Abstract
Background and Purpose:
Thrombectomy for large vessel occlusion acute ischemic stroke (AIS-LVO) may benefit patients up to 24 hour since last known normal (LKN). Prehospital tools, like the Cincinnati Stroke Triage Assessment Tool (C-STAT), are used to select hospital destination for suspected AIS-LVO patients. The objective of this study was to estimate the potential impact of the expanded thrombectomy time window on suspected AIS-LVO cases transported to the regional comprehensive stroke center (CSC).
Methods:
From June to November 2015, C-STAT was performed by prehospital providers following a positive prehospital Cincinnati Prehospital Stroke Scale (CPSS) stroke screen in suspected stroke/TIA patients. There was no preferential triage based on C-STAT results. Final diagnoses, including the presence of AIS-LVO was ascertained via medical record review. Impact of positive C-STAT cases on CSC volumes was estimated for up to 24 hours since LKN.
Results:
Of 158 patients with prehospital suspicion for stroke/TIA, 105 were CPSS positive within 24 hours of onset and had complete C-STAT and clinical data available for analysis. Forty-six percent (17/37) of C-STAT + were non-strokes. C-STAT sensitivity and specificity for LVO were 71% (95% CI 36–92) and 67% (95% CI 58–80), respectively. C-STAT triage would increase transport of prehospital suspected stroke cases to the CSC by 11% (12/105) within six hours and 21% (22/105) within 24 hours. Of 37 C-STAT + patients, only 5 (13.5%) had LVO as final diagnosis.
Conclusions:
Preferential triage of prehospital suspected stroke patients using C-STAT would increase the number of patients transported to the CSC by 11% within six hours and an additional 10% from six to 24 hours. For every patient with LVO as final diagnosis, approximately an additional 6 non-LVO patients would be triaged to a CSC.
Keywords: stroke, stroke scale, prehospital, triage
Introduction
Endovascular thrombectomy for patients with ischemic strokes due to a large vessel occlusion (AIS-LVO) is highly effective (1). Comprehensive Stroke Centers (CSC) offer advanced imaging, endovascular and surgical interventions, neurocritical care, post hospital care coordination, and stroke research (2).
Multiple clinical screening tools have been developed for prehospital triage of acute ischemic stroke patients to the appropriate location for care, however, no single tool has become widely accepted (3). The Cincinnati Stroke Triage Assessment Tool (C-STAT) (Figure 1) is a prehospital tool intended to be applied in suspected stroke patients to screen for severe versus non-severe stroke. C-STAT has been retrospectively derived, externally retrospectively validated, and prospectively evaluated in the prehospital setting (4, 5). We previously reported the performance of C-STAT in the prehospital setting in our region prior to initiation of severity-based prehospital triage of suspected stroke patients (5).
Figure 1.
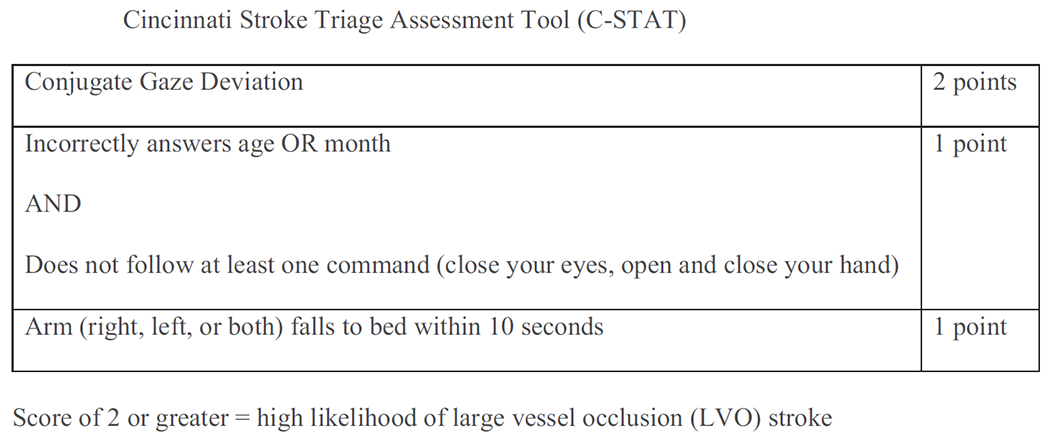
Cincinnati Stroke Triage Assessment Tool (C-STAT).
