Abstract
Limitations following stroke make it one of the leading causes of disability. The current medical pathway provides intensive care in the acute stages, but rehabilitation services are commonly discontinued after one year. While written home exercise programs are regularly prescribed at the time of discharge, compliancy is an issue. The goal of this study was to inform the design of a home-based portable rehabilitation system based on feedback from individuals with stroke and clinicians. A main component under consideration is the type and format of information feedback provided to the user, as this is hypothesized to support compliance with the rehabilitation program. From a series of focus groups and usability testing, a set of design requirements for the hardware and software were constructed. Essential features mentioned for the feedback interface included: task completion time, quality of movement, a selection of exercises, goal tracking, and a display of historical data.
INTRODUCTION
The population in the US is aging (Ortman, Velkoff, & Hogan, 2014), and with increased age there is diminished motor control (Francis, Macrae, Spirduso, & Eakin, 2012; Fraser, Li, & Penhune, 2010) in addition to higher risk for neurological insult such as stroke (Santalucia et al., 2015). Over 700,000 new cases of stroke occur each year (Rosamond et al., 2007). This number is projected to increase with the aging of the baby boomer generation. Despite evidence that improvements can still be made several years post-stroke (Wolf et al., 2010), rehabilitation options in chronic stages of stroke are not well established. Only 10–15% of stroke survivors had a follow-up with a physical therapist one year after their stroke (Langhammer & Stanghelle, 2003). While written home exercise programs are commonly prescribed at the end of formal therapies, this transition to self-management of a home rehabilitation program is not ideal for long-term management of functional mobility. As practice is a key component to improvement (Wolf, Lecraw, Barton, & Jann, 1989), participation is imperative for a home exercise program to lead to motor performance benefits (Novak, 2011). Hence, developing approaches to better support clients with their home program is important.
For any home rehabilitation to be effective, adherence is a key component. A patient-centered home exercise program can be a low-cost intervention. Training in an ecologically valid environment, the home, can give greater meaning to training activities (Hodson, Aplin, & Gustafsson, 2016). As demonstrated by previous research, exercise programs that include feedback from a person through a home visit, telephone call or clinic appointment have resulted in better outcomes compared to programs without feedback (Dobkin, Plummer-D’Amato, Elashoff, Lee, & Grp, 2010; Novak, 2011). Moreover, feedback from a virtual reality gait training system was as effective as a therapist’s verbal feedback in chronic stages of stroke (Byl, Zhang, Coo, & Tomizuka, 2015). However, individuals with stroke who do not routinely see rehabilitation professionals in chronic stages of recovery, do not receive feedback on their home exercise programs.
Sensory and motor deficits post-stroke can make it more difficult to perceive and correct movement error (Wutzke, Faldowski, & Lewek, 2015). Receiving feedback, particularly after performing the motor task well, can assist the individual’s performance (Chiviacowsky & Wulf, 2007). It is noted that participants controlling the timing of feedback preferentially seek feedback when they feel they have performed well (Chiviacowsky & Wulf, 2005). It is believed that receiving feedback after a “good” trial helps the participant develop error detection and a correction mechanism (Carter, Carlsen, & Ste-Marie, 2014). Feedback can give individuals a better understanding of their abilities, building self-efficacy and fostering the ability to set appropriate goals for themselves (Dobkin et al., 2010; Novak, 2011).
While feedback has been identified as an important component of rehabilitation programs, it is often lacking from home-based programs. Based on a survey of practicing occupational and physical therapists (Langan et al., 2017), approximately 74% of therapists report sending patients home with a written home program and non-technological equipment to continue rehabilitation efforts after formal therapies have concluded. Conventional therapy equipment such as stopwatches are more frequently used than newer technology like Wii™ and Kinect™ games. Still, less than 25% of therapists report using a stopwatch five or more times per week. Newer technology is typically used less than once per week and generally incorporated into interventions rather than assessments. Only 11% of respondents use objective feedback more than 75% of the time. However, a majority prioritized the need for a means to provide objective feedback to both therapists and patients. For any feedback system developed, they indicated it should include task completion time, smoothness of movement, and symmetry of movement.
