Abstract
Background:
Dislocation after total hip arthroplasty (THA) partly under the surgeon’s control, by appropriate placement of the components. We aimed in this study to determine the accuracy of using intra-operative smartphone applications (Apps) to place the acetabular cup within the safe abduction angle by less experienced surgeons during THA surgery when compared to the conventional freehand technique for cup placement.
Methods:
Sixty primary THAs were performed, 30 using the conventional freehand technique (control group) and 30 using the smartphone app technique (study group) to determine the acetabular cup abduction angle by the same young surgeon with less than one year of experience. Postoperative mean cup abduction angle, mean cup anteversion angle, and the percentage of cups within the safe abduction zone as measured on radiographs were compared between the two groups.
Results:
In the study group, the mean cup abduction angle was significantly lower (P=0.0008), and the acetabular cup was placed within the safe zone in a significantly higher (P<0.001) percentage of patients (93% vs 63%) when compared to the control group. However, there was no significant difference (P=0.40) between the two groups when the mean cup anteversion angle was compared.
Conclusion:
The smartphone app technique may help achieve an accurate acetabular cup abduction angle and a higher percentage of cups placed within the safe zone of abduction by a less experienced surgeon when compared to the conventional freehand technique. Using tools such as the smartphone app to measure the acetabular cup position can reduce intraoperative errors by young and less experienced surgeons during THA surgery.
Key Words: acetabular cup, Lewinnek safe zone, Total hip arthroplasty, total hip replacement, smartphone
Introduction
Dislocation is associated with primary total hip arthroplasty (THA) surgery with a reported incidence rate of up to 5% (1-3). The position and orientation of the acetabular cup, as decided and finalised by the surgeon, is an essential factor associated with the incidence of postoperative dislocation (4-6). Lewinnek et al. originally proposed an abduction angle of 40°±10° and an anteversion angle of 15° ±10° as the “safe zone” for cup placement during primary THA to prevent dislocation (7).
Conventionally, cup positioning in terms of version and abduction angle is adjusted during THA using the freehand technique where the floor or the bed level, position of the patient’s pelvis, and the relation of the transverse acetabular ligament (TAL) to the cup are used as reference points. However, utilising this freehand technique may lead to significant variation in cup placement from 25.7% to 70.5% within the “safe zone” (8-10).
Moreover, recent techniques such as patient-specific anatomical landmarks, computer-assisted surgery, and handheld navigation systems have been used to improve the accuracy of cup placement during primary THA surgery (10-13). However, these techniques have limited availability and may increase the cost of surgery (13). The use of smartphone applications (apps) intraoperatively to facilitate cup placement during primary THA surgery has been reported to be accurate and cost-effective (14, 15).
The purpose of this study was to evaluate the effectiveness of using an intra-operative smartphone app to accurately place the cup within the safe abduction angle by less experienced surgeons during THA surgery. This study also aimed to compare their results with cup placement accuracy of young, less experienced surgeons who used the conventional freehand technique for cup placement. We hypothesised that using intraoperative smart apps to determine cup position by young, less experienced surgeons can help achieve better cup placement accuracy than using the conventional freehand technique.
Materials and Methods
Patients
In this retrospective study, all consecutive patients who underwent primary THA for hip arthritis, avascular necrosis, and neck of femur fractures at the study centre between September 2018 to August 2019 using cemented or cementless implants where cup placement was performed using the conventional, freehand technique or the smartphone app technique were eligible for inclusion. The exclusion criteria were primary THAs due to post-traumatic arthritis or patients who required acetabular augments or reconstruction, or patients who did not consent to be part of the study. Included patients were divided into the conventional, freehand technique group (control group) or the smartphone app group (study group). Ethical approval was waived by the local Ethics Committee of our institution due to the retrospective nature of the study. Informed consent was obtained from all patients. Verbal consent to use the smartphone intraoperatively was obtained before surgery, as well as a written signed preoperative consent form as issued and required by our department, mentioning the use of a smartphone app during surgery.
