Abstract
Dynamic lung volumetric parameters are useful for clinical assessment of many thoracic disorders, given that respiration is a dynamic process. Estimation of such parameters based on imaging and analysis is an important goal to achieve if implementation in routine clinical practice is to become a reality. Compared to CT, dynamic thoracic MRI has several advantages including better soft tissue contrast, lack of ionizing radiation, and flexibility in selecting scanning planes. 4D dynamic MRI seems to be the best choice for some clinical applications, notwithstanding the major limitation of a long image acquisition time (~45 minutes). Therefore, approaches to acquire images and estimate volumetric parameters rapidly is highly desirable in dynamic MRI-based clinical applications. In this paper, we present a technique for estimating lung volumetric parameters from limited-slices dynamic thoracic MRI, greatly reducing the number of slices to be scanned and therefore also the time required for image acquisition. We demonstrate a relative RMS error of predicted lung volumes of less than 5% by utilizing only 5 sagittal MRI slices through each lung compared to the current full scan involving about 20 slices per lung. As such, this approach can lead to time-saving during scan acquisition and therefore increased patient comfort and convenience for practical real-world clinical applications. This may potentially also improve image quality and usability due to the reduction of patient motion, abnormal breathing patterns, etc. ensuing from improved patient comfort and scan duration.
Keywords: Volume estimation, dynamic MRI, limited-slices, imaging lungs
1. INTRODUCTION
Dynamic lung volumetric parameters are useful for clinical assessment of many thoracic disorders [1] such as scoliosis, Thoracic Insufficiency Syndrome (TIS) [2, 3], and various pulmonary disorders [7], as well as for determining the effects of therapeutic interventions. For some subjects with limited ability to cooperate, such as children or unconscious patients, imaging-based lung volume measurement may be more feasible than physiological measurement. Estimation of such parameters based on image analysis is an important goal to achieve if implementation in routine clinical practice is to become a reality. For this purpose, dynamic (or 4D) imaging, rather than static imaging, is necessary. Among different 4D dynamic imaging modalities, both dynamic computed tomography (CT) and dynamic magnetic resonance imaging (MRI) can be used for examination of the thorax. However, compared to dynamic CT, dynamic MRI has several advantages including better soft tissue contrast, lack of ionizing radiation, and flexibility in selecting scanning planes. 4D dynamic MRI seems to be the best choice for some clinical applications [4], notwithstanding the one major limitation of a rather long image acquisition time [2–4], that can take up to 45 minutes to complete a dynamic thoracic MRI examination that includes about 35 sagittal slices. Therefore, approaches to acquire the images and estimate the volumetric parameters rapidly is highly desirable in dynamic MRI-based clinical applications.
In this paper, we propose a technique for estimating lung volumetric parameters from limited-slices dynamic thoracic MRI, greatly reducing the number of slices to be scanned and therefore also the time required for image acquisition, without compromising the accuracy of volume estimation.
2. MATERIAL AND METHODS
2.1. Imaging Protocol
We will briefly describe the dynamic thoracic MRI protocol and 4D image construction first. There are two main approaches to form a 4D image through dynamic MRI [5]: (i) Real-time 3D volume approach: Use fast 3D MRI sequences to obtain real-time 3D volume data. (ii) Retrospective 2D slices approach: Use fast 2D MRI sequences to continuously acquire 2D images slice by slice while the subject is breathing freely, and then construct these slices post hoc to form a 4D image. For real-time methods, given the limitations of current hardware and software, it is difficult to achieve high spatial and contrast resolution, high signal-to-noise ratio, and sufficiently high time resolution simultaneously. Therefore, in this paper, we utilized the second approach for image acquisition and 4D image construction for each lung, the details of which have previously been reported [4, 6, 9].
