gabelt B.T., Geiger B., Kaufman P.L. The role of the actomyosin system in regulating trabecular fluid outflow. Exp. Eye Res. 2009;88:713–717. doi: 10.1016/j.exer.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Comes N., Borrás T. Individual molecular response to elevated intraocular pressure in perfused postmortem human eyes. Physiol. Genom. 2009;38:205–225. doi: 10.1152/physiolgenomics.90261.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Aksoy H., Akcay F., Kurtul N., Baykal O., Avci B. Serum 1,25 dihydroxy vitamin D (1,25(OH)2D3), 25 hydroxy vitamin D (25(OH)D) and parathormone levels in diabetic retinopathy. Clin. Biochem. 2000;33:47–51. doi: 10.1016/S0009-9120(99)00085-5. [DOI] [PubMed] [Google Scholar]
- 131.Suzuki A., Kotake M., Ono Y., Kato T., Oda N., Hayakawa N., Hashimoto S., Itoh M. Hypovitaminosis D in type 2 diabetes mellitus: Association with microvascular complications and type of treatment. Endocr. J. 2006;53:503–510. doi: 10.1507/endocrj.K06-001. [DOI] [PubMed] [Google Scholar]
- 132.Kaur H., Donaghue K.C., Chan A.K., Benitez-Aguirre P., Hing S., Lloyd M., Cusumano J., Pryke A., Craig M.E. Vitamin D deficiency is associated with retinopathy in children and adolescents with type 1 diabetes. Diabetes Care. 2011;34:1400–1402. doi: 10.2337/dc11-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Patrick P.A., Visintainer P.F., Shi Q., Weiss I.A., Brand D.A. Vitamin D and retinopathy in adults with diabetes mellitus. Arch. Ophthalmol. 2012;130:756–760. doi: 10.1001/archophthalmol.2011.2749. [DOI] [PubMed] [Google Scholar]
- 134.Ahmadieh H., Azar S.T., Lakkis N., Arabi A. Hypovitaminosis d in patients with type 2 diabetes mellitus: A relation to disease control and complications. ISRN Endocrinol. 2013;2013:641098. doi: 10.1155/2013/641098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Shimo N., Yasuda T., Kaneto H., Katakami N., Kuroda A., Sakamoto F., Takahara M., Irie Y., Horikawa K., Miyashita K., et al. Vitamin D deficiency is significantly associated with retinopathy in young Japanese type 1 diabetic patients. Diabetes Res. Clin. Pract. 2014;106:e41–e43. doi: 10.1016/j.diabres.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 136.He R., Shen J., Liu F., Zeng H., Li L., Yu H., Lu H., Lu F., Wu Q., Jia W. Vitamin D deficiency increases the risk of retinopathy in Chinese patients with type 2 diabetes. Diabet. Med. 2014;31:1657–1664. doi: 10.1111/dme.12581. [DOI] [PubMed] [Google Scholar]
- 137.Bajaj S., Singh R.P., Dwivedi N.C., Singh K., Gupta A., Mathur M. Vitamin D levels and microvascular complications in type 2 diabetes. Indian J. Endocrinol. Metab. 2014;18:537–541. doi: 10.4103/2230-8210.137512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Zoppini G., Galletti A., Targher G., Brangani C., Pichiri I., Trombetta M., Negri C., De Santi F., Stoico V., Cacciatori V., et al. Lower levels of 25-hydroxyvitamin D3 are associated with a higher prevalence of microvascular complications in patients with type 2 diabetes. BMJ Open Diabetes Res. Care. 2015;3:e000058. doi: 10.1136/bmjdrc-2014-000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Herrmann M., Sullivan D.R., Veillard A.S., McCorquodale T., Straub I.R., Scott R., Laakso M., Topliss D., Jenkins A.J., Blankenberg S., et al. Serum 25-hydroxyvitamin D: A predictor of macrovascular and microvascular complications in patients with type 2 diabetes. Diabetes Care. 2015;38:521–528. doi: 10.2337/dc14-0180. [DOI] [PubMed] [Google Scholar]
- 140.Usluogullari C.A., Balkan F., Caner S., Ucler R., Kaya C., Ersoy R., Cakir B. The relationship between microvascular complications and vitamin D deficiency in type 2 diabetes mellitus. BMC Endocr. Disord. 2015;15:33. doi: 10.1186/s12902-015-0029-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Long M., Wang C., Liu D. Glycated hemoglobin A1C and vitamin D and their association with diabetic retinopathy severity. Nutr. Diabetes. 2017;7:e281. doi: 10.1038/nutd.2017.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ashinne B., Rajalakshmi R., Anjana R.M., Narayan K.M.V., Jayashri R., Mohan V., Hendrick A.M. Association of serum vitamin D levels and diabetic retinopathy in Asian Indians with type 2 diabetes. Diabetes Res. Clin. Pract. 2018;139:308–313. doi: 10.1016/j.diabres.2018.02.040. [DOI] [PubMed] [Google Scholar]
- 143.Bener A., Eliacik M., Cincik H., Ozturk M., DeFronzo R.A., Abdul-Ghani M. The Impact of Vitamin D Deficiency on Retinopathy and Hearing Loss among Type 2 Diabetic Patients. Biomed. Res. Int. 2018;2018:2714590. doi: 10.1155/2018/2714590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Nadri G., Saxena S., Mahdi A.A., Kaur A., Ahmad M.K., Garg P., Meyer C.H. Serum vitamin D is a biomolecular biomarker for proliferative diabetic retinopathy. Int. J. Retin. Vitr. 2019;5:31. doi: 10.1186/s40942-019-0181-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Yuan J., Zhou J.B., Zhao W., Zhang R.H., Cai Y.H., Shu L.P., Qi L., Yang J.K. Could Vitamin D be Associated with Proliferative Diabetic Retinopathy? Evidence from Pooling Studies. Horm. Metab. Res. 2019;51:729–734. doi: 10.1055/a-1010-6449. [DOI] [PubMed] [Google Scholar]
- 146.Wan H., Wang Y., Zhang K., Chen Y., Fang S., Zhang W., Wang C., Li Q., Xia F., Wang N., et al. Associations between Vitamin D and Microvascular Complications in Middle-Aged and Elderly Diabetic Patients. Endocr. Pract. 2019;25:809–816. doi: 10.4158/EP-2019-0015. [DOI] [PubMed] [Google Scholar]
- 147.Butler A.E., Dargham S.R., Latif A., Mokhtar H.R., Robay A., Chidiac O.M., Jayyousi A., Al Suwaidi J., Crystal R.G., Abi Khalil C., et al. Association of vitamin D3 and its metabolites in patients with and without type 2 diabetes and their relationship to diabetes complications. Ther. Adv. Chronic. Dis. 2020;11:1–10. doi: 10.1177/2040622320924159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Afarid M., Ghattavi N., Johari M. Serum Levels of Vitamin D in Diabetic Patients with and Without Retinopathy. J. Ophthalmic Vis. Res. 2020;15:172–177. doi: 10.18502/jovr.v15i2.6734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Lopes M., Laiginhas R., Madeira C., Neves J.S., Barbosa M., Rosas V., Carvalho D., Falcao-Reis F., Falcao M. Association between Serum Vitamin D and Diabetic Retinopathy in Portuguese Patients with Type 1 Diabetes. Acta Med. Port. 2020;33:459–465. doi: 10.20344/amp.12890. [DOI] [PubMed] [Google Scholar]
