Abstract
Background
Alpha-fetoprotein (AFP) is a biomarker used in clinical management of hepatocellular carcinoma (HCC), however, approximately 40% of HCC patients do not present with elevated serum AFP levels. This study aimed to investigate the clinical and pathologic characteristics between AFP positive and negative HCC patients to allow for improved clinical management and prognostication of the disease.
Methods
This study observed a cohort of HCC patients from Eastern and Southern China with comparisons of the clinical and pathologic features between serum AFP positive and negative patient groups; patients with decompensated hepatic cirrhosis, those with chronic hepatitis B, and hepatitis B virus (HBV) asymptomatic carrier patients were used as controls. Data included the laboratory results, pathology diagnosis, clinical staging and scores were obtained from routine clinical diagnostic methods.
Results
Patients with HCC, larger tumor sizes, liver cancer with hepatic cirrhosis, portal vein thrombosis, metastasis, high Child–Pugh score, high Barcelona-Clínic Liver Cancer (BCLC) stage, and advanced clinical stage had significantly higher serum AFP levels. Also, patients with HBsAg and HBeAg positive, high HBV DNA levels had significantly higher serum AFP levels. Patients with high serum AFP levels had higher protein induced by vitamin K absence or antagonist-II (PIVKA-II), alanine aminotransferase (ALT), aspartate aminotransferase (AST), alpha-l-fucosidase (AFU), gamma-glutamyl transpeptidase (γ-GT), γ-GT /ALT, direct bilirubin (DBIL), indirect bilirubin (IDBIL), fibrinogen, and D-dimer levels. Patients with AFP positive had higher white blood cells (WBC), neutrophil, monocyte, and platelet count and neutrophil to lymphocyte ratio (NLR).
Conclusions
The are significant differences in clinical pathologic characteristics between AFP positive and negative HCC patients which may be helpful for the management and prognostication of the disease.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12876-022-02279-w.
Keywords: Alpha-fetoprotein (AFP), Hepatocellular carcinoma (HCC), Liver cirrhosis, Chronic hepatitis B, Protein induced vitamin K absence or antagonist-II (PIVKA-II), Hepatitis B virus DNA (HBV DNA), Carcinoembryonic antigen (CEA), Neutrophil to lymphocyte ratio (NLR)
Introduction
Hepatocellular carcinoma (HCC) is a common malignancy in Asia [1]. About 364,800 new cases of liver cancer were diagnosed in China, resulting in about 318,800 deaths in 2014 [2]. The incidence of liver cancer in China is mainly related to hepatitis B virus infection, hepatic fibrosis, and biliary cirrhosis. Treatments for liver cancer include surgical resection, interventional embolization, radiofrequency ablation, liver transplantation, and chemotherapy. However, the postoperative recurrence and metastases rates remain high and the 5 years survival rate is still very low [3, 4]. The bottle neck for long-term survival improvement is the inability for the diagnosis of early stages of the disease when the tumor size is under 3 cm. HCC screening in high-risk populations relies on serum tumor markers and ultrasonography. For serum biomarkers, the alpha-fetoprotein (AFP) is commonly used as a first line screening tool recommended by guidelines worldwide and is in clinical practice because of easy accessibility, non-invasive nature, and low cost. Serum AFP concentrations > 400 ng/ml is considered as reliable for supporting the diagnosis of hepatocellular carcinoma. However, about 30–40% of HCC are AFP-negative (< 20 ng/mL) [5, 6]. The mechanism of AFP repression is unknown, it is hypothesized that silencing of AFP promotors because of mutation or promoter inhibition is one of the reasons [7–9]. HCC patients with AFP negative or weak positive serum tests are usually consistent with the characteristics of high differentiated cancers. Although a negative serum AFP may be associated with favorable liver cancer outcomes, it results in a miss diagnosis of liver cancer in general [10, 11]. Efforts focusing on identifying new HCC serum biomarkers for risk evaluation, early diagnosis, recurrence, and prognosis prediction have been extensively studied, however, no new biomarkers are satisfactory thus far [12–16]. A study found that high neutrophil–lymphocyte ratio (NLR) was associated with low AFP expression in patients with hepatitis B virus (HBV) related HCC, therefore, NLR could be a potential clinical marker of the pathogenesis of AFP negative liver cancer [17]. Another study found that fibrinogen to pre-albumin ratio was gradually increased alongside with the development of AFP-negative HCC and positively correlated with tumor size and Barcelona Clinic Liver Cancer stages (BCLC) [18]. Thus, we hypothesize that serum biomarkers would vary between AFP-positive and negative HCC patients and could be indicators of liver cancer pathogenesis and possibly useful in clinical management and prognostication. In this study, we analyzed the laboratory parameters and clinical characteristics between AFP-positive and negative HCC patients from Eastern and Southern China to better understand the pathogenesis of the disease, improving the management, and prognostication.
Patients and methods
Patients
This study analyzed a total of 992 HCC patients from both Eastern and Southern China (861 males, 131 females, ages from 23 to 89 years) from 2016 to 2020. The diagnosis of HCC followed the 2019 Chinese clinical guidelines for the management of hepatocellular carcinoma: updates and insights [19, 20]. Since hepatitis B virus (HBV) infection is the major cause of HCC in China, this study detected the HBV DNA and it associated biomarkers in the HCC patients. Furthermore, the pathogenesis of HCC caused by different etiologies usually undergoes from chronic inflammation to liver cirrhosis, and then HCC. Thus, we included the liver cirrhosis patients as one of the control groups as well. All HCC patients met pretreatment requirement, patients transferred from other hospitals were also excluded. In addition, 121 patients with decompensated hepatic cirrhosis (DHC, 85 males, 36 females, ages from 30 to 86 years and 40 to 85 years, respectively), 114 with chronic hepatitis B (CHB, 80 males, 34 females, ages from 14 to 72 years and 21 to 68 years, respectively), and 127 with hepatitis B virus asymptomatic carriers (AsC, 68 males, 59 females, ages from 5 to 67 years and 25 to 80 years, respectively) were used as control groups. Diagnosis of DHC followed the EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis [21], and diagnosis of CHB virus infection followed the EASL Clinical Practice Guidelines: Management of chronic hepatitis B virus infection and AASLD 2018 hepatitis B guidance [22, 23]. This study was approved by the Institute Review Board/Ethics Committee of The Affiliated Hospital of Shandong University of Traditional Chinese Medicine and The People’s Hospital of Guangxi Zhuang Autonomous Region for the collection of patients’ information, study protocols used, and clinical practice guidelines to be followed. Patients’ demographics are listed in Additional file 2: Table S1.
