Abstract
Background Context:
Health can impact work performance through absenteeism, time spent away from work, and presenteeism, inhibited at-work performance. Low back pain is common and costly, both in terms of direct medical expenditures and indirect reduced work performance.
Purpose:
Surgery for lumbar spinal pathology is an important part of treatment for patients who do not respond to nonsurgical management. While the indirect costs of return to work and absenteeism among employed patients undergoing lumbar spine surgery have been studied, little work has been done to quantify presenteeism before and after lumbar spine surgery.
Study Design Setting:
Prospective cohort study at a single high-volume urban musculoskeletal specialty hospital.
Patient Sample:
Patients undergoing single-level lumbar spinal fusion and/or decompression surgery.
Outcome Measures:
Presenteeism and absenteeism were measured using the World Health Organization’s Health and Work Performance Questionnaire before surgery, as well as 6 weeks, 6 months, and 12 months after surgery.
Methods:
Average presenteeism and absenteeism were evaluated at pre-surgical baseline and each follow-up timepoint. Monthly average time lost to presenteeism and absenteeism were calculated before surgery and 12 months after surgery. Study data were collected and managed using REDCap electronic data capture tools with support from Clinical and Translational Science Center grant, UL1TR002384. One author discloses royalties, private investments, consulting fees, speaking/teaching arrangements, travel, board of directorship, and scientific advisory board membership totaling >$300,000.
Results:
We enrolled 134 employed surgical patients, among whom 115 (86%) responded at 6 weeks, 105 (78%) responded at 6 months, and 115 (86%) responded at 12 months. Preoperatively, mean age was 56.4 years (median 57.5), and 41.0% were women; 68 (50.7%) had only decompressions, while 66 (49.3%) had fusions. Among respondents at each time point, 98%, 92%, and 92% were still employed, among whom 76%, 96%, and 96% had resumed working, respectively (median 29 days). Average at-work performance among working patients (who responded at each pair of timepoints) moved from 75.4 to 78.7 between baseline and 6 weeks, 71.8 to 85.9 between baseline and 6 months, and 73.0 to 88.1 between baseline and 12 months. Gains were concentrated among the 52.0% of patients whose at-work performance was declining (and low) leading up to surgery. Average absenteeism was relatively unmoved between baseline and each follow-up. Before surgery, the monthly average time lost to presenteeism and absenteeism was 19.8% and 18.9%, respectively; 12 months after surgery, these numbers were 9.7% and 16.0%; changes represent a mitigated loss of 13.0 percentage points of average monthly value.
Conclusions:
Presenteeism and absenteeism contributed roughly evenly to preoperative average monthly lost time. Although average changes in absenteeism and 6-week at-work performance were small, average changes in at-work performance at 6 and 12 months were significant. Cost-benefit analyses of lumbar spine surgery should therefore consider improved presenteeism, which appears to offset some of the direct and indirect costs of surgical treatment.
Keywords: presenteeism, work performance, absenteeism, return to work, employment, spine surgery, lumbar, fusion, decompression, value
Introduction
The effect of individual health on job effectiveness can operate through at least two mechanisms: absenteeism and presenteeism. While most people are familiar with absenteeism – time spent away from work – fewer people are familiar with presenteeism, which refers to inhibited at-work performance from health or illness [1]. There is evidence to suggest that health-related absenteeism and presenteeism cost hundreds of billions of US dollars each year [2]. Most of those losses can be attributed to presenteeism, which can be higher than direct medical costs [3,4], across different occupations [5] and medical conditions [6-8].
Musculoskeletal disorders were estimated to have been responsible for $380.9 billion in health care spending in 2016 [9]. Among 154 conditions, low back and neck pain were responsible for the highest amount of healthcare spending ($134.5 billion) [9]. Musculoskeletal disorders, particularly those related to the lumbar spine, are also responsible for an enormous amount of lost workplace performance. From 2013 to 2015, an annual average of nearly 29% of the adult US population reported having low back pain during the last 3 months; among 6% of the adult working population who reported that they were limited or unable to work because of a medical condition, about 25% reported this was because of a back or neck problem [10]. Moreover, 385,000 workdays were lost due to back or neck pain in 2008, a figure that has fluctuated, but remained steady since 2012 [10].
While studies have established increased presenteeism in patients with broad musculoskeletal disorders [4], osteoarthritis [1,11-15], chronic knee pain [16], low back pain [17,18], axial spondyloarthritis [19], hand surgery [20,21], and total joint arthroplasty [22,23], there is little known specifically about presenteeism before and after lumbar spine surgery. Return to work [24-30] and absenteeism [31,32] after spine surgery are more commonly studied (e.g., one study of 4,694 American patients found 82% of patients had returned to work by 3 months after lumbar spine surgery [24]; another of 29,826 Swedish patients with lumbar disc herniation or spinal stenosis estimated the mean change in absenteeism one year before to one year after surgery was ~2.0 days [31]). Surgery for lumbar spinal pathology is an important part of treatment for patients who do not respond to nonsurgical management; the number of spinal fusion procedures in the US more than doubled from 220,000 in 1998 to 445,000 in 2013 [33].
One study touching on presenteeism interviewed patients undergoing lumbar surgery preoperatively about expected improvement in job performance and 2-years postoperatively about actual improvement [34]. However, no study to our knowledge has prospectively measured at-work performance (i.e., presenteeism) before and after surgery and measured improvement directly. As a result, cost effectiveness analyses related to spine surgery similarly often do not account for indirect costs associated with work beyond absenteeism, if at all [35,36]. Surgery, while having a significant up-front cost (e.g., among a cohort of 2.5 million commercially insured patients between 2008 and 2015 diagnosed with low back or lower extremity pain, only 1.2% had surgery, yet patients accounted for 29.3% of total 12-month costs [37]), may still lead to improved presenteeism without worsening absenteeism, and hence, from a societal or employer perspective, offset some of the direct and indirect costs of treatment.
The aim of this study was therefore to quantify presenteeism, absenteeism, and return to work among employed patients before and 6 weeks, 6 months, and 12 months after single-level lumbar spinal fusion and/or decompression, calculate how presenteeism and absenteeism changed, and quantify the monthly expected percentage of hours lost to presenteeism and absenteeism.
