Abstract
Introduction
DeSanto‐Shinawi syndrome is a rare neurodevelopmental disorder caused by loss‐of‐function variants of WAC, located on chromosome 10p12.1. This syndrome is characterized by dysmorphic facial features, intellectual disability, and behavioral problems.
Case report
In this case report, we present a new deletion case and summarize the clinical data of previously reported individuals, comparing the similarities and differences between cases caused by point mutations versus those which are caused by deletions in the 10p region.
Conclusion
Some differential features could facilitate the diagnostic suspicion guiding the optimal diagnostic tests that should be requested in each case scenario.
Keywords: 10p deletion, array CGH, DeSanto‐Shinawi syndrome, global developmental delay, WAC
DeSanto‐Shinawi syndrome is a rare neurodevelopmental disorder caused by loss‐of‐function variants of WAC, located on chromosome 10p12.1. This syndrome is characterized by dysmorphic facial features, intellectual disability, and behavioral problems. In this case report, we present a new deletion case and summarize the clinical data of previously reported individuals, comparing the similarities and differences between cases caused by point mutations versus those which are caused by deletions in the 10p region.
1. INTRODUCTION
DeSanto‐Shinawi syndrome (DESSH, OMIM #616708) was first described by de Santo et al. (2015). It is a rare neurodevelopmental disorder characterized by global developmental delay, behavioral abnormalities beginning in early childhood, and characteristic dysmorphic facial features.
It is caused by loss‐of‐function variants of WAC (OMIM #615049), located on chromosome 10p12.1. It encodes WW domain‐containing adaptor with coiled‐coil region (WAC), a nuclear protein that regulates histone H2B ubiquitination through interaction with RNF20/40, chromatin organization and ultimately gene transcription and cell cycle checkpoint activation in response to genotoxic stress (Alawadhi et al., 2021; de Santo et al., 2015). The protein encoded by this gene plays a vital role in gene transcription, microtubule development, autophagy, and Golgi apparatus function (Alsahlawi et al., 2020).
To our knowledge, an extensive clinical description has been reported in the literature for only 25 cases of point mutations (Alsahlawi et al., 2020; de Santo et al., 2015; Leonardi et al., 2020; Lugtenberg et al., 2016; Uehara et al., 2018; Vanegas et al., 2018; Zhang et al., 2019). Before the full description of the syndrome by DeSanto et al. in 2015, several studies had described the common phenotypic characteristics of patients with deletions in the WAC gene (Okamoto et al., 2012; Shahdadpuri et al., 2008; Wentzel et al., 2011).
2. MATERIAL AND METHODS
We report a case from a 6‐year‐old female patient who was born to non‐consanguineous Caucasian parents after a 41‐week, uncomplicated pregnancy. Father reported a mild gait delay, but both parents were not known to have any genetic or chronic disease.
At birth, Apgar score was 10/10, she weighed 2.970 Kg (10th centile), length 50.5 cm (60th centile), and her occipitofrontal head circumference (OFC) was 32 cm (10th centile).
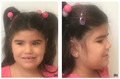
Developmental delay was first noticed at 19 months old, when patient was unable to walk. She started crawling at 14 months. Language development was also delayed, with first words spoken at 14 months. By the time of her first clinical evaluation (at 20 months old), she could say less than 10 words. She also presented repetitive behavior patterns, such as turning lights on and off. She showed characteristic facial dysmorphic features (Figure 1): synophrys with deeply set eyes, down slanted palpebral fissures, a bulbous nose with depressed nasal bridge, and posteriorly rotated ears with preauricular pits. She had the tendency to keep the mouth open with tongue protrusion, and she also presented diastema and an everted vermilion of the upper lip. Since early childhood she had sleep difficulties, such as snoring with occasional apnea pauses, sleep terrors, and enuresis.
FIGURE 1.

Patient's facial dysmorphic features
The patient is currently enrolled in early childhood education with educational and speech therapy support. She presents a mild gross motor clumsiness and social development and interactional difficulties due to her impulsive and aggressive behavior with her peers.