- 150.Ahmed L.H.M., Butler A.E., Dargham S.R., Latif A., Robay A., Chidiac O.M., Jayyousi A., Al Suwaidi J., Crystal R.G., Atkin S.L., et al. Association of vitamin D2 and D3 with type 2 diabetes complications. BMC Endocr. Disord. 2020;20:65. doi: 10.1186/s12902-020-00549-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Lu L., Zou G., Chen L., Lu Q., Wu M., Li C. Elevated NLRP3 Inflammasome Levels Correlate with Vitamin D in the Vitreous of Proliferative Diabetic Retinopathy. Front. Med. 2021;8:736316. doi: 10.3389/fmed.2021.736316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhao W.J., Xia X.Y., Yin J. Relationship of serum vitamin D levels with diabetic microvascular complications in patients with type 2 diabetes mellitus. Chin. Med. J. 2021;134:814–820. doi: 10.1097/CM9.0000000000001364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Zhao X., Huo L., Yu X., Zhang X. Association of Bone Metabolism Indices and Bone Mineral Density with Diabetic Retinopathy in Elderly Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Inpatient Study in China. J. Diabetes Res. 2021;2021:8853622. doi: 10.1155/2021/8853622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Alcubierre N., Valls J., Rubinat E., Cao G., Esquerda A., Traveset A., Granado-Casas M., Jurjo C., Mauricio D. Vitamin D Deficiency Is Associated with the Presence and Severity of Diabetic Retinopathy in Type 2 Diabetes Mellitus. J. Diabetes Res. 2015;2015:374178. doi: 10.1155/2015/374178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Engelen L., Schalkwijk C.G., Eussen S.J., Scheijen J.L., Soedamah-Muthu S.S., Chaturvedi N., Fuller J.H., Stehouwer C.D. Low 25-hydroxyvitamin D2 and 25-hydroxyvitamin D3 levels are independently associated with macroalbuminuria, but not with retinopathy and macrovascular disease in type 1 diabetes: The EURODIAB prospective complications study. Cardiovasc. Diabetol. 2015;14:67. doi: 10.1186/s12933-015-0231-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Gungor A., Ates O., Bilen H., Kocer I. Retinal Nerve Fiber Layer Thickness in Early-Stage Diabetic Retinopathy with Vitamin D Deficiency. Investig. Ophthalmol. Vis. Sci. 2015;56:6433–6437. doi: 10.1167/iovs.15-16872. [DOI] [PubMed] [Google Scholar]
- 157.Boyuk B., Atalay H., Degirmencioglu S., Altay M., Guzel S., Celebi A., Ekizoglu I., Ayar Y. Association between Vitamin D Level and Microvascular Complications in Patients with Type 2 Diabetes. Eurasian. J. Med. Oncol. 2017;1:190–196. [Google Scholar]
- 158.Chaurasia A., Jain S. Serum Vitamin D Levels in Diabetics and Its Correlation with Diabetic Retinopathy. J. Evol. Med. Dent. Sci. 2017;6:2735–2740. doi: 10.14260/Jemds/2017/590. [DOI] [Google Scholar]
- 159.Richter J., Zavorkova M., Vetvicka V., Liehneova I., Kral V., Rajnohova Dobiasova L. Effects of beta-glucan and Vitamin D Supplementation on Inflammatory Parameters in Patients with Diabetic Retinopathy. J. Diet. Suppl. 2019;16:369–378. doi: 10.1080/19390211.2018.1458769. [DOI] [PubMed] [Google Scholar]
- 160.Senyigit A. The association between 25-hydroxy vitamin D deficiency and diabetic complications in patients with type 2 diabetes mellitus. Diabetes Metab. Syndr. 2019;13:1381–1386. doi: 10.1016/j.dsx.2019.01.043. [DOI] [PubMed] [Google Scholar]
- 161.Almoosa A., Ayachit S., Aldoseri A., Wagih W. Incidence of Vitamin D Deficiency in Patients with Type II Diabetes Mellitus and its Relation to the Severity of Retinopathy. Bahrain Med. Bull. 2019;41:238–240. [Google Scholar]
- 162.Ahmed L.H.M., Butler A.E., Dargham S.R., Latif A., Ahmed E.A., Hassan A., Atkin S.L. Relationship between total vitamin D metabolites and complications in patients with type 2 diabetes. Biomed. Rep. 2021;14:18. doi: 10.3892/br.2020.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Nadri G., Saxena S., Kaur A., Ahmad K., Garg P., Mahdi A.A., Akduman L., Gazdikova K., Caprnda M., Vesely P., et al. Correlation between vitamin D serum levels and severity of diabetic retinopathy in patients with type 2 diabetes mellitus. J. Endocrinol. Metab. Diabetes South Afr. 2021;26:82–88. doi: 10.1080/16089677.2021.1903170. [DOI] [Google Scholar]
- 164.Castillo-Oti J.M., Galvan-Manso A.I., Callejas-Herrero M.R., Vara-Gonzalez L.A., Salas-Herrera F., Munoz-Cacho P. Vitamin D Deficiency Is Significantly Associated with Retinopathy in Type 2 Diabetes Mellitus: A Case-Control Study. Nutrients. 2021;14:84. doi: 10.3390/nu14010084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Tomic M., Vrabec R., Ljubic S., Bulum T., Rahelic D. Plasma homocysteine is associated with nonproliferative retinopathy in patients with type 2 diabetes without renal disease. Diabetes Metab. Syndr. 2022;16:102355. doi: 10.1016/j.dsx.2021.102355. [DOI] [PubMed] [Google Scholar]
- 166.Xiao Y., Wei L., Xiong X., Yang M., Sun L. Association Between Vitamin D Status and Diabetic Complications in Patients With Type 2 Diabetes Mellitus: A Cross-Sectional Study in Hunan China. Front. Endocrinol. 2020;11:564738. doi: 10.3389/fendo.2020.564738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Reddy G.B., Sivaprasad M., Shalini T., Satyanarayana A., Seshacharyulu M., Balakrishna N., Viswanath K., Sahay M. Plasma vitamin D status in patients with type 2 diabetes with and without retinopathy. Nutrition. 2015;31:959–963. doi: 10.1016/j.nut.2015.01.012. [DOI] [PubMed] [Google Scholar]
- 168.Reheem R., Fattah M. Serum vitamin D and parathormone (PTH) concentrations as predictors of the development and severity of diabetic retinopathy. Alex. J. Med. 2013;49:119–123. doi: 10.1016/j.ajme.2012.08.006. [DOI] [Google Scholar]
- 169.Jee D., Han K., Kim E.C. Inverse association between high blood 25-hydroxyvitamin D levels and diabetic retinopathy in a representative Korean population. PLoS ONE. 2014;9:e115199. doi: 10.1371/journal.pone.0115199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Alele J.D., Luttrell L.M., Hollis B.W., Luttrell D.K., Hunt K.J., Group V.S. Relationship between vitamin D status and incidence of vascular events in the Veterans Affairs Diabetes Trial. Atherosclerosis. 2013;228:502–507. doi: 10.1016/j.atherosclerosis.2013.03.024. [DOI] [PubMed] [Google Scholar]
- 171.Alam U., Amjad Y., Chan A.W., Asghar O., Petropoulos I.N., Malik R.A. Vitamin D Deficiency Is Not Associated with Diabetic Retinopathy or Maculopathy. J. Diabetes Res. 2016;2016:6156217. doi: 10.1155/2016/6156217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Balbaba M., Ulas F., Erdag M., Yildirim H., Celiker U., Aydin S. Evaluation of aqueous humor and serum cortistatin levels in diabetic patients with and without diabetic retinopathy. Eur. J. Ophthalmol. 2021;31:638–642. doi: 10.1177/1120672119894847. [DOI] [PubMed] [Google Scholar]
