Abstract
Purpose
To investigate the impact of sleep quality and chronotype on job burnout among medical residents under standardized residency training (SRT) in a tertiary hospital in Beijing, China.
Methods
Medical residents in the Department of Internal Medicine of Peking Union Medical College Hospital were assessed by Morning and Evening Questionaire-5 (MEQ-5), Pittsburgh sleep quality index (PSQI), and Maslach Burnout Inventory-General Survey (MBI-GS). Factors associated with burnout were analyzed.
Results
A total of 142 respondents returned completed questionnaires. Burnout was present in 85 (60%) residents. Prevalence of high emotional exhaustion, high depersonalization, and low personal accomplishment were 51%, 28%, and 18%, respectively. The global PSQI score of residents was 5.9 ± 2.4, and the self-reported sleep duration was 6.2 ± 0.8 h/day. The MEQ-5 distribution skewed towards morningness, with a median score of 14.5 [13.0, 16.3]. Poor daytime function significantly predicted emotional exhaustion and depersonalization. Chronotypes were not associated with any of the burnout components.
Conclusion
Sleep-related daytime dysfunction was strongly related to burnout. Strategies protecting the sleep of residents should be incorporated into the SRT programs for both efficiency and sustainability considerations.
Keywords: Residents, Chronotype, Sleep quality, Burnout
Introduction
Job burnout is a psychological response to chronic emotional and interpersonal job-related stressors. The concept is usually defined in three core dimensions: exhaustion, cynicism, and reduced personal accomplishment [1]. Burnout in the healthcare profession negatively affects both patient care and physician health, raising serious concerns for the healthcare system in the face of an aging society and physician workforce shortage [2].
Sleep and circadian disorders are common heath complaints clinicians encounter, yet the risk for such disorders is faced by clinicians themselves due to extended work hours, sleep interruptions, and shift work [3, 4]. The concept of sleep disorders has been broadened to a complex entity; still, the discrimination between “good” and “poor” sleepers (i.e., sleep quality) is widely adopted to identify possible sleep dysfunction, and predict physical and mental health [5]. Chronotype represents the behavioral pattern of organizing events, especially sleep and waking up, within the 24 h of a day. Misalignment of the chronotype with the environmental cycle may give rise to circadian disorders. An evening preference has also been associated with numerous psychological and metabolic hazards [6].
Conventionally, physician burnout has been attributed to factors including excessive workloads, unpredictable schedules, bureaucratic burdens, work-home conflicts, intense doctor-patient relationships, malpractice concerns, and financial hardships [2]. More recently, the impact of sleep and circadian disorders has been revealed [7]. As the risk for burnout and medical errors are increased among physicians with sleep impairment [8, 9], the American Academy of Sleep Medicine (AASM) calls for further investigation on the roles of sleep disruption, sleep deprivation, and circadian misalignment in physician burnout [10].
China has launched a nationwide Standardized Residency Training (SRT) program since 2013. The prevalence of burnout among SRT participants in China was 60–70% [11, 12], considerably higher than the rates reported in developed nations [13]. Higher occupational stress and limited social support due to a low physician-population ratio may, to some extent, explain the difference [14]. However, little is known on the association between sleep parameters and burnout in the SRT. This study sought to evaluate how sleep quality and chronotype would influence burnout among medical residents in a Chinese tertiary hospital.
Methods
Participants and procedures
A survey was conducted from April to May 2021 among all medical residents in the Peking Union Medical College Hospital (PUMCH), Beijing, China. The residents consist of clinical postgraduates and graduate students of PUMCH, as well as SRT trainees from other hospitals in the metropolitan area. The PUMCH is not a designated hospital for coronavirus disease 2019 (COVID-19), and none of the participants were involved in the care of COVID-19 patients. The survey was approved by the Research Ethics Committee of PUMCH (Approval No. JS-2860).
The questionnaires were distributed through an online open-access document application, Tencent Docs (Tencent, Shenzhen, Guangdong Province, China). Invitation letters with a brief introduction on the purpose and procedure of the survey were simultaneously sent by a chief resident of the Department of Internal Medicine. Participants completed the questionnaires anonymously.
Questionnaire and data collection
Four sections were included in a tailored questionnaire for this study: (1) personal and work characteristics, (2) Morning and Evening Questionaire-5 (MEQ-5), (3) Pittsburgh sleep quality index (PSQI), and (4) Maslach Burnout Inventory-General Survey (MBI-GS).
