Abstract
Introduction:
Federally Qualified Health Centers (FQHCs) serve 29.8 million low-income patients across the U.S., many of whom have unaddressed social risks. In 2019, for the first time, data on social risk screening capabilities were collected from every U.S. FQHC. The objectives of this study were to describe national rates of social risk screening capabilities across FQHCs, identify organizational predictors of screening, and assess between-state heterogeneity.
Methods:
Using a 100% sample of U.S. FQHCs (N=1,384, representing 29.8 million patients) from the 2019 Uniform Data System, the primary outcome was whether an FQHC collected data on patients’ social risk factors (yes/no). Summary statistics on rates of social risk screening capabilities were generated in aggregate and by state. Linear probability models were then used to estimate the relationship between probability of social risk screening and 7 key FQHC characteristics (e.g., FQHC size, Medicaid MCO contract, Medicaid accountable care organization presence). Data were analyzed in 2020–2021.
Results:
Most (71%) FQHCs collected social risk data, with between-state variation. The most common screener was the Protocol for Responding to and Assessing Patients’ Assets Risks and Experiences (43% of FQHCs that screened), whereas 22% collected social risk data using a non-standardized screener. After adjusting for other characteristics, FQHCs with social risk screening capabilities served more total patients, were more likely to be located in a state with a Medicaid accountable care organization, and were less likely to have an MCO contract.
Conclusions:
There has been widespread adoption of social risk screening tools across U.S. FQHCs, but between-state disparities exist. Targeting social risk screening resources to smaller FQHCs may increase adoption of screening tools.
INTRODUCTION
There is growing recognition that social risks such as housing instability or food insecurity are associated with delays in necessary care, lower-quality care, and worse health outcomes, especially among low-income patients.1–3 Federally Qualified Health Centers (FQHCs) provide primary care services to 29.8 million low-income patients across the U.S., who disproportionately experience social risks.4–6 FQHCs are uniquely positioned to help mimimize the social risks of patients by addressing social needs through federally required enabling services7 and community partnerships, and many FQHCs provide on-site assistance with care coordination, applying for government programs, transportation, and food needs.5,8–10 A likely important first step to addressing patients’ social risks in clinical settings is to adopt tools that systematically screen for social risk factors,11 for which there has been growing adoption by providers and support from professional organizations, including the National Academies.12–14 Some evidence suggests that, compared with other physician practices, FQHCs are more likely to screen for social risk factors13,15,16; however, these studies rely on samples of practices and there are no known national data on the extent to which FQHCs collect data on individual social risks.
There is also limited evidence on FQHC-level and between-state variation in social risk screening tool adoption. Several studies have examined strategies for initiating and integrating social risk screening tools in electronic health records (EHRs)17–21 and a few single-state or multistate studies have characterized screening rates within FQHCs.22–24 However, few studies have quantified organizational characteristics that might facilitate screening capabilities in FQHCs, where FQHCs with more resources—such as larger, more urban FQHCs, FQHCs with fewer uninsured patients including those in states with expanded Medicaid eligibility, or FQHCs with more grant revenue—may be better equipped to adopt screening protocols. There are also many different social risk screener tools (e.g., Protocol for Responding to and Assessing Patients’ Assets Risks and Experiences [PRAPARE]25) available; however, no studies have assessed which screeners are most commonly used nationwide, which may be important when considering if and how to better standardize social risk data across organizations. Further, state policies and delivery systems can influence adoption of social risk screening tools. In many states, Medicaid agencies require that accountable care organizations (ACOs) and MCOs screen for social risk factors,18 which could help facilitate adoption of social risk screening tools at the provider level. Despite the continued importance in state-led efforts to assess and address social risks, no known studies have examined between-state variation in adoption of social risk screening tools.
In 2019, for the first time, national data on social risk screening capabilities were collected from every FQHC in the U.S. The objectives of this study were to describe rates of social risk screening capabilities across FQHCs, assess heterogeneity across states, and identify organizational predictors of whether FQHCs screen for social risk.
METHODS
Study Sample
The primary data source was the Health Resources and Services Administration 2019 Uniform Data System (UDS),26 which includes a 100% sample of FQHCs (N=1,384) in the U.S., representing 29.8 million low-income patients across all 50 U.S. states, the District of Columbia, and 8 U.S. territories. UDS data are reported annually by all FQHCs that received grants under Section 330 of the Public Health Service Act. The data included detailed FQHC-level information on patient sociodemographic characteristics, quality of care and service utilization data, and FQHC organizational features.
Measures
The primary outcome was whether an FQHC screened for social risk (yes/no) in 2019, based on the UDS question: Does your health center collect data on individual patients’ social risk factors…? Among those that responded yes, type of standardized screener used was further assessed. FQHCs could select multiple screeners, and options included Accountable Health Communities Screening Tools; Upstream Risks Screening Tool and Guide; iHELP; Recommend Social and Behavioral Domains for EHRs; PRAPARE; Well Child Care, Evaluation, Community Resources, Advocacy Referral, Education (WE CARE); WellRx; Other, including a modified version of one of the above; or we do not use a standardized screener.26 Appendix Table 1 provides the domains and constructs measured by each tool.
