Abstract
Quality care requires collaborative communication, information exchange, and decision-making between patients and providers. Complete and accurate data about patients and from patients are especially important as high volumes of data are used to build clinical decision support tools and inform precision medicine initiatives. However, systematically missing data can bias these tools and threaten their effectiveness. Data completeness relies in many ways on patients being comfortable disclosing information to their providers without prohibitive concerns about security or privacy. Patients are likely to withhold information in the context of low trust relationships with providers, but it is unknown how experiences of discrimination in the healthcare system also relate to non-disclosure. In this study, we assess the relationship between withholding information from providers, experiences of discrimination, and multiple types of patient trust. Using a nationally representative sample of US adults (n = 2,029), weighted logistic regression modeling indicated a statistically significant relationship between experiences of discrimination and withholding information from providers (OR 3.7; CI [2.6–5.2], p < .001). Low trust in provider disclosure of conflicts of interest and low trust in providers' responsible use of health information were also positively associated with non-disclosure. We further analyzed the relationship between non-disclosure and the five most common types of discrimination (e.g., discrimination based on race, education/income, weight, gender, and age). We observed that all five types were statistically significantly associated with non-disclosure (p < .05). These results suggest that experiences of discrimination and specific types of low trust have a meaningful association with a patient's willingness to share information with their provider, with important implications for the quality of data available for medical decision-making and care. Because incomplete information can contribute to lower quality care, especially in the context of data-driven decision-making, patients experiencing discrimination may be further disadvantaged and harmed by systematic data missingness in their records.
Highlights
-
•
Experiences of discrimination and some types of low trust are significantly related to non-disclosure.
-
•
This is observed for all five most common types of discrimination (based on race, education/income, weight, gender, age).
-
•
Incomplete data can result in lower quality data-driven care, entrenching inequity.
-
•
Patients experiencing discrimination may be further harmed by systematic data missingness in their records.
1. Introduction
1.1. Data quality connection to care quality
Quality care requires collaborative communication, information exchange, and shared decision-making between patients and providers (Blanch-Hartigan et al., 2016; Bugge, Entwistle, & Watt, 2006; Finney Rutten et al., 2015, 2016). Lack of information sharing can result in misunderstandings by both patients and providers, impacting patients' experiences of health care and views about treatment (Entwistle, Williams, Skea, MacLennan, & Bhattacharya, 2006; Finney Rutten et al., 2015, 2016). It can also negatively impact the quality of data in a patient's medical record, which has consequences for future medical decision-making (Gianfrancesco, Tamang, Yazdany, & Schmajuk, 2018; Ng, Ye, Ward, Haffer, & Hudson Scholle, 2017). Data-driven approaches to care are built on high volumes of patient data. Precision medicine, for example, often combines genetic, clinical, environmental, and patient-reported data in order to tailor treatment to individual patients (Collins & Varmus, 2015; Ginsburg & Phillips, 2018). Clinical decision support (CDS) tools also draw on patient data to present relevant information to a provider at the point of care (Sutton et al., 2020). These tools and approaches rely directly on the quality and completeness of data on which they are built or trained.
Prior literature, both within and external to healthcare, emphasizes the importance of complete data for analysis and data-driven technologies to be valid and effective (Agarwala et al., 2018; Altman & Bland, 2007; Ngiam & Khor, 2019; Ross, Breskin, & Westreich, 2020; Wang & Preininger, 2019; Weiskopf, Hripcsak, Swaminathan, & Weng, 2013). Patient non-disclosure is especially important and consequential in this context because systematic data missingness across patient populations may result in biased outcomes (Barda et al., 2021). If this missingness reflects particular social positions, vulnerabilities, oppressive systems, and inequities, those inequities can be embedded in the data-driven tools being built and implemented throughout the healthcare system (Rajkomar, Hardt, Howell, Corrado, & Chin, 2018). Should data quality and completeness differ systematically according to experiences of discrimination, it could represent another mechanism through which social inequities are reproduced in health and healthcare.
1.2. Trust, communication, and sharing information in clinical care
Effective and complete information exchange does not always occur between patients and providers. There are a variety of reasons for this. Previous research has identified that patient-provider communication is positively related to patient trust in providers (Fiscella et al., 2004). Trust in providers is conceptualized as patient expectations that providers will meet their responsibilities to the patient (Mechanic, 1998), and comprises multiple dimensions aligning with different tasks or situations in which the patient is vulnerable to the physician (Campos-Castillo & Anthony, 2019; Hall et al., 2002). Patient trust is vital in decisions about disclosing personal information to a provider (Mechanic & Meyer, 2000; Ostertag, Wright, Broadhead, & Altice, 2006; Thom, Hall, & Pawlson, 2004; Verhaeghe & Bracke, 2011). Patients are more likely to withhold information when they are concerned about specific aspects of provider behavior, their privacy, and who will have access to their information (Campos-Castillo & Anthony, 2015). There is variation in the ways dimensions of trust relate to various patient experiences and perceptions. One specific dimension of trust, in physician confidentiality, has been shown to be associated with patient disclosure, while other dimensions of trust (e.g., in physician competence or fidelity) were not (Iott, Campos-Castillo, & Anthony, 2020).
The questions providers do and do not ask (Hahn, 2009; Horne, 2006) and the ways they interact with patients (Bugge et al., 2006) are important to patient disclosure, as these aspects of communication may discourage patients from disclosing information (Stevenson, Cox, Britten, & Dundar, 2004). There is a considerable body of evidence of inequity in provider decision-making and communication styles by patient race, gender, and stigmatized conditions (LaVeist, Nuru-Jeter, & Jones, 2003; Mitchell & Perry, 2020; N.; Trivedi, Moser, Breslau, & Chou, 2021; van Ryn & Fu, 2003). Thus, patient information sharing may be particularly sensitive to experiences of discrimination in the healthcare system.
