Abstract
Objective
To evaluate the effectiveness of immersive virtual reality (VR) on patient satisfaction as a distractive tool and pain relief among laboring women.
Methods
This was a randomized, controlled clinical trial with 42 laboring women allocated to VR intervention and control groups. Among women in the VR group, patient satisfaction with the use of VR was assessed by a Virtual Reality Satisfaction Survey, measured by a Visual Analog Scale (VAS) score and evaluated by questioning them about whether they would choose VR in future labor. As a primary outcome, patient satisfaction scores regarding the overall childbirth experience were compared between women in the two groups. A secondary outcome was pain assessed by a visual pain rating scale in the early and active phases of labor in women in both groups. Psychometric information was also collected from participants in each group using the Beck Anxiety Inventory and Beck Depression Inventory.
Results
We observed a high level of patient satisfaction with the use of immersive VR during labor. The VAS revealed a mean satisfaction score of 87.7 ± 12.9 out of a maximum of 100. Twenty out of 21 (95%) women in the VR group stated that they would like to use VR again in future labor. VR improved pain scores in early labor and contributed positively to the overall childbirth experience. The mean pain score pre-VR was 2.6 ± 1.2 compared to 2.0 ± 1.3 post-VR (p < 0.01). Anxiety and depression scores were similar in participants in the intervention and control groups (p = 0.103 and p = 0.13, respectively).
Conclusion
Immersive VR application during labor was associated with higher patient satisfaction based on our study findings. VR also improved participants’ pain scores in early labor before epidural administration. Immersive VR may find a place as an adjunct in labor and delivery units to improve lengthy labor experiences for women. Studies with larger groups of participants are needed to confirm these observations.
Trial Registration
ClinicalTrials.gov: NCT05032456
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-022-04598-y.
Keywords: Labor, Immersive Virtual Reality, Pain, Nonpharmacologic Treatment, Anxiety, Depression
Introduction
Neuraxial blockade, which includes epidural, spinal, and combined spinal-epidural analgesia, is presently the gold standard for pain control in laboring women [1, 2]. However, improving the whole childbirth experience for women is more complex and requires providing individualized care, including alternative treatments.
Opioid and nonopioid pharmacotherapies, patient-controlled analgesia (PCA), and nitrous oxide are all used with variable success for labor pain [3].
Acupuncture, hypnosis, yoga, hydrotherapy, massage, relaxation techniques, and transcutaneous electronic nerve stimulation (TENS) are among the adjuvant treatments provided to women in labor [4–7].
Recent literature indicates the successful use of immersive virtual reality (VR) for a variety of painful medical procedures [8–13]. Via wearing the VR goggles, the user has the illusion of going inside the 3D computer-generated world and visiting novel environments. Immersive VR is hypothesized to reduce pain through distraction, a nonpharmacologic attentional mechanism. With immersive VR, the user's brain is preoccupied with the flood of information presented by the virtual environment, thus reducing the mind’s ability to process pain signals [14].
We hypothesized that laboring women find immersive VR to be a beneficial tool for their overall childbirth experience. We randomly assigned women in labor admitted to our Labor and Delivery floor to a VR group or a control group.
Materials and methods
Study design
This was a randomized, controlled, single-center clinical trial in which we enrolled 42 women admitted during labor. We randomized these women to an immersive virtual reality (VR) or control group following their approval and written consent. The study was approved by the Institutional Ethics Committee of Acibadem Mehmet Ali Aydinlar University (IRB protocol no: 2020–18/07) and registered with clinicaltrials.gov (NCT05032456). The goal of this study was to assess whether immersive VR improved patient satisfaction in laboring women. We assessed patient satisfaction among VR users and compared patient satisfaction scores regarding the overall childbirth experience between the two groups as our primary objective. Our second objective was to assess whether VR provided pain relief in the latent or active phase of labor. We also evaluated anxiety and depression in both groups on admission as potential confounders. The study took place at Acibadem Maslak Hospital, a private hospital affiliated with Acibadem University School of Medicine in Istanbul, Turkey. Enrollment completed between November 2020 and June 2021.