Methods
All the procedures were performed by the same surgeon with less than one year of experience in surgical practice after his certification. The conventional, freehand technique or smartphone app technique was applied alternatively in patients by the operating surgeon (two operative lists a week in two different hospitals; in one, he used the smartphone technique while in the other he used the conventional technique). All procedures were performed under spinal anaesthesia through a modified direct lateral approach to the hip with the patient in the lateral decubitus position (16). The aim was to achieve an intraoperative cup abduction angle of 40° and reproduce the native acetabulum anteversion using the TAL as a landmark as described by Archbold et al. (10) in all patients. The implants and instruments were the same in both groups, where the ZCA all-poly cemented cup (Zimmer, Warsaw, Indiana, USA) was used in cemented THAs and the Pinnacle cementless cup (Depuy, Warsaw, Indiana, USA) was used in cementless THAs.
Surgical steps: draping was done in the same manner for all cases. In the smartphone app (study) group, a spirit level app with a built-in compass on an iPhone® 6 smartphone (Apple, Cupertino, CA, USA) was used (17). The app used the horizontal line of the floor as a reference point of 0°, and moving the smartphone at an angle showed the degrees at which the phone was tilted. After anaesthesia induction and before tilting the patient to the lateral decubitus position, we used the smartphone app to ensure that the operative table was parallel to the floor level and was set at 0°. A metallic marker (ECG lead) was placed on the ASIS bilaterally, and the patient turned in the lateral decubitus position on the table and was secured with posterior sacrum support. Before securing the anterior support, we measured the angle between the line connecting the two ASIS markers and the long edge of the table to detect any pelvic tilt which may happen after final patient positioning [Figure 1]. If the patient was obese and the marks could not be accurately placed over the ASIS, we used fluoroscopy to radiologically measure the angle between the line connecting the ASIS bilaterally and the long edge of the table. In an ideal situation, this ASIS line should be perpendicular to the long edge of the table in the coronal plane; however, if the pelvis is tilted towards the head of the patient (abduction), i.e., the angle is > 90°, we gave it a positive value, and if the pelvis was tilted towards the feet (adduction), we gave it a negative value. Any tilt or deviation from the 90° was taken into consideration during cup placement (e.g., if the pelvis was titled +5°, we will adjust the cup abduction angle to 45° instead of 40°, which was the target abduction angle in all cases) and vice versa.
Figure 1.
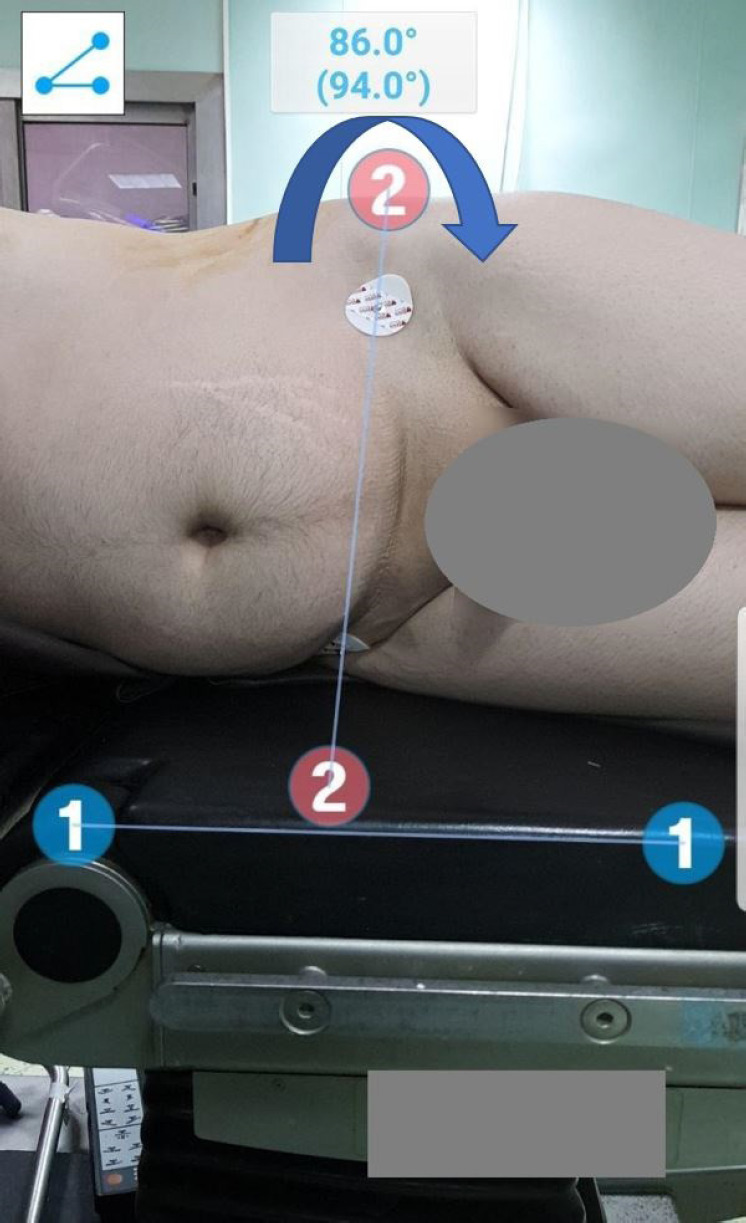
Patient positioned in the lateral decubitus position, the amount of pelvic tilt is measured as the angle between line 1 (table level) and line 2 (line connecting ASIS)