A comparative genomic hybridization (aCGH) was performed from peripheral blood sample obtained with prior written informed consent from parents. Analysis was carried out using 60 K SurePrint G3 Human CGH ISCA v2 Microarray from Agilent Technologies. Samples from patient and her parents were hybridized against a same‐sex hybridization control (Human Reference DNA, from Agilent Technologies).
3. RESULTS
A single dose of the 10p12.1p11.23 region was found in the proband. This deletion on 10 chromosome was approximately 2.49 Mb in size: arr[GRCh37] 10p12.1p11.23(27727630_30222261)x1, and included seven genes, where WAC gene was contained. Chromosomal formula is expressed according to the ISCN nomenclature against the GRCh37 reference assembly. Results have been aligned against the reference human genome and their possible pathogenicity was evaluated by querying databases.
Major features are summarized in Table 1 next to their HPO codes, as well as other clinical findings in the proband, comparing them with other cases published before deletions from 15.7 to 2 Mb that include WAC gene (Okamoto et al., 2012; Shahdadpuri et al., 2008; Wentzel et al., 2011) among other genes versus point mutations in WAC gene (Alsahlawi et al., 2020; de Santo et al., 2015; Leonardi et al., 2020; Lugtenberg et al., 2016; Uehara et al., 2018; Vanegas et al., 2018; Zhang et al., 2019).
TABLE 1.
Clinical features of the case reported compared to individuals previously reported in the literature
| Deletions | Deletions | Point mutations | |||||||
|---|---|---|---|---|---|---|---|---|---|
| This report | Okamoto et al. (2012) | Wentzel et al. (2011) | Shahdadpuri et al. (2008) | ||||||
| Sample | 1 patient | 2 patients | 6 patients | 1 patient | 10 patients | % | 25 patients | % | |
| Sex | F | 1 F, 1 M | 4 F, 2 M | 1 M | 6F, 4 M | 13 F, 12 M | |||
| Age | 6 y/o | 6, 7–7, 8 y/o | 3, 4–11 y/o | 1, 3 y/o | 1, 3–11 y/o | 1, 3–22 y/o | |||
| Delayed growth | − | 0/2 | 4/6 | − | 4/10 | 40.00% | 11/25 | 44.00% | |
| Perinatal abnormalities | − | 0/2 | 2/6 | − | 2/10 | 20.00% | 9/25 | 36.00% | |
| Development | |||||||||
| HP:0001270 | Motor delay | + | 2/2 | 6/6 | + | 10/10 | 100.00% | 24/25 | 96.00% |
| HP:0000750 | Delayed speech and language development | + | 1/2 | 5/6 | + | 8/10 | 80.00% | 24/25 | 96.00% |
| Dismorphic features | |||||||||
| HP:0000664 | Synophrys | + | 2/2 | 5/6 | NR | 8/9 | 88.89% | 9/25 | 36.00% |
| HP:0000490 | Deeply set eye | + | 2/2 | 4/6 | + | 8/10 | 80.00% | 12/25 | 48.00% |
| HP:0000414 | Bulbous nose | + | 1/2 | 4/6 | + | 7/10 | 70.00% | 13/15 | 86.67% |
| HP:0000158 | Macroglossia | − | 2/2 | NR | NR | 2/3 | 66.67% | 12/12 | 100.00% |
| HP:0004467 | Preauricular pit | + | 1/2 | NR | − | 2/4 | 50.00% | 2/12 | 16.67% |
| HP:0011297 | Abnormal digit morphology | + | 1/2 | 3/6 | − | 5/10 | 50.00% | 14/21 | 66.67% |
| HP:0005280 | Depressed nasal bridge | + | 2/2 | 1/6 | NR | 4/9 | 44.44% | 9/9 | 100.00% |
| HP:0001007 | Hirsutism | + | NR | 2/6 | NR | 3/7 | 42.86% | 7/25 | 28.00% |
| HP:0011220 | Prominent forehead | − | 2/2 | 1/6 | − | 3/10 | 30.00% | 21/25 | 84.00% |
