Abstract
The Latinx community in the U.S. continues to be disproportionately burdened by the HIV epidemic, especially among Latinx sexual minority men (LSMM). Research indicates that up to two-thirds of new HIV infections occur among men who have sex with men (MSM) within primary partnerships. One promising biomedical approach for HIV prevention includes community scale-up of pre-exposure prophylaxis (PrEP) among LSMM. We examine the relationship between community connectedness (with the Latinx and gay communities) and PrEP uptake among 307 partnered LSMM who reported casual partner sex (i.e., non-monogamous relationships). Within the sample, approximately thirty percent (29.7%) of participants were on PrEP, and nearly forty-four percent (43.3%) reported partner approval for PrEP, while only 7.2% were opposed to PrEP. Insurance status and income levels were significantly associated with PrEP uptake. There was a significant interaction between gay community connectedness and Latinx community connectedness, which was positively associated with PrEP uptake (OR = 2.18; p = .007). Findings suggest that there may be structural barriers preventing this population from seeking and initiating PrEP care. Results point to the utility of integrating content related to intersecting identities and their corresponding communities when conceptualizing community-based and culturally informed interventions to improve the PrEP care cascade among LSMM.
Keywords: Latinx, sexual minority men, pre-exposure prophylaxis, PrEP, community-based intervention
INTRODUCTION
The Latinx community in the U.S. continues to be disproportionately burdened by the HIV epidemic. Approximately 27% of new HIV diagnoses in the U.S. and dependent areas were among Hispanic or Latinx people, and Latinx sexual minority men (LSMM) were among the most affected minoritized populations [1]. Previous HIV prevention research and interventions among gay, bisexual, and other men who have sex with men (MSM) have predominately focused on risk behaviors during casual sexual partnerships.
Earlier research indicated that 35–68% of new HIV infections among sexual minority men (SMM) were transmitted between main partners [2–4]. Estimated rates were as high as 79% among younger SMM (aged 18–29) [4]. More recent research has indicated that the likelihood of having condomless sex with casual partners is comparable for single SMM and those in non-monogamous sexual agreements [5,6]. Moreover, some evidence suggests that SMM in monogamous relationships who break their agreement and engage in CAS with casual partners may actually do so more frequently than non-monogamous and single men [6].
One promising biomedical approach includes a community scale-up of pre-exposure prophylaxis (PrEP); however, PrEP uptake among LSMM populations remains low. Consequently, there is an urgent need to promote HIV prevention interventions such as PrEP among LSMM who are in primary relationships, especially among serodiscordant male couples as research has shown favorable support for dyad-level interventions among SMM [7]. In particular, a study conducted with 409 partnered HIV-negative seroconcordant men found that partner PrEP use influenced personal PrEP use [8]. However, given that the sample was majority white (73.8%) more research specifically focusing on the experiences of men of color, particularly LSMM, is needed.
Generally, community-based HIV-prevention interventions have been effective in reaching the broader sexual and gender minority (SGM) community, especially when services are delivered by peers [9]. Although there are disproportionately fewer of these interventions designed specifically for LSMM, the ones that have documented success include participatory elements and incorporate attention to population-specific social and structural determinants of HIV infection risk among LSMM [10,11]. For example, researchers have noted the importance of including faith leaders in prevention efforts for the broader Latinx community; yet, for some LSMM, many places of worship have been sources of stigma and anti-LGBTQ+ sentiments [12,13]. In contrast, other interventions have utilized the multiple identities of LSMM to guide the development of innovative prevention methods. For instance, one RCT of a couple-based HIV intervention for Latinx MSM attributed its success to its community-led and intersectional design. Researchers drew upon the knowledge of a local community advisory board whilst leveraging the lived experiences and expertise of peers who delivered services in both Spanish and English [14]. Additionally, structural factors may also affect accessibility and willingness to participate in interventions. Namely, PrEP costs for uninsured LSMM can be prohibitive, and mistrust of government and healthcare providers as a result of medical malpractice within Latinx immigrant communities also pose significant barriers [15,16].
