Abstract
Stellate ganglion nerve blockade (SGNB) is a vital tool in our armamentarium for the treatment of various chronic pain syndromes. SGNB can be performed using the traditional landmark-based approach, or with image guidance using either fluoroscopy or ultrasound. In this review, we systematically analyzed reported SGNB-related complications between 1990 and 2018. Seven databases were queried for SGNB between January 1, 1990 and November 27, 2018. Search results of the complications associated with SGNB were reported as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations. Out of a total of 1909 articles, 67 articles met our inclusion criteria, yielding 260 cases with adverse events. In 134 of the 260 (51.5%) cases, SGNB was performed with image guidance. Sixty-four (24.6%) and 70 (26.9%) of the complication cases reported the use of ultrasound and fluoroscopy guidance, respectively. One hundred and seventy-eight (68.4%) patients had medication-related or systemic side effects, and 82 (31.5%) had procedure-related or local side effects. There was one report of death due to massive hematoma leading to airway obstruction. There was one case report of quadriplegia secondary to pyogenic cervical epidural abscess and discitis following an SGNB. Complications following SGNB have been reported with both landmark-based techniques and with imaging guidance using fluoroscopy or ultrasound. In our systematic review, most adverse events that were reported occurred during or shortly after SGNB. Vigilance, American Society of Anesthesiologists standard monitors for conscious sedation, and accessibility to resuscitation equipment are vital to the safe performance of SGNB.
INTRODUCTION
The number of interventional pain procedures performed in the USA has markedly increased from year 2000 to year 2014.1 With concomitant increases in interventional pain management procedures and indications for stellate ganglion nerve blocks (SGNBs), it can be presumed that the SGNBs are performed at an increasing frequency. SGNBs are an important tool in our armamentarium for the management of a variety of chronic pain syndromes, including complex regional pain syndrome (CRPS), postherpetic neuralgia, migraine, facial pain syndromes, and postmastectomy pain syndromes.2–4 SGNBs are also reported to improve patient outcomes in drug-refractory ventricular arrhythmias, hot flashes associated with menopause, and some forms of post-traumatic stress disorder (PTSD).5–7
The stellate ganglion is irregularly star-shaped and is formed by the fusion of the inferior cervical and first thoracic ganglia with sometimes varying contributions from subsequent thoracic ganglia.8 It lies at the base of the seventh cervical transverse process and neck of the first rib, making the block challenging because of the critical structures in the vicinity and the potential for collateral damage during the procedure.9
SGNB was originally performed using anatomic landmarks,10 and subsequently using fluoroscopy11 or ultrasound guidance.12 The primary aim of our study was to perform a systematic review of reported complications associated with SGNB between 1990 and 2018. The secondary aim was to analyze the impact of imaging guidance.
METHODS
Protocol
The protocol was developed by two authors (VG and HS) at their respective academic center’s department of anesthesia and pain medicine. An information specialist (CLH) was involved in the question development (population, intervention, comparison, outcome, and timeframe (PICOT)), search, article retrieval, and reporting. The review was performed and reported using the guidelines set by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses.13 Due to significant heterogeneity of cases in published reports, we pursued a systematic review without meta-analysis.
Eligibility criteria
Studies were included if they contained information relating to complications, adverse effects, or toxicity associated with stellate ganglion blockade. Non-English publications, conference abstracts with insufficient data, and opinion pieces were excluded. References from SGNB review articles analyzing complications were considered if they met the inclusion criteria.
Search strategy
The information specialist (CLH) conducted searches in the following databases: Ovid MEDLINE, Elsevier/Embase, Elsevier/Scopus, Wiley/Cochrane Library, Clarivate/Web of Science, EBSCO/Cumulative Index to Nursing and Allied Health Literature, and ClinicalTrials.gov. Publication dates were limited to January 1, 1990-November 27, 2018, the date all searches were completed. The time frame was selected to reflect contemporary clinical practice and the availability of procedural details in published reports. All search strategies are available in online supplementary material appendix A.
Study selection
All citations were exported into EndNote and duplicates were removed. Titles and abstracts of retrieved citations were assessed by one reviewer (VG) for relevance. A second reviewer (HS) reviewed all excluded titles and abstracts, and discrepancies were then resolved by consensus. The full texts of the records thus selected were then screened by two independent reviewers (VG, HS), and disagreements were again resolved by consensus.
Data collection
The prespecified variables that were extracted from the included articles were as follows: indication for SGNB, laterality of the block, use of imaging guidance, aspiration test, contrast use, volume of injectate, type, and frequency of reported complication. Clinical outcomes following SGNB when reported were also collected. Microsoft Excel (V.2016, Microsoft, Washington) was used for data extraction and collection. The data collection forms were piloted using a small data set to ensure validity and reliability.
Overview of the procedure
SGNB was originally performed by the classic landmark-based or paratracheal approach. More recently, imaging guidance using fluoroscopy or ultrasound has become standard of care. The technique used by a particular provider depends on their training, expertise and available resources. Common medications used in SGNB include a variety of local anesthetics such as bupivacaine, lidocaine or mepivacaine, sometimes combined with steroid medication depending on the physician’s preference. The patient is positioned supine with the neck extended and the head may be turned to the opposite side during the procedure. Intravenous access is commonly obtained with physiologic monitoring during and shortly after the procedure. Relevant anatomy for the landmark-based approach on the right side and ultrasound-guided approach on the left side is shown in figure 1. Figures 2 and 3 illustrate the fluoroscopy-guided and ultrasound-guided approaches to SGNB.
Figure 1.
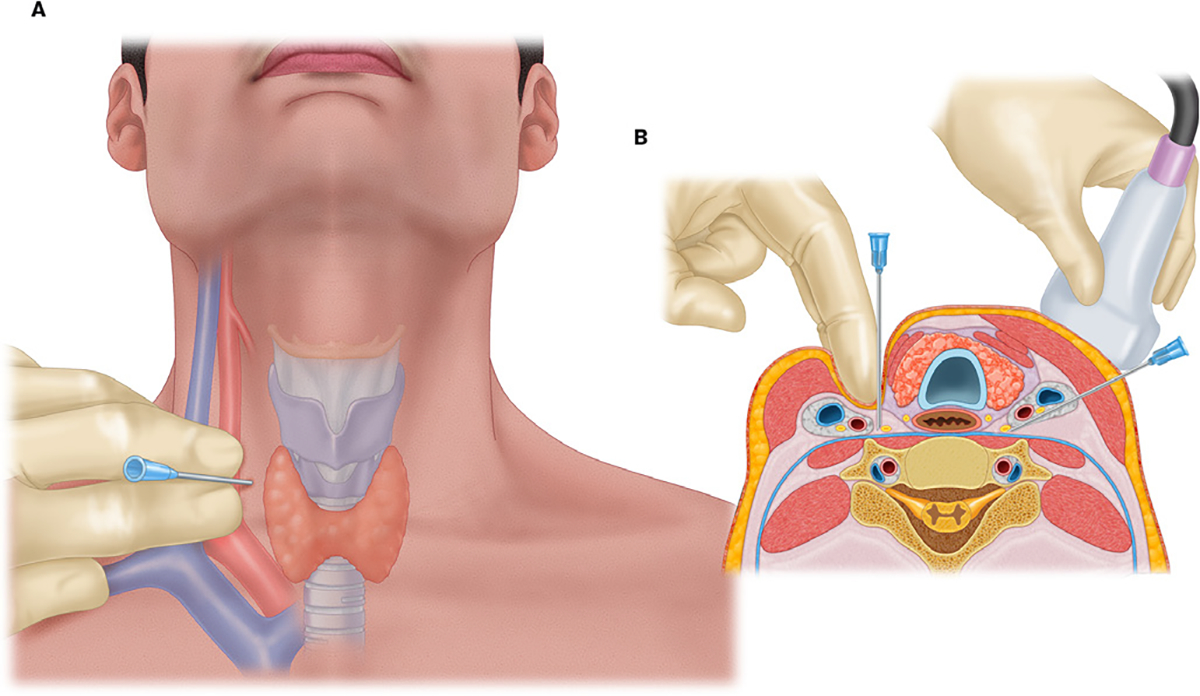
Panel A illustrates surface anatomy for stellate ganglion nerve block by the classic approach. The cricoid cartilage is palpated, and the vascular bundle is displaced laterally. The needle tip is inserted in a plane perpendicular to the insertion point on the skin. Panel B illustrates the cross section at the level of C6 showing the classic approach on the right side of the neck and ultrasound-guided approach on the left. Note the needle track is lateral to the vascular bundle and under the major vessels using inplane approach under ultrasound guidance. Proximity to various nerves, vessels, thyroid tissue, and esophagus can be appreciated in a cross-sectional view.