Statistical Analysis
The unit of analysis was the FQHC. First, summary statistics on rates of social risk screening capabilities were generated. Among those responding yes, types of standardized screeners used, if any, were further examined. Second, characteristics of FQHCs with versus without social risk screening capabilities were compared using Wilcoxon–Mann–Whitney tests. FQHC-level patient composition was examined, where characteristics included age, race/ethnicity, poverty level, health insurance coverage type, an indicator for experiencing homelessness, English proficiency, sexual orientation, and Veteran status. FQHC-level patient volume, total revenue per patient, urban service area, and other organizational characteristics (e.g., Medicaid managed care contract, EHR use) were also compared. State-level characteristics included Medicaid expansion status (Appendix Table 2) and having an active statewide Medicaid ACO model (Appendix Table 3) as of 2019. Third, rates of social risk screening capabilties were described by state, which measured the percentage of all FQHCs in each state, district, or territory that responded yes to screening patients for social risks.
To estimate the relationship between the probability of screening for social risks and key FQHC characteristics, a linear probability model was used that adjusted for the following covariates, for which there was a statistically significant difference between groups prior to adjustment or for which prior literature suggested a relationship with screening likelihood27: percentage of FQHC’s patients who were uninsured (measured in quartiles); whether an FQHC served an urban versus rural patient population; FQHC size, based on number of unique patients served (measured in quartiles); total revenue per patient served; whether an FQHC was located in a Medicaid expansion state; whether an FQHC was located in a state actively implementing a statewide Medicaid ACO model; and whether the FQHC participated in a Medicaid managed care contract. Models used robust Huber–White sandwich variance estimators and clustered errors at the state level. In subanalyses, main analyses were rerun, but excluded FQHCs located in U.S. territories.
All results and probabilities were reported on a scale of 0–100, and differences were measured in percentage point terms. All p-values were 2-tailed and statistical significance was set at α=0.05. Analyses were performed using Stata, version 17.0 in 2020–2021.
The IRB at Boston University deemed this study exempt.
RESULTS
Seventy-one percent of FQHCs reported social risk factor screening capabilities in 2019 (Figure 1). Among those that screened for social risk, the most common type of screener was the PRAPARE (43%); 11% of FQHCs used Recommended Social and Behavioral Domains for EHRs; 8% used Accountable Health Communities Screening Tools; 7% used WE CARE; 2% used either Upstream, WellRx, or iHELP; and 25% used another screener that was not included in the list of survey options, which was inclusive of modified versions of screening tools. Of note, 22% of FQHCs that screened for social risks did not use any standardized screener.
Figure 1.
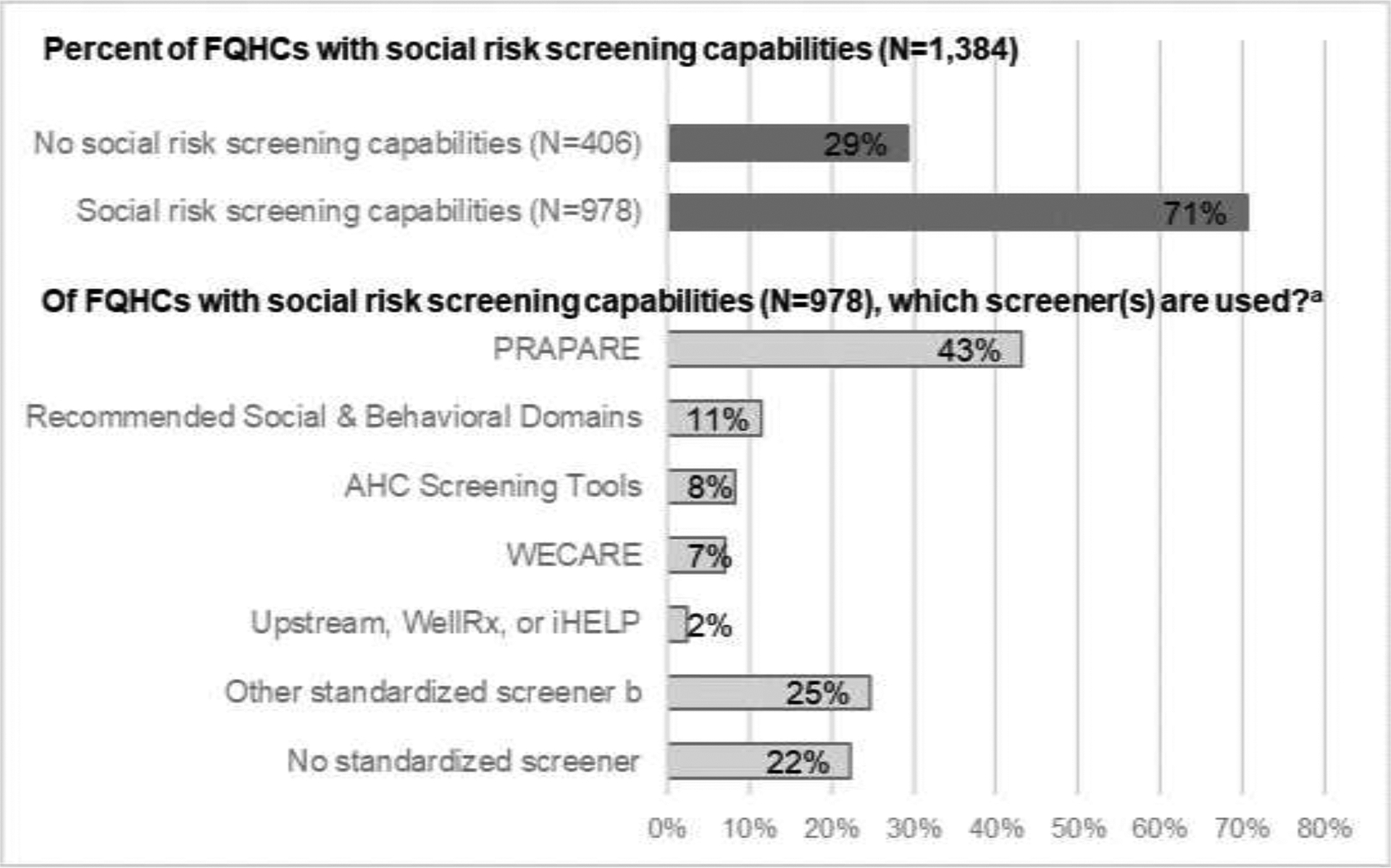
Rates of social risk screening capabilities across all U.S. FQHCs (2019).