Research on intersectional and community-based approaches offers promising results that shift the responsibility and burden away from LSMM. These interventions frame the problem of low PrEP uptake in terms of a failure in provider outreach and public policy rather than the result of low motivation or a lack of willingness inherent or inured in LSMM. Further, interventions built in the community and by the community may increase access for LSMM and in turn, may also encourage participation as research suggests a linkage between community connectedness and healthcare utilization [17,18]. Given the intersectional nature of LSMM identities, LSMM multiply belong to several communities as racially and ethnically minoritized individuals, sexual minorities, and immigrant/diasporic members. As such, LSMM may have access to benefits that are unique to each community. Conversely, LSMM may also be discouraged from accessing said benefits, particularly given that the white “mainstream” LGBTQ+ community has been described as exclusionary towards people of color [19].
Community-based interventions for HIV prevention have been promising and widely accepted among the larger SGM community, particularly PrEP [20]. Nevertheless, this success must be reconciled with the fact that many of these interventions are designed without considering the unique experiences of LSMM, as most intervention and outreach efforts have centered on the needs of white gay cismen [21,22]. Therefore, the current research seeks to examine the intersection of Latinx group and gay community connectedness and its association to PrEP uptake.
MATERIALS AND METHODS
Recruitment and Study Procedure
Recruitment and data collection occurred from November 2018 to May 2019 using an index approach. Eligible LSMM respondents were invited to complete an online survey. To qualify for the study; participants were required to (1) aged 18 and above; (2) self-identified as cis male; (3) identified as Hispanic or Latinx; (4) reside in the U.S. (including Puerto Rico); (5) in an ongoing relationship with a main partner who was 18 years and older and identified as cis male; (6) able to read Spanish or English. To approximate the behavioral criteria for CDC’s recommendation on PrEP eligibility, for this analysis, we only used data from participants who self-reported HIV-negative/unknown status and report casual partner sex (e.g., non-monogamous relationship). All participants provided informed consent and received a $10 Amazon gift card. Study procedures were reviewed and approved by the Institutional Review Board of Hunter College of the City University of New York.
Measures
Sociodemographic characteristics.
Participants reported their age, sexual orientation identity, income, health insurance status, and relationship length. They also provided immigration-related information and reported whether they were U.S.-born. Language preference was inferred from the language of survey completion (English vs. Spanish). Age was dichotomized to reflect participants greater or equal to 31 and those less than or equal to 30. relationship length was also dichotomized to reflect participants in relationship lengths greater than 3 years and those less than or equal to 3 years.
PrEP uptake and partner PrEP approval.
Participants indicated whether or not they were currently prescribed PrEP for HIV prevention. Separately, they indicated their partner’s approval of PrEP using the following nominal response options: “Which best describes how your partner feels about PrEP?” Response options include (1) He is in favor of PrEP; (2) He is opposed to PrEP; (3) He does not have strong opinions about PrEP either way; (4) He does not really know what PrEP is; (5) I do not have any idea how my partner feels about PrEP. We further coded the answers into a new three-category variable: (1) yes, he is in favor of PrEP; (2) no, he is opposed to PrEP; (3) I don’t know or he doesn’t know.
Condomless anal sex (CAS).
Participants reported the number of times they had anal sex without using a condom with their main partner and casual partner in the past 30 days.
Gay community connectedness (GCC).
Participants were asked how they feel about being a part of the gay community using the Gay Community Attachment Scale [23]. All items were scored on a 4-point scale ranging from 1 (strongly disagree) to 4 (strongly agree). We calculated the mean score to present the degree of gay community connectedness (GCC). The internal consistency in the current study was good (α = 0.86).
Latinx group membership.
Latinx group membership (LGM) was assessed using the 12-item Group Membership Questionnaire [24], which includes statements such as “Overall, my ethnic group is viewed positively by others.” All items were indicated on a 7-point Likert scale ranging from 1 (strongly disagrees) to 7 (strongly agree). A mean score was computed as the mean of response items after reverse-scoring negatively keyed items. The internal consistency in the current study was good (α = 0.79).
