Abstract
The current study aimed to investigate the diagnostic and prognostic value of urine biomarkers among female patients with dysfunctional voiding (DV). Urine samples were collected from 43 female patients with DV and 25 controls. Oxidative stress biomarkers (8-hydroxy-2-deoxyguanosine [8-OHdG], 8-isoprostane, and total antioxidant capacity [TAC]) and inflammatory markers (interleukin-1 beta [IL-1β], IL-2, IL-6, IL-8, tumor necrosis factor alpha, nerve growth factor, and brain-derived neurotrophic factor) levels were analyzed. In total, 26 patients with DV received further treatment with biofeedback pelvic floor muscle exercise or external urethral sphincter botulinum toxin A injections. Patients with DV had significantly higher urine 8-OHdG, IL-1β, IL-8, and brain-derived neurotrophic factor levels than controls. Both urine 8-OHdG and IL-1β levels were positively correlated with clinical symptoms. Patients with DV who had successful treatment outcomes had significantly lower pretreatment urine 8-isoprostane and TAC levels than those with unsuccessful outcomes. The pretreatment urine TAC level was the only independent predictor of successful treatment outcomes (odds ratio: 0.995). Compared with controls, female patients with DV had distinct urine oxidative stress biomarker and inflammatory marker profiles, which also mapped their clinical characteristics and treatment outcomes. These urine analytes might have diagnostic and prognostic values among female patients with DV.
Subject terms: Biomarkers, Urology
Introduction
During voluntary voiding, complete bladder emptying within a normal span of time is dependent on the initial relaxation of the external urethral sphincter (EUS) and subsequent sustained detrusor contraction. Abnormal activities of the EUS and/or pelvic floor muscle (PFM) during voiding can cause bladder outlet obstruction (BOO)1. Previously, in neurologically intact individuals, this condition is referred to as non-neurogenic bladder2. However, currently, it is more commonly called dysfunctional voiding (DV), and its occurrence among female individuals with voiding dysfunction has gained increasing attention recently3–5. The accurate diagnosis of DV relies on videourodynamic studies (VUDSs)3, which are invasive diagnostic procedures. The effective treatments for DV include biofeedback PFM exercise6,7 and EUS botulinum toxin A (BoNT-A) injections8. However, there is no consensus regarding the predictors of treatment outcomes.
In a retrospective analysis, 325 (17%) of 1914 women with refractory lower urinary tract symptoms who underwent VUDS were diagnosed with DV4. This condition is an important etiology of BOO among women3. In BOO progression, excessive oxidative stress and hypoxia-related inflammation resulting from cyclic ischemia–reperfusion injury involve in the bladder remodeling process9. The importance of oxidative stress markers (such as 8-hydroxy-2-deoxyguanosine [8-OHdG] and F2-isoprostane) and antioxidant biomarkers (such as total antioxidant capacity [TAC]) in BOO was assessed in animal model and human studies10. Urine is a highly attractive biospecimen for the biomarker analysis of different pathological diseases due to its non-invasive character11. Accordingly, urine oxidative stress and antioxidant biomarkers and their related inflammatory substances can be potential biomarkers of DV.
Despite some limitations, numerous research articles have reported about the association between urine biomarkers and lower urinary tract symptoms12. However, there is no study about female patients with DV. Therefore, the current research aimed to investigate the diagnostic and prognostic values of urine oxidative stress biomarkers and inflammatory markers levels among female patients with DV.
Materials and methods
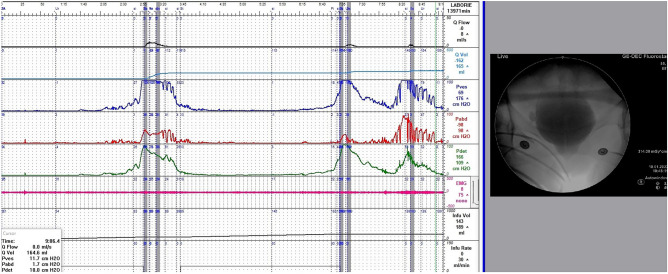
Patients and investigation of the clinical characteristics
From February 2015 to February 2021, we prospectively enrolled 46 female patients diagnosed with videourodynamic-confirmed DV at the department of urology of a single medical center. All patients underwent VUDS with the indication of refractory lower urinary tract symptoms. The diagnostic details were interpreted according to the International Continence Society terminology1. The following VUDS parameters were recorded: first sensation of bladder filling (FSF), bladder compliance, cystometric bladder capacity (CBC), detrusor voiding pressure (Pdet), maximal urinary flow rate (Qmax), corrected maximal urinary flow rate (cQmax, defined as Qmax/√CBC), voided volume (Vol), post-void residual volume (PVR), voiding efficacy (VE, defined as vol / CBC), and female bladder outlet obstruction index (BOOIf, defined as Pdet—2.2*Qmax)13. Patients with an open bladder neck but a narrow membranous urethra or PFM (a spinning top appearance) on real-time fluoroscopy, increased EUS electromyography activities, and low Qmax (with or without a high Pdet) during voiding were diagnosed with DV (Fig. 1). In addition, only patients without a history of neurological disease were eligible for this study. The exclusion criteria included genital prolapse, active urinary tract infection, interstitial cystitis, and previous surgery for urinary incontinence. In total, 25 women with stress urinary incontinence but without other significant storage or voiding dysfunction on VUDS were included as controls.