Methods
This prospective cohort study used a convenience sample of patients visiting a single high-volume urban musculoskeletal specialty hospital in the United States. Reporting followed STROBE guidelines [38]. Patients were eligible if 18 years or older, not retired, and scheduled to undergo single-level lumbar spinal fusion and/or decompression surgery between May 2018 and December 2019. We chose these procedures in the interest of gathering data on a sizeable but homogenous sample of patients undergoing a commonly performed spine surgery. Patients who were scheduled for surgery and had a valid email address in our electronic medical record were contacted by email 2 weeks before their procedure and invited to consent to participate, confirm employment and eligibility, and complete a preoperative survey [39,40]. We only attempted to enroll patients with a single email outreach. We did not attempt to contact patients for enrollment in-person during any of their pre-surgical screening or other appointments, nor via telephone, nor letter, nor through repeated email requests. The resulting cohort of patients who responded to this single email invitation constituted the convenience sample. Respondents were considered enrolled if they confirmed employment status and completed the online presenteeism questions preoperatively. Respondents were excluded if they were on workers’ compensation. Enrolled patients were invited to complete follow-up surveys 6 weeks after surgery, 6 months after surgery, and 12 months after surgery. Patients who did not complete each follow-up were reminded twice over email and called (at most one voicemail was left). At 12 months, patients were additionally mailed paper versions if prior methods did not produce a response. The study was approved by our hospital’s institutional review board.
Surveys
Presenteeism and absenteeism were quantified using self-reported patient survey responses using the World Health Organization’s Health and Work Performance Questionnaire (WHO-HPQ) [41,42]. Details of the survey instruments, including their appropriateness in this context, have been described in our prior report describing patients’ presenteeism and absenteeism before and after total joint arthroplasty [23]. The primary presenteeism battery contains three questions measured on a scale of 0 to 10 (performance from worst to top), asking about the performance of most workers in a job like yours, your performance over the last year or two, and your performance over the last 4 weeks. The third question is our focus; we multiply it by 10 to represent the percentage of time productive at work; this is called “absolute presenteeism” [43]. The absenteeism batteries ask questions about the last seven days (number of hours and days expected to work and hours actually worked) and about the last 28 days (number of workdays missed for personal health reasons, family health reasons—given patients are often caregivers for family members, other reasons including vacation, and days worked extra). We also ask about job industry; responsibilities at work; accommodations made by employer; commute; physical activities (job requirements and general difficulty); and a single-assessment numerical evaluation (SANE) of spine health. Follow-up surveys were identical to each other and asked about changes in employment status, whether and when the patient returned to work, as well as the same presenteeism and absenteeism questions asked as at baseline.
Analyses
Descriptive statistics were used to summarize preoperative patient characteristics, including demographics (age, BMI, sex, race, ethnicity), clinical characteristics (SANE score, procedure type, ambulatory versus inpatient), and job-related characteristics. Changes in employment status were described at each follow-up time point, including how many patients were still employed. We also report the average and median days to return to work. Given that patients could input return to work dates at each follow-up time point, if there were differences between responses, we used the response from the earliest available follow-up time point (assuming it would be most accurate).
Our primary metric was change in absolute presenteeism between baseline and 12 months, though we also evaluated its change between baseline and 6 weeks, as well as baseline and 6 months. Owing to non-normality (found to be ubiquitous based on visual inspections of the underlying distributions, visual inspection of quantile-quantile plots of the underlying variables against that of the normal distribution, in addition to Shapiro-Wilk tests for normality), we evaluated whether absolute presenteeism significantly differed between baseline and each time point using Wilcoxon matched-paired signed rank tests (among patients responding at each pair of timepoints). We further evaluated the percentage of patients who reported perfect (100/100) at-work performance between baseline and each follow-up time point using 2-sided, 2-sample tests of proportions. We also stratified our presenteeism analyses by whether patients reported static (identical), declining, or improving performance leading up to surgery by comparing the second and third presenteeism questions from the preoperative survey.
We next evaluated how each 7-day and 28-day absenteeism question differed between baseline and each time point using Wilcoxon matched-paired signed rank tests (again, given inspection of the relevant distributions and the noting of ubiquitous non-normality).
We also quantified the monthly average value an employer is expected to lose to presenteeism and absenteeism in terms of the percentage of hours lost. We used a human capital accounting approach [4,5,44] to combine presenteeism and absenteeism at a given time point, assuming the percentage of time scheduled to work but absent according to the 28-day metrics (combining time away because of own health problems, family health problems, or for other reasons, but not accounting for days worked extra) was lost to absenteeism, and the percentage of remaining time spent present but not productive at work was lost to presenteeism. We performed these analyses independently at baseline and 12 months after surgery and report the resulting average percentages across patients. At 12 months, among patients who reported having returned to work, but who did not report their absenteeism or presenteeism, we impute each to the mean among patients who did report. We also included patients who reported still being employed but not yet having returned to work, assuming their absenteeism was 100% of their baseline scheduled hours. Patients who were no longer employed were excluded, though we conducted a sensitivity analysis including these patients, but assuming 100% absenteeism. This latter calculation represents a societal perspective broader than any particular pre-surgical employer.
Finally, we conducted a heterogeneity analysis with respect to type of surgery. In particular, we compared the above metrics at baseline and 12 months between patients undergoing only decompressions versus fusions using unpaired two-sample t-tests or tests of proportions as appropriate.
All analyses were performed with Stata/SE version 14.2 for Windows.
Results
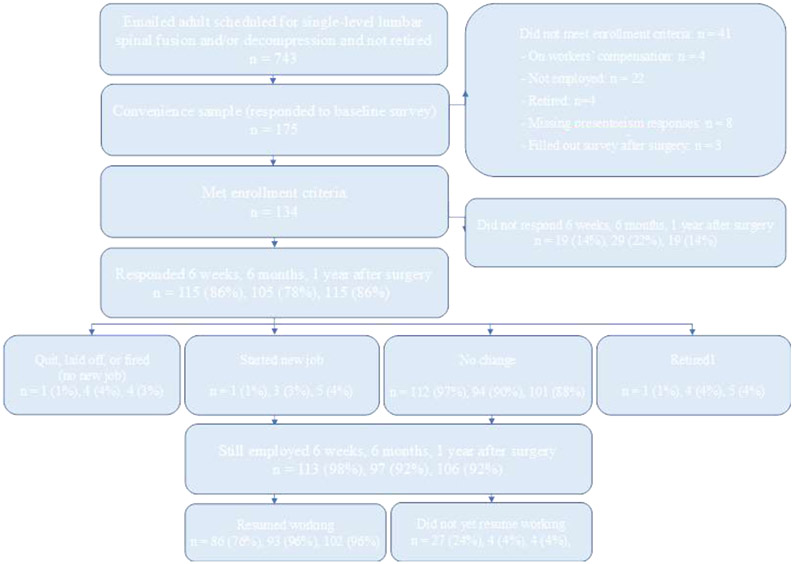
We initially emailed 743 patients. Our sample consisted of 175 patients (24% response rate) who filled out a preoperative survey, among whom 41 (23%) did not meet our enrollment criteria (Figure 1). This left 134 enrolled patients, among whom 115 (86%) responded at 6 weeks, 105 (78%) responded at 6 months, and 115 (86%) responded at 12 months.
