Abstract
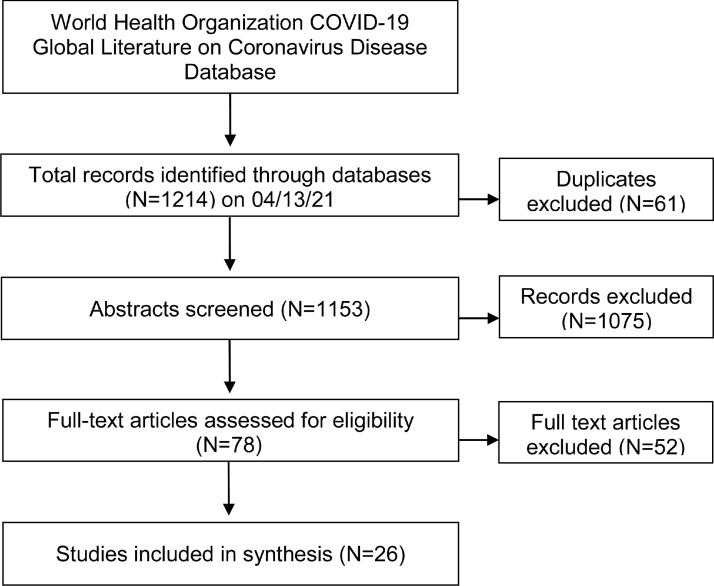
Health care policymaking during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic has questioned the precedent of restricting hospital visitors. We aimed to synthesize available data describing the resulting impact on patient, family/visitor, and health care provider well-being. We systematically reviewed articles from the World Health Organization COVID-19 Global Literature on Coronavirus Disease Database published between December 2019 through April 2021. Included studies focused on hospitalized patients and reported 1 or more prespecified main or secondary outcome (coronavirus disease 2019 [COVID-19] disease transmission, global well-being, mortality, morbidity, or health care resource utilization). Two authors independently extracted data into a standardized form with a third author resolving discrepancies. A total of 1153 abstracts were screened, and 26 final full-text articles were included. Ten studies were qualitative, with 7 cohort studies, and no randomized controlled trials. Critically ill patients were the most represented (12 out of 26 studies). Blanket hospital visitor policies were associated with failure to address the unique needs of patients, their visitors, and health care providers in various clinical environments. Overall, a patient-centered, thoughtful, and nuanced approach to hospital visitor policies is likely to benefit all stakeholders while minimizing potential harms.
Keywords: Coronavirus, COVID-19, Health care, Policy, Virus, Visitor
Clinical Significance.
-
•
Restrictive hospital visitor policies have differential effects on various populations, notably critically ill patients, clinicians, and family or support persons.
-
•
There may be challenges with effective and equitable implementation of video conferencing.
-
•
The effect of altering hospital visitor policies on coronavirus disease 2019 (COVID-19) transmission is poorly studied.
-
•
It is prudent to pursue a patient-centered, thoughtful, and nuanced approach to hospital visitor policies accounting for clinical judgment as opposed to blanket rulings produced by administrators.
Alt-text: Unlabelled box
SEE RELATED ARTICLES, p 1154 and 1156.
Alt-text: Unlabelled box
Introduction
In western tradition, only early in the 20th century did hospitals begin to allow visitors for paying patients.1 Fifty years later, after the establishment of newborn intensive care units (NICUs), visitor policies appeared more familiar to those of modern day with limited visiting hours for all patients.2 Additional restrictions for infection control is an established practice during respiratory syncytial virus and influenza seasons.3, 4, 5 Although not novel, the efficacy and guidance for visitor restrictions remains inconsistent, especially for the coronavirus disease 2019 (COVID-19) pandemic. The Centers for Disease Control and Prevention (CDC) recommended limiting visitors to inpatient facilities “to only those essential for the patient's physical or emotional well-being and care.”6 It is reasonable to suspect that practical application of this statement may vary across institutions and practices. Lack of clarity leaves the potential for inequities in implementation and raises ethical questions.7 , 8 Restriction of visitors is also discussed as a source of moral distress for health care providers who may not agree with hospital policies.9 , 10 Yet, a Cochrane rapid qualitative evidence synthesis review of barriers to health care providers’ adherence to infection control measures found an opposing effect. Health care workers experienced strain from being responsible for visitors’ adherence to infection control measures.11 The significance of the transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from visitors in hospitals, however, is also questionable.12 Therefore, we sought to critically appraise the evidence relating hospital visitor restrictions and COVID-19 transmission. We aimed to determine the impact of visitor restrictions on the well-being of hospitalized patients, their visitors, and health care providers during the COVID-19 pandemic.