Data analysis
Overall sample statistics were reported using frequency measures including mean, standard deviation (SD), and interquartile ranges for the condomless anal sex variables. Bivariate analyses were performed using logistic regression to examine the association between PrEP uptake, GCC LGM, demographic variables, and other variables of interest. Next, we used multivariable logistic regression to examine if LGM, GCC, and the interaction (LGM*GCC) are associated with PrEP uptake while adjusting for demographic variables and variables of interest. Results were reported as odds ratio (OR) for the bivariate model and adjusted odds ratio (AOR) for the multivariable model with corresponding 95% confidence intervals (CI). Associations with p-values less than 0.05 were considered statistically significant. Data were analyzed using IBM SPSS.
RESULTS
Participants Characteristics
The study recruited 625 index participants. A sample of 307 LSMM was included in the analysis. Nearly half of the sample was 31 years or older (49.5%). A majority (88.9%) of participants identified as gay. Nearly half (46.6%) of the participants had been in an ongoing relationship for more than three years by the time the study was conducted. Over half (54.4%) of the participants were born in the USA, and 41.0% had an annual income higher than $30,000. Almost three-fifths (59.3%) of the participants had health insurance. Notably, over eighty percent (80.8%) of the LSMM indicated English language preference. See Table 1 for sample characteristics.
Table 1.
Bivariable and multivariable analyses on factors associated with PrEP uptake among LSMM, 2018–2019.
| Overall N = 307 | Bivariate | Multivariable | |||||
|---|---|---|---|---|---|---|---|
| n (%) | OR | 95% CI | p | AOR | 95% CI | p | |
| Age (≥31) | 152 (49.5) | 0.89 | 0.54, 1.44 | 0.627 | 0.73 | (0.38, 1.37) | 0.322 |
| Sexual Identity (Ref: Queer) | 10 (3.3) | ||||||
| Gay | 273 (88.9) | 0.41 | 0.11, 1.47 | 0.173 | 0.73 | (0.16, 3.27) | 0.677 |
| Bisexual | 24 (7.8) | 0.33 | 0.71, 1.56 | 0.164 | 0.58 | (0.09, 3.65) | 0.564 |
| Relationship Length (>3 Years) | 143 (46.6) | 1.33 | 0.82, 2.18 | 0.248 | 0.72 | (0.37, 1.39) | 0.331 |
| U.S. Born (Yes) | 167 (54.4) | 0.91 | 0.56, 1.49 | 0.706 | 0.88 | (0.47, 1.62) | 0.680 |
| Language Preference (English) | 248 (80.8) | 1.29 | 0.68, 2.47 | 0.431 | 0.90 | (0.41, 1.98) | 0.801 |
| Income (>30K) | 126 (41.0) | 2.73 | 1.65, 4.52 | <0.001 | 1.45 | (0.76, 2.76) | 0.252 |
| Health Insurance (Yes) | 182 (59.3) | 6.46 | 3.39, 12.31 | <0.001 | 4.76 | (2.18, 10.39) | <0.001 |
| Partner PrEP Approval (Ref: Yes, he is in favor) | 133 (43.3) | ||||||
| No, he is opposed | 22 (7.2) | 0.26 | 0.08, 0.82 | 0.021 | 0.31 | (0.86, 1.15) | 0.081 |
| I don’t know | 152 (49.5) | 0.24 | 0.14, 0.42 | <0.001 | 0.27 | (0.14, 0.50) | <0.001 |
| Casual Partner CAS (M, IQR) | 2.15, 11.18 | 1.00 | 0.98, 1.02 | 0.995 | 1.02 | (0.99, 1.05) | 0.111 |
| Main Partner CAS (M, IQR) | 3.31, 12.32 | 0.91 | 0.81, 1.01 | 0.086 | 0.94 | (0.67, 1.50) | 0.278 |
| Latinx Group Membership (LGM) (M, SD) | 4.41, 0.76 | 1.56 | 1.13, 2.16 | 0.007 | 1.00 | (0.85, 1.05) | 0.986 |
| Gay Community Connectedness (GCC) (M, SD) | 2.92 (0.70) | 2.37 | 1.59, 3.52 | <0.001 | 2.12 | (1.32, 3.39) | 0.002 |
| Interaction Term (LGM*GCC) | - | - | - | - | 2.18 | (1.23, 3.84) | 0.007 |
Sample Characteristics
In total, 91 participants (29.6%) were currently prescribed PrEP. Nearly forty-four percent (43.3%) had partner approval for PrEP, and 7.2% were opposed to PrEP. Participants reported on average 3.31 (IQR=12.32) and 2.15 (IQR=11.18) instances of condomless anal sex with their main partner and casual partner in the past 30 days, respectively. The mean scores of overall gay community connectedness and Latinx group members were 2.92 (SD=0.7) out of a possible range of 4 and 4.41 (SD=0.76) out of a possible range of 7, respectively. See Table 1.