- 173.Girard E., Nacher M., Bukasa-Kakamba J., Fahrasmane A., Adenis A., Massicard M., Drak Alsibai K., De Toffol B., Bekima R., Thelusme L., et al. Vitamin D Deficiency in Patients with Diabetes in French Guiana: Epidemiology and Relation with Microvascular and Macrovascular Complications. Nutrients. 2021;13:4302. doi: 10.3390/nu13124302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Bonakdaran S., Shoeibi N. Is there any correlation between vitamin D insufficiency and diabetic retinopathy? Int. J. Ophthalmol. 2015;8:326–331. doi: 10.3980/j.issn.2222-3959.2015.02.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Joergensen C., Hovind P., Schmedes A., Parving H.H., Rossing P. Vitamin D levels, microvascular complications, and mortality in type 1 diabetes. Diabetes Care. 2011;34:1081–1085. doi: 10.2337/dc10-2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Payne J.F., Ray R., Watson D.G., Delille C., Rimler E., Cleveland J., Lynn M.J., Tangpricha V., Srivastava S.K. Vitamin D insufficiency in diabetic retinopathy. Endocr. Pract. 2012;18:185–193. doi: 10.4158/EP11147.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Poon M., Craig M.E., Kaur H., Cusumano J., Sasongko M.B., Wong T.Y., Donaghue K.C. Vitamin D deficiency is not associated with changes in retinal geometric parameters in young people with type 1 diabetes. J. Diabetes Res. 2013;2013:280691. doi: 10.1155/2013/280691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Millen A.E., Sahli M.W., Nie J., LaMonte M.J., Lutsey P.L., Klein B.E., Mares J.A., Meyers K.J., Andrews C.A., Klein R. Adequate vitamin D status is associated with the reduced odds of prevalent diabetic retinopathy in African Americans and Caucasians. Cardiovasc. Diabetol. 2016;15:128. doi: 10.1186/s12933-016-0434-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Jung C.H., Kim K.J., Kim B.Y., Kim C.H., Kang S.K., Mok J.O. Relationship between vitamin D status and vascular complications in patients with type 2 diabetes mellitus. Nutr. Res. 2016;36:117–124. doi: 10.1016/j.nutres.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 180.Yi X., Sun J., Li L., Wei Q., Qian Y., Chen X., Ma L. 1,25-Dihydroxyvitamin D3 Deficiency is Involved in the Pathogenesis of Diabetic Retinopathy in the Uygur Population of China. IUBMB Life. 2016;68:445–451. doi: 10.1002/iub.1501. [DOI] [PubMed] [Google Scholar]
- 181.Ezhilarasi K., Dhamodharan U., Vijay V. BSMI single nucleotide polymorphism in vitamin D receptor gene is associated with decreased circulatory levels of serum 25-hydroxyvitamin D among micro and macrovascular complications of type 2 diabetes mellitus. Int. J. Biol. Macromol. 2018;116:346–353. doi: 10.1016/j.ijbiomac.2018.05.026. [DOI] [PubMed] [Google Scholar]
- 182.Zavorkova M., Vetvicka V., Richter J., Kral V., Liehnova I., Rajnohova D.L. Effects of Glucan and Vitamin D Supplementation on Obesity and Lipid Metabolism in Diabetic Retinopathy. Open Biochem. J. 2018;12:36–45. doi: 10.2174/1874091X01812010036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Karimi S., Movafaghi V., Arabi A., Shahraki T., Safi S. Effects of Oral Vitamin D Supplement Therapy on Clinical Outcomes of Intravitreal Bevacizumab in Diabetic Macular Edema. J. Ophthalmic. Vis. Res. 2021;16:34–41. doi: 10.18502/jovr.v16i1.8249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Wan T.T., Li X.F., Sun Y.M., Li Y.B., Su Y. Recent advances in understanding the biochemical and molecular mechanism of diabetic retinopathy. Biomed. Pharmacother. 2015;74:145–147. doi: 10.1016/j.biopha.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 185.Milne R., Brownstein S. Advanced glycation end products and diabetic retinopathy. Amino Acids. 2013;44:1397–1407. doi: 10.1007/s00726-011-1071-3. [DOI] [PubMed] [Google Scholar]
- 186.Norman A.W., Frankel J.B., Heldt A.M., Grodsky G.M. Vitamin D deficiency inhibits pancreatic secretion of insulin. Science. 1980;209:823–825. doi: 10.1126/science.6250216. [DOI] [PubMed] [Google Scholar]
- 187.Cade C., Norman A.W. Vitamin D3 improves impaired glucose tolerance and insulin secretion in the vitamin D-deficient rat in vivo. Endocrinology. 1986;119:84–90. doi: 10.1210/endo-119-1-84. [DOI] [PubMed] [Google Scholar]
- 188.Ren Z., Li W., Zhao Q., Ma L., Zhu J. The impact of 1,25-dihydroxy vitamin D3 on the expressions of vascular endothelial growth factor and transforming growth factor–beta(1) in the retinas of rats with diabetes. Diabetes Res. Clin. Pract. 2012;98:474–480. doi: 10.1016/j.diabres.2012.09.028. [DOI] [PubMed] [Google Scholar]
- 189.Zhang J., Upala S., Sanguankeo A. Relationship between vitamin D deficiency and diabetic retinopathy: A meta-analysis. Can. J. Ophthalmol. 2017;52:219–224. doi: 10.1016/j.jcjo.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 190.Zhang Y., Xia W., Lu P., Yuan H. The Association between VDR Gene Polymorphisms and Diabetic Retinopathy Susceptibility: A Systematic Review and Meta–Analysis. Biomed. Res. Int. 2016;2016:5305282. doi: 10.1155/2016/5305282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Sugden J.A., Davies J.I., Witham M.D., Morris A.D., Struthers A.D. Vitamin D improves endothelial function in patients with Type 2 diabetes mellitus and low vitamin D levels. Diabet. Med. 2008;25:320–325. doi: 10.1111/j.1464-5491.2007.02360.x. [DOI] [PubMed] [Google Scholar]
- 192.Jha P., Dolan L.M., Khoury P.R., Urbina E.M., Kimball T.R., Shah A.S. Low Serum Vitamin D Levels Are Associated with Increased Arterial Stiffness in Youth With Type 2 Diabetes. Diabetes Care. 2015;38:1551–1557. doi: 10.2337/dc15-0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Ertek S., Akgül E., Cicero A.F., Kütük U., Demirtaş S., Cehreli S., Erdoğan G. 25-Hydroxy vitamin D levels and endothelial vasodilator function in normotensive women. Arch. Med. Sci. 2012;8:47–52. doi: 10.5114/aoms.2012.27280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Tohari A.M., Almarhoun M., Alhasani R.H., Biswas L., Zhou X., Reilly J., Zeng Z., Shu X. Protection by vitamin D against high–glucose–induced damage in retinal pigment epithelial cells. Exp. Cell Res. 2020;392:112023. doi: 10.1016/j.yexcr.2020.112023. [DOI] [PubMed] [Google Scholar]
- 195.Sinha A., Hollingsworth K.G., Ball S., Cheetham T. Improving the vitamin D status of vitamin D deficient adults is associated with improved mitochondrial oxidative function in skeletal muscle. J. Clin. Endocrinol. Metab. 2013;98:E509–E513. doi: 10.1210/jc.2012-3592. [DOI] [PubMed] [Google Scholar]
- 196.Ye X., Zuo D., Yu L., Zhang L., Tang J., Cui C., Bao L., Zan K., Zhang Z., Yang X., et al. ROS/TXNIP pathway contributes to thrombin induced NLRP3 inflammasome activation and cell apoptosis in microglia. Biochem. Biophys. Res. Commun. 2017;485:499–505. doi: 10.1016/j.bbrc.2017.02.019. [DOI] [PubMed] [Google Scholar]