Due to the limitations of current practice, and advances in technology that support application in the home, the objective of this study was to design a portable technology that can encourage better self-management in home-based stroke rehabilitation. In order to design an effective system that meets the needs of the target population, the first stage was to meet with stakeholders for requirements gathering and initial prototype evaluation. The objective of this paper is to provide a summary of user requirements for the design of a portable home rehabilitation system. This information can support the improved design of systems targeted toward individuals with stroke and other upper extremity motor impairments.
METHODS
A series of two sets of focus groups, followed by individual usability evaluation, were completed. In between each period of testing, the research team developed and redesigned a prototype of the rehabilitation system.
Design Concept
The research team designed a home-rehabilitation portable measurement system that provides data on upper extremity functional mobility across a range of capabilities. These capabilities include: general arm movement, forearm pronation and supination, elbow extension, and fine motor control. These motions are important for performing essential activities of daily living. The system pairs 3D printing with movement sensors to provide a scalable and customizable option. In order to be consistent with typical tasks needed in daily life, the system includes objects designed to mimic those encountered in the home, such as a mug or bowl. Built-in sensors from a phone embedded in the mug or bowl capture activity data, including movement time, acceleration, orientation, and smoothness, during rehabilitation. Figure 1 shows the current system after completion of the iterative design process.
Figure 1.
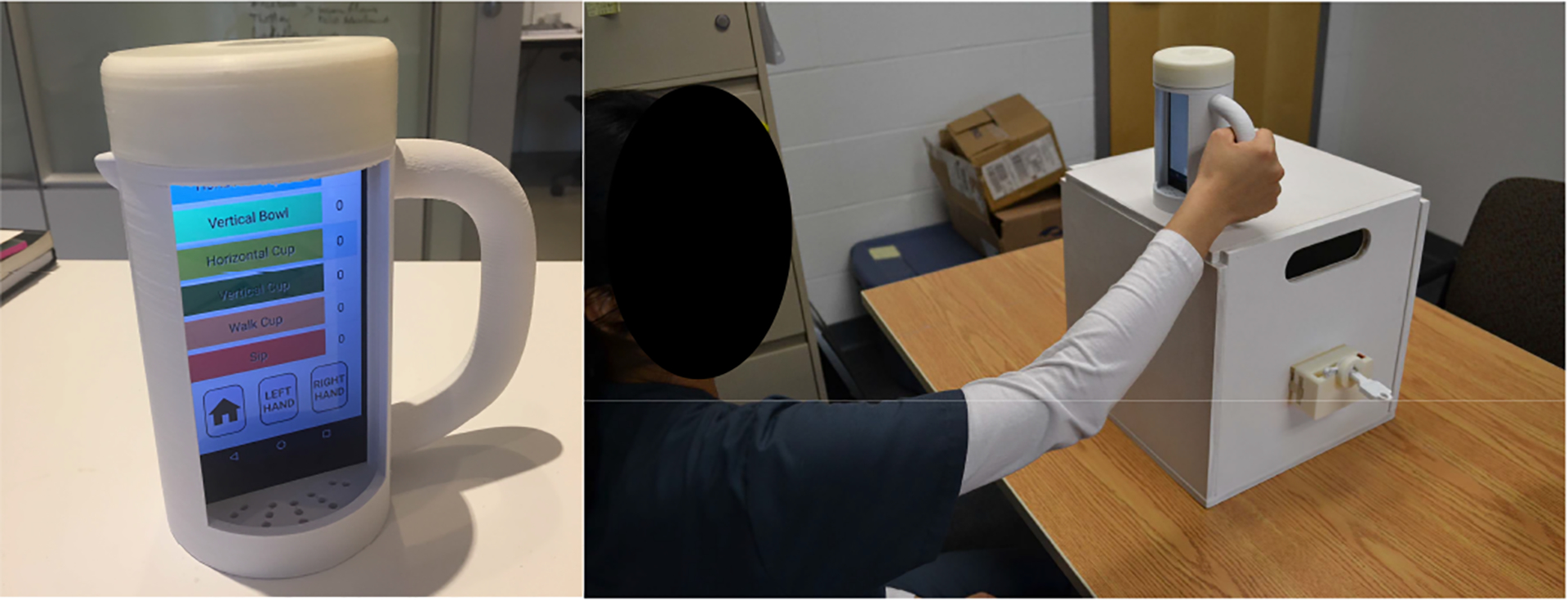
Left: 3D printed mug with phone inserted to provide user interface. Right: Example use of the system.