Intraoperatively, the smartphone was placed in a sealable zip plastic bag sterilised by gas plasma sterilisation. Full exposure of the acetabulum after performing initial neck osteotomy was the same for all patients. In the study group, through the proximal extent of the approach, a 4 mm Schanz screw (from the trauma external fixator set) was inserted in the supra-acetabular area about two centimetres proximal to the superior ridge of the acetabulum, and care was taken not to penetrate the acetabulum. A rod from the same set was then connected to the Schanz screw using a clamp, and the smartphone app was used to adjust the angle of the rod to be set to the desired cup abduction angle, which was previously decided based on measured pelvic tilt. Once the desired abduction angle was confirmed, the clamp was tightened, and the angle rechecked and recorded on the app [Figure 2A]. Central acetabular reaming was first performed using a small reamer to remove any central osteophyte. Reaming was progressed, ensuring that the reamer’s handle was parallel to the supra-acetabular rod, and the anteversion was adjusted using the TAL as a reference [Figure 2B]. Once the final reamer was reached, the rod angle was rechecked one final time using the smartphone app. The final acetabular cup was implanted, ensuring that the cup handle was parallel to the supraacetabular rod [Figure 2C].
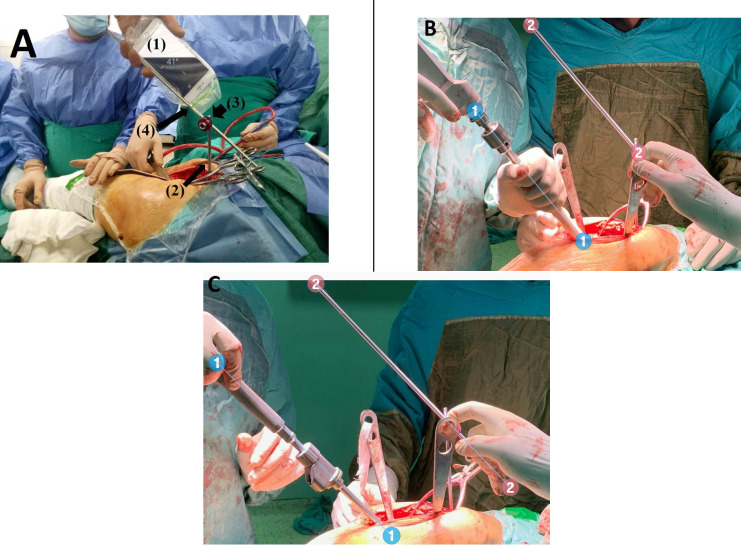
Figure 2.
Smartphone guided cup placement technique
A: angle of a rod connected to the supraacetabular Schanz is adjusted to the desired abduction angle using the smartphone app,
B: reaming is done with the reamer kept parallel to the rod,
C: final cup placement with the handle kept parallel to the rod. (1: smartphone inside a sterilized sealable zip plastic bag with spirit level app adjusted to the desired angle, 2: supraacetabular Schanz, 3: clamp, 4: rod)
All surgical steps followed in the control group were similar to the steps followed in the study group except for the steps where the smartphone app was used. In the control group, the acetabular cup abduction angle was determined visually using the floor or the bed level, while the anteversion was determined using TAL as a reference.
Methods of assessment
Postoperatively, anteroposterior radiographs of the pelvis with both hips were used to measure the postoperative acetabular cup abduction angle using the method described by Jolles et al. (18). In this previous study, the angle was measured between the inter-teardrop as a horizontal reference line and a second line drawn using the long axis of the eclipse formed by the cup using the superolateral edge and inferomedial edge as reference points [Figure 3]. Cup anteversion was also measured in all patients using the method described by Lewinnek et al. (19). All measurements were done using the IC Measure software (The Imaging Source Europe GmbH, Bremen, Germany) by one of the authors who was not the operating surgeon in either of the patient groups.