2.2. Framework
The framework of our scanning design is depicted in Figure 1. For each lung, we compare the performance of full-scan dynamic MRI 4D images to that of limited-slices dynamic MRI 4D images to reliably capture the dynamics of respiration. In particular, we determine the end-inspiration (EI) and end-expiration (EE) time points in both full-scan and limited-slices 4D images, and then estimate the lung volume parameters based on image segmentation techniques [8]. We then compare estimates of the functional parameters of each lung derived from limited-slices compared to those from full-scan (as reference standard). For demonstration in this paper, we use the limited-slices selected from the full-scan via simulation, since our 4D construction method will not be impacted by the number of slices we acquired in the original full scan, as demonstrated in [6]. In other words, it can be mathematically proved that the 4D image constructed from the sparse (limited-slices) scan will be a proper subset of the 4D image constructed from the full scan if the slice locations in the sparse scan are all included in the full scan. We are in the process of acquiring actual limited-slices scans simultaneously with full-scans from several subjects to demonstrate that what we show via simulation is perfectly valid in reality. The estimation process consists of several steps: i) Selection of sparse slices, ii) Volume estimation, iii) Regression, and iv) Prediction.
Figure 1.
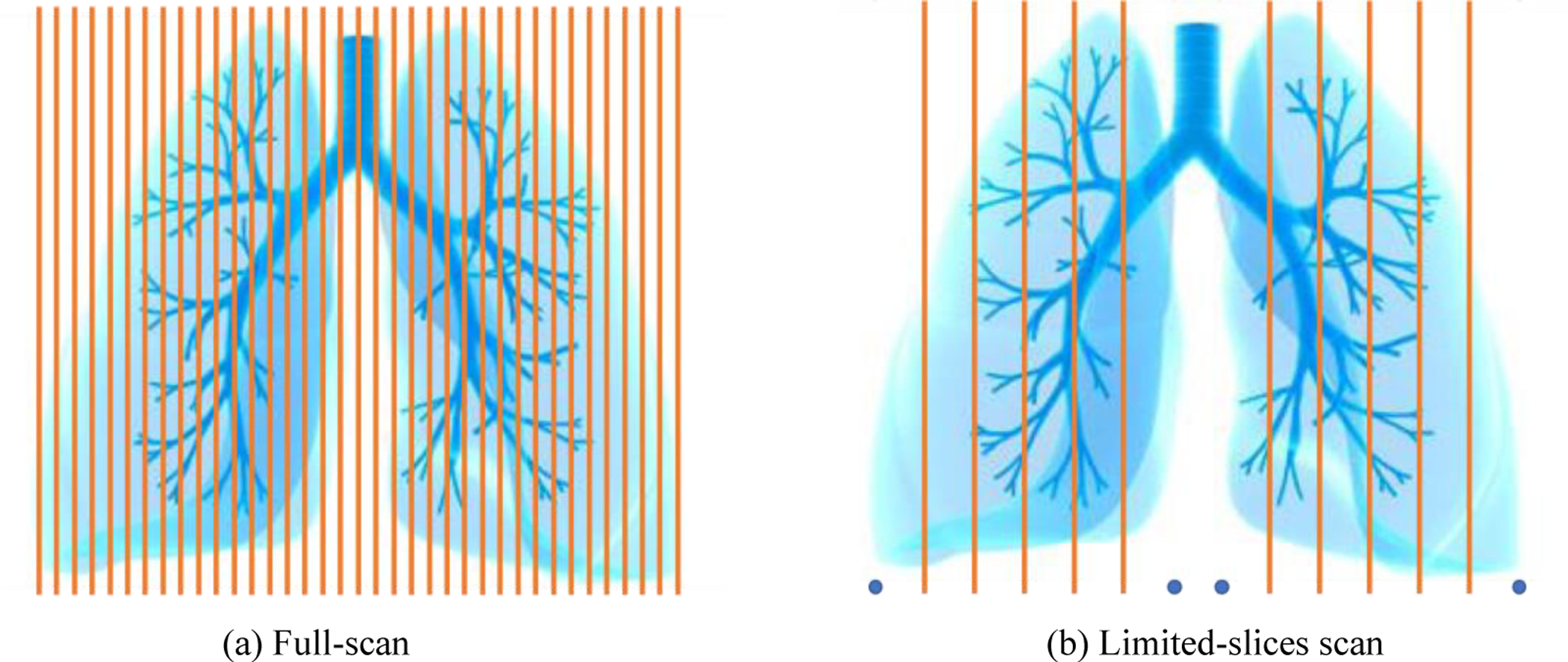
A schematic diagram of full-scan and limited-slices dynamic thoracic MRI scan. Each line represents a sagittal slice location, and the blue points in (b) represent the left and right edges of each lung. Figure courtesy: http://raiganbabay.blogspot.com/
2.3. Slice selection
In order to make our design feasible, the two problems we have to solve are: how to choose these limited slices; and how many slices should be selected to reliably estimate lung volume parameters. To make implementation of the slice selection protocol simple and practical for patient scanning, we decided to sample slices through each lung evenly. We define the sampling strategy as UFM as depicted in Figure 2. The UFM method samples all slices uniformly through each lung, which is based on slices acquired in the sagittal plane.