Stakeholder Focus Groups
Two main stakeholder groups were identified when considering the design: individuals with chronic stroke who are no longer participating in formal programs, and clinicians who work with individuals with stroke during formal clinic and home rehabilitation programs. Two separate rounds of focus groups were completed for each stakeholder group. Three individuals with stroke were in the first group, and three occupational therapists participated in the second.
During the first focus group, participants were asked to provide feedback on the design concept, the system hardware, and early prototype sketches for the feedback interface. The second focus group targeted identifying preferred timing and presentation of performance feedback. In each session, participants first completed a written questionnaire and then participated in a group discussion on their responses.
Usability Evaluation
After implementation of the tasks and user interface, the functional prototype was evaluated to identify areas of concern in the design. Eight participants volunteered for this study including four individuals with stroke and four healthy older adults. Each participant was instructed in the use of the system and then performed a set of rehabilitation tasks, replicating basic tasks such as mug pouring or lifting and object transport, with the system set for 10 repetitions. Participants were observed by a trained occupational therapist and a product designer to identify challenges with the system. Following the trial period, participants answered a series of usability questions adapted from the Questionnaire for User Interaction Satisfaction (QUIS), focusing on the overall reaction to the system, system learnability, and interface design. Participants then completed an interview, where they provided feedback on the system. This feedback, along with the responses from the focus groups, was then generalized into a set of design requirements for this and similar systems.
RESULTS
During the focus groups, the clinicians substantiated the need for better long-term options to promote home-based therapeutic practice. The clinicians prioritized motor coordination and functional skills for rehabilitation. Essential features mentioned for the feedback interface include: task completion time, quality of movement, a selection of exercises, goal tracking, and a display of historical data. Table 1 summarizes the ratings of importance for 13 features regarding the information presented in task feedback. As shown, the lowest rated items by both groups were having the ability to share information with either peers or caretakers and receiving rewards for progress.
Table 1.
Average (min, max) Ratings of Importance for Interface Design Features (1 = Not important at all, 5 = Very important)
| Feature | Therapists | Individuals with Stroke |
|---|---|---|
| Single task completion time | 3 (2, 4) | 4.7 (4, 5) |
| User’s smoothness (quality of movement) | 4.3 (4, 5) | 4 (2, 5) |
| Number of completed exercises | 3.7 (3, 4) | 3.7 (2, 5) |
| Selection of exercises to complete | 3.7 (3, 4) | 4.7 (4, 5) |
| Display of object position/trajectory | 4.7 (4, 5) | 4 (2, 5) |
| Ability to set and track progress toward goals | 5 | 4.7 (4, 5) |
| Display of user history showing trends over week | 4.7 (4, 5) | 4 (2, 5) |
| Display of user history showing trends over month | 4 (3, 5) | 4 (2, 5) |
| Rewards for meeting goals | 3 (2, 4) | 3.3 (2, 4) |
| Share information with peers | 2.7 (2, 3) | 2.7 (2, 3) |
| Share information with caretakers | 3.7 (3, 4) | 2.3 (2, 3) |
| Share information with therapists | 4.7 (4, 5) | 4.3 (4, 5) |
| Automatic notifications or alerts | 4.3 (4, 5) | 3 (2, 4) |
For the second focus group, individuals with stroke indicated a preference for receiving performance feedback either after each trial or at the end of a full rehabilitation session. Although they wanted the feedback to be shown during task performance, the individuals with stroke indicated that this would be too confusing to focus on while also trying to concentrate on the task itself. Two participants wanted to see their performance over the past week, while the third wanted to see the change from the previous day. They expressed a desire to compare the numbers for the performance with their own prior performance. As indicated by the clinicians during their focus group, comparison to one’s own performance is preferable so that the individual is not discouraged by seeing the performance of others. By both groups, visual information was requested to be numeric rather than graphical or picture-based. However, the clinicians also requested video or animated playback of the task to show movement quality and to be able to show clients where errors were made. This feature was not included in the current prototype due to an initial focus on individuals with stroke, but may be considered in future versions of the device.