Figure 2.
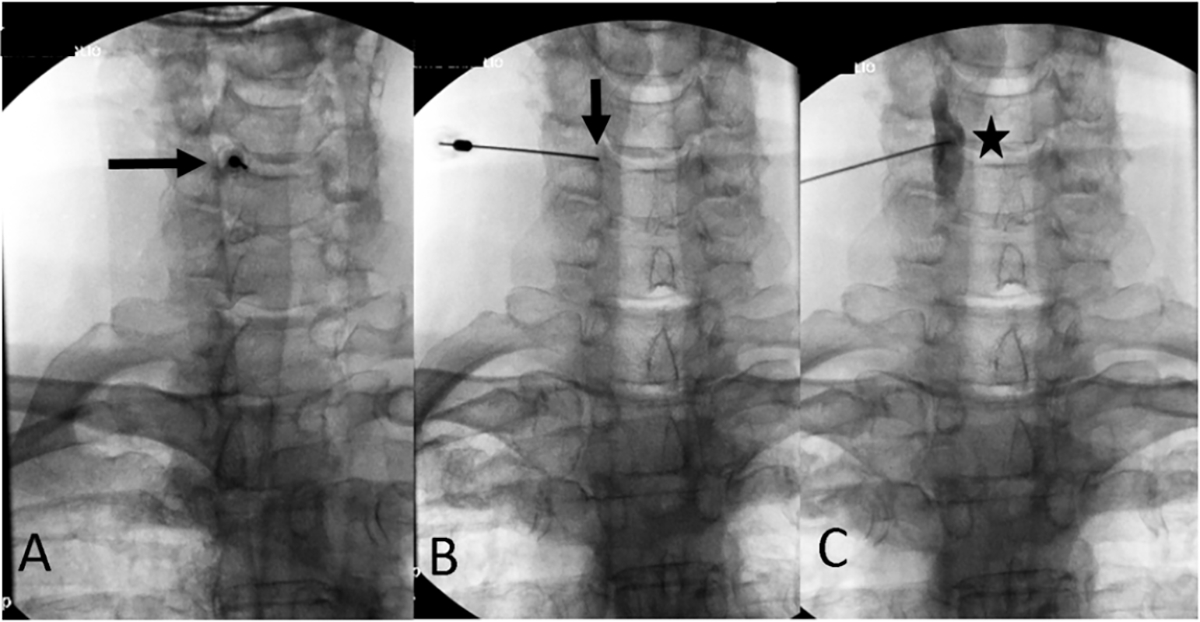
Fluoroscopy-guided oblique approach to stellate ganglion nerve block. Panel A illustrates the C5–C6 disc interspace in the right anterior oblique view. The needle is inserted coaxially to the beam targeting the C6 uncinate process (arrow). Panel B illustrates the final needle position (arrow) in the posteroanterior view. Panel C shows the contrast injection being performed to rule out vascular uptake. Contrast is seen to spread along the longus colli muscle in a craniocaudal fashion (star).
Figure 3.
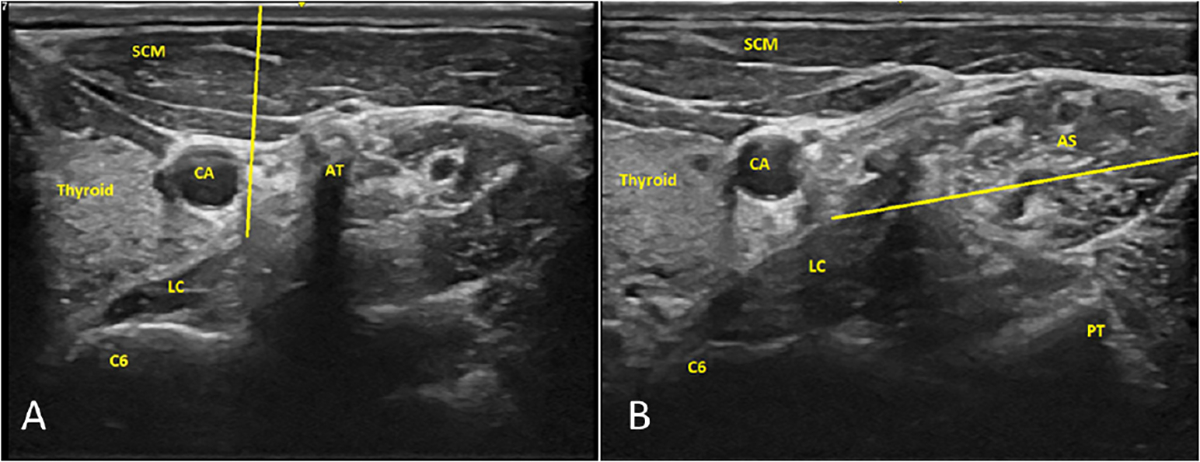
Ultrasound-guided imaging approach to stellate ganglion nerve block. Panel A illustrates the potential needle track (yellow line) with out-of-plane imaging. Panel B illustrates the potential needle track (yellow line) with inplane imaging. The ultrasound probe is placed on the right side of the neck at the C6 vertebral body level in the images. The yellow line is the trajectory for inplane needle ending at the prevertebral fascia covering the longus colli. AS, anterior scalene; AT, anterior tubercle; C6, cervical vertebra 6; CA, carotid artery; LC, longus colli muscle; PT, posterior tubercle; SCM, sternocleidomastoid muscle.
Complications related to SGNB can be broadly divided into systemic and local complications. Systemic complications are a result of medication entering an unintended space or a generalized reaction of the body such as an allergic reaction. Local complications refer to complications associated with unintentional injury to a structure in the path of the needle (online supplementary material appendix B). Narrative details of the complications for individual patients are described when available.
RESULTS
Study selection
Our initial literature search resulted in a total of 4812 studies. This resulted in a total of 1909 publications after duplicates were removed. Title and abstract screening was performed on these 1909 articles. The initial screen yielded a total of 513 articles, the full texts of which were retrieved for review. A total of 67 articles met the final inclusion criteria. A total of 260 cases with adverse events were reported in these 67 articles (figure 4). These complications are summarized in tables 1 and 2.
Figure 4.