Chemiluminescence immunoassay of serum biomarkers
Serum AFP, carcinoembryonic antigen (CEA), cancer antigen 125 (CA-125), and cancer antigen 199 (CA-199) were analyzed on the Cobas e801 platform (Roche, Rotkreuz, Switzerland) and UniCel DxI 800 Access (Beckman Coulter, Brea, California, USA); Protein induced by vitamin K absence or antagonist-II (PIVKA-II) was analyzed on the ARCHITECT i2000SR platform (Abbott Park, Illinois, USA); HBsAg and HBeAg were analyzed on the EasyCuta platform (PerkinElmer, Taicang, Suzhou, China) following the manufacturers’ instruction and laboratory standard operating procedures. Serum AFP level lower than 20 ng/mL was defined as AFP negative, while it was defined as AFP positive if the concentration was higher than 20 ng/mL.
Clinical chemistry analysis
Serum homocysteine (Hcy), ferritin (SF), alanine transaminase (ALT), γ-glutamyl transpeptidase (γ-GT), aspartate aminotransferase (AST), alpha-L-fucosidase (AFU), direct bilirubin (DBIL), indirect bilirubin (IBIL), total protein (TP), and albumin (ALB) were analyzed on the AU5800 platform (Beckman Coulter, Brea, California, USA) following the manufacturer’s instruction and laboratory standard operating procedures.
Hematology analysis
Hematology analysis of blood cells (complete blood count and differentiation) were performed on the XN 9000 hematology analyzer (Sysmex, Kobe, Japan) and BC 6900 hematology analyzer (Mindray, Shenzhen, China) following the manufacturers’ instruction and laboratory standard operating procedures.
Coagulation analysis
Prothrombin time (PT), fibrinogen, and D-dimer were analyzed using the STA-R Evolution (Diagnostica Stago S.A.S., Asnières sur Seine Cedex, France) following the manufacturer’s instruction and laboratory standard operating procedures. The international normalized ratio (INR) was automatically calculated by the analyzer.
Hepatitis B virus DNA detection
Hepatitis B virus (HBV) DNA was detected on the C1000 Touch Thermocycler (Bio-Rad, Hercules, California, USA) by using the real time polymerase chain reaction (PCR) technique following the manufacturer’s instruction and laboratory standard operating procedures. The cut-off value for DNA levels for analysis was set at 500 IU/mL.
Pathology diagnosis
The tumor histologic types and differentiation were characterized by pathology examination of routine pathologic diagnosis from surgical tissues.
Child–Pugh scoring and BCLC staging classification of hepatocellular carcinoma
The Child–Pugh Scoring was performed according to the scoring system [24]. The BCLC staging classification of hepatocellular carcinoma was used in routine clinical management [25].
Statistical analysis
All data was analyzed using the SPSS version 26 and GraphPad Prism version 9 software. Since the data sets were skewed, thus, nonparametric tests (Mann–Whitney U Test, Kruskai–Wallis H Test, Spearman Test, and Pairwise comparison) were used for the analysis. A p value < 0.05 was considered significant.
Results
Normality test result of data set
The statistical analysis indicated that the data was skewed. The distribution of serum AFP in patient groups is shown in Additional file 1: Figure S1. Most patients’ AFP levels were at the lower end (left in the histogram of Additional file 1: Fig. S1).
Comparison of serum AFP levels among patient groups
Table 1 lists the comparison of serum AFP levels among patient groups using the nonparametric method. Statistical results of pairwise comparison are shown in Additional file 1: Figure S2 A. The results show that serum AFP levels in HCC patients are significantly higher than in CHB, DHC, and AsC patients (p < 0.0001 for all). AFP level in CHB patients is significantly higher than in AsC patients (p < 0.0001); AFP level in DHC patients is significantly higher than in Asc patients (p = 0.0238); there is no significant difference in AFP level between CHB and DHC patients (p = 0.5050).
Table 1.
Comparison of serum AFP levels among patient groups
| n | Median | P25–P75 | Mean rank | Test statistic | P | |
|---|---|---|---|---|---|---|
| HCC | 992 | 177.80 | 9.25–1210.00 | 801.61 | 405.518 | 0.000 |
| CHB | 114 | 5.72 | 2.80–21.99 | 447.83 | ||
| DHC | 121 | 4.41 | 2.16–11.53 | 359.79 | ||
| AsC | 127 | 2.61 | 1.91–3.46 | 216.89 |
HCC: Hepatocellular carcinoma; DHC: Decompensated hepatic cirrhosis; CHB: Chronic hepatitis B; AsC: Hepatitis B virus asymptomatic carrier
Association between serum AFP levels and clinical pathologic features in HCC patients
Serum AFP levels in patients with tumor size ≥ 10 cm were significantly higher than that of < 10 cm (p = 0.000); there is no significant difference in AFP level between HCC patients with and without liver cirrhosis (p = 0.398). Patients with portal vein thrombosis had higher AFP levels (p = 0.000); patients who had metastasis also had higher AFP levels (p = 0.004); AFP levels in patients with large tumors were significantly higher than those with diffuse or single nodule tumors (p = 0.000); high Child–Pugh score patients had higher AFP levels than those with low scores (p = 0.000); patients with high BCLC stage had higher AFP levels than those with low stages (p = 0.000); similarly, patients with more advanced clinical stages had higher AFP levels than that of lower stages (p = 0.000). There was no significant correlation between tumor differentiation and serum AFP levels (p = 0.092) (Table 2). Additional file 1: Figure S2 B–E further show the pairwise comparison.
Table 2.