1.3. Experiences of discrimination in the healthcare system impact care relationships
Patient non-disclosure has often been conceptualized as a reflection of patients' desire to conceal certain health behaviors or potentially stigmatizing information like smoking or tobacco use, sexual behavior, or drug use because of concerns about how providers will treat or discriminate against them (Levy et al., 2018; Stablein, Hall, Pervis, & Anthony, 2015). As described above, non-disclosure has also been analyzed in relation to concerns about privacy, security, and trust in providers’ confidentiality related to stigma (Agaku, Adisa, Ayo-Yusuf, & Connolly, 2014; Campos-Castillo & Anthony, 2015, 2019). Patient withholding of information is thus often discussed in relation to concerns about the provider-patient relationship or clinical context. Recognizing that patient-provider relationships are situated within larger healthcare systems and social structures, it is also necessary to account for experiences of discrimination.
Here, discrimination refers specifically to discriminatory interpersonal interactions that occur in the larger context of systemic inequities (Jones, 2000; Krieger, 2000). For example, interpersonal racism is directly perceived racist treatment, occurring in the context of structural racism that confers advantages to people considered White while oppressing other racialized groups (Alang et al., 2021; Bonilla-Silva, 1997; Jones, 2000; Williams, Lawrence, & Davis, 2019; Williams & Mohammed, 2009). Similarly, an individual may directly experience discrimination based on their sexuality as a particular instance that reflects the larger social systems that grant advantages to heterosexual people (Friedman et al., 2014; Sabinet al., 2015). While these interpersonal discriminatory acts reflect systems of inequity, they do not capture the full effect of such systems. They do, however, provide vital information about patient experiences with the healthcare system and their providers that may impact trust (Armstrong et al., 2013) and disclosure.
Interpersonal discrimination in the healthcare system takes many forms, including disrespect, poor quality communication, devaluation, and differential clinical treatment that affects large groups of patients, reflecting different intersecting systems of inequity (A. N. Trivedi & Ayanian, 2006; Nong, Raj, Creary, Kardia, & Platt, 2020; Krieger, 2014; Stepanikova & Oates, 2017; LaVeist et al., 2003). Not only are patient trust and experiences of discrimination related, but like trust (Martin, Roter, Beach, Carson, & Cooper, 2013), discriminatory experiences are associated with diminished communication with providers (Dovidio et al., 2008; Mitchell & Perry, 2020; Tajeu et al., 2015; Williams, Lawrence, & Davis, 2019) as well as under-utilization of health services and disparities in specific health outcomes (Ben, Cormack, Harris, & Paradies, 2017; LaVeist, Isaac, & Williams, 2009).
Previous studies, particularly of ethnoracial differences in patient trust, examine how discrimination or experiences of unequal treatment may influence levels or dimensions of trust. Although findings vary (Armstrong et al., 2006; Boulware, Cooper, Ratner, LaVeist, & Powe, 2003; LaVeist, Nickerson, & Bowie, 2000; Sewell, 2015), experiences of discrimination are generally associated with lower trust. Accounting for discrimination provides additional insight into patient perceptions and trust (Armstrong et al., 2013). However, while many studies discuss issues of trust and discrimination, we are not aware of any that account for these factors together by analyzing multiple dimensions of trust and experiences of discrimination in relation to non-disclosure. Here we focus on whether experiences of discrimination and dimensions of patient trust in providers are associated with non-disclosure. We us both “withholding” and “non-disclosure” to refer to patients keeping information from their providers. We also place non-disclosure in the context of patient-provider relationships where provider behavior and the healthcare system shape a patient's experience and comfort sharing their information.
1.4. Objectives
We examine non-disclosure as an important factor in communication, data sharing, and quality of care relevant to health inequity (Levy et al., 2018). We draw from conceptual work on provider behavior and decision-making to identify two specific aspects of the patient experience as examples of inequity in healthcare (van Ryn et al., 2011). Specifically, we identify how experiences of discrimination and patient trust relate to a particular patient behavior in encounters with their providers (non-disclosure). We ask: 1) what is the relationship between experiences of discrimination, patient trust in providers, and withholding information? and 2) do different types of discrimination relate to withholding information differently?
2. Methods
2.1. Sample
In May 2019 we fielded an original survey with a National Opinion Research Center (NORC) probability-based, nationally representative sample of US adults at least 21 years of age. This included oversamples of Black respondents, Hispanic respondents, and respondents earning below 200% of the federal poverty level annually. The survey was pre-tested, piloted, and evaluated through cognitive interviews (n = 17) with adults who could speak English (Nong et al., 2020). A total of 2,157 respondents completed the survey for a 66% response rate. NORC calculated poststratification survey weights based on demographics from the Current Population Survey (age, sex, education, race/ethnicity, housing tenure, telephone status, Census division) and for nonresponse.
2.2. Measures
The outcome of withholding information from providers was measured by responses to the question: “Have you ever kept information from your healthcare provider because you were concerned about privacy or security?”. This item is adapted from the Health Information National Trends Survey (HINTS) and has been used in previous work (Campos-Castillo & Anthony, 2015). Response options were yes or no.