Figure 1.
Videourodynamic study of dysfunctional voiding in a woman with an open bladder neck but a narrow membranous urethra (a spinning top appearance) on real-time fluoroscopy, increased urethral sphincter electromyography activities, a high detrusor pressure, and a low maximum flow rate during voiding.
All patients were assessed with the International Prostate Symptom Score (IPSS), which included total IPSS, IPSS storage subscore (IPSS-S), and IPSS voiding subscore (IPSS-V). Biofeedback PFM exercise or EUS BoNT-A 100 U injection was recommended to patients with medically refractory DV according to the reported treatment protocols7,8. The treatment outcome was evaluated using the Global Response Assessment (GRA) as previous study7. Moreover, it was categorized as − 3, − 2, − 1, 0, 1, 2, and 3, which indicated markedly worse to markedly improved status) based on satisfaction 3 months after treatment. A successful outcome was defined as a GRA score of ≥ 2 (moderately and markedly improved).
Assessment of urine biomarker levels
Urine samples were collected from all patients with DV and controls. Urine was self-voided by patients who had a full bladder sensation. Then, urinalysis was performed simultaneously to confirm an infection-free status before urine samples were stored. In total, 50-mL urine samples were placed on ice immediately and transferred to the laboratory for preparation. The samples were centrifuged at 1800 rpm for 10 min at 4 °C. The supernatant was separated into aliquots in 1.5-mL tubes (1 mL per tube) and was preserved in a freezer at − 80 °C. Before further analyses were performed, the frozen urine samples were centrifuged at 12,000 rpm for 15 min at 4 °C, and the supernatants were used for subsequent evaluations.
Quantification of 8-OHdG
The quantification of 8-OHdG in urine samples was performed in accordance with the manufacturer’s instructions (8-OHdG ELISA Kit, BioVision). Briefly, 50 μL of biotin-detection antibody working solution and 50 μL of sample were sequentially added to 96-well plates (panel kits), and the plates were incubated for 45 min at 37 °C. The well contents were removed, and the plates were washed three times with 350 μL of wash buffer. Next, 100 mL of horseradish peroxidase-streptavidin conjugate working solution was added to each well, and the plates were incubated for 30 min at 37 °C. The solution was discarded, and 350 μL of wash buffer was used to wash the plates five times. Next, 90 mL of TMB substrate was added into each well; incubation was then performed in the dark for 30 min at 37 °C. Finally, 50 μL of stop solution was added, and the plates were evaluated on the microplate reader at 450 nm. The median fluorescence intensities of the targets were analyzed to calculate the corresponding concentrations in the samples.
Quantification of 8-isoprostane
Eight-isoprostane belongs to F2-isoprostane class. The quantification of 8-isoprostane in urine samples was performed in accordance with the manufacturer’s instructions (8 isoprostane ELIZA kit, Enzo). Briefly, 50 μL of 8-iso-PGF2α conjugate solution, 50 μL of 8-iso-PGF2α antibody solution, and 100 μL of sample were sequentially added to 96-well plates (panel kits), and the plates were incubated 2 h at room temperature on a plate shaker at 500 rpm. The well contents were removed, and the plates were washed three times with 400 μL of wash buffer. In total, 200 mL of the pNpp substrate solution was added to each well, and the plates were incubated for 45 min at room temperature without shaking. Finally, 50 μL of stop solution was added, and the plates were read immediately at 405 nm. The median fluorescence intensities of the targets were analyzed to calculate the corresponding concentrations in the samples. The measurement of urine 8-isoprostane levels was standardized using urinary creatinine levels.
Quantification of TAC
The quantification of TAC in the samples was performed in accordance with the manufacturer’s instructions (Total Antioxidant Capacity Assay Kit, abcam). Briefly, 100 μL of Cu2 + working solution and 100 μL of sample were sequentially added to 96-well plates (panel kits), and the plates were incubated for 90 min at room temperature on a shaker protected from light. Finally, the plates were evaluated on the microplate reader at 570 nm. The median fluorescence intensities of the target were analyzed to calculate the corresponding TAC concentrations in the samples.
Evaluation of inflammatory substances
Inflammatory markers including cytokines and neurotrophins in the urine samples were assayed using commercially available microspheres with the Milliplex® human cytokine/chemokine magnetic bead-based panel kit (Millipore, Darmstadt, Germany).