- 197.Lu L., Lu Q., Chen W., Li J., Li C., Zheng Z. Vitamin D(3) Protects against Diabetic Retinopathy by Inhibiting High–Glucose–Induced Activation of the ROS/TXNIP/NLRP3 Inflammasome Pathway. J. Diabetes Res. 2018;2018:8193523. doi: 10.1155/2018/8193523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Lee V., Rekhi E., Hoh Kam J., Jeffery G. Vitamin D rejuvenates aging eyes by reducing inflammation, clearing amyloid beta and improving visual function. Neurobiol. Aging. 2012;33:2382–2389. doi: 10.1016/j.neurobiolaging.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 199.Li Y.C., Kong J., Wei M., Chen Z.F., Liu S.Q., Cao L.P. 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin–angiotensin system. J. Clin. Investig. 2002;110:229–238. doi: 10.1172/JCI0215219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Burgess E.D., Hawkins R.G., Watanabe M. Interaction of 1,25-dihydroxyvitamin D and plasma renin activity in high renin essential hypertension. Am. J. Hypertens. 1990;3:903–905. doi: 10.1093/ajh/3.12.903. [DOI] [PubMed] [Google Scholar]
- 201.Talmor Y., Golan E., Benchetrit S., Bernheim J., Klein O., Green J., Rashid G. Calcitriol blunts the deleterious impact of advanced glycation end products on endothelial cells. Am. J. Physiol. Renal. Physiol. 2008;294:F1059–F1064. doi: 10.1152/ajprenal.00051.2008. [DOI] [PubMed] [Google Scholar]
- 202.Omidian M., Djalali M., Javanbakht M.H., Eshraghian M.R., Abshirini M., Omidian P., Alvandi E., Mahmoudi M. Effects of vitamin D supplementation on advanced glycation end products signaling pathway in T2DM patients: A randomized, placebo-controlled, double blind clinical trial. Diabetol. Metab. Syndr. 2019;11:86. doi: 10.1186/s13098-019-0479-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Yuan Y.F., Das S.K., Li M.Q. Vitamin D Ameliorates Impaired Wound Healing in Streptozotocin–Induced Diabetic Mice by Suppressing Endoplasmic Reticulum Stress. J. Diabetes Res. 2018;2018:1757925. doi: 10.1155/2018/1757925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Riek A.E., Oh J., Sprague J.E., Timpson A., de las Fuentes L., Bernal-Mizrachi L., Schechtman K.B., Bernal-Mizrachi C. Vitamin D suppression of endoplasmic reticulum stress promotes an antiatherogenic monocyte/macrophage phenotype in type 2 diabetic patients. J. Biol. Chem. 2012;287:38482–38494. doi: 10.1074/jbc.M112.386912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Jeremy M., Gurusubramanian G., Roy V.K. Vitamin D3 treatment regulates apoptosis, antioxidant defense system, and DNA integrity in the epididymal sperm of an aged rat model. Mol. Reprod. Dev. 2019;86:1951–1962. doi: 10.1002/mrd.23280. [DOI] [PubMed] [Google Scholar]
- 206.Van der Wijk A.E., Hughes J.M., Klaassen I., Van Noorden C.J.F., Schlingemann R.O. Is leukostasis a crucial step or epiphenomenon in the pathogenesis of diabetic retinopathy? J. Leukoc. Biol. 2017;102:993–1001. doi: 10.1189/jlb.3RU0417-139. [DOI] [PubMed] [Google Scholar]
- 207.Sabbaghi H., Daftarian N., Suri F., Mirrahimi M., Madani S., Sheikhtaheri A., Khorrami F., Saviz P., Nejad M.Z., Tivay A., et al. The First Inherited Retinal Disease Registry in Iran: Research Protocol and Results of a Pilot Study. Arch. Iran. Med. 2020;23:445–454. doi: 10.34172/aim.2020.41. [DOI] [PubMed] [Google Scholar]
- 208.Papas E.B. The global prevalence of dry eye disease: A Bayesian view. Ophthalmic Physiol. Opt. 2021;41:1254–1266. doi: 10.1111/opo.12888. [DOI] [PubMed] [Google Scholar]
- 209.Kanellopoulos A.J., Asimellis G. In pursuit of objective dry eye screening clinical techniques. Eye Vis. 2016;3:1. doi: 10.1186/s40662-015-0032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Kastelan S., Tomic M., Salopek-Rabatic J., Novak B. Diagnostic procedures and management of dry eye. Biomed. Res. Int. 2013;2013:309723. doi: 10.1155/2013/309723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Bang B., Asmussen K., Sorensen O.H., Oxholm P. Reduced 25-hydroxyvitamin D levels in primary Sjogren’s syndrome. Correlations to disease manifestations. Scand. J. Rheumatol. 1999;28:180–183. doi: 10.1080/03009749950154266. [DOI] [PubMed] [Google Scholar]
- 212.Galor A., Gardener H., Pouyeh B., Feuer W., Florez H. Effect of a Mediterranean dietary pattern and vitamin D levels on Dry Eye syndrome. Cornea. 2014;33:437–441. doi: 10.1097/ICO.0000000000000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Kurtul B.E., Ozer P.A., Aydinli M.S. The association of vitamin D deficiency with tear break-up time and Schirmer testing in non-Sjogren dry eye. Eye. 2015;29:1081–1084. doi: 10.1038/eye.2015.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Yildirim P., Garip Y., Karci A.A., Guler T. Dry eye in vitamin D deficiency: More than an incidental association. Int. J. Rheum. Dis. 2016;19:49–54. doi: 10.1111/1756-185X.12727. [DOI] [PubMed] [Google Scholar]
- 215.Jin K.W., Ro J.W., Shin Y.J., Hyon J.Y., Wee W.R., Park S.G. Correlation of vitamin D levels with tear film stability and secretion in patients with dry eye syndrome. Acta Ophthalmol. 2017;95:e230–e235. doi: 10.1111/aos.13241. [DOI] [PubMed] [Google Scholar]
- 216.Yoon S.Y., Bae S.H., Shin Y.J., Park S.G., Hwang S.H., Hyon J.Y., Wee W.R. Low Serum 25-Hydroxyvitamin D Levels Are Associated with Dry Eye Syndrome. PLoS ONE. 2016;11:e0147847. doi: 10.1371/journal.pone.0147847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Shetty R., Sethu S., Deshmukh R., Deshpande K., Ghosh A., Agrawal A., Shroff R. Corneal Dendritic Cell Density Is Associated with Subbasal Nerve Plexus Features, Ocular Surface Disease Index, and Serum Vitamin D in Evaporative Dry Eye Disease. Biomed. Res. Int. 2016;2016:4369750. doi: 10.1155/2016/4369750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Shetty R., Sethu S., Chevour P., Deshpande K., Pahuja N., Nagaraja H., Pindipapanahalli N., Ghosh A. Lower Vitamin D Level and Distinct Tear Cytokine Profile Were Observed in Patients with Mild Dry Eye Signs but Exaggerated Symptoms. Transl. Vis. Sci. Technol. 2016;5:16. doi: 10.1167/tvst.5.6.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Bae S.H., Shin Y.J., Kim H.K., Hyon J.Y., Wee W.R., Park S.G. Vitamin D Supplementation for Patients with Dry Eye Syndrome Refractory to Conventional Treatment. Sci. Rep. 2016;6:33083. doi: 10.1038/srep33083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Meng Y.F., Lu J., Xing Q., Tao J.J., Xiao P. Lower Serum Vitamin D Level Was Associated with Risk of Dry Eye Syndrome. Med. Sci. Monit. 2017;23:2211–2216. doi: 10.12659/MSM.901857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Demirci G., Karaman Erdur S., Ozsutcu M., Eliacik M., Olmuscelik O., Aydin R., Kocabora M.S. Dry Eye Assessment in Patients With Vitamin D Deficiency. Eye Contact Lens. 2018;44((Suppl. S1)):S62–S65. doi: 10.1097/ICL.0000000000000325. [DOI] [PubMed] [Google Scholar]