Figure 1.
Patient enrollment and follow-ups. One person who was retired at 1 year also reported being laid off; only counted above as retired. Percentages may not add to 100% because of rounding. We sent emails to 743 patients scheduled for single-level lumbar spinal fusion and/or decompression who were not retired according to our electronic medical record, inviting them to participate. This included 88 patients who were not employed according to our electronic medical record, 34 patients who were disabled, and 10 with missing or unknown work status. We emailed these patients because, although we the electronic medical record is typically reliable if it states someone is retired, there is enough year-to-year change in employment status for non-retirees that these other statuses can be temporary.
Preoperatively, mean age was 56.4 years (median 57.5), 41.0% were women, 90.3% were white, and 92.5% were not Hispanic (Table 1). Mean body mass index (BMI) was 28.1 kg/m^2 (median 27.4), while mean SANE score was 42.4/100 (median 40/100). In terms of procedures performed, 68 (50.7%) patients had only decompressions, while 66 (49.3%) had fusions (with or without decompression); 33.6% were ambulatory and 66.4% were inpatient surgeries.
Table 1.
Demographics and pre-operative work characteristics
| Variable | Descriptive Statistics (n = 134) | ||||
|---|---|---|---|---|---|
| Mean | SD | Median | Min | Max | |
| Age (years) | 56.4 | 10.9 | 57.5 | 26.0 | 84.0 |
| BMI (kg/m2) | 28.1 | 5.2 | 27.4 | 18.7 | 47.4 |
| SANE score * | 42.4 | 21.6 | 40.0 | 0.0 | 90.0 |
| Sex | Number (%) | ||||
| Female | 55 | 41.0% | |||
| Male | 79 | 59.0% | |||
| Race | Number (%) | ||||
| White or Caucasian | 121 | 90.3% | |||
| Asian | 3 | 2.2% | |||
| Black or African American | 2 | 1.5% | |||
| Other | 2 | 1.5% | |||
| Missing | 6 | 4.5% | |||
| Ethnicity | Number (%) | ||||
| Not Hispanic or Latino | 124 | 92.5% | |||
| Hispanic or Latino | 4 | 3.0% | |||
| Missing | 6 | 4.5% | |||
| Procedure Type | Number (%) | ||||
| Decompression only | 68 | 50.7% | |||
| Fusion | 66 | 49.3% | |||
| Patient Class | Number (%) | ||||
| Ambulatory | 45 | 33.6% | |||
| Inpatient | 89 | 66.4% | |||
| Employment | Number (%) | ||||
| Yes, full-time | 109 | 81.3% | |||
| Yes, part-time | 8 | 6.0% | |||
| Self-employed | 17 | 12.7% | |||
| How do you get to work? | Number (%) | ||||
| Bike | 1 | 0.7% | |||
| Drive | 64 | 47.8% | |||
| Public Transportation | 27 | 20.1% | |||
| Taxi | 5 | 3.7% | |||
| Walk | 5 | 3.7% | |||
| Work from home | 18 | 13.4% | |||
| Missing | 14 | 10.4% | |||
| Job Accommodations | Number (%) | ||||
| Change job to something you can do | 6 | 4.5% | |||
| Change time to start and stop work | 16 | 11.9% | |||
| More breaks and rest periods | 9 | 6.7% | |||
| Shorter work day | 3 | 2.2% | |||
| Someone to help you out | 7 | 5.2% | |||
| Special equipment | 6 | 4.5% | |||
| Special transportation | 2 | 1.5% | |||
| None | 71 | 53.0% | |||
| Missing | 14 | 10.5% | |||
SANE = Single Assessment Numerical Evaluation
Before surgery, most patients were employed full-time (81.3%) (Table 1). A majority commuted by driving (47.8%) or public transportation (20.1%). Approximately half had not been provided any specific job accommodations (53.0%); the most popular job accommodation was changing the time of starting and stopping work (11.9%).
The highest percentage of patients reported a job in educational services (11.2%), finance and insurance (10.4%), and professional, scientific, and technical services (9.7%), although many also reported some other sector (12.7%) (Supplemental Table 1). In terms of main job responsibilities, 29.1% reported professional (e.g., engineer, accountant, systems analyst), and 27.6% reported executive, administrator, or senior manager.
Squatting and lifting were seldom or never required by 52.3% and 50.0% of patients’ jobs, respectively (Supplemental Table 2). Standing, walking, and sitting, on the other hand, were always or often required by 61.2%, 59.0%, and 75.4% of patients’ jobs, respectively. Most patients had at least moderate difficulty with squatting (52.2%), standing (73.9%), lifting (64.2%), and walking (70.9%). Sitting was the only exception; 43.3% of patients had at least moderate difficulty sitting, but 44.0% had a little or no difficulty.
Turning to preoperative presenteeism and absenteeism, patients reported that most workers at-work job performance was 7.9/10 (median 8/10), their own usual performance over the last year or two was 8.6/10 (median 9/10), and their overall job performance on days worked in the past 4 weeks was 7.3/10 (median 8/10) (Table 2). Comparing the second and third questions, 44.0% of patients reported static at-work performance in the year or two before surgery (i.e., answered the same to the second and third presenteeism questions), 53.0% reported declining at-work performance in the year or two before surgery (i.e., answered a higher number in the second than third question), and 3.0% reported improving at-work performance (i.e., answered a lower number in the second than third question).
Table 2.