Recently, guidelines have extended the window for thrombectomy to 24 hours since last known normal (LKN) in carefully selected patients (1). As the majority of severe stroke patients are transported by Emergency Medical Services (EMS) (6), the accuracy of prehospital severity tools in potential AIS-LVO presenting in this expanded timeframe may meaningfully impact overall CSC volumes. Severe strokes present earlier than non-severe strokes (7), which may impact the prevalence of AIS-LVO in this expanded population. In this report, we estimated the potential impact of expansion of the thrombectomy time window to 24 hours since LKN on prehospital triage of suspected stroke patients to the regional CSC within six hours and from 6 to 24 hours.
Methods
This is an expanded secondary analysis of our previous prospective prehospital evaluation of the C-STAT (5).
Setting
Cincinnati Fire Department (CFD), an urban, firebased, advanced life support emergency medical services (EMS) system, is the sole 9-1-1 provider for approximately 60,000 annual emergency medical calls. Cincinnati Prehospital Stroke Scale (CPSS) (8) and C-STAT are performed whenever there is clinical suspicion for stroke. CPSS serves as a screening tool for strokes and is considered positive if one or more elements are abnormal. C-STAT is applied in CPSS-positive patients and considered positive for scores of 2 or more. During the study period, CFD did not preferentially triage subjects based on C-STAT score; there was one CSC and multiple, non-thrombectomy capable primary stroke centers receiving patients from CFD during the study period.
Subjects
The study population consisted of all patients transported to any hospital by CFD with a prehospital clinical impression of stroke or transient ischemic attack (TIA) from June 1 to November 30, 2015. Patient/caregiver preference determined hospital destination per existing standard of care. Patients 18 years or older were included in the data analysis if they were both CPSS positive by EMS and had a calculable C-STAT, and had outcome data in their medical records. The University of Cincinnati and all participating regional hospital Institutional Review Boards approved the study procedures without requirement of informed consent. Our previous analysis was limited to patients transported to the CSC (5); for this expanded analysis, we include all patients transported by CFD to regional hospitals.
Outcome Assessment
For this analysis, the outcome was the proportion of patients with a suspected stroke/TIA and LKN 0–6 or 6–24 hours that would be transported to a CSC with prehospital C-STAT-based triage.
Data Abstraction
CFD’s prehospital care record required entry of CPSS and C-STAT assessments to complete documentation for any patient with a prehospital clinical impression of stroke or TIA. EMS and hospital medical records were matched and underwent structured abstraction by a trained stroke research nurse or study physician. Final diagnoses and the presence or absence of LVO was ascertained via chart review.
Statistical Analysis
Demographic and clinical characteristics were summarized, using mean (standard deviation) for age and count (percentage) for all other variables, by final diagnosis of acute ischemic stroke/TIA, non-ischemic stroke, or non-stroke. C-STAT test characteristics, sensitivity and specificity, for LVO (defined as ICA and M1 occlusions only) were calculated with 95% confidence intervals (CI) using the Wilson interval. The number with preferential triage using C-STAT up to 24 hours from LKN was estimated along with 95% CIs using the Wilson interval (9).
Results
Of 158 patients with prehospital suspicion for stroke/TIA, 105 were CPSS positive, within 24 hours of onset, and had complete C-STAT and clinical data available for analysis. Of the 53 excluded patients, 22 had negative CPSS screen, 5 had incomplete CPSS data, 19 had incomplete C-STAT data, 4 had missing clinical data, and 3 had LKN >24 hours. Among CPSS positive patients, 56 out of 105 (53%) had a final diagnosis of stroke (Table 1). Thirty-seven (35%) CPSS positive patients were C-STAT positive. Of these, 15 (40%) were AIS/TIA, 5 (13%) were ICH and 17 (46%) were non-strokes; 5 out of 37 (14%) C-STAT positive cases had LVO. Two out of 68 (3%) of C-STAT negative patients were found to have an LVO. C-STAT sensitivity and specificity for LVO were 71% (95% CI 36–92) and 67% (95% CI 58–76), respectively. Table 2 shows final diagnoses in C-STAT positive and C-STAT negative subjects. Figure 2 provides a visual representation of our analysis.
