Abstract
Telemedicine was underused and understudied until the COVID-19 pandemic, during which reduced regulations and increased payment parity facilitated a rapid increase in telemedicine consultation. Telemedicine literature to date suggests that it holds benefits for patients and health care providers, may result in outcomes not inferior to in-person care, and has cost-saving implications. Future research should investigate which conditions are best suited to assess and treat via telemedicine (including physical exam elements), what techniques improve telemedicine communication, how to help patients equitably access telemedicine, and how to best educate the future health care workforce.
Keywords: Telemedicine, Telehealth, COVID-19, Health care outcomes, Access, Health equity, Education
Key points
-
•
Telemedicine health care has grown in the United States since the beginning of the COVID-19 pandemic and will remain an integral part of medical care.
-
•
Telemedicine is well received by many patients and health care providers but remains more accessible to certain groups of patients than others.
-
•
Telemedicine care can be equivalent to in-person care for certain acute and chronic conditions. The telemedicine physical examination should be further studied for how it may contribute to patient assessment.
-
•
Future clinicians and all levels of learners within health care will require more specific training on how to logistically manage telemedicine technology and how to clinically navigate a remote consultation.
Introduction
The “house call” from doctors is surging in the United States, and instead of ringing the doorbell, your doctor is pinging your smartphone. Telemedicine, or receiving one’s medical care remotely via synchronous, asynchronous, or store-and-forward technology, had been on a steady increase for the last decade, but the overall growth had remained slow until March 6, 2020. In response to the SARS-CoV-2 pandemic crisis, the US Congress toppled a multitude of telemedicine regulations, and telemedicine expanded rapidly. Although the acute pandemic crisis may be entering its long tail, telemedicine will remain a permanent fixture in routine American health care. How will this serve us as practitioners and patrons of medicine? The experiences of the last several years can help us forge our path forward into a future with virtual health care.
Definitions of Telemedicine and Telehealth
The definitions of these two terms depend upon whom you ask and what you read, as there are currently more than one hundred different peer-reviewed definitions.1 A general consensus shared by most is that telemedicine refers to providing clinical services (either in real time or asynchronously) between patient and clinician and/or between clinician and clinician when the two parties are physically remote from one another using some form of information-communication technology. The term telehealth is a larger umbrella term encompassing other remote health-related services, such as administration, continuing medical education, and/or provider training.
Telemedicine in the United States before March 2020
Before March 2020, telemedicine use in the United States was on a steadily increasing trajectory, but its absolute integration remained low, and the logistics were complex.2 , 3 Patients and providers who desired to use it navigated inconsistent and often inadequate reimbursement for services, restrictions on where each party must be located and what sort of technology interface they must use, and privacy regulations that necessitated costly investments in secure telecommunication technology. Providers were (and often still are even in a postpandemic landscape) limited from treating traveling patients by interstate licensing restrictions, and juggled miscellaneous rules about prescriptions, types of visits, and types of patients that were or were not acceptable for telemedicine.4 Despite these hurdles, 76% of US hospital systems used some form of telemedicine as of 2018, with radiology, psychiatry, and cardiology noted as the highest users of the modality.5 Systems factors, such as technology capability of the electronic medical record and other characteristics driven by reimbursement policies (such as rural location), influenced which hospitals or clinics were more likely to offer telehealth,6 , 7 further limiting which patients had the option of using this service.
Of the patients who were able to access telemedicine before March 2020, their overall impressions were positive.8, 9, 10, 11, 12, 13 In a systematic review on the topic, the most frequently cited factors associated with patient telehealth satisfaction included improved outcomes (defined a variety of ways owing to heterogeneity of the 44 included studies), preferred modality over face-to-face visits, ease of use, low cost, improved communication, and elimination of travel time.9 Patients also expressed some concerns about telemedicine, such as data security.14 The telemedicine appointments assessed in these studies were almost entirely video-conferencing rather than telephone-only owing to reimbursement restrictions on the latter.
Clinicians had a more variable opinion of telemedicine, perhaps driven by inexperienceas most were not using it before the pandemicand those who did use it still conducted most of their visits in person. About half of clinicians surveyed in one setting (respondents largely consisting of psychiatry providers) who were actively using both telehealth and office visits in their practices were concerned that the personal connection through telehealth was inferior to office visits.11 Approximately one-third of those clinicians also stated that the overall quality of the visit was better in person. Family medicine providers (N = 1630) surveyed about the reasons behind their nonuse of telehealth were more likely than current users to feel it was an inefficient use of their time, and to express concerns about the overall quality of care and the liability potential. Nonusers were also more likely to cite lack of training, equipment costs, liability concerns, and inadequate reimbursement as barriers to telehealth.15
COVID-19 drives telehealth expansion and gives new insights on patient and provider use
The widespread recognition of SARS-CoV-2 in the United States by March 2020 upended many of the prior barriers to telemedicine. Patients who would have had in-person office visits for their needs were isolating, quarantining, sheltering under health orders, or fearful to venture out. In early March 2020, Congress made major alterations to Medicare restrictions on where telemedicine must originate, what would be reimbursed, and what platforms could be used (Table 1 ). This paved the way for similar relaxations on interstate practice and privacy regulations, and reimbursements for telemedicine improved dramatically. State and private payors promptly followed Medicare’s lead in a collective effort to keep health care channels open and practices solvent.2
Table 1.