Pre-operative presenteeism and absenteeism
| Variable | Descriptive Statistics (n=134) | ||||
|---|---|---|---|---|---|
| Presenteeism (0: Worst, 10: Top) How would you rate the usual performance of… |
Mean | SD | Median | Min | Max |
| … most workers in a job similar to yours? | 7.9 | 1.7 | 8.0 | 0.0 | 10.0 |
| … your usual job performance over the past year or two? | 8.6 | 1.6 | 9.0 | 0.0 | 10.0 |
| … your overall job performance on the days you worked during the past 4 weeks (28 days)? | 7.3 | 2.3 | 8.0 | 0.0 | 10.0 |
| Absenteeism (7-Day Recall) | Mean | SD | Median | Min | Max |
| How many days are you expected to work in a typical 7-day week? | 5.1 | 0.8 | 5.0 | 2.0 | 7.0 |
| How many hours does your employer expect you to work in a typical 7-day week? | 38.9 | 14.1 | 40.0 | 3.0 | 80.0 |
| About how many hours altogether did you work in the past 7 days? | 40.5 | 18.7 | 44.0 | 0.0 | 97.0 |
| Absenteeism (28-Day Recall) In the past 4 weeks (28 days), how many days did you… |
Mean | SD | Median | Min | Max |
| … miss work because of problems with your physical or mental health? | 1.8 | 3.2 | 0.0 | 0.0 | 20.0 |
| … miss work because of problems with a family member's physical or mental health? | 0.4 | 1.1 | 0.0 | 0.0 | 7.0 |
| … miss work for any other reason (including vacation)? | 1.5 | 3.0 | 0.0 | 0.0 | 16.0 |
| … come in early, go home late, work extra from home, or work on your day off? | 6.8 | 8.5 | 3.0 | 0.0 | 28.0 |
Note: 7-day absenteeism questions answered by n=129. 28-day absenteeism questions answered by n=124.
Preoperatively, patients were expected to work 5.1 days on average per week (median 5.0), or 38.9 hours (median 40.0), and actually worked 40.5 hours (median 44.0) on average in the past 7 days (Table 2). In terms of preoperative absences in the past 28 days, patients missed an average of 1.8 days (median 0.0) because of problems with their health, 0.4 days (median 0.0) because of problems with a family member’s health, 1.5 days (median 0.0) for other reasons including vacation, but also worked extra on 6.8 days (median 3.0) (Table 2).
Among patients who responded at 6 weeks, 6 months, and 12 months, 97%, 90%, and 88% had no change in job status, respectively. Remaining patients either started a new job; retired; or quit, were laid off, or were fired without starting a new job (Figure 1). Combining patients with no change in job status and those who started a new job, 98%, 92%, and 92% were still employed at each follow-up time point, among whom 76%, 96%, and 96% had resumed working, respectively. Patients who had resumed work and reported the relevant return date took an average of 46.1 days (median 29 days) to return to work after surgery.
Turning to absolute presenteeism, among patients who responded at baseline and follow-up (and by that point had resumed work), average at-work performance moved from 75.4 to 78.7 between baseline and 6 weeks, 71.8 to 85.9 between baseline and 6 months, and 73.0 to 88.1 between baseline and 12 months (Table 3). While Wilcoxon matched-paired signed rank tests indicated that distributional changes between baseline and 6 weeks were not statistically significant (p=0.1461), changes between baseline and 6 months, as well as between baseline and 12 months, were both statistically significant (p<0.0001). It is not surprising that the baseline average is higher at 6 weeks; it is only calculated among patients who have already returned to work, and it is intuitive that patients who returned by 6 weeks would be relatively healthier and more productive preoperatively.
Table 3.
Changes in presenteeism and absenteeism at pairs of time points
| Presenteeism | Before Surgery to 6 Weeks After |
Before Surgery to 6 Months After |
Before Surgery to 1 Year After |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean Before |
Mean After |
Mean Δ |
Rank P- value |
N | Mean Before |
Mean After |
Mean Δ |
Rank P- value |
N | Mean Before |
Mean After |
Mean Δ |
Rank P- value |
|
| Absolute Presenteeism | 85 | 75.4 | 78.7 | 3.3 | 0.1461 | 90 | 71.8 | 85.9 | 14.1 | <0.0001 | 100 | 73.0 | 88.1 | 15.1 | <0.0001 |
| Full Performance (Absolute Presenteeism = 100%) | 85 | 17.6% | 18.8% | 1.2% | 0.8426* | 90 | 14.4% | 28.9% | 14.5% | 0.0187* | 100 | 16.0% | 29.0% | 13.0% | 0.0277* |
| Absenteeism (7-Day Recall) | Before Surgery to 6 Weeks After |
Before Surgery to 6 Months After |
Before Surgery to 1 Year After |
||||||||||||
| N | Mean Before |
Mean After |
mean Δ |
Rank P- value |
N | Mean Before |
Mean After |
Mean Δ |
Rank P- value |
N | Mean Before |
Mean After |
Mean Δ |
Rank P- value |
|
| How many days are you expected to work in a typical 7-day week? | 79 | 5.15 | 5.06 | −0.08 | 0.196 | 87 | 5.13 | 5.06 | −0.07 | 0.3716 | 95 | 5.13 | 4.98 | −0.14 | 0.0766 |
| How many hours does your employer expect you to work in a typical 7-day week? | 80 | 41.24 | 39.69 | −1.54 | 0.3191 | 87 | 39.68 | 39.13 | −0.55 | 0.8578 | 95 | 39.19 | 37.61 | −1.58 | 0.1892 |
| About how many hours altogether did you work in the past 7 days? | 80 | 43.33 | 40.16 | −3.17 | 0.4232 | 87 | 41.21 | 40.84 | −0.36 | 0.9897 | 96 | 41.48 | 38.88 | −2.60 | 0.1551 |
| Absenteeism (28-Day Recall) In the past 4 weeks (28 days), how many days did you… |
Before Surgery to 6 Weeks After |
Before Surgery to 6 Months After |
Before Surgery to 1 Year After |
||||||||||||
| N | Mean Before |
Mean After |
Mean Δ |
Rank P- value |
N | Mean Before |
Mean After |
Mean Δ |
Rank P- value |
N | Mean Before |
Mean After |
Mean Δ |
Rank P- value |
|
| … miss work because of problems with your physical or mental health? | 78 | 1.88 | 3.17 | 1.28 | 0.6838 | 83 | 1.95 | 0.90 | −1.05 | <0.0001 | 90 | 1.68 | 0.38 | −1.29 | <0.0001 |
| … miss work because of problems with a family member's physical or mental health? | 78 | 0.33 | 0.22 | −0.12 | 0.3618 | 83 | 0.40 | 0.28 | −0.12 | 0.39 | 90 | 0.39 | 0.28 | −0.11 | 0.3813 |
| … miss work for any other reason (including vacation)? | 78 | 1.44 | 1.27 | −0.17 | 0.0633 | 83 | 1.43 | 1.34 | −0.08 | 0.9923 | 90 | 1.39 | 1.97 | 0.57 | 0.9648 |
| … come in early, go home late, work extra from home, or work on your day off? | 79 | 7.78 | 6.82 | −0.96 | 0.3554 | 83 | 6.89 | 6.78 | −0.10 | 0.6899 | 89 | 7.00 | 7.61 | 0.61 | 0.832 |
Note: P-values are from Wilcoxon signed-rank tests, except those with an asterisks, which are from two-sample test of proportions.