Association between serum AFP levels and clinical pathologic features
| n | Median | P25–P75 | Mean rank | Test statistic | P | ||
|---|---|---|---|---|---|---|---|
| Tumor sizea | < 10 cm | 569 | 82.53 | 7.08–1000 | 379.83 | − 7.593 | 0.000 |
| (largest in diameter) | ≥ 10 cm | 279 | 928.70 | 51.83–3000 | 515.59 | ||
| Liver cirrhosisa | No | 439 | 211 | 7.31–1494.20 | 505.12 | − 0.845 | 0.398 |
| Yes | 553 | 160.7 | 11.29–1210.00 | 489.66 | |||
| PVTa | No | 711 | 97.63 | 6.98–1000.00 | 459.53 | − 6.472 | 0.000 |
| Yes | 281 | 844.1 | 49.49–1914.15 | 590.04 | |||
| Metastasisa | No | 699 | 138.00 | 7.60–1210 | 479.39 | − 2.909 | 0.004 |
| Yes | 293 | 390.10 | 17.67–1210 | 537.33 | |||
| Types of tumorb | Single nodule | 357 | 44.31 | 5.80–882.69 | 413.75 | 77.401 | 0.000 |
| Multiple nodules | 244 | 158.67 | 9.27–1210 | 480.64 | |||
| Infiltrative | 139 | 190.70 | 15.39–1097.22 | 514.60 | |||
| Large tumor | 252 | 993.00 | 79.95–3000.00 | 619.10 | |||
| TDb | Low | 44 | 94.98 | 7.68–750.92 | 104.66 | 4.769 | 0.092 |
| Medium | 111 | 86.59 | 4.33–780.26 | 92.46 | |||
| High | 17 | 63.94 | 3.34–64.84 | 70.67 | |||
| Child–Pughb | A | 585 | 77.02 | 6.56–1000.00 | 442.59 | 51.720 | 0.000 |
| B | 289 | 686.4 | 25.07–2644.37 | 557.29 | |||
| C | 116 | 1000 | 99.57–1210 | 608.37 | |||
| BCLCb | 0 | 22 | 12.65 | 4.34–70.97 | 233.55 | 54.373 | 0.000 |
| A | 201 | 39.50 | 5.16–541.49 | 289.41 | |||
| B | 221 | 334.60 | 17.50–1955.01 | 394.89 | |||
| C | 257 | 586.10 | 28.19–1210 | 405.95 | |||
| D | 34 | 1000 | 158.68–3000.00 | 457.93 | |||
| Clinical stagingb | I | 53 | 9.97 | 3.64–193.50 | 99.79 | 22.725 | 0.000 |
| II | 37 | 213.21 | 6.56–843.00 | 140.82 | |||
| III | 105 | 155.80 | 14.02–1210.00 | 146.92 | |||
| IV | 92 | 887.50 | 23.87–1210.00 | 167.41 |
aMann–Whitney U
bKruskai–Wallis H
PT: Thrombosis of portal vein; Metastasis: lymph nodes or distant organ metastasis; TD: tumor differentiation; BCLC: Barcelona clinic liver cancer staging
Association between serum AFP status and hepatitis B biomarkers in HCC patients
Patients with HBsAg and HBeAg positive and HBV DNA amount > 500 IU/mL had significantly higher serum AFP levels (p = 0.000 for all) (Table 3).
Table 3.
Association between serum AFP levels and hepatitis B biomarkers in liver cancer patients (Mann–Whitney)
| N | Median | P25–P75 | Mean rank | Z | P | ||
|---|---|---|---|---|---|---|---|
| HBsAg | Negative | 177 | 20.23 | 3.32–1000.00 | 371.13 | − 6.014 | 0.000 |
| Positive | 793 | 239.95 | 15.55–1210.00 | 511.03 | |||
| HBeAg | Negative | 849 | 159.21 | 7.93–1210.00 | 475.31 | − 3.527 | 0.000 |
| Positive | 125 | 417.20 | 41.91–3000.00 | 570.26 | |||
| HBV DNA (copies) | ≤ 500 | 389 | 110.69 | 7.35–1072.50 | 349.76 | − 4.456 | 0.000 |
| (IU/ml) | > 500 | 380 | 501.23 | 29.28–1598.65 | 421.07 |
Association between serum AFP status and other tumor markers in HCC patients
Patients with high serum AFP levels had higher serum PIVKA-II (p < 0.000). There is no significant correlation between serum AFP and CEA, CA-125, and CA-199 levels (p = 0.127, 0.469, and 0.170, respectively). Additional file 2: Table S2. The Overlay Scatter of serum AFP levels with CEA, PIVKA-II, CA-125, and CA-199 are shown in Fig. 1 for further demonstration.
Fig. 1.
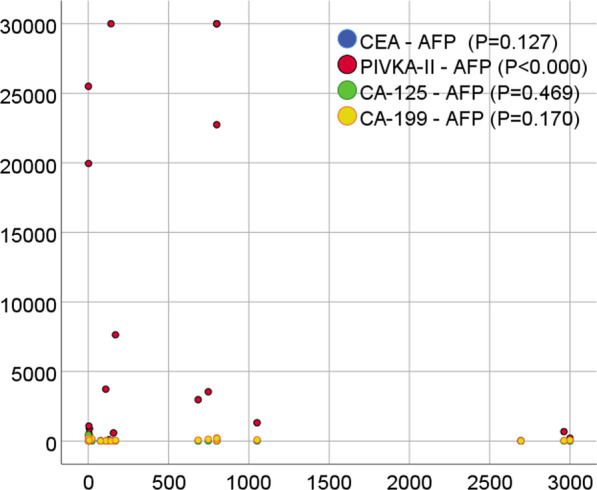
The overlay scatter of serum AFP and other tumor markers (PIVKA-II, CEA, CA-125, and CA-199). Figure shows the association between serum AFP levels and PIVKA-II, CEA, CA-125, and CA-199 in HCC patients using the overlay scatter plot, a p value is displayed
Association between serum AFP status and liver function biomarkers in HCC patients
Patients with high serum AFP levels had higher serum alanine aminotransferase (ALT), γ-glutamyl transpeptidase (γ-GT), aspartate aminotransferase (AST), alpha-L-fucosidase (AFU) activities (p = 0.000 for all), and higher γ-GT/ALT ratio (p = 0.000). Patients with high serum AFP levels also had higher serum direct bilirubin (DBIL) and indirect bilirubin (IBIL) levels (p = 0.000 and p = 0.015, respectively) and fibrinogen (p = 0.005) as well as D-Dimer (p = 0.000). There was no significant association between serum AFP levels and serum homocysteine (Hcy, p = 0.445), ferritin (SF, p = 0.830), total protein (TP, p = 0.093), and albumin (ALB, p = 0.496). The prothrombin time did not show significant different either (p = 0.204) between AFP negative and positive patients (Table 4).