Comparison of Centers for Medicare & Medicaid Services telehealth regulations before and after March 2020
| Before March 2020 | After CARES Act and CMS 1135 Waiver |
|---|---|
| Who can perform and receive telehealth | |
| Only certain licensed providers | Any type of clinician can bill for Medicare services |
| Patients and providers who have a preexisting relationship | No preexisting relationship will be required |
| Where can telehealth be done | |
| Only at prespecified sites (ie, designated rural areas, certain medical facilities) | Telehealth may originate and be conducted from any site, including patient’s home |
| Physicians must conduct telehealth from their place of practice | Physicians may conduct telehealth from home |
| Telehealth may not cross state lines | Telehealth can now be provided to patient in another state (state-specific restrictions may still apply) |
| What must be used for telehealth visits | |
| Must be audio-visual (ie, video technology) | Audio-visual OR audio-only are allowed |
| Only approved technology platforms | Expanded approved platforms, including FaceTime, Skype, and Zoom |
| How is telehealth reimbursed | |
| Medicare coinsurance and deductibles apply to telehealth visits | Providers may waive cost-sharing for telehealth paid for by federal programs |
| Reimbursements for telehealth services is lower than for in-person services | All telehealth visits, including audio-only, will be reimbursed as if the service was furnished in person |
Data from CARES Act AMA Covid-19 Fact Sheet (https://www.ama-assn.org/delivering-care/public-health/cares-act-ama-covid-19-pandemic-telehealth-fact-sheet) and Medicare Telemedicine Healthcare Provider Fact Sheet (https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet). Accessed 2/2/2022.
In response, practices greatly expanded telemedicine services during the long months of shelter in place and recurrent surges of COVID-19 infections, and patient use of telehealth services blossomed. A national study including 36 million working-age individuals with private insurance claims data showed that telemedicine encounters increased 766% in the first 3 months of the pandemic, from 0.3% of all interactions in March to June 2019, to 23.6% of all interactions in the same period.16 This is in line with research by the Doximity online medical networking service, which counts 1.8 million physicians (about 80% of the US physician workforce) among its membership, estimating with private claims data that approximately 20% of all US health care visits in 2020 were conducted by telemedicine.17 However, even as telemedicine skyrocketed, medical care in general across the United States showed a sharp decline that could not be made whole despite best efforts. One estimate using claims data from 16.7 million Medicare Advantage and commercial insurance patients estimated that total outpatient visits plummeted by 30% of usual volume between January and June 2020, and that telemedicine only compensated for about two-thirds of this loss.18 Physicians across the nation were severely impacted between reduction in overall visit volume, increased spending on personal protective equipment, and pervasive staffing challenges. Eighty percent of physicians surveyed by the American Medical Association reported a persistent reduction in income (average reported decrease of 32%) at 5 months into the pandemic.19
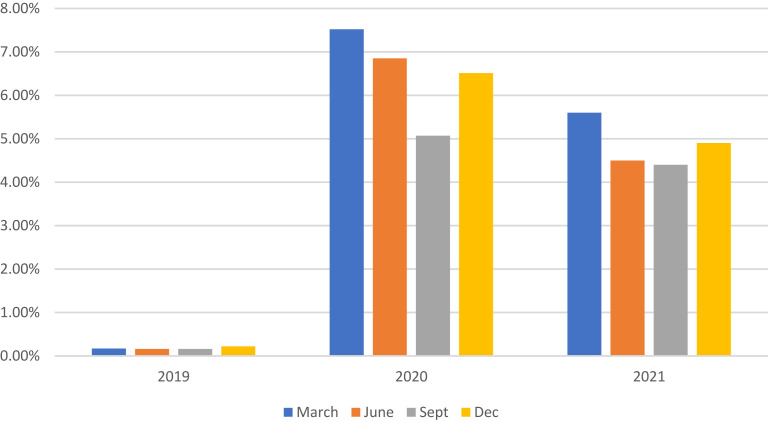
Even as isolation precautions have relaxed and shelter-in-place orders are past, telehealth is showing some staying power. FAIRHealth,20 which manages a large national database of both private and Medicare claims data, shows that although in-person care is still chosen most of the time, the overall percentage of telehealth claims has ballooned from 0.1% in 2019 to hover just around 5% at the close of 2021 (Fig. 1 ).
Fig. 1.
Telehealth claims (as a percentage of all claims) in the United States from 2019 to 2021, based on FAIRHealth reported claims data, which includes participating Medicare and private insurance plans.
(Data from FAIRHealth Monthly Telehealth Regional Tracker. https://www.fairhealth.org/states-by-the-numbers/telehealth. Accessed 12/10/2021.)
Discussion: telemedicine during and after COVID-19
Who Is Using Telemedicine Now?
Although disappearing regulations have somewhat leveled the playing field for all to participate, there are still various factors that predict which physicians and which patients are more likely to engage in telemedicine. What we know about physicians accessing telemedicine comes from studies of large academic practices, claims data from commercial insurance, and research from Doximity.
According to available data, the number of physicians reporting telemedicine as an active skill has doubled as of 2020, from 20% to just less than 40% of the Doximity survey.17 A physician most likely to be practicing telehealth today treats patients who have chronic diseases, such as in endocrinology, gastroenterology, rheumatology, nephrology, cardiology, and psychiatry, whereas physicians in dermatology, orthopedic surgery, or optometry are least likely to report telemedicine use (note: these references did not distinguish between subspecialists who treat chronic disease and primary care physicians who may treat the same conditions).17 , 18 , 21 Telemedicine practitioners tend to identify as female more often than male and are between 40 and 60 years of age.17 They live predominantly in large metropolitan areas or on the East Coast.17 , 18 The clinician demographics are likely influenced by the inherent demographics of the high-telemedicine specialties.