Study subjects
Participants in this study were primigravida or multigravida presenting with labor who were candidates for vaginal birth with no known risk factors. The inclusion criteria were women between 18–42 years of age at 37–41 weeks gestation with a singleton pregnancy, vertex presentation, no history of chronic medical conditions, absence of pregnancy complications, and admission with documented labor by cervical exam and regular uterine contractions. Women with a diagnosis of migraine, headache, dizziness, motion sickness, epilepsy, psychiatric disorders, visual or auditory disabilities, or history of cesarean section were excluded.
Pregnant women between 35 and 37 weeks gestation who were followed by our Obstetric Outpatient Clinic at Acibadem Maslak Hospital were provided information leaflets for our VR study by one of the authors (NA). We have ‘Preparation to birth’ classes for expecting couples one every 6 weeks, and during each of those courses, NA briefly introduced our study, its objectives and handed information leaflets to attendants.
VR group
We used an Oculus Quest All-in-one VR Gaming Headset (128 GB) VR system. Before the intervention, the authors introduced the equipment and instructed study participants on how to wear and activate the headsets. Anxiety and depression scales were also applied on admission. The laboring women who enrolled in the VR group first wore the headsets in early labor (cervical dilation 3 cm) for 20 min. The patients were offered to choose among several virtual environments, including orange sunset, green meadows, black beginning, red savannah, blue deep, blue moon, blue ocean, white winter, and red fall (Fig. 1). Cards printed out from the screenshots of the Nature Treks application representing these novel immersion options were provided to the patients to help them pick up their preferred environment in advance. The second implementation of VR headsets was after epidural analgesia was administered in the active phase of labor (cervical dilation 6–7 cm); this implementation was also for 20 min. After the second intervention, the “Virtual Reality Satisfaction Survey” was applied by the authors. Patients were asked to fill out a visual pain rating scale immediately before and after VR use in early and active labor.
Fig. 1.

Natural Treks environments
Control group
For participants randomized to the control group, VR headsets were not used, and our standard of care in laboring women was followed. Anxiety and depression scales were used to evaluate to each subject on admission. Participants in this group completed a visual pain rating scale both in the latent and active phases of labor.
Clinical measures
To evaluate the effectiveness of immersive VR in laboring women, we evaluated patient satisfaction with the use of VR among the intervention group. Patient satisfaction with the overall childbirth experience and pain scores were compared between the intervention and control groups.
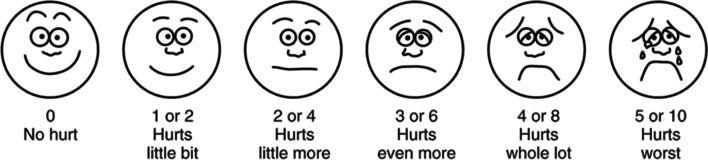
Patient satisfaction with the use of VR was assessed by a "Virtual Reality Satisfaction Survey", a 10-question survey prepared by our team and measured with a visual analog scale (VAS) score. 0 being the lowest and 100 being the highest possible VR satisfaction score. We also asked these women whether they would like to use VR in future labor. Patient satisfaction with overall labor and delivery experience was assessed using a numeric rating scale (NRS). All discharged women were called within a week following discharge and asked to rate their overall childbirth experience on a scale from 0 to 10. Zero indicates the most negative experience possible, and 10 indicates the highest satisfaction possible. We classified a score of 8 to 10 as high satisfaction and a score of 4 or less as poor childbirth experience. Pain scores in both early and active labor in each group were assessed using the Wong-Baker Faces Pain Rating Scale [15]. The scale shows a series of 6 faces ranging from a happy face at 0, or "no hurt", to a crying face at 5, which represents "hurts like the worst pain imaginable (Fig. 2).
Fig. 2.
Wong-Baker Faces Pain Scale
The anxiety levels of the study participants were assessed with the Beck Anxiety Inventory (BAI) [16]. This inventory consists of 21 items, each scored from 0 to 3. This is a self-report questionnaire measuring somatic and cognitive parts of anxiety. The total score is calculated by finding the sum of 21 items. A score of 0 to 7 indicates minimal anxiety, 8 to 15 indicates mild anxiety, 16 to 25 indicates moderate anxiety, and 30 to 63 is associated with severe anxiety.
For the assessment of depression in each group, the Beck Depression Inventory was used. It consists of 21 items, which is a multiple-choice test and gives a score ranging from 0 to 63. Each answer is scored on a scale value of 0–3. Measures of 0–9 indicate that a person is not depressed, 10–18 indicates mild-moderate depression, 19–29 indicates moderate-severe depression and 30–63 indicates severe depression. This self-rated test estimates the signs of depression, such as pessimism, feelings of failure, self-dissatisfaction, punishment, crying, and insomnia [17, 18].