Following creation of the prototype system, the older adults and individuals with stroke completed the usability evaluation. Overall, ratings of the system concept were positive, with one participant commenting “I could see what I had to do to improve the graphs…after a couple of times I could see what worked and what didn’t…I would use this, I don’t know that I would call it fun, but it makes it interesting to do rather than sitting with an inanimate object like clay or an elastic strap.”
In terms of the 3D printed hardware, particularly the mug since it is used most often in the planned exercises, participants commented that they liked the shape of the handle, the fact that the device did not look therapeutic, and that it was compatible with other kitchen equipment. One older adult commented that it required too little effort. Other negative features were the lack of stability of the phone inside the 3D printed object and the number of turns required for the screw top to secure the phone inside the mug.
With regards to the interface, the areas with the lowest average ratings (out of a maximum score of 9) across the 8 participants were overall frustration (6.6), level of stimulation (6.5), and the level of clarity on the level of progress (7.4). Highest ratings were received for the ease of learning to operate the system (8.75), the clarity of the sequence of screens (8.6), and the clarity of the organization of information (8.5).
Important positive characteristics that were commented on and that can be generalized to the design of other similar systems include:
A relevant set of exercises
A portable system that can be taken home
Supportive instructions
Large letters and numbers to support readability
A clear voice for instructions
Overall ease of use
Areas for improvement that will be incorporated into future iterations of the system and should be considered for future systems include:
Ensure the directions are clear
Provide positive feedback after completing an exercise
Ensure reliability of measurement system to have accurate counts that match user expectation
Loud volume for any auditory instructions or feedback
An angled phone screen for easier readability
Observations of participant use during the usability testing were consistent with the self-reported areas of difficulty.
DISCUSSION
This study was focused on the design of an effective home-based stroke rehabilitation system and identification of user requirements for the design of such a system. The results of this study support an interest from clinicians, older adults, and individuals with stroke for a home-based rehabilitation system that provides feedback on quality of movement and allows users to track their progress.
While many of the results are consistent with general principles of designing for older adults, such as ensuring clear directions and providing large lettering and numbering for improved readability, there were a number of specific design recommendations regarding the type of feedback users wanted to see. Contrary to expectation and the current trend in most mobile systems, the individuals with stroke placed low priority on sharing information with peers, even though most of the participants engage in community support groups for stroke survivors. Participants preferred immediate auditory feedback following task completion, but wanted a more detailed display of their performance at the end of the exercise that included pictures or graphics so that they could compare their current performance to their goals and to prior performance. They placed relatively low priority on receiving rewards for meeting goals. The participants were satisfied with receiving basic on-screen feedback for motivation, such as a star icon, and did not need a separate reward system. However, for long duration compliance of rehabilitation, further work should investigate the need for and design of a more elaborate reward system. Future work is also needed to identify the effectiveness of different forms of feedback provided to the user. The current work presents the expressed preferences, but trials are needed to compare the relative compliance and rehabilitation outcomes when different feedback modalities and timings are used.
ACKNOWLEDGEMENTS
Research reported in this publication was supported by the National Institute of Child Health & Human Development under award number 1 R21HD092243-01. The content is solely the responsibility of the authors and does not necessarily represent the view of the National Institutes of Health.