- 222.Khamar P., Nair A.P., Shetty R., Vaidya T., Subramani M., Ponnalagu M., Dhamodaran K., D’Souza S., Ghosh A., Pahuja N., et al. Dysregulated Tear Fluid Nociception–Associated Factors, Corneal Dendritic Cell Density, and Vitamin D Levels in Evaporative Dry Eye. Investig. Ophthalmol. Vis. Sci. 2019;60:2532–2542. doi: 10.1167/iovs.19-26914. [DOI] [PubMed] [Google Scholar]
- 223.Lee J.H., Kim S.J., Byun Y.S., Lee J., Park S.H., Chung S.H. The Association of Serum Vitamin D Level With the Severity of Dry Eye Parameters in Primary Sjogren Syndrome. Cornea. 2020;39:702–705. doi: 10.1097/ICO.0000000000002234. [DOI] [PubMed] [Google Scholar]
- 224.Fukuoka S., Arita R., Mizoguchi T., Kawashima M., Koh S., Shirakawa R., Suzuki T., Sasaki S., Morishige N. Relation of Dietary Fatty Acids and Vitamin D to the Prevalence of Meibomian Gland Dysfunction in Japanese Adults: The Hirado–Takushima Study. J. Clin. Med. 2021;10:350. doi: 10.3390/jcm10020350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Aksoy Aydemir G., Aydemir E., Asik A. Changes in Tear Meniscus Analysis of Children Who Have Type 1 Diabetes Mellitus, With and Without Vitamin D Deficiency. Cornea. 2021 doi: 10.1097/ICO.0000000000002908. [DOI] [PubMed] [Google Scholar]
- 226.Dikci S., Akatli A.N., Yildirim T. Conjunctival impression cytology and tear–film changes in cases with vitamin D deficiency. Int. Ophthalmol. 2020;40:1687–1694. doi: 10.1007/s10792-020-01336-1. [DOI] [PubMed] [Google Scholar]
- 227.Jee D., Kang S., Yuan C., Cho E., Arroyo J.G., The Epidemiologic Survey Committee of the Korean Ophthalmologic Society Serum 25-Hydroxyvitamin D Levels and Dry Eye Syndrome: Differential Effects of Vitamin D on Ocular Diseases. PLoS ONE. 2016;11:e0149294. doi: 10.1371/journal.pone.0149294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Kim M.J., Hwang H.R., Kim Y.J., Lee S.Y., Lee J.G., Jeong D.W., Kim Y.H. Association Between Serum 25-Hydroxyvitamin D Levels and Dry Eye in Korean Adults: A Study Based on Korean National Health and Nutrition Examination Survey, 2010–2011. Korean J. Fam. Med. 2017;38:81–85. doi: 10.4082/kjfm.2017.38.2.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Jeon D.H., Yeom H., Yang J., Song J.S., Lee H.K., Kim H.C. Are Serum Vitamin D Levels Associated With Dry Eye Disease? Results From the Study Group for Environmental Eye Disease. J. Prev. Med. Public Health. 2017;50:369–376. doi: 10.3961/jpmph.17.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Arman A., Petricli I.S., Kara C., Koksal Z., Gucel F. The relationship between serum vitamin D levels and dry eye syndrome in postmenopausal women. Ann. Clin. Anal. Med. 2020;11:91–94. [Google Scholar]
- 231.Arita R., Kawashima M., Ito M., Tsubota K. Clinical safety and efficacy of vitamin D3 analog ointment for treatment of obstructive meibomian gland dysfunction. BMC Ophthalmol. 2017;17:84. doi: 10.1186/s12886-017-0482-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Kizilgul M., Kan S., Ozcelik O., Beysel S., Apaydin M., Ucan B., Cakal E. Vitamin D Replacement Improves Tear Osmolarity in Patients with Vitamin D Deficiency. Semin. Ophthalmol. 2018;33:589–594. doi: 10.1080/08820538.2017.1358752. [DOI] [PubMed] [Google Scholar]
- 233.Yang C.H., Albietz J., Harkin D.G., Kimlin M.G., Schmid K.L. Impact of oral vitamin D supplementation on the ocular surface in people with dry eye and/or low serum vitamin D. Cont. Lens Anterior Eye. 2018;41:69–76. doi: 10.1016/j.clae.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 234.Hwang J.S., Lee Y.P., Shin Y.J. Vitamin D Enhances the Efficacy of Topical Artificial Tears in Patients With Dry Eye Disease. Cornea. 2019;38:304–310. doi: 10.1097/ICO.0000000000001822. [DOI] [PubMed] [Google Scholar]
- 235.Watts P., Sahai A., Kumar P.R., Shamshad M.A., Trivedi G.K., Tyagi L. A prospective study to assess the role of vitamin D individually and in combination with cyclosporine in the treatment of dry eye in patients with deficient serum 25(OH)D levels. Indian J. Ophthalmol. 2020;68:1020–1026. doi: 10.4103/ijo.IJO_1492_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Karaca E.E., Kemer O.E., Ozek D., Berker D., Imga N.N. Clinical outcomes of ocular surface in patients treated with vitamin D oral replacement. Arq. Bras. Oftalmol. 2020;83:312–317. doi: 10.5935/0004-2749.20200043. [DOI] [PubMed] [Google Scholar]
- 237.Eslampoor A., Najjaran M., Arjmand Askari E., Zarei-Ghanavati S., Ziaei M. Effect of oral vitamin D supplementation on dry eye disease patients with vitamin D deficiency. Clin. Exp. Optom. 2022:1–6. doi: 10.1080/08164622.2022.2033601. [DOI] [PubMed] [Google Scholar]
- 238.Jain N., Sharma P., Chouhan J.K. A study of the association between Vitamin D deficiency and Dry Eye Syndrome (DES) in the Indian population. Indian J. Ophthalmol. 2022;70:500–504. doi: 10.4103/ijo.IJO_1921_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Shab-Bidar S., Neyestani T.R., Djazayery A., Eshraghian M.R., Houshiarrad A., Gharavi A., Kalayi A., Shariatzadeh N., Zahedirad M., Khalaji N., et al. Regular consumption of vitamin D-fortified yogurt drink (Doogh) improved endothelial biomarkers in subjects with type 2 diabetes: A randomized double-blind clinical trial. BMC Med. 2011;9:125. doi: 10.1186/1741-7015-9-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Nagpal S., Na S., Rathnachalam R. Noncalcemic actions of vitamin D receptor ligands. Endocr. Rev. 2005;26:662–687. doi: 10.1210/er.2004-0002. [DOI] [PubMed] [Google Scholar]
- 241.Froicu M., Weaver V., Wynn T.A., McDowell M.A., Welsh J.E., Cantorna M.T. A crucial role for the vitamin D receptor in experimental inflammatory bowel diseases. Mol. Endocrinol. 2003;17:2386–2392. doi: 10.1210/me.2003-0281. [DOI] [PubMed] [Google Scholar]
- 242.Fattori E., Cappelletti M., Costa P., Sellitto C., Cantoni L., Carelli M., Faggioni R., Fantuzzi G., Ghezzi P., Poli V. Defective inflammatory response in interleukin 6-deficient mice. J. Exp. Med. 1994;180:1243–1250. doi: 10.1084/jem.180.4.1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Bascom A., Redfern R.L., Reins R.Y. Characterization of Vitamin D Levels in Ocular Surface Tissues and their Association with Dry Eye Disease. Investig. Ophthalmol. Vis. Sci. 2019;60:1414. [Google Scholar]