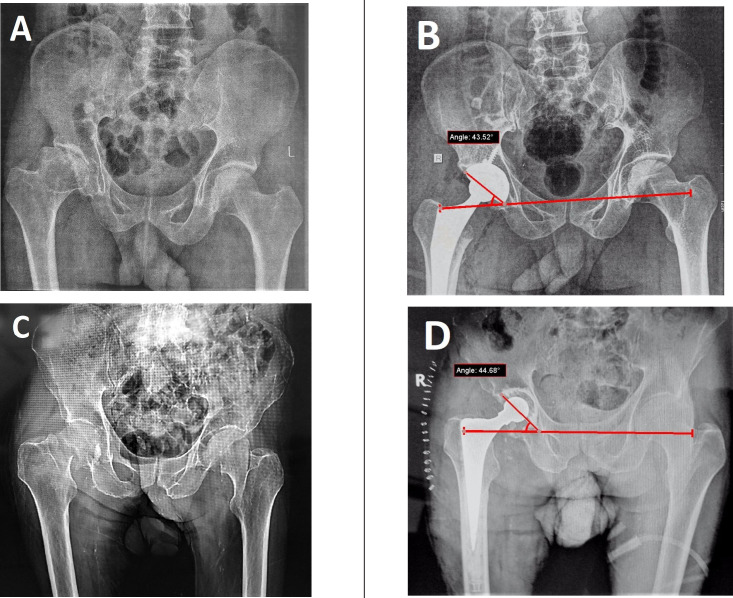
Figure 3.
Pre- and postoperative AP pelvis radiographs of patients in the smartphone (study) group
A: preoperative radiograph of a male patient, 45 years old with dysplastic right hip treated with cementless THA, B: postoperative radiograph.,
C: preoperative radiograph of a male patient 59 years old with fracture neck of the right femur treated with cemented THA, D: postoperative radiograph.
Statistical analysis
A post hoc power calculation using the primary variable of the percentage of cups within the safe zone was performed. Setting the type-I error at 0.05, the power of the study was found to be 81.8. A comparison of demographic and radiographic parameters was compared between the two groups using the t-test for continuous data and the Fisher’s test for categorical data. A P value < 0.05 was considered statistically significant. Statistical analysis was performed using the SPSS version 22 software (SPSS, Chicago, Illinois).
Results
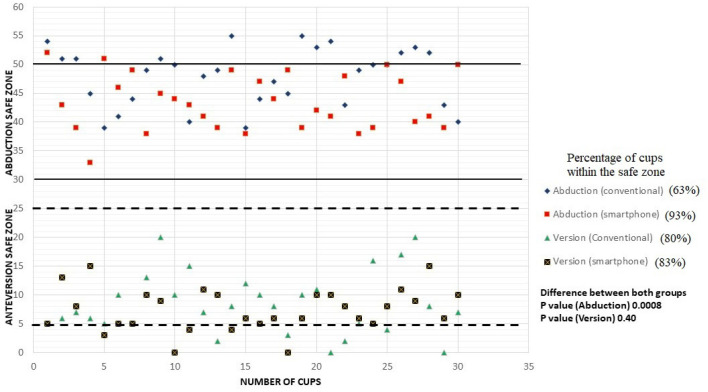
There were 30 patients in each group in this study, and there was no significant difference between the two groups in terms of baseline characteristics and preoperative diagnosis [Table 1]. However, a cementless cup was used in a significantly higher (P=0.001) percentage of patients in the study group when compared to the control group [Table 1]. In the study group, the mean cup abduction angle was significantly lower (P=0.0008), and the acetabular cup was placed within the safe zone in a significantly higher (P<0.001) percentage of patients when compared to the control group [Table 2, Figure 4]. However, there was no significant difference (P=0.40) between the two groups when the mean cup anteversion angle was compared [Table 2, Figure 4]. The average pelvic tilt measured in the study group was +0.9° (SD ± 4.52) and ranged from +7° to -5°.
Table 1.