The personal and work characteristics section collected the following information: gender, age, marital status, seniority, average weekly working hours in the last month, frequency of night shifts, somatic symptoms the participants found harmful to their sleep, previous diagnosis of psychological disorders. Rotation information for the month was obtained separately from the rotation schedule of the Internal Medicine department.
The MEQ-5 is a simplified 5-item version of the classical 19-item MEQ for evaluation of chronotype [15]. The total scores for the 5 items were calculated, with higher scores representing earlier chronotypes. The validity and reliability of the Chinese version of MEQ-5 used in this study have been verified previously [16]. Considering the relatively small sample size and non-normal distribution, the previously determined chronotype classification was not applied.
The PQSI assesses self-reported sleep quality and disturbances over 1 month’s time [17]. Nineteen items generate 7 components, namely subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. For each component, the score range is 0–3. The sum score for the 7 components yields a global score. A Chinese translation of PQSI was adopted from a previous study [18].
Burnout was measured with a modified Chinese version of the original MBI-GS [19]. The Chinese MBI-GS consists of three components: emotional exhaustion (EE, 5 items), depersonalization (DP, 4 items), and low personal accomplishment (PA, 6 items). The 7-grade Likert Scale was used for each item, with 0 representing “never” and 6 representing “very often.” For EE and DP, a mean score within the component was calculated. For PA, the score for each item was reversed in the Likert Scale before averaging. After modification, the Chinese version of the MBI-GS was tested to have good construct validity and the internal consistency coefficients for the three components were 0.88, 0.83, and 0.82, respectively [19]. Since there is no broad consensus on the cutoffs for burnout or its sub-components, we adopted the definitions previously used in a large sample study on Chinese healthcare workers: high EE > 2.8, high DP > 2.5, low PA > 3.57 [20]. Overall burnout is considered when either of these criteria has been met.
Statistical analysis
Quantitative data in normal distribution were expressed as mean standard deviation, otherwise as median [1st, 3rd quartile]. Qualitative data were expressed as percentages or the exact counts. Data were analyzed with SPSS v. 22.0 software (IBM, Armonk, NY, USA). Univariate analyses were performed by Student’s t-test and ANOVA for quantitative data, and chi-square test for qualitative data. Correlations between MBI-GS and MEQ-5, PSQI were examined by Spearman’s correlation analysis. The degree of correlation was defined by the coefficient of Spearman’s correlation (r = 0–0.3: negligible correlation; r = 0.3–0.5: low correlation; r = 0.5–0.7: moderate correlation; r = 0.7–0.9: high correlation; and r = 0.9–1.0: very high correlation). Factors associated with burnout subscales were analyzed with hierarchical multiple regression. Age and variables with P-value less than 0.2 in the univariate analysis were entered into the multiple linear regression. Demographics, work situations (if present), and sleep and circadian variables were entered in each of the steps. Multicollinearity was tested through the variance inflation factor (VIF). None of the VIF values were greater than 5. All tests were two-sided. P < 0.05 was considered statistically significant.
Results
Personal and work characteristics
A total of 148 questionnaires have been distributed. One hundred forty-two respondents, 103 (73%) females and 39 (28%) males, returned completed questionnaires and were enrolled in analyses. The response rate was 96%. Age ranged from 21 to 37 years old, with an average of 27.0 ± 2.6 years old. Twenty-eight (20%) residents were married; the remaining were all unmarried. At the time of the survey, 108 (76%) participants were working in the medical inpatient department, while 15 (11%) and 19 (13%) participants worked at the emergency room and ICUs, respectively. The total work time was 77.8 [64.0, 88.3] h/week, and the night shift interval was 5 [4, 6] days. Reported somatic symptoms include pain, fever, cough, and diarrhea. Reported psychological disorders were depression and anxiety.
Sleep quality and chronotype
The mean global PSQI score of residents was 5.9 ± 2.4. The average self-reported sleep duration was 6.2 ± 0.8 h/day, and 99 (70%) residents had sleep duration less than 7 h. Respondents had a sleep latency of 10 [5, 21] min and a habitual sleep efficiency of 94 ± 77%. Fifty-three (37%) residents reported shift duty being the main interfering factor in their sleep. Eleven (8%) residents reported taking sleep pills over the past month.
The PSQI global scores were significantly associated with psychological disorders and longer working hours ( 80 h/week) (Table 1). PSQI component score profiles grouped by work hours are presented in Fig. 1. Residents with longer working hours had higher scores in most of the components, with statistical significance in the component score for sleep duration (1.0 ± 0.8 versus 0.7 ± 0.7, P = 0.025).