Bivariate and Multivariable Associations
In the bivariate analysis (See Table 1), income level (OR=2.73, p<0.001) and health insurance (OR=6.46, p<0.001) were also significantly associated with PrEP uptake. Additionally, participants who indicated partner PrEP disapproval (OR=0.26, p=0.021) and those who did not know (OR=0.24 p<0.001) were less likely to be taking PrEP compared to those who had partner approval. Both, at average levels of GCC and LGM were positively associated with PrEP uptake (OR=2.37, p<0.001 and OR=1.56, p<0.001) in bivariate analyses.
There was a significant interaction between LGM and GCC in the prediction of PrEP uptake (AOR = 2.18, p = 0.007). At average levels of LGM, GCC was positively associated with PrEP uptake (AOR = 2.12, p = .002); meanwhile, at average levels of GCC the association between LGM and PrEP uptake was non-significant. The association between GCC and PrEP uptake increased in magnitude as LGM increased. Similarly, the association between LGM and PrEP uptake was amplified as GCC increased (Figure 1).
Figure 1:
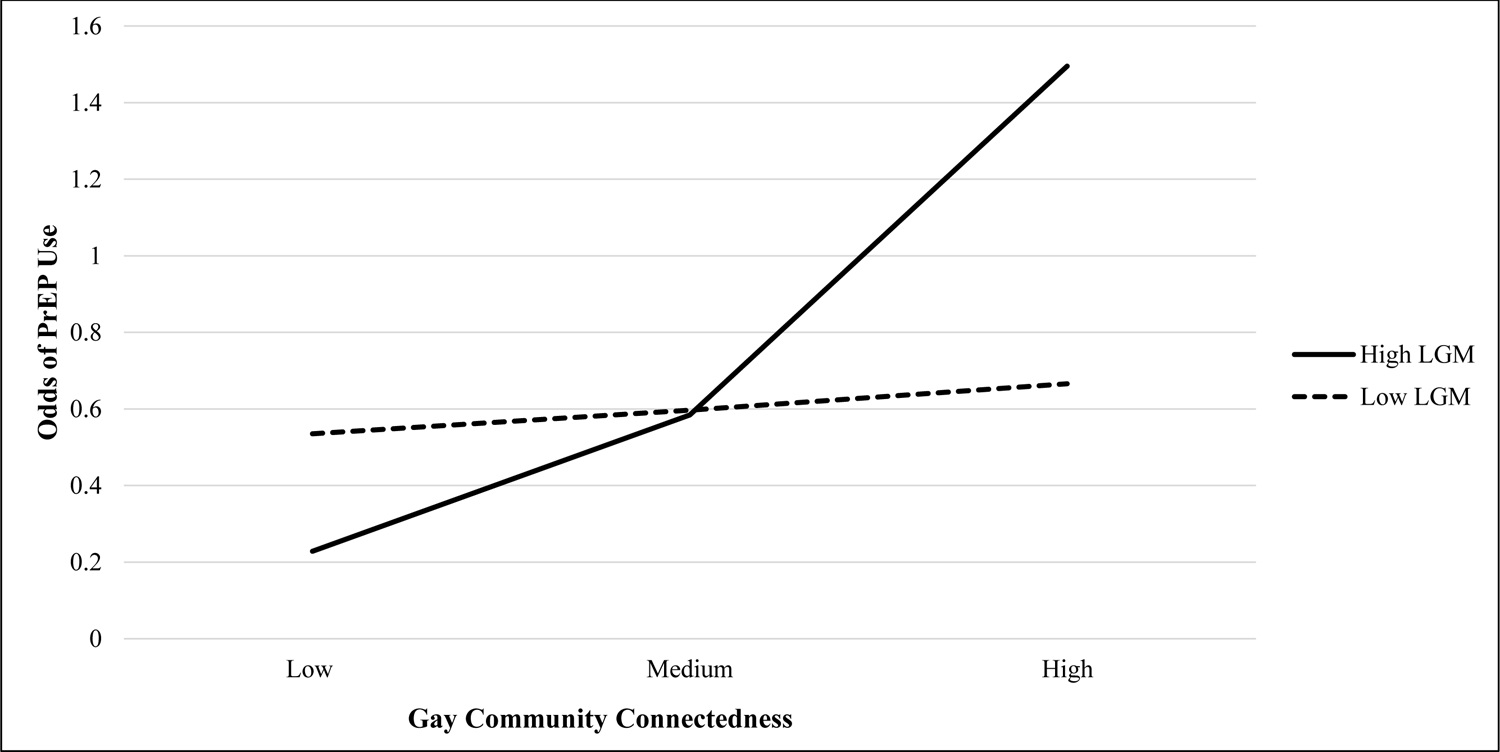
At high levels of GCC and LGM, the odds of PrEP use increased
DISCUSSION
These findings point to the importance of applying an intersectional lens to understanding the association between community connection and PrEP uptake among LSMM. Connection to ethnic and sexual identity communities interacted with one another such that higher levels of connectedness to one of these types of community amplified associations between connectedness to the other type of community and PrEP uptake. Specifically, GCC was positively associated with uptake at average to high levels of LGM, and at the same time, LGM was positively associated with PrEP uptake at high levels of GCC.
Community plays a vital role as the context in which SGM individuals connect with their health and social networks. Previous studies indicate that attachment to the LGBT + community is associated with lower minority stress among gay and bisexual men [25]. Our findings suggest that PrEP uptake is determined in many respects by synergistic