The key independent variable, experiencing discrimination in the healthcare system, was measured using two questions adapted from previously validated survey measures (Krieger, Smith, Naishadham, Hartman, & Barbeau, 2005; Williams, Yan, Jackson, & Anderson, 1997). Respondents indicated whether they had experienced discrimination or been hassled or made to feel inferior while seeking medical care. They also indicated what they thought was the main reason for the discrimination they experienced (Nong et al., 2020). The full text of the survey item is included in the Supplementary Material.
Respondents reported their trust in providers using four measures on a four-point scale indicating how true each statement was for them (1 = not true, 4 = very true). These statements included: 1) Healthcare providers care most about making money for themselves, 2) Healthcare providers disclose their conflicts of interest, 3) I trust healthcare providers to use my health information responsibly, and 4) All things considered, healthcare providers in this country can be trusted. These statements reflect types of trust identified as important to patient-provider relationships, like confidentiality and honesty (Campos-Castillo & Anthony, 2019; Hall et al., 2002; Iott et al., 2020). Each statement about trust in providers was coded for low trust. The value of the indicator for each type of trust was equal to one when respondents indicated low trust and equal to zero otherwise.
Respondents self-reported demographic information including age, binary sex, race/ethnicity, education, and annual household income. Respondents reported whether they had health insurance (yes or no) and their health status (on a 5-point scale from poor to excellent). Respondents also reported when their last visit to a healthcare provider happened (Approximately when was the last time you saw a healthcare provider?). General satisfaction with healthcare was reported on a 4-point scale from not true to very true (In general, I am satisfied with the treatment I receive from my healthcare providers). Respondents also reported whether they had a regular healthcare provider (What kind of healthcare provider do you typically go to if you are sick or need advice about your health?).
2.3. Data analysis
We analyzed the responses of 2,029 respondents with complete data. We conducted bivariable and multivariable logistic regressions to analyze the relationships between discrimination, trust, and withholding information from providers. Specifically, we constructed two weighted multivariable logistic regression models. Covariates included age, sex, race/ethnicity, education, income, self-reported health status, health insurance status, having a regular healthcare provider, high satisfaction with care, and most recent visit to a healthcare provider. In the first model, we included measures of trust in providers and experiences of discrimination generally. In the second model, we broke out the discrimination measure into multiple specific types of discrimination to identify whether they are differentially related to the outcome variable. We defined statistical significance as p < .05. All analyses were conducted using STATA, version 14 (StataCorp).
3. Ethical considerations
This survey was approved by the Institutional Review Board at the University of Michigan. Respondents were compensated for their participation according to NORC's standard remuneration for AmeriSpeak Panel surveys.
4. Results
Demographic characteristics of the sample are included in Table 1, Table 2. Using weighted percentages, 27.5% of respondents reported ever withholding information from healthcare providers and 19.1% reported experiencing discrimination while seeking medical care. Low trust in providers' disclosure of conflicts of interest (37.5%) was most common. Low trust in providers’ financial motivations (17.8%) and responsible use of health information (14.1%) were less frequently reported. Low general trust in providers was least common (12.3%).
Table 1.
Descriptive statistics (n = 2,029).
| Measure | Unweighted n | Weighted % |
|---|---|---|
| Sex | ||
| Female | 1036 | 48.2 |
| Male | 993 | 51.8 |
| Age | ||
| 18-29 | 242 | 16.3 |
| 30-44 | 599 | 26.0 |
| 45-59 | 526 | 27.5 |
| 60+ | 662 | 30.2 |
| Race/ethnicity | ||
| White | 1180 | 63.8 |
| Black | 321 | 11.9 |
| Hispanic | 396 | 15.8 |
| Asian | 48 | 3.8 |
| Other | 84 | 4.7 |
| Education | ||
| High school or less | 440 | 38.8 |
| Some college | 940 | 27.6 |
| BA or above | 649 | 33.6 |
| Annual household income | ||
| <$50,000 | 968 | 56.4 |
| At least $50,000 | 1061 | 43.6 |
| Health insurance coverage | ||
| Yes | 1797 | 88.1 |
| No | 232 | 11.9 |
| Has regular healthcare provider | ||
| Yes | 1629 | 78.1 |
| No | 400 | 21.9 |
| Self-reported health | ||
| Poor to good | 1402 | 67.6 |
| Very good to excellent | 627 | 32.4 |
| Last healthcare visit | ||
| Within past year | 1729 | 84.3 |
| Within past 2 years | 166 | 8.3 |
| Within past 5 years | 89 | 4.9 |
Weights calculated according to the Current Population Survey (age, sex, education, race/ethnicity, housing tenure, telephone status, Census division) and for nonresponse.
Table 2.
Descriptive statistics for discrimination and trust (n = 2,029).