Table 1.
Patient characteristics
| Acute Ischemic Stroke/TIA (N = 45) | Non-ischemic stroke (N = 11) (all ICH) | Non-stroke (N = 49) | |
|---|---|---|---|
| Age, mean (SD) | 73 (15) | 62 (16) | 64 (14) |
| Race, N (%) black | 20 (49%) (n = 41) | 5 (62%) (n = 8) | 25 (58%) (n = 43) |
| Gender, N (%) female | 25 (56%) | 5 (45%) | 26 (53%) |
| NIHSS ≥ 10, N (%) | 16 (36%) | 6 (67%) (n = 9) | NA |
| NIHSS ≥ 15, N (%) | 12 (27%) | 4 (44%) (n = 9) | NA |
| LVO Present, N (%) | 7 (16%) | NA | NA |
| C-STAT ≥ 2, N (%) | 15 (33%) | 5 (45%) | 17 (35%) |
| 0–6 hours from last known well, N (%) | 27 (60%) | 9 (82%) | 31 (63%) |
| 6–24 hours from last known well, N (%) | 18 (40%) | 2 (18%) | 18 (37%) |
| Transported to CSC, N (%) | 17 (38%) | 8 (73%) | 24 (49%) |
Table 2.
Final diagnoses by C-STAT positive and C-STAT negative
| C-STAT Positive (≥2) (N = 37) | C-STAT Negative (<2) (N = 68) | |
|---|---|---|
| Acute Ischemic Stroke | 12 (32%) | 20 (29%) |
| • LVO present | 5 (14%) | 2 (3%) |
| TIA | 3 (8%) | 10 (15%) |
| Non-ischemic stroke (ICH) | 5 (14%) | 6 (9%) |
| Non-stroke | 17 (46%) | 32 (47%) |
| • Seizure | 5 (14%) | 3 (4%) |
| • Altered mental status/encephalopathy | 5 (14%) | 12 (18%) |
Figure 2.
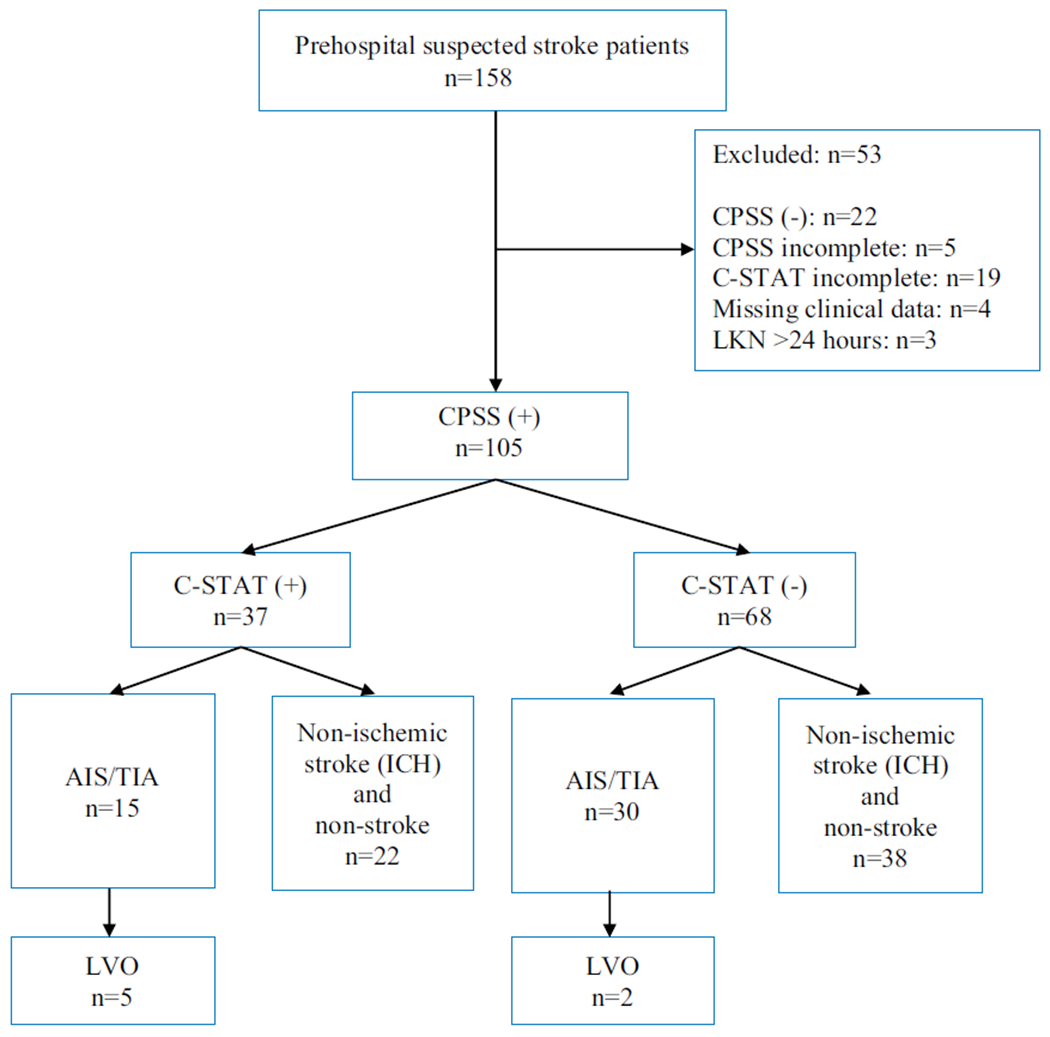
Consort diagram of study population.
Four of the C-STAT positive patients had a CTA (CT angiogram) performed in the emergency department based on chart review. Of the patients transported to a CSC 15/49 (31%) had a CTA in the emergency department, whereas 3/56 (5%) had a CTA in the emergency department among those that went to a primary stroke center (PSC).
Without a preferential triage protocol, 49 subjects (including 15C-STAT positive) were transported to the CSC. Within six hours, nine out of 21C-STAT positive prehospital suspected stroke patients were triaged to the CSC and 12 were not. From 6 to 24 hours, six C-STAT positive prehospital suspected stroke patients were triaged to the CSC and 10 were not.
Overall, preferential triage using C-STAT would increase transport of prehospital suspected stroke cases to the CSC by 11% (12/105) (95% CI 7–19%) within six hours and 21% (22/105) (95% CI 14–30%) within 24 hours.
Discussion
