Abstract
Simple Summary
Mitochondria are important organelles involved in several key cellular processes including energy production and cell death regulation. For this reason, it is unsurprising that mitochondrial function and structure are altered in several pathological states including cancer. Cancer cells present variate strategies to generate sufficient energy to sustain their high proliferation rates. These adaptative strategies can be mediated by extracellular signals such as extracellular vesicles. These vesicles can alter recipient cellular behavior by delivering their molecular cargo. This review explores the different EV-mediated mitochondrial reprogramming mechanisms supporting cancer survival and progression.
Abstract
Altered metabolism is a defining hallmark of cancer. Metabolic adaptations are often linked to a reprogramming of the mitochondria due to the importance of these organelles in energy production and biosynthesis. Cancer cells present heterogeneous metabolic phenotypes that can be modulated by signals originating from the tumor microenvironment. Extracellular vesicles (EVs) are recognized as key players in intercellular communications and mediate many of the hallmarks of cancer via the delivery of their diverse biological cargo molecules. Firstly, this review introduces the most characteristic changes that the EV-biogenesis machinery and mitochondria undergo in the context of cancer. Then, it focuses on the EV-driven processes which alter mitochondrial structure, composition, and function to provide a survival advantage to cancer cells in the context of the hallmarks of cancers, such as altered metabolic strategies, migration and invasiveness, immune surveillance escape, and evasion of apoptosis. Finally, it explores the as yet untapped potential of targeting mitochondria using EVs as delivery vectors as a promising cancer therapeutic strategy.
Keywords: tumor-derived EVs (TEVs), miRNA, mitochondrial dynamics, metabolism, tumor microenvironment (TME)
1. Introduction
One of the established hallmarks of cancer is the metabolic switch cancer cells undertake to satisfy energy demands and provide biomolecules to support heightened proliferation and adapt to a microenvironment that is often scarce in oxygen and nutrients [1]. Metabolic dysregulation suggests that the reprogramming of mitochondria is involved due to the key role of this organelle in the production of energy and the metabolic intermediates necessary for biosynthesis.
The cancer metabolic phenotype is more dependent on external cues from the tumor microenvironment (TME) than originally thought. The TME is a complex network that includes tissue stromal cells, immune cells, vessels, extracellular matrix proteins, adipocytes, and soluble factors. The TME is crucial for supporting cancer cells throughout all their developmental stages and is modulated by intercellular communication [2]. Functional interactions between cancer cells and non-malignant cells in the TME are mediated by several mechanisms including extracellular vesicles (EVs).
EVs are small vesicles generated by all cell types, including cancer cells, that contain a wide range of bioactive molecules that can be transferred to recipient cells, activating or silencing signaling pathways and therefore modulating cellular behavior. Tumor-derived EVs (TEVs) are acknowledged to be involved in regulating many of the hallmarks of cancer such as escaping immune surveillance, promoting angiogenesis, evading apoptosis, and inducing a metabolic switch [3].
Given the central role that mitochondria play in many of these processes, this review focuses on the EV-mediated mechanisms used by cancer cells to reprogram the mitochondria of recipient cells to support their growth. We also highlight the bidirectional communication that occurs between cancer and healthy cells and how this process is critical for supporting cancer survival. This review then concludes by assessing the potential of EV-mediated mitochondrial reprogramming as a therapeutic strategy for cancer treatment.
2. Extracellular Vesicle Release and Cargo in Cancer
2.1. Overview
EVs are membranous vesicles delimited by a lipid bilayer without replicative capacity, with sizes ranging from 30 to 1000 nm that are generated by all cells and have been found in multiple biofluids [4]. They differ according to their biogenesis, size, cargo, and cellular pathophysiological state. The main EV types are those derived from the outward shedding of the plasma membrane, called microvesicles or ectosomes, and those derived from the endocytic pathway, named exosomes. However, due to the difficulty in determining the pathway of vesicle biogenesis in experimental settings, the International Society of Extracellular Vesicles (ISEV) recently recommended a nomenclature based on particle size (small EVs (<200 nm) and big EVs (>200 nm)) [4]. Nonetheless, new technologies are in development in order to achieve selective isolation of EV subtypes. Specific isolation and characterization of EV subtypes will be key to a better understanding of their particular functions as well as for their application in clinical practice [5].
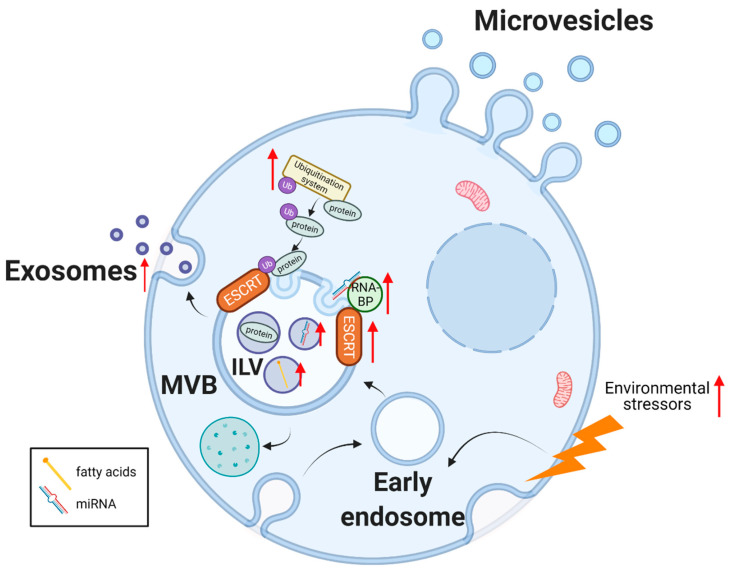
Exosome biogenesis starts with the formation of the early endosome by the inward budding of the cellular membrane. The limiting membrane buds inwards, creating intraluminal vesicles (ILV) within the late endosome or multivesicular body (MVB). Finally, the MVB contents can be degraded by fusing with lysosomes or secreted by the merging of its membrane with the cellular bilayer, thereby releasing the ILVs to the extracellular milieu in the form of exosomes (Figure 1) [6,7]. Exosome biogenesis is mainly regulated by the endosomal sorting complexes required for transport (ESCRT) machinery. ESCRT-independent mechanisms also exist including those mediated by ceramides and tetraspanin proteins [8]. EVs play an important role in intercellular communication, as they can be taken up by surrounding cells or enter the systemic circulation and target distant tissues. The cargo of EVs includes proteins, metabolites, lipids, and nucleic acids (mRNA, non-coding RNA (ncRNA), DNA, mitochondrial DNA (mtDNA)). The release of this cargo inside recipient cells can modulate cellular behavior by affecting gene and protein expression, and nutrient abundance, eventually impacting cell homeostasis. This stands true in both physiological and pathological situations such as cancer. The biological importance of EVs in cancer is supported by the observations that there is both an increased release of EVs, and an alteration in their cargo [9,10].
Figure 1.
EV biogenesis, release, and cargo in cancer. Exosome biogenesis starts with the inward budding of the plasma membrane (early endosome). The limiting membrane buds inwards, generating intraluminal vesicles (ILV) contained in a late endosome or multivesicular body (MVB). The membrane of the MVB body fuses with the plasma membrane releasing the exosomes to the extracellular milieu. Several of the elements involved in exosome biogenesis and cargo sorting are upregulated in cancer (marked with a red arrow). Microvesicles or ectosomes are generated by the direct outward budding of the plasma membrane. Abbreviations used: ESCRT: endosomal sorting complexes required for transport. RNA-BP: RNA binding proteins. Ub: ubiquitin. miRNA: microRNA. Figure created with BioRender.com (accessed on 31 March 2022).
2.2. Alterations in EV Biogenesis and Release
Cancer-enhanced EV release suggests a dysregulation in the components of the EV biogenesis machinery as a survival strategy. In support of this hypothesis, ESCRT proteins have been found to be upregulated in some cancer types [11,12,13] as well as other molecules involved in exosome biogenesis and release, such as heparanase [14,15] and syntenin [16]. Moreover, several oncogenic signaling pathways [reviewed in McAndrews et al. [17]] have been implicated in the upregulation of exosome biogenesis, however, further exploration of the underlying mechanisms is required. Extrinsic factors, such as environmental stressors, can also influence EV biogenesis. Cells subjected to stress conditions such as hypoxia, nutrient deprivation [18,19], mechanical strain [20], pH or with dysregulated protein synthesis [17] release more EVs as a compensatory mechanism.
2.3. Alteration in EV Cargo
The abundance of EV cargo molecules does not always reflect the intracellular content of their parental cell, indicating that these molecules are not passively loaded into EVs but through specific sorting systems that enrich for different cargo components (reviewed in [21,22]). Notably, EVs are highly enriched in small ncRNA such as microRNA (miRNA), which are increasingly recognized as playing an important role in gene regulation. The contribution of EV-derived miRNA to the hallmarks of cancer has been confirmed by many studies [23]. miRNAs typically bind to the 3′ untranslated region (UTR) of mRNA for translational repression. Interestingly, some miRNA species can also translocate into mitochondria and target mtDNA-derived mRNA [24] to alter the expression of the mitochondrial genome thereby modulating mitochondrial function [25]. The miRNA contained in EVs are enriched in specific short nucleotide motifs which act as loading signals, being recognized by RNA-binding proteins that interact with components of the ESCRT pathway [26,27,28]. Most of these RNA-binding proteins have been found to be dysregulated in cancer and are associated with poor clinical outcomes [29]. However, the mechanisms that these RNA-binding proteins use to interact with the endosomal machinery and thereby deliver the miRNA into the MVB need further study. The other main EV biomolecules that cancer can use to alter EV-recipient cell behavior are proteins [30]. These proteins can be sorted into EVs through post-translational modifications (PTMs) such as ubiquitination, a process that is often dysregulated in cancer [31]. These PTMs then act as loading signals to be recognized by the ESCRT pathway complexes [21].
EV nucleic acid and protein cargos have been extensively investigated for their potential role as biomarkers in cancer. However, lipids have also been found to be enriched in EVs, though their EV loading mechanisms remain largely unknown [32,33]. Most of these lipids are fatty acids, which can only be metabolized in mitochondria and can support cancer survival.
Despite lacking a comprehensive understanding of the cancer-specific mechanisms regulating EV biogenesis and cargo sorting, the alterations in these pathways, together with many functional studies, highlight the importance of EV biology in cancer progression.
3. Mitochondria in Cancer
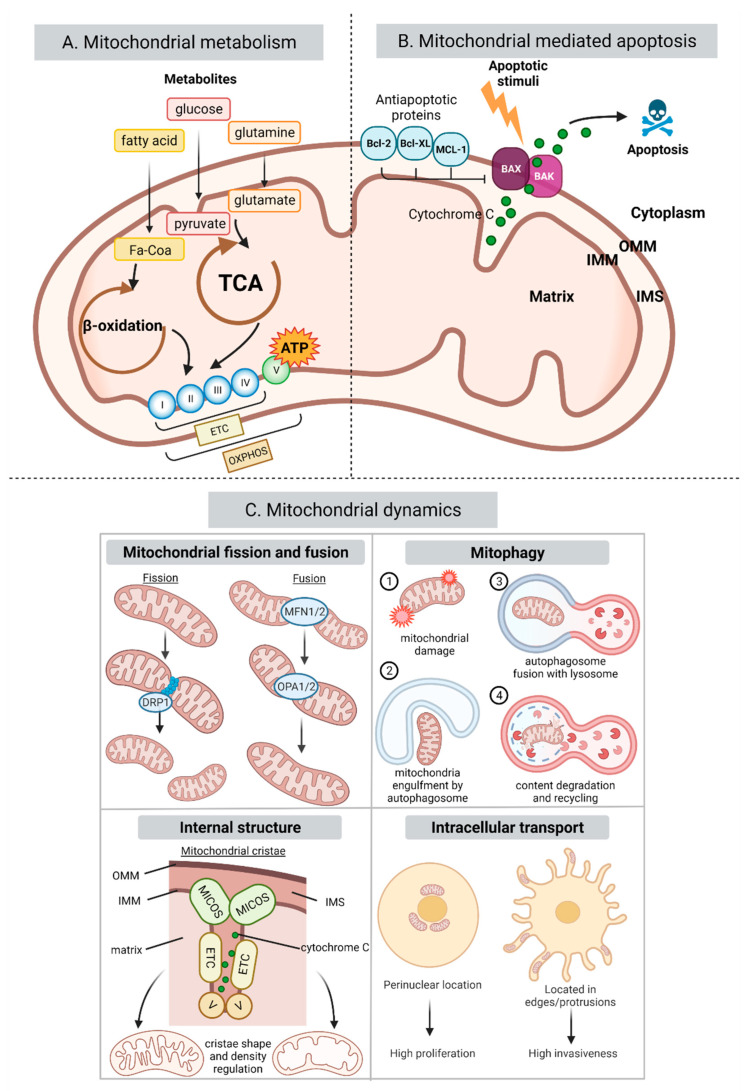
Mitochondria are essential organelles that play a central role in the cellular metabolic axis, generating most of the energy necessary for cell function, as well as participate in other key cell events, such as regulating apoptosis and lipid homeostasis (Figure 2A). Therefore, it is no surprise that mitochondrial dysregulation is involved in the pathogenesis and progression of very diverse diseases, from muscular dystrophy [34] to alcohol-related liver disease [35,36] and cancer [37,38].
Figure 2.
Mitochondrial processes affected in cancer. (A) Summarizes key metabolic processes in mitochondria. Metabolites such as glucose, fatty acids (FA) and glutamine are transformed into pyruvate, FA-CoA and glutamate and enter the TCA and β-oxidation cycles taking place in the mitochondrial matrix. These processes are used by the ETC to pump protons into the intermembrane space creating a chemical gradient used by complex V to generate ATP in a process called OXPHOS. (B) Summarizes the role of the Bcl-2 family proteins in the mitochondrial intrinsic pathway. Briefly, apoptotic stimuli lead to the formation of the pores in the OMM by Bax and Bak releasing cytochrome c into the cytoplasm which triggers the caspase cascade inducing apoptosis. The antiapoptotic members of the Bcl-2 family inhibit this process. (C) Summarizes the four main mitochondrial dynamics processes: mitochondrial fusion and fission, mitophagy, internal cristae architecture, and mitochondrial intracellular trafficking. In cancer, all these mitochondrial activities are dysregulated to support cancer energetic and biosynthetic demands, as well as survival. Abbreviations used: TCA: tricarboxylic acid. ATP: adenosine triphosphate. ETC: electron transport chain. OXPHOS: oxidative phosphorylation. I: complex I. II: complex II. III: complex III. IV: complex IV. V: complex V. OMM: outer mitochondrial membrane. IMM: inner mitochondrial membrane. IMS: intermembrane space. MICOS: mitochondrial contact site and cristae organizing system. Figure created with BioRender.com (accessed on 31 March 2022).
3.1. Mitochondrial Metabolism
Tumor cells undergo a series of metabolic changes that allow them to sustain an increased proliferation and to survive environmental stressors. Cancer metabolic adaptative strategies are heterogeneous, but many of them are connected to a reprogramming of mitochondria [39]. One of the most well-known and common alterations is the Warburg effect, namely a substantial increase in the glycolytic rate independent of the oxygen concentration. Despite the prevalence of glycolysis for energy production, mitochondrial oxidative phosphorylation (OXPHOS) is still required to support tumor formation, progression, and metastasis [38,40,41,42,43], highlighting the fundamental role that mitochondrial machinery plays in cancer biology.
In addition, the adaptation of cancer cells to alternative metabolite use can also be mediated by a mitochondrial reprogramming [44]. Interestingly, EVs have been found to modulate glucose metabolism in the context of cancer through a variety of cargo molecules including miRNA [45], long non-coding RNA (lncRNA) [46], integrins [47], enzymes and metabolites [48]. Fatty acid metabolism, which only occurs within the mitochondrial matrix, is also altered in cancer. Changes in fatty acid oxidation (FAO) are instrumental in cancer progression, metastasis, drug resistance and cell growth [49,50]. Again, EVs are implicated in lipid metabolism [51] and in the FAO changes of cancer, as they contain both mitochondrial FAO enzymes and substrates that are transferred to recipient cells [52,53,54,55,56]. In addition, glutamine, another mitochondrial metabolic substrate, is important for cancer cell growth [57] as both a source for tricarboxylic acid (TCA) cycle intermediates [58,59] as well as an antioxidant [60,61]. Increased levels of glutamine in the TME have been found to promote mitochondrial biogenesis [62]. Intriguingly, the cellular stress induced by glutamine deprivation leads to the release of EVs with a different formation mechanism containing an altered protumorigenic cargo [63].
3.2. Mitochondrial Dynamics
Effective mitochondrial functionality is tightly correlated with their number, size, mass, internal architecture, and intracellular location. Several processes are in place to regulate these parameters including fission, fusion, mitophagy, and intracellular trafficking which are collectively known as mitochondrial dynamics (Figure 2C). These events are important in defining cellular bioenergetics in health, but they can be perturbed in disease and promote tumorigenesis or tumor progression [64,65].
The alteration in the balance of mitochondrial fusion/fission events affects multiple aspects of tumor biology such as cell migration and proliferation, metabolism, cellular stemness and apoptosis [66,67]. Mitochondrial fusion and fission are mediated by several GTPases in the outer mitochondrial membrane such as dynamin-related protein 1 (Drp-1) (which promotes fission) and mitofusin 1 and 2 (Mfn-1/2) (which promote fusion). A typical change occurring in cancer is a higher expression and activity of Drp1, with the resulting increase in mitochondrial fission having been found to enhance the metastatic capacity and progression of breast [68,69] lung [70] and brain cancer [71]. In contrast, Mfn-2 has been found to inhibit the invasion and growth of lung [70] and breast [72] cancer. Moreover, low levels of Mfn-2 expression correlate with a poorer prognosis in breast cancer patients and low Mfn-1 is associated with an increased metastatic capacity in hepatocellular carcinoma (HCC) [65].