aFQHCs may report using more than one screener and therefore, distributions of “which screener(s) used” do not add up to 100%.
b”Other standardized screener” is inclusive of modified versions of the other listed screeners.
c “Capabilities” indicates any social risk data collection (yes/no) and not the extent of data collection.
FQHC, Federally Qualified Health Center; PRAPARE, Protocol for Responding to and Assessing Patients’ Assets Risks and Experiences; AHC, Accountable Health Communities; WECARE, Well Child Care, Evaluation, Community Resources, Advocacy, Referral, Education; iHELP, Income, Housing, Education, Legal Status, Literacy, Personal Safety.
Characteristics of FQHCs that did versus did not have social risk screening capabilities were statistically similar, with some exceptions (Table 1). FQHCs that did not screen patients had a greater proportion of patients who were uninsured (27% vs 24%) and were less likely to serve an urban area (56% vs 63%) relative to those that screened. FQHCs that did not screen also served fewer unique patients per year on average (17,200 vs 23,368), had more total revenue per patient, and were much less likely to be located in a Medicaid expansion state (64% vs 72%) or in a state with an active Medicaid ACO (11% vs 24%).
Table 1.
Characteristics of FQHCs With Versus Without Social Risk Screening Capabilities (2019)
| Characteristics | Screen for social risk N=978 FQHCs, serving 22.9 million patients | Do not screen for social risk N=406 FQHCs, serving 7.0 million patients | Difference |
|---|---|---|---|
| Age, years, % | |||
| 0‒17 | 26.5 | 26.7 | |
| 18‒64 | 62.7 | 62.2 | |
| ≥65 | 10.8 | 11.2 | |
| Female, % | 56.2 | 56.7 | |
| Race/ethnicity, % | |||
| White, non-Hispanic | 41.5 | 39.8 | |
| Black, non-Hispanic | 18.4 | 18.5 | |
| Hispanic | 28.3 | 28.8 | |
| Asian, non-Hispanic | 3.4 | 2.8 | |
| American Indian/Alaskan Native, non-Hispanic | 1.7 | 2.9 | * |
| Other race, non-Hispanic | 5.8 | 7.5 | * |
| Poverty level, % | |||
| Below 100% FPL | 64.0 | 65.1 | |
| Above 200% FPL | 10.7 | 10.5 | |
| Insurance coverage, % | |||
| Medicaid | 43.4 | 41.1 | |
| Medicare | 11.2 | 10.9 | |
| Other public | 0.7 | 0.7 | |
| Private | 20.8 | 20.1 | |
| Uninsured | 23.9 | 27.2 | ** |
| Other patient characteristics, % | |||
| Experiencing homelessness | 7.7 | 5.7 | |
| English is not primary language | 19.8 | 19.7 | |
| Sexual minority | 4.9 | 4.1 | |
| Veteran | 1.8 | 1.6 | |
| FQHC-level characteristics | |||
| Urban service area, % | 63.2 | 56.2 | ** |
| Number of unique patients, n | 23,368 | 17,200 | *** |
| Total revenue/patient, $ | $458 | $552 | * |
| EHR use, % | 99.7 | 99.3 | |
| Medicaid managed care contract, % | 23.1 | 25.4 | |
| State-level characteristics (excluding territories), %a | |||
| Medicaid expansion state of 2019 | 72.1 | 63.5 | *** |
| Active state Medicaid ACO | 23.7 | 11.1 | *** |
Notes:
p<0.05;
p<0.01;
p<0.001.
Excludes FQHCs located in the 8 US territories; when including territories, 71.0% vs 60.8% were located in a Medicaid expansion state and 23.3% vs 10.6% were in a Medicaid ACO state (p<0.001).
FPL, federal poverty level; EHR, electronic health record; ACO, accountable care organization; FQHC, Federally Qualified Health Center.
There was variation in use of social risk screening tool adoption between states (Figure 2). States with highest rates of screening adoption included Colorado (95% of FQHCs), Connecticut (100%), the District of Columbia (88%), Delaware (100%), Massachusetts (92%), Missouri (100%), North Dakota (100%), New Hampshire (90%), Rhode Island (100%), and Vermont (100%). States with the lowest rates of screening implementation included Alaska (56% of FQHCs), Florida (55%), Louisiana (56%), Maryland (41%), New Jersey (58%), Nevada (50%), South Dakota (20%), Wisconsin (56%), West Virginia (54%), and Wyoming (33%).
Figure 2.