As telehealth rapidly evolves, it is important to note what has changed (and what has not) now that insurance type, physical location, and technology platform should present fewer barriers for all to use telemedicine. Historically, it has been challenging to describe the typical “telemedicine user,” because telemedicine use was such a small proportion of care before the pandemic. What has been reported about the demographics of telemedicine users before 2020 reflects what would be expected of those select patients that either were granted access (eg, large academic centers, Veterans Administration health system, integrated health systems) or purchased access (eg, through direct-to-consumer telemedicine services). In contrast, some patients who might be expected to frequently use telemedicine (including those who live far away from in-person care, such as large areas in the middle of the United States) were often effectively excluded owing to lower rates of household internet access. Others who suffered from the digital divide included households of lower socioeconomic status and patients with disabilities.22
With the advent of the pandemic in 2020, reimbursable telemedicine services expanded to include telephone-only visits and removed geographic barriers and platform restrictions. Interestingly, this has not addressed the inequities in telemedicine use as much as one might predict. Studies inclusive of March to August 2020, which examined demographics of new telemedicine users, show a surprisingly similar picture to the prepandemic period: patients who use telemedicine still tend to be white, younger, wealthier, and more urban-dwelling than non-telemedicine-using peers.16 , 23, 24, 25, 26 This demographic discrepancy becomes even more apparent when examining video telemedicine users compared with telephone (audio-only) users.23 , 24 , 26 Although this picture of the typical telemedicine user may reflect the larger troubling patterns of inequitable access to medical care in general in our country, these data should still guide us as we move into a more telemedicine-dependent future. Our most vulnerable, marginalized, and chronically ill patients will need additional attention and funding dollars to understand all their barriers (digital and otherwise) to this type of care that we hope could address their care gaps, and to prevent telemedicine from becoming yet another wedge to widen medical disparities in our country.
Despite the observed differences in utilization, telemedicine visits did globally increase for all types of patients compared with rates in 2019 and prior, especially among those with chronic illnesses.17 Perceptions of telemedicine care from this much larger sample of users continue to be positive overall whether they are new to telemedicine or experienced. One survey of 800 patients at Penn Medicine in the first half of 2020 reported that 67% of respondents considered their video or telephone visit “as good or better” than a standard in-person visit.27 A similar survey of 1011 University of Michigan Medicine patients in early 2020 showed similar degrees of high satisfaction between first-time users and repeat patient users of telemedicine.28 In addition, although telemedicine use varies significantly based on certain demographics (as described above) because of either preference or barriers, those who use it across different demographics can have a similar experience. A nationally representative sample of US households (N = 3454) surveyed on telemedicine use during the pandemic affirmed that telemedicine use differed significantly based on race, household income, insurance status, and presence of high-speed internet (in keeping with the literature cited above), but that those who did use telemedicine even in lower-income households or non-white households seemed equally satisfied with their experience.29
What Do We Know About Conditions that Are Evaluated by Telemedicine?
In the literature to date, telemedicine is most often evaluated by examining patient acceptance of care using technology, patient and clinician satisfaction with the visit, and patient perception of care they received. Studies examining patient-oriented health outcomes or economic impact on individuals and systems are less common and are needed to delineate how telemedicine can be best used for future medical care.
Before the COVID-19 pandemic, research on telemedicine health care outcomes had some inherent challenges. Patients using telemedicine were a self-selected audience with the inherent differences that accompany this, and telemedicine is a broad category that encompasses many different intervention types ranging from simple telephone encounters to highly intensive encounters involving facilitators or digital examination equipment, such as stethoscopes or otoscopes able to transmit audio-visual information to a remote provider. Likewise, it is challenging to compare outcomes between telemedicine and face-to-face care in a prepandemic world where clinicians might prioritize in-person encounters for more high-risk or medically complex individuals when there is no limitation or disincentive for doing so.
Despite these challenges, there is now more literature to support telemedicine as a viable alternative to in-person care in certain situations. One of the more comprehensive looks at this topic was a systematic review of telemedicine practice in primary care before the pandemic, including 81 studies conducted both domestically and abroad.30 The results from this study have been supplemented by other publications conducted during the pandemic, and general conclusions about patient outcomes for different categories of careare summarized below.