Table 1.
Univariate analysis of PSQI global scores
| Variables | n (%) | PSQI global score() | F/t | P |
|---|---|---|---|---|
| Gender | ||||
| Female | 103 (73) | 6.1 ± 2.3 | 1.092 | 0.277 |
| Male | 39 (28) | 5.6 ± 2.7 | ||
| Age | ||||
| 20–29 | 118 (83) | 6.1 ± 2.4 | 1.507 | 0.134 |
| 30 | 24 (17) | 5.3 ± 2.3 | ||
| Marital status | ||||
| Unmarried | 114 (80) | 6.0 ± 2.5 | 0.772 | 0.441 |
| Married | 28 (20) | 5.6 ± 1.7 | ||
| Years in SRT | ||||
| Year 1–2 | 79 (56) | 6.1 ± 2.6 | 1.068 | 0.287 |
| Year 3 or completed | 63 (44) | 5.7 ± 2.2 | ||
| Department | ||||
| Medical inpatient | 108 (76) | 6.0 ± 2.5 | 0.097 | 0.908 |
| Emergency | 15 (11) | 5.7 ± 2.6 | ||
| ICUs | 19 (13) | 5.8 ± 1.8 | ||
| Night shift frequency | ||||
| one in 5 days | 102 (72) | 6.0 ± 2.5 | 0.843 | 0.4 |
| one in 4 days | 40 (28) | 5.7 ± 2.2 | ||
| Total working hours | ||||
| 80/week | 74 (52) | 5.5 ± 2.3 | − 2.357 | 0.02 |
| 80/week | 68 (48) | 6.4 ± 2.4 | ||
| Somatic symptoms | ||||
| No | 124 (87) | 5.9 ± 2.3 | − 0.878 | 0.381 |
| Yes | 18 (13) | 6.4 ± 3.3 | ||
| Psychological disorders | ||||
| No | 126 (89) | 5.7 ± 2.3 | − 3.335 | 0.001 |
| Yes | 16 (11) | 7.8 ± 2.5 |
Abbreviations: F/t F value for ANOVA or t value for Student’s test; ICU intensive care unit; PSQI Pittsburgh sleep quality index; SRT standardized residency training
Fig. 1.
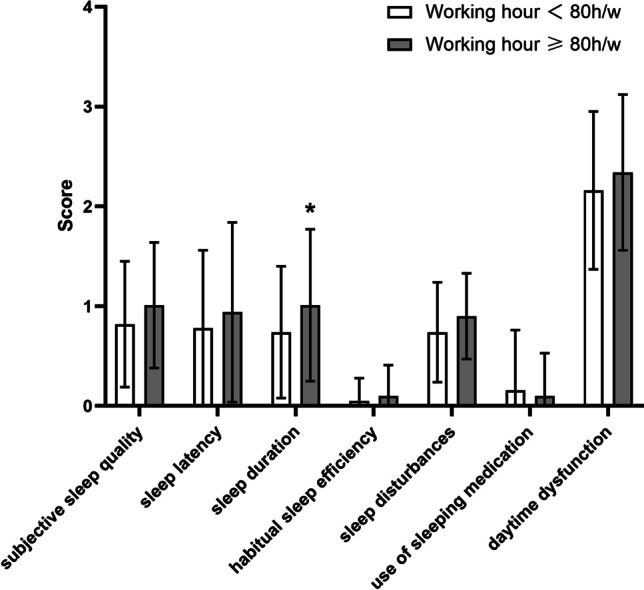
PSQI component score profiles. *P < 0.05. Abbreviation: PSQI, Pittsburgh sleep quality index
The scores for MEQ-5 showed a skewed distribution (coefficient of skewness 0.44, coefficient of kurtosis 0.10) towards morning type, with a median score of 14.5 [13.0, 16.3]. The MEQ-5 scores presented a negligible correlation with sleep duration (r = 0.207, P = 0.014), and were not correlated with other PSQI components.
Job burnout
The scores for MBI-GS components (range 0–6) were EE 3.0 ± 1.2, DP 1.9 ± 1.3, and PA 2.4 ± 1.2. According to the empirical cutoffs, the numbers of residents with high EE, high DP, and low PA were 73 (51%), 40 (28%), and 26 (18%), respectively. Overall, burnout was present in 85 (60%) residents.
In bivariate analysis, younger residents had a higher level of EE, and residents with longer working hours had a higher level of PA (Table 2). Correlations between MBI-GS and PSQI, MEQ-5 scores are detailed in Table 3. Daytime dysfunction showed a moderate positive correlation with EE and a low positive correlation with DP.