Table 4.
Association between serum AFP levels and liver function markers in patients with AFP negative and AFP positive (Mann–Whitney)
| AFP | n | Median | P25–P75 | Mean rank | Z | P | |
|---|---|---|---|---|---|---|---|
| Hcy (µg/L) | – | 88 | 15.10 | 12.10–20.85 | 87.94 | − 0.764 | 0.445 |
| + | 93 | 15.60 | 12.40–21.80 | 93.89 | |||
| SF (µg/L) | – | 142 | 560.79 | 235.18–1125.95 | 197.35 | − 0.214 | 0.830 |
| + | 142 | 575.8 | 268.20–1195.70 | 199.92 | |||
| ALT (U/L) | – | 312 | 32.00 | 20.00–52.00 | 418.30 | − 5.733 | 0.000 |
| + | 677 | 42.00 | 27.00–68.00 | 530.35 | |||
| γ-GT (U/L) | – | 312 | 71.00 | 38.00–148.50 | 388.43 | − 7.965 | 0.000 |
| + | 677 | 142.00 | 67.00–269.00 | 544.11 | |||
| γ-GT/ALT | – | 312 | 2.24 | 1.32–4.82 | 442.96 | − 3.889 | 0.000 |
| + | 677 | 3.25 | 1.67–5.80 | 518.98 | |||
| AST (U/L) | – | 313 | 41.00 | 27.00–63.00 | 378.04 | − 8.815 | 0.000 |
| + | 678 | 64.50 | 39.00–125.25 | 550.45 | |||
| AFU (U/L) | – | 297 | 27.40 | 22.80–34.00 | 353.55 | − 9.265 | 0.000 |
| + | 654 | 36.33 | 27.18–50.03 | 531.61 | |||
| DBIL (μmol/L) | – | 311 | 4.90 | 3.30–9.70 | 437.47 | − 4.258 | 0.000 |
| + | 677 | 6.50 | 4.00–13.90 | 520.7 | |||
| IBIL (μmol/L) | – | 311 | 11.40 | 7.50–17.30 | 461.86 | − 2.437 | 0.015 |
| + | 677 | 12.30 | 8.20–20.65 | 509.49 | |||
| TP (g/L) | – | 312 | 67.10 | 62.23–71.98 | 471.6 | − 1.678 | 0.093 |
| + | 675 | 67.40 | 62.80–73.00 | 504.35 | |||
| ALB (g/L) | – | 312 | 35.85 | 30.80–40.68 | 504.17 | − 0.686 | 0.493 |
| + | 677 | 35.10 | 30.80–39.90 | 490.77 | |||
| PT (sec) | – | 311 | 14.20 | 13.40–15.40 | 475.56 | − 1.271 | 0.204 |
| + | 673 | 14.40 | 13.60–15.40 | 500.33 | |||
| INR | – | 234 | 1.13 | 1.05–1.23 | 387.1 | − 0.475 | 0.635 |
| + | 551 | 1.14 | 1.06–1.24 | 395.5 | |||
| Fibrinogen | 233 | 3.09 | 2.51–4.30 | 358.29 | − 2.786 | 0.005 | |
| 552 | 3.48 | 2.67–4.54 | 407.65 | ||||
| D-dimer | 216 | 0.89 | 0.45–2.53 | 326.11 | − 3.592 | 0.000 | |
| 523 | 1.35 | 0.68–2.94 | 388.13 |
AFP (−): < 20 µg/L; AFP (+): ≥ 20 µg/L; Hcy: homocysteine; SF: serum ferritin; ALT: alanine aminotransferase; γ-GT: γ-glutamyl transpeptidase; AST: Aspartate aminotransferase; AFU: alpha-L-fucosidase; DBIL: direct bilirubin; IBIL: indirect bilirubin; TP: total protein; ALB: albumin; PT: prothrombin time; INR: international normalized ratio
Association between serum AFP status and hematology parameters in HCC patients
Table 5 shows that serum AFP status is positively associated with white blood cell (WBC) count, neutrophils, monocytes, and platelets (p = 0.002, 0.000, 0.020, and 0.006, respectively). Serum AFP positive patients have lower lymphocyte percentage than negative patients (p = 0.000), thus, the neutrophils to lymphocytes ration (NLR) is higher in serum AFP positive patients (p = 0.000).
Table 5.
Association between serum AFP levels and hematology parameters (Mann–Whitney)
| AFP | N | Median | P25–P75 | Mean rank | Z | P | |
|---|---|---|---|---|---|---|---|
| WBC | – | 313 | 5.91 | 4.45–7.68 | 487.43 | − 3.068 | 0.002 |
| + | 679 | 6.45 | 5.00–8.38 | 542.28 | |||
| Neu | – | 313 | 3.48 | 2.45–5.46 | 444.02 | − 3.917 | 0.000 |
| + | 679 | 4.17 | 3.00–5.99 | 520.69 | |||
| Neu% | – | 313 | 63.00 | 55.00–73.00 | 495.6 | − 3.933 | 0.000 |
| + | 679 | 67.00 | 59.00–74.10 | 538.2 | |||
| Lym | – | 313 | 1.43 | 1.00–1.89 | 508.97 | − 0.931 | 0.352 |
| + | 679 | 1.37 | 1.00–1.86 | 490.75 | |||
| Lym% | – | 313 | 26.00 | 16.00–33.15 | 547.13 | − 3.779 | 0.000 |
| + | 679 | 22.00 | 15.00–29.4 | 473.16 | |||
| NLR | – | 313 | 2.36 | 1.67–4.52 | 444.65 | − 3.870 | 0.000 |
| + | 679 | 3.04 | 2.03–4.89 | 520.4 | |||
| Mon | – | 313 | 0.46 | 0.32–0.64 | 465.43 | − 2.319 | 0.020 |
| + | 679 | 0.5 | 0.37–0.69 | 510.82 | |||
| Mon% | – | 313 | 8.00 | 6.00–10.00 | 493.93 | − 0.192 | 0.848 |
| + | 679 | 8.00 | 6.20–10.00 | 497.68 | |||
| PLT | – | 236 | 166 | 125–226 | 361.68 | − 2.755 | 0.006 |
| + | 555 | 191 | 127–260 | 410.6 |
AFP (−): < 20 µg/L; AFP (+): ≥ 20 µg/L; WBC: white blood cell count; Neu: neutrophil count; Neu%: percentage of neutrophils; Lym: lymphocyte count; Lym%: percentage of lymphocytes; NLR: neutrophil to lymphocyte ratio; Mon: monocyte count; Mon%: percentage of monocytes; PLT: platelet count
Discussion
AFP is a major plasma protein produced by the yolk sac and the liver during fetal life. AFP expression in adults is often associated with hepatoma or teratoma [26].