Acute care using telemedicine
Telemedicine has been studied in various acute conditions as compared with usual care, including uncomplicated cystitis, upper respiratory tract infections (URI), pharyngitis, and low-back pain. Results of these studies are heterogenous. Some suggest that telemedicine care for conditions such as URI and low-back pain can result in similar or improved clinical outcomes for patients, with “clinical outcomes” usually defined narrowly as a single categorical item (such as appropriate vs inappropriate use of antibiotics for a given diagnosis). In a nurse-administered telephone or a Web-based protocol for URI and sinusitis treatment, overall antibiotic administration with telemedicine for viral URI was less than usual care, and first-line antibiotics were more often prescribed for cases of sinusitis meeting clinical criteria.31 , 32 In an evaluation of care administered by Teladoc, a direct-to-consumer telemedicine consultation service, telemedicine consultations did not order imaging for low-back pain (appropriately so) at about the same rate as in-person evaluations.33
Other studies in direct-to-consumer telemedicine differ, suggesting that patients who received telemedicine may be more likely to receive inappropriate antibiotics than when seen in face-to-face care33, 34, 35 and are less likely to receive an appropriate rapid strep test for evaluation of pharyngitis.33 The variations in medication use and diagnostic testing seen in these studies may be explained by the context of a direct-to-consumer telemedicine encounter. The typical model for direct-to-consumer telemedicine is a single encounter between a clinician and patient who have no preceding relationship, and the clinician is often limited by lack of on-site testing, no means to bring patient in for a face-to-face examination, and little way to ensure the patient will access follow-up care if they get worse. Telemedicine outcomes may look different when delivered within a context where physicians and patients know one another, a consistent medical record is available, on-site testing may be achievable, and there is more readily accessible follow-up care. An observational study in this type of setting (a large integrated health system) analyzed more than 1 million visits: telephone, video, and office visits, for any type of initial concern (excluding routine physical examination) during a 2-year period. Patients initiated scheduling of the visit modality themselves via a Web-based scheduling portal. The investigators found that rates of overall prescribing of medication or imaging (across all diagnoses as well as a subanalysis of visits only for URI symptoms) were actually lower for telemedicine (telephone or video) as opposed to in-person care, and that the need for emergency department (ED) or hospital visit within 7 days following the index visit did not differ between telemedicine and in person.36 This suggests that clinicians using telemedicine may be less likely to overprescribe or overuse testing as a precautionary measure when they have some prior knowledge of the patient and when they feel confident that follow-up care is available should things get worse.
This study also demonstrates that when examined in a very large sample and over a broad array of diagnoses, assessment and treatment via telemedicine seem no more likely to result in acute decompensation requiring emergency room services or hospitalization than traditional in-person care. However, emergency and hospital care is an uncommon outcome to begin with; in this study, overall rates of ER visits within a week of index visits were approximately 1% across all visit types, and hospitalizations were less than 0.5%. Future studies may do well to see if this conclusion holds true when telemedicine care is used for specific diagnoses (dizziness, abdominal pain, dyspnea) that may be more challenging to assess, or for different types of telemedicine users that may have communication barriers.
For acute skin concerns, tele-dermatology is already used in multiple countries for routine dermatologic management, to consult on patients in remote locales, or for medical support in nursing homes or home care settings.37 However, most studies to this point have not examined a specific comparison with usual (in-person) consultation. Tele-dermatology may serve an intuitive role as a follow-up method once a diagnosis has been established, to triage whether an in-person consultation is needed, or to guide primary physicians on the best next steps in management for routine conditions.
Chronic care using telemedicine
Telemedicine has been studied for many chronic conditions, such as asthma, chronic obstructive pulmonary disease (COPD), depression, diabetes, hypertension, hyperlipidemia, and heart failure. Some of the most robust evidence for improved patient outcomes with telemedicine care comes from pharmacist-based telemedicine interventions. A systematic review of 34 studies looking at chronic disease management using pharmacist-delivered telemedicine care protocols examined outcomes for different conditions (hypertension, diabetes, anticoagulation, depression, hyperlipidemia, asthma, heart failure, HIV, posttraumatic stress disorder, chronic kidney disease, stroke, COPD, and smoking cessation).38 The investigators noted the heterogeneity of studies and for this reason did not perform a data synthesis to quantify collective results and instead performed a narrative review. Most included studies (N = 25) examined telephone-only interventions as opposed to more technology-intensive ones, and studies were included in the final review if they used a comparison (ie, face-to-face, usual care, or no intervention) and if they evaluated as outcomes either chronic disease management (ie, achievement of laboratory values specific to therapeutic goals), patient self-management (ie, self-monitoring blood pressure or demonstration of inhaler use), or adherence (ie, patient self-report or pharmacy records showing medication fills). Results showed good success for telemedicine interventions, with 23 out of 34 studies logging positive improvements in disease management, self-management, or adherence measures. Another 10 studies reported neutral outcomes (noninferior to the comparison), and only one study concluded any sort of negative outcome for the telemedicine group. A scheduled model of care, described as pharmacists delivering telemedicine interventions to patients at predetermined times, was the most common and the most successful delivery system for improved outcomes as opposed to a responsive/reactive model (pharmacist reaching out to patient when being prompted to do so by a health system alert). Similar benefits of pharmacist-led virtual care have been documented as health systems rapidly transitioned chronic disease care to virtual visits during the pandemic.39
One notable aspect of this systemic review is the increased success of scheduled telemedicine care as opposed to a more responsive/reactive model, affirming that a high degree of reinforcement and support is beneficial for chronic disease management in general whether in person or otherwise. Shifting some of this care to telemedicine could conceivably lower overall system costs through reduced overhead and possibly improved patient outcomes (if evidence cited above proves accurate) but would likely require upfront investment in clinicians or other personnel to support the consistent, high-frequency visits. The overall impact on physician and practice revenue is also unclear, as reimbursement for telemedicine may become less favorable when the pandemic wanes.