Mitochondrial fusion/fission processes are closely coordinated with the mitophagy machinery, which is responsible for the degradation and recycling of dysfunctional mitochondria. Mitophagy can be both tumor suppressive or protumorigenic depending on the tumor type, stage, or metabolic phenotype of the cancer [73]. In accordance with this dual role, mitophagy-related proteins have been found to be dysregulated in a number of cancers, being up or downregulated depending on cancer type [74]. Very recently, a functional connection has been found between EV secretion and mitophagy in melanoma through CD9, a member of the tetraspanin family. The inhibition of CD9 leads to mitochondrial malfunction that is compensated for by an increase in mitochondrial mass through a reduction in mitophagy [75].
Reported internal structural changes occurring in the mitochondria of cancer cells are related to mitochondrial cristae shape and density. Both are important as they affect the production of ATP by influencing function, stability and organization of the respiratory enzymes of the electron transport chain (ETC) into supercomplexes [76], thereby impacting all cellular processes that rely on mitochondrial respiration [77]. Further biological relevance of cristae architecture occurs when the cristae structure loosens allowing the release of proapoptotic factors [78]. The cristae structure has been found to be altered in cancer [79] and this has been attributed to changes in the composition of the mitochondrial contact site and cristae organizing system (MICOS) subunits that can vary according to cancer type [80].
3.3. Mitochondrial-Mediated Apoptosis
The mitochondrial dynamics machinery is also involved in the process of apoptosis or programmed cell death [81]. Resistance to apoptosis is one of the hallmarks of cancer and inducing apoptosis has been a leading cancer therapeutic approach for decades [82]. Apoptosis can either start through the activation of death receptors on the cell surface (extrinsic pathway) or through the involvement of mitochondria (intrinsic pathway) with molecular stressors increasing mitochondrial permeability leading to the release of cytochrome c. The intrinsic pathway is mainly regulated by the Bcl-2 family, through the balance of its proapoptotic (i.e., Bax, Bak) and antiapoptotic protein family members (i.e., Bcl-2, MCL-1, Bcl-XL) (Figure 2B) [83]. Cancer cells have been found to present an altered expression of Bcl-2 family members with EV cargo being found to modulate apoptosis by affecting Bcl-2 family members (reviewed in Section 4). Importantly, mitochondria are not passive actors in this process as mitochondrial architecture, lipid and protein composition are crucial in regulating apoptosis [81].
Taken together, these studies underline the active role of mitochondria in facilitating cancer survival through the adaptation of metabolic strategies, hijacking of mitochondrial dynamics, and suppression of the mitochondrial apoptotic pathways while emerging data is highlighting the role of EVs as mediators of these changes.
4. EV Modulation of Mitochondrial Processes in Cancer
Tumors are complex systems in constant communication with their microenvironment on which they rely for growth and survival. EVs, as intercellular communicators, are involved in several hallmarks of cancers, being active players in the remodeling of the TME and priming metastatic niches to support tumor survival, progression, and invasion. Although the importance of mitochondrial state and reprogramming in cancer progression has been established, the underlying mechanisms and metabolic phenotypes are incredibly varied, and knowledge is still lacking. Thus, the following section focuses on the role of EVs in mitochondrial reprogramming to support tumor survival by modulation of the TME in the context of the hallmarks of cancer (Table 1).
Table 1.
EV-mediated modulation of mitochondrial processes in cancer. This table summarizes EV studies according to the hallmarks of cancer where a mitochondrial effect was observed in recipient cells. Abbreviations and symbols used: n.i.: not investigated. NA: not applicable. CRC: colorectal cancer. OXPHOS: oxidative phosphorylation. TCA: tricarboxylic acid. CI: complex I. CIII: complex III. CIV: complex IV. CV: complex V. CAF: cancer-associated fibroblast. LncRNA: long non-coding RNA. FA: fatty acid. FAO: fatty acid oxidation. HCC: hepatocellular carcinoma. MSC: mesenchymal stem cell. HNSCC: head and neck squamous cell carcinoma. NSCLC: non-small cell lung cancer. MDSC: myeloid-derived suppressor cell. Mito: mitochondria/l. ↑: increase. ↓ decrease. →: leading to.
| EV Donor Cell | EV Recipient Cell | EV Cargo | ncRNA Target | Mitochondrial Effect | References |
|---|---|---|---|---|---|
| Dysregulation of cellular energetics | |||||
| Metabolic coupling with CAFs | |||||
| Prostate cancer cells | Fibroblasts | miR-424 | n.i. | IDH3a↓, NDUFA4L2(CI)↑→OXPHOS↓ | [84,85] |
| CRC cells | Fibroblasts | n.i. | n.i. | ATP5H(CV)↑, IDH2↑, ECH1↑, TUFM↓, ALSDH2↓ | [86] |
| Melanoma cells | Fibroblasts | miR-155, miR-210 | n.i. | OXPHOS↓ | [87] |
| Lung cancer cells | Fibroblasts | miR-210 | NDUFA4 (CI), SDHD (CII) | SDHD↓ → OXPHOS↓ | [88,89] |
| Nasopharyngeal carcinoma cells | Fibroblasts | LMP1 | NA | OXPHOS↓ | [90] |
| CAFs | Breast cancer cells | lncRNA SNHG3 | n.i. | OXPHOS↓ | [91] |
| CAFs | Prostate cancer cells | miR-22, let7a, miR-125b and metabolites (amino acids, lipids, TCA intermediates) | n.i. | CYTB(CIII)↓, COXI (CIV) ↓→ OXPHOS↓ | [92] |
| CAFs | Pancreatic cancer cells | miRNA, TCA metabolites | n.i. | TCA↑ | [93] |
| CAFs | CRC cells | miR-92a | n.i. | OXPHOS↓ | [94,95] |
| Metabolic coupling with adipocytes | |||||
| Breast cancer cells | Adipocytes | miR-155 | PPARγ | UCP1↑ | [96] |
| Breast cancer cells | Adipocytes | miR-144, miR-126 | n.i. | UCP1↑, mito matrix density↑ | [97] |
| Adipocytes | Melanoma, prostate tumor cells | FAO proteins (ECHA, HCDH), TCA proteins, OXPHOS proteins | NA | Mito number and density↑, FAO↑ | [98] |
| Adipocytes | Melanoma cells | FAO enzymes (HCDH, ECHA, HCD2), OXPHOS subunits (NDUA6 and NDUAS2 (CI) and ATPG (CV)), mitochondrial ADP/ATP transporters (ADT1, ADT2 and ADT3), fatty acids | NA | FAO↑, mito activity↑, mito intracellular trafficking↑ | [55] |
| Adipocytes | HCC cells | miR-23a/b | Mitochondrial glutaminase | Glutamine metabolism regulation | [99,100] |
| Metabolic subjugation of neighboring cells | |||||
| Kaposi’s sarcoma-associated herpes virus cells | Uninfected cells | miRNA | n.i. | Mito biogenesis↓, mito respiration↓ | [101] |
| Resistance to cell death | |||||
| Modulation of the Bcl-2 pathway | |||||
| Melanoma cells | Melanoma cells | n.i. | n.i. | Bax↓, Bcl-2↑ | [102] |
| Bladder cancer cells | Bladder cancer cells | n.i. | n.i. | Bax↓, Bcl-2↑ | [103] |
| Acute myeloid leukemia cells | Acute myeloid leukemia cells | circ_0009910 | miR-5195–3p | Bax↓, Bcl-2↑ | [104] |
| Glioma cells | Endothelial cells | lncRNA-CCAT2 | n.i. | Bax↓, Bcl-2↑ | [105] |
| MSCs | Multiple myeloma cells | lncRNA LINC00461 | miR-15a/16 | Bcl-2↑ | [106] |
| Chemotherapy resistance | |||||
| Trastuzamab-resistant breast cancer cells | Trastuzamab-sensitive breast cancer cells | lncRNA snhg14 | n.i. | Bax↓, Bcl-2↑ | [107] |
| Gefitinib-resistant esophageal squamous cell carcinoma cells | Esophageal squamous cell carcinoma cells | lncRNA PART1 | miR-129 | Bax↓, Bcl-2↑ | [108] |
| Gefitinib-resistant non-small cell lung cancer cells | Gefitinib-sensitive non-small cell lung cancer cells | miR-214 | n.i. | Bax↓, Bcl-2↑ | [109] |
| Vincristine-resistant gastric cancer cells | Vincristine-sensitive gastric cancer cells | CLIC1 | NA | Bcl-2↑ | [110] |
| Doxorubicin-resistant breast cancer cells | Doxorubicin-sensitive breast cancer cells | Hsp70 | NA | mito damage↑→ OXPHOS↓ | [111] |
| Temozolomide-resistant glioblastoma cells | Temozolomide-sensitive glioblastoma cells | Connexin 43 | NA | Bax↓, Bcl-2↑ | [112] |
| Gefitinib-treated NSCLC cells | Untreated NSCLC cells | n.i. | n.i. | Bax↓, Bcl-2↑ | [113] |
| CAFs | CRC cells | miR-92a-3p | n.i. | Bax↓ | [114] |
| Enhancing survival and chemoresistance through transfer of mitochondrial components | |||||
| Astrocytes | Glioma cells | mitochondria | NA | Mito metabolism↑ | [115] |
| Tumor-activated stromal cells | Glioblastoma cells | mitochondria | NA | OXPHOS↑ | [116] |
| CAFs | Breast cancer cells | mtDNA | NA | OXPHOS↑ | [117] |
| Aldh2-deficient hepatocytes | HCC cells | Oxidized mtDNA | NA | Bcl-2↑ | [118] |
| Escape from immune destruction | |||||
| Macrophage mitochondrial reprogramming in cancer | |||||
| Lung tumor cells | M0 macrophages | n.i. | n.i. | CI↓→OXPHOS ↓ | [119] |
| Hypoxia-induced TEVs | Infiltrating macrophages | let-7a | n.i. | OXPHOS↑ | [120] |
| Immunosuppression of T cells | |||||
| Melanoma cells | Tumor infiltrating cytotoxic CD8+ T lymphocytes | n.i. | n.i. | OXPHOS↑ | [121] |
| Melanoma cells | CD4+ T helper cells | miR-690 | n.i. | Bcl-2↓, MCL-1↓, Bcl-xl↓ | [122] |
| Renal carcinoma cells | Jurkat T Lymphocytes | FasL | NA | Bax↑, Bcl-2↓ | [123] |
| HNSCC cells | CD8+ T cells | FasL | NA | Release of CytC, mito membrane potential↓, Bcl-2↓, Bcl-XL↓, Bax↑, Bim↑ | [124] |
| MDSCs | CD8+ T cells | immuno-modulatory cytokines | NA | Mito ROS↑ → Bcl-2↓ | [125,126] |
| Activation of invasion and metastasis | |||||
| Increased motility and migration | |||||
| Hypoxic breast cancer cells | Epithelial cells | n.i. | n.i. | Drp1 phosphorylation, Mfn-1↑, Mfn-2↑, mito intracellular movement↑ | [127] |
| Bladder cancer cells | Urothelial cells | n.i. | n.i. | Mito size↓ | [128] |
| Adipocytes | Melanoma cells | Fission regulators (FIS1, OPA1), FA, FAO enzymes, OXPHOS proteins | NA | fission↑, mito size↓, mito intracellular movement↑ | [55] |
| CAFs | Pancreatic cancer cells | miR-106b | n.i. | Mfn-2↓ | [129,130] |
| Intravasation | |||||
| Breast cancer cells | Liver sinusoidal endothelial cells | n.i. | n.i. | Mito disfunction | [131,132] |
| Brain metastatic cancer cells | Endothelial cells | miR-181c | COX1 | Bax↑, Bcl-2↓ | [133,134,135] |
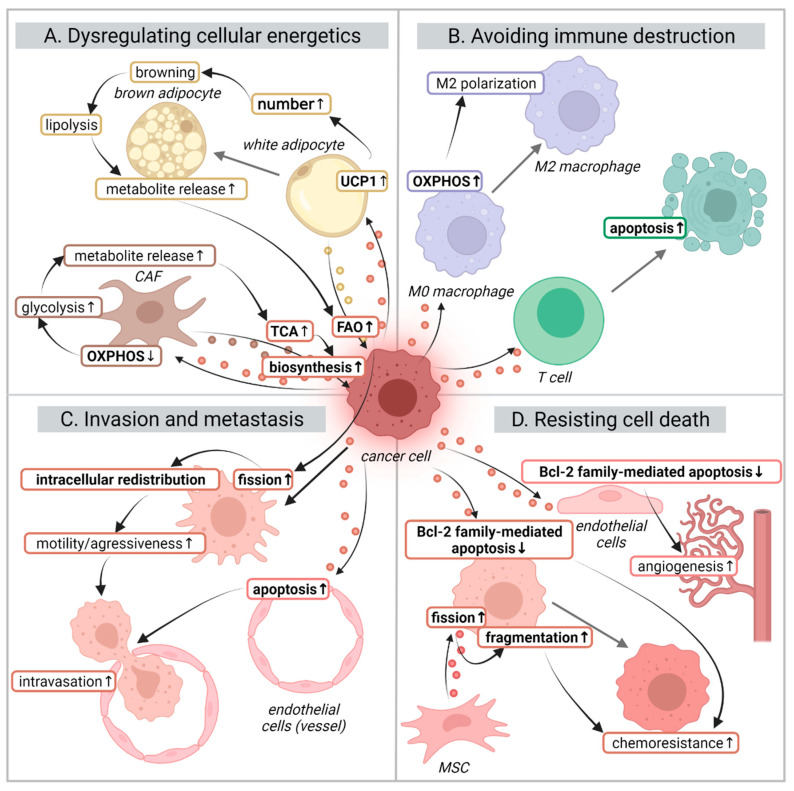
4.1. Dysregulating Cellular Energetics
4.1.1. Metabolic Coupling with Cancer-Associated Fibroblasts (CAFs)
Among the different TME players, fibroblasts are key in metabolically supporting tumor progression [136]. Crosstalk between tumor cells and fibroblasts in the TME induces a phenotype change of the latter into cancer-associated fibroblasts (CAFs). CAFs display a hyperactive behavior facilitating tumor survival and migration [137]. During this transformation, fibroblasts switch to a glycolytic phenotype to provide cancer cells with energy-rich metabolic intermediates that fuel both mitochondrial ATP generation and biosynthesis [138]. This process, in which glycolytic CAFs support mitochondrial respiration in cancer cells, has been termed the reverse Warburg effect [139]. Reprogramming resulting from the crosstalk between cancer cells and local fibroblasts can occur through different mechanisms which can be mediated by TEVs (Figure 3A) [138].
Figure 3.
EV modulation of mitochondria and its effects in the context of hallmarks of cancer. Cancer cells generate tumor-derived EVs (TEVs) that alter the mitochondrial behavior of different cell types of the tumor microenvironment to support cancer progression, invasion, and survival. Through these effects, TEVs are mediators of several of the hallmarks of cancer such as: (A) dysregulation of cellular energetics: cancer cells can induce the release of metabolites from CAFs and adipocytes to be used for cancer cell biosynthesis and FAO; (B) avoiding immune destruction: TEVs can induce immunosuppression by inducing M2 polarization in macrophages or T cell apoptosis via the mitochondrial intrinsic pathway; (C) promoting cell motility and facilitating invasiveness: increased FAO leads to an intracellular trafficking of mitochondria towards edge protrusions facilitating their migration. At the same time, they can induce mitochondrial apoptosis in endothelial barrier cells to permit intravasation; (D) resisting cell death: alterations in Bcl-2 family members leads to inhibition of mitochondrial apoptosis resulting in chemotherapy resistance and angiogenesis. Abbreviations used: OXPHOS: oxidative phosphorylation. TCA: tricarboxylic acid cycle. FAO: fatty acid metabolism. UCP1: uncoupling protein 1. MSC: mesenchymal stem cell. Labels in bold represent mitochondria-related elements and processes. The colors of the EVs reflect those of the parental cell that produced them. The colors of the text borders reflect the cells where the indicated processes take place. Figure created with BioRender.com (accessed on 31 March 2022).
One of these mechanisms is through the transfer of miRNAs affecting the expression of mitochondrial proteins. Melanoma TEVs have been found to contain miR-155 and miR-210 that lead to the reprogramming of stromal fibroblast metabolism by promoting glycolysis and inhibiting OXPHOS [87]. Similarly, miR-424, found in TEVs, downregulates the TCA enzyme IDH3a leading to the inhibition of OXPHOS through the upregulation of mitochondrial NDUFA4L2 [84,85]. Another mechanism of OXPHOS downregulation is through lung cancer TEVs transfer of miR-210 to CAFs [88]. Mechanistically, miR-210 directly downregulates ETC complex I subunit NDUFA4 and complex II subunit SDHD, resulting in mitochondrial dysfunction, as evidenced by an alteration in mitochondrial membrane potential. Interestingly, this miRNA also modifies mitochondria size and cristae organization [89]. In cancer associated with viral infection, it has been observed that TEVs contain viral proteins that, upon delivery to normal fibroblasts, induce their transformation into CAFs. This transformation is associated with a decrease in OXPHOS [90]. Moreover, further work on fibroblasts incubated with colorectal cancer (CRC) TEVs exhibited dysregulated expression of a number of mitochondrial proteins such as upregulation of a complex V subunit (ATP5H), TCA cycle enzyme IDH2 and the β-oxidation enzyme ECH1, as well as downregulation of mitochondrial protein translation factor TUFM and detoxifying enzyme ALDH2 [86].
In turn, CAF-derived EVs (CAF-EVs) also participate in cancer’s metabolic switch. For instance, breast cancer CAF-EVs transfer the lncRNA SNHG3 that inhibits OXPHOS and increases glycolysis, driving an increased tumor cell proliferation [91]. Similarly, Zhao and colleagues showed that CAF-EVs were able to inhibit OXPHOS through the transfer of miRNAs such as miR-22, let7a and miR-125b. Moreover, CAF-EVs can modulate mitochondrial metabolism by the transfer of lipids, amino-acids, and de novo complete TCA metabolites. Of note, the most abundant miRNAs found in CAF-EVs targeted OXPHOS genes with downregulation in the expression of subunits in complexes III and IV of the ETC [92]. The same group later demonstrated that CAF-EV-derived metabolites were able to support nutrient-deprived pancreatic cancer cell metabolism by modulating the TCA cycle [93]. Moreover, CAF-EVs delivered miR-92a to CRC [94]. Inhibition of this miRNA has been found to enhance oxygen consumption as well as increase the expression of mitochondrial proteins in adipocytes [95], suggesting a mitochondrial effect in cancer cells. However, fibroblasts metabolically reprogrammed by TEVs can also lead to increased OXPHOS, mitochondrial activity and number through the supply of energy-rich metabolites to cancer cells [90]. Consequently, the observed capacity of CAF-EVs to support the cancer cell TCA cycle while generally inhibiting OXPHOS, suggests a repurposing of mitochondria from an energy “powerhouse” to a biosynthetic “factory”.