Statistical methods
Sample size calculation and randomization
A priori power analysis was performed to estimate the sample size with a power (1-β) of 80%, a significance (α) of 0.05 and an allocation ratio of 1. We assumed a neutral satisfaction score of 50 out of 100 (SD = 12.5) for the control group and hypothesized.
25% increase in satisfaction scores with the use of VR. A sample size of 17 subjects per group was computed to observe this difference. For this analysis, G*Power software was used. For potential dropouts, we decided to enroll 21 subjects in each group. We used a random sequence generator (www.random.org), which picked a random sequence of 21 numbers (ranging from 1 to 42) for VR and control columns, respectively. This list was printed and kept in a locked cabinet at the nurses` station of Labor and Delivery floor. Following consent, we asked study participants to pick up a sealed opaque envelope, each containing a number from 1 to 42. Our charge nurse matched this number to the list of numbers for VR or the control group determining their assignment. This method helped to conceal the allocation sequence and provided that an equal number of subjects (n = 21) were randomized to the intervention (VR) and control groups. Since the intervention group wore VR headsets and the control group did not, blinding was not possible.
Data analysis
Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp. Descriptive statistics are presented as the mean score, standard deviation and absolute frequency. The Shapiro–Wilk test was used to analyze whether the continuous variables followed a normal distribution. To compare the mean overall childbirth satisfaction scores as well as anxiety and depression scores between the two groups, an independent t test or Mann–Whitney U test was used where appropriate. We used a paired samples t test or Wilcoxon t test where appropriate for the comparison of pain scores before and after the VR experience in early and active labor. A p value of less than 0.05 was considered statistically significant.
Results
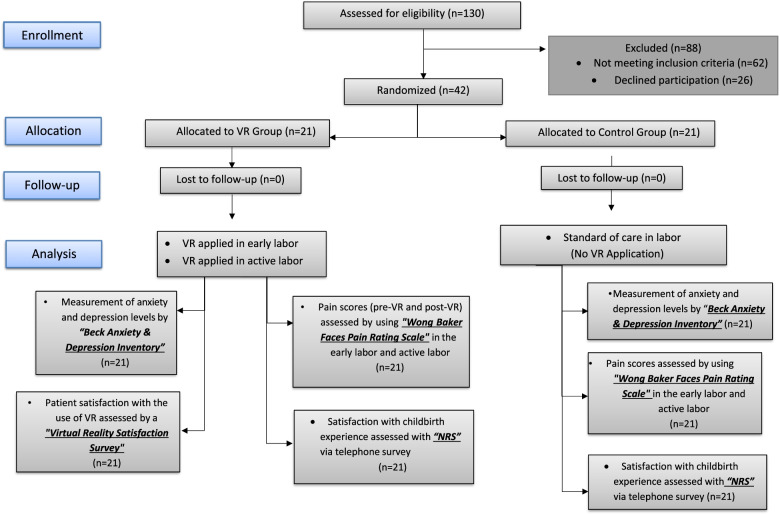
Of the 130 women admitted in labor, 68 were eligible for inclusion in the study, and 42 agreed to participate in this study (Fig. 3). The characteristics of laboring women randomized to either the immersive VR or the control group are shown in Table 1. There was no difference between the two groups in terms of these baseline characteristics.
Fig. 3.
Flowchart of the study
Table 1.
Characteristics of the Study Subjects
| VR GROUP (n = 21) |
CONTROL GROUP (n = 21) |
|
|---|---|---|
| Age, Mean ± SD | 31.0 ± 2.6 | 31.8 ± 3.6 |
| Gestational age, Mean ± SD | 39.5 ± 0.6 | 39.0 ± 1.0 |
| Body Mass Index (BMI), Mean ± SD | 26.2 ± 2.7 | 26.7 ± 3.1 |
| Parity | ||
| Primiparous (n) (%) | 18(86%) | 17(81%) |
| Multiparous (n) (%) | 3(14%) | 4(19%) |
| Delivery Type | ||
| Vaginal Birth (n) (%) | 18(86%) | 18(86%) |
| Cesarean Section (n) (%) | 3(14%) | 3(14%) |
All women in the VR group stated they enjoyed the VR experience reflected by the Virtual Reality satisfaction survey. The VAS revealed a mean satisfaction score of 87.7 ± 12.9 out of a maximum of 100. Twenty out of 21 (95%) women in the VR group stated that they would like to use VR again in future labor.