Other small studies show some benefit of telemedicine for other chronic conditions. One study demonstrates that telemedicine intervention delivered over an extended period (ie, 24 months) can be as successful as in-person care for weight loss of primary care patients, with either telemedicine or in-person treatment groups achieving equivalent weight loss and more so than the “no-treatment” arm.40 Telemedicine also shows some promise with management of chronic musculoskeletal pain; patients who participate in a 12-month telemedicine intervention with algorithmic guide to pharmacologic management had improved pain scores at 1 year as compared with usual care.41
Despite the promise of evidence above, conclusions about telemedicine effectiveness overall can be difficult to determine, as the types and intensity of interventions vary drastically from study to study. In the case of asthma care, for example, one frequently cited telemedicine study entitled “Telemedicine is as effective as in-person visits for patients with asthma” concludes that children in the telemedicine group and children in an in-person visit group had similar degrees of asthma control over a 6-month study period.42 However, the intervention described in the article is a highly intensive “Remote Presence Solution” involving a digital stethoscope and otoscope and a high-resolution camera situated at the patient's home site. Therefore, broad conclusions about equivalency of care must be interpreted in the context of the intervention being delivered (and whether it is feasible in most practices) as well as the outcome of interest, all of which tend to be variable across telemedicine literature. A more recent narrative review on the topic of asthma care via telemedicine looked at a variety of interventions ranging from telephone-only follow-ups to the Remote Presence Solution described above, and concluded that data remain limited for clinical outcomes on this condition.43 In addition, many studies in this review that used a telemedicine intervention combined it with a school-based care program, making it difficult to conclude what effects (if any) might be due to the telemedicine itself.
Similar challenges in drawing firm conclusions have been noted in a recent umbrella review of systematic reviews regarding telemedicine interventions for diabetes care, cholesterol, and hypertension.44 Although the investigators concluded that telemedicine may improve outcomes for patients with diabetes and there are trends favoring certain subgroups in other conditions, the overall quality of the current evidence is low or very low because of potential bias in study design, heterogeneity in subgroups, imprecision of results or small effect sizes (due to small sample sizes), publication bias, and underreporting of relevant information, such as the treatment of dropout or missing data. Larger, more robust studies that address specific questions on clinical outcomes of telemedicine-supported chronic disease care as pandemic-era data come to publication are eagerly awaited.
Impacts on systems and resource utilization
Using telemedicine for select cases of both acute and chronic disease management may decrease the need for some routine face-to-face visits. In addition, there is interest in whether early triage and intervention for patient concerns via telemedicine could decrease face-to-face visits in urgent care and ED settings. A study by Reed and colleagues36 showed that over a very large sample of appointments (more than one million visits for all types of complaints performed via telephone, video, or office visits), short-term hospital and ED utilization did not differ between patients who used telemedicine and patients who scheduled in-person visits. This preliminarily suggests that when patients are free to choose their own mode of care within a clinical context that has consistent physicians and ready follow-up care, telemedicine may be a reasonable initial alternative to in-person care and may not lead to increased emergency care. Further research in the same setting as the Reed study showed that e-visits for patients who met specific, low-risk criteria for one of five different complaints (eg, URI, emergency contraception, conjunctivitis, pharyngitis, and urinary tract infections) had overall low rates of in-office follow-up (about 13.5% of the entire cohort), and less than 1% used emergency services.45 The e-visits took about two to three minutes of clinician time, suggesting this could be a very cost-effective and efficient intervention for common low-acuity complaints.
Even asynchronous patient-physician communication could be a timely way to reduce the need for more intensive care. Patient access to physician-patient messaging through a secure portal may not decrease face-to-face visits overall,46 , 47 but for those with multiple chronic conditions (in this study defined as diabetes plus another chronic condition, such as asthma, coronary artery disease, congestive heart failure, or hypertension), it can decrease ED and hospital utilization.47 This may be particularly significant during times when hospital care is severely overburdened, such as flu seasons, pandemics, or natural disasters. However, increased care burden may fall on outpatient clinicians handling the message volume and could contribute to fatigue or burnout over time if not addressed.
A key health outcome for telemedicine visits that has not been well studied is the diagnostic accuracy of telemedicine evaluation compared with standard care, and the association of delayed diagnosis and adverse health outcomes with each modality. Delayed diagnosis is a frequent allegation in malpractice claims, and to date, the medical-legal footprint of telemedicine has been very small.48 The medical-legal implications of telemedicine are limited at the time of this publication and will certainly be an area of future research.
Summary and future directions
As we prepare to enter a future with widespread telemedicine, we should consider what will be gained and what may be lost. The benefits of telemedicine after its pandemic renaissance are apparent now more than ever: convenient and timely access to care that overcomes geographic barriers, reduced burden on medical infrastructure (e.g., traffic, facilities’ wear, perhaps reduced staff needs), and minimal exposure to infectious diseases for all participants. However, concerns still exist that something may be lost if telemedicine becomes standard practice for all. Many telehealth investigators and enthusiasts assert that telemedicine should play a role as an adjunct rather than a replacement for in-person care.48 This is certainly the most likely scenario, because pandemic restrictions have lessened at the time of authorship of this article, and it remains unclear whether payment parity and other legislation supporting telemedicine care will remain in effect long term. It seems clear thattelemedicine is likely to remain pervasive in some fashion, and this author’s review of telemedicine both prepandemic and during the pandemic shows that it is widely agreeable to those who use it and it can stand alongside standard care for a variety of acute and chronic medical conditions, with the opportunity for more research ready to be explored in the future.
Going forward, many questions remain ripe for study on what makes for an effective telemedicine encounter. The relative importance of a physical examination in general and for what types of concerns will need to be considered, as well as to what extent patient-provided vital signs and physician-directed virtual examinations can fill this need. Beyond the physical examination, it is not clear whether patient-clinician relationships, rapport, and trust will suffer through the loss of nonverbal communication and therapeutic touch. Technology challenges from all directions, including poor reception, blurry screen resolution, or choppy Internet connections, may impair the telemedicine rapport. Questions on the impact of telemedicine to specific aspects of the physician-patient relationship deserve further study, as patient adherence and outcomes are known to be heavily influenced by physician communication techniques.49, 50, 51, 52 Perhaps tried-and-true patient communication techniques that have been successfully used in traditional practice to improve patient care53 can translate relatively easily into telemedicine care and show similar benefits.