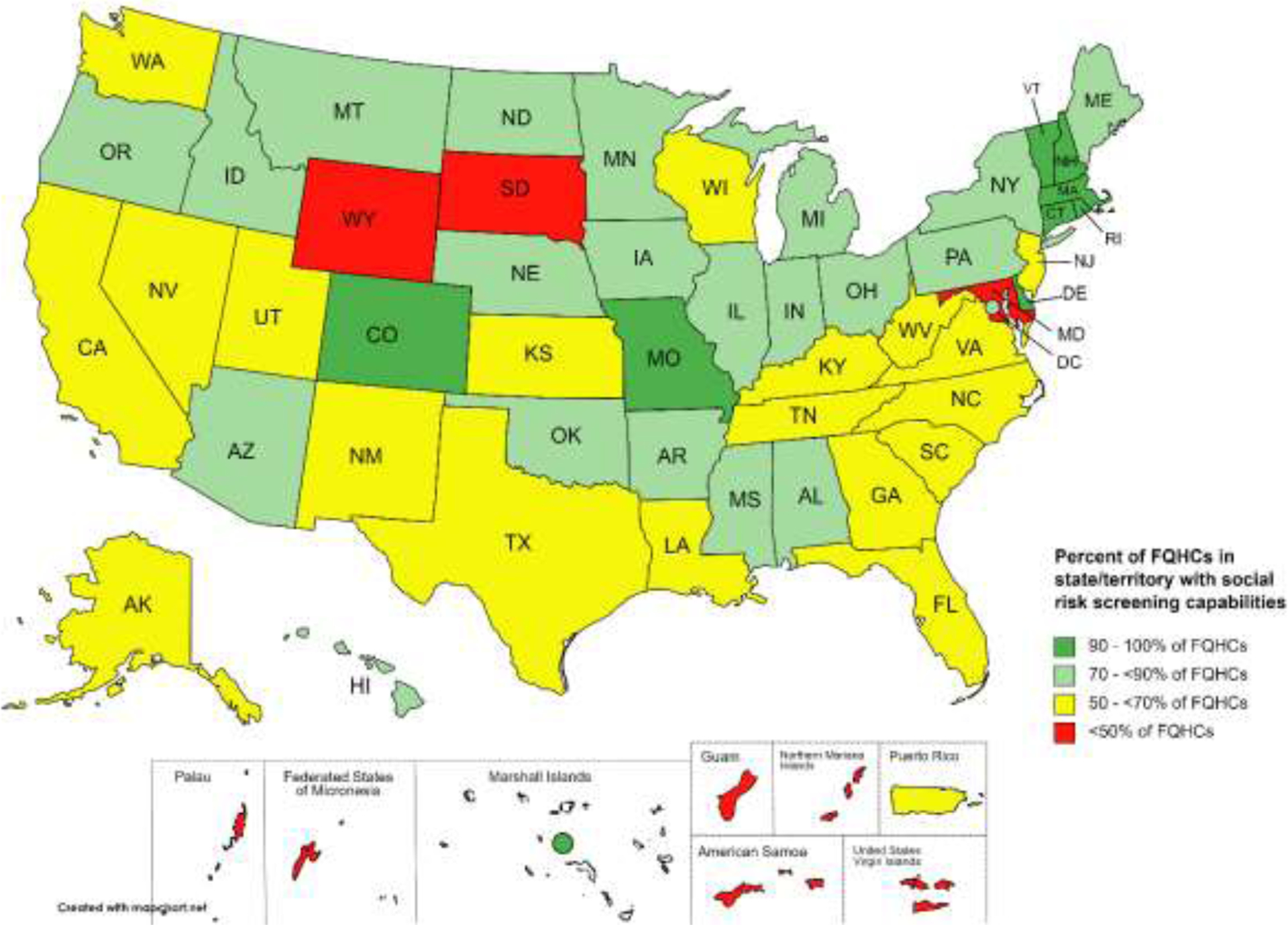
Percent of FQHCs with social risk capabilities by state, unadjusted (2019).
Notes: States with fewer than 5 FQHCs have wider CIs around screening adoption rates. This includes the states of Delaware, North Dakota, and South Dakota, plus all territories except for Puerto Rico. However, because the data include the universe of FQHCs in the U.S., rather than a sample, data are reported for each state regardless of number of FQHCs.
FQHC, Federally Qualified Health Center.
Finally, when examining the adjusted association between key FQHC characteristics and probability of social risk screening capabilities (Table 2), 3 characteristics were statistically associated with probability of social risk screening. FQHC size was a significant predictor of screening, where the smallest FQHCs were 14.3 percentage points (95% CI=7.6, 21.0) less likely to screen for social risks, relative to the largest FQHCs. In addition, being located in a state with an active Medicaid ACO was associated with a 15.2 percentage point (95% CI=9.1, 21.4) increase in the probability of social risk screening. Finally, FQHCs that participated in a Medicaid managed care contract were 9.5 percentage points (95% CI=4.8, 14.2) less likely to screen for social risks, relative to FQHCs without Medicaid managed care, after adjusting for the other characteristics.
Table 2.