VR intervention improved pain scores in early labor before epidural administration. The mean pain score pre-VR was 2.6 ± 1.2 compared to 2.0 ± 1.3 post-VR (p < 0.01). Following epidural analgesia, pain scores were significantly lower, with a mean pain score of 0.8 ± 0.5, which remained unchanged (0.8 ± 0.5) post-VR.
Within one week following discharge, we conducted a telephone survey where we found a significant difference when patient satisfaction with the overall childbirth experience was questioned in the VR and control groups. The NRS score of women in the VR group was 8.8 ± 1.1 compared to 7.9 ± 1.6 in the control group (p = 0.04).
The Beck Anxiety Inventory revealed similar anxiety scores in the VR (11.2 ± 7.5) and control groups (7.5 ± 6.7) (p = 0.103). The Beck Depression Inventory also revealed similar depression scores in women in the VR (7.6 ± 5.8) and control groups (5.0 ± 5.0) (p = 0.13).
Women in the VR group tolerated the VR application very well. No significant adverse events were observed requiring exclusion from the study.
Discussion
We found that the use of immersive VR in laboring women was associated with a high level of patient satisfaction and likely served as a distractive tool. There are very limited data regarding the use of VR in laboring women. An earlier study evaluated VR use during episiotomy repair and reported less anxiety in the intervention group [15]. Two recent studies reported reduced labor pain and anxiety with the use of VR [19, 20]. Kist et al. showed that VR provided anxiolysis to laboring women undergoing epidural placement [21]. Hajesmeel-Gohari et al. very recently published a scoping review which included a total of nine VR studies on pregnant women and childbirth, vast majority finding VR useful in reducing anxiety and pain [22]. In our study, we also noticed an improvement in pain scores following the use of VR in early labor before epidural administration. Epidural administration afterward obviously provided substantial pain relief, as evidenced by dramatically decreased pain scores in both groups. It is important to clarify that we did not test VR as a substitute for epidural analgesia. Laboring women both in the intervention and control groups received epidural analgesia at their request as part of our standard of care. Our study is the first to assess whether VR might be used as an adjunct to improve the childbirth experience of women. Our awareness regarding the importance of a positive childbirth experience and its impact on women’s physical, psychological and social well-being has gradually increased [23–25]. In addition to ensuring maternal and neonatal health and safety, improving patient satisfaction during childbirth has become an integral part of high-quality care, as also underscored by the WHO [26].
The amount of support from caregivers and a quality caregiver-patient relationship are paramount for patient satisfaction during childbirth [27]. Accordingly, many labor and delivery units provide one-on-one nursing support for laboring women if possible. Most laboring women want to be involved in care decisions and demand that their input be respected. Attendance to antenatal classes and having birth plans are encouraged and increase the odds of a positive childbirth experience [28].
Poor childbirth experience, on the other hand, is a complex issue, which is reported more commonly in primiparous women, in cases of induced labor, operative delivery, emergency cesarean, postpartum hemorrhage, low Apgar score, shoulder dystocia, sphincter injury and maternal infection [29]. The VAS was found to be suitable in the assessment of negative birth experiences [30], and our study supports its potential to evaluate positive childbirth experiences as well.
Since labor is associated with severe pain in most women, pain control is very important to improve patient satisfaction [31, 32]. Currently, epidural analgesia is considered the gold standard in labor analgesia, providing the most effective pain relief during childbirth [33, 34]. On the other hand, many women with healthy pregnancies want to minimize medical interventions and seek nonpharmacological ways to cope with labor pain. In addition, they want to be relaxed yet remain active during labor. Many labor and delivery units are equipped to provide warm showers and birth ball exercises to those in labor. Warm showers in labor were associated with pain reduction and contributed to a positive overall experience [35]. Birth ball exercises also provided significant improvements in childbirth self-efficacy and pain [36]. Some units work with professional therapists and offer massage therapies during labor. Massage therapy during labor was associated with pain relief and decreased anxiety as well as shorter labor duration [37].