It will be to everyone’s benefit to understand how to participate in telemedicine care most effectively,as telemedicine is projected to remain more widely available to Americans moving forward. It is time for all of us to become adept at the twenty-first-century house call.
Clinics care points
-
•
Telemedicine use between physicians and patients of all types has greatly expanded with the arrival of the COVID-19 pandemic. It is predicted to remain more prevalent in future US health care.
-
•
Patients who are older, are non-white, live in a rural area, or are from a lower socioeconomic group continue to use telemedicine at lower rates. Some of this inequity is due to inconsistent technology access, but more research is needed in this area.
-
•
Telemedicine is generally well liked by patients who use it, both before and during the pandemic.
-
•
Research supports a role for telemedicine in both acute care and chronic disease management and suggests that it is noninferior to in-person care for health outcomes in certain conditions, such as uncomplicated upper respiratory tract infection, urinary tract infection, low-back pain, initial dermatologic concerns (with the help of high-definition photography), and chronic disease management (with the strongest evidence to date being for diabetes care). Telemedicine may also decrease, or at least not add to, short-term hospital and emergency department utilization.
-
•
Systems-level interventions are needed to solidify telemedicine as a fixture in American health care and ensure more equitable access to it, including more universal service and payment parity, expanded broadband and digital technology access to patients and practices, and the allowance of audio-only telemedicine visits as an acceptable alternative to video.
-
•
Clinicians have cited lack of training as a barrier to practicing telemedicine, and more robust training is needed at the undergraduate and graduate medical education levels. The Association of American Medical Colleges has released telehealth competencies to guide these efforts, and the Society of Teachers of Family Medicine has spearheaded the development of a national telemedicine curriculum.
-
•
Areas of future study should include the development of telemedicine best practices for common acute and chronic conditions and examination of how they affect patient-oriented health outcomes, assessment of physician communication techniques that are suited to remote and audio-only care, study of the economic impact of providing telemedicine care either as adjunct to or in place of in-person care, and the provision of telemedicine access to less represented groups.
Acknowledgments
Disclosure
None.
References
- 1.Sood S., Mbarika V., Jugoo S., et al. What Is Telemedicine? A Collection of 104 Peer-Reviewed Perspectives and Theoretical Underpinnings. Telemed J E Health. 2007;13(5):573–590. doi: 10.1089/tmj.2006.0073. [DOI] [PubMed] [Google Scholar]
- 2.Weigel G., Ramaswamy A., May 11 M.F.P. Opportunities and Barriers for Telemedicine in the U.S. During the COVID-19 Emergency and Beyond. KFF. Published May 11, 2020. 2020. https://www.kff.org/womens-health-policy/issue-brief/opportunities-and-barriers-for-telemedicine-in-the-u-s-during-the-covid-19-emergency-and-beyond/ Available at: Accessed December 21, 2021.
- 3.Telehealth Is Here to Stay—In the United States and in Germany. AICGS. https://www.aicgs.org/2020/06/telehealth-is-here-to-stay-in-the-united-states-and-in-germany/ Available at: Accessed December 7, 2021.
- 4.Hyder M.A., Razzak J. Telemedicine in the United States: An Introduction for Students and Residents. J Med Internet Res. 2020;22(11):e20839. doi: 10.2196/20839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kane C.K., Gillis K. The Use Of Telemedicine By Physicians: Still The Exception Rather Than The Rule. Health Aff (Millwood) 2018;37(12):1923–1930. doi: 10.1377/hlthaff.2018.05077. [DOI] [PubMed] [Google Scholar]
- 6.Huilgol Y.S., Miron-Shatz T., Joshi A.U., et al. Hospital Telehealth Adoption Increased in 2014 and 2015 and Was Influenced by Population, Hospital, and Policy Characteristics. Telemed J E Health. 2020;26(4):455–461. doi: 10.1089/tmj.2019.0029. [DOI] [PubMed] [Google Scholar]
- 7.Ranganathan C., Balaji S. Key Factors Affecting the Adoption of Telemedicine by Ambulatory Clinics: Insights from a Statewide Survey. Telemed J E Health. 2020;26(2):218–225. doi: 10.1089/tmj.2018.0114. [DOI] [PubMed] [Google Scholar]
- 8.Polinski J.M., Barker T., Gagliano N., et al. Patients’ Satisfaction with and Preference for Telehealth Visits. J Gen Intern Med. 2016;31(3):269–275. doi: 10.1007/s11606-015-3489-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kruse C.S., Krowski N., Rodriguez B., et al. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pflugeisen B.M., Mou J. Patient Satisfaction with Virtual Obstetric Care. Matern Child Health J. 2017;21(7):1544–1551. doi: 10.1007/s10995-017-2284-1. [DOI] [PubMed] [Google Scholar]
- 11.Karen Donelan S., Esteban A., Barreto M.A., et al. Patient and Clinician Experiences With Telehealth for Patient Follow-up Care. Published online January 14, 2019. https://www.ajmc.com/view/patient-and-clinician-experiences-with-telehealth-for-patient-followup-care Available at: Accessed December 9, 2021. [PubMed]
- 12.Orlando J.F., Beard M., Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS One. 2019;14(8):e0221848. doi: 10.1371/journal.pone.0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hsu H., Greenwald P.W., Clark S., et al. Telemedicine Evaluations for Low-Acuity Patients Presenting to the Emergency Department: Implications for Safety and Patient Satisfaction. Telemed J E Health. 2020;26(8):1010–1015. doi: 10.1089/tmj.2019.0193. [DOI] [PubMed] [Google Scholar]
- 14.Haluza D., Naszay M., Stockinger A., et al. Prevailing Opinions on Connected Health in Austria: Results from an Online Survey. Int J Environ Res Public Health. 2016;13(8):813. doi: 10.3390/ijerph13080813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Klink K., Coffman M., Moore M., et al. Family Physician and Telehealth: Findings from a National Survey. Robert Graham Center; 2015. https://www.graham-center.org/content/dam/rgc/documents/publications-reports/reports/RGC%202015%20Telehealth%20Report.pdf Available at: Accessed February 4, 2022.