Table 2.
Univariate analysis of job burnout
| Variables | EE | DP | PA | ||||||
|---|---|---|---|---|---|---|---|---|---|
| F/t | P | F/t | P | F/t | P | ||||
| Gender | |||||||||
| Female | 3.0 ± 1.2 | − 0.112 | 0.911 | 1.9 ± 1.3 | 0.393 | 0.695 | 2.5 ± 1.2 | 0.832 | 0.407 |
| Male | 3.0 ± 1.2 | 1.8 ± 1.5 | 2.3 ± 1.2 | ||||||
| Age | |||||||||
| 20–29 | 3.1 ± 1.2 | 2.157 | 0.033 | 2.0 ± 1.3 | 1.955 | 0.053 | 2.5 ± 1.2 | 1.085 | 0.28 |
| 30 | 2.5 ± 1.0 | 1.4 ± 1.2 | 2.2 ± 1.1 | ||||||
| Marital status | |||||||||
| Unmarried | 3.0 ± 1.2 | 1.148 | 0.253 | 2.0 ± 1.3 | 0.921 | 0.358 | 2.5 ± 1.2 | 1.296 | 0.197 |
| Married | 2.7 ± 1.2 | 1.7 ± 1.5 | 2.2 ± 1.1 | ||||||
| Years in SRT | |||||||||
| Year 1–2 | 3.0 ± 1.2 | 0.821 | 0.413 | 1.9 ± 1.3 | − 0.201 | 0.841 | 2.4 ± 1.2 | − 0.124 | 0.902 |
| Year 3 or completed | 2.9 ± 1.1 | 1.9 ± 1.4 | 2.4 ± 1.2 | ||||||
| Department | |||||||||
| Medical inpatient | 3.0 ± 1.2 | 0.193 | 0.824 | 2.0 ± 1.4 | 1.464 | 0.235 | 2.5 ± 1.2 | 0.676 | 0.51 |
| Emergency | 3.1 ± 0.9 | 2.1 ± 1.0 | 2.4 ± 0.9 | ||||||
| ICUs | 2.8 ± 1.0 | 1.4 ± 1.0 | 2.1 ± 1.3 | ||||||
| Total working hours | |||||||||
| 80/week | 2.8 ± 1.1 | − 1.463 | 0.146 | 2.0 ± 1.4 | 0.529 | 0.598 | 2.6 ± 1.1 | 2.183 | 0.031 |
| 80/week | 3.1 ± 1.2 | 1.9 ± 1.3 | 2.2 ± 1.2 | ||||||
Abbreviations: DP depersonalization; EE emotional exhaustion; F/t F value for ANOVA or t value for Student’s test; ICU intensive care unit; PA personal accomplishment; PSQI Pittsburgh sleep quality index; SRT standardized residency training
Table 3.
Spearman’s correlation analysis between MBI-GS, MEQ-5, and PSQI
| EE | DP | PA | ||||
|---|---|---|---|---|---|---|
| r | P | r | P | r | P | |
| MEQ-5 | − 0.029 | 0.728 | − 0.098 | 0.245 | − 0.157 | 0.062 |
| PSQI | ||||||
| Subjective sleep quality | 0.211 | 0.012 | 0.127 | 0.132 | 0.003 | 0.975 |
| Sleep latency | 0.059 | 0.487 | 0.069 | 0.416 | 0.053 | 0.534 |
| Sleep duration | 0.197 | 0.018 | 0.121 | 0.152 | 0.039 | 0.643 |
| Habitual sleep efficiency | 0.065 | 0.444 | 0.017 | 0.843 | − 0.014 | 0.864 |
| Sleep disturbance | 0.109 | 0.198 | 0.047 | 0.58 | − 0.09 | 0.288 |
| Use of sleep medication | 0.112 | 0.186 | 0.086 | 0.31 | 0.026 | 0.761 |
| Daytime dysfunction | 0.589 | < 0.001 | 0.358 | < 0.001 | − 0.179 | 0.034 |
Abbreviations: DP depersonalization; EE emotional exhaustion; MBI-GS Maslach Burnout Inventory-General Survey; MEQ-5 Morning and Evening Questionaire-5; PA personal accomplishment; PSQI Pittsburgh sleep quality index
The results of hierarchical linear model analyses of the factors associated with MBI-GS are shown in Table 4. For EE and DP, age and daytime dysfunction were included in the final model. Younger age and severe daytime dysfunction predicted higher EE (F = 8.749, P < 0.01) and DP (F = 4.459, P < 0.01). The sleep-related factor explained 27% of the variance in EE, and 7.5% of the variance in DP. For PA, only the weekly working hour was incorporated in the final model, and longer working hours predicted higher PA (F = 3.176, P < 0.01).