connections to multiple communities, demonstrating the importance of community-based interventions and community engagement on HIV prevention behaviors and outcomes. More importantly, the interaction of GCC and the LGM was found to be strongly associated with PrEP uptake when controlling for other study covariates. These findings are consistent with prior research suggesting that culturally informed interventions effectively increase PrEP engagement for LSMM [26].
We also anticipate that the integration of Latinx relevant content into community-based interventions that are traditionally centered on the experiences of white queer men can potentially promote PrEP uptake and contribute to increasing the engagement along the PrEP cascade among LSMM (i.e., making existing queer interventions more Latinx-relevant). Conversely, the integration of queer-relevant content into Latinx programming may be a novel approach needing further consideration and research (i.e., making existing Latinx-focused interventions more queer-relevant). Yet, another approach is to develop interventions with the intersecting identities are centered from conceptualization. There is a growing body of literature and evidence-based resources demonstrating the efficacy of integrating sociocultural-specific content and values in community-based programs in HIV prevention. For instance, the HOLA en Grupos, a locally developed community-based behavioral HIV/STD prevention intervention executively for Spanish-speaking Hispanic/Latinx MSM implemented in North Carolina [27], was found to be efficacious for increasing consistent condom use and HIV testing among Hispanic/Latinx MSM and their partners [28]. These interventions reinforced the value of the local Latinx culture and incorporate local data on risks and were highly appreciated by the study participants [28]. Researchers should consider designing and developing interventions that meet the community’s expressed needs while presenting such interventions in ways that are engaging. Such considerations may enhance the interventions based on individual needs and priorities.