| HP:0000316 | Hypertelorism | − | 0/2 | NR | + | 1/4 | 25.00% | 14/19 | 73.68% |
| HP:0000369 | Low‐set ears | − | 0/2 | NR | + | 1/4 | 25.00% | 5/15 | 33.33% |
| HP:0000272 | Malar flattening | − | 0/2 | 1/6 | NR | 1/9 | 11.11% | 4/9 | 44.44% |
| Behavioral problems | |||||||||
| HP:0000752 | Hyperactivity | + | NR | 4/6 | NR | 5/7 | 71.43% | 9/24 | 37.50% |
| HP:0100852 | Anxiety‐related behavior | + | NR | 3/6 | NR | 4/7 | 57.14% | 9/24 | 37.50% |
| HP:0002360 | Sleep disturbance | + | NR | 3/6 | NR | 4/7 | 57.14% | 12/25 | 48.00% |
| HP:0000729 | Autistic behavior | + | NR | 2/6 | NR | 3/7 | 42.86% | 7/23 | 30.43% |
| Neurological | |||||||||
| HP:0001252 | Hypotonia | − | 0/2 | 3/6 | + | 4/10 | 40.00% | 18/24 | 75.00% |
| HP:0001250 | Seizures | − | 0/2 | 2/6 | NR | 2/9 | 22.22% | 6/24 | 25.00% |
| Other | |||||||||
| HP:0000486 | Strabismus | − | NR | 3/6 | − | 3/8 | 37.50% | 8/24 | 33.33% |
| HP:0002019 | Constipation | − | 1/2 | 2/6 | NR | 3/9 | 33.33% | 8/14 | 57.14% |
| HP:0011968 | Feeding difficulties | − | 1/2 | 1/6 | NR | 2/9 | 22.22% | 10/24 | 41.67% |
| Diagnostic tests | |||||||||
| HP:0002353 | EEG abnormalities | + | NR | NR | NR | 1/1 | 100.00% | 2/8 | 25.00% |
| HP:0002500 | MRI abnormalities | NR | 0/2 | 4/6 | + | 5/9 | 55.56% | 6/21 | 28.57% |
| HP:0000364 | Hearing abnormality | − | 1/2 | 2/6 | + | 4/10 | 40.00% | 3/15 | 20.00% |
Note: NR, not reported; +, present; −, absent.
4. DISCUSSION
Almost all patients described in cases of point mutations and in the deletion group presented motor developmental delay. More than 80% of them presented language difficulties as well, without significant differences between the two groups.
According to the dysmorphic characteristics, there were some recognizable craniofacial characteristics in both groups. Nevertheless, some of them were described with significant differences between them, being more frequent in the deletion group, such as synophrys (8/9), deeply set eyes (8/10), or depressed nasal bridge (4/9) (Okamoto et al., 2012; Shahdadpuri et al., 2008; Wentzel et al., 2011).
On the other hand, features such as prominent forehead (3/10) or malar flattening (1/9) were less frequent in this group compared to the point mutations one (Alsahlawi et al., 2020; de Santo et al., 2015; Leonardi et al., 2020; Lugtenberg et al., 2016; Uehara et al., 2018; Vanegas et al., 2018; Zhang et al., 2019).
Some dysmorphic characteristics like bulbous nose or abnormal digit morphology were reported without significant differences between both groups.
Most of the patients presented behavioral problems. In the deletion group, ADHD was detected in greater than 70% of the cases (Okamoto et al., 2012; Shahdadpuri et al., 2008; Wentzel et al., 2011). Anxiety‐related behavior, sleep disturbances, or autistic features were also described in both groups.
In the patient described in this report, no anomalies were found in metabolic and immunology tests, polysomnography, or auditory evoked potentials.
The EEG showed a normal background activity with right middle temporal epileptiform activity more intense during sleep. However, no clinical crises have been reported to date.