Table 4.
Hierarchical multiple regression of MBI-GS
| Variables | EE | DP | PA | |||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model2 | Model 3 | Model 1 | Model2 | Model 1 | Model2 | Model 3 | |
| Demographics | ||||||||
| Age (yr) | − 0.203* | − 0.2* | − 0.2** | − 0.203* | − 0.2* | − 0.125 | − 0.135 | − 0.117 |
| Marital status (married) | − 0.06 | − 0.062 | − 0.047 | |||||
| Work situations | ||||||||
| Weekly working hour (h) | 0.054 | − 0.013 | − 0.228** | − 0.246** | ||||
| Sleep and circadian parameters | ||||||||
| MEQ-5 | − 0.109 | |||||||
| PSQI | ||||||||
| Subjective sleep quality | 0.031 | 0.006 | ||||||
| Sleep duration | 0.000 | 0.016 | ||||||
| Sleep disturbance | − 0.013 | |||||||
| Use of sleep medication | 0.01 | |||||||
| Daytime dysfunction | 0.516** | 0.267** | 0.129 | |||||
| ΔR2 | 0.041 | 0.003 | 0.27 | 0.04 | 0.075 | 0.025 | 0.052 | 0.028 |
| R2 | 0.041 | 0.044 | 0.314 | 0.04 | 0.115 | 0.025 | 0.077 | 0.105 |
| F | 5.99* | 3.192* | 8.749** | 5.903* | 4.459** | 1.78 | 3.818* | 3.176** |
*P < 0.05, **P < 0.01. In step 1, demographics were added. For EE and PA, work situations were added in step 2, and sleep and circadian parameters were added in step 3. For DP, sleep and circadian parameters were added in step 2
Abbreviations: DP depersonalization; EE emotional exhaustion; MBI-GS Maslach Burnout Inventory-General Survey; MEQ-5 Morning and Evening Questionaire-5; PA personal accomplishment; PSQI Pittsburgh sleep quality index
Discussion
The current survey evaluated sleep quality, chronotype, and their effect on burnout among medical residents in PUMCH. The PUMCH is the birthplace of medical residency in China, and one of the pilot training centers for the newly implemented SRT. The survey confirmed a high prevalence of burnout and identified an association between poor daytime dysfunction and burnout. The findings emphasize the importance of sleep protection during resident training and point directions for further improvement of the program.
The sleep quality of medical residents, with a mean PSQI score near 6, was worse than the community populations in urban China, whose mean global PSQI was 3.88–4.18 [22, 23]. This was primarily contributed by the pronounced level of daytime dysfunction among residents, as scores on other components were comparable between residents and general citizens. It is of note that residents with longer working hours had significantly higher PSQI global scores and shorter sleep duration. These results raise concern as SRT in China has been known for heavy workloads and high work pressure [11, 24]. The USA enacted an 80 h per week limitation for residents since 2003, partially for the improvement of sleep deprivation [25]. While the regulation improved residents’ quality of life, apprehension exists about the continuity of patient care and adequacy of medical training [26, 27]. The scenario in China is further complicated by the limited human resource in the healthcare profession [14]. Nevertheless, the intensity of training should be carefully balanced with the protection of sleep in the design of a sustainable and healthy SRT program.
In the present study, the total prevalence of burnout was 60%. Although various assessment methods and cutoffs were applied, previous studies on Chinese residents using a similar definition for burnout (i.e., at least one symptom of burnout) yielded comparable overall burnout rates [11, 12]. Corresponding to other domestic and international studies [28, 29], EE was identified as the predominant burnout symptom in our participants, followed by DP and low PA. Among physicians, EE refers to feelings of exhaustion or used up at the end of the day, while DP and low PA refer to objectivation of patients and questioning over the meaning of patient care. In other words, burnout in our SRT trainees is primarily intrapersonal feelings, rather than feelings towards patients or the profession.