Seven targeted analytes were used for the multiplex kit, and these included the following inflammatory cytokines: catalog number HCYTMAG-60 K (interleukin-1 beta [IL-1β], IL-2, IL-6, IL-8, and tumor necrosis factor alpha [TNFα]), catalog number HADK2MAG-61 K (nerve growth factor [NGF]), and catalog number HNDG3MAG-36 K (brain-derived neurotrophic factor [BDNF]). The following laboratory procedures for the quantification of these targeted analytes were similar to those reported in our previous studies14,15.
This study was approved by the Institutional Review Board and Ethics Committee of Buddhist Tzu Chi General Hospital (no. IRB107-37-A and IRB: 109-095-B). All methods/study were performed in accordance with the relevant guidelines and regulations. All patients with DV and controls were provided with information about the risk, rationale, procedures, ethics, and costs of this study, and they provided informed consent.
Statistical analysis
Continuous variables were presented as means ± standard deviations and categorical variables as numbers and percentages. Outliers were defined as values outside the range between the means ± three standard deviations for each biomarker in either the study or the control group, and these were excluded from further analysis. The clinical data and urine biomarker levels between the study and control groups and between the different treatment outcome groups were analyzed using analysis of variance. Post-hoc power calculation was performed in the biomarker with significant difference between the study and control groups. Linear regression analysis with Pearson correlation was performed to determine the association between clinical characteristics and urine biomarker levels. To predict successful treatment outcomes, univariate and multivariate logistic regression model analyses were conducted with the calculation of odds ratio (OR). All calculations were performed using SPSS Statistics software for Windows version 20.0 (IBM Corp., Armonk, NY, the USA). A p value of < 0.05 was considered statistically significant.
Results
The mean age of female patients with DV (n = 43) was 54.0 ± 14.1 (range: 24–77) years, and that of controls (n = 25) was 60.5 ± 10.6 (range: 41–68) years (Table 1). Based on the VUDS, patients with DV had a significantly lower CBC and Qmax and higher Pdet, PVR, and BOOIf than controls.
Table 1.
Clinical characteristics of patients with DV and controls.
| DV group (n = 43) |
Control group (n = 25) |
P value | |
|---|---|---|---|
| Age | 54.0 ± 14.1 | 60.5 ± 10.6 | 0.069 |
| IPSS-V | 9.1 ± 7.2 | 1.4 ± 1.6 | < 0.001 |
| IPSS-S | 6.0 ± 4.0 | 2.5 ± 2.0 | 0.001 |
| IPSS | 15.1 ± 9.9 | 3.9 ± 2.2 | < 0.001 |
| VUDS | |||
| FSF | 127.1 ± 54.4 | 164.6 ± 65.3 | 0.012 |
| Bladder compliance | 77.6 ± 84.1 | 158.1 ± 93.7 | < 0.001 |
| CBC | 290.3 ± 125.6 | 379.0 ± 179.0 | 0.004 |
| Pdet | 47.79 ± 42.74 | 14.62 ± 7.19 | 0.001 |
| Qmax | 10.66 ± 6.85 | 19.41 ± 8.64 | < 0.001 |
| cQmax | 0.63 ± 0.37 | 0.91 ± 0.39 | < 0.001 |
| Vol | 232.7 ± 114.2 | 406.3 ± 143.7 | < 0.001 |
| PVR | 57.7 ± 66.2 | 5.7 ± 12.4 | < 0.001 |
| VE | 0.79 ± 0.23 | 0.98 ± 0.05 | < 0.001 |
| BOOIf | 24.33 ± 47.82 | − 30.41 ± 18.16 | < 0.001 |
DV Dysfunctional voiding, IPSS International prostate symptom score, IPSS-S International prostate symptom score storage subscore, IPSS-V International prostate symptom score voiding subscore, VUDS Videourodynamic study, FSF First sensation of bladder filling, CBC Cystometric bladder capacity, Pdet Detrusor voiding pressure, Qmax Maximal urinary flow rate, cQmax Corrected maximal urinary flow rate, Vol Voided volume, PVR Post-void residual volume, VE Voiding efficacy, BOOIf Female bladder outlet obstruction index.
Table 2 shows the urine biomarker levels of patients with DV and controls. For each targeted analyte, the numbers of outliers in patients with DV and controls ranged from 0 to 2 and from 0 to 1, respectively, and all were < 5%. Patients with DV had higher urine 8-OHdG, IL-1β, IL-8, and BDNF levels than controls. Post-hoc power analysis reported 94.9, 89.3, 40.4, and 35.6% power (with alpha value of 0.05) in the evaluation of 8-OHdG, IL-1β, IL-8, and BDNF levels, respectively.
Table 2.