Comparison of patient demographic data in the conventional free-hand group and smartphone application groups
| Parameters |
Conventional free-hand group
(Control group) |
Smartphone application group
(Study group) |
p value |
|---|---|---|---|
| Number of patients (n) | 30 | 30 | - |
| Age | 58±8.6 (45-72) | 55±2.3 (40-61) | 0.07 |
| Gender Male Female |
18 (60%) 12 (40%) |
20 (67%) 10 (33%) |
0.37 |
| Side Right Left |
13 (43%) 17 (57%) |
16 (53%) 14 (47%) |
0.20 |
| THA Implant Cemented Cementless |
20 (67%) 10 (33%) |
13 (43%) 17 (57%) |
0.001 |
| Diagnosis Osteoarthritis Avascular necrosis NOF fracture Rheumatoid arthritis |
7 (23%) 5 (17%) 15 (50%) 3 (10%) |
6 (20%) 8 (27%) 12 (40%) 4 (13%) |
0.73 |
Data presented as mean ± standard deviation (range) or as number (%).
p <0.05 considered as statistically significant
THA – total hip arthroplasty; NOF – neck of femur
Table 2.
Comparison of postoperative cup abduction angle and “safe zone” placement in the conventional free-hand group and smartphone application groups
| Parameters |
Conventional free-hand group
(Control group) |
Smartphone application group
(Study group) |
p value |
|---|---|---|---|
| Number of patients (n) | 30 | 30 | - |
| Mean Cup Abduction Angle | 48°±5.0° | 43.5°±4.8° | 0.0008 |
| Mean Cup Anteversion angle | 8.4°±5.3° | 7.4°±3.7° | 0.40 |
| Number (%) of cups within the safe zone of abduction | 19 (63) | 27 (93) | <0.001 |
Data presented as mean ± standard deviation (range) or as number (%).
p <0.05 considered as statistically significant (bold)
Figure 4.
Scatter plot showing the percentage of cups (in both groups) placed within the safe zone of abduction and anteversion according to Lewinnek
Discussion
The important finding in this study is that using a smartphone app intraoperatively helps achieve accurate acetabular cup abduction angle and a higher percentage of cups being placed within the safe zone of abduction by a less experienced surgeon when compared to a conventional freehand technique; this proves the hypothesis of this study.
Although safe zone for cup placement target described by Lewinnek et al. is commonly accepted, various definitions of this safe zone have been proposed by both clinical and biomechanical studies where the target safe zone varies between 20° to 55° of abduction and 0° to 40° of anteversion (7, 20, 21). Meermans et al. suggested that placing a digital protractor over the cup inserter handle can improve the accuracy of cup placement compared to visual estimation of the cup position, which may lead to significant error (22). Similarly, navigation systems, while associated with increased cost and time of the procedure, have also been associated with errors (23). Jolles et al. reported that 20% of the press-fit cups were placed outside the desired cup alignment in a computer-assisted THA group (23).
The intraoperative use of smartphone technology in THA for improving the accuracy of acetabular cup placement has been reported previously (14, 15, 24). Peters et al., in a study of 50 THAs where a phone app was used to improved accuracy of acetabular cup placement, reported good results with all cups being placed within the Lewinnek safe zone, with less than 5% difference between the preoperative (native hip inclination), intraoperative (desired inclination angle), and postoperative acetabular inclinations (15). Similarly, Pongkunakorn et al., in a comparative study between conventional versus smartphone app-based THAs reported that the smartphone group had more cups positioned within the Lewinnek safe zone when compared to the conventional group (90.2% vs. 56.1%, P<0.001) (14). These findings are similar to the findings in the current study, where 93% of the cups were placed within the safe zone for cup abduction in the smartphone app group when compared to 63% of cups in the conventional group. However, our smartphone app-based technique was less demanding and more surgeon-friendly compared to the technique described by Pongkunakorn et al., where intra-operative fluoroscopy was also used to confirm the position of the cup and involved inserting a pin in the ASIS outside the surgical approach, making the technique more complex (14).
Callanan et al., in an analysis of 2061 consecutive THAs or hip resurfacing, reported that the risk of malpositioning increased in low-volume surgeons and found that the accuracy of cup placement was only 63% within the targeted safe zone of inclination with a low-volume and less-experienced surgeon (8). However, in an in vitro study by Tay et al., where they compared three methods for cup placement, i.e., freehand, alignment jig, and phone app, to determine the most accurate technique for a young inexperienced surgeon to achieve accurate cup abduction angle, the phone app technique showed significantly higher accuracy when compared to the freehand method (24). This is similar to the findings of the current study, where the accuracy of cup placement improved significantly in the majority of the THAs (93%) performed by a less experienced surgeon with the phone app technique when compared to the freehand technique, where the less experienced surgeon could place the cup within the safe abduction zone in only 63% of the THAs.