Figure 2.
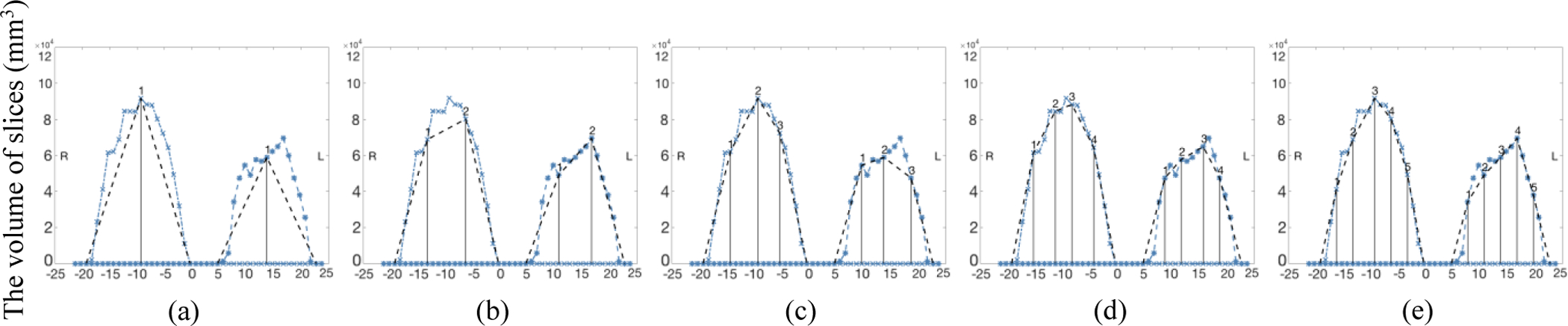
The slice selection method UFM: (a-e) The number of selected slices (NSS) from 1 to 5. The curve shown in blue represents the volume VF obtained from full scan. The selected slice locations and their volumes are shown as vertical bars.
In Figure 2, the x-axis represents the index of the (sagittal) slice locations from right to left through each lung, and the y-axis represents the volume of lung on each slice in mm3, which is derived by manual segmentation of the lung in each slice. The graph for the right lung appears on the left in the figure and for the left lung it appears on the right (to be consistent with how anatomy is portrayed in images). The graphs corresponding to the full scan are shown in color. Note that the area under the colored curve in each graph denotes the volume estimated from full scan, which we denote by VF. We employ UFM strategy to approximate the volume of each lung and denote the volume estimated from limited-slices scan by VL. As the number of selected slices (NSS), shown as vertical bars in the figure, increases, the accuracy of approximation of VF via VL will increase (see the curve in black), but the image acquisition time will also increase.
2.4. Volume estimation
A straightforward way to estimate VF from the limited slices is via nearest-neighbor interpolation - that is, to use the sum of the lung volume segmentations of all selected slices. We denote it as NN. However, this provides only a very rough approximation. To make the estimation more accurate, we use the liner spline interpolation (LIN) for the estimation. Clearly, the more slices that are selected, the better VL will fit VF. We may also use more sophisticated strategies to interpolate the volume curve in an attempt to bring the black curve in Figure 2 as close as possible to the colored curve. In Figure 2, we illustrate the use of linear (spline) interpolation (LIN) to estimate VL.
2.5. Regression
Upon obtaining the estimated VL via interpolation, we fit a model via linear regression to predict VF from VL. In the plot of VL vs. VF, we observe an obvious linear relationship between VL and VF; see Figure 3. The predicted volume derived from VL with the linear model is designated as VP. We use relative Root Mean Squared (rRMS) error, defined as follows, to evaluate the accuracy of the predictive model:
| (1) |
where N represents the number of samples used in the regression.