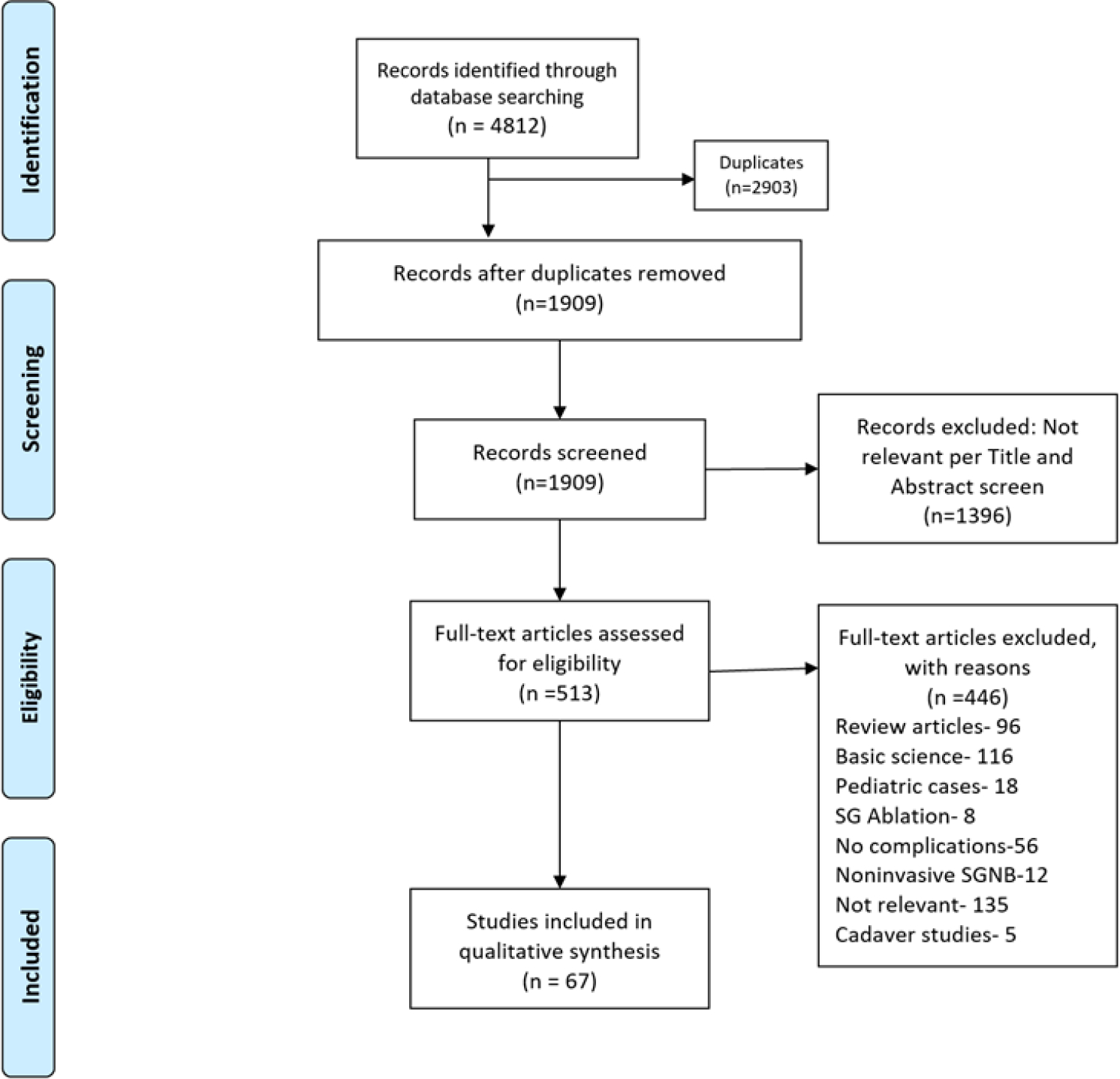
Flow chart of the process of literature search and extraction of studies meeting the inclusion criteria. SGNB, stellate ganglion nerve block.
Table 1.
Systemic complications identified in our review of SGNB-related complications reported in the literature
| Complication | Reported cases(n) | uSG guidance | Fluoroscopy guidance |
|---|---|---|---|
|
| |||
| Systemic complications | |||
|
| |||
| Hoarseness* | 73 | 32 | 12 |
| Light-headedness | 20 | 4 | |
| Hypertension | 13 | ||
| Brachial plexus block | 12 | 1 | 9 |
| Dysphagia | 11 | 9 | |
| Cough | 7† | 3 | 1 |
| Subdural block/intraspinal blockade | 5 | ||
| Seizures | 5 | 3 | |
| Transient locked-in syndrome | 4 | ||
| Dyspnea and respiratory depression | 4 | 2 | 1 |
| Migraine and headaches | 4 | ||
| Persistent ptosis | 3 | 2 | |
| Bilateral sympathetic blockade | 2 | ||
| Decreased contralateral blood flow | 2 | ||
| Contralateral Horner’s syndrome | 2 | 1 | |
| Visual hallucinations | 1 | ||
| Bloodshot conjunctiva | 1 | ||
| Myoclonus | 1 | ||
| Arm numbness | 1 | 1 | |
| Reading difficulty | 1 | ||
| Bilateral Horner’s syndrome | 1 | ||
| Lower limb edema | 1 | 1 | |
| Transient global amnesia | 1 | 1 | |
| IJ vein thrombosis | 1 | ||
| Allergic reaction | 1 | 1 | |
| Hemidiaphragmatic paralysis | 1 | ||
Two patients under SGNB with both ultrasound and fluoroscopy guidance.
One patient developed a transient cough, while the other six developed a persistent cough.
IJ, internal jugular; SGNB, stellate ganglion nerve block; USG, ultrasonography.
Table 2.
Local complications identified in our review of SGNB-related complications reported in the literature
| Complication | Reported cases(n) | USG guidance | Fluoroscopy guidance |
|---|---|---|---|
|
| |||
| Local complications | |||
|
| |||
| Hematoma | 41 | 11 | 23 |
| Blood aspiration | 20* | 8 | |
| Intrathoracic bleeding† | 7 | 6 | |
| Pneumothorax | 3 | 1 | |
| Infection | 3 | ||
| Bradycardia | 2 | ||
| Dural puncture | 1 | ||
| Hemomediastinum | 1 | ||
| Sinus arrest due to vasovagal | 1 | ||
| reflux | |||
| Transient neurologic injury | 1 | 1 | |
| LMA puncture | 1 | ||
| Asystolic cardiac arrest | 1 | ||
| Total (systemic and local) | 260 | 64 (24.6%) | 70 (26.9%) |
Among these 20 patients, 12 patients underwent SGNB by landmark-based technique and 8 patients with fluoroscopy guidance.
One patient was found to have an intrathoracic and retrotracheal hematoma on autopsy.
LMA, laryngeal mask airway; SGNB, stellate ganglion nerve block; USG, ultrasonography.
Patient characteristics and indications for SGNB
Among the 260 cases of complications associated with SGNB, 36 (13.8%) were in women, 24 (9.2%%) in men, and in 200 (76.9%) cases gender information was not available as they were a part of a larger series. SGNB was performed for a variety of pain-related indications such as CRPS, brachial plexus injury, facial pain, shoulder and arm pain, postherpetic neuralgia, neck pain, and for postoperative pain control. SGNB was also performed for vascular indications such as Raynaud syndrome, central retinal artery occlusion, thromboangiitis obliterans (Buerger’s disease), hearing loss, and progressive systemic sclerosis.14–17 There were also reports of SGNB complications among volunteers.18
Image guidance for SGNB
Out of the 260 total complications, 126 (48.5%) were performed with landmark-only guidance for SGNB. Seventy (26.9 %) cases were performed using fluoroscopy and were all published after the year 2000.19–23 There were 64 (24.6%) cases of SGNB-related complications in procedures using ultrasound imaging, all of which were published in 2010 or later.24–27 There were three cases with complications in a study report that used a combination of fluoroscopy and ultrasound in performing SGNB.28 Some case reports did not clearly mention the technical details of the block or the approach that was taken.
Systemic adverse events
The most commonly reported systemic adverse events are hoarseness and light-headedness (73 and 20 cases, respectively). Many of the reports are from large series, and individual patientlevel details are unavailable.
Severe hypertension
Kimura et al29 presented a case series of seven patients who developed severe hypertension after stellate ganglion blockade. All the blocks were performed via the landmark-based approach using 5 mL mepivacaine. Some patients presented with symptoms of headaches along with an increase in blood pressure. The authors postulated that the increase in blood pressure was the result of local anesthetic spread along the carotid sheath resulting in vagal block.
Transient cough
Atici and Akoz30 reported a case of transient cough developing in a 69-year-old woman who received her fourth SGNB for a diagnosis of CRPS. The cough lasted for 1–2 hours. The patient had subsequent blocks that resulted in similar transient coughing episodes, even with reduced local anesthetic volumes. The postulated cause was recurrent laryngeal nerve paralysis. This patient’s treatment was changed to medication management, and SGNBs were discontinued.