Hill et al. reported a 12.7° discrepancy between intraoperative intended cup abduction angle and postoperative radiographic cup inclination when using the floor level as a reference; they attributed this to the unattended pelvis adduction after the patient positioning on the table (25). However, in the current study, we measured the pelvic tilt or adduction using the same phone app used for cup position and found that our patients had a mean pelvic tilt of +0.9° (range, +7° to -5°), which was similar to the mean pelvic tilt reported in the literature (9, 25). This pelvic tilt was adjusted to the final cup abduction angle to eliminate the error, which may be caused due to the pelvic tilt.
This study has some limitations. First, the study’s retrospective design has its limitations and biases, and our results should be validated with a prospective randomised controlled trial. Second, the app technique can only determine the cup abduction angle and not the cup anteversion, which is then dependent on the surgeons’ skill. Third, the measurements were performed by one of the authors, which were not repeated with no interobserver or intraobserver validation. Fourth, the actual surgical time difference between both techniques was not calculated to define whether the smartphone technique will need extra time than the conventional technique. Fifth, as the two patient groups were operated upon in two different hospitals, this could create patient selection bias; however, the two hospitals were located in the same geographical area which makes the basic characteristics of the patients nearly the same. Moreover, no selection was implemented regarding the diagnosis or the complexity of the case to assign patients to either group. Finally, we have not reported any medium or long-term clinical follow-up to detect any incident of instability or dislocation in the current study.
Acknowledgements
None.
References
- 1.Delaunay C, Hamadouche M, Girard J, Duhamel A. What are the causes for failures of primary hip arthroplasties in France? Clinical orthopaedics and related research. 2013;471(12):3863–9. doi: 10.1007/s11999-013-2935-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hailer NP, Weiss RJ, Stark A, Kärrholm J. The risk of revision due to dislocation after total hip arthroplasty depends on surgical approach, femoral head size, sex, and primary diagnosis. Acta Orthopaedica. 2012;83(5):442–8. doi: 10.3109/17453674.2012.733919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noticewala M, Murtaugh TS, Danoff J, Cunn GJ, Shah RP, Geller J. Has the risk of dislocation after total hip arthroplasty performed for displaced femoral neck fracture improved with modern implants? Journal of clinical orthopaedics and trauma. 2018;9(4):281–4. doi: 10.1016/j.jcot.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ha Y-C, Yoo JJ, Lee Y-K, Kim JY, Koo K-H. Acetabular Component Positioning Using Anatomic Landmarks of the Acetabulum. Clinical Orthopaedics and Related Research®. 2012;470(12):3515–23. doi: 10.1007/s11999-012-2460-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patil S, Bergula A, Chen PC, Colwell CWJ, D’Lima DD. Polyethylene Wear and Acetabular Component Orientation. JBJS. 2003;85(suppl_4):56–63. doi: 10.2106/00004623-200300004-00007. [DOI] [PubMed] [Google Scholar]
- 6.Little NJ, Busch CA, Gallagher JA, Rorabeck CH, Bourne RB. Acetabular polyethylene wear and acetabular inclination and femoral offset. Clinical Orthopaedics and Related Research®. 2009;467(11):2895–900. doi: 10.1007/s11999-009-0845-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60(2):217–20. [PubMed] [Google Scholar]
- 8.Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, et al. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clinical orthopaedics and related research. 2011;469(2):319–29. doi: 10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beverland DE, O’Neill CK, Rutherford M, Molloy D, Hill JC. Placement of the acetabular component. Bone Joint J. 2016;98-b(1 Suppl A):37–43. doi: 10.1302/0301-620X.98B1.36343. [DOI] [PubMed] [Google Scholar]
- 10.Archbold HA, Mockford B, Molloy D, McConway J, Ogonda L, Beverland D. The transverse acetabular ligament: an aid to orientation of the acetabular component during primary total hip replacement: a preliminary study of 1000 cases investigating postoperative stability. The Journal of bone and joint surgery. British volume. 2006;88(7):883–6. doi: 10.1302/0301-620X.88B7.17577. [DOI] [PubMed] [Google Scholar]