| Measure | Unweighted n | Weighted % |
|---|---|---|
| Experienced discrimination in the healthcare system | ||
| Yes | 425 | 19.1 |
| No | 1604 | 81.0 |
| Ever withheld information from a provider | ||
| Yes | 617 | 27.5 |
| No | 1519 | 72.5 |
| Low trust in providers' financial motivations | ||
| Yes | 357 | 17.8 |
| No | 1672 | 82.2 |
| Low trust that providers disclose conflicts of interest | ||
| Yes | 774 | 37.5 |
| No | 1255 | 62.5 |
| Low trust that providers use health information responsibly | ||
| Yes | 299 | 14.1 |
| No | 1730 | 85.9 |
| Low trust in providers generally | ||
| Yes | 258 | 12.3 |
| No | 1771 | 87.7 |
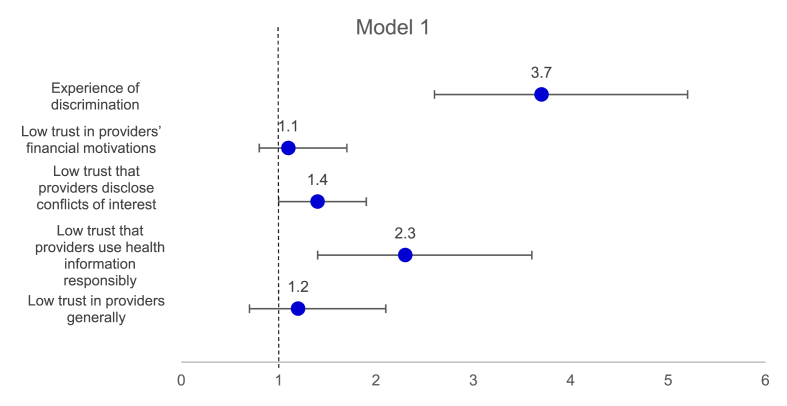
In the weighted multivariable logistic regression (Model 1, shown in Fig. 1), experiences of discrimination in the healthcare system were most strongly associated with withholding information from providers (OR 3.7; CI [2.6–5.2], p < .001). Those reporting low trust in providers using health information responsibly (OR 2.3 [CI 1.4–3.6], p = .001) and low trust in providers disclosing conflicts of interest (OR 1.4 [CI 1.0–1.9], p = .03) were also more likely to withhold information from providers. Respondents who were very satisfied with their care were less likely to withhold information than those who were dissatisfied (OR 0.6 [CI 0.4–0.8], p = .001).
Fig. 1.
Odds ratios [95% CI] from weighted multivariable logistic regression of withholding information from providers on experiences of discrimination and low trust in providers, (n = 2,029).
Source: Lifecycle of Data NORC Survey 2019. Covariates include age, sex, race/ethnicity, education, income, self-reported health status, health insurance status, having a regular healthcare provider, high satisfaction with care, and most recent visit to a healthcare provider. For the table of full results, see Supplementary Table 1.
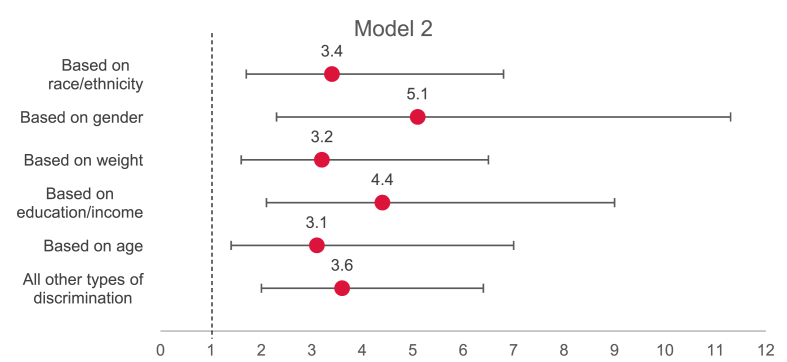
In order to identify potential differences according to the type of discrimination, Model 2 includes specific measures of the type of discrimination reported rather than the binary measure of whether or not a respondent reported discrimination. In addition to the same covariates as Model 1, Model 2 includes a variable for each of the five most common types of discrimination reported by respondents (in descending order of frequency: racial discrimination, gender-based discrimination, discrimination based on education or income, weight-based discrimination, and discrimination based on age) and a sixth category that included all other types of discrimination. Respondents who did not report an experience of discrimination are the reference group. Each type of discrimination was individually positively associated with withholding information from providers (Fig. 2).
Fig. 2.
Odds ratios [95% CI] from weighted multivariable logistic regression of withholding information from providers on five most common experiences of discrimination (n = 2,029).
Source: Lifecycle of Data NORC Survey 2019. Covariates include age, sex, race/ethnicity, education, income, self-reported health status, health insurance status, having a regular healthcare provider, high satisfaction with care, and most recent visit to a healthcare provider. For the table of full results, see Supplementary Table 2.
In sensitivity analysis, the sample was restricted to respondents who reported an experience of discrimination (n = 457). A modified version of Model 2 was constructed to include the most common types of discrimination reported, with the sixth category including all other types of discrimination as the reference group. The modified multivariable model was run on this restricted sample to identify whether there were differences in withholding information among respondents reporting discrimination according to the type of discrimination. There were no statistically significant differences between types of discrimination in relation to withholding information from providers. (See Supplementary Material for table of full output).
5. Discussion
Using weighted multivariable logistic regression, we identify that experiences of discrimination in the healthcare system are significantly associated with withholding information from providers. We also observe a positive association between some types of low trust in providers and withholding. These results reflect and expand on prior analysis of the role discrimination plays in patient experiences and perceptions (Armstrong et al., 2013), even when including patient trust measures. They also highlight the importance of examining specific dimensions of trust in understanding patient experiences and engagement with the healthcare system (Campos-Castillo & Anthony, 2019; Sewell, 2015).