Lastly, we found that only about 30% of the LSMM in our sample were currently using PrEP, which supports prior research demonstrating that current HIV prevention efforts do not adequately reach LSMM resulting in lower utilization of this biomedical HIV prevention intervention relative to other SMM populations [1]. The rate of PrEP uptake is especially concerning given that LSMM are still disproportionately affected by HIV infections. There is a pressing need for increased efforts to promote PrEP accessibility for LSMM. Unsurprisingly, income and insurance were found to be significantly associated with PrEP uptake, indicating that LSMM face significant financial barriers when seeking PrEP care, such as cost and lack of insurance. Prior research has identified multiple multilevel barriers and obstacles to PrEP uptake among racialized and minoritized ethnic communities, such as racism, homophobia, concerns about side effects, low awareness of PrEP, and perceived risk of HIV infection [29]. Taken together, these findings highlighted not only the complex issues that contribute to the disparities in HIV among racial and SGM, including the intersecting factors that influence health behaviors and outcomes, but also the urgent need to address the disparities in social determinants in HIV prevention interventions, such as by expanding medication assistance programs and health care coverage.
Our study findings should be interpreted in light of some limitations. First, the nature of the cross-sectional survey limited our ability to draw causal inferences from the analyses. The self-reported data we used are subject to recall and social desirability biases, although social desirability bias is reduced when surveys are self-administered. Partnered LSMM participants were recruited online through gay geo-social networking app and social media. Therefore, the generalizability of our findings to LSMM who do not use these platforms or who do not have a main partner is uncertain. In addition, while all participants were in non-monogamous relationships, we did not necessarily conduct a comprehensive assessment of PrEP eligibility such as being diagnosed with a sexually transmitted infection in the past 6 months, injection drug use, partner living with HIV, among others. Further longitudinal research is needed to understand the relationship between community connectedness and PrEP implementation and to examine the factors associated with PrEP persistence among LSMM over time.
CONCLUSION
Despite the limitations, our study suggested that PrEP uptake among LSMM remains low, and there may be structural barriers preventing this population from seeking and initiating PrEP care. Culturally relevant interventions may not only extend to the inclusion of Latinx culture, but also the integration of queer-related content. The findings offer important insight into how community-based and culturally informed interventions can improve the PrEP care cascade among LSMM and indicate future research pathways to examine the efficacy of such intervention to improve PrEP care LSMM.
Acknowledgements:
This work was supported by Research Supplements to Promote Diversity in Health-Related Research through the U.S. National Institute on Drug Abuse under Grant R01DA045613-01S1.
Footnotes
Employment
All authors certify that no recent (while engaged in the research project), present or anticipated employment by any organizations or affiliations will gain or lose financially through publication of this manuscript. This includes multiple affiliations.
Financial interests/Non-financial interests
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethics approval
All participants provided informed consent. Study procedures were reviewed and approved by the Institutional Review Board of Hunter College of the City University of New York.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
As part of the informed consent procedures, participants were notified that their data would be used for scientific publication. No pictures or videos were part of the data collection process.
Code availability
The data analyzed in this manuscript were analyzed by using IBM SPSS. Code for data cleaning and analyses is available upon request.
Availability of data and material
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is only available upon request.