Figure 3.
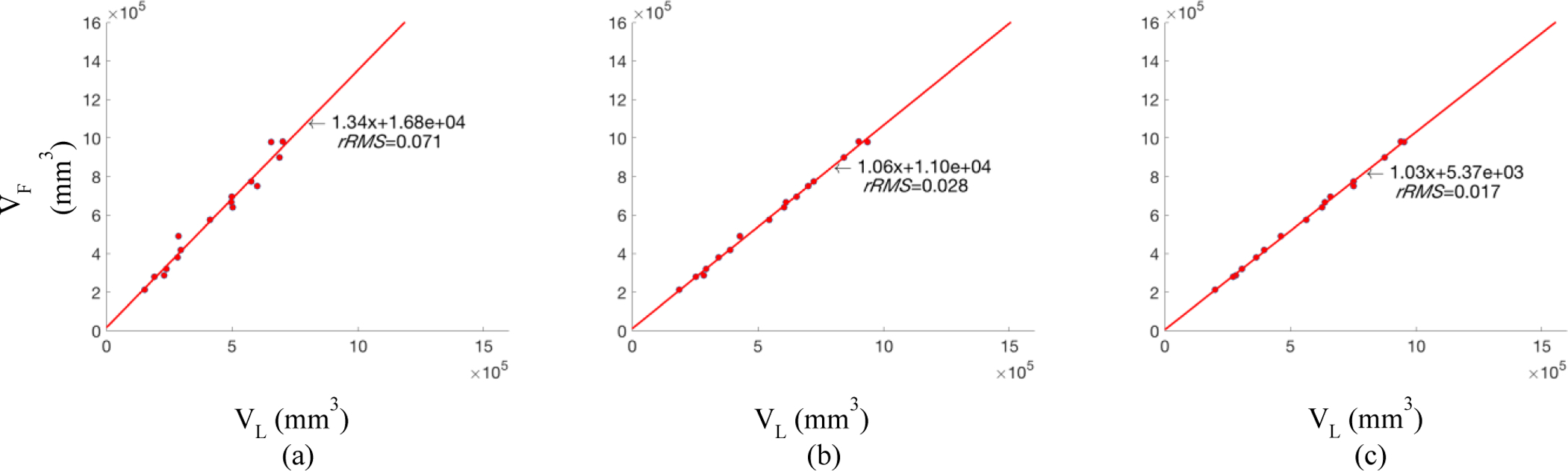
Examples of linear regression from VL to VF (from Left Lung End-Expiration). All examples use the UFM method for slice selection and LIN method for volume approximation. (a) NSS=1; (b) NSS=3; (c) NSS=5.
2.6. Prediction
Once the regression model is found, we use it to predict VF from VL for any given samples.
3. EXPERIMENTS AND RESULTS
3.1. Interpolation Methods
All data were acquired under an ongoing research protocol approved by the Institutional Review Board at the Children’s Hospital of Philadelphia (CHOP) and University of Pennsylvania, along with Health Insurance Portability and Accountability Act waiver. Our method involves three sets of parameters: slice selection method, interpolation strategy, and number of selected slices (NSS). We compare among different choices of these parameters on dynamic thoracic MRI datasets from 20 normal pediatric subjects, including 9 females and 11 males. The age is between 6.2–13.7 years old with an average of 10.739. We focus on 4 lung volume measurements: left lung volume at end-inspiration (LLVEI), left lung volume at end-expiration (LLVEE), right lung volume at end-inspiration (RLVEI), and right lung volume at end-expiration (RLVEE). Firstly, to compare different interpolation methods, we fix NSS = 5 and slice selection method as UFM, and evaluate the rRMS of the final prediction error as shown in Table 1. We see that linear interpolation achieved the best results. Second, to compare different slice selection strategies and to assess rRMS in relation to NSS, we plot the results as shown in Figure 4. An example of the selected slices by UFM method is depicted in Figure 5.