The proportion of patients who reported full (100/100) performance moved from 17.6% to 18.8% between baseline and 6 weeks (p=0.8426), from 14.4% to 28.9% between baseline and 6 months (p=0.0187), and from 16.0% to 29.0% between baseline and 12 months (p=0.0277) (Table 3).
Among patients whose performance was declining before surgery and who responded at baseline and follow-up (at by that point had resumed work), average at-work performance moved from 61.8 to 73.9 between baseline and 6 weeks, 60.4 to 85.0 between baseline and 6 months, 61.4 to 86.4 between baseline and 12 months. Wilcoxon matched-paired signed rank tests indicated all underlying distributional changes were significant (p=0.0002, p<0.0001, p<0.0001, respectively). Average at-work performance for patients whose performance was static leading up to surgery was essentially flat between baseline and each follow-up time point (averages ranging from 85 to 90). That is, the gains in average at-work performance were concentrated among patients whose at-work performance was declining (and low) leading up to surgery.
Turning to 7-day absenteeism, among patients who responded at baseline and follow-up (and by that point had resumed work), the average number of days expected to work in a typical week was always approximately 5 days for each pair of time points (Table 3). A similar result held for the average number of hours expected to work in a typical week, always approximately 40 hours at each pair of time points. Average differences were greatest between baseline and 12 months, dropping by 0.14 days and 1.58 hours, respectively. None of the underlying distributional changes for these, as well as between other pairs of time points, were statistically significant. Average actual hours worked over the past seven days also were always approximately 40 hours for each pair of time points, but again no distributional differences were statistically significant, aligning with the fact that the mean differences were always small in magnitude (no greater than 3.2 hours per month).
For 28-day absenteeism, among patients who responded at baseline and follow-up (and by that point had resumed work), average reported days missed because of own’s own health moved from 1.88 to 3.17 days between baseline and 6 weeks, from 1.95 to 0.90 days between baseline and 6 months, and from 1.68 to 0.38 days between baseline and 12 months (Table 3). Wilcoxon matched-paired signed rank tests indicated the distributional changes were not statistically significant between baseline and 6 weeks (p=0.6838) but were between baseline and 6 months and between baseline and 12 months (both p<0.0001). Average reported days missed because of family member’s health was always small in magnitude (0.2 to 0.4 days); no difference between pairs of time points was statistically significant. The same was true for average days missing work for any other reason (including vacation), which held between 1 and 2 days with no statistically significant changes, as well as average days working extra, which held between 6 and 8 days with no statistically significant changes.
Combining metrics, the monthly average value an employer was estimated to lose to presenteeism and absenteeism before surgery was 19.8% and 18.9%, respectively (i.e., a combined loss of 38.7%). Said differently, before surgery, an employer would only reap 61.3% of an average employee’s monthly value because of presenteeism and absenteeism. At 12 months after surgery, the monthly average value an employer was estimated to lose to presenteeism and absenteeism was 9.7% and 16.0%, respectively (i.e., a combined loss of 25.7%). That is, 12 months after surgery, an employer would reap 74.3% of an average employee’s monthly value. Relative to preoperative baseline, this represents a mitigated loss of 13.0 percentage points of average value per month. Even if we were to include patients at 12 months who were no longer employed (and assume 100% absenteeism), thereby taking a societal instead of an employer perspective, an average worker would still be estimated to produce at 68.5% of full value, or a mitigated loss of 7.2 percentage points of value per month relative to baseline.
Finally, our heterogeneity analysis comparing patients undergoing only decompressions to fusions yielded one clinically meaningful difference between the groups: conditional on still working, as well as returning to work, patients undergoing fusions returned a mean 56.9 days after surgery while patients undergoing only decompressions returned a mean 36.6 days after (p=0.02); medians were 19.0 days and 37.9 days, respectively. No other differences were statistically significant, including the percentage of respondents still working (89% versus 96%, p=0.15); conditional on still working, the percentage having already returned to work (95% versus 92%, p=0.52); mean baseline absolute presenteeism (73.4 v 72.7, p=0.87); mean 12-month absolute presenteeism (87.0 v 89.3, p=0.36); mean change in absolute presenteeism from baseline to 12 months (15.4 v 14.8, p=0.90); 53% of patients had declining productivity leading up to surgery in both groups; mean baseline 28-day total absences (3.9 v 3.5 days, p=0.59); mean 12-month 28-day total absences (3.0 v 2.4, p=0.55); and mean change in 28-day total absences from baseline to 12 months among those answering at both time points (−1.0 vs. −0.6, p=.75). Numbers were similar and statistically indistinguishable between groups for 7-day absences as well. Monthly average value an employer was estimated to lose to presenteeism and absenteeism before and 12 months after surgery was therefore also similar and statistically indistinguishable between groups.
Discussion
We have shown that employed patients concentrated in professional, executive, and administrative roles (whose jobs often involve standing, walking, and sitting) undergoing single-level lumbar spinal surgery (decompression, fusion, or both) report substantial preoperative absenteeism and presenteeism. In terms of average value of an employee’s time lost before surgery, about half was attributable to presenteeism and half to absenteeism (19.8% and 18.9%, respectively), which is consistent with prior reports of presenteeism being just as (if not more) costly than absenteeism [3,4]. It is also consistent with lack of impact of pre-surgical nonoperative treatment among these patients. Six weeks after surgery 98% of patients were still employed, among whom 76% had returned to work; by 12 months after surgery, 92% were still employed, among whom 96% had returned to work, altogether taking an average of 46 days (median of 29 days) to return, with the only notable differences between procedure types being in this latter statistic. Average at-work performance by 12 months improved by ~20%. Improvement was concentrated among patients who reported declining productivity leading up to surgery, who saw an average of ~40% improvement in at-work performance. Most improvement appeared to happen by 6 months after surgery. Changes in absenteeism by 12 months after surgery were much smaller, indicating no more than a day or two fewer absences per month.