The rapid advancement in stroke care in recent years has reemphasized the importance of recognition of AIS and LVO in the prehospital setting in order to appropriately triage stroke patients. Emergency medical dispatchers and EMS are essential in the identification of stroke patients, and have relatively high sensitivity in identifying AIS patients (10). Existing stroke triage tools such as the CPSS can reliably identify LVO in prehospital AIS patients with higher cutoff scores (11). Multiple prediction tools for prehospital identification of severe strokes have been developed, but none have been shown to have sufficiently high specificity and sensitivity based on an AHA/ASA 2018 systematic review (3).
When applied within six hours of LKN, prehospital triage based on C-STAT would have resulted in 11% more prehospital suspected stroke patients transported to the CSC; an additional 10% would be transported to the CSC if the LKN time window was expanded from 6 to 24 hours. As such, the expansion of the thrombectomy time window to 24 hours may approximately double the total number of prehospital suspected stroke patients triaged to our regional CSC. The study was conducted during a time window where there was no preferential triage, and there was only one thrombectomy-capable facility in the region. Thus, these estimates represent the maximum amount of increased triage likely in our region. In this study, the absolute number of increased patients at the CSC was low and should not significantly impact ED and CSC operations, though with rapidly changing stroke care and potential future changes in guidelines and protocol, this number may change.
The current Mission:Lifeline Severity-based Stroke Triage Algorithm for EMS currently recommends transport of suspected LVO patients with LKN time under six hours to the closest appropriate stroke center if transport to CSC adds more than 15 minutes or will preclude the use of alteplase (12). Recent publications suggest longer bypass time for suspected stroke patients may be reasonable. Holodinsky et al. estimated similar outcomes when the centers are less than 60 minutes apart in a study that modeled outcomes when transporting to a closer alteplase facility versus transporting directly to an endovascular capable center (13). Benoit et al. suggested bypass time to an endovascular ready hospital up to 44 additional minutes may be reasonable (14). If increased bypass times are incorporated in EMS protocols, CSCs/ thrombectomy centers may see even higher suspected stroke patients arriving at their facilities.