The underlying mechanism of AFP expression status in HCC and its role in the development and prognosis is still unclear; promoter polymorphism or silencing of AFP gene is believed to be the major reason [27, 28]. Understanding the clinical pathologic characteristics of liver cancer patients with low and high serum AFP could be helpful for clinical management and prognostication of this deadly disease.
Serum AFP status among patient groups
In this observation, we found that serum AFP levels in HCC patients were significantly higher than in chronic hepatitis B, decompensated hepatic cirrhosis, and hepatitis B virus asymptomatic carrier patients. This further indicates that tumor cells secret AFP into the serum, the detailed mechanism is still unclear. Cellular membrane damage and/or eruption of tumor cells are believed to involved in the pathogenesis [29]. One study mentioned that HCC patients with negative AFP tended to be older males with less HBV infection, more non-viral etiology, and less cirrhosis [30]. Table 1 and Additional file 1: Figure S2 A indicate a trend from high to low in median AFP levels of different patient groups, consistent with this report.
High serum AFP level was associated with unfavorable prognostic factors
We also found that patients with larger tumors, hepatic cirrhosis, portal vein thrombosis, metastasis, and massive hepatocellular carcinomas had higher serum AFP levels. These suggest that patients with higher serum AFP levels tend to have poor clinical outcome [31–34]. It is also possible that higher burden of disease exists in these patients accounting for the increased AFP levels.
Association of serum AFP levels between Child–Pugh score, BCLC stage, and clinical stage
Serum AFP levels were significantly higher in patients with high Child–Pugh score, high BCLC stage, and advanced clinical stage. Lim et al. reported that AFP levels and Child–Pugh scores were associated with brain metastasis in HCC patients [35]. Liu et al. reported that based on BCLC staging, serum AFP response was correlated with the efficacy of transarterial chemoembolization in HCC patients [36]. Incorporation of serum AFP into the BCLC staging system was helpful in predicting the outcome of HCC patients, and AFP positive was an independent poor prognostic factor [37]. Gomaa et al. found that the addition of AFP and ascites to the BCLC staging system improved the prognostic prediction for early and intermediate stages of liver cancer patients [38].
Patients with HBsAg and HBeAg positive, and high HBV DNA levels had significantly higher serum AFP levels
Again, our observation further confirmed that serum AFP levels were associated with hepatitis B viral biomarkers positivity as reported previously [39]. HCC patients with positive HBsAg and HBeAg, high levels of HBV DNA had higher serum AFP levels. This further indicates that active viral replication and chronic liver disorder and hepatocyte damage is occurring in liver cancer patients [40, 41].
Association between serum AFP levels and other tumor markers
Patients with high serum AFP levels also had higher serum PIVKA-II. PIVKA-II is usually used in addition to AFP measurement for HCC diagnosis [42]. However, in this study, we found that there was a positive association between serum AFP and PIVKA-II levels in HCC patients. Si et al. reported that combined analyses of serum AFP and PIVKA-II increased the diagnostic performance for HBV-related HCC [43]. We found that there was no association between serum AFP and CEA, CA-125, and CA-199 levels. Report mentioned that elevated serum AFP and CEA were found in advanced hepatocellular carcinoma with extrahepatic metastasis [44]. Gou et al. found that both serum CEA and CA-199 increased but not AFP in primary adenosquamous carcinoma of the liver [45]. Serum CEA level may differ according to HCC subgroups which needs to be further investigated [46].
Association between serum AFP status and liver function, hemostatic status in HCC patients
As described above, serum AFP status was associated with Child–Pugh score. We further analyzed individual elements of the Child–Pugh scoring system, the ALT, AST, AFU, γ-GT, γ-GT/ALT ratio, DBIL, IBIL levels, fibrinogen, and D-dimer levels with serum AFP status. Results showed that patients with high serum AFP levels had higher serum ALT, AST, AFU, γ-GT, γ-GT/ALT ratio, DBIL, and IBIL levels, as well as fibrinogen and D-dimer levels. These results further confirmed the clinical usage of Child–Pugh scoring system for liver cancers. Elevated fibrinogen and D-dimer levels may suggest a potential deep venous thrombosis, or other complications in advanced tumors including liver cancer.
Association of serum AFP status with hematology parameters
Our observation found that serum AFP status was positively associated with peripheral blood WBC, neutrophils, monocytes, platelets, and the neutrophils to lymphocytes ratio (NLR). These parameters may suggest that an inflammatory or infection condition occurred in patients with high serum AFP levels, since the AFP status was associated with unfavorable clinical pathologic features as described above. Shiraki et al. reported that elevated NLR is predictive of a poor survival in patients with primary HCC showing normal AFP levels [47]. Another report on a systemic review of the literature showed that NLR and albumin in HCC predicted survival better than the conventional AFP [48]. Our finding on NLR was opposite to that of Huang et al. [18].
Conclusions
In summary, the results especially the laboratory parameters observed in our study in AFP negative HCC patients could be used for diagnosis and prognostic evaluation of these patients. HBV DNA viral load and hematologic indices are especially new parameters in associating with serum AFP status in HCC.