In addition to established downstream consequences of discrimination and non-disclosure like under-utilization, there are further implications for healthcare as it increasingly relies on patient data in clinical decision support and precision medicine. Systemic inequities in society are reflected in the data available to healthcare systems and providers (Ferryman, 2020). Measurement of these biases is difficult as such tools are often proprietary (Obermeyer, Powers, Vogeli, & Mullainathan, 2019), but understanding the relationship between discrimination and data quality can serve as a starting point for identifying and mitigating some forms of data bias. It is possible that, in addition to the many harms of interpersonal discrimination in healthcare, patients who are discriminated against experience further harms through systematic data missingness that could negatively impact the quality of their care. For example, if patients who have experienced discrimination in the healthcare system withhold information such that relevant data is not available in their records, precision medicine approaches that seek to tailor individual treatment may be less effective for these patients than for patients with complete data. Similarly, clinical decision support tools may not adequately or effectively support the care of patients who have experienced discrimination if they are unrepresented or inaccurately represented in the data used to build these tools. These potential implications of discrimination in data-driven healthcare are under-explored and require sustained focus and analysis.
The work presented here focuses on reported experiences of interpersonal discrimination. Although these experiences reflect systemic inequities, they do not incorporate the myriad systemic barriers to trust and quality communication patients face. As clarified in conceptual work on racism and discriminatory provider behavior (Gee, Ro, Shariff-Marco, & Chae, 2009; Hausmann et al., 2011; LaVeist et al., 2003; Spencer & Grace, 2016; van Ryn et al., 2011), systemic social inequities operate both within and external to the healthcare system, informing provider perceptions and behaviors. Attempts to improve patient-provider information exchange and the completeness of data for all patients will need to address and engage with discrimination in the healthcare system at the organizational policy level (Williams, Lawrence, & Davis, 2019). Rather than problematizing patient perceptions or behaviors, efforts to build trust and improve data quality through patient disclosure should focus on ensuring healthcare providers and systems are trustworthy, by recognizing that discrimination operates as an exposure. Efforts to facilitate patient information disclosure and improve data quality will be more effective if they deal with discrimination in healthcare rather than problematizing patients' protective behaviors. Additional analyses of the roles of systemic inequities that build on a growing literature engaging with such systemic rather than solely individual factors are also necessary.
5.1. Limitations
Since trust in physicians is multi-dimensional and situational (Campos-Castillo & Anthony, 2019; Hall, Dugan, Zheng, & Mishra, 2001) it is important to measure multiple dimensions. Although we were able to measure multiple dimensions of trust previously implicated in patient information sharing (i.e., trust in confidentiality), other dimensions of trust are not included. Additionally, although our analysis clearly defines the trustor (patients), the trustee (providers), and trust objects (patient-provider interactions) (Schilke, Reimann, & Cook, 2021), further information about additional dimensions of trust may contribute important knowledge about patient non-disclosure. Future work should incorporate additional dimensions of trust from the literature and ideally draw on multiple survey measures of each dimension.
There are also limitations related to the data source. First, Asian respondents and Native American respondents are underrepresented in our sample which means that their experiences of discrimination may be underestimated in our dataset. Second, the measure of sex in the dataset is binary. This is limiting and future work should allow for more comprehensive sex and gender identity reporting. Third, the data is cross-sectional. Future longitudinal work on the relationships between discrimination and withholding information would expand our understanding of the relationships identified here. Finally, our measure of discrimination does not capture who in the healthcare system discriminated against the respondent. As indicated in prior work (Tajeu et al., 2015), non-clinical staff in a healthcare setting can discriminate against patients and negatively impact their experiences. This information is particularly important for interventions and policies designed to ameliorate discrimination.
6. Conclusion
Systematic data missingness within patient records has long been a concern, which grows more pressing as patient data is increasingly used for data-driven approaches to care like precision medicine. Our study suggests that discrimination, in addition to being a direct personal harm with a multitude of negative consequences, could also be a driver of biased data that contributes to inequitable care. If patients who experience discrimination are more likely to withhold information from their providers, it is more likely that their care will also suffer in both the short and long term. The odds of withholding information from a provider are much higher for those who have experienced discrimination while seeking medical care, even when controlling for low trust in providers. Our findings contribute evidence on discrimination as a barrier to quality care for marginalized patients through data missingness. They also highlight the importance of focusing interventions on discrimination in the healthcare system rather than patient perceptions or behaviors.
Authorship contributions
PN: Conceptualization, design and data collection, visualization and analysis, writing. AW: Conceptualization, analysis, writing. DA: Conceptualization, methodology, analysis, writing. JP: Conceptualization, design and data collection, review and editing. SK: Conceptualization, design and data collection, review and editing, supervision.
Declaration of competing interest
The authors have no conflicts of interest or financial conflicts to disclose.
Acknowledgment
This project was funded by the NIH (NIH 1R01CA214829).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2022.101092.
Contributor Information
Paige Nong, Email: ptassie@umich.edu.
Alicia Williamson, Email: akwill@umich.edu.