- 11.Gandhi R, Marchie A, Farrokhyar F, Mahomed N. Computer navigation in total hip replacement: a meta-analysis. International Orthopaedics. 2009;33(3):593–7. doi: 10.1007/s00264-008-0539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tagomori H, Kaku N, Tabata T, Kubota Y, Tsumura H. Comparison of cementless and cemented cups in revision total hip arthroplasty using a computed tomography-based navigation system. Journal of clinical orthopaedics and trauma. 2020;11(Suppl 2):S206–s10. doi: 10.1016/j.jcot.2019.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morgenstern R, Su EP. Handheld navigation for direct anterior total hip arthroplasty. Seminars in Arthroplasty. 2018;29(3):153–6. [Google Scholar]
- 14.Pongkunakorn A, Chatmaitri S, Diewwattanawiwat K. Use of smartphone to improve acetabular component positioning in total hip athroplasty: A comparative clinical study. Journal of orthopaedic surgery (Hong Kong). 2019;27(1):2309499019825578. doi: 10.1177/2309499019825578. [DOI] [PubMed] [Google Scholar]
- 15.Peters FM, Greeff R, Goldstein N, Frey CT. Improving Acetabular Cup Orientation in Total Hip Arthroplasty by Using Smartphone Technology. The Journal of Arthroplasty. 2012;27(7):1324–30. doi: 10.1016/j.arth.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 16.Pai VS. A Modified Direct Lateral Approach in Total Hip Arthroplasty. Journal of Orthopaedic Surgery. 2002;10(1):35–9. doi: 10.1177/230949900201000107. [DOI] [PubMed] [Google Scholar]
- 17.Khalifa AA, Bakr HM, Said E, Mahran MA. Technical Note on Using Intraoperative Smartphone Applications to Adjust Cup Inclination Angle during Total Hip Arthroplasty (THA) Archives of Bone and Joint Surgery. 2020;8(6):734. doi: 10.22038/abjs.2020.44466.2217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: A multivariate analysis. The Journal of Arthroplasty. 2002;17(3):282–8. doi: 10.1054/arth.2002.30286. [DOI] [PubMed] [Google Scholar]
- 19.Alzohiry MA, Abdelnasser MK, Moustafa M, Mahran M, Bakr H, Khalifa Y, et al. Accuracy of plain antero-posterior radiographic-based methods for measurement of acetabular cup version. Int Orthop. 2018;42(12):2777–85. doi: 10.1007/s00264-018-3984-x. [DOI] [PubMed] [Google Scholar]
- 20.Elkins JM, Callaghan JJ, Brown TD. The 2014 Frank Stinchfield Award: The ‘Landing Zone’ for Wear and Stability in Total Hip Arthroplasty Is Smaller Than We Thought: A Computational Analysis. Clinical Orthopaedics and Related Research®. 2015;473(2):441–52. doi: 10.1007/s11999-014-3818-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abdel MP, von Roth P, Jennings MT, Hanssen AD, Pagnano MW. What Safe Zone? The Vast Majority of Dislocated THAs Are Within the Lewinnek Safe Zone for Acetabular Component Position. Clinical Orthopaedics and Related Research®. 2016;474(2):386–91. doi: 10.1007/s11999-015-4432-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meermans G, Goetheer-Smits I, Lim RF, Van Doorn WJ, Kats J. The difference between the radiographic and the operative angle of inclination of the acetabular component in total hip arthroplasty: use of a digital protractor and the circumference of the hip to improve orientation. The bone & joint journal. 2015;97(5):603–10. doi: 10.1302/0301-620X.97B5.34781. [DOI] [PubMed] [Google Scholar]
- 23.Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted Cup Placement Techniques in Total Hip Arthroplasty Improve Accuracy of Placement. Clinical Orthopaedics and Related Research (1976-2007). 2004;426:174–9. doi: 10.1097/01.blo.0000141903.08075.83. [DOI] [PubMed] [Google Scholar]
- 24.Tay XW, Zhang BX, Gayagay G. Use of iPhone technology in improving acetabular component position in total hip arthroplasty. Arthroplasty Today. 2017;3(3):167–70. doi: 10.1016/j.artd.2017.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hill JC, Gibson DP, Pagoti R, Beverland DE. Photographic measurement of the inclination of the acetabular component in total hip replacement using the posterior approach. The Journal of bone and joint surgery. British volume. 2010;92(9):1209–14. doi: 10.1302/0301-620X.92B9.24476. [DOI] [PubMed] [Google Scholar]