Persistent cough
Naveira and Rauck31 reported two cases of persistent cough following SGNBs performed with 10 mL 0.5% bupivacaine via the landmark-based approach.
Both Naveira and Rauck31 and Atici and Akoz30 postulated that the coughing attacks were a result of recurrent laryngeal nerve blockade leading to aspiration of saliva into the trachea. All three cases complicated by cough involved right-sided SGNBs. Atici and Akoz30 hypothesized that cough might be a more common occurrence after right-sided SGNB because of the anatomic placement of recurrent laryngeal nerves.
Subdural block and intrathecal block
There were four case reports where the authors believe it was a delayed subdural block,32–35 and one reported a case of an intraspinal block. Balaban et al32 described the case of a 21-year-old man who underwent a right-sided SGNB for CRPS with a 22 G needle via the landmark-based approach. The patient had undergone 11 previous uneventful SGNBs. After negative aspiration test, a 2 mL test dose of prilocaine was administered uneventfully. Subsequently, a solution of 10 mL prilocaine was administered. After 25 min the patient was noted to have severe stridor, apnea and then paralysis of all four extremities. The patient recovered in 3 hours with supportive care. Bruyns et al33 reported a case of a 38-year-old woman who underwent a right-sided SGNB landmark-based approach with 10 mL 0.5% bupivacaine which was complicated by a subdural block. Within 1–2 min of completion of the block, the patient complained of tingling in both upper extremities along with nausea. She subsequently lost consciousness and stopped breathing. The patient required respiratory support for approximately 3 hours. Leong and Mackey34 described a delayed subdural block in a patient who underwent a landmark-based, right-sided SGNB for CRPS with 13 mL of 0.25% bupivacaine. Saruki et al35 described a 56-year-old man with right shoulder pain who underwent a right-sided SGNB with 6 mL of 1% mepivacaine, following a negative aspiration test. The patient complained of heaviness in the left leg, followed by a similar sensation in the opposite leg and upper extremity; 50 min after SGNB, he experienced 20 s of convulsions every 10 min. The patient recovered without sequelae in 4 hours. Another intraspinal block was reported by Sari and Aydin.36 In this instance a 44-year-old woman underwent a right-sided SGNB for a diagnosis of CRPS. The patient experienced respiratory arrest in 4–5 min after completion of the block. She required mechanical ventilation for 2 hours and was discharged home in 24 hours. Among the four cases with subdural blockade, two patients had a negative aspiration test. Two of the cases had delayed onset of subdural block. All cases were done via a landmark-based technique using a moderate volume of local anesthetic injected. On average, most patients who required ventilatory support needed it for 3–4 hours, an interval consistent with the duration of local anesthetic.
Seizures
Eyigor et al20 reported a case, the only pediatric case we came across in our review, of intra-arterial injection and grand mal seizures in a 16-year-old girl undergoing SGNB. The patient received a right-sided stellate ganglion blockade for CRPS under fluoroscopy guidance. After appropriate contrast spread and negative aspiration test, a 5 mg lidocaine test dose was administered which resulted in grand mal seizures, loss of consciousness, and respiratory arrest. The patient was treated appropriately during the acute event and proceeded to complete the remaining five SGNBs in the series. Mahli et al16 reported two cases of seizures after SGNB. A 28-year-old woman with Raynaud disease and a 31-year-old man with thromboangiitis obliterans (Buerger’s disease) who underwent SGNB via the landmark-based approach with previous uneventful blocks both experienced seizures as a complication. The first patient had a negative aspiration test and then received a test dose. Blood was noted during the second aspiration. She subsequently had seizures after needle redirection. The authors noted that she fully recovered within 2 min. The second patient had a negative aspiration test but developed seizures once the medication was injected. The patient was successfully resuscitated without sequelae and went on to complete his series of 10 SGNBs. Rastogi and Tripathi26 described a patient who underwent a left-sided, ultrasound-guided stellate block for facial pain. After appropriate needle positioning, 10 mL 0.5% bupivacaine was injected; this resulted in seizures and was followed by cardiac arrest. These two cases demonstrate that an aspiration test is not foolproof and that complications can occur even using image guidance techniques.
In contrast, Fujiwara et al24 reported a rare case of accidental arterial local anesthetic injection while performing SGNB under ultrasound guidance with only 2 mL 1% mepivacaine. In this case, the physician realized that there was an arterial injury with the first pass of the needle. They withdrew the needle and waited 5 min and reattempted the block. The authors proposed that the patient’s known enlarged thyroid made the area more vascular and advised extreme caution when reattempting to complete SGNB after an initial arterial puncture. The patient experienced convulsions with the injections of local anesthetic and was treated with midazolam and ventilatory support. The patient regained consciousness in 20 min and was discharged home without any long-term sequelae. The seizures described in the cases above were a result of unintentional placement of the needle tip within an artery, or because of injury to the artery itself during the procedure. The symptoms were a result of local anesthetic being introduced into the vasculature and are thus classified under systemic complications. It must be noted that none of the seizures were captured on electroencephalography and the details of postictal state are not well described in the reports.
Transient locked-in syndrome
Transient locked-in syndrome, paralysis of all voluntary muscles except those controlling eye movements, was described as being associated with SGNB in four case reports.37–40 Chaturvedi and Dash39 described a case of transient locked-in syndrome during an SGNB in a 25-year-old male patient undergoing a right-sided SGNB without image guidance for brachial plexus injury. After the needle was positioned using the landmark-based approach, and the aspiration test was negative, the patient received a total of 2 mL 1% lidocaine when blood was noted in the injecting syringe. Injection of the remainder of the solution was aborted; however, the patient had already developed transient locked-in syndrome. He regained consciousness in 2 min, and subsequently underwent an additional six SGNBs without any sequelae. Dukes and Alexander37 described a case of transient locked-in syndrome following a left-sided SGNB, performed without image guidance, in a 47-year-old woman for Raynaud syndrome. After the needle was positioned and the aspiration test was negative, a test dose of 0.5 mL 0.25% bupivacaine was injected uneventfully. After the subsequent 2.5 mL of 0.25% bupivacaine was administered, the patient suddenly developed transient locked-in syndrome. Although she was unable to vocalize, she was able to blink her eyes. The patient was supported with facemask ventilation, and the team performed the block 30 min later without incidence. Tüz et al38 reported a case of transient locked-in syndrome with a local anesthetic solution of 10 mL prilocaine administered after negative aspiration test during an SGNB. The approach or image guidance was not specified. The patient was able to respond by blinking their eyes, and both vocal cords were noted to be in complete abduction. Corsaro et al40 reported the case of a 45-year-old man who underwent a landmark-based approach stellate ganglion blockade with 8–10 mL 0.35% bupivacaine and suffered from transient locked-in syndrome. The patient was provided with ventilatory support and recovered in 2 hours without sequelae. All the four cases of SGNB complicated by transient locked-in syndrome were performed without image guidance. Although transient locked-in syndrome is commonly reported in patients with brain stem stroke, none of the reported patients had permanent neurologic deficits. The reported symptoms differ from classic presentations in patients with brain stem stroke and may represent possible vasospasm or even panic attack, but the exact etiology is unknown. All the patients recovered uneventfully with supportive care, and the first two patients completed their planned series of SGNBs uneventfully.
Dyspnea
Kim22 reported a case of respiratory depression in a 43-year-old woman after a right-sided SGNB with fluoroscopy guidance for CRPS. The block was performed with a low dose of 3 mL 0.25% bupivacaine. The patient complained of difficulty breathing and required intubation and ventilation support for several hours. Jadon19 reported a similar case of a 60-year-old woman who developed shortness of breath after completion of SGNB with a larger volume of 10 mL 1% lidocaine mixed with methylprednisolone. The patient was observed and did not need supportive treatment.