- 16.Weiner J.P., Bandeian S., Hatef E., et al. In-Person and Telehealth Ambulatory Contacts and Costs in a Large US Insured Cohort Before and During the COVID-19 Pandemic. JAMA Netw Open. 2021;4(3):e212618. doi: 10.1001/jamanetworkopen.2021.2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Doximity. 2020 State of Telemedicine Report: Examining Patient Perspectives and Physician Adoption of Telemedicine Since the COVID-19 Pandemic. Published online September 2020. https://c8y.doxcdn.com/image/upload/Press%20Blog/Research%20Reports/2020-state-telemedicine-report.pdf Available at: Accessed December 10, 2021.
- 18.Patel S.Y., Mehrotra A., Huskamp H.A., et al. Variation In Telemedicine Use And Outpatient Care During The COVID-19 Pandemic In The United States. Health Aff (Millwood) 2021;40(2):349–358. doi: 10.1377/hlthaff.2020.01786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.COVID-19 financial impact on physician practices | American Medical Association. https://www.ama-assn.org/practice-management/sustainability/covid-19-financial-impact-physician-practices Available at: Accessed February 2, 2022.
- 20.FAIRHealth Monthly Telehealth Regional Tracker. fairhealth.org. http://www.fairhealth.org/states-by-the-numbers/telehealth Available at: Accessed December 7, 2021.
- 21.Drake C., Lian T., Cameron B., et al. Understanding Telemedicine’s “New Normal”: Variations in Telemedicine Use by Specialty Line and Patient Demographics. Telemed J E Health. 2021 doi: 10.1089/tmj.2021.0041. tmj.2021.0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.SHADAC analysis of the American Community Survey (ACS) Public Use Microdata Sample (PUMS) files. State Health Compare, SHADAC, University of Minnesota. statehealthcompare.shadac.org Available at: Accessed December 21, 2021.
- 23.Eberly L.A., Kallan M.J., Julien H.M., et al. Patient Characteristics Associated With Telemedicine Access for Primary and Specialty Ambulatory Care During the COVID-19 Pandemic. JAMA Netw Open. 2020;3(12):e2031640. doi: 10.1001/jamanetworkopen.2020.31640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gilson S.F., Umscheid C.A., Laiteerapong N., et al. Growth of Ambulatory Virtual Visits and Differential Use by Patient Sociodemographics at One Urban Academic Medical Center During the COVID-19 Pandemic: Retrospective Analysis. JMIR Med Inform. 2020;8(12):e24544. doi: 10.2196/24544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hsiao V., Chandereng T., Lankton R.L., et al. Disparities in Telemedicine Access: A Cross-Sectional Study of a Newly Established Infrastructure during the COVID-19 Pandemic. Appl Clin Inform. 2021;12(3):445–458. doi: 10.1055/s-0041-1730026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodriguez J.A., Saadi A., Schwamm L.H., et al. Disparities In Telehealth Use Among California Patients With Limited English Proficiency: Study examines disparities in telehealth use among California patients with limited English proficiency. Health Aff (Millwood) 2021;40(3):487–495. doi: 10.1377/hlthaff.2020.00823. [DOI] [PubMed] [Google Scholar]
- 27.Research Shows Patients and Clinicians Rated Telemedicine Care Positively During COVID-19 Pandemic - Penn Medicine. https://www.pennmedicine.org/news/news-releases/2020/june/patients-and-clinicians-rated-telemedicine-care-positively-during-covid Available at: Accessed December 14, 2021.