Urine biomarker levels of patients with DV and controls.
| Urine biomarkers@ | DV group (n = 43) |
Control group (n = 25) |
P value |
|---|---|---|---|
| 8-OHdG | 32.09 ± 19.72 (0) | 17.01 ± 14.59 (0) | 0.002 |
| 8-isoprostane | 12.94 ± 14.88 (1) | 15.32 ± 15.34 (1) | 0.098 |
| TAC | 607.28 ± 418.15 (2) | 1006.32 ± 984.39 (0) | 0.144 |
| IL-1β | 1.19 ± 1.43 (1) | 0.48 ± 0.20 (1) | < 0.001 |
| IL-2* | 0.26 ± 0.21 (0) | 0.73 ± 0.18 (0) | < 0.001 |
| IL-6 | 2.21 ± 5.28 (2) | 0.74 ± 0.35 (1) | 0.729 |
| IL-8 | 31.83 ± 65.21 (1) | 12.68 ± 25.3 (0) | 0.020 |
| TNFα* | 1.23 ± 0.33 (2) | 0.69 ± 0.19 (0) | < 0.001 |
| NGF* | 0.22 ± 0.05 (1) | 0.25 ± 0.06 (0) | 0.033 |
| BDNF | 0.64 ± 0.15 (0) | 0.58 ± 0.15 (0) | 0.030 |
DV Dysfunctional voiding, 8-OHdG 8-hydroxy-2-deoxyguanosine, TAC Total antioxidant capacity, TNFα Tumor necrosis factor alpha, NGF Nerve growth factor, BDNF Brain-derived neurotrophic factor.
(): number of outliers.
*: Mean values of the study group that were below the minimum detectable concentrations as per the assay manufacturer.
@: units: all pg/mL, except for ng/mL in 8-OHdG and mmol/μL in TAC.
Table 3 depicts the correlation coefficients between urine biomarker levels and the clinical characteristics of patients with DV. Urine 8-OHdG and IL-1β levels were positively correlated with the clinical symptom scores, and urine 8-isoprostane and TAC levels were negatively associated with GRA in patients with DV. There were also significant correlations between VUDS parameters and urine biomarker levels (including TAC and BDNF).
Table 3.
Correlation coefficient (r value) between urine biomarker levels and the clinical characteristics of patients with DV.
| Urine biomarkers* | |||||||
|---|---|---|---|---|---|---|---|
| 8-OHdG | 8-isoprostane | TAC | IL-1β | IL-6 | IL-8 | BDNF | |
| Clinical symptoms | |||||||
| IPSS-V | 0.455 | n.s | n.s | 0.522 | n.s | n.s | n.s |
| IPSS-S | 0.289 | n.s | n.s | n.s | n.s | n.s | n.s |
| IPSS | 0.438 | n.s | n.s | 0.438 | n.s | n.s | n.s |
| VUDS | |||||||
| FSF | n.s | n.s | n.s | n.s | n.s | n.s | n.s |
| Bladder compliance | n.s | n.s | n.s | n.s | n.s | n.s | − 0.261 |
| CBC | n.s | n.s | 0.275 | n.s | n.s | n.s | n.s |
| Pdet | n.s | n.s | n.s | n.s | n.s | n.s | n.s |
| Qmax | n.s | n.s | 0.272 | n.s | n.s | n.s | n.s |
| cQmax | n.s | n.s | n.s | n.s | n.s | n.s | n.s |
| Vol | n.s | n.s | 0.298 | n.s | n.s | n.s | n.s |
| PVR | n.s | n.s | n.s | n.s | n.s | n.s | n.s |
| VE | n.s | n.s | n.s | n.s | n.s | n.s | n.s |
| BOOIf | n.s | n.s | n.s | n.s | n.s | n.s | n.s |
| Treatment outcomes (n = 26) | |||||||
| GRA | n.s | − 0.440 | − 0.605 | n.s | n.s | n.s | n.s |
DV Dysfunctional voiding, 8-OHdG 8-hydroxy-2-deoxyguanosine, TAC Total antioxidant capacity, VEGF Vascular endothelial growth factor, NGF Nerve growth factor, BDNF Brain-derived neurotrophic factor, IPSS International prostate symptom score, IPSS-S International prostate symptom Score storage subscore, IPSS-V International prostate symptom score voiding subscore, VUDS Videourodynamic study, FSF First sensation of bladder filling, CBC Cystometric bladder capacity, Pdet Detrusor voiding pressure, Qmax Maximal urinary flow rate, cQmax Corrected maximal urinary flow rate, Vol Voided volume, PVR Post-void residual volume, VE Voiding efficacy, BOOIf Female bladder outlet obstruction index, GRA Global response assessment; n.s. Not significant.
*: Mean analyte volumes of the study group that were below the minimum detectable concentrations as per the assay manufacturer were excluded from further analysis.