Table 1:
rRMS for different interpolation methods. The slice selection method is UFM and NSS=5.
| Method | LLVEE | RLVEE | LLVEI | RLVEI | |
|---|---|---|---|---|---|
| NN | 0.095 | 0.098 | 0.091 | 0.095 | |
| LIN | 0.017 | 0.020 | 0.016 | 0.015 |
Figure 4.
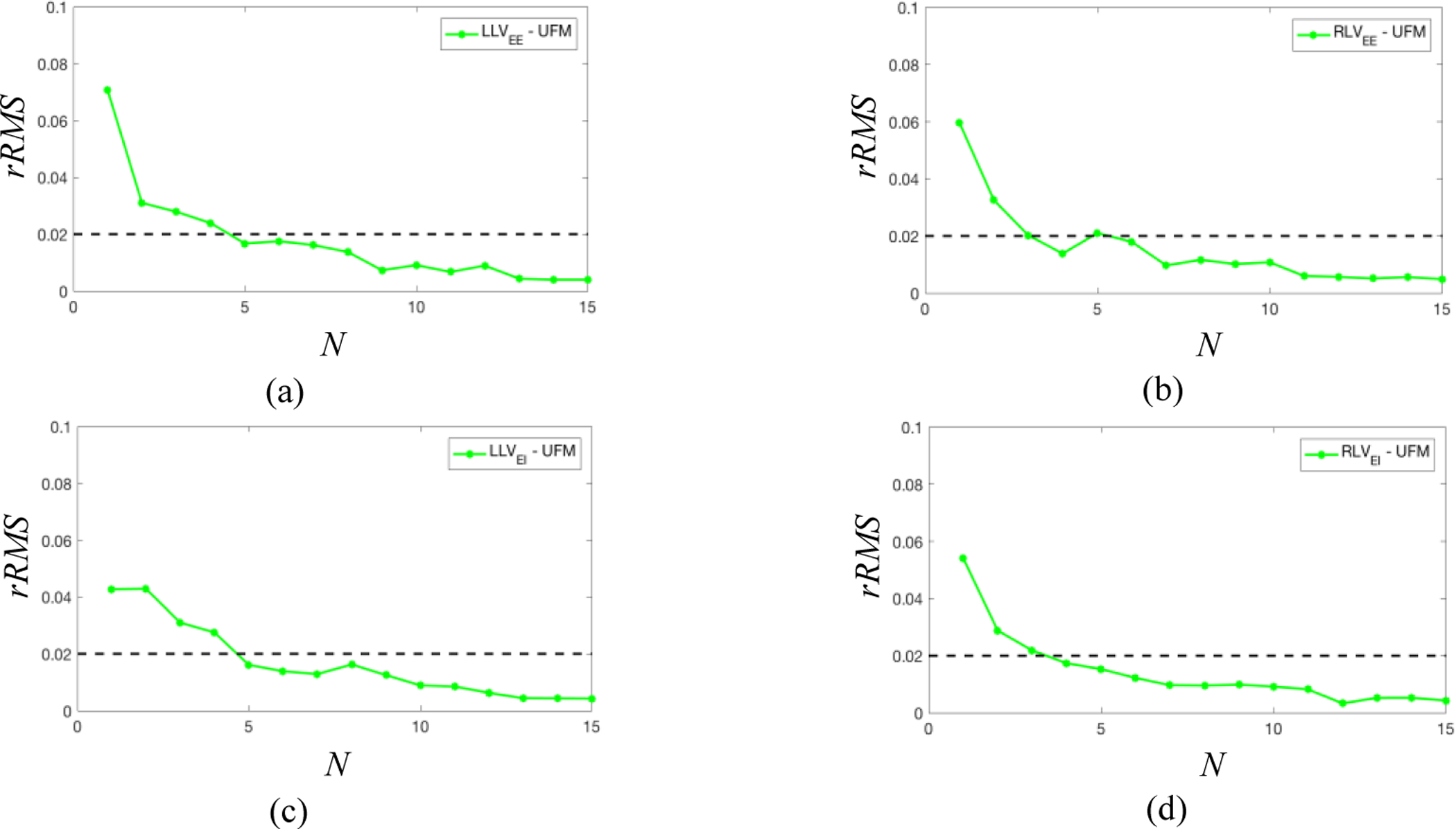