Supplementary Information
Additional file 1. Patients’ demographics and the association between serum AFP levels and other tumor markers in patients with AFP negative and AFP positive.
Additional file 2. Distribution of AFP in patient groups and the comparison of serum AFP levels among patient groups and among clinical pathologic features.
Acknowledgements
The authors would like to thank The People’s Hospital of Guangxi Zhuang Autonomous Region and The Affiliated Hospital of Shandong University of Traditional Chinese Medicine for supporting on this study.
Abbreviations
- HCC
Hepatocellular carcinoma
- PLC
Primary liver cancer
- CCA
Cholangiocarcinoma
- H-ChC
Hepatocellular-cholangiocarcinoma
- DHC
Decompensated hepatic cirrhosis
- CHB
Chronic hepatitis B
- AsC
Hepatitis B virus asymptomatic carrier
- PVT
Portal vein thrombosis
- MHC
Massive hepatocellular carcinoma
- BCLC
Barcelona clinic liver cancer staging
- CEA
Carcinoembryonic antigen
- PIVKA-II
Protein induced by vitamin K absence or antagonist-II
- CA-125
Cancer antigen 125
- CA-199
Cancer antigen 199
- Hcy
Homocysteine
- SF
Serum ferritin
- ALT
Alanine aminotransferase
- γ-GT
γ-Glutamyl transpeptidase
- AST
Aspartate aminotransferase
- AFU
Alpha-L-fucosidase
- DBIL
Direct bilirubin
- IBIL
Indirect bilirubin
- TP
Total protein
- ALB
Albumin
- PT
Prothrombin time
- INR
International normalized ratio
- WBC
White blood cell count
- Neu
Neutrophil count
- Neu%
Percentage of neutrophils
- Lym
Lymphocyte count
- Lym%
Percentage of lymphocytes
- NLR
Neutrophil to lymphocyte ratio
- Mon
Monocyte count
- Mon%
Percentage of monocytes
Author contributions
XC: collected clinical and pathologic data; LJ: collected data and data analysis; YY: collected data; XH: collected data; XY: collected data; Steven Hochwald: discussion and clinical instruction; JL: project organization; HH: conceived the study and writing. All authors read and approved the final manuscript..
Funding
No specific funding was disclosed.
Availability of data and materials
Data is available by contacting Huayi Huang at Henry.Huang@Mindray.com.
Declarations
Ethics approval and consent to participate
This study was approved by the Institute Review Board (Ethics Committee) of The Affiliated Hospital of Shandong University of Traditional Chinese Medicine (approval No. 2021 (025)) and The People’s Hospital of Guangxi Zhuang Autonomous Region (approval No. KY-LW-2021-6) for the collection of patients’ information. Patients’ written informed consent was waived by the Institutional Review Board/ Ethics Committee of The Affiliated Hospital of Shandong University of Traditional Chinese Medicine and The People’s Hospital of Guangxi Zhuang Autonomous Region. All methods used in this study were performed in accordance with the relevant guidelines and regulations in routine clinical practice. All experimental protocols were approved by The Affiliated Hospital of Shandong University of Traditional Chinese Medicine and The People’s Hospital of Guangxi Zhuang Autonomous Region.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiaowei Chi and Liejun Jiang have contributed equally to this work
Contributor Information
Jie Liu, Email: labmed@163.com.
Huayi Huang, Email: Henry.Huang@Mindray.com.
References
- 1.https://www.iarc.who.int/featured-news/new-world-cancer-report/
- 2.Zheng R, Qu C, Zhang S, Zeng H, Sun K, Gu X, Xia C, Yang Z, Li H, Wei W, Chen W, He J. Liver cancer incidence and mortality in China: temporal trends and projections to 2030. Chin J Cancer Res. 2018;30(6):571–579. doi: 10.21147/j.issn.1000-9604.2018.06.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarveazad A, Agah S, Babahajian A, Amini N, Bahardoust M. Predictors of 5 year survival rate in hepatocellular carcinoma patients. J Res Med Sci. 2019;24:86. doi: 10.4103/jrms.JRMS_1017_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang XH, Long LH, Cui Y, Jia AY, Zhu XG, Wang HZ, Wang Z, Zhan CM, Wang ZH, Wang WH. MRI-based radiomics model for preoperative prediction of 5-year survival in patients with hepatocellular carcinoma. Br J Cancer. 2020;122(7):978–985. doi: 10.1038/s41416-019-0706-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Enguita-Germán M, Fortes P. Targeting the insulin-like growth factor pathway in hepatocellular carcinoma. World J Hepatol. 2014;6(10):716–737. doi: 10.4254/wjh.v6.i10.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guo W, Sun YF, Shen MN, Ma XL, Wu J, Zhang CY, Zhou Y, Xu Y, Hu B, Zhang M, Wang G, Chen WQ, Guo L, Lu RQ, Zhou CH, Zhang X, Shi YH, Qiu SJ, Pan BS, Cao Y, Zhou J, Yang XR, Fan J. Circulating tumor cells with stem-like phenotypes for diagnosis, prognosis, and therapeutic response evaluation in hepatocellular carcinoma. Clin Cancer Res. 2018;24(9):2203–2213. doi: 10.1158/1078-0432.CCR-17-1753. [DOI] [PubMed] [Google Scholar]
- 7.Li XJ, Shao DH, He ML, Liang GW. Association of common variants in HNF1A gene with serum AFP level in healthy chinese individuals and HCC patients. Dis Markers. 2019;2019:6273497. doi: 10.1155/2019/6273497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shen S, Feng H, Liu L, Su W, Yu L, Wu J. TCP10L negatively regulates alpha-fetoprotein expression in hepatocellular carcinoma. BMB Rep. 2020;53(8):431–436. doi: 10.5483/BMBRep.2020.53.8.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang L, Wang K, Deng Q, Li W, Zhang X, Liu X. Identification of key hydroxymethylated genes and transcription factors associated with alpha-fetoprotein-negative hepatocellular carcinoma. DNA Cell Biol. 2019;38(11):1346–1356. doi: 10.1089/dna.2019.4689. [DOI] [PubMed] [Google Scholar]