In total, 26 patients with DV received further treatment, with a total of 12 biofeedback PFM exercises and 14 EUS BoNT-A injections. Three months after treatment, 15 (57.7%) patients with DV had a successful outcome (as evidenced by a GRA score of ≥ 2). Table 4 shows the pretreatment clinical characteristics and urine biomarker levels of patients with DV with different treatment outcomes (GRA score of ≥ and < 2), and there were no significant differences in terms of pretreatment clinical symptoms or VUDS parameters. However, patients with DV who presented with a GRA score of ≥ 2 had significantly lower pretreatment urine 8-isoprostane (6.94 ± 4.92 vs 16.80 ± 14.19 pg/mL, p = 0.019) and TAC (388.31 ± 151.73 vs 977.63 ± 549.86 mmol/μL, p = 0.014) levels than those with a GRA score of < 2 (Table 4, and Fig. 2). In addition, the biofeedback PFM exercise group had a higher rate of successful outcome than the EUS BoNT-A injection group.
Table 4.
Pretreatment clinical characteristics and urine biomarker levels of patients with DV who presented with different treatment outcomes.
| GRA score of ≥ 2 (n = 15) |
GRA score of < 2 (n = 11) |
P value | |
|---|---|---|---|
| Age | 48.4 ± 13.66 | 55.82 ± 12.38 | 0.212 |
| IPSS-V | 9.67 ± 7.10 | 11 ± 7.11 | 0.567 |
| IPSS-S | 6 ± 3.82 | 6 ± 4.43 | 0.875 |
| IPSS | 15.67 ± 10.2 | 17 ± 10.09 | 0.658 |
| VUDS | |||
| FSF | 124.7 ± 60.2 | 128.0 ± 40.8 | 0.603 |
| Bladder compliance | 52.4 ± 77.9 | 79.7 ± 68.5 | 0.102 |
| CBC | 256.2 ± 110.0 | 319.6 ± 121.2 | 0.126 |
| Pdet | 60.07 ± 63.73 | 50.55 ± 37.18 | 0.662 |
| Qmax | 8.00 ± 4.05 | 11.50 ± 10.24 | 0.481 |
| cQmax | 0.49 ± 0.22 | 0.65 ± 0.54 | 0.755 |
| Vol | 202.2 ± 95.5 | 239.8 ± 120.4 | 0.551 |
| PVR | 54.0 ± 42.4 | 79.8 ± 71.2 | 0.343 |
| VE | 0.76 ± 0.26 | 0.73 ± 0.25 | 0.621 |
| BOOIf | 42.47 ± 64.65 | 25.25 ± 49.58 | 0.500 |
| Urine biomarkers@ | |||
| 8-OHdG | 31.94 ± 19.39 (0) | 42.01 ± 19.35 (0) | 0.154 |
| 8-isoprostane | 6.94 ± 4.92 (1) | 16.80 ± 14.19 (0) | 0.019 |
| TAC | 388.31 ± 151.73 (1) | 977.63 ± 549.86 (0) | 0.014 |
| IL-1β | 0.86 ± 0.13 (1) | 0.85 ± 0.25 (0) | 0.365 |
| IL-2* | 0.15 ± 0.03 (1) | 0.20 ± 0.09 (0) | 0.111 |
| IL-6 | 4.06 ± 13.12 (1) | 3.93 ± 8.40 (0) | 0.511 |
| IL-8 | 17.78 ± 22.3 5(0) | 12.77 ± 16.05 (1) | 0.677 |
| TNFα* | 1.24 ± 0.19 (1) | 1.31 ± 0.15 (0) | 0.443 |
| NGF* | 0.20 ± 0.03 (0) | 0.22 ± 0.06 (1) | 0.502 |
| BDNF | 0.64 ± 0.10 (0) | 0.62 ± 0.08 (0) | 0.751 |
| Treatment | 0.014 | ||
| Biofeedback PFM exercise | 10 | 2 | |
| EUS BoNT-A injections | 5 | 9 | |
DV Dysfunctional voiding, GRA Global response assessment, IPSS International prostate symptom score, IPSS-S International prostate symptom Score storage subscore, IPSS-V International prostate symptom score voiding subscore, VUDS Videourodynamic study, FSF First sensation of bladder filling, CBC Cystometric bladder capacity, Pdet Detrusor voiding pressure, Qmax Maximal urinary flow rate, cQmax Corrected maximal urinary flow rate, Vol Voided volume, PVR Post-void residual volume, VE Voiding efficacy, BOOIf Female bladder outlet obstruction index, 8-OHdG 8-hydroxy-2-deoxyguanosine, TAC Total antioxidant capacity, TNF Alpha, tumor necrosis factor α, NGF Nerve growth factor, BDNF Brain-derived neurotrophic factor, PFM Pelvic floor muscle, EUS External urethral sphincter, BoNT-A Botulinum toxin A.
(): number of outliers.
*: Mean values of the study group that were below the minimum detectable concentrations as per the assay manufacturer.
@: units: all pg/mL, except for ng/mL in 8-OHdG and mmol/μL in TAC.
Figure 2.