Comparison of slice selection method UFM for (a) LLVEE, (b) RLVEE, (c) LLVEI and (d)
Figure 5:
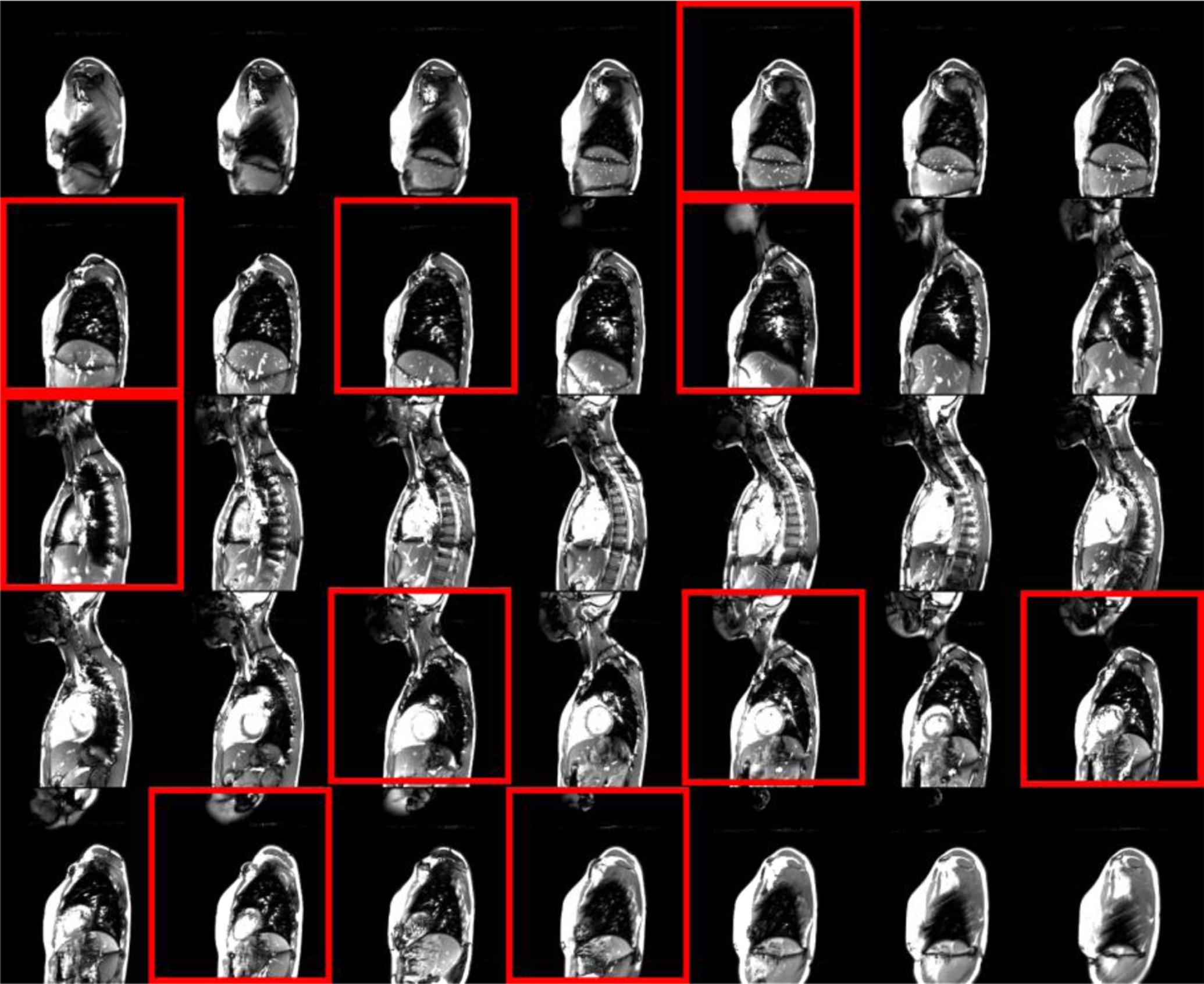
An example of the sagittal slices selected by UFM method. The 35 sagittal slices are from a full-scan, and the 10 slices within red box are the selected slices by setting NSS as 5.