EV-mediated mitochondrial reprogramming is bidirectional, the direction and nature of this reprogramming being dependent on cancer type and pathological stage. Supporting evidence for the changing role of EVs in the natural history of cancer comes from early and late-stage colorectal cancer TEVs being able to induce different phenotypes in fibroblasts, from protumorigenic to prometastatic phenotypes [86]. These observed differences in fibroblast function and phenotype suggest that the cargo of the TEVs can be adjusted to satisfy the varying needs of cancer cells throughout their developmental process.
4.1.2. Metabolic Coupling with Adipocytes
Adipose tissue, composed mainly of adipocytes, has been found to promote tumor progression [140]. The main role of adipocytes is to maintain a physiological energy balance by storing fat and releasing it according to energy demands. Adipocyte function depends on its differentiation status which is linked to mitochondrial changes. Typically, differentiation of white adipocytes into brown/beige adipocytes is characterized by an increase in mitochondrial number and activity, as well as an increase in the expression of mitochondrial uncoupling protein (UCP1) that uncouples respiration from ATP synthesis to generate heat and stimulate lipolysis [141]. This phenotype change leads to the release of metabolites that, upon uptake by cancer cells, promote tumor progression (Figure 3A) [97].
TEVs have been demonstrated to induce lipolysis and browning in adipocytes through the transfer of miRNAs such as miR-155, miR-144 and miR-126. Consequently, adipocytes release fatty acids, glutamine, pyruvate, lactate, and ketone bodies for cancer cell utilization [96,97,142]. In parallel, experimental work with adipocytes in melanoma and prostate cancer has shown that adipocytes secrete EVs (adEVs) that increase their malignant potential. This observed phenotypic change was related to metabolic reprogramming, characterized by an increase in fatty acid catabolism via FAO. This catabolic switch was also accompanied by an increase in mitochondrial number and density [98]. The same group also showed that adipocytes can influence tumor metabolism by EV transfer of mitochondrial FAO enzymes, OXPHOS subunits, mitochondrial ADP/ATP transporters, TCA cycle proteins, and fatty acids [55]. AdEVs have also been shown to transfer miR-23a/b to HCC cells [99] and, in the context of prostate cancer, these miRNAs have been found to target mitochondrial glutaminase [100].
In a similar way to CAFs, cancer cells and adipocytes develop a metabolic relationship, where TEVs induce a metabolic shift in adipocytes encouraging the formation and release of energy-rich metabolites to provide nutritional support to cancer cells, thereby promoting a metabolic remodeling favoring FAO for their progression and invasion. This experimental evidence supports the need for further studies to investigate EV-mediated molecular mechanisms by which adipocytes can support tumor growth metabolically.
4.1.3. Metabolic Subjugation of Neighboring Cells
The EV-mediated metabolic manipulation of healthy cells in cancer is not just limited to fibroblasts and adipocytes. Kaposi’s sarcoma-associated herpes virus-derived EVs transfer miRNA to uninfected cells resulting in reduced mitochondrial biogenesis and respiration, with an induction of aerobic glycolysis. The reduction in respiration observed was related to a decrease in mitochondrial volume in EV-treated cells by 40%. Overall, mitochondrial activity was also reduced as reflected by a lower level of TCA cycle metabolites [101]. Unfortunately, the underlying mechanisms leading to this alteration in mitochondrial biogenesis were not explored in greater depth. However, similarly to what occurs with CAFs and adipocytes, the purpose of this change in mitochondrial behavior is to turn EV recipient cells into feeder cells, by the release and transfer of glycolytic end products to infected cells to fuel their TCA cycle for growth advantage.
4.2. Resisting Cell Death
Resistance to apoptosis is a hallmark of cancer and apoptosis is a biological process that can be regulated by mitochondrial events. Chemotherapy ultimately exerts its function by inducing apoptosis which makes the mitochondrial state an important determinant of tumor response to therapy [143]. Mitochondrial dysfunction is associated with tumor cell resistance to both chemotherapy and radiotherapy by impeding apoptosis [144,145], with cancer cells being able to modulate mitochondrial apoptotic priming through EVs to benefit their survival (Figure 3D).
4.2.1. Modulation of the Bcl-2 Pathway
Some of cancer’s EV strategies to evade apoptosis do not necessarily target mitochondrial proteins, but act indirectly on other aspects of the apoptotic cascade, for example transferring proteins such as survivin, which blocks cell death by inhibiting caspases [146], or miR-21 that targets the tumor suppressor programmed cell death 4 (PDCD4) [147]. However, there is also evidence that TEVs are taken up by melanoma and bladder cancer cells inhibiting apoptosis and favoring cell proliferation by targeting mitochondria through the regulation of the Bax/Bcl-2 signaling pathway [102,103]. However, the molecular basis of these observations needs further investigation.
EV-mediated resistance to apoptosis can also occur between cancer cells and other cell types in the TME. For instance, glioma cells transfer EVs containing lncRNA-CCAT2 to endothelial cells in order to promote angiogenesis by decreasing apoptosis in these cells through Bcl-2 increase and suppression of Bax and Caspase-3 expression [105]. The same effect also occurs in the opposite direction, such as between mesenchymal stem cells (MSCs) and cancer cells. MSCs are important players in maintaining tissue homeostasis as they promote processes involved in tissue regeneration, angiogenesis, and cell survival, and their EVs are one way they exert their function. However, MSC function can be hijacked by cancer to enhance its own survival [148]. MSC-derived EVs (MSC-EVs) have been found to contain lncRNA LINC00461 and, on uptake by multiple myeloma cells, it relieved the inhibitory effect of miR-15a/miR-16 on Bcl-2, therefore suppressing apoptosis and promoting myeloma proliferation [106].
4.2.2. Chemotherapy Resistance
The antiapoptotic effect of TEVs has a direct implication on determining the response of tumor cells to therapy. TEVs can spread resistance to chemotherapeutic agents by transferring ncRNAs such as lncRNA-SNHG14, lncRNA PART1 and miR-214, as well as proteins such as chloride intracellular channel 1 (CLIC1) and connexin 43 to chemosensitive cells by modulating components of the Bcl-2 family [107,108,109,110,112,113]. Although the development of chemoresistance caused by the modulation of the Bcl-2 family appears to be common and consistent across a number of cancer and drug types, many of the underlying molecular mechanisms remain unknown.
Besides acting on mitochondrial apoptotic pathways, TEVs have been shown to modulate chemoresistance via the metabolic regulation of drug-sensitive cells. For instance, in doxorubicin-resistant breast cancer cells, TEVs were able to affect the balance between glycolysis and OXPHOS in recipient cells via mechanisms involving heat shock protein-70 (Hsp70). After Hsp-70 delivery by TEVs, this protein translocates into mitochondria and induces mitochondrial damage through increasing reactive oxygen species (ROS) levels. Consequently, recipient cells with impaired mitochondrial respiration switch to an enhanced glycolytic activity [111].
EVs from other cells in the TME also enhance drug resistance. For instance, CAF-EVs transfer miR-92a-3p and miR-103a-3p to cancer cells inhibiting mitochondrial apoptosis [114,149]. In another study, the co-culture of MSCs with tumor cells activated the mitochondrial fission mediator Drp1, inducing an increased fragmentation of mitochondria in a T-cell lymphoblastic leukemia model. This alteration in mitochondrial fission dynamics was related to a decrease in mitochondrial ROS, a glycolytic switch and contributed to the development of chemoresistance [150]. Although the specific extracellular mechanism was not studied, EV capacity to promote mitochondrial fission has been previously demonstrated [55,127].
4.2.3. Enhancing Cancer Survival and Chemotherapy Resistance through EV Transfer of Functional Mitochondria and Mitochondrial Components
Besides the intercellular transfer of molecules such as miRNAs that regulate the expression of mitochondrial components, several studies have also described the transfer of whole functional organelles. The transfer of whole mitochondria has been proven to be a protective strategy for a range of conditions such as lung or stroke-induced injury which require a metabolic rescue [151,152]. There are a number of different mechanisms for horizontal transfer of mitochondria such as cell fusion, gap junctions, tunnelling nanotubes and EVs [153,154]. In the context of cancer, this is another strategy undertaken to alter mitochondrial respiration.
MSCs have been found to transfer whole mitochondria via big MSC-EVs to recipient cells and rescue their metabolic function (see Section 5). However, the mechanisms that are beneficial for regenerative medicine (e.g., cells with a metabolic disease) can also be exploited by cancer cells to increase their mitochondrial number for ATP production to favor their progression [155]. Genetic aberrations and high proliferation in tumor cells increase the likelihood of mitochondrial dysfunction and instability. Therefore, receiving functional mitochondria or mitochondrial components could help restore or enhance mitochondrial function. In the context of chemotherapy, it has been shown that the horizontal transfer of mitochondria from MSC to leukemic cells led to an increase in OXPHOS and cancer cell survival advantage [156].
Further evidence for EV transfer of mitochondria has been seen in the exchange from astrocytes to glioma cells. This was found to improve the metabolism of the recipient cancer cell and contribute to chemotherapy resistance. Mechanistically, mitochondria-derived NAD+ metabolic enzymes increase the availability of NAD+ in recipient cancer cells, inducing the PARP-mediated DNA repair pathway [115]. In turn, tumor-activated stromal cells were also found to transfer mitochondria to glioblastoma cells through a number of different mechanisms, including EVs, with the co-culture of both cell types increasing glioblastoma proliferation and resistance to anticancer treatments [116].
In addition to whole mitochondria, the transfer of mitochondrial components such as mtDNA [157], membrane proteins, and active mitochondrial enzymes also occurs. Mitochondrial proteins can account for up to 10% of the total protein content of small EVs [158]. TEVs from melanoma, ovarian, and breast cancer have all been found to contain mitochondrial components that were not present in healthy controls [159]. Interestingly, a recent study showed that trastuzumab was able to modulate the mitochondrial protein cargo of breast cancer cells with most of the affected proteins being involved in mitochondrial membrane organization. It was also observed that trastuzumab reduced mitochondrial cristae numbers. Therefore, the authors hypothesized that damaged mitochondrial components are packed into EVs for disposal. However, the effect of these EVs and their mitochondrial cargo on potential recipient cells needs further investigation [160].
mtDNA is also selectively packaged into EVs as demonstrated by the higher copy numbers found in EVs in blood compared to cell-free plasma and whole blood [161]. Specifically, cancer cells have been found to release TEVs carrying mtDNA [162]. Moreover, mtDNA copy numbers change according to cancer stage and when compared to healthy controls suggesting a potential role in cancer progression [157,163]. Further evidence for EV mtDNA involvement in cancer biology is from their ability to restore OXPHOS and induce resistance to hormonal therapy in breast cancer cells [117]. Tumor cells that lack mtDNA exhibit delayed tumor growth and cells in the TME can transfer mtDNA to mtDNA-depleted tumor cells thereby re-establishing mitochondrial respiration and enhancing tumorigenic potential. Although the transfer process was not studied, EVs were proposed as a potential mechanism [164]. In the context of chronic alcohol exposure, mitochondrial aldehyde dehydrogenase (Aldh2)-deficient hepatocytes produce oxidized mtDNA, which can be delivered into neighboring HCC cells via EVs activating multiple oncogenic pathways which promote HCC [118]. These results highlight a biological role for EV mtDNA cargo in cancer behavior.
4.3. Avoiding Immune Destruction
A relevant hallmark of cancer is immune evasion as cancer cells have the capacity to alter both immune surveillance and its response. Tumors utilize different strategies to silence the immune response in order to create a tolerant TME [165,166]. Cancer cells are known to produce immunosuppressive EVs that contain bioactive molecules with immunomodulatory effects [167]. Recent reviews extensively cover the various mechanisms of TEV-mediated immune suppression [168,169]. However, those affecting mitochondrial function remained largely unaddressed. Potential TEV-mediated immune suppression mechanisms involving the reprogramming of immune cell mitochondria include (i) modulating metabolism to inactivate their tumor suppressor function and (ii) triggering mitochondria mediated apoptosis (Figure 3B). Interestingly, immunoregulatory effects can also be induced by the transfer of whole mitochondria via EVs [170].
4.3.1. Macrophage Mitochondrial Reprogramming in Cancer
In recent years, the link between metabolic reprogramming and immune cell function has attracted increasing attention, giving rise to the field of immunometabolism. The metabolic profile of immune cells can define their phenotype and antitumor capabilities [171]. One of the TEV-mediated mechanisms promoting immune evasion is through shifting macrophages towards an anti-inflammatory M2 phenotype [119,172,173]. Macrophage M2 polarization is considered a key component for tumor progression and is linked to mitochondrial metabolism [172]. However, little attention has been paid to TEVs and their role in mediating immune escape through macrophage mitochondrial reprogramming [173,174,175,176,177]. Proinflammatory M1 macrophages have suppressed mitochondrial function and increased glycolysis to support the shift in their energy demands. In contrast, M2 macrophages present an increase in mitochondrial respiration, a preserved TCA cycle and an enhanced fatty acid metabolism [172]. TEVs can alter mitochondrial respiration in non-committed M0 macrophages and polarize them to the M2 phenotype, and their miRNA cargo has been hypothesized as the basis for this observation [119]. Supporting experimental evidence comes from hypoxic TEV inducing M2-like polarization in infiltrating macrophages by enhancing mitochondrial OXPHOS through the transfer of let-7a miRNA which suppresses the insulin mediated mTOR signaling pathway [120]. Many of the underlying mechanisms of macrophage M2 polarization in cancer remain unexplored. Despite this, adaptations of the ETC complexes are recognized to play an important role in defining macrophage immune response by contributing to the immune metabolic switch [178]. Given the importance of bioenergetics in macrophage polarization and the ability of TEVs to modulate cell metabolism, further research is needed on EV-induced mitochondrial reprogramming of macrophages to potentially provide insight into how cancer promotes its own growth and immune escape.
4.3.2. EV-Related Immunosuppression of T Cells
Other cell types, such as T cells, play a significant role in the regulation of antitumor immune response [179], therefore becoming the target of immunomodulatory mechanisms aimed to reduce cancer cell killing. TEVs have been found to induce apoptosis of activated T cells [180,181] via modulation of the Bcl-2/Bax pathway [123]. TEVs are also responsible for driving antitumor CD8+ effector T cell apoptosis by the presence of FasL and MHC class I as cargo molecules that trigger caspase activation. This, in turn, initiates the release of cytochrome c from mitochondria, leading to a loss of mitochondrial membrane potential and subsequent DNA fragmentation [124,181]. This process is not only modulated by TEVs but also by myeloid-derived suppressor cells EVs (MDSC-EVs). These cells are found in the TME and are recognized for their role in tumor progression. MDSC-EVs contain protumorigenic factors, such as death receptor proteins Fas and TNF-1α, inherited from their parental cells that are capable of immunosuppression by promoting mitochondrial apoptosis in CD8+ T cells through enhanced ROS [125]. The levels of internal ROS in antigen-specific T cells determine cell fate through reciprocal modulation of FasL and antiapoptotic Bcl-2 [126]. In addition to death ligands, melanoma TEVs can eliminate CD4+ T cells by directly targeting mitochondrial apoptosis regulator Bcl-2 through miR-690 [122]. Beyond Bcl-2 family regulation, melanoma cells were also found to enrich their EVs with certain RNAs that, upon delivery, altered mitochondrial function of tumor infiltrating cytotoxic T lymphocytes [121].
Another strategy employed by cancer cells to induce immunosuppression is through EV-encapsulated mtDNA. Mitochondria are a key source of damage-associated molecular patterns (DAMPs) and mtDNA is a large contributing component of mitochondrial DAMPs [182]. As described earlier (Section 4.2.3), TEVs have been found to have a higher copy number of mtDNA compared to healthy controls [163]. Mitochondrial Lon protease (Lon) plays many roles in mitochondrial homeostasis including ROS regulation. Lon drives ROS-induced mtDNA damage which results in its translocation into the cytosol. In the context of cancer, cytosolic mtDNA can affect the immune checkpoint receptors (known as the gatekeepers of the immune response) by causing overexpression of PD-L1 and subsequent activation of immune inhibitory pathways. In parallel, Lon increases the production of TEVs enriched with mtDNA and PD-L1 which inhibit T-cell activation. These Lon-induced EVs further contribute to cancer immune escape by silencing CD9+ T-cell immunity by inducing production of IFN and IL-6 from macrophages [183]. A further link between mitochondria and checkpoint receptors has been shown in a recent study, where the activation of the T-cell surface receptor PD-1 has been associated with downregulation of Drp1 phosphorylation on Ser616 and the consequent reduction of mitochondrial fission in T cells. The effect on mitochondrial dynamics causes a crucial impairment of T-cell functionality and therefore significantly affects antitumor response [184].
4.4. Activating Invasion and Metastasis
4.4.1. Increased Motility and Migration
Alterations in mitochondrial dynamics play different roles in the TME by both inducing and supporting malignant transformation, and these effects can be mediated by TEVs. More specifically, EV-mediated dysregulation of mitochondrial dynamics appears to have a direct impact on cancer motility and migration capabilities (Figure 3C). For instance, hypoxic breast cancer cells have been shown to release EVs containing integrin-linked kinase (ILK) that increase epithelial cell migration, a requirement for epithelial-to-mesenchymal transition (EMT). As a result, mitochondrial movement was stimulated by promoting their intracellular trafficking and accumulation in the cortical cytoskeleton of epithelial cells. This observation was mediated by the phosphorylation of Ser616 in mitochondrial fission protein Drp1 combined with the increased expression of mitochondrial fusion proteins Mfn-1 and Mfn-2 [127]. Wu and colleagues similarly showed that TEVs could induce malignant transformation in healthy cells. EV-treated cells were found to have a higher number of small-sized mitochondria. The authors proposed that this effect was related to the downregulation of Mfn-2 altering the balance of mitochondrial fusion/fission, but further research is needed to elucidate this process [128].