Previously, the main risk factors for physician burnout are linked to heavy workload (longer total working hours, longer continuous working hours, night shifts, etc.) and dissatisfaction with the current situation (training program, doctor-patient relationship, income, etc.) [11, 12, 28]. More recent studies have put sleep disturbances under the spotlight. In surveys conducted among medical students, both sleep duration and sleep quality correlated with higher risks for burnout [21, 30]. Among interns and residents, this association was maintained in only some of the studies [31–33]. Our study demonstrated daytime dysfunction predicts exhaustion and depersonalization. This association was independent of workload-related factors such as total working hours. Proposed models linking sleep disorders and burnout include (1) burnout is the result of physical, emotional, and mental depletion, which can be restored through healthy sleep; (2) chronic stress hyperactivates the hypothalamic–pituitary–adrenal axis and mediates both burnout and sleep deprivation [7]. These models take burnout as an integrated concept. Together with findings from other studies [33], our data highlights the complexity of burnout, as the influence of sleep-related parameters varies substantially on different dimensions of burnout. At present, commonly used interventions for physician burnout include institutional support individual-focused stress management, and self-care training [34]. A recent feasibility study demonstrated sleep hygiene interventions might have beneficial effects on burnout [35], yet, additional research is required to establish the role of sleep-targeted interventions in the field of burnout control.
An individual’s circadian rhythm is influenced by both the intrinsic biological rhythms and the external environments. Since industrialization, the timing of sleep has been greatly influenced by weekly working schedules and daily working patterns. People with late chronotypes tend to accumulate sleep debt over the workdays and compensate by prolonged sleep on weekends [36]. In addition, working at periods distant from the best performance phase could bring damage to attention and cause safety concerns [37]. Results from our single-center study, however, identified only a poor correlation between chronotype and sleep duration, and did not associate the chronotype with daytime dysfunction or any of the burnout scales. The exact effect of chronotype on burnout among medical workers remains largely unclear, as only a few studies have addressed the problem, and yielded controversial results [38, 39]. Whether circadian rhythm has an independent impact on job performance and job well-being should be evaluated in larger populations in the future.
Our study explored the role of sleep quality in physician well-being among Chinese SRT trainees with validated instruments and high response rate. However, the study is not without limitations. First, the result only represents a single SRT center in the capital of China, while regional development is highly uneven in the country. Second, sleep is measured with self-reported data, and may lead to bias. Finally, potential contributing factors for burnout (e.g., social support, income, relationship status, presence of children) were not evaluated.
In conclusion, EE is the primary burnout component among medical residents in China. Poor daytime function strongly predicts higher EE and DP. Protection of residents’ sleep should be taken into account in the improvement of SRT programs.
Acknowledgements
The authors thank the directors (Dr. Xuemei Li, Ms. Qing Jia, Dr. Hang Li) and secretaries for education (Dr. Chao Li, Dr. Jianzhong Shen, Dr. Xuan Qu) of the Department of Internal Medicine, Peking Union Medical Hospital, for their help coordinating the study.
Abbreviations
- AASM
American Academy of Sleep Medicine
- ANOVA
Analysis of variance
- CI
confidence interval
- COVID-19
coronavirus disease 2019
- DE
definite evening
- DM
definite morning
- DP
depersonalization
- EE
emotional exhaustion
- MBI-GS
Maslach Burnout Inventory-General Survey
- ME
moderately evening
- MEQ-5
Morning and Evening Questionaire-5
- MM
moderately morning
- NT
neither type
- OR
odds ratio
- PA
personal accomplishment
- PSQI
Pittsburgh sleep quality index
- PUMCH
Peking Union Medical College Hospital
- SRT
standardized residency training
- VIF
variance inflation factor
Author contribution
All authors contributed to the study’s conception and design. CS and JML carried out the study and collected the data. CS analyzed the data and drafted the manuscript. JML and XY revised the manuscript. All authors read and approved the final manuscript.
Funding
The current study was funded by National Natural Science Foundation of China (Grant No. 81570085) and CAMS Innovation Fund for Medical Sciences (CIFMS) (2021-I2M-C&T-B-013).
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval
The current study has been approved by the Research Ethics Committee of Peking Union Medical College Hospital (Approval No. JS-2860) and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Conflict of interest
The authors declare no competing interests.