Fear of childbirth is common, which leads to increasing rates of cesarean on maternal request [38] and contributes to already high cesarean rates in countries such as Turkey [39]. Considering that cesarean rates have remained high in our centers with 24-h epidural analgesia availability, it is certain that we need to improve the overall childbirth experience beyond pain relief. Our findings of high patient satisfaction with VR use in labor along with routine epidural administration on demand further support this point. We need to present several options to laboring women to choose from, such as warm showers, birth ball exercises, yoga, massage, etc., possibly in an alternating fashion. Our study suggested that immersive VR might also be a valuable tool to distract and potentially entertain women during long hours of labor. VR may especially be instrumental during intermittent fetal monitoring episodes when most of the abovementioned activities are not feasible.
VR users may experience adverse effects, including headache, dizziness, motion sickness, and blurry vision. Immersive VR may also negatively affect static balance [40, 41]. Women in our study did not experience any significant side effects. This might be secondary to our small study size as well as our exclusion of all subjects with a diagnosis of migraine, headache, dizziness, motion sickness, and epilepsy. It is also worth mentioning that prior to this study, we conducted a survey among several volunteer pregnant women, and the vast majority indicated that they preferred immersion in nature (Nature Treks environments) compared to other options, including playing games.
Although randomization and strict adherence to the standard of care in both groups of laboring women are strengths of our study, it has several limitations as well. The numbers are relatively small, and obviously larger studies are needed to support our findings. It is also worth mentioning that this study was performed at a single upscale health center serving an affluent cohort potentially biased toward newer technology such as VR.
Conclusion
Based on the results of this preliminary study, immersive VR may improve pain scores likely through distraction in the latent phase of labor prior to epidural administration. VR might also improve patient satisfaction, an important indicator for the quality of care in childbirth.
Supplementary Information
Acknowledgements
We would like to thank all the laboring women who participated in this study. We would also like to thank all the staff members, nurses and midwives of the Labor and Delivery Unit at Acibadem Maslak Hospital. Finally we would like to thank Dr Emel Timucin for her support and guidance in statistics.
Abbreviations
- VR
Virtual Reality:
- PCA
Patient-Controlled Analgesia
- NRS
Numerical Rating Scale:
- BAI
Beck Anxiety Inventory
- BDI
Beck Depression Inventory
- WHO
World Health Organization
Authors’ contributions
GC and HMB presented the idea of a VR study to SG. SG helped them to mature the idea and finalize the study protocol, collaborated with NA and performed the computations. SG and GC performed the analysis of the results by using IBM Statistics SPSS 25 program. NA prepared and distributed information leaflets for the VR study and helped with study recruitment. HMB provided his Oculus Quest All-in-one VR Gaming headset for the study. GC and HMB introduced the Oculus Quest All-in-one VR Gaming headset and instructed study participants on how to wear and activate the headsets. HMB applied the anxiety and depression scales on admission. GC collected the data of the “Virtual Reality Satisfaction Survey” and applied it. GC imported the data into an Excel spreadsheet with support from HMB. HMB searched for possible applications of the device (Oculus Quest All-in-one VR Gaming Headset (128 GB) VR system) and helped the authors to conclude on the use of Nature Treks for laboring women. HMB took screenshots of the environments and presented them to patients to pick up their preferred environment. NA conducted a telephone survey about overall patient satisfaction with childbirth experience within one week following discharge. GC and NA processed the experimental data, performed the analysis, drafted the manuscript and designed the figures. NA, GC and HMB contributed to the final version of manuscript. SG supervised the project. The author(s) read and approved the final manuscript.
About the Authors
Elif Gizem Carus, is physical therapy graduate of Acibadem Mehmet Ali Aydinlar University, and now studying on her master thesis at Bahçehir University School of Health Sciences focusing on neuroscience. Nazli Albayrak, is a medical graduate of Acibadem Mehmet Ali Aydinlar University where she is working as Obstetrics& Gynecology resident. She is studying and working on the area of Obstetrics& Gynecology.Halit Mert Bildirici, is a senior student at American Robert College of Istanbul, completed several neuroscience courses and AP Biology, and aspires a career in Life Sciences.Selen Gur Ozmen, is an associate Professor of Neurology at Bahcesehir University School of Medicine, Department of Physical Therapy. She is a lecturer, and keeps her research focus on neuroscience.
Funding
Not applicable.