Conversely, EVs derived from cells within the TME can also affect cancer cell mitochondrial dynamics. Adipocytes have been found to induce a more aggressive phenotype and promote invasiveness of cancer cells [96]. This observation can be achieved by the adipocyte transfer of FA and FAO enzymes via EVs to enhance FAO in cancer cells. This, in turn, alters mitochondrial dynamics to drive increased tumor cell migration. Specifically, increased FAO induces mitochondrial fission and intracellular redistribution of mitochondria to cell protrusions to facilitate cancer cell migration. In parallel, observed mitochondrial size reduction was attributed to EV transfer of mitochondrial fission regulators FIS1 and OPA1, with mitochondrial fission events being identified as crucial for cell migration [55]. CAF-EVs have also been shown to transfer miR-106b to pancreatic cancer where it has been associated with chemotherapy resistance [129]. On a mechanistic level, this miRNA species has been found to induce mitochondrial dysfunction in skeletal muscle by targeting Mfn-2 [130] but more studies are required in the context of cancer.
4.4.2. Intravasation (Trans-Endothelial Migration into Vessels)
After increased cell motility, the next step in the metastatic cascade is the intravasation of tumor cells into the vasculature. TEVs have the capacity to destroy vessel barriers to promote this aspect (Figure 3C). Breast cancer TEVs are able to destroy endothelial barriers by activating endothelial to mesenchymal transition [131], which can be driven by mitochondrial dysfunction [132] and is required for the preparation of the premetastatic niche. miR-34a, present in TEVs [185], can also induce breakdown of the blood–brain barrier (BBB) by inducing a reduction in endothelial OXPHOS, ATP production and cytochrome c, the latter being a downstream target of miR-34a [186]. Another miRNA delivered through EVs that can promote destruction of the BBB is miR-181c [133]. A target of miR-181c is COX1 [134], whose downregulation results in mitochondrial apoptosis [135]. These preliminary but interesting results encourage the need for further investigation that strengthens the knowledge in the link between TEV cargo and the loss of endothelial barrier integrity via manipulation of mitochondrial biology.
5. Nanoparticle-Based Therapeutic Strategies Targeting Mitochondria in Cancer
EVs are key players in intercellular communication through their ability to deliver biological cargo to recipient cells. Thanks to this property, EVs have been considered as vectors for the delivery of both therapeutic endogenous and exogenous cargo. These therapeutic molecules can be loaded into EVs through a number of different mechanisms such as electroporation, or sonication [187]. Synthetic nanoparticles mimicking EVs are also being developed for drug delivery. These synthetic nanoparticles present the advantage of higher standardization, reproducibility, and yield, as well as control over the cargo. However, EVs have the advantage of presenting minimal toxic and immune-related side effects compared to synthetic nanoparticles. A number of studies have explored the potential use of EVs as a cancer therapy by suppressing tumor proliferation, invasion or reversing chemoresistance [188,189]. Given the role of mitochondrial reprogramming in cancer survival through metabolic adaptations and apoptosis resistance, this chapter focuses on the use of EVs as a vehicle to deliver molecules specifically targeting this organelle as a potential cancer therapeutic strategy (Table 2).
Table 2.
Artificially modified EVs as delivery vectors for therapeutic cargo targeting mitochondria. This table summarizes the literature on the use of modified EVs as delivery vectors to obtain a therapeutic effect in the context of cancer by targeting the mitochondria. “EV source” refers to the cell type or biomaterial from which EVs were isolated. “Target cancer” refers to the cancer type investigated in the study. “Enrichment method” refers to the method by which EVs were enriched with the therapeutic molecule of interest. “(Bio)molecule” refers to the therapeutic molecule loaded into EVs. “Target” refers to the mitochondrial component targeted by the therapeutic biomolecule used. “Study type” classifies the studies into in vitro and in vivo depending on the models used. Abbreviations and symbols used: n.i.: not investigated. NA: not applicable. MSC: mesenchymal stem cell. HUVEC: human umbilical vein endothelial cells. ASO: antisense oligonucleotide. ASncmtRNA: antisense non-coding mitochondrial RNA. Mito: mitochondria/l. ↑: increase. ↓ decrease.
| EV Source | Target Cancer | Enrichment Method | (Bio)molecule | Target | Effect on Recipient Cell Mitochondria | Study Type | References |
|---|---|---|---|---|---|---|---|
| EVs enriched in biological cargo | |||||||
| MSCs | Breast | Cell transfection with lentivector | miR-34a | Bcl-2 | Bcl-2↓ | In vitro | [190] |
| HUVECs | Malignant mesothelioma | Cell transfection with transfection reagent | miR-126 | IRS1 | Affected mito metabolism, mito respiration↓ | In vitro | [191,192] |
| Human embryonic kidney (HEK293) cells | Pancreatic | EV transfection via ultrasound | miR-34 | Bcl-2 | Bcl-2↓ | In vitro and in vivo | [193] |
| Human bladder cancer (BIU-87) cells | Bladder | Cell transfection via viral vector (adenovirus) | miR-29c | n.i. | Bcl-2↓, MCL-1↓ | In vitro | [194] |
| Breast cancer (MDA-MB-231 class) cells | Breast | Cell transfection | miR-205 | n.i. | Bcl-2↓ | In vitro | [195] |
| Bovine milk | Pancreatic and colorectal | EV transfection via ultrasound | siRNA | Bcl-2 | Bcl-2↓ | In vitro and in vivo | [196] |
| Acute myeloid leukemia (HL-60 and MOLM-13) cells | Acute myeloid leukemia | Cell transfection with lipofectamine | siRNA | circ_0009910 | Bcl-2↓, Bax↑ | In vitro | [104] |
| Hepatocellular carcinoma (HepG2) cells | Liver | EV transfection via coincubation and oscillation | ASO-G3139 | Bcl-2 | Bcl-2↓ | In vitro | [197] |
| Breast cancer (MDA-MB-231) cells | Breast | Cell transfection with lipofectamine | ASO-1537S | ASncmtRNA | ASncmtRNA↓ | In vitro and in vivo | [198] |
| EVs loaded with exogenous drugs | |||||||
| Tumor cells | Metastatic breast | EV transfection with electroporation | Manganese carbonyl (MnCO) | NA | CO generation which induces mito toxicity | In vitro and in vivo | [199] |
| Non-small cell lung cancer (H1299) cells | Lung | EV coincubation with gold nanoparticles conjugated with doxorubicin | Doxorubicin | NA | Mito damage (perturbation of mito membrane potential), apoptosis via mito pathway↑ | In vitro | [200] |
| Epithelial-like breast cancer (MDA MB-231) cell | Estrogen receptor negative breast | Protein anchorage | Staphylococcal enterotoxin B (SEB) | NA | Bax↑, Bak↑, Bcl-2↓ | In vitro | [201] |
| Epithelial-like pancreatic cancer (MIA Paca-2) | Pancreatic | Protein anchorage | Staphylococcal enterotoxin B (SEB) | NA | Bax↑, Bak↑ | In vitro | [202] |
| Natural Killer (NK-92) | Breast | EV transfection via electroporation | Paclitaxel | NA | Bax/Bcl-2↑ | In vitro | [203] |
5.1. Naturally Occurring EVs
Different cells produce EVs that contain biomolecules with the capacity to eradicate tumor cells through mechanisms that specifically target their mitochondria. For instance, MSC-EVs have a number of potential therapeutic properties without the limitations of their parental cells [204]. Specifically, the potential of stem cell-derived EVs for therapy through the restoration of normal mitochondrial function and reduction of mitochondrial regulated apoptosis has been demonstrated in a variety of conditions such as kidney injury [205,206,207], myocardial infarction [208], Huntington’s disease [209], acute respiratory distress syndrome [210,211] or amyotrophic lateral sclerosis (ALS) [212,213,214]. Unfortunately, cancer cells can take advantage of the therapeutic effects of MSC-EVs in restoring mitochondrial function (see Section 4). Consequently, the role of MSC-EVs in cancer biology is still under investigation as there is supporting evidence for both pro- and antitumor properties [215,216]. For instance, MSC-EVs can induce apoptosis in ovarian cancer [216], HCC [215], leukemia [217], and breast cancer [218] by modulating Bcl-2 family proteins. This effect can be enhanced by combining MSC-EVs with chemotherapeutic agents [219,220]. Although the underlying molecular mechanisms remain unexplored, this effect could be mediated by miRNA cargo as MSC-EV miRNA has been shown to modulate pathways involved in mitochondrial function [216,221]. Furthermore, this mitochondria-mediated therapeutic action is not limited to apoptosis. In the context of cancer cachexia, muscle stem cell derived-EVs can reverse mitochondrial injury through their protein cargo by improving maximal oxygen consumption rate and spare respiratory capacity [222,223], which is a parameter indicative of mitochondrial adaptability to stress conditions [224].
The role of immune cells in killing abnormal cells suggests that their EVs might also hold therapeutic potential. EVs isolated from immune cells have been found to suppress tumor growth [225]. For instance, natural killer (NK)-derived EVs (NK-EVs) have recognized cytotoxic effects and can kill cancer cells through a number of different mechanisms. NK-EVs contain proteins such as granzyme A (GzmA), granzyme B (GzmB) and granulysin (GNLY) all of which have been reported to induce mitochondrial damage [226]. In particular, GzmB induces apoptosis by activating BIG, a member of the proapoptotic Bcl-2 family [227]. NK-EVs have also been shown to induce mitochondria-mediated apoptosis in cancer cells by triggering the release of cytochrome c [226] and altering the expression of Bcl-2 family members [228].
Interestingly, TEVs have also been found to have antitumor properties that can be achieved by activating the mitochondrial apoptotic pathway [229], arresting ATP production [230], and enhancing mitochondrial fusion [69,231]. Unfortunately, the evidence for these effects across different cancer types and the responsible underlying molecular mechanisms is sparse. One example of this effect is the higher level of let-7a found in CRC EVs. This miRNA is able to suppress mitochondrial OXPHOS and, therefore, ATP synthesis through the Lin28a/SDHA signaling pathway, thereby slowing tumor progression [230]. Apart from human cell-derived EVs, EVs from bacteria present in the intestines have also been shown to have antitumor effects on hepatic cancer cells by increasing the Bax/Bcl-2 expression ratio [232].
5.2. Altered EVs
5.2.1. EVs Enriched with Biological Cargo
The high EV efficiency in delivering their cargo to recipient cells has led to the development of several strategies to enrich EVs with therapeutic biomolecules such as miRNAs. Many of these miRNAs are found to be downregulated in cancer and can induce their antitumor effect by altering mitochondrial function (Table 2). For instance, miR-126-enriched EVs can inhibit cell growth by modulating mitochondrial metabolism [191,192]. EVs can also be loaded with different miRNAs that induce cell death via the intrinsic mitochondrial pathway by downregulating Bcl-2 family antiapoptotic proteins [190,193,194,195]. Bcl-2 downregulation can also be achieved by delivering alternative EV cargo biomolecules including silencing RNA (siRNA) and antisense oligonucleotides (ASOs) [196,197] or by depleting EVs of tumorigenic circular RNA (circRNA) [104]. Interestingly, targeting mitochondrial proteins are not the only therapeutic option, as the knock down of antisense non-coding mitochondrial RNA (ASncmtRNA) via EVs was also shown to reduce tumorigenesis [198].
5.2.2. EVs Loaded with Exogenous Drugs
Several cancer therapy strategies have focused on sensitizing cells to mitochondrial apoptosis, for instance, via Bcl-2 inhibitors [233]. In order to deliver these compounds more efficiently and selectively, chemotherapeutic drugs can be packaged into EVs (Table 2). Examples of this approach have been shown with manganese carbonyl and doxorubicin, which selectively induced mitochondrial damage in breast and lung cancer cells [199,200]. In other studies, staphylococcal enterotoxin B-coated TEVs were able to induce apoptosis by targeting Bcl-2 family proteins in estrogen receptor-negative breast and pancreatic cancer cells [201,202]. Apart from TEVs, NK-EVs loaded with paclitaxel were also found to enhance their antitumor effects by inducing apoptosis through the regulation of the Bcl-2/Bax axis [203].
Unsurprisingly, most of the presented EV-mediated strategies focus on reprogramming the mitochondria by inducing apoptosis via the regulation of Bcl-2 family. However, the importance of metabolism in tumor progression has led to the development of clinical trials targeting mitochondrial metabolic pathways as cancer therapy [43]. Given the evidence on the capacity of EV cargo to modulate mitochondrial metabolism, innovative approaches should include cancer therapeutic strategies aimed at tailoring EVs to deliver molecules, such as miRNA, that target this pathway.
6. Conclusions
In the last decade, EVs have emerged as important intercellular communicators involved in the development and progression of a number of pathological conditions including cancer. Cancers exploit dysregulated metabolic pathways to adapt to stress conditions, resist cell death, and alter biosynthesis to sustain increased proliferation. All these events point to a reprogramming of the mitochondria. EVs, through their cargo molecules, can alter mitochondrial biology to give cancer advantages such as metabolic benefits, immune escape, enhanced invasion, and apoptosis escape. However, many of the underlying mechanisms have not been explored in depth and the limited evidence in some cases presents contradictions that highlight the complexity and heterogeneity of cancer mitochondrial phenotypes. For this reason, further studies are needed to better understand the EV-mediated mechanisms and signaling pathways that modulate mitochondria in the TME. Obtaining this knowledge, together with the EV capacity to efficiently transfer molecules to recipient cells, holds the potential to offer new cancer therapeutic avenues based on restoring mitochondrial function using EVs as delivery vectors.
Author Contributions
Conceptualization: R.C.-F., E.P. and S.E.K.; writing—original draft: R.C.-F.; writing—review and editing: R.C.-F., N.H., E.P. and S.E.K.; supervision: N.H., E.P. and S.E.K. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by a donation from the McAlpine family via King’s College Hospital Charity (UK registered charity 1165593).