Prior work-related research on patients undergoing lumbar spine surgery has focused on return to work. Our results in this area are similar. One study of over 4000 patients found 82% of patients had returned to work by 3 months after lumbar spine surgery [24], which is intermediate to (and consistent with) our findings that 76% returned to work by 6 weeks and 96% returned to work by 6 months. Another study focused on prediction found 75% of patients undergoing lumbar spine surgery returned to work by 1 month and 96% returned by 3 months, which is also similar to our findings [25].
Prior work about worker “productivity” after lumbar spine surgery is often about absenteeism but not presenteeism [31,32]. For example, one study [31] sought to evaluate the trajectory of productivity loss (defined as “the sum of days with sick insurance benefits multiplied with the proportion of the patient’s working time covered by a benefit”) in Swedish patients diagnosed with lumbar disc herniation or spinal stenosis before and after surgery. They found that their metric gradually increased during the year leading up to surgery, peaking at the first month after surgery (when patients were absent nearly full-time), and then gradually decreased. Although they measured two years before and after surgery, which we do not, their estimate of mean change in absences one year before to one year after surgery was approximately 2.0 days. Although our baseline measurement is a few months before surgery, not a year before surgery, this finding is consistent with our finding that changes in 28-day absences were on the order of days (i.e., not large in magnitude).
The closest study to ours, which used patients undergoing lumbar spine surgery from the same hospital (from an earlier time period), investigated preoperative expectations about at-work performance after surgery, as well as actual 2-year postoperative perceptions of at-work performance [34]. They found that preoperatively 74% expected surgery would yield improved ability to fulfill job responsibilities, and postoperatively 82% reported some improvement (42% reported less improvement than expected and 40% as much or more improvement than expected). We also found that the majority of patients have improved at-work performance: comparing patients who responded at baseline and 12 months, 62% had improved at-work performance, 23% had the same at-work performance, and 15% had worse at-work performance. Our study differs in that it did not measure preoperative expectations, but actual preoperative self-reported at-work performance; we also did not measure postoperative perceptions of changes in at-work performance, but actual postoperative self-reported at-work performance; we used both to measure changes in at-work performance.
It is interesting to compare these results to our prior study, which used identical questionnaires, but investigated patients before and after total joint arthroplasty (TJA) [23]. In that study, we only measured follow-ups at 6 months and 12 months (not at 6 weeks). Compared to TJA, patients undergoing lumbar spine surgery had lower average preoperative at-work performance by 5 to 10 points, but by 12 months, among those who returned to work, patients had reached a similar level of average at-work performance. Patients undergoing spine surgery therefore had greater average improvement, i.e., average improvement of ~20% versus ~10% among patients undergoing TJA. Average gains in both instances were concentrated among patients who had declining productivity leading up to surgery, who had lower baseline scores, although more spine patients reporting declining productivity leading up to surgery (53% versus 42%). Among all TJA patients, the percentage of patients with full productivity moved from 20.9% to 36.8% between baseline and 12 months, but among spine patients, it moved from 16.0% to 29.0%. Again, patients undergoing spine surgery had lower preoperative at-work performance according to this metric. But, despite larger average gains, fewer achieved full at-work performance 12 months later. Numbers for 7-day and 28-day absenteeism were also similarly small in magnitude and change.
Our study has several limitations. First, our patients were recruited from a single high-volume specialty musculoskeletal hospital located in a large urban setting, and had mostly professional, executive, and administrative jobs. We also enrolled a convenience sample of patients based on an initial single-email outreach, which had a relatively low response rate. It is therefore likely that enrolled patients are not representative of the full population of employed patients who undergo lumbar spinal surgery along several dimensions. We acknowledge that future work would benefit from conducting a similar analysis on a broader, potentially more representative sample of such patients. We also focused solely on single-level lumbar decompression and/or fusion; it is likely that outcomes would differ for patients undergoing spinal surgery on different parts of the spine or with greater complexity. Differences might also exist among patients undergoing surgery with different surgical techniques (e.g., open versus minimally invasive, posterolateral versus interbody fusion). Further research is warranted to investigate these distinct subpopulations. However, as we have noted, there is no other research directly quantifying return to work, absenteeism, and presenteeism before and after lumbar spine surgery. Also, our absenteeism and presenteeism metrics are derived from self-reported surveys, which are subject to misreporting and recall bias. However, there is no other practical way to measure this information; it would be unrealistic to gain access to this sort of information from patients’ employers. Moreover, for our value calculations, we could not leverage days patients worked extra, because working extra one day does not necessarily completely offset one day absent; we therefore only used 28-day absences from own health problems, family health problems, and other reasons including vacation. This likely leads to the cost of absenteeism being overestimated at each time point.
In conclusion, we are the first to measure employed patients’ presenteeism and absenteeism before and after single-level lumbar fusion and/or decompression. Presenteeism and absenteeism contributed roughly evenly in terms of preoperative average monthly value lost. By 12 months, the vast majority of patients were still employed and had returned to work. Although patients did not report much change in absenteeism at any time, nor did they report significantly increased average at-work performance at 6 weeks, they did report significantly increased average at-work performance at both 6 months and 12 months, concentrated among patients who reported declining at-work performance in the years leading up to surgery. Cost-benefit analyses of lumbar spine surgery should therefore consider improved presenteeism among employed patients, which, from a societal or employer perspective, appear to offset some of the direct and indirect costs of treatment.
Supplementary Material
Highlights.
We measured employed patients’ presenteeism and absenteeism before and after surgery
Presenteeism is illness-related reduced at-work productivity or performance
Average at-work performance moved 73.0 to 88.1 (of 100) between baseline and 1 year
Average changes in absenteeism were small between baseline and 1 year
Changes represent an average 13.0 percentage points of mitigated monthly time lost
Acknowledgments
Study data were collected and managed using REDCap electronic data capture tools hosted at Weill Cornell Medicine with support from Clinical and Translational Science Center grant, UL1TR002384.