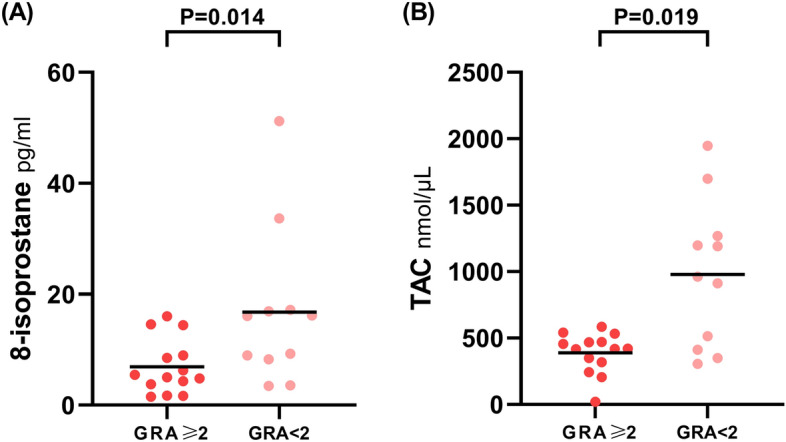
Difference in urine biomarker levels in patients with dysfunctional voiding who presented with different treatment outcomes. Patients with dysfunctional voiding who presented with a GRA score of ≥ 2 had significantly lower pretreatment urine 8-isoprostane (6.94 ± 4.92 vs 16.80 ± 14.19 pg/mL, p0.019) and TAC (388.31 ± 151.73 vs 977.63 ± 549.86 mmol/μL, p = 0.014) levels than those with a GRA score of < 2.
Univariate logistic regression analysis revealed that the pretreatment urine TAC levels (OR: 0.994) and the treatment strategies with biofeedback PFM exercise (OR: 9.000) were predictors of successful treatment outcomes (Table 5). Multivariate logistic regression analysis revealed that the pretreatment urine TAC level (OR: 0.995) was the only independent predictor of successful treatment.
Table 5.
Univariate and multivariate logistic regression analyses for predicting successful treatment outcomes in patients with DV.
| GRA score of ≥ 2 | ||||||
|---|---|---|---|---|---|---|
| Univariate analysis | Multivariate analysis | |||||
| OR | 95% CI | P value | OR | 95% CI | P value | |
| Urine biomarkers | ||||||
| 8-isoprostane | 0.853 | 0.726–1.003 | 0.054 | |||
| TAC | 0.994 | 0.989–1.000 | 0.033 | 0.995 | 0.990–1.000 | 0.049 |
| Treatment | ||||||
| Biofeedback PFM exercise (ref. EUS BoNT-A injection) | 9.000 | 1.386–58.443 | 0.021 | 7.742 | 0.691–86.731 | 0.097 |
DV Dysfunctional voiding, GRA Global response assessment, TAC Total antioxidant capacity, PFM Pelvic floor muscle, EUS External urethral sphincter, BoNT-A Botulinum toxin A.
Discussion
To the best of our knowledge, this study first investigated the value of urine oxidative stress biomarker and inflammatory marker levels among female patients with DV. These patients had distinct urine oxidative stress biomarker and inflammatory marker profiles compared with controls. Moreover, there were significant correlations between urine biomarker levels and clinical characteristics in this patient group, and the pretreatment urine TAC level was an independent factor for predicting successful treatment outcomes. Urine component analysis, which is a noninvasive approach, might provide important clinical information in the establishment of diagnosis, mapping of clinical characteristics, and prediction of prognosis in female patients with DV. These urine analytes might have diagnostic and prognostic values and could be biomarkers in female patients with DV.
One recent review summarized studies about the biomarkers of oxidative stress, which included 8-OHdG, F2-isoprostane, and TAC, in BOO. Results revealed the significant association between oxidative stress and BOO-related urinary dysfunctions10. Moreover, 8-OHdG is a stable end product of DNA oxidation 16. F2-isoprostane is a chemically stable compound and is formed by free radical-induced perioxidation of arachidonic acid17. TAC reflects the cumulative effect of all antioxidants from different endogenous antioxidative defense systems against harmful activities caused by oxidative stress18. Tissue hypoxia and hypoxia-induced inflammatory pathways play critical roles in disease progression and bladder remodeling in BOO 9,19. These oxidative stress biomarkers might be applied in DV, which is an important etiology of BOO.
In redox signaling and oxidative stress, reactive oxygen species affect the release of proinflammatory cytokines including IL-1β, TNFα, and interferon beta, thereby resulting in related immune responses and metabolism20. In a previous rabbit study, the 8-OHdG levels in the urine, plasma, and tissue increased, and the plasma TAC levels decreased under partial BOO21. In a rat study of chronic bladder ischemia induced by atherosclerosis, the study group had significantly higher urine 8-OHdG and proinflammatory cytokine (TNFα, IL-6, and IL-8) levels in the bladder tissue than controls22. In this study, patients with DV had significantly higher urine 8-OHdG, IL-1β, and IL-8 levels than controls. In addition, urine 8-OHdG and IL-1β levels were positively correlated with the symptom scores in patients with DV. Elevated urine 8-OHdG and IL-1β levels might reflect more oxidative stress and increasing hypoxia-related inflammation in the urinary bladder among patients with DV, which corresponds to clinical symptom severity. The noninvasive investigation of urine specimen might provide information about clinical symptoms and the pathology in the urinary bladder. Both urine 8-OHdG and IL-1β levels might have diagnostic values among female patients with DV. Our results were in accordance with the findings about the importance of elevated oxidative stress biomarker and proinflammatory cytokine levels in chronic bladder ischemia 22.