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 2.Cassim S., Pouyssegur J. Tumor Microenvironment: A Metabolic Player that Shapes the Immune Response. Int. J. Mol. Sci. 2019;21:157. doi: 10.3390/ijms21010157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bebelman M., Smit M.J., Pegtel D.M., Baglio S.R. Biogenesis and function of extracellular vesicles in cancer. Pharmacol. Ther. 2018;188:1–11. doi: 10.1016/j.pharmthera.2018.02.013. [DOI] [PubMed] [Google Scholar]
- 4.Théry C., Witwer K.W., Aikawa E., Alcaraz M.J., Anderson J.D., Andriantsitohaina R., Antoniou A., Arab T., Archer F., Atkin-Smith G.K., et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): A position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles. 2018;7:1535750. doi: 10.1080/20013078.2018.1535750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maisano D., Mimmi S., Dattilo V., Marino F., Gentile M., Vecchio E., Fiume G., Nisticò N., Aloisio A., de Santo M.P., et al. A novel phage display based platform for exosome diversity characterization. Nanoscale. 2022;14:2998–3003. doi: 10.1039/D1NR06804K. [DOI] [PubMed] [Google Scholar]
- 6.Hurley J.H., Hanson P.I. Membrane Budding and Scission by the Escrt Machinery: It’s All in the Neck. Mol. Cell Biol. 2010;11:556–566. doi: 10.1038/nrm2937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raiborg C., Stenmark H. The ESCRT machinery in endosomal sorting of ubiquitylated membrane proteins. Nature. 2009;458:445–452. doi: 10.1038/nature07961. [DOI] [PubMed] [Google Scholar]
- 8.Gurunathan S., Kang M.-H., Kim J.-H. A Comprehensive Review on Factors Influences Biogenesis, Functions, Therapeutic and Clinical Implications of Exosomes. Int. J. Nanomed. 2021;16:1281–1312. doi: 10.2147/IJN.S291956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xavier C.P.R., Caires H.R., Barbosa M.A.G., Bergantim R., Guimarães J.E., Vasconcelos M.H. The Role of Extracellular Vesicles in the Hallmarks of Cancer and Drug Resistance. Cells. 2020;9:1141. doi: 10.3390/cells9051141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jabalee J., Towle R., Garnis C. The Role of Extracellular Vesicles in Cancer: Cargo, Function, and Therapeutic Implications. Cells. 2018;7:93. doi: 10.3390/cells7080093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu R.-T., Huang C.-C., You H.-L., Chou F.-F., Hu C.-C.A., Chao F.-P., Chen C.-M., Cheng J.-T. Overexpression of tumor susceptibility gene TSG101 in human papillary thyroid carcinomas. Oncogene. 2002;21:4830–4837. doi: 10.1038/sj.onc.1205612. [DOI] [PubMed] [Google Scholar]
- 12.Oh K.B., Stanton M.J., West W.W., Todd G.L., Wagner K.-U. Tsg101 is upregulated in a subset of invasive human breast cancers and its targeted overexpression in transgenic mice reveals weak oncogenic properties for mammary cancer initiation. Oncogene. 2007;26:5950–5959. doi: 10.1038/sj.onc.1210401. [DOI] [PubMed] [Google Scholar]
- 13.Toyoshima M., Tanaka N., Aoki J., Tanaka Y., Murata K., Kyuuma M., Kobayashi H., Ishii N., Yaegashi N., Sugamura K. Inhibition of Tumor Growth and Metastasis by Depletion of Vesicular Sorting Protein Hrs: Its Regulatory Role on E-Cadherin and β-Catenin. Cancer Res. 2007;67:5162–5171. doi: 10.1158/0008-5472.CAN-06-2756. [DOI] [PubMed] [Google Scholar]
- 14.Roucourt B., Meeussen S., Bao J., Zimmermann P., David G. Heparanase activates the syndecan-syntenin-ALIX exosome pathway. Cell Res. 2015;25:412–428. doi: 10.1038/cr.2015.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vlodavsky I., Friedmann Y., Elkin M., Aingorn H., Atzmon R., Ishai-Michaeli R., Bitan M., Pappo O., Peretz T., Michal I., et al. Mammalian heparanase: Gene cloning, expression and function in tumor progression and metastasis. Nat. Med. 1999;5:793–802. doi: 10.1038/10518. [DOI] [PubMed] [Google Scholar]
- 16.Kegelman T.P., Das S.K., Emdad L., Hu B., Menezes M.E., Bhoopathi P., Wang X.-Y., Pellecchia M., Sarkar D., Fisher P.B. Targeting Tumor Invasion: The Roles of Mda-9/Syntenin. Expert Opin. Ther. Targets. 2015;19:97–112. doi: 10.1517/14728222.2014.959495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McAndrews K.M., Kalluri R. Mechanisms associated with biogenesis of exosomes in cancer. Mol. Cancer. 2019;18:52. doi: 10.1186/s12943-019-0963-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kucharzewska P., Belting M. Emerging roles of extracellular vesicles in the adaptive response of tumour cells to microenvironmental stress. J. Extracell. Vesicles. 2013;2:20304. doi: 10.3402/jev.v2i0.20304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.King H.W., Michael M.Z., Gleadle J.M. Hypoxic enhancement of exosome release by breast cancer cells. BMC Cancer. 2012;12:421. doi: 10.1186/1471-2407-12-421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Y., Severino P.E., Goliwas K., Hough K., Van Vessem D., Wang H., Frost A.R., Ponnazhagen S., Berry J.L., Deshane J.S. Abstract 1177: Mechanical strain induces phenotypic changes in breast cancer cells and promotes immunosuppression in the tumor microenvironment. Lab. Investig. 2019;100:1503–1516. doi: 10.1038/s41374-020-0452-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen Y., Zhao Y., Yin Y., Jia X., Mao L. Mechanism of cargo sorting into small extracellular vesicles. Bioengineered. 2021;12:8186–8201. doi: 10.1080/21655979.2021.1977767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anand S., Samuel M., Kumar S., Mathivanan S. Ticket to a bubble ride: Cargo sorting into exosomes and extracellular vesicles. Biochim. Biophys. Acta Proteins Proteom. 2019;1867:140203. doi: 10.1016/j.bbapap.2019.02.005. [DOI] [PubMed] [Google Scholar]
- 23.Ruan K., Fang X., Ouyang G. MicroRNAs: Novel regulators in the hallmarks of human cancer. Cancer Lett. 2009;285:116–126. doi: 10.1016/j.canlet.2009.04.031. [DOI] [PubMed] [Google Scholar]
- 24.Macgregor-Das A.M., Das S. A Microrna’s Journey to the Center of the Mitochondria. Am. J. Physiol. -Heart Circ. Physiol. 2018;315:H206–H215. doi: 10.1152/ajpheart.00714.2017. [DOI] [PubMed] [Google Scholar]
- 25.Dragomir M.P., Knutsen E., Calin G. SnapShot: Unconventional miRNA Functions. Cell. 2018;174 doi: 10.1016/j.cell.2018.07.040. [DOI] [PubMed] [Google Scholar]
- 26.Wozniak A.L., Adams A., King K.E., Dunn W., Christenson L.K., Hung W.-T., Weinman S.A. The RNA binding protein FMR1 controls selective exosomal miRNA cargo loading during inflammation. J. Cell Biol. 2020;219:e201912074. doi: 10.1083/jcb.201912074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Villarroya-Beltri C., Gutierrez-Vazquez C., Sanchez-Cabo F., Pérez-Hernández D., Vázquez J., Martin-Cofreces N., Martinez-Herrera D.J., Pascual-Montano A., Mittelbrunn M., Sánchez-Madrid F. Sumoylated hnRNPA2B1 controls the sorting of miRNAs into exosomes through binding to specific motifs. Nat. Commun. 2013;4:2980. doi: 10.1038/ncomms3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Santangelo L., Giurato G., Cicchini C., Montaldo C., Mancone C., Tarallo R., Battistelli C., Alonzi T., Weisz A., Tripodi M. The RNA-Binding Protein SYNCRIP Is a Component of the Hepatocyte Exosomal Machinery Controlling MicroRNA Sorting. Cell Rep. 2016;17:799–808. doi: 10.1016/j.celrep.2016.09.031. [DOI] [PubMed] [Google Scholar]
- 29.Fabbiano F., Corsi J., Gurrieri E., Trevisan C., Notarangelo M., D’Agostino V.G. Rna Packaging into Extracellular Vesicles: An Orchestra of Rna-Binding Proteins? J. Extracell. Vesicles. 2020;10:e12043. doi: 10.1002/jev2.12043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krishn S.R., Salem I., Quaglia F., Naranjo N.M., Agarwal E., Liu Q., Sarker S., Kopenhaver J., McCue P.A., Weinreb P.H., et al. The Avβ6 Integrin in Cancer Cell-Derived Small Extracellular Vesicles Enhances Angiogenesis. J. Extracell. Vesicles. 2020;9:1763594. doi: 10.1080/20013078.2020.1763594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mansour M.A. Ubiquitination: Friend and Foe in Cancer. Int. J. Biochem. Cell Biol. 2018;101:80–93. doi: 10.1016/j.biocel.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 32.Colombo M., Raposo G., Théry C. Biogenesis, secretion, and intercellular interactions of exosomes and other extracellular vesicles. Annu. Rev. Cell Dev. Biol. 2014;30:255–289. doi: 10.1146/annurev-cellbio-101512-122326. [DOI] [PubMed] [Google Scholar]
- 33.Möller A., Lobb R.J. The evolving translational potential of small extracellular vesicles in cancer. Nat. Cancer. 2020;20:697–709. doi: 10.1038/s41568-020-00299-w. [DOI] [PubMed] [Google Scholar]
- 34.Palma E., Tiepolo T., Angelin A., Sabatelli P., Maraldi N.M., Basso E., Forte M.A., Bernardi P., Bonaldo P. Genetic ablation of cyclophilin D rescues mitochondrial defects and prevents muscle apoptosis in collagen VI myopathic mice. Hum. Mol. Genet. 2009;18:2024–2031. doi: 10.1093/hmg/ddp126. [DOI] [PubMed] [Google Scholar]
- 35.Palma E., Riva A., Moreno C., Odena G., Mudan S., Manyakin N., Miquel R., Degré D., Trepo E., Sancho-Bru P., et al. Perturbations in Mitochondrial Dynamics Are Closely Involved in the Progression of Alcoholic Liver Disease. Alcohol. Clin. Exp. Res. 2020;44:856–865. doi: 10.1111/acer.14299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Palma E., Ma X., Riva A., Iansante V., Dhawan A., Wang S., Ni H.-M., Sesaki H., Williams R., Ding W.-X., et al. Dynamin-1–Like Protein Inhibition Drives Megamitochondria Formation as an Adaptive Response in Alcohol-Induced Hepatotoxicity. Am. J. Pathol. 2018;189:580–589. doi: 10.1016/j.ajpath.2018.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zong W.-X., Rabinowitz J.D., White E. Mitochondria and Cancer. Mol. Cell. 2016;61:667–676. doi: 10.1016/j.molcel.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cassim S., Vučetić M., Ždralević M., Pouyssegur J. Warburg and Beyond: The Power of Mitochondrial Metabolism to Collaborate or Replace Fermentative Glycolysis in Cancer. Cancers. 2020;12:1119. doi: 10.3390/cancers12051119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martínez-Reyes I., Chandel N.S. Cancer metabolism: Looking forward. Nat. Cancer. 2021;21:669–680. doi: 10.1038/s41568-021-00378-6. [DOI] [PubMed] [Google Scholar]
- 40.LeBleu V.S., O’Connell J.T., Gonzalez Herrera K.N.G., Wikman H., Pantel K., Haigis M.C., De Carvalho F.M., Damascena A., Domingos Chinen L.T., Rocha R.M., et al. PGC-1α mediates mitochondrial biogenesis and oxidative phosphorylation in cancer cells to promote metastasis. Nat. Cell Biol. 2014;16:992–1003. doi: 10.1038/ncb3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Viale A., Pettazzoni P., Lyssiotis C.A., Ying H., Sanchez N., Marchesini M., Carugo A., Green T., Seth S., Giuliani V., et al. Oncogene ablation-resistant pancreatic cancer cells depend on mitochondrial function. Nature. 2014;514:628–632. doi: 10.1038/nature13611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weinberg F., Hamanaka R., Wheaton W.W., Weinberg S., Joseph J., Lopez M., Kalyanaraman B., Mutlu G.M., Budinger G.R.S., Chandel N.S. Mitochondrial metabolism and ROS generation are essential for Kras-mediated tumorigenicity. Proc. Natl. Acad. Sci. USA. 2010;107:8788–8793. doi: 10.1073/pnas.1003428107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vasan K., Werner M., Chandel N.S. Mitochondrial Metabolism as a Target for Cancer Therapy. Cell Metab. 2020;32:341–352. doi: 10.1016/j.cmet.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pavlova N.N., Thompson C.B. The Emerging Hallmarks of Cancer Metabolism. Cell Metab. 2016;23:27–47. doi: 10.1016/j.cmet.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fong M.Y., Zhou W., Liu L., Alontaga A.Y., Chandra M., Ashby J., Chow A., O’Connor S.T.F., Li S., Chin A.R., et al. Breast-cancer-secreted miR-122 reprograms glucose metabolism in premetastatic niche to promote metastasis. Nat. Cell Biol. 2015;17:183–194. doi: 10.1038/ncb3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen F., Chen J., Yang L., Liu J., Zhang X., Zhang Y., Tu Q., Yin D., Lin D., Wong P.P., et al. Extracellular vesicle-packaged HIF-1α-stabilizing lncRNA from tumour-associated macrophages regulates aerobic glycolysis of breast cancer cells. Nat. Cell Biol. 2019;21:498–510. doi: 10.1038/s41556-019-0299-0. [DOI] [PubMed] [Google Scholar]
- 47.Sung J.S., Kang C.W., Kang S., Jang Y., Chae Y.C., Kim B.G., Cho N.H. ITGB4-mediated metabolic reprogramming of cancer-associated fibroblasts. Oncogene. 2020;39:664–676. doi: 10.1038/s41388-019-1014-0. [DOI] [PubMed] [Google Scholar]
- 48.Fonseca P., Vardaki I., Occhionero A., Panaretakis T. Chapter Five—Metabolic and Signaling Functions of Cancer Cell-Derived Extracellular Vesicles. In: Kwang W.J., Lorenzo G., editors. International Review of Cell and Molecular Biology. Academic Press; Cambridge, MA, USA: 2016. [DOI] [PubMed] [Google Scholar]
- 49.Ma Y., Temkin S.M., Hawkridge A.M., Guo C., Wang W., Wang X.-Y., Fang X. Fatty acid oxidation: An emerging facet of metabolic transformation in cancer. Cancer Lett. 2018;435:92–100. doi: 10.1016/j.canlet.2018.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Deep G., Schlaepfer I.R. Aberrant Lipid Metabolism Promotes Prostate Cancer: Role in Cell Survival under Hypoxia and Extracellular Vesicles Biogenesis. Int. J. Mol. Sci. 2016;17:1061. doi: 10.3390/ijms17071061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang W., Zhu N., Yan T., Shi Y.-N., Chen J., Zhang C.-J., Xie X.-J., Liao D.-F., Qin L. The crosstalk: Exosomes and lipid metabolism. Cell Commun. Signal. 2020;18:1–12. doi: 10.1186/s12964-020-00581-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hurwitz S.N., Rider M.A., Bundy J.L., Liu X., Singh R.K., Meckes D.G., Jr. Proteomic profiling of NCI-60 extracellular vesicles uncovers common protein cargo and cancer type-specific biomarkers. Oncotarget. 2016;7:86999–87015. doi: 10.18632/oncotarget.13569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liang B., Peng P., Chen S., Li L., Zhang M., Cao D., Yang J., Li H., Gui T., Li X., et al. Characterization and proteomic analysis of ovarian cancer-derived exosomes. J. Proteom. 2013;80:171–182. doi: 10.1016/j.jprot.2012.12.029. [DOI] [PubMed] [Google Scholar]
- 54.Park J.O., Choi D.-Y., Choi D.-S., Kim H.J., Kang J.W., Jung J.H., Lee J.H., Kim J., Freeman M.R., Lee K.Y., et al. Identification and characterization of proteins isolated from microvesicles derived from human lung cancer pleural effusions. Proteomics. 2013;13:2125–2134. doi: 10.1002/pmic.201200323. [DOI] [PubMed] [Google Scholar]
- 55.Clement E., Lazar I., Attané C., Carrié L., Dauvillier S., Ducoux-Petit M., Esteve D., Menneteau T., Moutahir M., Le Gonidec S., et al. Adipocyte extracellular vesicles carry enzymes and fatty acids that stimulate mitochondrial metabolism and remodeling in tumor cells. EMBO J. 2020;39:e102525. doi: 10.15252/embj.2019102525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Puhka M., Takatalo M., Nordberg M.-E., Valkonen S., Nandania J., Aatonen M., Yliperttula M., Laitinen S., Velagapudi V., Mirtti T., et al. Metabolomic Profiling of Extracellular Vesicles and Alternative Normalization Methods Reveal Enriched Metabolites and Strategies to Study Prostate Cancer-Related Changes. Theranostics. 2017;7:3824–3841. doi: 10.7150/thno.19890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yang L., Achreja A., Yeung T.-L., Mangala L.S., Jiang D., Han C., Baddour J., Marini J.C., Ni J., Nakahara R., et al. Targeting Stromal Glutamine Synthetase in Tumors Disrupts Tumor Microenvironment-Regulated Cancer Cell Growth. Cell Metab. 2016;24:685–700. doi: 10.1016/j.cmet.2016.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Villar V.H., Merhi F., Djavaheri-Mergny M., Durán R.V. Glutaminolysis and Autophagy in Cancer. Autophagy. 2015;11:1198–1208. doi: 10.1080/15548627.2015.1053680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Altman B.J., Stine Z.E., Dang C.V. From Krebs to Clinic: Glutamine Metabolism to Cancer Therapy. Nat. Rev. Cancer. 2016;16:619–634. doi: 10.1038/nrc.2016.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wu Q., Li B., Li Z., Li J., Sun S., Sun S. Cancer-associated adipocytes: Key players in breast cancer progression. J. Hematol. Oncol. 2019;12:95. doi: 10.1186/s13045-019-0778-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Balendiran G.K., Dabur R., Fraser D. The role of glutathione in cancer. Cell Biochem. Funct. 2004;22:343–352. doi: 10.1002/cbf.1149. [DOI] [PubMed] [Google Scholar]