Footnotes
Disclosures: There was no specific financial support for this study. All work was performed at Hospital for Special Surgery. MAF, WI, MAR, CKM, ECK, and CHM have no relevant disclosures. SAQ has relevant disclosures, which are enumerated in the attached ICMJE form.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Zhang W, Gignac MA, Beaton D, Tang K, Anis AH. Productivity loss due to presenteeism among patients with arthritis: Estimates from 4 instruments. J Rheumatol 2010;37:1805–14. 10.3899/jrheum.100123. [DOI] [PubMed] [Google Scholar]
- [2].Stewart WF, Ricci JA, Chee E, Morganstein D. Lost Productive Work Time Costs from Health Conditions in the United States: Results from the American Productivity Audit. J Occup Environ Med 2003;45:1234–46. 10.1097/01.jom.0000099999.27348.78. [DOI] [PubMed] [Google Scholar]
- [3].Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, Absence, Disability, and Presenteeism Cost Estimates of Certain Physical and Mental Health Conditions Affecting U.S. Employers. J Occup Environ Med 2004;46:398–412. 10.1097/01.jom.0000121151.40413.bd. [DOI] [PubMed] [Google Scholar]
- [4].Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the us workforce. JAMA 2003;290:2443–54. [DOI] [PubMed] [Google Scholar]
- [5].Pauly MV, Nicholson S, Polsky D, Berger ML, Sharda C. Valuing reductions in on-the-job illness: “Presenteeism” from managerial and economic perspectives. Health Econ 2008;17:469–85. 10.1002/hec.1266. [DOI] [PubMed] [Google Scholar]
- [6].Lamb CE, Ratner PH, Johnson CE, Ambegaonkar AJ, Joshi A V, Day D, et al. Economic impact of workplace productivity losses due to allergic rhinitis compared with select medical conditions in the United States from an employer perspective. Curr Med Res Opin 2006;22:1203–10. 10.1007/BF00345338. [DOI] [PubMed] [Google Scholar]
- [7].Canavan C, West J, Card T. Review article: The economic impact of the irritable bowel syndrome. Aliment Pharmacol Ther 2014;40:1023–34. 10.1111/apt.12938. [DOI] [PubMed] [Google Scholar]
- [8].Wada K, Arakida M, Watanabe R, Negishi M, Sato J, Tsutsumi A. The economic impact of loss of performance due to absenteeism and presenteeism caused by depressive symptoms and comorbid health conditions among Japanese workers. Ind Health 2013;51:482–9. 10.2486/indhealth.2013-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Dieleman JL, Cao J, Chapin A, Chen C, Li Z, Liu A, et al. US Health Care Spending by Payer and Health Condition, 1996-2016. JAMA - J Am Med Assoc 2020;323:863–84. 10.1001/jama.2020.0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Burden of Back Pain ∣ BMUS: The Burden of Musculoskeletal Diseases in the United States n.d. https://www.boneandjointburden.org/fourth-edition/iiac0/burden-back-pain (accessed June 3, 2021). [Google Scholar]
- [11].Gignac MAM, Cao X, Tang K, Beaton DE. Examination of arthritis-related work place activity limitations and intermittent disability over four-and-a-half years and its relationship to job modifications and outcomes. Arthritis Care Res 2011;63:953–62. 10.1002/acr.20456. [DOI] [PubMed] [Google Scholar]
- [12].Beaton DE, Tang K, Gignac MAM, Lacaille D, Badley EM, Anis AH, et al. Reliability, validity, and responsiveness of five at-work productivity measures in patients with rheumatoid arthritis or osteoarthritis. Arthritis Care Res 2010;62:28–37. 10.1002/acr.20011. [DOI] [PubMed] [Google Scholar]
- [13].Lerner D, Reed JI, Massarotti E, Wester LM, Burke TA, Knottnerus JA, et al. The Work Limitations Questionnaire’s validity and reliability among patients with osteoarthritis. J Clin Epidemiol 2002;55:197–208. 10.1016/S0895-4356(01)00424-3. [DOI] [PubMed] [Google Scholar]
- [14].Zhang W, Bansback N, Kopec J, Anis AH. Measuring time input loss among patients with rheumatoid arthritis: validity and reliability of the Valuation of Lost Productivity questionnaire. J Occup Environ Med 2011;53:530–6. 10.1097/JOM.0b013e318218abf1. [DOI] [PubMed] [Google Scholar]
- [15].Bansback N, Zhang W, Walsh D, Kiely P, Williams R, Guh D, et al. Factors associated with absenteeism, presenteeism and activity impairment in patients in the first years of RA. Rheumatology 2012;51:375–84. 10.1093/rheumatology/ker385. [DOI] [PubMed] [Google Scholar]
- [16].Agaliotis M, Mackey MG, Jan S, Fransen M. Burden of reduced work productivity among people with chronic knee pain: A systematic review. Occup Environ Med 2014;71:651–9. 10.1136/oemed-2013-101997. [DOI] [PubMed] [Google Scholar]
- [17].Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J 2008;8:8–20. 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- [18].Lerner D, Rogers WH, Chang H, Rodday AM, Greenhill A, Villagra VG, et al. The health care and productivity costs of back and neck pain in a multi-employer sample of utility industry employees. J Occup Environ Med 2015;57:32–43. 10.1097/JOM.0000000000000280. [DOI] [PubMed] [Google Scholar]
- [19].van Lunteren M, Ez-Zaitouni Z, Fongen C, Landewé R, Ramonda R, van der Heijde D, et al. Disease activity decrease is associated with improvement in work productivity over 1 year in early axial spondyloarthritis (SPondyloArthritis Caught Early cohort). Rheumatol (United Kingdom) 2017;56:2222–8. 10.1093/rheumatology/kex365. [DOI] [PubMed] [Google Scholar]
- [20].Marks M, Vliet Vlieland TPM, Audigé L, Herren DB, Nelissen RGHH, Van Den Hout WB. Healthcare costs and loss of productivity in patients with trapeziometacarpal osteoarthritis. J Hand Surg Eur Vol 2015;40:927–34. 10.1177/1753193414568293. [DOI] [PubMed] [Google Scholar]