- 10.Wang X, Wang Q. Alpha-fetoprotein and hepatocellular carcinoma immunity. Can J Gastroenterol Hepatol. 2018;2018:9049252. doi: 10.1155/2018/9049252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carr BI, Akkiz H, Üsküdar O, Yalçın K, Guerra V, Kuran S, Karaoğullarından Ü, Altıntaş E, Özakyol A, Tokmak S, Ballı T, Yücesoy M, Bahçeci Hİ, Ülkü A, Akçam T, Polat KY, Ekinci N, Şimşek H, Örmeci N, Sonsuz A, Demir M, Kılıç M, Uygun A, Demir A, Delik A, Arslan B, Doran F, Yilmaz S, Tokat Y. HCC with low- and normal-serum alpha-fetoprotein levels. Clin Pract (Lond) 2018;15(1):453–464. doi: 10.4172/clinical-practice.1000393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang K, Li M, Qin J, Sun G, Dai L, Wang P, Ye H, Shi J, Cheng L, Yang Q, Qiu C, Jiang D, Wang X, Zhang J. Serological biomarkers for early detection of hepatocellular carcinoma: a focus on autoantibodies against tumor-associated antigens encoded by cancer driver genes. Cancers (Basel) 2020;12(5):1271. doi: 10.3390/cancers12051271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen H, Zhang Y, Li S, Li N, Chen Y, Zhang B, Qu C, Ding H, Huang J, Dai M. Direct comparison of five serum biomarkers in early diagnosis of hepatocellular carcinoma. Cancer Manag Res. 2018;10:1947–1958. doi: 10.2147/CMAR.S167036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang X, Wang T, Zhang KH, Chen SH, He YT, Wang YQ. Simple clinical metrics enhance AFP to effectively identify cirrhotic patients with complicating hepatocellular carcinoma at various AFP levels. Front Oncol. 2020;9:1478. doi: 10.3389/fonc.2019.01478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang T, Zhang KH. New blood biomarkers for the diagnosis of AFP-negative hepatocellular carcinoma. Front Oncol. 2020;10:1316. doi: 10.3389/fonc.2020.01316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang X, Mao M, He Z, Zhang L, Li H, Lin J, He Y, Dai S, Hu W, Liu W. Development and validation of a prognostic nomogram in AFP-negative hepatocellular carcinoma. Int J Biol Sci. 2019;15(1):221–228. doi: 10.7150/ijbs.28720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang H, Xiang Y, Li X, Liu S, Liu L. High lymphocyte-to-monocyte ratio is associated with low α-fetoprotein expression in patients with hepatitis B virus-associated hepatocellular carcinoma. Mol Med Rep. 2020;22(4):2673–2684. doi: 10.3892/mmr.2020.11387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang L, Mo Z, Hu Z, Zhang L, Qin S, Qin X, Li S. Diagnostic value of fibrinogen to prealbumin ratio and gamma-glutamyl transpeptidase to platelet ratio in the progression of AFP-negative hepatocellular carcinoma. Cancer Cell Int. 2020;20:77. doi: 10.1186/s12935-020-1161-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xie DY, Ren ZG, Zhou J, Fan J, Gao Q. 2019 Chinese clinical guidelines for the management of hepatocellular carcinoma: updates and insights. Hepatobiliary Surg Nutr. 2020;9(4):452–463. doi: 10.21037/hbsn-20-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.http://guide.medlive.cn/
- 21.European Association for the Study of the Liver EASL Clinical Practice Guidelines for the management of patients with decompensated cirrhosis. J Hepatol. 2018;69:406–460. doi: 10.1016/j.jhep.2018.03.024. [DOI] [PubMed] [Google Scholar]
- 22.European Association for the Study of the Liver EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67:370–398. doi: 10.1016/j.jhep.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 23.Terrault NA, Lok ASF, McMahon BJ, Chang KM, Hwang JP, Jonas MM, Brown RS, Jr, Bzowej NH, Wong JB. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology. 2018;67(4):1560–1599. doi: 10.1002/hep.29800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tsoris A, Marlar CA. Use of the child pugh score in liver disease. 2021. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 [PubMed]
- 25.Pons F, Varela M, Llovet JM. Staging systems in hepatocellular carcinoma. HPB (Oxford) 2005;7:35–41. doi: 10.1080/13651820410024058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.https://genecards.weizmann.ac.il/v3/cgi-bin/carddisp.pl?gene=AFP
- 27.Chen GG, Ho RL, Wong J, Lee KF, Lai PB. Single nucleotide polymorphism in the promoter region of human alpha-fetoprotein (AFP) gene and its significance in hepatocellular carcinoma (HCC) Eur J Surg Oncol. 2007;33(7):882–886. doi: 10.1016/j.ejso.2007.02.036. [DOI] [PubMed] [Google Scholar]
- 28.Suriapranata IM, Sudania WM, Tjong WY, Suciptan AA, Gani RA, Hasan I, Sanityoso A, Budihusodo U, Miskad UA, Akil F, Lelosutan SA, Martamala R, Yusuf I, Lesmana LA, Sulaiman A, Tai S. Alpha-fetoprotein gene polymorphisms and risk of HCC and cirrhosis. Clin Chim Acta. 2010;411(5–6):351–358. doi: 10.1016/j.cca.2009.11.030. [DOI] [PubMed] [Google Scholar]
- 29.Zhou L, Liu J, Luo F. Serum tumor markers for detection of hepatocellular carcinoma. World J Gastroenterol. 2006;12(8):1175–1181. doi: 10.3748/wjg.v12.i8.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee CW, Tsai HI, Lee WC, Huang SW, Lin CY, Hsieh YC, Kuo T, Chen CW, Yu MC. Normal alpha-fetoprotein hepatocellular carcinoma: are they really normal? J Clin Med. 2019;8(10):1736. doi: 10.3390/jcm8101736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Balogh J, Victor D, 3rd, Asham EH, Burroughs SG, Boktour M, Saharia A, Li X, Ghobrial RM, Monsour HP., Jr Hepatocellular carcinoma: a review. J Hepatocell Carcinoma. 2016;3:41–53. doi: 10.2147/JHC.S61146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Poddar N, Avezbakiyev B, He Z, Jiang M, Gohari A, Wang JC. Hepatocellular carcinoma presenting as an incidental isolated malignant portal vein thrombosis. J Gastrointest Cancer. 2012;43(3):486–489. doi: 10.1007/s12029-010-9235-z. [DOI] [PubMed] [Google Scholar]