Migraine headaches
Migraine headaches41 42 as a complication of SGNB were described in two case reports. Fortunately, the headache symptoms of both patients improved over time.
Persistent ptosis
Lake and Puvanachandra43 presented a case of persistent ptosis after SGNB. A 25-year-old woman underwent an SGNB by the landmark-based approach with 10 mL of 0.5% bupivacaine for chronic shoulder pain. The patient had a successful block and developed Horner’s syndrome on the treatment side. She continued to have unilateral ptosis, conjunctival hyperemia, and erythema of the lids without miosis and anhidrosis. The patient’s symptoms improved with a 2-week course of non-steroidal anti-inflammatory medication.
Bilateral sympathetic blockade
Wallace and Milholland44 presented two cases of SGNB that resulted in bilateral nerve blockade. The first patient experienced bilateral sympathetic blockade. The patient complained of contralateral shoulder pain and eye-watering. The second patient developed stridor, presumably secondary to bilateral recurrent laryngeal nerve block. The stridor resolved in 4 hours. These cases resulting in symptoms on both sides were completed with 15 mL of 0.25% bupivacaine.
Reduced blood flow on the contralateral side of SGNB
Omote et al14 reported two cases in which SGNB was performed on patients with Raynaud phenomenon for the relief of reduced finger perfusion and resultant cyanosis and ulceration. Although both experienced increased blood flow in the affected hand after SGNB on that side, they exhibited the opposite effect in the contralateral hand. This phenomenon did not occur in healthy volunteers. The authors postulated that this effect was due to stimulation of the stellate ganglion on the opposite side or because of a “steal” phenomenon. The affected patients in this study did not have untoward effects, and the change in blood flow reverted to baseline 90 min after the block.
Visual hallucinations
Kurimoto et al15 presented a rare case of visual hallucinations lasting 10 days after SGNB was performed for central retinal artery occlusion. The authors attributed the hallucinations to the presence of Charles Bonnet syndrome triggered by the SGNB. The hallucinations were of a scene familiar to the patient and resolved over several days. The authors postulated that the release phenomenon threshold was reduced for this patient because of coexisting central nervous system disease; in this case, MRI revealed ischemic changes from microemboli in the frontal lobe.
Myoclonus
Watanabe et al reported myoclonus in a 55-year-old woman with deafness and tinnitus who underwent a right-sided SGNB. This was her 13th SGNB without image guidance. The patient reported tingling and numbness in the fifth finger and developed myoclonic movements. The movements subsided spontaneously about an hour after the procedure. The authors postulated that the myoclonus could have been a result of neuraxial block from the medication, nerve root irritation by the medication or needle, intra-arterial injection, or altered blood flow in the extremity as a result of the SGNB.
Bilateral Horner’s syndrome
Manchikanti45 presented a case of SGNB resulting in bilateral Horner’s syndrome after a large volume of 15 mL 0.5% lidocaine was used during the procedure.
Allergic reaction
Allergic reaction to local anesthetic is rare. Espinar González et al25 reported a case of allergic reaction to bupivacaine used in a second SGNB. The patient developed symptoms of neck swelling, difficulty swallowing, and stridor after a few hours of the block. The initial diagnosis was of cervical hematoma. In their report, the authors explained that the surgeon used bupivacaine in the surgical field, which led to severe desaturation and hypotension in the operating room. The patient underwent a tracheostomy and required intensive care unit admission for treatment and recovery.
Hemidiaphragmatic paralysis/phrenic nerve injury
Kay et al46 completed a study in 50 patients receiving SGNB via the landmark-based approach with 12 mL 0.25% bupivacaine. One patient developed hemidiaphragmatic paralysis.
Local adverse events
The most common local adverse event is hematoma formation. Many of the cases are from large series, and individual case details are not reported.
Local blood aspiration
The aspiration test is performed before injecting medication to make sure no blood or clear fluid is aspirated, thereby ensuring the needle tip is not in a vessel or in the intrathecal space. Karaman21 reported a total of 20 instances of blood aspirations in their retrospective study comparing SGNB via the landmark-based technique with SGNB with fluoroscopic guidance. There were a total of 12 instances of positive blood aspiration with the landmark-based approach (out of 223 SGNBs) vs 8 instances in the fluoroscopy group (out of 197 SGNBs). They concluded there was no statistical difference between the two groups.
Bleeding and hematoma formation
We identified several cases of hematoma resulting from SGNB. Notably, five patients had significant adverse events with hematoma formation. All five patients had a delayed presentation, underwent tracheostomy, prolonged hospitalization, and approximately 30+ days to stoma closure. Mishio et al17 reported a 62-year-old woman undergoing a fourth SGNB block without image guidance who experienced throat discomfort 30 min after the procedure. Two hours after the procedure, she developed dyspnea, painful swallowing, swelling in the anterior neck and chest, and stridor. The patient underwent tracheostomy, which was complicated by methicillin-resistant Staphylococcus aureus infection. Her tracheostomy stoma was closed after 33 days. Okuda et al47 reported a similar complication in a 60-year-old man who underwent an SGNB for shoulder and neck pain. This patient had a history of nine previous uneventful blocks. SGNB was completed without image guidance. Subsequently, 2.5 hours after the block, the patient’s voice became hoarse. After 3.5 hours, he then developed dyspnea and neck pain and required an emergency tracheostomy; the stoma was closed 37 days later. Takanami et al48 reported a case of a 53-year-old woman who underwent an SGNB for left facial pain. She subsequently developed a retropharyngeal and cervicomediastinal hematoma from bleeding of the ascending cervical artery resulting in airway obstruction. The patient required embolization, thoracotomy, and neck exploration, and had a 30-day hospital course. Uchida et al49 reported a case of a 44-year-old man who developed neck and mediastinal venous hematoma, ultimately requiring tracheostomy, after a left-sided SGNB for lower lip pain. Kashiwagi et al50 described a 29-year-old woman who described pain and dyspnea following landmark-guided SGNB for facial nerve palsy. She was found to have airway obstruction from post-tracheal hematoma on autopsy. All five patients required emergent airway management. None of the five patients had a history of bleeding disorders or medications that would alter their coagulation profile.
Dural puncture
Stannard et al51 described a 40-year-old woman with left arm pain who underwent a left-sided SGNB via the landmark-based technique. After needle positioning, the aspiration test revealed clear fluid presumed to be cerebrospinal fluid (CSF). The procedure was aborted, and the patient did not experience long-term side effects.
Pneumothorax
SGNB is most often completed at the C6 level for feasibility and to avoid puncture of the pleura. During our review we came across only two reports, both reported by Karaman, of pneumothorax as a complication of SGNB.21 Karaman reported both in their retrospective study comparing landmark-based SGNB performed with fluoroscopic approach; both cases occurred in the landmark-based approach group (n=223). The author concluded that stellate ganglion blockade was a safe procedure when performed by an experienced person.
Local infections
Masuda et al52 reported a case of a 68-year-old man who underwent a left-sided SGNB for left facial paralysis. The patient developed delayed complication of cervical abscess and spondylitis, ultimately resulting in C6–C7 fusion. Vadodaria et al53 presented a case of discitis after SGNB in a patient who was on concomitant oral steroids. The patient subsequently developed quadriplegia. Shimada et al54 reported the case of a 65-year-old man who developed spondylitis of C5 and C6 3 weeks after a right-sided SGNB. The patient had had four previous uneventful blocks. This patient was on systemic steroids, possibly increasing the risk of an infection in the periprocedure period. All three patients with infectious complications had a late presentation and long-term sequelae.