- [21].Amick BC, Habeck RV, Ossmann J, Fossel AH, Keller R, Katz JN. Predictors of Successful Work Role Functioning after Carpal Tunnel Release Surgery. J Occup Environ Med 2004;46:490–500. 10.1097/01.jom.0000126029.07223.a0. [DOI] [PubMed] [Google Scholar]
- [22].Hylkema TH, Stevens M, Selzer F, Amick BA, Katz IN, Brouwer S. Activity Impairment and Work Productivity Loss After Total Knee Arthroplasty: A Prospective Study. J Arthroplasty 2019;34:2637–45. 10.1016/j.arth.2019.06.015. [DOI] [PubMed] [Google Scholar]
- [23].Fontana MA, Islam W, Richardson MA, Medina CK, McLawhorn AS, MacLean CH. Presenteeism and Absenteeism Before and After Total Hip and Knee Arthroplasty. J Arthroplasty 2020;36. 10.1016/j.arth.2020.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Asher AL, Devin CJ, Archer KR, Chotai S, Parker SL, Bydon M, et al. An analysis from the Quality Outcomes Database, Part 2. Predictive model for return to work after elective surgery for lumbar degenerative disease. J Neurosurg Spine SPI 2017;27:370–81. 10.3171/2016.8.SPINE16527. [DOI] [PubMed] [Google Scholar]
- [25].McGirt MJ, Sivaganesan A, Asher AL, Devin CJ. Prediction model for outcome after lowback surgery: individualized likelihood of complication, hospital readmission, return to work, and 12-month improvement in functional disability. Neurosurg Focus 2015;39:E13–E13. [DOI] [PubMed] [Google Scholar]
- [26].Parker SL, Lerner J, McGirt MJ. Effect of minimally invasive technique on return to work and narcotic use following transforaminal lumbar inter-body fusion: a review. Prof Case Manag 2012;17:229–35. [DOI] [PubMed] [Google Scholar]
- [27].Lee YP, Farhan SD, Kiester D, Rosen C, Pendi A, Bhatia N. Variables affecting return to work after spinal surgery in a nonworkers’ compensation population: A retrospective cohort study. J Am Acad Orthop Surg 2017;25:e282–8. 10.5435/JAAOS-D-17-00098. [DOI] [PubMed] [Google Scholar]
- [28].Adogwa O, Parker SL, Bydon A, Cheng J, McGirt MJ. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J Spinal Disord Tech 2011;24:479–84. 10.1097/BSD.0b013e3182055cac. [DOI] [PubMed] [Google Scholar]
- [29].Anderson JT, Haas AR, Percy R, Woods ST, Ahn UM, Ahn NU. Clinical depression is a strong predictor of poor lumbar fusion outcomes among workers’ compensation subjects. Spine (Phila Pa 1976) 2015;40:748–56. 10.1097/BRS.0000000000000863. [DOI] [PubMed] [Google Scholar]
- [30].Liow MHL, Goh GSH, Yeo W, Ling ZM, Yue WM, Guo CM, et al. Time Taken to Return to Work Does Not Influence Outcomes of Minimally Invasive Transforaminal Lumbar Interbody Fusion: A 5-Year Follow-Up Study. Spine (Phila Pa 1976) 2019;44:503–9. 10.1097/BRS.0000000000002863. [DOI] [PubMed] [Google Scholar]
- [31].Jonsson E, Olafsson G, Fritzell P, Hägg O, Borgström F. Productivity Loss In Patients Diagnosed With Spinal Stenosis And Lumbar Disc Herniation. Value Heal 2016;19:A347–766. 10.1016/j.jval.2016.09.1128. [DOI] [Google Scholar]
- [32].Koenig L, Dall TM, Gu Q, Saavoss J, Schafer MF. How does accounting for worker productivity affect the measured cost-effectiveness of lumbar discectomy? Clin Orthop Relat Res 2014;472:1069–79. 10.1007/s11999-013-3440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Spine Procedures ∣ BMUS: The Burden of Musculoskeletal Diseases in the United States n.d. https://www.boneandjointburden.org/fourth-edition/iiad0/spine-procedures (accessed June 3, 2021). [Google Scholar]
- [34].Mancuso CA, Duculan R, Cammisa FP, Sama AA, Hughes AP, Girardi FP. Positive and negative work events attributed to the spine 2 years after lumbar surgery among patients working preoperatively. J Neurosurg Spine 2019;30:736–42. 10.3171/2018.12.SPINE18840. [DOI] [PubMed] [Google Scholar]
- [35].Glassman SD, Polly DW, Dimar JR, Carreon LY. The cost effectiveness of single-level instrumented posterolateral lumbar fusion at 5 years after surgery. Spine (Phila Pa 1976) 2012;37:769–74. 10.1097/BRS.0b013e3181e03099. [DOI] [PubMed] [Google Scholar]
- [36].Devin CJ, Chotai S, Parker SL, Tetreault L, Fehlings MG, McGirt MJ. A cost-utility analysis of lumbar decompression with and without fusion for degenerative spine disease in the elderly. Neurosurgery 2015;77:S116–24. 10.1227/NEU.0000000000000949. [DOI] [PubMed] [Google Scholar]
- [37].Kim LH, Vail D, Azad TD, Bentley JP, Zhang Y, Ho AL, et al. Expenditures and health care utilization among adults with newly diagnosed lowback and lower extremity pain. JAMA Netw Open 2019;2:193676. 10.1001/jamanetworkopen.2019.3676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann Intern Med 2007;147:573–7. 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- [39].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019;95:31078660. 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Kessler RC, Ames M, Hymel PA, Loeppke R, McKenas DK, Richling DE, et al. Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to evaluate the indirect workplace costs of illness. J Occup Environ Med 2004;46:23–37. 10.1097/01.jom.0000126683.75201.c5. [DOI] [PubMed] [Google Scholar]
- [42].Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, et al. The World Health Organization Health and Work Performance Questionnaire (HPQ). J Occup Env Med 2003;45:156–74. 10.1097/01.jom.0000052967.43131.51. [DOI] [PubMed] [Google Scholar]
- [43].Kessler R, Petukhova M, McInnes K, Üstün TB. Re: Content and scoring rules for the WHO HPQ absenteeism and presenteeism questions 2007:1–8. https://www.hcp.med.harvard.edu/hpq/ftpdir/absenteeismpresenteeismscoring050107.pdf. [Google Scholar]
- [44].Ospina MB, Dennett L, Waye A, Jacobs P, Thompson AH. A systematic review of measurement properties of instruments assessing presenteeism. Am J Manag Care 2015;21:e171–85. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.