Availability of data and materials
All data generated/analysed during the current study are provided as a supplementary information file.
Declarations
Ethics approval and consent to participate
This study was approved by the Institutional Ethics Committee of Acibadem Mehmet Ali Aydinlar University (IRB protocol no: 2020–18/07) and registered with clinicaltrials.gov (NCT05032456).
The date of disclosure of study information and trial start was November 13, 2020. The objectives, methods, and other details of this study were explained to the participants. Written informed consent was obtained before participation in this study.
We confirm that all methods were carried out in accordance with relevant guidelines and regulations under Ethics approval and consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Elif Gizem Carus, Email: elifcarus@gmail.com.
Nazli Albayrak, Email: nazli.albayrak@acibadem.com.
Halit Mert Bildirici, Email: hmertbildirici@gmail.com.
Selen Gur Ozmen, Email: selen.gurozmen@ou.bau.edu.tr.
References
- 1.ACOG Committee. Pain relief during labor. Obstet Gynecol. 2004;104(1):213. PMID: 15229040 [PubMed]
- 2.Anim-Somuah M, Smyth RM, Jones L. Epidural versus non-epidural or no analgesia in labour. Cochrane Database Syst Rev. 2011;(12):CD000331. 10.1002/14651858.CD000331.pub3. Update in: Cochrane Database Syst Rev. 2018 May 21;5:CD000331. PMID: 22161362. [DOI] [PubMed]
- 3.Nanji JA, Carvalho B. Pain management during labor and vaginal birth. Best Pract Res Clin Obstet Gynaecol. 2020;67:100–112. 10.1016/j.bpobgyn.2020.03.002. Epub 2020 Mar 7. PMID: 32265134. [DOI] [PubMed]
- 4.Smith CA, Levett KM, Collins CT, Armour M, Dahlen HG, Suganuma M. Relaxation techniques for pain management in labour. Cochrane Database Syst Rev. 2018;3(3):CD009514. 10.1002/14651858.CD009514.pub2. Published 2018 Mar 28. [DOI] [PMC free article] [PubMed]
- 5.Madden K, Middleton P, Cyna AM, Matthewson M, Jones L. Hypnosis for pain management during labour and childbirth. Cochrane Database Syst Rev. 2012;11:CD009356. 10.1002/14651858.CD009356.pub2. Update in: Cochrane Database Syst Rev. 2016;(5):CD009356. PMID: 23152275. [DOI] [PubMed]
- 6.Smith CA, Levett KM, Collins CT, Jones L. Massage, reflexology and other manual methods for pain management in labour. Cochrane Database Syst Rev. 2012;(2):CD009290. 10.1002/14651858.CD009290.pub2. PMID: 22336862. [DOI] [PubMed]
- 7.Dowswell T, Bedwell C, Lavender T, Neilson JP. Transcutaneous electrical nerve stimulation (TENS) for pain relief in labour. Cochrane Database Syst Rev. 2009;(2):CD007214.10.1002/14651858.CD007214.pub2. PMID: 19370680; PMCID: PMC4297467. [DOI] [PMC free article] [PubMed]
- 8.Maani CV, Hoffman HG, Morrow M, Maiers A, Gaylord K, McGhee LL, DeSocio PA. Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like arm mounted VR goggles. J Trauma. 2011;71(1 Suppl):S125–30. 10.1097/TA.0b013e31822192e2. PMID: 21795888; PMCID: PMC4460976. [DOI] [PMC free article] [PubMed]
- 9.Mosadeghi S, Reid MW, Martinez B, Rosen BT, Spiegel BM. Feasibility of an Immersive Virtual Reality Intervention for Hospitalized Patients: An Observational Cohort Study. JMIR Ment Health. 2016;3(2):e28. 10.2196/mental.5801. PMID: 27349654; PMCID: PMC4940605. [DOI] [PMC free article] [PubMed]
- 10.Atzori B, Lauro Grotto R, Giugni A, Calabrò M, Alhalabi W, Hoffman HG. Virtual Reality Analgesia for Pediatric Dental Patients. Front Psychol. 2018;9:2265. 10.3389/fpsyg.2018.02265. Published 2018 Nov 23. [DOI] [PMC free article] [PubMed]
- 11.Walther-Larsen S, Petersen T, Friis SM, Aagaard G, Drivenes B, Opstrup P. Immersive Virtual Reality for Pediatric Procedural Pain: A Randomized Clinical Trial. Hosp Pediatr. 2019;9(7):501–507. 10.1542/hpeds.2018-0249. Epub 2019 Jun 3. PMID: 31160472. [DOI] [PubMed]