Jodyn Platt, Email: jeplatt@umich.edu.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Agaku I.T., Adisa A.O., Ayo-Yusuf O.A., Connolly G.N. Concern about security and privacy, and perceived control over collection and use of health information are related to withholding of health information from healthcare providers. Journal of the American Medical Informatics Association : JAMIA. 2014;21(2):374–378. doi: 10.1136/amiajnl-2013-002079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwala V., Khozin S., Singal G., O'Connell C., Kuk D., Li G., et al. Real-world evidence in support of precision medicine: Clinico-genomic cancer data as A case study. Health Affairs. 2018;37(5):765–772. doi: 10.1377/hlthaff.2017.1579. [DOI] [PubMed] [Google Scholar]
- Alang S., Hardeman R., Karbeah J., Akosionu O., McGuire C., Abdi H., et al. White supremacy and the core functions of public health. American Journal of Public Health. 2021;111(5):815–819. doi: 10.2105/AJPH.2020.306137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman D.G., Bland J.M. Missing data. BMJ. 2007;334(7590):424. doi: 10.1136/bmj.38977.682025.2C. 424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong K., Putt M., Halbert C.H., Grande D., Schwartz J.S., Liao K., et al. Prior experiences of racial discrimination and racial differences in health care system distrust. Medical Care. 2013;51(2):144–150. doi: 10.1097/MLR.0b013e31827310a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstrong K., Rose A., Peters N., Long J.A., McMurphy S., Shea J.A. Distrust of the health care system and self-reported health in the United States. Journal of General Internal Medicine. 2006;21(4):292–297. doi: 10.1111/j.1525-1497.2006.00396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barda N., Yona G., Rothblum G.N., Greenland P., Leibowitz M., Balicer R., et al. Addressing bias in prediction models by improving subpopulation calibration. Journal of the American Medical Informatics Association. 2021 doi: 10.1093/jamia/ocaa283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben J., Cormack D., Harris R., Paradies Y. Racism and health service utilisation: A systematic review and meta-analysis. PLoS One. 2017;12(12) doi: 10.1371/journal.pone.0189900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanch-Hartigan D., Chawla N., Moser R.P., Finney Rutten L.J., Hesse B.W., Arora N.K. Trends in cancer survivors' experience of patient-centered communication: Results from the health information national Trends survey (HINTS) Journal of Cancer Survivorship. 2016;10(6):1067–1077. doi: 10.1007/s11764-016-0550-7. [DOI] [PubMed] [Google Scholar]
- Bonilla-Silva E. Rethinking racism: Toward a structural interpretation. American Sociological Review. 1997;62(3):465–480. doi: 10.2307/2657316. [DOI] [Google Scholar]
- Boulware L.E., Cooper L.A., Ratner L.E., LaVeist T.A., Powe N.R. Race and trust in the health care system. Public Health Reports. 2003;118:8. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bugge C., Entwistle V.A., Watt I.S. The significance for decision-making of information that is not exchanged by patients and health professionals during consultations. Social Science & Medicine. 2006;63(8):2065–2078. doi: 10.1016/j.socscimed.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Campos-Castillo C., Anthony D.L. The double-edged sword of electronic health records: Implications for patient disclosure. Journal of the American Medical Informatics Association. 2015;22(e1):e130–e140. doi: 10.1136/amiajnl-2014-002804. [DOI] [PubMed] [Google Scholar]
- Campos-Castillo C., Anthony D. Situated trust in a physician: Patient health characteristics and trust in physician confidentiality. The Sociological Quarterly. 2019;60(4):559–582. doi: 10.1080/00380253.2018.1547174. [DOI] [Google Scholar]
- Collins F.S., Varmus H. A new initiative on precision medicine. New England Journal of Medicine. 2015;372(9):793–795. doi: 10.1056/NEJMp1500523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovidio J.F., Penner L.A., Albrecht T.L., Norton W.E., Gaertner S.L., Shelton J.N. Disparities and distrust: The implications of psychological processes for understanding racial disparities in health and health care. Social Science & Medicine. 2008;67(3):478–486. doi: 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- Entwistle V., Williams B., Skea Z., MacLennan G., Bhattacharya S. Which surgical decisions should patients participate in and how? Reflections on women's recollections of discussions about variants of hysterectomy. Social Science & Medicine. 2006;62(2):499–509. doi: 10.1016/j.socscimed.2005.06.027. [DOI] [PubMed] [Google Scholar]
- Ferryman K. Addressing health disparities in the Food and Drug Administration's artificial intelligence and machine learning regulatory framework. Journal of the American Medical Informatics Association. 2020;27(12):2016–2019. doi: 10.1093/jamia/ocaa133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finney Rutten L.J., Agunwamba A.A., Beckjord E., Hesse B.W., Moser R.P., Arora N.K. The relation between having a usual source of care and ratings of care quality: Does patient-centered communication play a role? Journal of Health Communication. 2015;20(7):759–765. doi: 10.1080/10810730.2015.1018592. [DOI] [PubMed] [Google Scholar]
- Finney Rutten L.J., Hesse B.W., St Sauver J.L., Wilson P., Chawla N., Hartigan D.B., et al. Health self-efficacy among populations with multiple chronic conditions: The value of patient-centered communication. Advances in Therapy. 2016;33(8):1440–1451. doi: 10.1007/s12325-016-0369-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella K., Meldrum S., Franks P., Shields C.G., Duberstein P., McDaniel S.H., et al. Patient trust: Is it related to patient-centered behavior of primary care physicians? Medical Care. 2004;42(11):1049–1055. doi: 10.1097/00005650-200411000-00003. [DOI] [PubMed] [Google Scholar]