Only 5 out of 37 C-STAT positive patients had a final diagnosis of LVO. Additionally, we found that about half of CPSS positive and CPSS and C-STAT positive prehospital suspected stroke patients ultimately had non-stroke final diagnoses. EMS evaluation of stroke patients has shown great accuracy in finding large motor cortical deficits (unilateral weakness, facial weakness, and speech problem), though patients who had atypical presentations (dizziness, headache, and malaise) resulted in both missed strokes and false-positives. Posterior circulation strokes also have atypical presentations and can be difficult to evaluate with current screening tools (15). Pickham et al. evaluated whether adding balance/coordination and eye/diplopia evaluation to CPSS in the prehospital setting would improve stroke detection. Their modified CPSS performed about the same as the CPSS with regard to stroke detection and mimics (16). Given that these stroke and stroke severity screening tools currently form the backbone of prehospital stroke evaluation and triage and all have similarly limited performance in real-life scenarios, future investigation and research in improved prehospital diagnostics for severe strokes and LVOs are warranted.
Our study had several limitations. Generalizability is limited by our relatively small sample size in one geographic region. The data were limited to patients who had both a CPSS and C-STAT completed, meaning cases where the prehospital provider did not suspect stroke would have been missed. These criteria mirror clinical reality, as such “missed” cases would not factor into prehospital triage decisions. Increased transports to CSCs may be overestimated since thrombectomy-capable hospitals are a new designation that may result in fewer subjects being transported directly to the CSC.
Conclusion
Within the Cincinnati Fire Department, triage of suspected stroke patients using C-STAT would increase transport of prehospital suspected stroke cases to the regional CSC by 11% within six hours since LKN and an additional 10% when LKN is expanded from 6 to 24 hours. Given the accuracy of prehospital stroke triage tools, additional prospective study to improve evaluation, diagnosis, treatment and outcomes of prehospital suspected stroke cases is warranted.
Acknowledgments
This work was supported by UC Garner Neuroscience Institute.
Footnotes
No potential conflict of interest was reported by the authors.
Color versions of one or more of the figures in the article can be found online at www.tandfonline.com/ipec.
Contributor Information
James L. Li, Department of Emergency Medicine, University of Cincinnati, Cincinnati, OH.
Jason T. McMullan, Department of Emergency Medicine, University of Cincinnati, Cincinnati, OH.
Heidi Sucharew, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH.
Joseph P. Broderick, Department of Neurology and Rehabilitation, University of Cincinnati, Cincinnati, OH; University of Cincinnati Gardner Neuroscience Institute, Cincinnati, OH.
Brian Katz, Ohio Health Neurological Physicians, Ohio Health, Columbus, OH.
Pamela Schmit, Department of Emergency Medicine, University of Cincinnati, Cincinnati, OH.
Opeolu Adeoye, Department of Emergency Medicine, University of Cincinnati, Cincinnati, OH; University of Cincinnati Gardner Neuroscience Institute, Cincinnati, OH.