- 62.Ko Y.-H., Lin Z., Flomenberg N., Pestell R.G., Howell A., Sotgia F., Lisanti M.P., Martinez-Outschoorn U.E. Glutamine Fuels a Vicious Cycle of Autophagy in the Tumor Stroma and Oxidative Mitochondrial Metabolism in Epithelial Cancer Cells: Implications for Preventing Chemotherapy Resistance. Cancer Biol. Ther. 2011;12:1085–1097. doi: 10.4161/cbt.12.12.18671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fan S., Kroeger B., Marie P.P., Bridges E.M., Mason J.D., McCormick K., E Zois C., Sheldon H., Alham N.K., Johnson E., et al. Glutamine deprivation alters the origin and function of cancer cell exosomes. EMBO J. 2020;39:e103009. doi: 10.15252/embj.2019103009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Simula L., Nazio F., Campello S. The mitochondrial dynamics in cancer and immune-surveillance. Semin. Cancer Biol. 2017;47:29–42. doi: 10.1016/j.semcancer.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 65.Zhang Z., Li T.-E., Chen M., Xu D., Zhu Y., Hu B.-Y., Lin Z.-F., Pan J.-J., Wang X., Wu C., et al. MFN1-dependent alteration of mitochondrial dynamics drives hepatocellular carcinoma metastasis by glucose metabolic reprogramming. Br. J. Cancer. 2019;122:209–220. doi: 10.1038/s41416-019-0658-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kashatus D.F. The regulation of tumor cell physiology by mitochondrial dynamics. Biochem. Biophys. Res. Commun. 2018;500:9–16. doi: 10.1016/j.bbrc.2017.06.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ma Y., Wang L., Jia R. The role of mitochondrial dynamics in human cancers. Am. J. Cancer Res. 2020;10:1278–1293. [PMC free article] [PubMed] [Google Scholar]
- 68.Zhao J., Zhang J., Yu M., Xie Y., Huang Y., Wolff D.W., Abel P.W., Tu Y. Mitochondrial dynamics regulates migration and invasion of breast cancer cells. Oncogene. 2013;32:4814–4824. doi: 10.1038/onc.2012.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kannan A., Wells R.B., Sivakumar S., Komatsu S., Singh K.P., Samten B., Philley J.V., Sauter E.R., Ikebe M., Idell S., et al. Mitochondrial Reprogramming Regulates Breast Cancer Progression. Clin. Cancer Res. 2016;22:3348–3360. doi: 10.1158/1078-0432.CCR-15-2456. [DOI] [PubMed] [Google Scholar]
- 70.Rehman J., Zhang H.J., Toth P.T., Zhang Y., Marsboom G., Hong Z., Salgia R., Husain A.N., Wietholt C., Archer S.L. Inhibition of Mitochondrial Fission Prevents Cell Cycle Progression in Lung Cancer. FASEB J. 2012;26:2175–2186. doi: 10.1096/fj.11-196543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Xie Q., Wu Q., Horbinski C.M., Flavahan W.A., Yang K., Zhou W., Dombrowski S.M., Huang Z., Fang X., Shi Y., et al. Mitochondrial control by DRP1 in brain tumor initiating cells. Nat. Neurosci. 2015;18:501–510. doi: 10.1038/nn.3960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Xu K., Chen G., Li X., Wu X., Chang Z., Xu J., Zhu Y., Yin P., Liang X., Dong L. Mfn2 Suppresses Cancer Progression through Inhibition of Mtorc2/Akt Signaling. Sci. Rep. 2017;7:41718. doi: 10.1038/srep41718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Panigrahi D.P., Praharaj P.P., Bhol C.S., Mahapatra K.K., Patra S., Behera B.P., Mishra S.R., Bhutia S.K. The emerging, multifaceted role of mitophagy in cancer and cancer therapeutics. Semin. Cancer Biol. 2019;66:45–58. doi: 10.1016/j.semcancer.2019.07.015. [DOI] [PubMed] [Google Scholar]
- 74.Ferro F., Servais S., Besson P., Roger S., Dumas J.-F., Brisson L. Autophagy and Mitophagy in Cancer Metabolic Remodelling. Semin. Cell Dev. Biol. 2020;98:129–138. doi: 10.1016/j.semcdb.2019.05.029. [DOI] [PubMed] [Google Scholar]
- 75.Suárez H., Andreu Z., Mazzeo C., Toribio V., Pérez-Rivera A.E., López-Martín S., García-Silva S., Hurtado B., Morato E., Peláez L., et al. CD9 inhibition reveals a functional connection of extracellular vesicle secretion with mitophagy in melanoma cells. J. Extracell. Vesicles. 2021;10:e12082. doi: 10.1002/jev2.12082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Letts J., Sazanov L. Clarifying the supercomplex: The higher-order organization of the mitochondrial electron transport chain. Nat. Struct. Mol. Biol. 2017;24:800–808. doi: 10.1038/nsmb.3460. [DOI] [PubMed] [Google Scholar]
- 77.Cogliati S., Frezza C., Soriano M.E., Varanita T., Quintana-Cabrera R., Corrado M., Cipolat S., Costa V., Casarin A., Gomes L.C., et al. Mitochondrial Cristae Shape Determines Respiratory Chain Supercomplexes Assembly and Respiratory Efficiency. Cell. 2013;155:160–171. doi: 10.1016/j.cell.2013.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pernas L., Scorrano L. Mito-Morphosis: Mitochondrial Fusion, Fission, and Cristae Remodeling as Key Mediators of Cellular Function. Annu. Rev. Physiol. 2016;78:505–531. doi: 10.1146/annurev-physiol-021115-105011. [DOI] [PubMed] [Google Scholar]
- 79.Colina-Tenorio L., Horten P., Pfanner N., Rampelt H. Shaping the mitochondrial inner membrane in health and disease. J. Intern. Med. 2020;287:645–664. doi: 10.1111/joim.13031. [DOI] [PubMed] [Google Scholar]
- 80.Eramo M., Lisnyak V., Formosa L., Ryan M.T. The ‘mitochondrial contact site and cristae organising system’ (MICOS) in health and human disease. J. Biochem. 2019;167:243–255. doi: 10.1093/jb/mvz111. [DOI] [PubMed] [Google Scholar]
- 81.Peña-Blanco A., García-Sáez A.J. Bax, Bak and Beyond—Mitochondrial Performance in Apoptosis. FEBS J. 2018;285:416–431. doi: 10.1111/febs.14186. [DOI] [PubMed] [Google Scholar]
- 82.Carneiro B.A., El-Deiry W.S. Targeting apoptosis in cancer therapy. Nat. Rev. Clin. Oncol. 2020;17:395–417. doi: 10.1038/s41571-020-0341-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wong R.S.Y. Apoptosis in Cancer: From Pathogenesis to Treatment. J. Exp. Clin. Cancer Res. 2011;30:87. doi: 10.1186/1756-9966-30-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang D., Wang Y., Shi Z., Liu J., Sun P., Hou X., Zhang J., Zhao S., Zhou B.P., Mi J. Metabolic Reprogramming of Cancer-Associated Fibroblasts by IDH3α Downregulation. Cell Rep. 2015;10:1335–1348. doi: 10.1016/j.celrep.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 85.Albino D., Falcione M., Uboldi V., Temilola D.O., Sandrini G., Merulla J., Civenni G., Kokanovic A., Stürchler A., Shinde D., et al. Circulating extracellular vesicles release oncogenic miR-424 in experimental models and patients with aggressive prostate cancer. Commun. Biol. 2021;4:119. doi: 10.1038/s42003-020-01642-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rai A., Greening D.W., Chen M., Xu R., Ji H., Simpson R.J. Exosomes Derived from Human Primary and Metastatic Colorectal Cancer Cells Contribute to Functional Heterogeneity of Activated Fibroblasts by Reprogramming Their Proteome. Proteomics. 2019;19:1800148. doi: 10.1002/pmic.201800148. [DOI] [PubMed] [Google Scholar]
- 87.La Shu S., Yang Y., Allen C.L., Maguire O., Minderman H., Sen A., Ciesielski M.J., Collins K.A., Bush P.J., Singh P., et al. Metabolic reprogramming of stromal fibroblasts by melanoma exosome microRNA favours a pre-metastatic microenvironment. Sci. Rep. 2018;8:12905. doi: 10.1038/s41598-018-31323-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fan J., Xu G., Chang Z., Zhu L., Yao J. Mir-210 Transferred by Lung Cancer Cell-Derived Exosomes May Act as Proangiogenic Factor in Cancer-Associated Fibroblasts by Modulating Jak2/Stat3 Pathway. Clin. Sci. 2020;134:807–825. doi: 10.1042/CS20200039. [DOI] [PubMed] [Google Scholar]
- 89.Puissegur M.-P., Mazure N.M., Bertero T., Pradelli L., Grosso S., Robbe-Sermesant K., Maurin T., Lebrigand K., Cardinaud B., Hofman V., et al. miR-210 is overexpressed in late stages of lung cancer and mediates mitochondrial alterations associated with modulation of HIF-1 activity. Cell Death Differ. 2010;18:465–478. doi: 10.1038/cdd.2010.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wu X., Zhou Z., Xu S., Liao C., Chen X., Li B., Peng J., Li D., Yang L. Extracellular vesicle packaged LMP1-activated fibroblasts promote tumor progression via autophagy and stroma-tumor metabolism coupling. Cancer Lett. 2020;478:93–106. doi: 10.1016/j.canlet.2020.03.004. [DOI] [PubMed] [Google Scholar]
- 91.Li Y., Zhao Z., Liu W., Li X. SNHG3 Functions as miRNA Sponge to Promote Breast Cancer Cells Growth Through the Metabolic Reprogramming. Appl. Biochem. Biotechnol. 2020;191:1084–1099. doi: 10.1007/s12010-020-03244-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhao H., Yang L., Baddour J., Achreja A., Bernard V., Moss T., Marini J.C., Tudawe T., Seviour E.G., Lucas F.A.S., et al. Author response: Tumor microenvironment derived exosomes pleiotropically modulate cancer cell metabolism. eLife. 2015 doi: 10.7554/elife.10250.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Achreja A., Zhao H., Yang L., Yun T.H., Marini J., Nagrath D. Exo-MFA—A 13C metabolic flux analysis framework to dissect tumor microenvironment-secreted exosome contributions towards cancer cell metabolism. Metab. Eng. 2017;43:156–172. doi: 10.1016/j.ymben.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ham I.-H., Lee D., Hur H. Cancer-Associated Fibroblast-Induced Resistance to Chemotherapy and Radiotherapy in Gastrointestinal Cancers. Cancers. 2021;13:1172. doi: 10.3390/cancers13051172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Zhang Z., Jiang H., Li X., Chen X., Huang Y. Mir-92a Regulates Brown Adipocytes Differentiation, Mitochondrial Oxidative Respiration, and Heat Generation by Targeting Smad7. J. Cell. Biochem. 2020;121:3825–3836. doi: 10.1002/jcb.29539. [DOI] [PubMed] [Google Scholar]
- 96.Wu Q., Sun S., Li Z., Yang Q., Li B., Zhu S., Wang L., Wu J., Yuan J., Yang C., et al. Tumour-originated exosomal miR-155 triggers cancer-associated cachexia to promote tumour progression. Mol. Cancer. 2018;17:155. doi: 10.1186/s12943-018-0899-5. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 97.Wu Q., Li J., Li Z., Sun S., Zhu S., Wang L., Wu J., Yuan J., Zhang Y., Sun S., et al. Exosomes from the tumour-adipocyte interplay stimulate beige/brown differentiation and reprogram metabolism in stromal adipocytes to promote tumour progression. J. Exp. Clin. Cancer Res. 2019;38:223. doi: 10.1186/s13046-019-1210-3. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 98.Lazar I., Clement E., Dauvillier S., Milhas D., Ducoux-Petit M., LeGonidec S., Moro C., Soldan V., Dalle S., Balor S., et al. Adipocyte Exosomes Promote Melanoma Aggressiveness through Fatty Acid Oxidation: A Novel Mechanism Linking Obesity and Cancer. Cancer Res. 2016;76:4051–4057. doi: 10.1158/0008-5472.CAN-16-0651. [DOI] [PubMed] [Google Scholar]
- 99.Liu Y., Tan J., Ou S., Chen J., Chen L. Adipose-derived exosomes deliver miR-23a/b to regulate tumor growth in hepatocellular cancer by targeting the VHL/HIF axis. J. Physiol. Biochem. 2019;75:391–401. doi: 10.1007/s13105-019-00692-6. [DOI] [PubMed] [Google Scholar]
- 100.Gao P., Tchernyshyov I., Chang T.-C., Lee Y.-S., Kita K., Ochi T., Zeller K.I., De Marzo A.M., Van Eyk J.E., Mendell J.T., et al. c-Myc suppression of miR-23a/b enhances mitochondrial glutaminase expression and glutamine metabolism. Nature. 2009;458:762–765. doi: 10.1038/nature07823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yogev O., Henderson S., Hayes M.J., Marelli S.S., Ofir-Birin Y., Regev-Rudzki N., Herrero J., Enver T. Herpesviruses shape tumour microenvironment through exosomal transfer of viral microRNAs. PLoS Pathog. 2017;13:e1006524. doi: 10.1371/journal.ppat.1006524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Matsumoto A., Takahashi Y., Nishikawa M., Sano K., Morishita M., Charoenviriyakul C., Saji H., Takakura Y. Accelerated growth of B16 BL 6 tumor in mice through efficient uptake of their own exosomes by B16 BL 6 cells. Cancer Sci. 2017;108:1803–1810. doi: 10.1111/cas.13310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yang L., Wu X.-H., Wang D., Luo C.-L., Chen L.-X. Bladder cancer cell-derived exosomes inhibit tumor cell apoptosis and induce cell proliferation in vitro. Mol. Med. Rep. 2013;8:1272–1278. doi: 10.3892/mmr.2013.1634. [DOI] [PubMed] [Google Scholar]
- 104.Wang D., Ming X., Xu J., Xiao Y. Circ_0009910 Shuttled by Exosomes Regulates Proliferation, Cell Cycle and Apoptosis of Acute Myeloid Leukemia Cells by Regulating Mir-5195-3p/Grb10 Axis. Hematol. Oncol. 2021;39:390–400. doi: 10.1002/hon.2874. [DOI] [PubMed] [Google Scholar]
- 105.Lang H.-L., Hu G.-W., Zhang B., Kuang W., Chen Y., Wu L., Xu G.-H. Glioma cells enhance angiogenesis and inhibit endothelial cell apoptosis through the release of exosomes that contain long non-coding RNA CCAT2. Oncol. Rep. 2017;38:785–798. doi: 10.3892/or.2017.5742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Deng M., Yuan H., Liu S., Hu Z., Xiao H. Exosome-transmitted LINC00461 promotes multiple myeloma cell proliferation and suppresses apoptosis by modulating microRNA/BCL-2 expression. Cytotherapy. 2019;21:96–106. doi: 10.1016/j.jcyt.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 107.Dong H., Wang W., Chen R., Zhang Y., Zou K., Ye M., He X., Zhang F., Han J. Exosome-mediated transfer of lncRNA-SNHG14 promotes trastuzumab chemoresistance in breast cancer. Int. J. Oncol. 2018;53:1013–1026. doi: 10.3892/ijo.2018.4467. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 108.Kang M., Ren M., Li Y., Fu Y., Deng M., Li C. Exosome-mediated transfer of lncRNA PART1 induces gefitinib resistance in esophageal squamous cell carcinoma via functioning as a competing endogenous RNA. J. Exp. Clin. Cancer Res. 2018;37:171. doi: 10.1186/s13046-018-0845-9. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 109.Zhang Y., Li M., Hu C. Exosomal transfer of miR-214 mediates gefitinib resistance in non-small cell lung cancer. Biochem. Biophys. Res. Commun. 2018;507:457–464. doi: 10.1016/j.bbrc.2018.11.061. [DOI] [PubMed] [Google Scholar]
- 110.Zhao K., Wang Z., Li X., Liu J.-L., Tian L., Chen J.-Q. Exosome-mediated transfer of CLIC1 contributes to the vincristine-resistance in gastric cancer. Mol. Cell. Biochem. 2019;462:97–105. doi: 10.1007/s11010-019-03613-9. [DOI] [PubMed] [Google Scholar]
- 111.Hu W., Xu Z., Zhu S., Sun W., Wang X., Tan C., Zhang Y., Zhang G., Xu Y., Tang J. Small extracellular vesicle-mediated Hsp70 intercellular delivery enhances breast cancer adriamycin resistance. Free Radic. Biol. Med. 2021;164:85–95. doi: 10.1016/j.freeradbiomed.2020.12.436. [DOI] [PubMed] [Google Scholar]
- 112.Yang Z.-J., Zhang L.-L., Bi Q.-C., Gan L.-J., Wei M.-J., Hong T., Tan R.-J., Lan X.-M., Liu L.-H., Han X.-J., et al. Exosomal connexin 43 regulates the resistance of glioma cells to temozolomide. Oncol. Rep. 2021;45:44. doi: 10.3892/or.2021.7995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Li X.-Q., Liu J.-T., Fan L.-L., Liu Y., Cheng L., Wang F., Yu H.-Q., Gao J., Wei W., Wang H., et al. Exosomes derived from gefitinib-treated EGFR-mutant lung cancer cells alter cisplatin sensitivity via up-regulating autophagy. Oncotarget. 2016;7:24585–24595. doi: 10.18632/oncotarget.8358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hu J.L., Wang W., Lan X.L., Zeng Z.C., Liang Y.S., Yan Y.R., Song F.Y., Wang F.F., Zhu X.H., Liao W.J., et al. CAFs secreted exosomes promote metastasis and chemotherapy resistance by enhancing cell stemness and epithelial-mesenchymal transition in colorectal cancer. Mol. Cancer. 2019;18:91. doi: 10.1186/s12943-019-1019-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Liu Y., Lu Y., Li A., Song H., Zhang W., Gilbert M., Yang C. CBMT-46, Microenvironment-derived mitochondria prime glioma chemoresistance by augmenting Nad+ Metabolism and parp-dependent DNA repair. Neuro Oncol. 2018;20:vi42. doi: 10.1093/neuonc/noy148.165. [DOI] [Google Scholar]
- 116.Salaud C., Alvarez-Arenas A., Geraldo F., Belmonte-Beitia J., Calvo G.F., Gratas C., Pecqueur C., Garnier D., Pérez-Garcià V., Vallette F.M., et al. Mitochondria transfer from tumor-activated stromal cells (TASC) to primary Glioblastoma cells. Biochem. Biophys. Res. Commun. 2020;533:139–147. doi: 10.1016/j.bbrc.2020.08.101. [DOI] [PubMed] [Google Scholar]
- 117.Sansone P., Savini C., Kurelac I., Chang Q., Amato L.B., Strillacci A., Stepanova A., Iommarini L., Mastroleo C., Daly L., et al. Packaging and transfer of mitochondrial DNA via exosomes regulate escape from dormancy in hormonal therapy-resistant breast cancer. Proc. Natl. Acad. Sci. USA. 2017;114:E9066–E9075. doi: 10.1073/pnas.1704862114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Seo W., Gao Y., He Y., Sun J., Xu H., Feng D., Park S.H., Cho Y.-E., Guillot A., Ren T., et al. ALDH2 deficiency promotes alcohol-associated liver cancer by activating oncogenic pathways via oxidized DNA-enriched extracellular vesicles. J. Hepatol. 2019;71:1000–1011. doi: 10.1016/j.jhep.2019.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pritchard A., Tousif S., Wang Y., Hough K., Khan S., Strenkowski J., Chacko B.K., Darley-Usmar V.M., Deshane J.S. Lung Tumor Cell-Derived Exosomes Promote M2 Macrophage Polarization. Cells. 2020;9:1303. doi: 10.3390/cells9051303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Park J.E., Dutta B., Tse S.W., Gupta N., Tan C.F., Low J.K., Yeoh K.W., Kon O.L., Tam J.P., Sze S.K. Hypoxia-Induced Tumor Exosomes Promote M2-Like Macrophage Polarization of Infiltrating Myeloid Cells and Microrna-Mediated Metabolic Shift. Oncogene. 2019;38:5158–5173. doi: 10.1038/s41388-019-0782-x. [DOI] [PubMed] [Google Scholar]