Adjusted Association Between Key FQHC Characteristics and Probability of Having Social Risk Screening Capabilitiesa
| Variable | Difference in probability of social risk screening capabilitiesb (95% CI) | p-value |
|---|---|---|
| Percent patients who are uninsured | ||
| q1: 0‒<11.5% | ref | ref |
| q2: 11.5‒<20.6% | 7.27 (‒0.54, 15.08) | 0.068 |
| q3: 20.6‒<32.8% | 4.38 (‒3.00, 11.78) | 0.24 |
| q4: ≥32.8% | 5.14 (‒1.98, 12.27) | 0.154 |
| Urban service area (ref=rural) | 4.03 (‒2.48, 10.54) | 0.22 |
| FQHC size | ||
| q1: >25,892 unique patients | ref | ref |
| q2: 13,146 to 25,862 pts | ‒3.20 (‒10.57, 4.16) | 0.387 |
| q3: 6,530 to 13,146 pts | ‒9.15 (‒2.98, ‒15.31) | 0.004 |
| q4: <6,530 pts | ‒14.29 (‒7.58, ‒21.00) | <0.001 |
| Total revenue ($)/1,000 patients served | ‒1.92 (‒4.62, 7.80) | 0.16 |
| FQHC has Medicaid managed care contract | ‒9.50 (‒4.80, ‒14.20) | <0.001 |
| Medicaid expansion state as of 2019 | 5.50 (‒1.88, 12.89) | 0.141 |
| Active Medicaid ACO in state | 15.22 (9.07, 21.37) | <0.001 |
N=1,384 federally qualified health centers (FQHCs), representing 29.8 million FQHC patients across all 50 U.S. states, the District of Columbia, and 8 U.S. territories, based on data from the 2019 Uniform Data System (UDS).
All coefficients are based on results from a linear probability regression model that adjusts for percent of patients who are uninsured, FQHC size (number of patients), urban vs rural service area, total revenue per 1,000 unique patients served, location in a Medicaid expansion state, location in a state with an active Medicaid accountable care organization (ACO), and participation in at least 1 Medicaid managed care contract, with robust SEs clustered at the state-level. Boldface indicates statistical significance (p<0.05).
When excluding U.S. territories from the main analyses, results were similar (Appendix Table 4).
DISCUSSION
Using the first known national data on social risk screening at FQHCs, this study found that most (71%) FQHCs across the U.S. collected data on patient social risk factors, although there was between-state variation in FQHC adoption. Among FQHCs with social risk screening capabilities, the most commonly used screener was the PRAPARE tool, whereas about one quarter collected social risk data but did not use any standardized screener. After adjusting for other characteristics, FQHCs that did not screen patients for social risks served fewer total patients, were less likely to be located in a state with an active Medicaid ACO model, and were more likely to have an MCO contract.
To the authors’ knowledge, no studies have quantified the prevalence of social risk screening capabilities using a national census of facilities; rather, most have relied on samples and have focused on a specific set of social risk factors. A study using 2017–2018 data from a nationally representative sample of providers estimated that 16% of physician practices, 24% of hospitals, and 30% of FQHCs screened for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence,13 and a recent 2021 study found that, across these same domains, FQHCs were consistently more likely to screen than non–FQHC safety net primary care practices or non–safety net primary care practices.16 In a recent study, 39% of a regional sample of emergency departments reported screening for housing instability, food insecurity, transportation needs, or trouble paying utilities.28 This study builds upon these estimates in important ways. It uses a census of all FQHCs to present national and between-state variation. Compared with previous regional or nationally representative estimates, it finds that a higher proportion of FQHCs nationwide use a social risk screener. It also adds new national data on type of screeners implemented by FQHCs.
Despite high rates of social screening capabilities across FQHCs, a fairly large proportion (29%) of FQHCs did not collect any social risk data as of 2019. Findings indicate that smaller FQHCs may be less resourced to implement social risk screening tools. Prior work has indicated that lack of financial resources is a barrier to social risk screening or, more broadly, care delivery innovation.13 Integrating social risk screening tools into EHRs and workflow processes can be costly, time intensive, and require additional staffing.17,29–31 Even if FQHCs are motivated to screen for and address unmet social needs, smaller FQHCs may be under-resourced to invest in the necessary infrastructural changes. Federal grant dollars and technical assistance that target adoption and implementation of social risk screening tools may help overcome barriers in resources and technical expertise, which may be particularly beneficial to smaller sites.
Study results also suggest there is wide between-state variation in adoption of social risk screening, including more widespread adoption in the Northeast and less adoption in the South. This is likely driven in part by state-level policies, including but not limited to policies directly explored in this paper, and other political influences and budgetary priorities.32 In lower-adopter states, there may be missed opportunity for linking patients with social services given that all FQHCs are federally required to provide enabling services, such as eligibility assistance for the “provision of medical, social, housing, educational, or other related services.”7 This in turn may exacerbate between-state inequities in access to social services and associated health outcomes, although there still remain significant differences in between-state availability of social services.32 More so, in January 2021, the Centers for Medicare and Medicaid Services issued guidance indicating that FQHCs could be reimbursed with Medicaid dollars to screen patients for social needs, collect and analyze social needs data to develop interventions, or co-locate social services,33 suggesting that implementation of social risk screening may be driven by state-led Medicaid payment and delivery efforts. Participation in innovative Medicaid delivery models such as Medicaid ACOs that include quality metrics associated with social risk screening and aim to integrate social services with physical and behavioral services may also increase adoption.34 Recent evidence suggests that Medicaid ACO participation is associated with a higher likelihood of social risk screening and screening for more social risks,13,15 as supported by the study results.