References
- 1.Latinos | Race/Ethnicity | HIV by Group | HIV/AIDS | CDC. Published March 18, 2021. Accessed May 24, 2021. https://www.cdc.gov/hiv/group/racialethnic/hispaniclatinos/index.html
- 2.Goodreau SM, Carnegie NB, Vittinghoff E, et al. What Drives the US and Peruvian HIV Epidemics in Men Who Have Sex with Men (MSM)? Sullivan PS, ed. PLoS ONE. 2012;7(11):e50522. doi: 10.1371/journal.pone.0050522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goodreau SM, Carnegie NB, Vittinghoff E, et al. Correction: What Drives the US and Peruvian HIV Epidemics in Men Who Have Sex with Men (MSM)? PLoS ONE. 2013;8(7). doi: 10.1371/annotation/9a6a0c8e-2d01-4f36-9ab8-f9fdfce6497b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. AIDS. 2009;23(9):1153–1162. doi: 10.1097/QAD.0b013e32832baa34 [DOI] [PubMed] [Google Scholar]
- 5.Starks TJ, Robles G, Bosco SC, Dellucci TV, Grov C, Parsons JT. The Prevalence and Correlates of Sexual Arrangements in a National Cohort of HIV-Negative Gay and Bisexual Men in the United States. Arch Sex Behav. 2019;48(1):369–382. doi: 10.1007/s10508-018-1282-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Starks TJ, Jones SS, Kyre K, et al. Testing the drug use and condomless anal sex link among sexual minority men: The predictive utility of marijuana and interactions with relationship status. Drug Alcohol Depend. 2020;216:108318. doi: 10.1016/j.drugalcdep.2020.108318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagenaar BH, Christiansen-Lindquist L, Khosropour C, et al. Willingness of US Men Who Have Sex with Men (MSM) to Participate in Couples HIV Voluntary Counseling and Testing (CVCT). Niccolai LM, ed. PLoS ONE. 2012;7(8):e42953. doi: 10.1371/journal.pone.0042953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.John SA, Starks TJ, Rendina HJ, Grov C, Parsons JT. Should I Convince My Partner to Go on Pre-Exposure Prophylaxis (PrEP)? The Role of Personal and Relationship Factors on PrEP-Related Social Control among Gay and Bisexual Men. AIDS Behav. 2018;22(4):1239–1252. doi: 10.1007/s10461-017-1835-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hart TA, Noor SW, Skakoon-Sparling S, et al. GPS: A Randomized Controlled Trial of Sexual Health Counseling for Gay and Bisexual Men Living With HIV. Behav Ther. 2021;52(1):1–14. doi: 10.1016/j.beth.2020.04.005 [DOI] [PubMed] [Google Scholar]
- 10.Rhodes SD, Alonzo J, Mann-Jackson L, et al. A peer navigation intervention to prevent HIV among mixed immigrant status Latinx GBMSM and transgender women in the United States: outcomes, perspectives and implications for PrEP uptake. Health Educ Res. 2020;35(3):165–178. doi: 10.1093/her/cyaa010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sutton MY, Martinez O, Brawner BM, et al. Vital Voices: HIV Prevention and Care Interventions Developed for Disproportionately Affected Communities by Historically Underrepresented, Early-Career Scientists. J Racial Ethn Health Disparities. Published online October 30, 2020. doi: 10.1007/s40615-020-00908-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sutton MY, Parks CP. HIV/AIDS Prevention, Faith, and Spirituality among Black/African American and Latino Communities in the United States: Strengthening Scientific Faith-Based Efforts to Shift the Course of the Epidemic and Reduce HIV-Related Health Disparities. J Relig Health. 2013;52(2):514–530. doi: 10.1007/s10943-011-9499-z [DOI] [PubMed] [Google Scholar]
- 13.Brooks RA, Etzel MA, Hinojos E, Henry CL, Perez M. Preventing HIV Among Latino and African American Gay and Bisexual Men in a Context of HIV-Related Stigma, Discrimination, and Homophobia: Perspectives of Providers. AIDS Patient Care STDs. 2005;19(11):737–744. doi: 10.1089/apc.2005.19.737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martinez O, Isabel Fernandez M, Wu E, et al. A couple-based HIV prevention intervention for Latino men who have sex with men: study protocol for a randomized controlled trial. Trials. 2018;19(1):218. doi: 10.1186/s13063-018-2582-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suzanne P Fiorillo G JK. Attitudes and Barriers towards Pre-Exposure Prophylaxis (Prep) among High-Risk HIV-Seronegative Men who have Sex with Men. J AIDS Clin Res. 2014;05(08). doi: 10.4172/2155-6113.1000335 [DOI] [Google Scholar]