- 121.Bland C.L., Byrne-Hoffman C.N., Fernandez A., Rellick S.L., Deng W., Klinke D.J. Exosomes derived from B16F0 melanoma cells alter the transcriptome of cytotoxic T cells that impacts mitochondrial respiration. FEBS J. 2018;285:1033–1050. doi: 10.1111/febs.14396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhou J., Yang Y., Wang W., Zhang Y., Chen Z., Hao C., Zhang J. Melanoma-released exosomes directly activate the mitochondrial apoptotic pathway of CD4+ T cells through their microRNA cargo. Exp. Cell Res. 2018;371:364–371. doi: 10.1016/j.yexcr.2018.08.030. [DOI] [PubMed] [Google Scholar]
- 123.Yang L., Wu X., Wang D., Luo C., Chen L. Renal Carcinoma Cell-Derived Exosomes Induce Human Immortalized Line of Jurkat T Lymphocyte Apoptosis in vitro. Urol. Int. 2013;91:363–369. doi: 10.1159/000348747. [DOI] [PubMed] [Google Scholar]
- 124.Czystowska-Kuźmicz M., Han J., Szczepanski M.J., Szajnik M., Quadrini K., Brandwein H., Hadden J.W., Signorelli K., Whiteside T.L. IRX-2, a novel immunotherapeutic, protects human T cells from tumor-induced cell death. Cell Death Differ. 2009;16:708–718. doi: 10.1038/cdd.2008.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Rashid M.H., Borin T.F., Ara R., Piranlioglu R., Achyut B.R., Korkaya H., Liu Y., Arbab A.S. Critical immunosuppressive effect of MDSC-derived exosomes in the tumor microenvironment. Oncol. Rep. 2021;45:1171–1181. doi: 10.3892/or.2021.7936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hildeman D.A., Mitchell T., Kappler J., Marrack P. T cell apoptosis and reactive oxygen species. J. Clin. Investig. 2003;111:575–581. doi: 10.1172/JCI200318007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bertolini I., Ghosh J.C., Kossenkov A.V., Mulugu S., Krishn S.R., Vaira V., Qin J., Plow E.F., Languino L.R., Altieri D.C. Small Extracellular Vesicle Regulation of Mitochondrial Dynamics Reprograms a Hypoxic Tumor Microenvironment. Dev. Cell. 2020;55:163–177.e6. doi: 10.1016/j.devcel.2020.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wu C.-H., Silvers C.R., Messing E.M., Lee Y.-F. Bladder cancer extracellular vesicles drive tumorigenesis by inducing the unfolded protein response in endoplasmic reticulum of nonmalignant cells. J. Biol. Chem. 2019;294:3207–3218. doi: 10.1074/jbc.RA118.006682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Fang Y., Zhou W., Rong Y., Kuang T., Xu X., Wu W., Wang D., Lou W. Exosomal miRNA-106b from cancer-associated fibroblast promotes gemcitabine resistance in pancreatic cancer. Exp. Cell Res. 2019;383:111543. doi: 10.1016/j.yexcr.2019.111543. [DOI] [PubMed] [Google Scholar]
- 130.Zhang Y., Yang L., Gao Y.-F., Fan Z.-M., Cai X.-Y., Liu M.-Y., Guo X.-R., Gao C.-L., Xia Z.-K. MicroRNA-106b induces mitochondrial dysfunction and insulin resistance in C2C12 myotubes by targeting mitofusin-2. Mol. Cell. Endocrinol. 2013;381:230–240. doi: 10.1016/j.mce.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 131.Kim J., Lee C., Kim I., Ro J., Kim J., Min Y., Park J., Sunkara V., Park Y.-S., Michael I., et al. Three-Dimensional Human Liver-Chip Emulating Premetastatic Niche Formation by Breast Cancer-Derived Extracellular Vesicles. ACS Nano. 2020;14:14971–14988. doi: 10.1021/acsnano.0c04778. [DOI] [PubMed] [Google Scholar]
- 132.Hua W., Dijke P.T., Kostidis S., Giera M., Hornsveld M. TGFβ-induced metabolic reprogramming during epithelial-to-mesenchymal transition in cancer. Cell. Mol. Life Sci. 2019;77:2103–2123. doi: 10.1007/s00018-019-03398-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tominaga N., Kosaka N., Ono M., Katsuda T., Yoshioka Y., Tamura K., Lötvall J., Nakagama H., Ochiya T. Brain metastatic cancer cells release microRNA-181c-containing extracellular vesicles capable of destructing blood–brain barrier. Nat. Commun. 2015;6:6716. doi: 10.1038/ncomms7716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Gusic M., Prokisch H. Ncrnas: New Players in Mitochondrial Health and Disease? Front. Genet. 2020;11:95. doi: 10.3389/fgene.2020.00095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Ding L., Gu H., Lan Z., Lei Q., Wang W., Ruan J., Yu M., Lin J., Cui Q. Downregulation of Cyclooxygenase-1 Stimulates Mitochondrial Apoptosis through the Nf-Κb Signaling Pathway in Colorectal Cancer Cells. Oncol. Rep. 2019;41:559–569. doi: 10.3892/or.2018.6785. [DOI] [PubMed] [Google Scholar]
- 136.Gentric G., Mechta-Grigoriou F. Tumor Cells and Cancer-Associated Fibroblasts: An Updated Metabolic Perspective. Cancers. 2021;13:399. doi: 10.3390/cancers13030399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Nurmik M., Ullmann P., Rodriguez F., Haan S., Letellier E. In search of definitions: Cancer-associated fibroblasts and their markers. Int. J. Cancer. 2019;146:895–905. doi: 10.1002/ijc.32193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Avagliano A., Granato G., Ruocco M.R., Romano V., Belviso I., Carfora A., Montagnani S., Arcucci A. Metabolic Reprogramming of Cancer Associated Fibroblasts: The Slavery of Stromal Fibroblasts. BioMed Res. Int. 2018;2018:6075403. doi: 10.1155/2018/6075403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Roy A., Bera S. CAF cellular glycolysis: Linking cancer cells with the microenvironment. Tumor Biol. 2016;37:8503–8514. doi: 10.1007/s13277-016-5049-3. [DOI] [PubMed] [Google Scholar]
- 140.Lengyel E., Makowski L., DiGiovanni J., Kolonin M.G. Cancer as a Matter of Fat: The Crosstalk between Adipose Tissue and Tumors. Trends Cancer. 2018;4:374–384. doi: 10.1016/j.trecan.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Barquissau V., Beuzelin D., Pisani D.F., Beranger G.E., Mairal A., Montagner A., Roussel B., Tavernier G., Marques M.-A., Moro C., et al. White-to-brite conversion in human adipocytes promotes metabolic reprogramming towards fatty acid anabolic and catabolic pathways. Mol. Metab. 2016;5:352–365. doi: 10.1016/j.molmet.2016.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Sah R.P., Sharma A., Nagpal S., Patlolla S.H., Sharma A., Kandlakunta H., Anani V., Angom R.S., Kamboj A.K., Ahmed N., et al. Phases of Metabolic and Soft Tissue Changes in Months Preceding a Diagnosis of Pancreatic Ductal Adenocarcinoma. Gastroenterology. 2019;156:1742–1752. doi: 10.1053/j.gastro.2019.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sarosiek K.A., Ni Chonghaile T., Letai A. Mitochondria: Gatekeepers of response to chemotherapy. Trends Cell Biol. 2013;23:612–619. doi: 10.1016/j.tcb.2013.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Elliott R.L., Jiang X.P., Head J.F. Mitochondria organelle transplantation: Introduction of normal epithelial mitochondria into human cancer cells inhibits proliferation and increases drug sensitivity. Breast Cancer Res. Treat. 2012;136:347–354. doi: 10.1007/s10549-012-2283-2. [DOI] [PubMed] [Google Scholar]
- 145.Sun C., Wang Z., Liu Y., Liu Y., Li H., Di C., Wu Z., Gan L., Zhang H. Carbon ion beams induce hepatoma cell death by NADPH oxidase-mediated mitochondrial damage. J. Cell. Physiol. 2013;229:100–107. doi: 10.1002/jcp.24424. [DOI] [PubMed] [Google Scholar]
- 146.Kreger B.T., Johansen E.R., Cerione R.A., Antonyak M.A. The Enrichment of Survivin in Exosomes from Breast Cancer Cells Treated with Paclitaxel Promotes Cell Survival and Chemoresistance. Cancers. 2016;8:111. doi: 10.3390/cancers8120111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Cappellesso R., Tinazzi A., Giurici T., Simonato F., Guzzardo V., Ventura L., Crescenzi M., Chiarelli S., Fassina A. Programmed cell death 4 and microRNA 21 inverse expression is maintained in cells and exosomes from ovarian serous carcinoma effusions. Cancer Cytopathol. 2014;122:685–693. doi: 10.1002/cncy.21442. [DOI] [PubMed] [Google Scholar]
- 148.Hmadcha A., Martin-Montalvo A., Gauthier B., Soria B., Capilla-Gonzalez V. Therapeutic Potential of Mesenchymal Stem Cells for Cancer Therapy. Front. Bioeng. Biotechnol. 2020;8:43. doi: 10.3389/fbioe.2020.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wang H., Huang H., Wang L., Liu Y., Wang M., Zhao S., Lu G., Kang X. Cancer-associated fibroblasts secreted miR-103a-3p suppresses apoptosis and promotes cisplatin resistance in non-small cell lung cancer. Aging. 2021;13:14456–14468. doi: 10.18632/aging.103556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Cai J., Wang J., Huang Y., Wu H.-X., Xia T., Xiao J., Chen X., Li H., Qiu Y., Wang Y., et al. ERK/Drp1-dependent mitochondrial fission is involved in the MSC-induced drug resistance of T-cell acute lymphoblastic leukemia cells. Cell Death Dis. 2016;7:e2459. doi: 10.1038/cddis.2016.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Islam M.N., Das S.R., Emin M.T., Wei M., Sun L., Westphalen K., Rowlands D.J., Quadri S.K., Bhattacharya S., Bhattacharya J. Mitochondrial transfer from bone-marrow–derived stromal cells to pulmonary alveoli protects against acute lung injury. Nat. Med. 2012;18:759–765. doi: 10.1038/nm.2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Hayakawa K., Esposito E., Wang X., Terasaki Y., Liu Y., Xing C., Ji X., Lo E.H. Transfer of mitochondria from astrocytes to neurons after stroke. Nature. 2016;535:551–555. doi: 10.1038/nature18928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.MohammadAlipour A., Dumbali S.P., Wenzel P.L. Mitochondrial Transfer and Regulators of Mesenchymal Stromal Cell Function and Therapeutic Efficacy. Front. Cell Dev. Biol. 2020;8:603292. doi: 10.3389/fcell.2020.603292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Hough K., Trevor J.L., Strenkowski J.G., Wang Y., Chacko B.K., Tousif S., Chanda D., Steele C., Antony V.B., Dokland T., et al. Exosomal transfer of mitochondria from airway myeloid-derived regulatory cells to T cells. Redox Biol. 2018;18:54–64. doi: 10.1016/j.redox.2018.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Dong L.-F., Kovarova J., Bajzikova M., Bezawork-Geleta A., Svec D., Endaya B., Sachaphibulkij K., Coelho A.R., Sebkova N., Ruzickova A., et al. Horizontal transfer of whole mitochondria restores tumorigenic potential in mitochondrial DNA-deficient cancer cells. eLife. 2017;6:e22187. doi: 10.7554/eLife.22187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Griessinger E., Moschoi R., Biondani G., Peyron J.-F. Mitochondrial Transfer in the Leukemia Microenvironment. Trends Cancer. 2017;3:828–839. doi: 10.1016/j.trecan.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 157.Li Y., Guo X., Guo S., Wang Y., Chen L., Liu Y., Jia M., An J., Tao K., Xing J. Next generation sequencing-based analysis of mitochondrial DNA characteristics in plasma extracellular vesicles of patients with hepatocellular carcinoma. Oncol. Lett. 2020;20:2820–2828. doi: 10.3892/ol.2020.11831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Schwarzenbach H., Gahan P. Exosomes in Immune Regulation. Non-Coding RNA. 2021;7:4. doi: 10.3390/ncrna7010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Jang S.C., Crescitelli R., Cvjetkovic A., Belgrano V., Bagge R.O., Sundfeldt K., Ochiya T., Kalluri R., Lötvall J. Mitochondrial protein enriched extracellular vesicles discovered in human melanoma tissues can be detected in patient plasma. J. Extracell. Vesicles. 2019;8:1635420. doi: 10.1080/20013078.2019.1635420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Marconi S., Santamaria S., Bartolucci M., Stigliani S., Aiello C., Gagliani M., Bellese G., Petretto A., Cortese K., Castagnola P. Trastuzumab Modulates the Protein Cargo of Extracellular Vesicles Released by ERBB2+ Breast Cancer Cells. Membranes. 2021;11:199. doi: 10.3390/membranes11030199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ruivo C.F., Adem B., Silva M., Melo S.A. The Biology of Cancer Exosomes: Insights and New Perspectives. Cancer Res. 2017;77:6480–6488. doi: 10.1158/0008-5472.CAN-17-0994. [DOI] [PubMed] [Google Scholar]
- 162.Guescini M., Genedani S., Stocchi V., Agnati L.F. Astrocytes and Glioblastoma cells release exosomes carrying mtDNA. J. Neural Transm. 2010;117:1. doi: 10.1007/s00702-009-0288-8. [DOI] [PubMed] [Google Scholar]
- 163.Keserű J.S., Soltész B., Lukács J., Márton É., Szilágyi-Bónizs M., Penyige A., Póka R., Nagy B. Detection of cell-free, exosomal and whole blood mitochondrial DNA copy number in plasma or whole blood of patients with serous epithelial ovarian cancer. J. Biotechnol. 2019;298:76–81. doi: 10.1016/j.jbiotec.2019.04.015. [DOI] [PubMed] [Google Scholar]
- 164.Tan A.S., Baty J.W., Dong L.-F., Bezawork-Geleta A., Endaya B., Goodwin J., Bajzikova M., Kovarova J., Peterka M., Yan B., et al. Mitochondrial Genome Acquisition Restores Respiratory Function and Tumorigenic Potential of Cancer Cells without Mitochondrial DNA. Cell Metab. 2015;21:81–94. doi: 10.1016/j.cmet.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 165.Kim R., Emi M., Tanabe K. Cancer immunoediting from immune surveillance to immune escape. Immunology. 2007;121:1–14. doi: 10.1111/j.1365-2567.2007.02587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Bates J.P., Derakhshandeh R., Jones L., Webb T.J. Mechanisms of Immune Evasion in Breast Cancer. BMC Cancer. 2018;18:556. doi: 10.1186/s12885-018-4441-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Whiteside T.L. Exosomes and tumor-mediated immune suppression. J. Clin. Investig. 2016;126:1216–1223. doi: 10.1172/JCI81136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Li Q., Cai S., Li M., Salma K.I., Zhou X., Han F., Chen J., Huyan T. Tumor-Derived Extracellular Vesicles: Their Role in Immune Cells and Immunotherapy. Int. J. Nanomed. 2021;16:5395–5409. doi: 10.2147/IJN.S313912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Sheehan C., D’Souza-Schorey C. Tumor-derived extracellular vesicles: Molecular parcels that enable regulation of the immune response in cancer. J. Cell Sci. 2019;132:jcs235085. doi: 10.1242/jcs.235085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.She Z., Xie M., Hun M., Abdirahman A.S., Li C., Wu F., Luo S., Wan W., Wen C., Tian J. Immunoregulatory Effects of Mitochondria Transferred by Extracellular Vesicles. Front. Immunol. 2021;11:628576. doi: 10.3389/fimmu.2020.628576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Biswas S.K. Metabolic Reprogramming of Immune Cells in Cancer Progression. Immunity. 2015;43:435–449. doi: 10.1016/j.immuni.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 172.Russell D.G., Huang L., VanderVen B.C. Immunometabolism at the Interface between Macrophages and Pathogens. Immunology. 2019;19:291–304. doi: 10.1038/s41577-019-0124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Raimondo S., Pucci M., Alessandro R., Fontana S. Extracellular Vesicles and Tumor-Immune Escape: Biological Functions and Clinical Perspectives. Int. J. Mol. Sci. 2020;21:2286. doi: 10.3390/ijms21072286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Graner M.W., Schnell S., Olin M.R. Tumor-Derived Exosomes, Micrornas, and Cancer Immune Suppression. Semin. Immunopathol. 2018;40:505–515. doi: 10.1007/s00281-018-0689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Syed S.N., Frank A.-C., Raue R., Brüne B. Microrna-a Tumor Trojan Horse for Tumor-Associated Macrophages. Cells. 2019;8:1482. doi: 10.3390/cells8121482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Kwon Y., Kim M., Kim Y., Jung H.S., Jeoung D. Exosomal MicroRNAs as Mediators of Cellular Interactions Between Cancer Cells and Macrophages. Front. Immunol. 2020;11:1167. doi: 10.3389/fimmu.2020.01167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Yi M., Xu L., Jiao Y., Luo S., Li A., Wu K. The role of cancer-derived microRNAs in cancer immune escape. J. Hematol. Oncol. 2020;13:25. doi: 10.1186/s13045-020-00848-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Garaude J., Acín-Pérez R., Martínez-Cano S., Enamorado M., Ugolini M., Nistal-Villán E., Hervás-Stubbs S., Pelegrín P., Sander L.E., Enríquez J.A., et al. Mitochondrial Respiratory-Chain Adaptations in Macrophages Contribute to Antibacterial Host Defense. Nat. Immunol. 