REFERENCES
- Byl N, Zhang WL, Coo S, & Tomizuka M (2015). Clinical impact of gait training enhanced with visual kinematic biofeedback: Patients with Parkinson’s disease and patients stable post stroke. Neuropsychologia, 79, 332–343. doi: 10.1016/j.neuropsychologia.2015.04.020 [DOI] [PubMed] [Google Scholar]
- Carter MJ, Carlsen AN, & Ste-Marie DM (2014). Self-controlled feedback is effective if it is based on the learner’s performance: a replication and extension of Chiviacowsky and Wulf (2005). Frontiers in Psychology, 5, 10. doi: 10.3389/fpsyg.2014.01325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiviacowsky S, & Wulf G (2005). Self-controlled feedback is effective if it is based on the learner’s performance. Research Quarterly for Exercise and Sport, 76(1), 42–48. [DOI] [PubMed] [Google Scholar]
- Chiviacowsky S, & Wulf G (2007). Feedback after good trials enhances learning. Research Quarterly for Exercise and Sport, 78(2), 40–47. [DOI] [PubMed] [Google Scholar]
- Dobkin BH, Plummer-D’Amato P, Elashoff R, Lee J, & Grp S (2010). International Randomized Clinical Trial, Stroke Inpatient Rehabilitation With Reinforcement of Walking Speed (SIRROWS), Improves Outcomes. Neurorehabilitation and Neural Repair, 24(3), 235–242. doi: 10.1177/1545968309357558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francis KL, Macrae PG, Spirduso WW, & Eakin T (2012). The effects of age on precision pinch force control across five days of practice. Current Aging Science, 5(1), 2–12. [PubMed] [Google Scholar]
- Fraser SA, Li KZH, & Penhune VB (2010). Dual-Task Performance Reveals Increased Involvement of Executive Control in Fine Motor Sequencing in Healthy Aging. Journals of Gerontology Series B-Psychological Sciences and Social Sciences, 65(5), 526–535. doi: 10.1093/geronb/gbq036 [DOI] [PubMed] [Google Scholar]
- Hodson T, Aplin T, & Gustafsson L (2016). Understanding the dimensions of home for people returning home post stroke rehabilitation. British Journal of Occupational Therapy, 79(7), 427–433. doi: 10.1177/0308022615619420 [DOI] [Google Scholar]
- Langan J, Subryan H, Nwogu I, & Cavuoto L (2017). Reported use of technology in stroke rehabilitation by physical and occupational therapists. Disability and Rehabilitation: Assistive Technology, 1–7. [DOI] [PubMed] [Google Scholar]
- Langhammer B, & Stanghelle JK (2003). Bobath or Motor Relearning Programme? A follow-up one and four years post stroke. Clinical Rehabilitation, 17(7), 731–734. doi: 10.1191/0269215503cr670oa [DOI] [PubMed] [Google Scholar]
- Novak I (2011). Effective home programme intervention for adults: a systematic review. Clinical Rehabilitation, 25(12), 1066–1085. doi: 10.1177/0269215511410727 [DOI] [PubMed] [Google Scholar]
- Ortman J, Velkoff V, & Hogan H (2014). An Aging Nation: The Older Population in the United States, Population Estimates and Projections, Current Population Reports Retrieved from http://www.census.gov/prod/2014pubs/p25-1140.pdf
- Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, … Amer Heart A (2007). Heart disease and stroke statistics - 2007 update - A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation, 115(5), E69–E171. doi: 10.1161/circulationaha.106.179918 [DOI] [PubMed] [Google Scholar]
- Santalucia P, Baviera M, Cortesi L, Tettamanti M, Marzona I, Nobili A, … Roncaglioni MC (2015). Epidemiologic Trends in Hospitalized Ischemic Stroke from 2002 to 2010: Results from a Large Italian Population-Based Study. Journal of Stroke & Cerebrovascular Diseases, 24(8), 1917–1923. doi: 10.1016/j.jstrokecerebrovasdis.2015.05.008 [DOI] [PubMed] [Google Scholar]
- Wolf SL, Lecraw DE, Barton LA, & Jann BB (1989). Forced use of hemiplegic upper extremities to reverse the effect of learned nonuse among chronic stroke and head-injured patients Experimental Neurology, 104(2), 125–132. doi: 10.1016/s0014-4886(89)80005-6 [DOI] [PubMed] [Google Scholar]
- Wolf SL, Thompson PA, Winstein CJ, Miller JP, Blanton SR, Nichols-Larsen DS, … Sawaki L (2010). The EXCITE Stroke Trial Comparing Early and Delayed Constraint-Induced Movement Therapy. Stroke, 41(10), 2309–2315. doi: 10.1161/strokeaha.110.588723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wutzke CJ, Faldowski RA, & Lewek MD (2015). Individuals Poststroke Do Not Perceive Their Spatiotemporal Gait Asymmetries as Abnormal. Physical Therapy, 95(9), 1244–1253. doi: 10.2522/ptj.20140482 [DOI] [PMC free article] [PubMed] [Google Scholar]