- 12.Faruki A, Nguyen T, Proeschel S, Levy N, Yu J, Ip V, Mueller A, Banner-Goodspeed V, O'Gara B. Virtual reality as an adjunct to anesthesia in the operating room. Trials. 2019;20(1):782. 10.1186/s13063-019-3922-2. PMID: 31882015; PMCID: PMC6935058. [DOI] [PMC free article] [PubMed]
- 13.Wang, YL., Gao, HX., Wang, JS. et al. Immersive virtual reality as analgesia for women during hysterosalpingography: study protocol for a randomized controlled trial. Trials. 2020;21:102. 10.1186/s13063-019-4023-y. [DOI] [PMC free article] [PubMed]
- 14.Hoffman HG, Richards TL, Coda B, Bills AR, Blough D, Richards AL, Sharar SR. Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. Neuroreport. 2004;15(8):1245–8. 10.1097/01.wnr.0000127826.73576.91. PMID: 15167542. [DOI] [PubMed]
- 15.Shourab N, Zagami S, Golmakhani N, Mazlom S, Nahvi A, Pabarja F, et al. Virtual reality and anxiety in primiparous women during episiotomy repair. Iran J Nurs Midwifery Res. 2016;21:521–526. doi: 10.4103/1735-9066.193417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56(6):893–7. 10.1037//0022-006x.56.6.893. PMID: 3204199. [DOI] [PubMed]
- 17.Beck AT, Steer RA & Brown GK. Manual for the Beck Depression Inventory-II. San Antonio: Psychological Corporation; 1996.
- 18.Aaron T. Beck, Robert A. Steer and Margery G. Carbin. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin Psychol Rev. 8(1):77–100. 10.1016/0272-7358(88)90050-5.
- 19.Frey DP, Bauer ME, Bell CL, Low LK, Hassett AL, Cassidy RB, et al. Virtual Reality Analgesia in Labor: The VRAIL Pilot Study - A Preliminary Randomized Controlled Trial Suggesting Benefit of Immersive Virtual Reality Analgesia in Unmedicated Laboring Women. Anesth Analg. 2019;128:E93–E96. doi: 10.1213/ANE.0000000000003649. [DOI] [PubMed] [Google Scholar]
- 20.Wong MS, Spiegel BM, Gregory KD. Virtual reality reduces pain in laboring women: a randomized controlled trial. Am J Perinatolo. 2021;38:e167–e172. doi: 10.1055/s-0040-1708851. [DOI] [PubMed] [Google Scholar]
- 21.Kist M, Bekemeyer Z, Ralls L, Carvalho B, Rodriguez ST, Caruso TJ. Virtual reality successfully provides anxiolysis to laboring women undergoing epidural placement. J Clin Anesth. 2020;61:109635. doi: 10.1016/j.jclinane.2019.109635. [DOI] [PubMed] [Google Scholar]
- 22.Hajesmeel-Gohari S, Sarpourian F, Shafiei E. Virtual reality applications to assist pregnant women: a scoping review. BMC Pregnancy Childbirth. 2021;21:249. doi: 10.1186/s12884-021-03725-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Attanasio LB, McPherson ME, Kozhimannil KB. Positive childbirth experiences in US hospitals: A mixed methods analysis. Matern Child Health J. 2014;18:1280–1290. doi: 10.1007/s10995-013-1363-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karlström A, Nystedt A, Hildingsson I. The meaning of a very positive birth experience: Focus groups discussions with women. BMC Pregnancy Childbirth. 2015;15:1–8. doi: 10.1186/s12884-015-0683-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dencker A, Bergqvist L, Berg M, Greenbrook JTV, Nilsson C, Lundgren I. Measuring women’s experiences of decision-making and aspects of midwifery support: A confirmatory factor analysis of the revised Childbirth Experience Questionnaire. BMC Pregnancy Childbirth. 2020;20:1–8. doi: 10.1186/s12884-020-02869-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tunçalp. Were WM, Maclennan C, Oladapo OT, Gülmezoglu AM, Bahl R, et al. Quality of care for pregnant women and newborns - The WHO vision. BJOG: Int J Obstet Gynaecol. 