3.2. Different lung volumes
To compare the settings of the approach on different lung volumes, we also conduct experiments on the 4 different volumes, LLVEI, LLVEE, RLVEI, and RLVEE, with the same setting. As with previous experiments, we also use the rRMS as the measurement. The results are plotted in Figure 6. We observe that the performance of our approach is not much different on different lung volume parameters.
Figure 6.
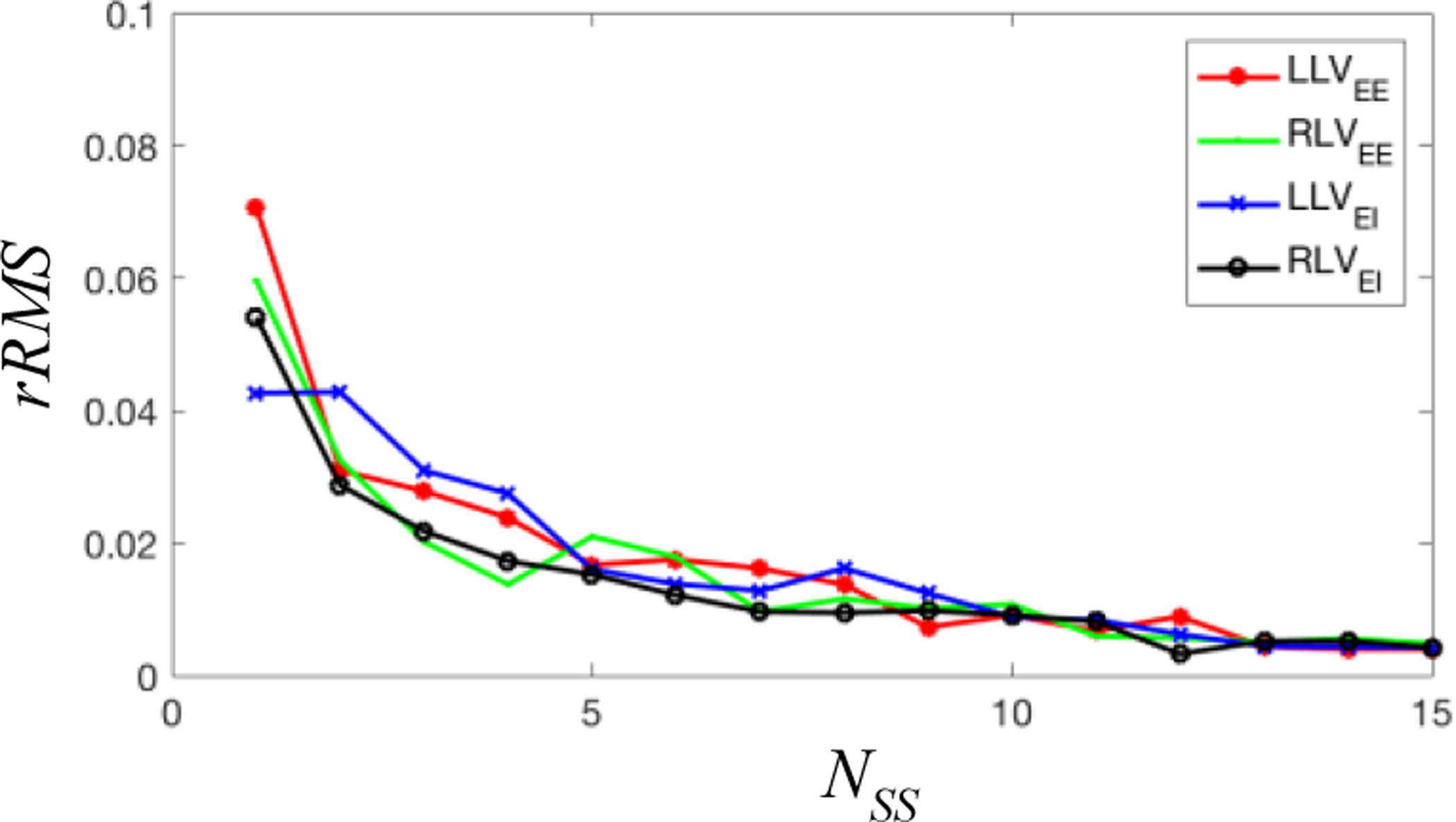
Comparison of rRMS of different lung volumes of UFM method.