Methods
Further details are available in the PROSPERO protocol associated with this study (CRD42021248603) that was developed in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) checklist.13
Data Sources and Searches
We searched the World Health Organization (WHO) COVID-19 Global Literature on Coronavirus Disease Database, which includes more than 30 databases, at https://www.who.int/publications/m/item/quick-search-guide-who-covid-19-database, using the following search strategy: (ti:(visit*)) OR (ab:(visit* AND (restrict*))) OR (mj:(MH:"Visitors to Patients")).
Study Selection
We included quantitative and qualitative studies as well as conference abstracts from December 2019 to April 2021. Studies must have focused on hospitalized patients, their families and visitors, or health care providers of all ages in the setting of the COVID-19 pandemic. “Hospital” was defined as a public or academic institution in which a patient was admitted for inpatient medical care. Studies were in English and reported at least 1 of the prespecified main or secondary outcomes (COVID-19 disease transmission, global well-being, mortality, morbidity, or health care resource utilization).
Reviews of existing literature, editorials, and expert opinions were excluded. Studies that did not fit into the conceptual framework of this systematic review or focused on a population other than hospitalized patients were also excluded. Long-term care and skilled nursing facilities were excluded because they are not considered hospitals but places of permanent residence.
Using a systematic review software, Rayyan,14 2 independent reviewers screened abstracts based on the predefined criteria. Discrepancies were discussed with a third reviewer until a consensus was reached. This same process was repeated with full articles.
Data Extraction and Quality Assessment
For each included study, 2 reviewers extracted data independently using a standardized data extraction form (Supplementary Table 1, available online). This process occurred without blinding of study authors, institutions, journals, or results. Discrepancies were resolved by discussion with a third reviewer and the research team, as necessary.
Supplementary Table 1.
Data Extraction Form
| Criteria | Data Entry |
|---|---|
| Study characteristics and data quality | |
| General | Article ID #, First author, Journal, Year of publication |
| Geographic location | 0=USA (please list state[s]), 1=Other country (please list) |
| Setting | 0=General ward, 1=Stepdown, 2=ICU |
| Level of Care | 0=Regular visit, 1=End-of-life care, 2=Other special circumstance |
| Type | 0=Clinical trial/interventional, 1=Observational |
| Study design | General design, Inclusion criteria, Exclusion criteria |
| Study quality and risk of bias | GRADE: 0=not needed, 1=very low, 2=low, 3=moderate, 4=high |
| ROBINS-I (if applicable), ROB 2 (if applicable), CASP (if applicable) | |
| Studies of patients | |
| Sample size | |
| Patient population | 0=Adults (mean age >18), 1=Geriatrics (mean age >65), 2=Neonates (mean age <4 weeks), 4=Pediatrics (mean age >4 weeks, <18 years) |
| Percent male | |
| Special population | |
| COVID-19 status: 0=Diagnosed, 1=Symptomatic, 2=Suspected, 3=No COVID | |
| Visitation policy | Type and description: 0=Unrestricted, 1=Some restrictions, 2=No visitors |
| Outcome measures (method and result) | Primary: Global well-being, Quality of life, Satisfaction survey, Moral distress |
| Secondary: Morbidity, Mortality, Health care resource utilization | |
| Studies of health care providers | |
| Sample size | |
| Subjects | 0=Physician, 1=Student, 2=Nurse, 3=Ancillary staff |
| Percent male | |
| Visitation policy | Type and description: 0=Unrestricted,1=Some restrictions, 2=No visitors |
| Outcome measures (method and result) | Primary: Global well-being, Quality of life, Satisfaction survey, Moral distress |
| Secondary: Morbidity, Mortality, Healthcare resource utilization | |
| Studies of family members | |
| Sample size | |
| Patient population | 0=Adults (mean age >18), 1=Geriatrics (mean age >65), 2=Neonates (mean age <4 weeks), 4=Pediatrics (mean age >4 weeks, <18 years) |
| Percent male | |
| Special population | |
| COVID-19 status: 0=Diagnosed, 1=Symptomatic, 2=Suspected, 3=No COVID | |
| Visitation policy | Type and description: 0=Unrestricted,1=Some restrictions, 2=No visitors |
| Outcome measures (method and result) | Primary: Global well-being, Quality of life, Satisfaction survey, Moral distress |
| Secondary: Morbidity, Mortality, Health care resource utilization | |
CASP = Critical Appraisal Skills Programme; COVID-19 = coronavirus disease 2019; ICU = intensive care unit; ROBINS-I = Risk Of Bias In Nonrandomized Studies of Interventions.