Results suggest that, after accounting for Medicaid ACO status and select other organizational characteristics, FQHCs with Medicaid MCO contracts—health insurance plans that provide comprehensive benefits to Medicaid beneficiaries—were somewhat less likely to have social risk screening capabilities. Though this may be due, in part, to collinearity with other organizational characteristics, this suggests that there are untapped opportunities to leverage MCOs to promote social risk screening. States can direct MCOs to implement alternative payment models that incentivize providers to screen for social risk factors, or they can require MCOs to collect these data from participating providers. They can also require use of a standardized screening tool. As of 2019, among 40 states with MCOs, 25 reported having an MCO contract requirement to screen enrollees for social risk factors and 28 required that enrollees are referred to social services.27 Modifying managed care contracts to incentivize social risk screening and linkages to social services could further accelerate adoption,35 and this may be particularly important in states without other adoption mechanisms such as Medicaid ACOs.
About 1 in 4 FQHCs that screened for social risks did not use a standardized tool or a modified standardized tool, which could limit the ability of FQHCs to aggregate and share data with other practices or providers.36,37 Non-standardized screeners may also impact the number and types of risks that are assessed and in turn addressed. Further research is needed to understand the content of non-standardized tools used by U.S. FQHCs and if and how lack of having a standardized or modified standardized tool may affect the ability of FQHCs to understand and address important social risk factors.
Finally, although this study focuses on social risk screening as a structural measure, it is important to note that screening capability does not equate to adequately screening all patients (a process measure) nor addressing the unmet social needs of patients. Though adopting a social risk screening tool may be an important first step to identifying and addressing social risks of patients, there is likely significant heterogeneity in when, where, and how often FQHCs screen patients, where the reported extent of social risk screening may also depend on the survey language used when FQHCs are asked about screening implementation.38 It is critical that further research is conducted to better quantify the extent to which patients are screened for social risks within U.S. FQHCs. Furthermore, beyond screening, addressing unmet social needs among patients who want assistance requires developing relationships with community partners, maintaining updated resource lists, and creating appropriate workflows and referral processes,20 frequently including some degree of data sharing, all of which are resource-intensive activities. However, there is limited evidence to date on how providers can effectively address social needs,39–41 and even organizations that are committed to addressing the social needs of patients continue to face considerable challenges.37 For instance, FQHC survey data from 2014 found that only 8% of patients reported receiving FQHC assistance to address basic needs such as food, housing, or employment, despite large proportions of patients reporting social risk factors.5 For FQHCs that do not screen for social risks, this could in part be due to provider disinterest in screening if they do not otherwise have resources, partnerships, or appropriate workflows in place to actually address the needs of patients. Thus, efforts to incentivize screening must be coupled with investment in social services, community organizations, and organizational resources that empower providers to address patients’ social risk factors. This is particularly critical now, during the coronavirus disease 2019 (COVID-19) pandemic, when underlying social risks of low-income patients have risen to historic levels.42–44
Limitations
This study has limitations. First, although it examined the relationship between select FQHC characteristics and the probability of using social risk screening tools, these estimates should be interpreted as associations only. For instance, states that are already more invested in addressing the social needs of patients may be more likely to implement a Medicaid ACO; causality or directionality cannot be inferred from any of the results. Second, though this study captures whether FQHCs have adopted a social risk screening tool (a structural measure), it does not capture the percentage of the FQHC population that has been screened (a process measure), where the latter may be a more useful measure of impact. Although valid data on percentage of patients screened across all U.S. FQHCs are currently unavailable, in the future, standardized EHR documentation that allows for valid national reporting of patient screening rates and positivity rates by domain would enable research in this area. Third, screening for social risk does not imply that patients’ social needs are being addressed, which the authors were also unable to measure in this study. Finally, this study was limited by the organizational characteristics reported in UDS, and it possible that other characteristics (e.g., number of full-time equivalents, FQHC-related capabilities, management or leadership) could drive adoption of social risk screening.17
CONCLUSIONS
There has been widespread adoption of social risk screening tools across U.S. FQHCs. However, vast between-state disparities exist, where FQHCs in states with Medicaid ACOs are significantly more likely to have social risk screening capabilities. In low-adopter states, there may be missed opportunities for linking low-income FQHC patients with social services and supports. Targeting social risk screening resources and support to smaller, less resourced FQHCs may be one way to increase social risk screening at the remaining FQHCs. Finally, there remain untapped opportunities to leverage Medicaid MCOs to promote social risk screening.
Supplementary Material
ACKNOWLEDGMENTS
The research presented in this paper is that of the authors and does not reflect the official policy of NIH.
This study was supported by the National Center for Advancing Translational Sciences, NIH, through BU-CTSI Grant Number KL2TR001411 (Dr. Cole). The study sponsor had no role in any part of this work. Dr. Nguyen completed this work while supported by the Robert Wood Johnson Foundation Health Policy Research Scholars program. Dr. Byhoff completed this work while supported by the NIH National Institute on Minority Health and Health Disparities K23 Grant Number MD015267. Dr. Murray completed this work while supported by the Agency for Healthcare Research and Quality Grant Number T32HS022242.