F2-isoprostatne is a reliable indicator of oxidative stress and can be detected in all tissues and fluids10,16. In a mouse bladder model of partial BOO, the assessment of F2-isoprostane in the bladder tissue reflects the progression of oxidative stress19. However, studies about the presence of isoprostane in the urine in lower urinary tract diseases are limited. Eight-isoprostane belongs to F2-isoprostane class. In this study, the urine 8-isoprostane levels did not significantly differ between patients with DV and controls. However, patients with DV who presented with successful treatment outcomes had significantly lower pretreatment urine 8-isoprostane levels, and the pretreatment urine 8-isoprostane level was found to be negatively correlated with GRA. Patients with DV who presented with lower urine 8-isoprostane levels might achieve better therapeutic effects. Although both 8-OHdG and 8-isoprostane are oxidative stress biomarkers, their respective levels in the urine might reflect unique underlying metabolic processes and clinical values. In patients with DV, urine 8-OHdG and 8-isoprostane levels could possibly have diagnostic and prognostic values, respectively.
TAC is an available biomarker for assessing the antioxidant potential of body fluids including urine23,24. Urine TAC levels might be affected by infection, renal status, systemic diseases, nutrition and supplemental intervention, and lifestyle factors24. The interplay between oxidative stress and antioxidative stress is dynamic and complex20. Therefore, the association between the expressions of oxidative stress biomarker (e.g., 8-OHdG and 8-isoprostane) and TAC in the urine cannot be definitely reversed, as shown in the current study. Different stages of pathological conditions can possibly have distinct oxidative stress and antioxidative stress profiles. In this study, the urine TAC levels of patients with DV was non-significantly lower than that of controls, and a low urine TAC level is an independent predictor of successful outcome, thereby indicating its prognostic value. Currently, the treatment outcomes of patients with DV varied without convincing predictors7,8, and the influencing factors might be complex and multifactorial. The urine oxidative stress and antioxidative stress biomarker profiles might be the summarized index reflecting the overall current status of lower urinary tract functions in individuals.
The current study had several limitations. First, it included women. Hence, sex bias might have existed. Second, although the design of the current study was similar to that of previous ones14,15, all controls presented with SUI. Third, even though oxidative stress biomarkers are more stable compounds than inflammatory cytokines, both might have intra-individual variations. Fourth, the overall hypoxia and oxidative stress status of the bladder was not completely attributed to DV. Both systemic inflammatory diseases and comorbidities and local bladder insults might affect the expressions of these urine substances. Finally, we excluded extreme values from analysis, as in previous studies14,15. However, the percentage of outliers was low.
Conclusion
Compared with controls, female patients with DV had distinct urine oxidative stress biomarker and inflammatory marker profiles. They had elevated urine 8-OHdG and IL-1β levels, which were also positively correlated with clinical symptoms. The pretreatment urine TAC level was an independent predictor of successful treatment outcomes. These urine analytes might have diagnostic and prognostic values and could be used as biomarkers of DV among women.
Author contributions
Y.-H.J. collected and analyzed data and wrote the manuscript. J.-F.J. analyzed the data and provided critical revision of the manuscript. H.-C.H., and Y.-H.H. performed the laboratory procedures and performed the statistical analysis. H. –C.K. conceived and designed the study and critically revised the manuscript.