Footnotes
The original online version of this article was revised: In the originally published version of this article, the third author, Yi Xiao, was listed as Yi Xiao MD. Yi is the GIVEN name, Xiao is the FAMILY name, and MD is not part of the name.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/9/2022
A Correction to this paper has been published: 10.1007/s11325-022-02654-7
References
- 1.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52(1):397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 2.West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516–529. doi: 10.1111/joim.12752. [DOI] [PubMed] [Google Scholar]
- 3.Shockey TM, Wheaton AG. Short sleep duration by occupation group - 29 states, 2013–2014. MMWR Morb Mortal Wkly Rep. 2017;66(8):207–213. doi: 10.15585/mmwr.mm6608a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pascoe M, Alberts J, Wang L, et al. Feasibility of electronic sleep disorder screening in healthcare workers of a large healthcare system. Sleep Med. 2020;73:181–186. doi: 10.1016/j.sleep.2020.07.028. [DOI] [PubMed] [Google Scholar]
- 5.Ohayon M, Wickwire EM, Hirshkowitz M, et al. National Sleep Foundation’s sleep quality recommendations: first report. Sleep Health. 2017;3(1):6–19. doi: 10.1016/j.sleh.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 6.Gentry NW, Ashbrook LH, Fu Y-H, Ptáček LJ. Human circadian variations. J Clin Invest. 2021;131(16):e148282. doi: 10.1172/JCI148282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stewart NH, Arora VM. The impact of sleep and circadian disorders on physician burnout. Chest. 2019;156(5):1022–1030. doi: 10.1016/j.chest.2019.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quan SF, Weaver MD, Barger LK, O’Brien CS, Viyaran N, Qadri S, Czeisler CA. 0996 interim findings from a sleep health and wellness program to reduce occupational burnout. Sleep. 2019;42(Supplement 1):A401. doi: 10.1093/sleep/zsz067.993. [DOI] [Google Scholar]
- 9.Trockel MT, Menon NK, Rowe SG, et al. Assessment of physician sleep and wellness, burnout, and clinically significant medical errors. JAMA Netw Open. 2020;3(12):e2028111. doi: 10.1001/jamanetworkopen.2020.28111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kancherla BS, Upender R, Collen JF, et al. Sleep, fatigue and burnout among physicians: an American Academy of Sleep Medicine position statement. J Clin Sleep Med. 2020;16(5):803–805. doi: 10.5664/jcsm.8408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Y, Huang X, Li H, Zeng X, Shen T. Survey results of job status of residents in a standardized residency training program. BMC Med Educ. 2019;19(1):281. doi: 10.1186/s12909-019-1718-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huang L, Caspari JH, Sun X, Thai J, Li Y, Chen FZ, Zhao XD. Risk and protective factors for burnout among physicians from standardized residency training programs in Shanghai: a cross-sectional study. BMC Health Serv Res. 2020;20(1):965. doi: 10.1186/s12913-020-05816-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, Mata DA. Prevalence of burnout among physicians: a systematic review. JAMA. 2018;320(11):1131–1150. doi: 10.1001/jama.2018.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization (2021) Global Health Workforce statistics database: Medical doctors (per 10 000 population). WHO. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/medical-doctors-(per-10-000-population). Accessed 06 Jan 2022
- 15.Adan A, Almirall H. Horne & Östberg morningness-eveningness questionnaire: a reduced scale. Pers Individ Dif. 1991;12(3):241–253. doi: 10.1016/0191-8869(91)90110-W. [DOI] [Google Scholar]
- 16.Li WX, Muyese A, Xie ZT, Liu WH, Zhang B. Validity and reliability of the Chinese version of Morningness/Eveningness Questionnaire-5 items (MEQ-5) in students of technical schools. Chin Ment Health J. 2016;30(6):406–412. doi: 10.3969/j.issn.1000-6729.2016.06.002. [DOI] [Google Scholar]
- 17.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 18.Liu XC, Tang MQ, Hu L, Wang AZ, Wu HX, Zhao GF, Gao CN, Li WS. Reliability and validity of the Pittsburgh Sleep Quality Index. Chin J Psychiatry. 1996;29(02):103–107. [Google Scholar]
- 19.Li CP, Shi K. The influence of distributive justice and procedural justice on job burnout. Acta Psychol Sin. 2003;35(5):677–684. [Google Scholar]