- 244.Meng Y.F., Xin Q., Lu J., Xiao P., Li J. Association Between Single Nucleotide Polymorphisms in the Vitamin D Receptor and Incidence of Dry Eye Disease in Chinese Han Population. Med. Sci. Monit. 2019;25:4759–4765. doi: 10.12659/MSM.915434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Sadaka A., Nguyen K., Malik A., Brito R., Berry S., Lee A.G. Vitamin D and Selenium in a Thyroid Eye Disease Population in Texas. Neuroophthalmology. 2019;43:291–294. doi: 10.1080/01658107.2019.1566382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Heisel C.J., Riddering A.L., Andrews C.A., Kahana A. Serum Vitamin D Deficiency Is an Independent Risk Factor for Thyroid Eye Disease. Ophthalmic Plast Reconstr. Surg. 2020;36:17–20. doi: 10.1097/IOP.0000000000001437. [DOI] [PubMed] [Google Scholar]
- 247.Planck T., Shahida B., Malm J., Manjer J. Vitamin D in Graves Disease: Levels, Correlation with Laboratory and Clinical Parameters, and Genetics. Eur. Thyroid J. 2018;7:27–33. doi: 10.1159/000484521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Nian H., Liang D., Zuo A., Wei R., Shao H., Born W.K., Kaplan H.J., Sun D. Characterization of autoreactive and bystander IL-17+ T cells induced in immunized C57BL/6 mice. Investig. Ophthalmol. Vis. Sci. 2012;53:897–905. doi: 10.1167/iovs.11-8297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Tang J., Zhou R., Luger D., Zhu W., Silver P.B., Grajewski R.S., Su S.B., Chan C.-C., Adorini L., Caspi R.R. Calcitriol Suppresses Antiretinal Autoimmunity through Inhibitory Effects on the Th17 Effector Response. J. Immunol. 2009;182:4624–4632. doi: 10.4049/jimmunol.0801543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.González M.M., Solano M.M., Porco T.C., Oldenburg C.E., Acharya N.R., Lin S.C., Chan M.F. Epidemiology of uveitis in a US population-based study. J. Ophthalmic Inflamm. Infect. 2018;8:6. doi: 10.1186/s12348-018-0148-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Llop S.M., Davoudi S., Stanwyck L.K., Sathe S., Tom L., Ahmadi T., Grotting L., Papaliodis G.N., Sobrin L. Association of Low Vitamin D Levels with Noninfectious Uveitis and Scleritis. Ocul. Immunol. Inflamm. 2019;27:602–609. doi: 10.1080/09273948.2018.1434208. [DOI] [PubMed] [Google Scholar]
- 252.Sobrin L., Stanwyck L.K., Pan W., Hubbard R.A., Kempen J.H., VanderBeek B.L. Association of Hypovitaminosis D With Increased Risk of Uveitis in a Large Health Care Claims Database. JAMA Ophthalmol. 2018;136:548–552. doi: 10.1001/jamaophthalmol.2018.0642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Mitulescu T.C., Stavaru C., Voinea L.M., Banica L.M., Matache C., Predeteanu D. The role of Vitamin D in immuno–inflammatory responses in Ankylosing Spondylitis patients with and without Acute Anterior Uveitis. J. Med. Life. 2016;9:26–33. [PMC free article] [PubMed] [Google Scholar]
- 254.Dadaci Z., Cetinkaya S., Oncel Acir N., Oncel M., Borazan M. Serum Vitamin D Levels in Patients with Acute Anterior Uveitis. Ocul. Immunol. Inflamm. 2017;25:492–496. doi: 10.3109/09273948.2016.1139735. [DOI] [PubMed] [Google Scholar]
- 255.Grotting L.A., Davoudi S., Palenzuela D., Papaliodis G.N., Sobrin L. Association of Low Vitamin D Levels With Noninfectious Anterior Uveitis. JAMA Ophthalmol. 2017;135:150–153. doi: 10.1001/jamaophthalmol.2016.4888. [DOI] [PubMed] [Google Scholar]
- 256.Yi X., Yang P., Sun M., Yang Y., Li F. Decreased 1,25-Dihydroxyvitamin D3 level is involved in the pathogenesis of Vogt-Koyanagi-Harada (VKH) disease. Mol. Vis. 2011;17:673–679. [PMC free article] [PubMed] [Google Scholar]
- 257.Rohmer J., Hadjadj J., Bouzerara A., Salah S., Paule R., Groh M., Blanche P., Mouthon L., Monnet D., Le Jeunne C., et al. Serum 1,25(OH)2 Vitamin D and 25(OH) Vitamin D Ratio for the Diagnosis of Sarcoidosis–Related Uveitis. Ocul. Immunol. Inflamm. 2020;28:341–347. doi: 10.1080/09273948.2018.1537399. [DOI] [PubMed] [Google Scholar]
- 258.Sengler C., Zink J., Klotsche J., Niewerth M., Liedmann I., Horneff G., Kessel C., Ganser G., Thon A., Haas J.P., et al. Vitamin D deficiency is associated with higher disease activity and the risk for uveitis in juvenile idiopathic arthritis—Data from a German inception cohort. Arthritis Res. Ther. 2018;20:276. doi: 10.1186/s13075-018-1765-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Chiu Z.K., Lim L.L., Rogers S.L., Hall A.J. Patterns of Vitamin D Levels and Exposures in Active and Inactive Noninfectious Uveitis Patients. Ophthalmology. 2020;127:230–237. doi: 10.1016/j.ophtha.2019.06.030. [DOI] [PubMed] [Google Scholar]
- 260.Cooper J.D., Smyth D.J., Walker N.M., Stevens H., Burren O.S., Wallace C., Greissl C., Ramos-Lopez E., Hypponen E., Dunger D.B., et al. Inherited variation in vitamin D genes is associated with predisposition to autoimmune disease type 1 diabetes. Diabetes. 2011;60:1624–1631. doi: 10.2337/db10-1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Sawcer S., Hellenthal G., Pirinen M., Spencer C.C., Patsopoulos N.A., Moutsianas L., Dilthey A., Su Z., Freeman C., Hunt S.E., et al. Genetic risk and a primary role for cell–mediated immune mechanisms in multiple sclerosis. Nature. 2011;476:214–219. doi: 10.1038/nature10251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Pillar S., Amer R. The association between vitamin D and uveitis: A comprehensive review. Surv. Ophthalmol. 2021;67:321–330. doi: 10.1016/j.survophthal.2021.07.006. [DOI] [PubMed] [Google Scholar]
- 263.Fang J., Hou S., Xiang Q., Qi J., Yu H., Shi Y., Zhou Y., Kijlstra A., Yang P. Polymorphisms in genetics of vitamin D metabolism confer susceptibility to ocular Behcet disease in a Chinese Han population. Am. J. Ophthalmol. 2014;157:488–494.e6. doi: 10.1016/j.ajo.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 264.Audo I., Darjatmoko S.R., Schlamp C.L., Lokken J.M., Lindstrom M.J., Albert D.M., Nickells R.W. Vitamin D analogues increase p53, p21, and apoptosis in a xenograft model of human retinoblastoma. Investig. Ophthalmol. Vis. Sci. 2003;44:4192–4199. doi: 10.1167/iovs.02-1198. [DOI] [PubMed] [Google Scholar]
- 265.Albert D.M., Kumar A., Strugnell S.A., Darjatmoko S.R., Lokken J.M., Lindstrom M.J., Patel S. Effectiveness of vitamin D analogues in treating large tumors and during prolonged use in murine retinoblastoma models. Arch. Ophthalmol. 2004;122:1357–1362. doi: 10.1001/archopht.122.9.1357. [DOI] [PubMed] [Google Scholar]
- 266.Mejia-Rodriguez F., Flores-Aldana M.E., Quezada-Sanchez A.D., Shamah-Levy T., Villalpando S., Contreras-Manzano A., Bhatt-Carreno S., Orjuela-Grimm M. Association between Predictors of Vitamin D Serum Levels and Risk of Retinoblastoma in Children: A Case-Control Study. Nutrients. 2021;13:2510. doi: 10.3390/nu13082510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Orjuela-Grimm M., Carreno S.B., Liu X., Ruiz A., Medina P., Ramirez Ortiz M.A., Rendon J.R., Molina N.C.L., Pinilla H., Hinojosa D., et al. Sunlight exposure in infancy decreases risk of sporadic retinoblastoma, extent of intraocular disease. Cancer Rep. 2021;4:e1409. doi: 10.1002/cnr2.1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Schündeln M.M., Hauffa P.K., Bauer J.J., Temming P., Sauerwein W., Biewald E., Bornfeld N., Hauffa B.P., Grasemann C. Pediatric Survivors of Retinoblastoma Are at Risk for Altered Bone Metabolism After Chemotherapy Treatment Early in Life. Pediatr. Hematol. Oncol. 2015;32:455–466. doi: 10.3109/08880018.2015.1048912. [DOI] [PubMed] [Google Scholar]