- 28.Holtz B.E. Patients Perceptions of Telemedicine Visits Before and After the Coronavirus Disease 2019 Pandemic. Telemed J E Health. 2021;27(1):107–112. doi: 10.1089/tmj.2020.0168. [DOI] [PubMed] [Google Scholar]
- 29.Kyle M.A., Blendon R.J., Findling M.G., et al. Telehealth use and Satisfaction among U.S. Households: Results of a National Survey. J Patient Exp. 2021;8 doi: 10.1177/23743735211052737. 23743735211052736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bashshur R.L., Howell J.D., Krupinski E.A., et al. The Empirical Foundations of Telemedicine Interventions in Primary Care. Telemed J E Health. 2016;22(5):342–375. doi: 10.1089/tmj.2016.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chaudhry R., Stroebel R., McLeod T., et al. Nurse-based telephone protocol versus usual care for management of URI and acute sinusitis: a controlled trial. Manag Care Interf. 2006;19(8):26–31. [PubMed] [Google Scholar]
- 32.Stroebel R., McLeod T., Kitsteiner J., et al. Clinical outcomes of patients with upper respiratory tract infections and acute sinusitis managed with a Web-based protocol in primary care practice. Manag Care Interf. 2007;20(6):17–22. [PubMed] [Google Scholar]
- 33.Uscher-Pines L., Mulcahy A., Cowling D., et al. Access and Quality of Care in Direct-to-Consumer Telemedicine. Telemed J E Health. 2016;22(4):282–287. doi: 10.1089/tmj.2015.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Foster C.B., Martinez K.A., Sabella C., et al. Patient Satisfaction and Antibiotic Prescribing for Respiratory Infections by Telemedicine. Pediatrics. 2019;144(3):e20190844. doi: 10.1542/peds.2019-0844. [DOI] [PubMed] [Google Scholar]
- 35.Ray K.N., Shi Z., Gidengil C.A., et al. Antibiotic Prescribing During Pediatric Direct-to-Consumer Telemedicine Visits. Pediatrics. 2019;143(5):e20182491. doi: 10.1542/peds.2018-2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reed M., Huang J., Graetz I., et al. Treatment and Follow-up Care Associated With Patient-Scheduled Primary Care Telemedicine and In-Person Visits in a Large Integrated Health System. JAMA Netw Open. 2021;4(11):e2132793. doi: 10.1001/jamanetworkopen.2021.32793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trettel A., Eissing L., Augustin M. Telemedicine in dermatology: findings and experiences worldwide - a systematic literature review. J Eur Acad Dermatol Venereol. 2018;32(2):215–224. doi: 10.1111/jdv.14341. [DOI] [PubMed] [Google Scholar]
- 38.Niznik J.D., He H., Kane-Gill S.L. Impact of clinical pharmacist services delivered via telemedicine in the outpatient or ambulatory care setting: A systematic review. Res Soc Adm Pharm. 2018;14(8):707–717. doi: 10.1016/j.sapharm.2017.10.011. [DOI] [PubMed] [Google Scholar]
- 39.Thomas A.M., Baker J.W., Hoffmann T.J., et al. Clinical pharmacy specialists providing consistent comprehensive medication management with increased efficiency through telemedicine during the COVID19 pandemic. J Am Coll Clin Pharm. 2021;4(8):934–938. doi: 10.1002/jac5.1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Appel L.J., Clark J.M., Yeh H.C., et al. Comparative Effectiveness of Weight-Loss Interventions in Clinical Practice. N Engl J Med. 2011;365(21):1959–1968. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kroenke K., Krebs E.E., Wu J., et al. Telecare Collaborative Management of Chronic Pain in Primary Care: A Randomized Clinical Trial. JAMA. 2014;312(3):240–248. doi: 10.1001/jama.2014.7689. [DOI] [PubMed] [Google Scholar]
- 42.Portnoy J.M., Waller M., Lurgio S.D., et al. Telemedicine is as effective as in-person visits for patients with asthma. Ann Allergy Asthma Immunol. 2016;117(3):241–245. doi: 10.1016/j.anai.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 43.Davies B., Kenia P., Nagakumar P., et al. Paediatric and adolescent asthma: A narrative review of telemedicine and emerging technologies for the post-COVID-19 era. Clin Exp Allergy. 2021;51(3):393–401. doi: 10.1111/cea.13836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Timpel P., Oswald S., Schwarz P.E.H., et al. Mapping the evidence on the effectiveness of telemedicine interventions in diabetes, dyslipidemia, and hypertension: an umbrella review of systematic reviews and meta-analyses. J Med Internet Res. 2020;22(3):e16791. doi: 10.2196/16791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bhargava R., Gayre G., Huang J., et al. Patient e-Visit Use and Outcomes for Common Symptoms in an Integrated Health Care Delivery System. JAMA Netw Open. 2021;4(3):e212174. doi: 10.1001/jamanetworkopen.2021.2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.North F., Crane S.J., Chaudhry R., et al. Impact of Patient Portal Secure Messages and Electronic Visits on Adult Primary Care Office Visits. Telemed J E Health. 2014;20(3):192–198. doi: 10.1089/tmj.2013.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reed M.E., Huang J., Brand R.J., et al. Patients with complex chronic conditions: Health care use and clinical events associated with access to a patient portal. PLoS One. 2019;14(6):e0217636. doi: 10.1371/journal.pone.0217636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.The Doctors Company Your Patient Is Logging On Now: The Risks and Benefits of Telehealth in the Future of Healthcare. The Doctors Company TDC Group. https://www.thedoctors.com/articles/your-patient-is-logging-on-now--the-risks-and-benefits-of-telehealth-in-the-future-of-healthcare/ Available at: Accessed December 21, 2021.
- 49.Stewart M.A. Effective physician-patient communication and health outcomes: a review. CMAJ Can Med Assoc J. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 50.Levinson W., Roter D.L., Mullooly J.P., et al. Physician-patient communication: The relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277(7):553–559. doi: 10.1001/jama.277.7.553. [DOI] [PubMed] [Google Scholar]
- 51.Haskard Zolnierek K.B., DiMatteo M.R. Physician Communication and Patient Adherence to Treatment: A Meta-analysis. Med Care. 2009;47(8):826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Strumann C., Steinhaeuser J., Emcke T., et al. Communication training and the prescribing pattern of antibiotic prescription in primary health care. PLoS One. 2020;15(5):e0233345. doi: 10.1371/journal.pone.0233345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stein T. A Decade of Experience with a Multiday Residential Communication Skills Intensive: Has the Outcome Been Worth the Investment? Perm J. 2007;11(4):30–40. doi: 10.7812/tpp/07-069. [DOI] [PMC free article] [PubMed] [Google Scholar]