2016;17:1037–1045. doi: 10.1038/ni.3509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Zaini R.G., Al-Rehaili A.A. The Therapeutic Strategies of Regulatory T Cells in Malignancies and Stem Cell Transplantations. J. Oncol. 2019;2019:5981054. doi: 10.1155/2019/5981054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Robbins P.D., Dorronsoro A., Booker C.N. Regulation of chronic inflammatory and immune processes by extracellular vesicles. J. Clin. Investig. 2016;126:1173–1180. doi: 10.1172/JCI81131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Whiteside T.L. Immune modulation of T-cell and NK (natural killer) cell activities by TEXs (tumour-derived exosomes) Biochem. Soc. Trans. 2013;41:245–251. doi: 10.1042/BST20120265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.West A.P., Shadel G.S. Mitochondrial DNA in innate immune responses and inflammatory pathology. Nat. Rev. Immunol. 2017;17:363–375. doi: 10.1038/nri.2017.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Cheng A.N., Cheng L.-C., Kuo C.-L., Lo Y.K., Chou H.-Y., Chen C.-H., Wang Y.-H., Chuang T.-H., Cheng S.-J., Lee A.Y.-L. Mitochondrial Lon-induced mtDNA leakage contributes to PD-L1–mediated immunoescape via STING-IFN signaling and extracellular vesicles. J. Immunother. Cancer. 2020;8:e001372. doi: 10.1136/jitc-2020-001372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Simula L., Antonucci Y., Scarpelli G., Cancila V., Colamatteo A., Manni S., De Angelis B., Quintarelli C., Procaccini C., Matarese G., et al. Pd-1-Induced T Cell Exhaustion Is Controlled by a Drp1-Dependent Mechanism. Mol. Oncol. 2022;16:188–205. doi: 10.1002/1878-0261.13103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Ge L., Wu Y., Wan M., You Y., Zhai Z., Song Z. Metformin Increases Sensitivity of Melanoma Cells to Cisplatin by Blocking Exosomal-Mediated miR-34a Secretion. J. Oncol. 2021;2021:5525231. doi: 10.1155/2021/5525231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Bukeirat M., Sarkar S.N., Hu H., Quintana D.D., Simpkins J.W., Ren X. Mir-34a Regulates Blood-Brain Barrier Permeability and Mitochondrial Function by Targeting Cytochrome C. J. Cereb. Blood Flow Metab. 2016;36:387–392. doi: 10.1177/0271678X15606147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Claridge B., Lozano J., Poh Q.H., Greening D.W. Development of Extracellular Vesicle Therapeutics: Challenges, Considerations, and Opportunities. Front. Cell Dev. Biol. 2021;9:734720. doi: 10.3389/fcell.2021.734720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Kobayashi M., Sawada K., Miyamoto M., Shimizu A., Yamamoto M., Kinose Y., Nakamura K., Kawano M., Kodama M., Hashimoto K., et al. Exploring the potential of engineered exosomes as delivery systems for tumor-suppressor microRNA replacement therapy in ovarian cancer. Biochem. Biophys. Res. Commun. 2020;527:153–161. doi: 10.1016/j.bbrc.2020.04.076. [DOI] [PubMed] [Google Scholar]
- 189.Zhang K., Shao C.-X., Zhu J.-D., Lv X.-L., Tu C.-Y., Jiang C., Shang M.-J. Exosomes function as nanoparticles to transfer miR-199a-3p to reverse chemoresistance to cisplatin in hepatocellular carcinoma. Biosci. Rep. 2020;40 doi: 10.1042/BSR20194026. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 190.Vakhshiteh F., Rahmani S., Ostad S.N., Madjd Z., Dinarvand R., Atyabi F. Exosomes derived from miR-34a-overexpressing mesenchymal stem cells inhibit in vitro tumor growth: A new approach for drug delivery. Life Sci. 2020;266:118871. doi: 10.1016/j.lfs.2020.118871. [DOI] [PubMed] [Google Scholar]
- 191.Tomasetti M., Nocchi L., Staffolani S., Manzella N., Amati M., Goodwin J., Kluckova K., Nguyen M., Strafella E., Bajzikova M., et al. MicroRNA-126 Suppresses Mesothelioma Malignancy by Targeting IRS1 and Interfering with the Mitochondrial Function. Antioxid. Redox Signal. 2014;21:2109–2125. doi: 10.1089/ars.2013.5215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Monaco F., Gaetani S., Alessandrini F., Tagliabracci A., Bracci M., Valentino M., Neuzil J., Amati M., Bovenzi M., Tomasetti M., et al. Exosomal transfer of miR-126 promotes the anti-tumour response in malignant mesothelioma: Role of miR-126 in cancer-stroma communication. Cancer Lett. 2019;463:27–36. doi: 10.1016/j.canlet.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 193.Zuo L., Tao H., Xu H., Li C., Qiao G., Guo M., Cao S., Liu M., Lin X. Exosomes-Coated miR-34a Displays Potent Antitumor Activity in Pancreatic Cancer Both in vitro and in vivo. Drug Des. Dev. Ther. 2020;14:3495–3507. doi: 10.2147/DDDT.S265423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Xu X.D., Wu X.H., Fan Y.R., Tan B., Quan Z., Luo C.L. Exosome-Derived Microrna-29c Induces Apoptosis of Biu-87 Cells by Down Regulating Bcl-2 and Mcl-1. Asian Pac. J. Cancer Prev. 2014;15:3471–3476. doi: 10.7314/APJCP.2014.15.8.3471. [DOI] [PubMed] [Google Scholar]
- 195.Maleki N., MirHakimi S., Babashah S., Sayadi A., Parnian G., HadiZadeh M. Use of cellular exosomes as a new carrier in breast cancer gene therapy. Klin. Onkol. 2021;34:300–305. doi: 10.48095/ccko2021300. [DOI] [PubMed] [Google Scholar]
- 196.Tao H., Xu H., Zuo L., Li C., Qiao G., Guo M., Zheng L., Leitgeb M., Lin X. Exosomes-coated bcl-2 siRNA inhibits the growth of digestive system tumors both in vitro and in vivo. Int. J. Biol. Macromol. 2020;161:470–480. doi: 10.1016/j.ijbiomac.2020.06.052. [DOI] [PubMed] [Google Scholar]
- 197.Xu H., Liao C., Liang S., Ye B.-C. A Novel Peptide-Equipped Exosomes Platform for Delivery of Antisense Oligonucleotides. ACS Appl. Mater. Interfaces. 2021;13:10760–10767. doi: 10.1021/acsami.1c00016. [DOI] [PubMed] [Google Scholar]
- 198.Lobos-González L., Bustos R., Campos A., Silva V., Silva V., Jeldes E., Salomon C., Varas-Godoy M., Cáceres-Verschae A., Duran E., et al. Exosomes released upon mitochondrial ASncmtRNA knockdown reduce tumorigenic properties of malignant breast cancer cells. Sci. Rep. 2020;10:343. doi: 10.1038/s41598-019-57018-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Zhu D., Liu Z., Li Y., Huang Q., Xia L., Li K. Delivery of manganese carbonyl to the tumor microenvironment using Tumor-Derived exosomes for cancer gas therapy and low dose radiotherapy. Biomaterials. 2021;274:120894. doi: 10.1016/j.biomaterials.2021.120894. [DOI] [PubMed] [Google Scholar]
- 200.Srivastava A., Amreddy N., Babu A., Panneerselvam J., Mehta M., Muralidharan R., Chen A., Zhao Y.D., Razaq M., Riedinger N., et al. Nanosomes carrying doxorubicin exhibit potent anticancer activity against human lung cancer cells. Sci. Rep. 2016;6:38541. doi: 10.1038/srep38541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hosseini H.M., Fooladi A.A.I., Soleimanirad J., Nourani M.R., Davaran S., Mahdavi M. Staphylococcal entorotoxin B anchored exosome induces apoptosis in negative esterogen receptor breast cancer cells. Tumor Biol. 2014;35:3699–3707. doi: 10.1007/s13277-013-1489-1. [DOI] [PubMed] [Google Scholar]
- 202.Hosseini H.M., Fooladi A.A.I., Soleimanirad J., Nourani M.R., Mahdavi M. Exosome/staphylococcal enterotoxin B, an anti tumor compound against pancreatic cancer. J. BUON. 2014;19:440–448. [PubMed] [Google Scholar]
- 203.Han D., Wang K., Zhang T., Gao G.-C., Xu H. Natural killer cell-derived exosome-entrapped paclitaxel can enhance its anti-tumor effect. Eur. Rev. Med Pharmacol. Sci. 2020;24:5703–5713. doi: 10.26355/eurrev_202005_21362. [DOI] [PubMed] [Google Scholar]
- 204.Phinney D.G., Pittenger M.F. Concise Review: MSC-Derived Exosomes for Cell-Free Therapy. Stem Cells. 2017;35:851–858. doi: 10.1002/stem.2575. [DOI] [PubMed] [Google Scholar]
- 205.Cao H., Cheng Y., Gao H., Zhuang J., Zhang W., Bian Q., Wang F., Du Y., Li Z., Kong D., et al. In Vivo Tracking of Mesenchymal Stem Cell-Derived Extracellular Vesicles Improving Mitochondrial Function in Renal Ischemia–Reperfusion Injury. ACS Nano. 2020;14:4014–4026. doi: 10.1021/acsnano.9b08207. [DOI] [PubMed] [Google Scholar]
- 206.Zhao M., Liu S., Wang C., Wang Y., Wan M., Liu F., Gong M., Yuan Y., Chen Y., Cheng J., et al. Mesenchymal Stem Cell-Derived Extracellular Vesicles Attenuate Mitochondrial Damage and Inflammation by Stabilizing Mitochondrial DNA. ACS Nano. 2021;15:1519–1538. doi: 10.1021/acsnano.0c08947. [DOI] [PubMed] [Google Scholar]
- 207.Collino F., Lopes J.A., Tapparo M., Tortelote G.G., Kasai-Brunswick T.H., Lopes G.M., Almeida D.B., Skovronova R., Wendt C.H.C., De Miranda K.R., et al. Extracellular Vesicles Derived from Induced Pluripotent Stem Cells Promote Renoprotection in Acute Kidney Injury Model. Cells. 2020;9:453. doi: 10.3390/cells9020453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Liu X., Li X., Zhu W., Zhang Y., Hong Y., Liang X., Fan B., Zhao H., He H., Zhang F. Exosomes from mesenchymal stem cells overexpressing MIF enhance myocardial repair. J. Cell. Physiol. 2020;235:8010–8022. doi: 10.1002/jcp.29456. [DOI] [PubMed] [Google Scholar]
- 209.Lee M., Liu T., Im W., Kim M. Exosomes from Adipose-Derived Stem Cells Ameliorate Phenotype of Huntington’s Disease in Vitro Model. Eur. J. Neurosci. 2016;44:2114–2119. doi: 10.1111/ejn.13275. [DOI] [PubMed] [Google Scholar]
- 210.Silva J.D., Su Y., Calfee C.S., Delucchi K.L., Weiss D., McAuley D.F., O’Kane C., Krasnodembskaya A.D. Mesenchymal stromal cell extracellular vesicles rescue mitochondrial dysfunction and improve barrier integrity in clinically relevant models of ARDS. Eur. Respir. J. 2020;58:2002978. doi: 10.1183/13993003.02978-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Morrison T.J., Jackson M.V., Cunningham E.K., Kissenpfennig A., McAuley D.F., O’Kane C.M., Krasnodembskaya A.D. Mesenchymal Stromal Cells Modulate Macrophages in Clinically Relevant Lung Injury Models by Extracellular Vesicle Mitochondrial Transfer. Am. J. Respir. Crit. Care Med. 2017;196:1275–1286. doi: 10.1164/rccm.201701-0170OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Lee M., Ban J.-J., Kim K.Y., Jeon G.S., Im W., Sung J.-J., Kim M. Adipose-derived stem cell exosomes alleviate pathology of amyotrophic lateral sclerosis in vitro. Biochem. Biophys. Res. Commun. 2016;479:434–439. doi: 10.1016/j.bbrc.2016.09.069. [DOI] [PubMed] [Google Scholar]
- 213.Bonafede R., Brandi J., Manfredi M., Scambi I., Schiaffino L., Merigo F., Turano E., Bonetti B., Marengo E., Cecconi D., et al. The Anti-Apoptotic Effect of ASC-Exosomes in an In Vitro ALS Model and Their Proteomic Analysis. Cells. 2019;8:1087. doi: 10.3390/cells8091087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Calabria E., Scambi I., Bonafede R., Schiaffino L., Peroni D., Potrich V., Capelli C., Schena F., Mariotti R. ASCs-Exosomes Recover Coupling Efficiency and Mitochondrial Membrane Potential in an in vitro Model of ALS. Front. Neurosci. 2019;13:1070. doi: 10.3389/fnins.2019.01070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Bruno S., Collino F., Deregibus M.C., Grange C., Tetta C., Camussi G. Microvesicles Derived from Human Bone Marrow Mesenchymal Stem Cells Inhibit Tumor Growth. Stem Cells Dev. 2013;22:758–771. doi: 10.1089/scd.2012.0304. [DOI] [PubMed] [Google Scholar]
- 216.Reza A.M.M.T., Choi Y.-J., Yasuda H., Kim J.-H. Human Adipose Mesenchymal Stem Cell-Derived Exosomal-Mirnas Are Critical Factors for Inducing Anti-Proliferation Signalling to A2780 and Skov-3 Ovarian Cancer Cells. Sci. Rep. 2016;6:38498. doi: 10.1038/srep38498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Ji Y., Ma Y., Chen X., Ji X., Gao J., Zhang L., Ye K., Qiao F., Dai Y., Wang H., et al. Microvesicles released from human embryonic stem cell derived-mesenchymal stem cells inhibit proliferation of leukemia cells. Oncol. Rep. 2017;38:1013–1020. doi: 10.3892/or.2017.5729. [DOI] [PubMed] [Google Scholar]
- 218.Ardeshirylajimi A., Ashkezari M.D., Rezaie Z., Seifati S.M. Antitumoral potential of microvesicles extracted from human adipose-derived mesenchymal stem cells on human breast cancer cells. J. Cancer Res. Ther. 2019;15:1114–1119. doi: 10.4103/jcrt.JCRT_147_18. [DOI] [PubMed] [Google Scholar]
- 219.Dibavar M.A., Soleimani M., Atashi A., Rassaei N., Amiri S. The effect of simultaneous administration of arsenic trioxide and microvesicles derived from human bone marrow mesenchymal stem cells on cell proliferation and apoptosis of acute myeloid leukemia cell line. Artif. Cells Nanomed. Biotechnol. 2018;46:S138–S146. doi: 10.1080/21691401.2018.1489821. [DOI] [PubMed] [Google Scholar]
- 220.Liu Y., Song B., Wei Y., Chen F., Chi Y., Fan H., Liu N., Li Z., Han Z., Ma F. Exosomes from mesenchymal stromal cells enhance imatinib-induced apoptosis in human leukemia cells via activation of caspase signaling pathway. Cytotherapy. 2018;20:181–188. doi: 10.1016/j.jcyt.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 221.Loussouarn C., Pers Y.-M., Bony C., Jorgensen C., Noël D. Mesenchymal Stromal Cell-Derived Extracellular Vesicles Regulate the Mitochondrial Metabolism via Transfer of miRNAs. Front. Immunol. 2021;12 doi: 10.3389/fimmu.2021.623973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Brown J.L., Rosa-Caldwell M.E., Lee D.E., Blackwell T.A., Brown L.A., Perry R.A., Haynie W.S., Hardee J.P., Carson J.A., Wiggs M.P., et al. Mitochondrial Degeneration Precedes the Development of Muscle Atrophy in Progression of Cancer Cachexia in Tumour-Bearing Mice. J. Cachexia Sarcopenia Muscle. 2017;8:926–938. doi: 10.1002/jcsm.12232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Shuler K.T., Wilson B.E., Muñoz E.R., Mitchell A.D., Selsby J.T., Hudson M.B. Muscle Stem Cell-Derived Extracellular Vesicles Reverse Hydrogen Peroxide-Induced Mitochondrial Dysfunction in Mouse Myotubes. Cells. 2020;9:2544. doi: 10.3390/cells9122544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Marchetti P., Fovez Q., Germain N., Khamari R., Kluza J. Mitochondrial Spare Respiratory Capacity: Mechanisms, Regulation, and Significance in Non-Transformed and Cancer Cells. FASEB J. 2020;34:13106–13124. doi: 10.1096/fj.202000767R. [DOI] [PubMed] [Google Scholar]
- 225.Greening D.W., Gopal S.K., Xu R., Simpson R.J., Chen W. Exosomes and Their Roles in Immune Regulation and Cancer. Semin. Cell Dev. Biol. 2015;40:72–81. doi: 10.1016/j.semcdb.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 226.Wu C.-H., Li J., Li L., Sun J., Fabbri M., Wayne A.S., Seeger R.C., Jong A.Y. Extracellular vesicles derived from natural killer cells use multiple cytotoxic proteins and killing mechanisms to target cancer cells. J. Extracell. Vesicles. 2019;8:1588538. doi: 10.1080/20013078.2019.1588538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Waterhouse N.J., Sedelies K.A., Browne K.A., Wowk M.E., Newbold A., Sutton V.R., Clarke C.J.P., Oliaro J., Lindemann R.K., Bird P., et al. A Central Role for Bid in Granzyme B-induced Apoptosis. J. Biol. Chem. 2005;280:4476–4482. doi: 10.1074/jbc.M410985200. [DOI] [PubMed] [Google Scholar]
- 228.Lee J., Lee S.-A., Gu N.-Y., Jeong S.Y., Byeon J.S., Jeong D.-U., Ouh I.-O., Lee Y.-H., Hyun B.-H. Canine Natural Killer Cell-Derived Exosomes Exhibit Antitumor Activity in a Mouse Model of Canine Mammary Tumor. BioMed Res. Int. 2021;2021:6690704. doi: 10.1155/2021/6690704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Ristorcelli E., Beraud E., Verrando P., Villard C., Lafitte D., Sbarra V., Lombardo D., Verine A. Human tumor nanoparticles induce apoptosis of pancreatic cancer cells. FASEB J. 2008;22:3358–3369. doi: 10.1096/fj.07-102855. [DOI] [PubMed] [Google Scholar]
- 230.Liu Y.D., Zhuang X.P., Cai D.L., Cao C., Gu Q.S., Ni Liu X., Bin Zheng B., Guan B.J., Yu L., Li J.K., et al. Let-7a regulates EV secretion and mitochondrial oxidative phosphorylation by targeting SNAP23 in colorectal cancer. J. Exp. Clin. Cancer Res. 2021;40:31. doi: 10.1186/s13046-020-01813-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Philley J.V., Kannan A., Qin W., Sauter E.R., Ikebe M., Hertweck K.L., Troyer D.A., Semmes O.J., Dasgupta S. Complex-I Alteration and Enhanced Mitochondrial Fusion Are Associated With Prostate Cancer Progression. J. Cell. Physiol. 2015;231:1364–1374. doi: 10.1002/jcp.25240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Behzadi E., Mahmoodzadeh Hosseini H., Imani Fooladi A.A. The inhibitory impacts of Lactobacillus rhamnosus GG-derived extracellular vesicles on the growth of hepatic cancer cells. Microb. Pathog. 2017;110:1–6. doi: 10.1016/j.micpath.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 233.Kang M.H., Reynolds C.P. Bcl-2 Inhibitors: Targeting Mitochondrial Apoptotic Pathways in Cancer Therapy. Clin. Cancer Res. 2009;15:1126–1132. doi: 10.1158/1078-0432.CCR-08-0144. [DOI] [PMC free article] [PubMed] [Google Scholar]