- Friedman M.R., Dodge B., Schick V., Herbenick D., Hubach R.D., Bowling J., et al. From bias to bisexual health disparities: Attitudes toward bisexual men and women in the United States. LGBT Health. 2014;1(4):309–318. doi: 10.1089/lgbt.2014.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee G.C., Ro A., Shariff-Marco S., Chae D. Racial discrimination and health among Asian Americans: Evidence, assessment, and directions for future research. Epidemiologic Reviews. 2009;31(1):130–151. doi: 10.1093/epirev/mxp009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianfrancesco M.A., Tamang S., Yazdany J., Schmajuk G. Potential biases in machine learning algorithms using electronic health record data. JAMA Internal Medicine. 2018;178(11):1544–1547. doi: 10.1001/jamainternmed.2018.3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg G.S., Phillips K.A. Precision medicine: From science to value. Health Affairs. 2018;37(5):694–701. doi: 10.1377/hlthaff.2017.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn S.R. Patient-Centered communication to assess and enhance patient Adherence to glaucoma medication. Ophthalmology. 2009;116(11):S37–S42. doi: 10.1016/j.ophtha.2009.06.023. Supplement. [DOI] [PubMed] [Google Scholar]
- Hall M.A., Dugan E., Zheng B., Mishra A.K. Trust in physicians and medical institutions: What is it, can it Be measured, and does it matter? The Milbank Quarterly. 2001;79(4):613–639. doi: 10.1111/1468-0009.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall M.A., Zheng B., Dugan E., Camacho F., Kidd K.E., Mishra A., et al. Measuring patients' trust in their primary care providers. Medical Care Research and Review. 2002;59(3):293–318. doi: 10.1177/1077558702059003004. Scopus. [DOI] [PubMed] [Google Scholar]
- Hausmann L.R.M., Hannon M.J., Kresevic D.M., Hanusa B.H., Kwoh C.K., Ibrahim S.A. Impact of perceived discrimination in health care on patient-provider communication. Medical Care. 2011;49(7):626–633. doi: 10.1097/MLR.0b013e318215d93c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horne R. Compliance, adherence, and concordance: Implications for asthma treatment. Chest. 2006;130(1):65S–72S. doi: 10.1378/chest.130.1_suppl.65S. Supplement. [DOI] [PubMed] [Google Scholar]
- Iott B.E., Campos-Castillo C., Anthony D.L. Trust and privacy: How patient trust in providers is related to privacy behaviors and attitudes. AMIA Annual Symposium Proceedings. 2020:487–493. 2019. [PMC free article] [PubMed] [Google Scholar]
- Jones C.P. Levels of racism: A theoretic framework and a gardener's tale. American Journal of Public Health. 2000;90(8):1212–1215. doi: 10.2105/ajph.90.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. In: Social epidemiology. Berkman L.F., Kawachi I., editors. Oxford University Press; 2000. Discrimination and health. [Google Scholar]
- Krieger N. Discrimination and health inequities. International Journal of Health Services. 2014;44(4):643–710. doi: 10.2190/HS.44.4.b. [DOI] [PubMed] [Google Scholar]
- Krieger N., Smith K., Naishadham D., Hartman C., Barbeau E.M. Experiences of discrimination: Validity and reliability of a self-report measure for population health research on racism and health. Social Science & Medicine. 2005;61(7):1576–1596. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- LaVeist T.A., Isaac L.A., Williams K.P. Mistrust of health care organizations is associated with underutilization of health services. Health Services Research. 2009;44(6):2093–2105. doi: 10.1111/j.1475-6773.2009.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist T.A., Nickerson K.J., Bowie J.V. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Medical Care Research and Review. 2000;57:146–161. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- LaVeist T.A., Nuru-Jeter A., Jones K.E. The association of doctor-patient race concordance with health services utilization. Journal of Public Health Policy. 2003;24(3):312–323. doi: 10.2307/3343378. [DOI] [PubMed] [Google Scholar]
- Levy A.G., Scherer A.M., Zikmund-Fisher B.J., Larkin K., Barnes G.D., Fagerlin A. Prevalence of and factors associated with patient nondisclosure of medically relevant information to clinicians. JAMA Network Open. 2018;1(7) doi: 10.1001/jamanetworkopen.2018.5293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin K.D., Roter D.L., Beach M.C., Carson K.A., Cooper L.A. Physician communication behaviors and trust among Black and white patients with hypertension. Medical Care. 2013;51(2):151–157. doi: 10.1097/MLR.0b013e31827632a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechanic D. The functions and limitations of trust in the provision of medical care. Journal of Health Politics, Policy and Law. 1998;23(4):661–686. doi: 10.1215/03616878-23-4-661. [DOI] [PubMed] [Google Scholar]
- Mechanic D., Meyer S. Concepts of trust among patients with serious illness. Social Science & Medicine. 2000;51(5):657–668. doi: 10.1016/S0277-9536(00)00014-9. [DOI] [PubMed] [Google Scholar]
- Mitchell J.A., Perry R. Disparities in patient-centered communication for Black and Latino men in the U.S.: Cross-sectional results from the 2010 health and retirement study. PLoS One. 2020;15(9 September) doi: 10.1371/journal.pone.0238356. Scopus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngiam K.Y., Khor I.W. Big data and machine learning algorithms for health-care delivery. The Lancet Oncology. 2019;20(5):e262–e273. doi: 10.1016/S1470-2045(19)30149-4. [DOI] [PubMed] [Google Scholar]
- Ng J., Ye F., Ward L., Haffer S., Hudson Scholle S. Data on race, ethnicity, and language largely incomplete for managed care plan members | health affairs. Health Affairs. 2017;36(3) doi: 10.1377/hlthaff.2016.1044. https://www.healthaffairs.org/doi/10.1377/hlthaff.2016.1044 [DOI] [PubMed] [Google Scholar]
- Nong P., Raj M., Creary M., Kardia S.L.R., Platt J.E. Patient-reported experiences of discrimination in the US health care system. JAMA Network Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.29650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obermeyer Z., Powers B., Vogeli C., Mullainathan S. Dissecting racial bias in an algorithm used to manage the health of populations. Science. 2019;366(6464):447–453. doi: 10.1126/science.aax2342. [DOI] [PubMed] [Google Scholar]