- 269.Liu Y.C., Wilkins M., Kim T., Malyugin B., Mehta J.S. Cataracts. Lancet. 2017;390:600–612. doi: 10.1016/S0140-6736(17)30544-5. [DOI] [PubMed] [Google Scholar]
- 270.Delcourt C., Cougnard-Gregoire A., Boniol M., Carriere I., Dore J.F., Delyfer M.N., Rougier M.B., Le Goff M., Dartigues J.F., Barberger-Gateau P., et al. Lifetime exposure to ambient ultraviolet radiation and the risk for cataract extraction and age-related macular degeneration: The Alienor Study. Investig. Ophthalmol. Vis. Sci. 2014;55:7619–7627. doi: 10.1167/iovs.14-14471. [DOI] [PubMed] [Google Scholar]
- 271.Zhu M., Yu J., Gao Q., Wang Y., Hu L., Zheng Y., Wang F., Liu Y. The relationship between disability–adjusted life years of cataracts and ambient erythemal ultraviolet radiation in China. J. Epidemiol. 2015;25:57–65. doi: 10.2188/jea.JE20140017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Yu J.M., Yang D.Q., Wang H., Xu J., Gao Q., Hu L.W., Wang F., Wang Y., Yan Q.C., Zhang J.S., et al. Prevalence and risk factors of lens opacities in rural populations living at two different altitudes in China. Int. J. Ophthalmol. 2016;9:610–616. doi: 10.18240/ijo.2016.04.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Vinson J.A. Oxidative stress in cataracts. Pathophysiology. 2006;13:151–162. doi: 10.1016/j.pathophys.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 274.Park S., Choi N.K. Serum 25-hydroxyvitamin D and Age-Related Cataract. Ophthalmic Epidemiol. 2017;24:281–286. doi: 10.1080/09286586.2017.1281427. [DOI] [PubMed] [Google Scholar]
- 275.Jee D., Kim E.C. Association between serum 25-hydroxyvitamin D levels and age-related cataracts. J. Cataract Refract. Surg. 2015;41:1705–1715. doi: 10.1016/j.jcrs.2014.12.052. [DOI] [PubMed] [Google Scholar]
- 276.Abdellah M.M., Mohamed Mostafa E., Salama E.H., Roshdy Mohamed E. Association of Serum 25-Hydroxyl Vitamin D Deficiency and Age-Related Cataract: A Case-Control Study. J. Ophthalmol. 2019;2019:9312929. doi: 10.1155/2019/9312929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Atalay K., Gezer Savur F., Kirgiz A., Erdogan Kaldirim H., Zengi O. Serum Vitamin D Levels in Different Morphologic Forms of Age Related Cataract. Acta Endocrinol. 2020;16:178–182. doi: 10.4183/aeb.2020.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Oktem C., Aslan F. Vitamin D Levels in Young Adult Cataract Patients: A Case-Control Study. Ophthalmic Res. 2021;64:116–120. doi: 10.1159/000509602. [DOI] [PubMed] [Google Scholar]
- 279.Brown C.J., Akaichi F. Vitamin D deficiency and posterior subcapsular cataract. Clin. Ophthalmol. 2015;9:1093–1098. doi: 10.2147/OPTH.S84790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Rao P., Millen A.E., Meyers K.J., Liu Z., Voland R., Sondel S., Tinker L., Wallace R.B., Blodi B.A., Binkley N., et al. The Relationship Between Serum 25-Hydroxyvitamin D Levels and Nuclear Cataract in the Carotenoid Age-Related Eye Study (CAREDS), an Ancillary Study of the Women’s Health Initiative. Investig. Ophthalmol. Vis. Sci. 2015;56:4221–4230. doi: 10.1167/iovs.15-16835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Jee D., Kim E.C., Cho E., Arroyo J.G. Positive Association between Blood 25-Hydroxyvitamin D Levels and Pterygium after Control for Sunlight Exposure. PLoS ONE. 2016;11:e0157501. doi: 10.1371/journal.pone.0157501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Samadi Aidenloo N., Motarjemizadeh Q., Moradi Nahriq S. Serum concentrations of 25-hydroxyvitamin D and different subtypes of age-related cataract; a case-control study. Immunopathol. Persa. 2022;8:e16. doi: 10.34172/ipp.2022.16. [DOI] [Google Scholar]
- 283.Cho M.C., Kim R.B., Ahn J.Y., Yoo W.S., Kim S.J. Aqueous humor and serum 25-Hydroxyvitamin D levels in patients with cataracts. BMC Ophthalmol. 2020;20:6. doi: 10.1186/s12886-019-1293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Karatas Durusoy G., Karakucuk Y., Tulu Aygun B., Solmaz B. Serum Vitamin D Level and Body Mass Index in Children with Vernal Keratoconjunctivitis. Beyoglu Eye J. 2020;5:102–107. doi: 10.14744/bej.2020.75047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Bozkurt B., Artac H., Ozdemir H., Ünlü A., Bozkurt M.K., Irkec M. Serum Vitamin D Levels in Children with Vernal Keratoconjunctivitis. Ocul. Immunol. Inflamm. 2018;26:435–439. doi: 10.1080/09273948.2016.1235714. [DOI] [PubMed] [Google Scholar]
- 286.Zicari A.M., Cafarotti A., Occasi F., Lollobrigida V., Nebbioso M., Pecorella I., De Castro G., Spalice A., Loffredo L., Villa M.P., et al. Vitamin D levels in children affected by vernal keratoconjunctivitis. Curr. Med. Res. Opin. 2017;33:269–274. doi: 10.1080/03007995.2016.1254602. [DOI] [PubMed] [Google Scholar]
- 287.Sorkhabi R., Ahoor M.H., Ghorbanihaghjo A., Jafari S. Serum vitamin D levels in patients with vernal keratoconjunctivitis and its relationship with disease severity. Eur. J. Ophthalmol. 2021;31:3259–3264. doi: 10.1177/1120672120978886. [DOI] [PubMed] [Google Scholar]
- 288.Aslan M.G., Findik H., Okutucu M., Aydin E., Oruç Y., Arpa M., Uzun F. Serum 25-Hydroxy Vitamin D, Vitamin B12, and Folic Acid Levels in Progressive and Nonprogressive Keratoconus. Cornea. 2021;40:334–341. doi: 10.1097/ICO.0000000000002475. [DOI] [PubMed] [Google Scholar]
- 289.Akkaya S., Ulusoy D.M. Serum Vitamin D Levels in Patients with Keratoconus. Ocul. Immunol. Inflamm. 2020;28:348–353. doi: 10.1080/09273948.2019.1604002. [DOI] [PubMed] [Google Scholar]
- 290.Zarei-Ghanavati S., Yahaghi B., Hassanzadeh S., Mobarhan M.G., Hakimi H.R., Eghbali P. Serum 25-Hydroxyvitamin D, Selenium, Zinc and Copper in Patients with Keratoconus. J. Curr. Ophthalmol. 2020;32:26–31. doi: 10.1016/j.joco.2019.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Epstein D., Kvanta A., Lindqvist P.G. Vitamin D Deficiency in Patients with Central Retinal Vein Occlusion: A Case Control Study. Curr. Eye Res. 2017;42:448–451. doi: 10.1080/02713683.2016.1188117. [DOI] [PubMed] [Google Scholar]