Seizures or epilepsy had been described only in patients with WAC point mutations. The typical EEG pattern of electrical status epilepticus during slow sleep, has been reported only in one patient by Leonardi et al. (2020), but due to the importance of early diagnosis it should be taken into account from now on in new diagnoses of DESSH.
5. CONCLUSION
So far, few cases have been reported. We intend to further delineate the phenotypic spectrum of DESSH, emphasizing the possible differences depending on the type of variant found. As we describe in this report, synophrys, deeply set eyes, or depressed nasal bridge were features found more frequently in the large deletions group, which were detected by aCGH. However, patients who showed a prominent forehead or malar flattening, were more likely to present a point mutation, in which we would perform the sequencing of the WAC gene.
We could improve the genotype–phenotype correlations described in DESSH patients and we could decide which is the technical method used in each case.
Broadening the knowledge about WAC‐DESSH phenotype may contribute to improving the management of patients and the counseling to the families.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
Cristina Toledo‐Gotor: collected the data, contributed data or analysis tools, and wrote the paper. Cristina García‐Muro: collected the data, contributed data, or analysis tools. Alberto García‐Oguiza: contributed data or analysis tools, revised the draft. Mª Luisa Poch‐Olivé: revised the draft critically for important intellectual content. Mª Yolanda Ruiz‐del Prado: approved the version to be published. Elena Domínguez‐Garrido: conceived and designed the analysis, revised the draft, approved the version to be published.
ETHICAL APPROVAL
All procedures performed were in accordance with the ethical standards with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Patient’s family provided written informed consent.
ACKNOWLEDGMENTS
We thank the patient and her family for their participation.
Toledo‐Gotor, C. , García‐Muro, C. , García‐Oguiza, A. , Poch‐Olivé, M. L. , Ruiz‐del Prado, M. Y. & Domínguez‐Garrido, E. (2022). Phenotypic comparison of patients affected with DeSanto‐Shinawi syndrome: Point mutations in WAC gene versus a 10p12.1 microdeletion including WAC . Molecular Genetics & Genomic Medicine, 10, e1910. 10.1002/mgg3.1910
DATA AVAILABILITY STATEMENT
All data generated or analyzed during this study are included in this published article (and its supplementary information files). If you have any further questions, data are available from the corresponding author upon reasonable request.
REFERENCES
- Alawadhi, A. , Morgan, A. T. , Mucha, B. E. , Scheffer, I. E. , & Myers, K. A. (2021). Self‐limited focal epilepsy and childhood apraxia of speech with WAC pathogenic variants. European Journal of Paediatric Neurology, 30, 25–28. 10.1016/j.ejpn.2020.12.010 [DOI] [PubMed] [Google Scholar]
- Alsahlawi, Z. , Jailani, M. , Alaradi, H. , & AlAbbad, A. (2020). A case of DeSanto‐Shinawi syndrome in Bahrain with a novel mutation. Case Reports in Pediatrics, 2020, 1–6. 10.1155/2020/8820966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Santo, C. , D'Aco, K. , Araujo, G. C. , Shannon, N. , Study, D. D. D. , Vernon, H. , Rahrig, A. , Monaghan, K. G. , Niu, Z. , Vitazka, P. , Dodd, J. , Tang, S. , Manwaring, L. , Martir‐Negron, A. , Schnur, R. E. , Juusola, J. , Schroeder, A. , Pan, V. , Helbig, K. L. , … Shinawi, M. (2015). WAC loss‐of‐function mutations cause a recognisable syndrome characterised by dysmorphic features, developmental delay and hypotonia and recapitulate 10p11.23 microdeletion syndrome. Journal of Medical Genetics, 52, 754–761. 10.1136/jmedgenet-2015-103069 [DOI] [PubMed] [Google Scholar]