3.3. Evaluation
Finally, we choose the UFM method finally since it is more convenient to operate in practice. Considering the trade-off between accuracy of lung volume estimation and the time required for image acquisition, we can choose NSS = 5, for which we observe a rRMS of less than 2% for every lung volume parameter. By the limited-scans approach, the image acquisition time of dynamic thoracic MRI can be reduced to around 11–13 min compared to ~45 min required for the full-scan, improving the convenience and comfort of patients, with an error no more than 2%!
4. CONCLUSION
In this paper, we propose a novel approach using limited-slices dynamic thoracic MRI scanning to predict lung volumetric parameters. We demonstrate a relative RMS error of predicted lung volumes of less than 2 percent compared to the reference standard of full scan by utilizing only 5 sagittal MRI slices through each lung. As such, this approach can lead to significant time-saving during scan acquisition and therefore increased patient comfort and convenience for practical real-world clinical application. This may potentially also improve image quality and usability due to the reduction of patient motion, abnormal breathing patterns, etc. ensuing from improved patient comfort and scan duration.
5. ACKNOWLEDGMENT
This research is partly supported by a “Frontier Grant” from The Children’s Hospital of Philadelphia, an NIH grant 1R01HL150147-01, and by the Institute for Translational Medicine and Therapeutics of the University of Pennsylvania through a grant by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR001878. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The support provided by China Scholarship Council (CSC) during a visit of Mr. You Hao to Medical Image Processing Group, Department of Radiology, University of Pennsylvania, is acknowledged.
REFERENCES
- [1].Crompton G, “A brief history of inhaled asthma therapy over the last fifty years,” Primary care respiratory journal 15(6), 326 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Campbell Robert M Jr, Smith Melvin D, Mayes Thomas C, Mangos John A, Willey-Courand Donna B, Kose Nusret, Pinero Ricardo F, Alder Marden E, Duong Hoa L, and Surber Jennifer L. The effect of opening wedge thoracostomy on thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. JBJS, 86(8):1659–1674, 2004. [DOI] [PubMed] [Google Scholar]
- [3].Campbell Robert M Jr and Smith Melvin D. Thoracic insufficiency syndrome and exotic scoliosis. JBJS, 89:108–122, 2007. [DOI] [PubMed] [Google Scholar]
- [4].Tong Y, Udupa JK, Ciesielski KC, Wu C, McDonough JM, Mong DA, and Campbell RM Jr, “Retrospective 4D MR image construction from free-breathing slice acquisitions: A novel graph-based approach,” Medical image analysis 35, 345–359 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Cai J, Chang Z, Wang Z, Paul Segars W, and Yin F-F, “Four-dimensional magnetic resonance imaging (4D-MRI) using image-based respiratory surrogate: a feasibility study,” Medical physics 38(12), 6384–6394 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hao Y, Udupa JK, Tong Y, Wu C, Li H, McDonough JM, Torigian DA, and Cahill PJ, “4D image construction from free-breathing MRI slice acquisitions of the thorax based on a concept of flux”, Proc. SPIE 11312, Medical Imaging 2020: Physics of Medical Imaging, 113122K (16 March 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Wanger J, Clausen JL, Coates A, Pedersen OF, Brusasco V, Burgos F, Casaburi R, Crapo R, Enright P, Van Der Grinten CPM, et al. Standardisation of the measurement of lung volumes. European respiratory journal, 26(3):511–522, 2005. [DOI] [PubMed] [Google Scholar]
- [8].Clausen J Measurement of absolute lung volumes by imaging techniques. European Respiratory Journal, 10(10):2427–2431, 1997. [DOI] [PubMed] [Google Scholar]
- [9].Tong Y, Udupa JK, McDonough JM, Wileyto EP, Capraro A, Wu C, Ho S, Galagedera N, Talwar D, Mayer OH, Torigian DA, and Campbell RM, “Quantitative dynamic thoracic MRI: application to thoracic insufficiency syndrome in pediatric patients,” Radiology 292(1), 206–213 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]