- 20.Wu H, Liu L, Wang Y, Gao F, Zhao X, Wang L. Factors associated with burnout among Chinese hospital doctors: a cross-sectional study. BMC Public Health. 2013;13:786. doi: 10.1186/1471-2458-13-786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee KP, Yeung N, Wong C, Yip B, Luk LHF, Wong S. Prevalence of medical students’ burnout and its associated demographics and lifestyle factors in Hong Kong. PLoS One. 2020;15(7):e0235154. doi: 10.1371/journal.pone.0235154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu W, Jiang Y, Wang N, et al. Sleep quality of Shanghai residents: population-based cross-sectional study. Qual Life Res. 2019;29(4):1055–1064. doi: 10.1007/s11136-019-02371-x. [DOI] [PubMed] [Google Scholar]
- 23.Tang J, Liao Y, Kelly BC, et al. Gender and regional differences in sleep quality and insomnia: a general population-based study in Hunan Province of China. Sci Rep. 2017;7:43690. doi: 10.1038/srep43690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hou JJ, He YF, Zhao XD, Thai J, Fan MX, Feng Y, Huang L. The effects of job satisfaction and psychological resilience on job performance among residents of the standardized residency training: a nationwide study in China. Psychol Health Med. 2020;25(9):1106–1118. doi: 10.1080/13548506.2019.1709652. [DOI] [PubMed] [Google Scholar]
- 25.Philibert I, Friedmann P, Williams WT. New requirements for resident duty hours. JAMA. 2002;288(9):1112–1114. doi: 10.1001/jama.288.9.1112. [DOI] [PubMed] [Google Scholar]
- 26.Fletcher KE, Underwood W, Davis SQ, Mangrulkar RS, McMahon LF, Saint S. Effects of work hour reduction on residents’ lives: a systematic review. JAMA. 2005;294(9):1088–1100. doi: 10.1001/jama.294.9.1088. [DOI] [PubMed] [Google Scholar]
- 27.Bolster L, Rourke L. The effect of restricting residents’ duty hours on patient safety, resident well-being, and resident education: an updated systematic review. J Grad Med Educ. 2015;7(3):349–363. doi: 10.4300/JGME-D-14-00612.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen K-Y, Yang C-M, Lien C-H, Chiou H-Y, Lin M-R, Chang H-R, Chiu W-T. Burnout, job satisfaction, and medical malpractice among physicians. Int J Med Sci. 2013;10(11):1471–1478. doi: 10.7150/ijms.6743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, West CP, Sloan J, Oreskovich MR. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199. [DOI] [PubMed] [Google Scholar]
- 30.Wolf MR, Rosenstock JB. Inadequate sleep and exercise associated with burnout and depression among medical students. Acad Psychiatry. 2017;41(2):174–179. doi: 10.1007/s40596-016-0526-y. [DOI] [PubMed] [Google Scholar]
- 31.Rosen IM, Gimotty PA, Shea JA, Bellini LM. Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad Med. 2006;81(1):82–85. doi: 10.1097/00001888-200601000-00020. [DOI] [PubMed] [Google Scholar]
- 32.Driesman AS, Strauss EJ, Konda SR, Egol KA. Factors associated with orthopaedic resident burnout: a pilot study. J Am Acad Orthop Surg. 2020;28(21):900–906. doi: 10.5435/JAAOS-D-19-00648. [DOI] [PubMed] [Google Scholar]
- 33.Geng H, Tan F, Deng Y, Lai LF, Zhang JQ, Wu ZL, Liu PB, Zhu QQ. High rate of burnout among residents under standardized residency training in a tertiary teaching hospital of middle China: results from a cross-sectional survey. Medicine (Baltimore) 2020;99(27):e20901. doi: 10.1097/MD.0000000000020901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388(10057):2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 35.Brubaker JR, Swan A, Beverly EA. A brief intervention to reduce burnout and improve sleep quality in medical students. BMC Med Educ. 2020;20(1):345. doi: 10.1186/s12909-020-02263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Roenneberg T, Wirz-Justice A, Merrow M. Life between clocks: daily temporal patterns of human chronotypes. J Biol Rhythms. 2003;18(1):80–90. doi: 10.1177/0748730402239679. [DOI] [PubMed] [Google Scholar]
- 37.Mtchoch RL, Mordkoff JT. Chronotype and time-of-day influences on the alerting, orienting, and executive components of attention. Exp Brain Res. 2009;192(2):189–198. doi: 10.1007/s00221-008-1567-6. [DOI] [PubMed] [Google Scholar]
- 38.Cheng W-J, Hang L-W. Late chronotype and high social jetlag are associated with burnout in evening-shift workers: assessment using the Chinese-version MCTQ. Chronobiol Int. 2018;35(7):910–919. doi: 10.1080/07420528.2018.1439500. [DOI] [PubMed] [Google Scholar]
- 39.Gohar AA, Knauert M, Kalot MA, et al (2021) Influence of medical trainee sleep pattern (chronotype) on burn-out and satisfaction with work schedules: a multicentre observational study. Postgrad Med J postgradmedj-2021–140975. 10.1136/postgradmedj-2021-140975 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.