- Ostertag S., Wright B.R.E., Broadhead R.S., Altice F.L. Trust and other characteristics associated with health care utilization by injection drug users. Journal of Drug Issues. 2006;36(4):953–974. doi: 10.1177/002204260603600409. [DOI] [Google Scholar]
- Rajkomar A., Hardt M., Howell M.D., Corrado G., Chin M.H. Ensuring fairness in machine learning to advance health equity. Annals of Internal Medicine. 2018;169(12):866–872. doi: 10.7326/M18-1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross R.K., Breskin A., Westreich D. When is a complete-case approach to missing data valid? The importance of effect-measure modification. American Journal of Epidemiology. 2020;189(12):1583–1589. doi: 10.1093/aje/kwaa124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ryn M., Burgess D.J., Dovidio J.F., Phelan S.M., Saha S., Malat J., et al. The impact of racism on clinician cognition, behavior, and clinical decision making. Du Bois Review : Social Science Research on Race. 2011;8(1):199–218. doi: 10.1017/S1742058X11000191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ryn M., Fu S.S. Paved with good intentions: Do public health and human service providers contribute to racial/ethnic disparities in health? American Journal of Public Health. 2003;93(2):248. doi: 10.2105/ajph.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin J.A., Riskind R.G., Nosek B.A. Health care providers' implicit and explicit attitudes toward lesbian women and gay men. American Journal of Public Health. 2015;105(9):1831–1841. doi: 10.2105/AJPH.2015.302631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schilke O., Reimann M., Cook K.S. Trust in social relations. Annual Review of Sociology. 2021;47(1) doi: 10.1146/annurev-soc-082120-082850. [DOI] [Google Scholar]
- Sewell A.A. Disaggregating ethnoracial disparities in physician trust. Social Science Research. 2015;54:1–20. doi: 10.1016/j.ssresearch.2015.06.020. [DOI] [PubMed] [Google Scholar]
- Spencer K.L., Grace M. Social foundations of health care inequality and treatment bias. Annual Review of Sociology. 2016;42(1):101–120. doi: 10.1146/annurev-soc-081715-074226. [DOI] [Google Scholar]
- Stablein T., Hall J.L., Pervis C., Anthony D.L. Negotiating stigma in health care: Disclosure and the role of electronic health records. Health Sociology Review. 2015;24(3):227–241. doi: 10.1080/14461242.2015.1078218. [DOI] [Google Scholar]
- Stepanikova I., Oates G.R. Perceived discrimination and privilege in health care: The role of socioeconomic status and race. American Journal of Preventive Medicine. 2017;52(1S1):S86–S94. doi: 10.1016/j.amepre.2016.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson F.A., Cox K., Britten N., Dundar Y. A systematic review of the research on communication between patients and health care professionals about medicines: The consequences for concordance. Health Expectations. 2004;7(3):235–245. doi: 10.1111/j.1369-7625.2004.00281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton R.T., Pincock D., Baumgart D.C., Sadowski D.C., Fedorak R.N., Kroeker K.I. An overview of clinical decision support systems: Benefits, risks, and strategies for success. Npj Digital Medicine. 2020;3(1):1–10. doi: 10.1038/s41746-020-0221-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tajeu G.S., Cherrington A.L., Andreae L., Prince C., Holt C.L., Halanych J.H. We’ll get to you when we get to you”: Exploring potential contributions of health care staff behaviors to patient perceptions of discrimination and satisfaction. American Journal of Public Health. 2015;105(10):2076–2082. doi: 10.2105/AJPH.2015.302721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thom D.H., Hall M.A., Pawlson L.G. Measuring patients' trust in physicians when assessing quality of care. Health Affairs. 2004;23(4):124–132. doi: 10.1377/hlthaff.23.4.124. [DOI] [PubMed] [Google Scholar]
- Trivedi A.N., Ayanian J.Z. Perceived discrimination and use of preventive health services. Journal of General Internal Medicine. 2006;21(6):553–558. doi: 10.1111/j.1525-1497.2006.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi N., Moser R.P., Breslau E.S., Chou W.-Y.S. Predictors of patient-centered communication among U.S. Adults: Analysis of the 2017-2018 health information national Trends survey (HINTS) Journal of Health Communication. 2021;26(1):57–64. doi: 10.1080/10810730.2021.1878400. [DOI] [PubMed] [Google Scholar]
- Verhaeghe M., Bracke P. Stigma and trust among mental health service users. Archives of Psychiatric Nursing. 2011;25(4):294–302. doi: 10.1016/j.apnu.2011.02.001. [DOI] [PubMed] [Google Scholar]
- Wang F., Preininger A. AI in health: State of the art, challenges, and future directions. Yearbook of Medical Informatics. 2019;28(1):16–26. doi: 10.1055/s-0039-1677908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiskopf N.G., Hripcsak G., Swaminathan S., Weng C. Defining and measuring completeness of electronic health records for secondary use. Journal of Biomedical Informatics. 2013;46(5):830–836. doi: 10.1016/j.jbi.2013.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Lawrence J., Davis B. Racism and health: Evidence and needed research. Annual Review of Public Health. 2019;40:105–125. doi: 10.1146/annurev-publhealth-040218-043750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Lawrence J.A., Davis B.A., Vu C. Understanding how discrimination can affect health. Health Services Research. 2019;54(S2):1374–1388. doi: 10.1111/1475-6773.13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Mohammed S.A. Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Yan Y., Jackson J.S., Anderson N.B. Racial differences in physical and mental health: Socio-economic status, stress and discrimination. Journal of Health Psychology. 1997;2(3):335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.