Miscellaneous local complications
Saxena et al55 reported a case of bradycardic cardiac arrest after a landmark-based SGNB in a 29-year-old woman for right shoulder and hand pain. The patient received an uneventful 1 mL 1.5% lidocaine test dose followed by 10 mL 1.5% lidocaine. She complained of a lumpy sensation in her throat and trouble speaking after the medication was administered, followed by bradycardic cardiac arrest. After 3 min of cardiopulmonary resuscitative effort, spontaneous rhythm returned. Spontaneous respiratory activity returned after another 2 min. Hypotension improved within 5 min. The patient was discharged home after 36 hours of observation in the hospital. Transient neurologic injury was reported by Shankar and Simhan27 in a 41-year-old man who underwent SGNB with ultrasound guidance for CRPS performed by an experienced pain medicine fellow. During the procedure, the patient complained of painful paresthesia in the corresponding arm. The needle was immediately withdrawn, and the SGNB was completed by the attending physician via out-of-plane technique (entire needle track is not visualized). After the procedure, the patient continued to experience occasional fullness in his ears, which resolved over the course of a few months. Masuda and Fujiki18 reported a case of sinus arrest in a young healthy volunteer after a right-sided stellate ganglion block. The arrest, which was probably secondary to a vasovagal reflex, lasted for 15 s with spontaneous resolution. One of the more unusual complications we encountered in the course of this review was the one described by Drolet56 of a 39-year-old man undergoing a right-sided SGNB via the landmark-based approach for pain relief under general anesthesia with laryngeal mask airway (LMA) in situ. The block was performed, and postanesthesia it was noted there was a needle puncture at the distal portion of the LMA. No air leaks were observed during the period of anesthesia. Other adverse events reported during SGNB include internal jugular vein thrombosis,57 arm numbness,58 lower extremity edema,4 injected conjunctiva, reading difficulties,59 and transient global amnesia.60
Summary of adverse events
In our review, we identified a total of 260 cases reporting adverse events with SGNB. One hundred and seventy-four (51.5%) of the SGNBs were performed with image guidance. Among these 260 cases, 82 (31.5%) patients had procedure-related or local side effects, and 178 (68.5%) experienced systemic or medication-related side effects. There was one report of death following landmark-guided SGNB and a report of a patient who developed quadriplegia secondary to a pyogenic cervical epidural abscess and discitis following SGNB. There was a total of five (1.9%) cases of patients who required tracheostomy, all of which were due to cervical area hematomas and one was a result of an allergic reaction to bupivacaine. Each of these patients had a delayed presentation of their complication. The patient with an allergic reaction to bupivacaine was diagnosed with cervical hematoma initially because of the sequence and timing of events. Many patients who experienced adverse events secondary to SGNB had had uneventful prior procedures, and many subsequently proceeded to complete the block successfully after recovery from the adverse event. Successful previous SGNBs with no complications did not, therefore, predict freedom from complications with future blocks. This review highlights the importance of vigilance, American Society of Anesthesiologists (ASA) standard monitors for conscious sedation, and accessibility to resuscitation equipment. It is assuring that most patients with complications recovered without any long-term morbidity. The most commonly reported adverse event reported was hoarseness in 72 (27.6%) patients. Most patients continued with their planned series of blocks uneventfully. Additional details of cases with complications, such as the volume of injectate and the type of ultrasound guidance, are included in online supplementary material appendix C.
DISCUSSION
SGNB is a common procedure with a growing list of indications. It is considered a relatively safe procedure, with Wulf and Maier61 reporting incidence of severe complications as 1.7 per 1000 blocks.
The first reported case of SGNB performed using landmark-based approach was described by Murphey62 in 1944. Over the years the procedures, tools, techniques, equipment for imaging guidance, and training methods for physicians performing SGNB have evolved.
The main findings of our systematic review are as follows: (1) Most complications after SGNB are transient, although we identified six cases of significant morbidity following the procedure. There were five cases of hematoma requiring tracheostomy, with one patient experiencing death and one case of quadriplegia secondary to infection. (2) The aspiration test was negative in the majority of the case reports. (3) Most of the transient complications were recognized during the procedure or shortly thereafter. (4) The complications were mainly due to disruption of local structure, introducing anesthetic medications in the wrong space, or an effect created by autonomic imbalance due to the SGNB.
Vascular disruption
Vascular disruption can occur as the needle traverses through the tissue planes to reach the target, near the target as the physician makes final adjustments to the needle, or during the change of medication syringes. Vascular disruption can result in medication entering the vascular system directly, leading to adverse events such as transient locked-in syndrome or seizures. Transient locked-in syndrome is due to a reduction of blood flow through the basilar artery because of negative pressure or spasm. Vascular disruption may also lead to hemorrhage and hematoma, both of which can potentially be life-threatening. SGNB is usually contraindicated in anticoagulated patients. The risk of such complications can be reduced, however cannot be completely eliminated by appropriate planning of the needle trajectory and performing aspiration test before injection of medication.
Injection of medication in the wrong space
Injection of anesthetic medication into the wrong space, such as into the vasculature or into the subdural or intrathecal space, is associated with adverse events requiring mechanical ventilation and cardiopulmonary resuscitation. The volume of injected anesthetic may be associated with bilateral sympathetic blockade.
Alterations in autonomic tone
In our review, we identified various adverse events relating to the autonomic system, including migraine headaches, visual hallucinations, and ptosis. The autonomic nervous system is very complex and varies from individual to individual. We have yet to learn the full implications of blocking the SGNB or ways to predict susceptibility to untoward experiences.
Complication rates associated with imaging techniques
Since the initial reports of SGNB, there have been numerous articles describing adverse events in the literature. However, many of the reports include only minimal details and may not be relevant to contemporary practice. There is potential for significant risk of bias in combining adverse events associated with techniques reported in publications over the years to determine incidence rates. The definition of the adverse event also varies from publication to publication. Complications reported in randomized clinical trials evaluating SGNB and complications reported between 1950 and 1989 are included in online supplementary material appendices D and E, respectively.
Our review highlights the need for intravenous access when performing SGNB, as well as ASA standard monitors for conscious sedation and accessibility to resuscitation equipment during and after the procedure. A longer recovery room stay for about 30–60 min should be strongly considered. However, as we have noted, adverse events secondary to bleeding and infection can have a delayed presentation. Providers performing SGNB should clearly communicate the warning signs relating to bleeding and infection to patients after their uneventful recoveries post-SGNB.
This systematic review of stellate ganglion block-related complications demonstrates that no one technique is perfect. Complications have been reported not only with the landmark-based technique but more recently with fluoroscopy and ultrasound guidance as well. In his editorial, Narouze63 states that fluoroscopy can help prevent injection of medicine into a vessel, and ultrasound, providing detailed soft tissue visualization, can help prevent vessel puncture and penetration through unwanted structures.63 Ultrasound is a relatively new technology in the hands of pain medicine physicians, and further research is needed to elucidate its efficacy, safety, and economic benefit. Combining imaging techniques within one SGNB procedure, such that ultrasound is used to help avoid vessels and other critical structures, and fluoroscopy is used to confirm dye spread, may offer a promising option to reduce the rate of complications further.
Future directions
The growing number of indications for SGNB increases the importance of effective education and training in techniques in performing SGNB successfully and safely. Simulation training may hold the key to achieving this formidable task.64 Image guidance continues to be widely accepted. Despite their limitations, fluoroscopy and ultrasound imaging techniques have opened new possibilities. Combining both imaging modalities may overcome limitations of any single modality, although the additional steps and expense must also be weighed. Targeted delivery of medications using micropuncture needles that may lead to minimal tissue disruption and vascular injury offers another avenue of exploration. Dry pericardial access using a needle-in-needle technique65 has been described, and such technique can be considered in some patients at increased risk of complications. Similar techniques could potentially be considered for SGNB by incorporating a blunt needle66 or echogenic needles67 to limit vascular injury and nerve damage. The medications used for SGNB in the studies we identified were local anesthetics. We did not come across any case reports of adverse events secondary to steroid medications injected in the vicinity of the stellate ganglion. New medications may also offer additional possibilities for SGNB. Qureshi et al68 described a 43-year-old patient who underwent an SGNB for refractory right-sided headaches with liposomal bupivacaine. The safety and efficacy of these newer drugs, however, remain yet to be determined in large systematic studies. This intriguing report raises several questions regarding the potential for reducing the frequency of injections, timing of presentation, and duration of complications.