- 33.Hsu CY, Lee YH, Huang YH, Hsia CY, Su CW, Lin HC, Lee RC, Chiou YY, Lee FY, Huo TI, Lee SD. Ascites in patients with hepatocellular carcinoma: prevalence, associated factors, prognostic impact, and staging strategy. Hepatol Int. 2013;7(1):188–198. doi: 10.1007/s12072-011-9338-z. [DOI] [PubMed] [Google Scholar]
- 34.Carr BI, Guerra V. Thrombocytosis and hepatocellular carcinoma. Dig Dis Sci. 2013;58(6):1790–1796. doi: 10.1007/s10620-012-2527-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lim S, Lee S, Lim JY, Park JS, Seong JS, Chang WS, Han KH, Choi HJ. Hepatocellular carcinoma specific graded prognostic assessment can predict outcomes for patients with brain metastases from hepatocellular carcinoma. J Neurooncol. 2014;120(1):199–207. doi: 10.1007/s11060-014-1546-7. [DOI] [PubMed] [Google Scholar]
- 36.Liu G, Ouyang Q, Xia F, Fan G, Yu J, Zhang C, Wang D. Alpha-fetoprotein response following transarterial chemoembolization indicates improved survival for intermediate-stage hepatocellular carcinoma. HPB (Oxford) 2019;21(1):107–113. doi: 10.1016/j.hpb.2018.06.1800. [DOI] [PubMed] [Google Scholar]
- 37.Zhang N, Gu J, Yin L, Wu J, Du MY, Ding K, Huang T, He X. Incorporation of alpha-fetoprotein(AFP) into subclassification of BCLC C stage hepatocellular carcinoma according to a 5-year survival analysis based on the SEER database. Oncotarget. 2016;7(49):81389–81401. doi: 10.18632/oncotarget.13232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gomaa AI, Al-Khatib A, Abdel-Razek W, Hashim MS, Waked I. Ascites and alpha-fetoprotein improve prognostic performance of Barcelona Clinic Liver Cancer staging. World J Gastroenterol. 2015;21(18):5654–5662. doi: 10.3748/wjg.v21.i18.5654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Akuta N, Suzuki F, Kobayashi M, Hara T, Sezaki H, Suzuki Y, Hosaka T, Kobayashi M, Saitoh S, Ikeda K, Kumada H. Correlation between hepatitis B virus surface antigen level and alpha-fetoprotein in patients free of hepatocellular carcinoma or severe hepatitis. J Med Virol. 2014;86(1):131–138. doi: 10.1002/jmv.23790. [DOI] [PubMed] [Google Scholar]
- 40.Chen DS, Sung JL. Relationship of hepatitis B surface antigen to serum alpha-fetoprotein in nonmalignant diseases of the liver. Cancer. 1979;44(3):984–992. doi: 10.1002/1097-0142(197909)44:3<984::AID-CNCR2820440328>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 41.Ding Y, Liu K, Xu Y, Zhao Q, Lou S, Xiang X, Yan L, Cao Z, Xie Q, Zhu C, Bao S, Wang H. Combination of inflammatory score/liver function and AFP improves the diagnostic accuracy of HBV-related hepatocellular carcinoma. Cancer Med. 2020;9(9):3057–3069. doi: 10.1002/cam4.2968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Feng H, Li B, Li Z, Wei Q, Ren L. PIVKA-II serves as a potential biomarker that complements AFP for the diagnosis of hepatocellular carcinoma. BMC Cancer. 2021;21(1):401. doi: 10.1186/s12885-021-08138-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Si YQ, Wang XQ, Fan G, Wang CY, Zheng YW, Song X, Pan CC, Chu FL, Liu ZF, Lu BR, Lu ZM. Value of AFP and PIVKA-II in diagnosis of HBV-related hepatocellular carcinoma and prediction of vascular invasion and tumor differentiation. Infect Agent Cancer. 2020;15(1):70. doi: 10.1186/s13027-020-00337-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hanazawa T, Fukami Y, Osawa T, Kurahashi S, Matsumura T, Saito T, Komatsu S, Kaneko K, Tsuzuki T, Sano T. A case of resected hepatocellular carcinoma with gallbladder metastasis. Surg Case Rep. 2021;7(1):145. doi: 10.1186/s40792-021-01222-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gou Q, Fu S, Xie Y, Zhang M, Shen Y. Treatment and survival patterns of primary adenosquamous carcinoma of the liver: a retrospective analysis. Front Oncol. 2021;11:621594. doi: 10.3389/fonc.2021.621594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Abdelgawad IA. Epithelial cell adhesion molecule mRNA can be a potential marker to predict metastasis in hepatocellular carcinoma patients. Asian Pac J Cancer Prev. 2020;21(3):861–866. doi: 10.31557/APJCP.2020.21.3.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shiraki T, Ishizuka M, Kubota K, Kato M, Matsumoto T, Mori S, Shimizu T, Aoki T. An elevated neutrophil-to-lymphocyte ratio predicts a poor postoperative survival in primary hepatocellular carcinoma patients with a normal preoperative serum level of alpha-fetoprotein. Surg Today. 2019;49(8):661–669. doi: 10.1007/s00595-019-01781-1. [DOI] [PubMed] [Google Scholar]
- 48.Bannaga A, Arasaradnam RP. Neutrophil to lymphocyte ratio and albumin bilirubin grade in hepatocellular carcinoma: a systematic review. World J Gastroenterol. 2020;26(33):5022–5049. doi: 10.3748/wjg.v26.i33.5022. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Patients’ demographics and the association between serum AFP levels and other tumor markers in patients with AFP negative and AFP positive.
Additional file 2. Distribution of AFP in patient groups and the comparison of serum AFP levels among patient groups and among clinical pathologic features.
Data Availability Statement
Data is available by contacting Huayi Huang at Henry.Huang@Mindray.com.