No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CRediT author statement
MB Cole: conceptualization; methodology; software; validation; formal analysis; resources; data curation; writing – original draft; writing - review & editing; visualization; supervision; project administration; funding acquisition. KH Nguyen: conceptualization; writing - original draft; writing - review & editing. E Byhoff: writing - review & editing. G Murray: conceptualization; writing - review & editing
REFERENCES
- 1.Cole MB, Nguyen KH. Unmet social needs among low-income adults in the United States: associations with health care access and quality. Health Serv Res. 2020;55(suppl 2):873–882. 10.1111/1475-6773.13555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006;21(1):71–77. 10.1111/j.1525-1497.2005.00278.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berkowitz SA, Hulberg AC, Hong C, et al. Addressing basic resource needs to improve primary care quality: a community collaboration programme. BMJ Qual Saf. 2016;25(3):164–172. 10.1136/bmjqs-2015-004521. [DOI] [PubMed] [Google Scholar]
- 4.Health Center Program: Impact and Growth. Bureau of Primary Health Care. https://bphc.hrsa.gov/about/healthcenterprogram/index.html. Published August 20, 2018. Accessed September 24, 2020.
- 5.De Marchis E, Pantell M, Fichtenberg C, Gottlieb LM. Prevalence of patient-reported social risk factors and receipt of assistance in federally funded health centers. J Gen Intern Med. 2020;35(1):360–364. 10.1007/s11606-019-05393-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baggett TP, Berkowitz SA, Fung V, Gaeta JM. Prevalence of housing problems among community health center patients. JAMA. 2018;319(7):717–719. 10.1001/jama.2017.19869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.[USC05] 42 USC 254b: Health centers. http://uscode.house.gov/view.xhtml?req=granuleid:USC-prelim-title42-section254b&num=0&edition=prelim. Accessed July 21, 2021.
- 8.Yue D, Pourat N, Chen X, et al. Enabling services improve access to care, preventive services, and satisfaction among health center patients. Health Aff (Millwood). 2019;38(9):1468–1474. 10.1377/hlthaff.2018.05228. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen KH, Trivedi AN, Cole MB. Receipt of social needs assistance and health center patient experience of care. Am J Prev Med. 2021;60(3):e139–e147. 10.1016/j.amepre.2020.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kranz AM, Mahmud A, Agniel D, Damberg C, Timbie JW. Provision of social services and health care quality in US community health centers, 2017. Am J Public Health. 2020;110(4):567–573. 10.2105/ajph.2019.305519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gottlieb L, Sandel M, Adler NE. Collecting and applying data on social determinants of health in health care settings. JAMA Intern Med. 2013;173(11):1017–1020. 10.1001/jamainternmed.2013.560. [DOI] [PubMed] [Google Scholar]
- 12.Andermann A Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Rev. 2018;39:19. 10.1186/s40985-018-0094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by us physician practices and hospitals. JAMA Netw Open. 2019;2(9):e1911514. 10.1001/jamanetworkopen.2019.11514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Academies of Sciences - Engineering - Medicine. Integrating Social Needs Care into the Delivery of Health Care to Improve the Nation’s Health. https://www.nationalacademies.org/our-work/integrating-social-needs-care-into-the-delivery-of-health-care-to-improve-the-nations-health. Published 2019. Accessed July 29, 2021. [PubMed]
- 15.Brewster AL, Fraze TK, Gottlieb LM, Frehn J, Murray GF, Lewis VA. The role of value-based payment in promoting innovation to address social risks: a cross-sectional study of social risk screening by US physicians. Milbank Q. 2020;98(4):1114–1133. 10.1111/1468-0009.12480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewis VA, Spivack S, Murray GF, Rodriguez HP. FQHC designation and safety net patient revenue associated with primary care practice capabilities for access and quality. J Gen Intern Med. 2021;36(10):2922–2928. 10.1007/s11606-021-06746-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gold R, Bunce A, Cowburn S, et al. Adoption of social determinants of health EHR tools by community health centers. Ann Fam Med. 2018;16(5):399–407. 10.1370/afm.2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.LaForge K, Gold R, Cottrell E, et al. How 6 organizations developed tools and processes for social determinants of health screening in primary care: an overview. J Ambulatory Care Manage. 2018;41(1):2–14. 10.1097/jac.0000000000000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gottlieb LM, Tirozzi KJ, Manchanda R, Burns AR, Sandel MT. Moving electronic medical records upstream: incorporating social determinants of health. Am J Prev Med. 2015;48(2):215–218. 10.1016/j.amepre.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 20.Cantor MN, Thorpe L. Integrating data on social determinants of health into electronic health records. Health Aff (Millwood). 2018;37(4):585–590. 10.1377/hlthaff.2017.1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gruß I, Bunce A, Davis J, Dambrun K, Cottrell E, Gold R. Initiating and implementing social determinants of health data collection in community health centers. Popul Health Manag. 2021;24(1):52–58. 10.1089/pop.2019.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Byhoff E, Cohen AJ, Hamati MC, Tatko J, Davis MM, Tipirneni R. Screening for social determinants of health in Michigan health centers. J Am Board Fam Med. 2017;30(4):418–427. 10.3122/jabfm.2017.04.170079. [DOI] [PubMed] [Google Scholar]
- 23.Palakshappa D, Scheerer M, Semelka CTA, Foley KL. Screening for social determinants of health in free and charitable clinics in North Carolina. J Health Care Poor Underserved. 2020;31(1):382–397. 10.1353/hpu.2020.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weir RC, Proser M, Jester M, Li V, Hood-Ronick CM, Gurewich D. Collecting social determinants of health data in the clinical setting: findings from national PRAPARE implementation. J Health Care Poor Underserved. 2020;31(2):1018–1035. 10.1353/hpu.2020.0075. [DOI] [PubMed] [Google Scholar]
- 25.National Association of Community Health Centers. PRAPARE. https://www.nachc.org/research-and-data/prapare/. Accessed July 21, 2021.