- 292.Oli A., Joshi D. Serum vitamin D levels in Indian patients with retinal venous occlusions. Saudi J. Ophthalmol. 2017;31:76–79. doi: 10.1016/j.sjopt.2017.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Gao M., Yao X., Ding J., Hong R., Wu Y., Huang H., Zhuang L., Li Z., Wang Y., Zhang Y., et al. Low levels of vitamin D and the relationship between vitamin D and Th2 axis–related cytokines in neuromyelitis optica spectrum disorders. J. Clin. Neurosci. 2019;61:22–27. doi: 10.1016/j.jocn.2018.11.024. [DOI] [PubMed] [Google Scholar]
- 294.Jitprapaikulsan J., Siritho S., Prayoonwiwat N. Vitamin D level status in Thai neuromyelitis optica patients. J. Neuroimmunol. 2016;295–296:75–78. doi: 10.1016/j.jneuroim.2016.03.016. [DOI] [PubMed] [Google Scholar]
- 295.Kusumadewi W., Imran D., Witjaksono F., Pakasi T.A., Rusmana A.I., Pangeran D., Marwadhani S.S., Maharani K., Estiasari R. Low vitamin D-25(OH) level in Indonesian multiple sclerosis and neuromyelitis optic patients. Mult. Scler. Relat. Disord. 2018;25:329–333. doi: 10.1016/j.msard.2018.08.030. [DOI] [PubMed] [Google Scholar]
- 296.Goksugur S.B., Erdurmus M., Bekdas M., Erkocoglu M., Agca S., Tosun M., Goksugur N., Demircioglu F. Tear and serum vitamin D levels in children with allergic rhinoconjunctivitis. Allergol. Immunopathol. 2015;43:533–537. doi: 10.1016/j.aller.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 297.Al-wailmi F.K., Shah S.I.A., Al-Mazaideh G.M., Sikandar M.Z. Serum Vitamin D and Immunoglobulin E Levels in Patients With Seasonal Allergic Conjunctivitis. IIUM Med. J. Malays. 2021;20 doi: 10.31436/imjm.v20i3.1756. [DOI] [Google Scholar]
- 298.Yenigun A., Dadaci Z., Oncel M. Plasma vitamin D levels of patients with allergic rhino–conjunctivitis with positive skin prick test. Am. J. Rhinol. Allergy. 2015;29:e46–e49. doi: 10.2500/ajra.2015.29.4164. [DOI] [PubMed] [Google Scholar]
- 299.Dadaci Z., Borazan M., Kiyici A., Oncel Acir N. Plasma vitamin D and serum total immunoglobulin E levels in patients with seasonal allergic conjunctivitis. Acta Ophthalmol. 2014;92:e443–e446. doi: 10.1111/aos.12398. [DOI] [PubMed] [Google Scholar]
- 300.Arikan S., Kamis F. Effect of vitamin D deficiency on spatial contrast sensitivity function. Clin. Exp. Optom. 2021:1–7. doi: 10.1080/08164622.2021.1969212. [DOI] [PubMed] [Google Scholar]
- 301.Ozturk E., Cankaya C. Effect of Vitamin D Deficiency on Contrast Sensitivity Function. Curr. Eye Res. 2020;45:1619–1624. doi: 10.1080/02713683.2020.1781194. [DOI] [PubMed] [Google Scholar]
- 302.Aksoy Aydemir G., Yetkin E., Aydemir E., Bolu S., Asik A. Changes in the macular choroidal thickness of children who have type–1 diabetes mellitus, with and without vitamin D deficiency. Int. Ophthalmol. 2022 doi: 10.1007/s10792-021-02185-2. in press. [DOI] [PubMed] [Google Scholar]
- 303.Vural E., Hazar L., Çağlayan M., Şeker Ö., Çelebi A.R.C. Peripapillary choroidal thickness in patients with vitamin D deficiency. Eur. J. Ophthalmol. 2021;31:578–583. doi: 10.1177/1120672120902025. [DOI] [PubMed] [Google Scholar]
- 304.Öncül H., Alakus M.F., Çağlayan M., Öncül F.Y., Dag U., Arac E. Changes in choroidal thickness after vitamin D supplementation in patients with vitamin D deficiency. Can. J. Ophthalmol. 2020;55:486–491. doi: 10.1016/j.jcjo.2020.06.014. [DOI] [PubMed] [Google Scholar]
- 305.Cankaya C., Cumurcu T., Gunduz A. Corneal endothelial changes in patients with vitamin D deficiency. Indian J. Ophthalmol. 2018;66:1256. doi: 10.4103/ijo.IJO_238_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Graffe A., Beauchet O., Fantino B., Milea D., Annweiler C. Vitamin D and Macular Thickness in the Elderly: An Optical Coherence Tomography Study. Investig. Ophthalmol. Vis. Sci. 2014;55:5298–5303. doi: 10.1167/iovs.14-13918. [DOI] [PubMed] [Google Scholar]
- 307.Kara N., Ceri S. Vitamin D level in patients with pterygium. Arq. Bras. Oftalmol. 2017;80:229–233. doi: 10.5935/0004-2749.20170056. [DOI] [PubMed] [Google Scholar]
- 308.Lee Y.B., Kim S.Y., Park Y.G., Han K.D., Kim J.W., Chae H.S., Lee Y.C. Evaluation of socioeconomic status as a risk factor of pterygium using the Korean National Health and Nutrition Examination Survey 2010 to 2011: A STROBE–compliant article. Medicine. 2017;96:e6343. doi: 10.1097/MD.0000000000006343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Maxia C., Murtas D., Corrias M., Zucca I., Minerba L., Piras F., Marinelli C., Perra M.T. Vitamin D and vitamin D receptor in patients with ophthalmic pterygium. Eur. J. Histochem. 2017;61:2837. doi: 10.4081/ejh.2017.2837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Ornek N., Ogurel T., Kisa U. Tear Fluid and Serum Vitamin D Concentrations in Unilateral Pterygium. Optom. Vis. Sci. 2021;98:170–174. doi: 10.1097/OPX.0000000000001640. [DOI] [PubMed] [Google Scholar]
- 311.Droutsas K., Sekundo W. Epidemiology of pterygium. A review. Ophthalmologe. 2010;107:511–512, 514–516. doi: 10.1007/s00347-009-2101-3. [DOI] [PubMed] [Google Scholar]
- 312.Singh S.K. Pterygium: Epidemiology prevention and treatment. Community Eye Health. 2017;30:S5–S6. [PMC free article] [PubMed] [Google Scholar]
- 313.Ghiglioni D.G., Bruschi G., Gandini S., Osnaghi S., Peroni D., Marchisio P. Vitamin D serum levels in children with vernal keratoconjunctivitis and disease control. Int. J. Immunopathol. Pharmacol. 2019;33:1–5. doi: 10.1177/2058738419833468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Chen L., Chen X., Xiang Q., Zheng Y., Pi L., Liu Q., Xiao J., Ke N., Fang J. Prevalence of Low Serum Vitamin A Levels in Young Children with Chalazia in Southwest China. Am. J. Ophthalmol. 2014;157:1103–1108.e2. doi: 10.1016/j.ajo.2014.02.020. [DOI] [PubMed] [Google Scholar]
- 315.Kabataş E.U., Dinlen N.F., Zenciroğlu A., Dilli D., Beken S., Okumuş N. Relationship between serum 25-hydroxy vitamin D levels and retinopathy of prematurity. Scott. Med. J. 2017;62:129–135. doi: 10.1177/0036933017701867. [DOI] [PubMed] [Google Scholar]
- 316.Mutlu U., Ikram M.A., Hofman A., de Jong P., Uitterlinden A.G., Klaver C.C.W., Ikram M.K. Vitamin D and retinal microvascular damage: The Rotterdam Study. Medicine. 2016;95:e5477. doi: 10.1097/MD.0000000000005477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Daldal H., Gokmen Salici A. Ocular Findings Among Patients with Vitamin D Deficiency. Cureus. 2021;13:e15159. doi: 10.7759/cureus.15159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Karabulut M., Karabulut S., Canbek T.D., Sül S., Karalezli A. The effect of vitamin D deficiency on the retinal microvasculature: An observational case-control study. Arq. Bras. Oftalmol. 2022 doi: 10.5935/0004-2749.20220089. [DOI] [PubMed] [Google Scholar]
- 319.Malabanan A., Veronikis I.E., Holick M.F. Redefining vitamin D insufficiency. Lancet. 1998;351:805–806. doi: 10.1016/S0140-6736(05)78933-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.