Funding
This study was funded by the Tzu Chi Medical Foundation (Grant Number: TCMMP109-02-01 and TCMMP 109-02-02)
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Haylen BT, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol. Urodyn. 2010;29:4–20. doi: 10.1002/nau.20798. [DOI] [PubMed] [Google Scholar]
- 2.Allen TD. The non-neurogenic neurogenic bladder. J. Urol. 1977;117:232–238. doi: 10.1016/s0022-5347(17)58412-8. [DOI] [PubMed] [Google Scholar]
- 3.Hsiao SM, Lin HH, Kuo HC. Videourodynamic studies of women with voiding dysfunction. Sci. Rep. 2017;7:6845. doi: 10.1038/s41598-017-07163-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peng CH, Chen SF, Kuo HC. Videourodynamic analysis of the urethral sphincter overactivity and the poor relaxing pelvic floor muscles in women with voiding dysfunction. Neurourol. Urodyn. 2017;36:2169–2175. doi: 10.1002/nau.23263. [DOI] [PubMed] [Google Scholar]
- 5.Carlson KV, Rome S, Nitti VW. Dysfunctional voiding in women. J. Urol. 2001;165:143–147. doi: 10.1097/00005392-200101000-00035. [DOI] [PubMed] [Google Scholar]
- 6.Minardi D, et al. The role of uroflowmetry biofeedback and biofeedback training of the pelvic floor muscles in the treatment of recurrent urinary tract infections in women with dysfunctional voiding: A randomized controlled prospective study. Urology. 2010;75:1299–1304. doi: 10.1016/j.urology.2009.11.019. [DOI] [PubMed] [Google Scholar]
- 7.Chiang CH, Jiang YH, Kuo HC. Therapeutic efficacy of biofeedback pelvic floor muscle exercise in women with dysfunctional voiding. Sci. Rep. 2021;11:13757. doi: 10.1038/s41598-021-93283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ou YC, et al. Therapeutic efficacy of urethral sphincteric botulinum toxin injections for female sphincter dysfunctions and a search for predictive factors. Toxins (Basel) 2021 doi: 10.3390/toxins13060398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fusco F, et al. Progressive bladder remodeling due to bladder outlet obstruction: A systematic review of morphological and molecular evidences in humans. BMC Urol. 2018;18:15. doi: 10.1186/s12894-018-0329-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miyata Y, et al. A review of oxidative stress and urinary dysfunction caused by bladder outlet obstruction and treatments using antioxidants. Antioxidants (Basel) 2019 doi: 10.3390/antiox8050132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harpole M, Davis J, Espina V. Current state of the art for enhancing urine biomarker discovery. Expert Rev. Proteom. 2016;13:609–626. doi: 10.1080/14789450.2016.1190651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siddiqui NY, et al. Biomarkers implicated in lower urinary tract symptoms: systematic review and pathway analyses. J. Urol. 2019;202:880–889. doi: 10.1097/JU.0000000000000257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Solomon E, et al. Developing and validating a new nomogram for diagnosing bladder outlet obstruction in women. Neurourol. Urodyn. 2018;37:368–378. doi: 10.1002/nau.23307. [DOI] [PubMed] [Google Scholar]
- 14.Jiang YH, et al. Urine cytokines as biomarkers for diagnosing interstitial cystitis/bladder pain syndrome and mapping its clinical characteristics. Am. J. Physiol. Renal Physiol. 2020;318:F1391–F1399. doi: 10.1152/ajprenal.00051.2020. [DOI] [PubMed] [Google Scholar]
- 15.Jiang YH, et al. Urine biomarkers in ESSIC type 2 interstitial cystitis/bladder pain syndrome and overactive bladder with developing a novel diagnostic algorithm. Sci. Rep. 2021;11:914. doi: 10.1038/s41598-020-80131-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Il'yasova D, Scarbrough P, Spasojevic I. Urinary biomarkers of oxidative status. Clin. Chim. Acta. 2012;413:1446–1453. doi: 10.1016/j.cca.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roberts LJ, Morrow JD. Measurement of F(2)-isoprostanes as an index of oxidative stress in vivo. Free Radic. Biol. Med. 2000;28:505–513. doi: 10.1016/s0891-5849(99)00264-6. [DOI] [PubMed] [Google Scholar]
- 18.Fraga CG, Oteiza PI, Galleano M. In vitro measurements and interpretation of total antioxidant capacity. Biochim. Biophys. Acta. 1840;1840:931–934. doi: 10.1016/j.bbagen.2013.06.030. [DOI] [PubMed] [Google Scholar]
- 19.Iguchi N, Hou A, Koul HK, Wilcox DT. Partial bladder outlet obstruction in mice may cause E-cadherin repression through hypoxia induced pathway. J. Urol. 2014;192:964–972. doi: 10.1016/j.juro.2014.03.037. [DOI] [PubMed] [Google Scholar]
- 20.Schieber M, Chandel NS. ROS function in redox signaling and oxidative stress. Curr. Biol. 2014;24:R453–R462. doi: 10.1016/j.cub.2014.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin WY, et al. Reversing bladder outlet obstruction attenuates systemic and tissue oxidative stress. BJU Int. 2012;110:1208–1213. doi: 10.1111/j.1464-410X.2012.11185.x. [DOI] [PubMed] [Google Scholar]
- 22.Nomiya M, et al. Increased bladder activity is associated with elevated oxidative stress markers and proinflammatory cytokines in a rat model of atherosclerosis-induced chronic bladder ischemia. Neurourol. Urodyn. 2012;31:185–189. doi: 10.1002/nau.21191. [DOI] [PubMed] [Google Scholar]
- 23.Niki E. Assessment of antioxidant capacity in vitro and in vivo. Free Radic. Biol. Med. 2010;49:503–515. doi: 10.1016/j.freeradbiomed.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 24.Peluso I, Raguzzini A. Salivary and urinary total antioxidant capacity as biomarkers of oxidative stress in humans. Patholog. Res. Int. 2016;2016:5480267. doi: 10.1155/2016/5480267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.