Limitations
Our study has several limitations. The screening for eligibility of articles and case reports was completed by sequential review instead of by two or more simultaneous independent observers. There may be a risk of reporting and publication bias because of the limited number of reports on the side effects from SGNB. We found only 67 articles describing 260 cases with reported side effects of SGNB. It was not possible to determine the number of SGNBs completed with or without complications, and therefore we were unable to determine the relative frequency of each type of adverse event. It must be noted that most of the publications we identified were case reports or case series rather than large multi-institution cohort studies, which would offer a stronger evidence base. It is additionally possible that we missed reports in the gray literature that were not accessible by the search engines we used. Significant heterogeneity of published reports precluded us from providing summary measures such as incidence rates with each imaging technique. Due to the retrospective nature of the reported cases in the literature, we are unable to establish the superiority of one imaging technique over the other.
CONCLUSION
SGNB is increasingly performed for a variety of diagnostic and therapeutic indications. As with any invasive procedure, complications following SGNB have been reported with the landmark technique, as well as with imaging guidance by fluoroscopy and ultrasound. In our systematic review, most adverse events that were reported occurred during or shortly after SGNB. The importance of constant vigilance along with accessibility to resuscitation equipment for all SGNB procedures cannot be overstated.
Supplementary Material
Acknowledgements
The authors would like to thank Pushpraj for creating the illustrations.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Footnotes
Competing interests None declared.
Patient consent for publication Not required.
Ethics approval The study was reviewed by the institutional review board and was exempt given its retrospective data analysis nature.
Provenance and peer review Not commissioned; externally peer reviewed.
Author note The manuscript submitted is original, with no portion under simultaneous consideration for publication elsewhere, and has not been previously published.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplementary material.
REFERENCES
- 1.Manchikanti L, Pampati V, Hirsch JA. Utilization of interventional techniques in managing chronic pain in Medicare population from 2000 to 2014: an analysis of patterns of utilization. Pain Physician 2016;19:E531–46. [PubMed] [Google Scholar]
- 2.Jeon Y Therapeutic potential of stellate ganglion block in orofacial pain: a mini review. J Dent Anesth Pain Med 2016;16:159–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nabil Abbas D, Abd El Ghafar EM, Ibrahim WA, et al. Fluoroscopic stellate ganglion block for postmastectomy pain: a comparison of the classic anterior approach and the oblique approach. Clin J Pain 2011;27:207–13. [DOI] [PubMed] [Google Scholar]
- 4.Makharita MY, Amr YM, El-Bayoumy Y. Effect of early stellate ganglion blockade for facial pain from acute herpes zoster and incidence of postherpetic neuralgia. Pain Physician 2012;15:467–74. [PubMed] [Google Scholar]
- 5.Ander M Ultrasound-guided left cervical stellate ganglion block for recurrent ventricular tachycardia (electrical storm). Reg Anesth Pain Med 2016;41. [Google Scholar]
- 6.Haest K, Kumar A, Van Calster B, et al. Stellate ganglion block for the management of hot flashes and sleep disturbances in breast cancer survivors: an uncontrolled experimental study with 24 weeks of follow-up. Ann Oncol 2012;23:1449–54. [DOI] [PubMed] [Google Scholar]
- 7.Lipov E The use of stellate ganglion block in the treatment of panic/anxiety symptoms (including suicidal ideation), with combat-related posttraumatic stress disorder. In: Posttraumatic stress disorder and related diseases in combat veterans. Springer International Publishing, 2015. [Google Scholar]
- 8.Standring S Gray’s Anatomy: the anatomical basis of clinical anatomy 2016. [Google Scholar]
- 9.Baig S, Moon JY, Shankar H. Review of sympathetic blocks: anatomy, sonoanatomy, evidence, and techniques. Reg Anesth Pain Med 2017;42:377–91. [DOI] [PubMed] [Google Scholar]
- 10.PP R Stellate ganglion block. Philadelphia: W B Saunders Co, 1996. [Google Scholar]
- 11.Abdi S, Zhou Y, Patel N, et al. A new and easy technique to block the stellate ganglion. Pain Physician 2004;7:327–31. [PubMed] [Google Scholar]
- 12.Kapral S, Krafft P, Gosch M, et al. Ultrasound imaging for stellate ganglion block: direct visualization of puncture site and local anesthetic spread. A pilot study. Reg Anesth 1995;20:323–8. [PubMed] [Google Scholar]
- 13.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 2009;62:e1–34. [DOI] [PubMed] [Google Scholar]
- 14.Omote K, Kawamata M, Namiki A. Adverse effects of stellate ganglion block on Raynaud’s phenomenon associated with progressive systemic sclerosis. Anesth Analg 1993;77:1057–60. [DOI] [PubMed] [Google Scholar]
- 15.Kurimoto T, Takata M, Nishimura M, et al. Visual hallucinations following stellate ganglion block in a patient with central retinal artery occlusion. Jpn J Ophthalmol 2006;50:567–9. [DOI] [PubMed] [Google Scholar]
- 16.Mahli A, Coskun D, Akcali DT. Aetiology of convulsions due to stellate ganglion block: a review and report of two cases. Eur J Anaesthesiol 2002;19:376–80. [DOI] [PubMed] [Google Scholar]
- 17.Mishio M, Matsumoto T, Okuda Y, et al. Delayed severe airway obstruction due to hematoma following stellate ganglion block. Reg Anesth Pain Med 1998;23:516–9. [DOI] [PubMed] [Google Scholar]
- 18.Masuda A, Fujiki A. Sinus arrest after right stellate ganglion block. Anesth Analg 1994;79. [DOI] [PubMed] [Google Scholar]
- 19.Jadon A Revalidation of a modified and safe approach of stellate ganglion block. Indian J Anaesth 2011;55:52–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eyigor C, Erhan E, Yegul I. Grand mal seizure following stellate ganglion block after negative aspiration. Pain Practice 2009;9:37–8. [Google Scholar]
- 21.Karaman H. Complications and success rates of stellate ganglion blockade; blind technique vs fluoroscopic guidance. Biomed Res 2017;28:1677–82. [Google Scholar]
- 22.Kim CH. Respiratory depression following stellate ganglion block. PM&R 2013;5. [Google Scholar]
- 23.Harano K, Takasaki M, Araki K, et al. Probability of definite stellate ganglion block (sgb) at the 7th cervical vertebral level (C7). Anesthesiology 2000;93. [Google Scholar]
- 24.Fujiwara S, Komasawa N, Kido H, et al. A rare case of accidental arterial local anesthetic injection under ultrasound-guided stellate ganglion block. J Clin Anesth 2016;29:3–4. [DOI] [PubMed] [Google Scholar]
- 25.Espinar González MJ, Sanchez del Aguila M, Alonso M I, et al. Severe allergic reaction after bupivacaine injection for a stellate ganglion blockade. Reg Anesth Pain Med 2010;35. [Google Scholar]
- 26.Rastogi S, Tripathi S. Cardiac arrest following stellate ganglion block performed under ultrasound guidance. Anaesthesia 2010;65. [DOI] [PubMed] [Google Scholar]