2015;122:1045–9. doi: 10.1111/1471-0528.13451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lazzerini M, Mariani I, Semenzato C, Valente EP. Association between maternal satisfaction and other indicators of quality of care at childbirth: a cross-sectional study based on the WHO standards. BMJ Open. 2020;10:e037063. doi: 10.1136/bmjopen-2020-037063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jolles MW, de Vries M, Hollander MH, van Dillen J. Prevalence, characteristics, and satisfaction of women with a birth plan in The Netherlands. Birth. 2019;46:686–692. doi: 10.1111/birt.12451. [DOI] [PubMed] [Google Scholar]
- 29.Adler K, Rahkonen L, Kruit H. Maternal childbirth experience in induced and spontaneous labour measured in a visual analog scale and the factors influencing it; a two year cohort study. BMC Pregnancy Childbirth. 2020;20:415. doi: 10.1186/s12884-020-03106-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Larsson C, Saltvedt S, Edman G, Wiklund I, Andolf E. Factors independently related to a negative birth experience in first-time mothers. Sex Reprod Healthc. 2011;2:83–89. doi: 10.1016/j.srhc.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 31.Hawkins JL. Epidural Analgesia for Labor and Delivery. N Engl J Med. 2010;362:1503–1510. doi: 10.1056/NEJMct0909254. [DOI] [PubMed] [Google Scholar]
- 32.Ashagrie HE, Fentie DY, Kassahun HG. A review article on epidural analgesia for labor pain management: A systematic review. Int J Surg Open. 2020;24:100–4.
- 33.Fyneface-Ogan S, Mato CN, Anya SE. Epidural anesthesia: Views and outcomes of women in labor in a Nigerian hospital. Ann Afr Med. 2009;8:250–256. doi: 10.4103/1596-3519.59580. [DOI] [PubMed] [Google Scholar]
- 34.Tulp MJ, Paech MJ. Analgesia for childbirth: modern insights into an age-old challenge and the quest for an ideal approach. Pain management. 2014;4:69–78. doi: 10.2217/pmt.13.63. [DOI] [PubMed] [Google Scholar]
- 35.Lee SL, Liu CY, Lu YY, Gau ML. Efficacy of Warm Showers on Labor Pain and Birth Experiences During the First Labor Stage. JOGNN - J Obstet Gynecol Neonatal Nurs. 2013;42:19–28. doi: 10.1111/j.1552-6909.2012.01424.x. [DOI] [PubMed] [Google Scholar]
- 36.Gau ML, Chang CY, Tian SH, Lin KC. Effects of birth ball exercise on pain and self-efficacy during childbirth: a randomised controlled trial in Taiwan. Midwifery. 2011;27(6):e293–300. 10.1016/j.midw.2011.02.004. Epub 2011 Apr 3. PMID: 21459499. [DOI] [PubMed]
- 37.Smith CA, Levett KM, Collins CT, Dahlen HG, Ee CC, Suganuma M. Massage, reflexology and other manual methods for pain management in labour. Cochrane Database Syst Rev. 2018;2018. 10.1002/14651858.CD009290.pub3. [DOI] [PMC free article] [PubMed]
- 38.Nieminen K, Stephansson O, Ryding EL. Women’s fear of childbirth and preference for cesarean section - A cross-sectional study at various stages of pregnancy in Sweden. Acta Obstet Gynecol Scand. 2009;88:807–813. doi: 10.1080/00016340902998436. [DOI] [PubMed] [Google Scholar]
- 39.Eyi EGY, Mollamahmutoglu L. An analysis of the high cesarean section rates in Turkey by Robson classification. J Maternal-Fetal Neonatal Med. 2019 doi: 10.1080/14767058.2019.1670806. [DOI] [PubMed] [Google Scholar]
- 40.Moro C, Stromberga Z, Raikos A, Stirling A. The effectiveness of virtuaş and augmented reality in health sciences and medical anatomy. Anat Sci Educ. 2017;10:549–559. doi: 10.1002/ase.1696. [DOI] [PubMed] [Google Scholar]
- 41.Park SH, Lee GC. Full-immersion virtual reality: Adverse effects related to static balance. Neurosci Lett. 2020;733:134974. doi: 10.1016/j.neulet.2020.134974. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated/analysed during the current study are provided as a supplementary information file.