- 16.Lawrence M. Reproductive Rights and State Institutions: The Forced Sterilization of Minority Women in the United States. :52. [Google Scholar]
- 17.Anderson-Carpenter KD, Sauter HM, Luiggi-Hernández JG, Haight PE. Associations between Perceived Homophobia, Community Connectedness, and Having a Primary Care Provider among Gay and Bisexual Men. Sex Res Soc Policy. 2019;16(3):309–316. doi: 10.1007/s13178-018-0347-8 [DOI] [Google Scholar]
- 18.Kaniuka A, Pugh KC, Jordan M, et al. Stigma and suicide risk among the LGBTQ population: Are anxiety and depression to blame and can connectedness to the LGBTQ community help? J Gay Lesbian Ment Health. 2019;23(2):205–220. doi: 10.1080/19359705.2018.1560385 [DOI] [Google Scholar]
- 19.Han C. They Don’t Want To Cruise Your Type: Gay Men of Color and the Racial Politics of Exclusion. Soc Identities. 2007;13(1):51–67. doi: 10.1080/13504630601163379 [DOI] [Google Scholar]
- 20.Patel VV, Ginsburg Z, Golub SA, et al. Empowering With PrEP (E-PrEP), a Peer-Led Social Media–Based Intervention to Facilitate HIV Preexposure Prophylaxis Adoption Among Young Black and Latinx Gay and Bisexual Men: Protocol for a Cluster Randomized Controlled Trial. JMIR Res Protoc. 2018;7(8):e11375. doi: 10.2196/11375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Truman BI, Moonesinghe R, Brown YT, Chang M-H, Mermin JH, Dean HD. Differential Association of HIV Funding With HIV Mortality by Race/Ethnicity, United States, 1999–2017. Public Health Rep. 2020;135(1_suppl):149S–157S. doi: 10.1177/0033354920912716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.M DG Jr. Poor Black and Hispanic Men Are the Face of H.I.V. The New York Times. https://www.nytimes.com/2013/12/05/us/poor-black-and-hispanic-men-are-face-of-hiv.html. Published December 5, 2013. Accessed March 30, 2021. [Google Scholar]
- 23.Grov C. HIV Risk and Substance Use in Men Who Have Sex with Men Surveyed in Bathhouses, Bars/Clubs, and on Craigslist.org: Venue of Recruitment Matters. AIDS Behav. 2012;16(4):807–817. doi: 10.1007/s10461-011-9999-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Contrada RJ, Ashmore RD, Gary ML, et al. Measures of Ethnicity-Related Stress: Psychometric Properties, Ethnic Group Differences, and Associations With Well-Being1. J Appl Soc Psychol. 2001;31(9):1775–1820. doi: 10.1111/j.1559-1816.2001.tb00205.x [DOI] [Google Scholar]
- 25.Meyer Mechthild C., Torres Sara, Cermeño Nubia, MacLean Lynne, Monzón Rosa. Immigrant Women Implementing Participatory Research in Health Promotion. West J Nurs Res. 2003;25(7):815–834. [DOI] [PubMed] [Google Scholar]
- 26.Kimball D, Rivera D, Gonzales M, Blashill AJ. Medical Mistrust and the PrEP Cascade Among Latino Sexual Minority Men. AIDS Behav. 2020;24(12):3456–3461. doi: 10.1007/s10461-020-02916-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rhodes SD, Alonzo J, Mann L, et al. Enhancement of a Locally Developed HIV Prevention Intervention for Hispanic/Latino MSM: A Partnership of Community-Based Organizations, a University, and the Centers for Disease Control and Prevention. AIDS Educ Prev. 2015;27(4):312–332. doi: 10.1521/aeap.2015.27.4.312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rhodes SD, Alonzo J, Mann L, et al. Small-Group Randomized Controlled Trial to Increase Condom Use and HIV Testing Among Hispanic/Latino Gay, Bisexual, and Other Men Who Have Sex With Men. Am J Public Health. 2017;107(6):969–976. doi: 10.2105/AJPH.2017.303814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brooks RA, Landrian A, Nieto O, Fehrenbacher A. Experiences of Anticipated and Enacted Pre-exposure Prophylaxis (PrEP) Stigma Among Latino MSM in Los Angeles. AIDS Behav. 2019;23(7):1964–1973. doi: 10.1007/s10461-019-02397-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is only available upon request.