- 27.Shankar H, Simhan S. Transient neuronal injury followed by intravascular injection during an ultrasound guided stellate ganglion block. Anesth Pain Med 2013;2:134–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vinod K, Kurhekar P, Sharanya K, et al. Efficacy of the stellate ganglion block through the lateral approach using ultrasonogram and fluoroscopy. Turk J Anaesthesiol Reanim 2018;46:393–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kimura T, Nishiwaki K, Yokota S, et al. Severe hypertension after stellate ganglion block. Br J Anaesth 2005;94:840–2. [DOI] [PubMed] [Google Scholar]
- 30.Atici S, Akoz K. Transient cough attacks after right stellate ganglion block. Reg Anesth Pain Med 2010;35:318–9. [DOI] [PubMed] [Google Scholar]
- 31.Naveira FA, Rauck RL. Blocks of the sympathetic nervous system. Progress in Anesthesiology 1999;13:167–90. [Google Scholar]
- 32.Balaban B, Baklaci K, Taskaynatan MA, et al. Delayed subdural block as an unusual complication following stellate ganglion blockade. The Pain Clinic 2005;17:407–9. [Google Scholar]
- 33.Bruyns T, Devulder J, Vermeulen H, et al. Possible inadvertent subdural block following attempted stellate ganglion blockade. Anaesthesia 1991;46:747–9. [DOI] [PubMed] [Google Scholar]
- 34.Leong MS, Mackey S. Delayed subdural block after a stellate ganglion block. Anesthesiology 2001;94:358–9. [DOI] [PubMed] [Google Scholar]
- 35.Saruki N, Shiga T, Hasegawa M, et al. Rare complication after stellate ganglion block. Can J Anaesth 1997;44. [DOI] [PubMed] [Google Scholar]
- 36.Sari S, Aydin ON. Intraspinal blockade after stellate ganglion blockade in trauma patient. Reg Anesth Pain Med 2012;37:E239–E240. [Google Scholar]
- 37.Dukes RR, Alexander LA. Transient locked-in syndrome after vascular injection during stellate ganglion block. Reg Anesth 1993;18:378–80. [PubMed] [Google Scholar]
- 38.Tüz M, Erodlu F, Dodru H, et al. Transient locked-in syndrome resulting from stellate ganglion block in the treatment of patients with sudden hearing loss. Acta Anaesthesiol Scand 2003;47:485–7. [DOI] [PubMed] [Google Scholar]
- 39.Chaturvedi A, Dash H. Locked-in syndrome during stellate ganglion block. Indian J Anaesth 2010;54:324–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Corsaro ME, Averni F, Messina A, et al. Clinical evidence on risk and complications of the stellate ganglion block: transient locked-in syndrome. Acta Medica Mediterranea 2009;25:7–8. [Google Scholar]
- 41.Beleña J, Petersen I, Cabeza R, et al. Migraine headache: a rare complication after cervicothoracic block. J Headache Pain 2006;7:367–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lehmann LJ, Warfield CA, Bajwa ZH. Migraine headache following stellate ganglion block for reflex sympathetic dystrophy. Headache 1996;36:335–7. [DOI] [PubMed] [Google Scholar]
- 43.Lake APJ, Puvanachandra K. A complication of stellate ganglion block? Pain Pract 2004;4:130–1. [DOI] [PubMed] [Google Scholar]
- 44.Wallace MS, Milholland AV. Contralateral spread of local anesthetic with stellate ganglion block. Reg Anesth 1993;18:55–9. [PubMed] [Google Scholar]
- 45.Manchikanti L Bilateral Horner’s syndrome following stellate ganglion block. Anesthesiol Rev 1990;17:41–3.10149045 [Google Scholar]
- 46.Kay J, Lam-McCullouch J, Carmody E. Incidence of hemidiaphragm paresis with stellate ganglion block. Reg Anesth Pain Med 1999;24(Supplement 1). [Google Scholar]
- 47.Okuda Y, Urabe K, Kitajima T. Retropharyngeal or cervicomediastinal haematomas following stellate ganglion block. Eur J Anaesthesiol 2003;20:757–9. [DOI] [PubMed] [Google Scholar]
- 48.Takanami I, Abiko T, Koizumi S. Life-threatening airway obstruction due to retropharyngeal and cervicomediastinal hematomas following stellate ganglion block. Thorac Cardiovasc Surg 2009;57:311–2. [DOI] [PubMed] [Google Scholar]
- 49.Uchida T, Nakao S, Morimoto M, et al. Serious cervical hematoma after stellate ganglion block. J Anesth 2015;29. [DOI] [PubMed] [Google Scholar]
- 50.Kashiwagi M, Ikeda N, Tsuji A, et al. Sudden unexpected death following stellate ganglion block. Leg Med 1999;1:262–5. [DOI] [PubMed] [Google Scholar]
- 51.Stannard CF, Glynn CJ, Smith SP. Dural puncture during attempted stellate ganglion block. Anaesthesia 1990;45:952–4. [DOI] [PubMed] [Google Scholar]
- 52.Masuda R, Yokoyama K, Inoue T, et al. Clinical evaluation of cervical pyogenic spondylitis/spondylodiscitis after stellate ganglion block. The Pain Clinic 2004;16:89–96. [Google Scholar]
- 53.Vadodaria B, Bridgens J, Richmond M. Pyogenic cervical epidural abscess and discitis following stellate ganglion block. Anaesthesia 2001;56:871–2. [Google Scholar]
- 54.Shimada Y, Marumo H, Kinoshita T, et al. A case of cervical spondylitis during stellate ganglion block. J Nippon Med Sch 2005;72:295–9. [DOI] [PubMed] [Google Scholar]
- 55.Saxena AK, Saxena N, Aggarwal B, et al. An unusual complication of sinus arrest following right-sided stellate ganglion block: a case report. Pain Pract 2004;4:245–8. [DOI] [PubMed] [Google Scholar]
- 56.Drolet S Puncture of the laryngeal mask airway during stellate ganglion block. Can J Anesth/J Can Anesth 2001;48. [DOI] [PubMed] [Google Scholar]
- 57.Radhakrishnan L, Mathews A, Lin ES, et al. Thrombosis of internal jugular vein following stellate ganglion block. Pain Practice 2009;9:111–2. [Google Scholar]
- 58.Datta R, Agrawal J, Sharma A, et al. A study of the efficacy of stellate ganglion blocks in complex regional pain syndromes of the upper body. J Anaesthesiol Clin Pharmacol 2017;33:534–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Devulder J, DeLaat M, ROLLY G. Stellate ganglion block alleviates pseudo-obstruction symptoms followed by episodes of hypermetropia: case report. Reg Anesth Pain Med 1997;22:284–6. [DOI] [PubMed] [Google Scholar]
- 60.Park S, Park S, Jang Y. Transient global amnesia after stellate ganglion block. J 2015;29. [DOI] [PubMed] [Google Scholar]
- 61.Wulf H, Maier C. [Complications and side effects of stellate ganglion blockade. Results of a questionnaire survey]. Anaesthesist 1992;41:146–51. [PubMed] [Google Scholar]
- 62.MURPHEY R Stellate ganglion block a new anterior approach. Annals of Surgery 1944;120:759–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Narouze SN. Ultrasound-guided cervical spine injections: ultrasound "prevents" whereas contrast fluoroscopy "detects" intravascular injections. Reg Anesth Pain Med 2012;37:127–30. [DOI] [PubMed] [Google Scholar]
- 64.Chen XX, Trivedi V, AlSaflan AA, et al. Ultrasound-guided regional anesthesia simulation training: a systematic review. Reg Anesth Pain Med 2017;42:741–50. [DOI] [PubMed] [Google Scholar]
- 65.Kumar S, Bazaz R, Barbhaiya CR, et al. "Needle-in-needle" epicardial access: Preliminary observations with a modified technique for facilitating epicardial interventional procedures. Heart Rhythm 2015;12:1691–7. [DOI] [PubMed] [Google Scholar]
- 66.Heavner JE, Racz GB, Jenigiri B, et al. Sharp versus blunt needle: a comparative study of penetration of internal structures and bleeding in dogs. Pain Pract 2003;3:226–31. [DOI] [PubMed] [Google Scholar]
- 67.Hebard S, Hocking G. Echogenic technology can improve needle visibility during ultrasound-guided regional anesthesia. Reg Anesth Pain Med 2011;36:185–9. [DOI] [PubMed] [Google Scholar]
- 68.Qureshi AI, Waqas MA, Jadhav V, et al. Long acting liposomal bupivacaine for percutaneous sympathetic stellate ganglion blockade: a technical note. J Vasc Interv Neurol 2017;9:49–53. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplementary material.