- 26.Health Resources and Services Administration, Bureau of Primary Health Care. Uniform Data System (UDS) Resources. https://bphc.hrsa.gov/datareporting/reporting/index.html. Published August 16, 2020. Accessed July 21, 2021.
- 27.Gifford K, Ellis E, Lashbrook A, et al. A View from the states: key Medicaid policy changes: results from a 50-state Medicaid budget survey for state fiscal years 2019 and 2020. Kaiser Family Foundation. https://www.kff.org/medicaid/report/a-view-from-the-states-key-medicaid-policy-changes-results-from-a-50-state-medicaid-budget-survey-for-state-fiscal-years-2019-and-2020/. Published October 18, 2019. Accessed July 21, 2021. [Google Scholar]
- 28.Samuels-Kalow ME, Boggs KM, Cash RE, et al. Screening for health-related social needs of emergency department patients. Ann Emerg Med. 2021;77(1):62–68. 10.1016/j.annemergmed.2020.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Center for Health Care Strategies. Screening for social determinants of health in populations with complex needs: implementation considerations. https://www.chcs.org/resource/screening-social-determinants-health-populations-complex-needs-implementation-considerations/. Published October 26, 2017. Accessed July 21, 2021.
- 30.Davidson KW, McGinn T. Screening for social determinants of health: the known and unknown. JAMA. 2019;322(11):1037–1038. 10.1001/jama.2019.10915. [DOI] [PubMed] [Google Scholar]
- 31.Browne J, Mccurley JL, Fung V, Levy DE, Clark CR, Thorndike AN. Addressing social determinants of health identified by systematic screening in a Medicaid accountable care organization: a qualitative study. J Prim Care Community Health. 2021;12:2150132721993651. 10.1177/2150132721993651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bradley EH, Canavan M, Rogan E, et al. Variation in health outcomes: the role of spending on social services, public health, and health care, 2000–09. Health Aff (Millwood). 2016;35(5):760–768. 10.1377/hlthaff.2015.0814. [DOI] [PubMed] [Google Scholar]
- 33.Centers of Medicare and Medicaid Services. CMS issues new roadmap for states to address the social determinants of health to improve outcomes, lower costs, support state value-based care strategies. https://www.cms.gov/newsroom/press-releases/cms-issues-new-roadmap-states-address-social-determinants-health-improve-outcomes-lower-costs. Accessed July 21, 2021.
- 34.Tobin-Tyler E, Ahmad B. Marrying value-based payment and the social determinants of health through Medicaid ACOs: implications for policy and practice. Milbank Memorial Fund. May 2020. https://www.milbank.org/publications/marrying-value-based-payment-and-the-social-determinants-of-health-through-medicaid-acos-implications-for-policy-and-practice/. Accessed July 21, 2012. [Google Scholar]
- 35.Byhoff E, Freund KM, Garg A. Accelerating the implementation of social determinants of health interventions in internal medicine. J Gen Intern Med. 2018;33(2):223–225. 10.1007/s11606-017-4230-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gold R, Gottlieb L. National data on social risk screening underscore the need for implementation research. JAMA Netw Open. 2019;2(9):e1911513. 10.1001/jamanetworkopen.2019.11513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murray GF, Rodriguez HP, Lewis VA. Upstream with a small paddle: how ACOs are working against the current to meet patients’ social needs. Health Aff (Millwood). 2020;39(2):199–206. 10.1377/hlthaff.2019.01266. [DOI] [PubMed] [Google Scholar]
- 38.Cartier Y, Gottlieb L. The prevalence of social care in US health care settings depends on how and whom you ask. BMC Health Serv Res. 2020;20(1):481. 10.1186/s12913-020-05338-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alex Krist MD, Davidson KW, Ngo-Metzger Q. What evidence do we need before recommending routine screening for social determinants of health? Am Fam Physician. 2019;99(10):602–605. [PubMed] [Google Scholar]
- 40.Leavitt Partners. Social determinants matter, but who is responsible? https://leavittpartners.com/whitepaper/social-determinants-matter-but-who-is-responsible/. Accessed July 22, 2021.
- 41.Abir M, Hammond S, Iovan S, Lantz PM. Why more evidence is needed on the effectiveness of screening for social needs among high-use patients in acute care settings. Health Affairs Blog. May 23, 2019. 10.1377/hblog20190520.243444. [DOI] [Google Scholar]
- 42.Berkowitz SA, Basu S. Unemployment insurance, health-related social needs, health care access, and mental health during the COVID-19 pandemic. JAMA Intern Med. 2021;181(5):699–702. 10.1001/jamainternmed.2020.7048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Niles MT, Bertmann F, Belarmino EH, Wentworth T, Biehl E, Neff R. The early food insecurity impacts of COVID-19. Nutrients. 2020;12(7):2096. 10.3390/nu12072096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sandhu S, Lemmon ME, Eisenson H, Crowder C, Bettger JP. Addressing the social determinants of health during the COVID-19 pandemic: ensuring equity, quality, and sustainability. Fam Community Health. 2021;44(2):78–80. 10.1097/fch.0000000000000290. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