References
- 1.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, et al. 2018. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/ American Stroke Association. Stroke. 2018;49:e46–e99. [DOI] [PubMed] [Google Scholar]
- 2.Gorelick PB. Primary and comprehensive stroke centers: history, value and certification criteria. J Stroke. 2013;15:78–89. doi: 10.5853/jos.2013.15.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith EE, Kent DM, Bulsara KR, Leung LY, Lichtman JH, Reeves MJ, Towfighi A, Whiteley WN, Zahuranec DB. Accuracy of prediction instruments for diagnosing large vessel occlusion in individuals with suspected stroke: a systematic review for the 2018 guidelines for the early management of patients with acute ischemic stroke. Stroke. 2018;49: e111–22. doi: 10.1161/STR.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 4.Katz BS, McMullan JT, Sucharew H, Adeoye O, Broderick JP. Design and validation of a prehospital scale to predict stroke severity: Cincinnati Prehospital Stroke Severity Scale. Stroke. 2015;46:1508–12. doi: 10.1161/STROKEAHA.115.008804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McMullan JT, Katz B, Broderick J, Schmit P, Sucharew H, Adeoye O. Prospective prehospital evaluation of the cincinnati stroke triage assessment tool. Prehospital Emerg Care. 2017;21:481–8. doi: 10.1080/10903127.2016.1274349. [DOI] [PubMed] [Google Scholar]
- 6.Mochari-Greenberger H, Xian Y, Hellkamp AS, Schulte PJ, Bhatt DL, Fonarow GC, Saver JL, Reeves MJ, Schwamm LH, Smith EE. Racial/ethnic and sex differences in emergency medical services transport among hospitalized US stroke patients: analysis of the National Get With The Guidelines-Stroke Registry. JAHA. 2015;4:e002099. doi: 10.1161/JAHA.115.002099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lichtman JH, Watanabe E, Allen NB, Jones SB, Dostal J, Goldstein LB. Hospital arrival time and intravenous t-PA use in US Academic Medical Centers, 2001–2004. Stroke. 2009;40: 3845–50. doi: 10.1161/STROKEAHA.109.562660. [DOI] [PubMed] [Google Scholar]
- 8.Kothari RU, Pancioli A, Liu T, Brott T, Broderick J. Cincinnati prehospital stroke scale: reproducibility and validity. Ann Emerg Med. 1999;33:373–8. doi: 10.1016/S0196-0644(99)70299-4. [DOI] [PubMed] [Google Scholar]
- 9.Brown LD, Cai TT, DasGupta A. Interval estimation for a binomial proportion. Statist Sci. 2001;16:101–33. doi: 10.1214/ss/1009213286. [DOI] [Google Scholar]
- 10.Richards CT, Huebinger R, Tataris KL, Weber JM, Eggers L, Markul E, Stein-Spencer L, Pearlman KS, Holl JL, Prabhakaran S. Cincinnati prehospital stroke scale can identify large vessel occlusion stroke. Prehospital Emerg Care. 2018;22:312–8. doi: 10.1080/10903127.2017.1387629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mould-Millman N-K, Meese H, Alattas I, Ido M, Yi I, Oyewumi T, Colman M, Frankel M, Yancey A. Accuracy of prehospital identification of stroke in a large stroke belt municipality. Prehospital Emerg Care. 2018;22:734–42. doi: 10.1080/10903127.2018.1447620. [DOI] [PubMed] [Google Scholar]
- 12.American Heart Association/American Stroke Association. Severity-based stroke triage algorithm for EMS. Available from: http://www.heart.org/mission-lifelinestroke. Accessed December 1, 2017.
- 13.Holodinsky JK, Williamson TS, Demchuk AM, Zhao H, Zhu L, Francis MJ, Goyal M, Hill MD, Kamal N. Modeling stroke patient transport for all patients with suspected large-vessel occlusion. JAMA Neurol. 2018;75:1477–86. doi: 10.1001/jama-neurol.2018.2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benoit JL, Khatri P, Adeoye OM, Broderick JP, McMullan JT, Scheitz JF, Vagal AS, Eckman MH. Prehospital triage of acute ischemic stroke patients to an intravenous tPA-ready versus endovascular-ready hospital: a decision analysis. Prehospital Emerg Care. 2018;22:722–33. doi: 10.1080/10903127.2018.1465500. [DOI] [PubMed] [Google Scholar]
- 15.Brandler ES, Sharma M, McCullough F, Ben-Eli D, Kaufman B, Khandelwal P, Helzner E, Sinert RH, Levine SR. Prehospital stroke identification: factors associated with diagnostic accuracy. J Stroke Cerebrovasc Dis. 2015;24:2161–6. doi: 10.1016/j.jstrokecerebrovasdis.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 16.Pickham D, Valdez A, Demeestere J, Lemmens R, Diaz L, Hopper S, de la Cuesta K, Rackover F, Miller K, Lansberg MG. Prognostic value of BEFAST vs. FAST to identify stroke in a prehospital setting. Prehospital Emerg Care. 2019;23: 195–200. doi: 10.1080/10903127.2018.1490837. [DOI] [PubMed] [Google Scholar]