- Leonardi, E. , Bellini, M. , Aspromonte, M. C. , Polli, R. , Mercante, A. , Ciaccio, C. , Granocchio, E. , Bettella, E. , Donati, I. , Cainelli, E. , Boni, S. , Sartori, S. , Pantaleoni, C. , Boniver, C. , & Murgia, A. (2020). A novel WAC loss of function mutation in an individual presenting with encephalopathy related to status epilepticus during sleep (ESES). Genes, 11, 344. 10.3390/genes11030344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lugtenberg, D. , Reijnders, M. R. F. , Fenckova, M. , Bijlsma, E. K. , Bernier, R. , van Bon, B. W. M. , Smeets, E. , Vulto‐van Silfhout, A. T. , Bosch, D. , Eichler, E. E. , Mefford, H. C. , Carvill, G. L. , Bongers, E. M. H. F. , Schuurs‐Hoeijmakers, J. H. M. , Ruivenkamp, C. A. , Santen, G. W. E. , van den Maagdenberg, A. M. J. M. , Peeters‐Scholte, C. M. P. C. D. , Kuenen, S. , … Vissers, L. E. L. M. (2016). De novo loss‐of‐function mutations in WAC cause a recognizable intellectual disability syndrome and learning deficits in drosophila. European Journal of Human Genetics, 24, 1145–1153. 10.1038/ejhg.2015.282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamoto, N. , Hayashi, S. , Masui, A. , Kosaki, R. , Oguri, I. , Hasegawa, T. , Imoto, I. , Makita, Y. , Hata, A. , Moriyama, K. , & Inazawa, J. (2012). Deletion at chromosome 10p11.23‐p12.1 defines characteristic phenotypes with marked midface retrusion. Journal of Human Genetics, 57, 191–196. 10.1038/jhg.2011.154 [DOI] [PubMed] [Google Scholar]
- Shahdadpuri, R. , de Vries, B. , Pfundt, R. , de Leeuw, N. , & Reardon, W. (2008). Pseudoarthrosis of the clavicle and copper beaten skull associated with chromosome 10p11.21p12.1 microdeletion. American Journal of Medical Genetics, Part A, 146, 233–237. 10.1002/ajmg.a.32088 [DOI] [PubMed] [Google Scholar]
- Uehara, T. , Ishige, T. , Hattori, S. , Yoshihashi, H. , Funato, M. , Yamaguchi, Y. , Takenouchi, T. , & Kosaki, K. (2018). Three patients with DeSanto‐Shinawi syndrome: Further phenotypic delineation. American Journal of Medical Genetics, Part A, 176, 1335–1340. 10.1002/ajmg.a.38703 [DOI] [PubMed] [Google Scholar]
- Vanegas, S. , Ramirez‐Montanõ, D. , Candelo, E. , Shinawi, M. , & Pachajoa, H. (2018). DeSanto‐shinawi syndrome: First case in South America. Molecular Syndromology, 9, 154–158. 10.1159/000488815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wentzel, C. , Rajcan‐Separovic, E. , Ruivenkamp, C. A. L. , Chantot‐Bastaraud, S. , Metay, C. , Andrieux, J. , Annerén, G. , Gijsbers, A. C. J. , Druart, L. , Hyon, C. , Portnoi, M. F. , Stattin, E. L. , Vincent‐Delorme, C. , Kant, S. G. , Steinraths, M. , Marlin, S. , Giurgea, I. , & Thuresson, A. C. (2011). Genomic and clinical characteristics of six patients with partially overlapping interstitial deletions at 10p12p11. European Journal of Human Genetics, 19, 959–964. 10.1038/ejhg.2011.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. J. , Yao, P. L. , Zhou, Y. F. , Qiu, T. , Wang, J. , Wang, X. H. , Zhou, S. Z. , Wu, B. B. , & Wang, Y. (2019). WAC gene pathogenic variation cause DeSanto‐Shinawi syndrome with electrical status epilepticus during sleep. Chinese Journal of Pediatrics, 57, 802–804. 10.3760/cma.j.issn.0578-1310.2019.10.015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article (and its supplementary information files). If you have any further questions, data are available from the corresponding author upon reasonable request.