We evaluated the risk of bias using the Cochrane Collaboration's tool Risk Of Bias In Non randomized Studies of Interventions (ROBINS-I), Critical Appraisal Skills Programme (CASP) appraisal tool for qualitative studies, and Oxford Centre for Evidence-based Medicine quality scheme.15, 16, 17 Two authors ranked each study's risk of bias separately. Disagreements were resolved by discussion with a third reviewer.
Data Synthesis and Analysis
Given the heterogeneity in methodologies across the literature, we comprehensively tabulated study characteristics, permitting critique of design and enumeration of potential biases. Two authors (ANI and JOA) independently made this determination, with input from a third author in the event of a discrepancy (WS). A narrative synthesis was performed including study design, patient population, hospital visitor policy changes, and reported outcomes. Mean COVID-19 transmission rate was the primary outcome. Thorough documentation was prioritized given the paucity of high-quality studies on this emerging topic and with predominance of descriptive outcomes. Studies were grouped by population (eg, neonatal, pediatric, or adult patients), clinical setting (eg, intensive care unit, general floor unit, end-of-life care vs general care, etc.), and visitation policy. Data were handled by groups as opposed to individual participant data.
Results
Description of Included Studies
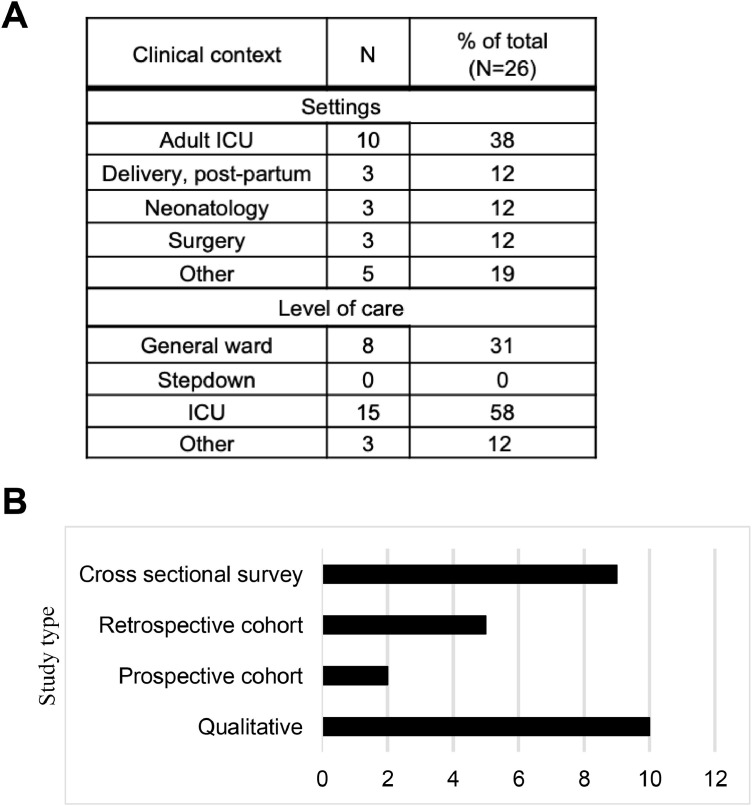
We identified 1153 abstracts, which were read in full. A total of 78 articles met criteria for screening of the study report. Of these, 26 studies met prespecified criteria for inclusion (Figure 1 ). Half of the studies were published in 2020, the first year of the pandemic and half in 2021. Most studies took place in North America (46%), specifically the United States, followed by Europe (42%), including the UK, France, and Italy. Patients were the population of interest in 37% of included studies; family, support persons, or visitors were the focus of 33%; 29% assessed the impact of visitor restrictions on health care providers; and the remaining 11% addressed multiple populations. As may be expected with severe COVID-19 infection, a plurality of studies took place in intensive care units (ICUs) (Figure 2 A). Finally, the majority of the included studies were qualitative or survey-based; only 7 of 26 were cohort studies (Figure 2B).
Figure 1.
Systematic review protocol workflow. Flowchart is adapted from the PRISMA flow diagram for included studies. PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Figure 2.
Characterization of included studies. (A) Clinical context of included studies broken down by clinical setting and level of care/acuity with most studies taking place in the ICU. (B) Graph tabulating the number of each study methodology. For all, N = 26. ICU = intensive care unit.
Inpatient Wards
We found 5 of 26 included studies focused on the inpatient ward setting, and a common theme among them was attention to vulnerable populations with potentially impaired decision-making capacity (Table 1 ). Visitors or support persons may serve as patient advocates and aid in decision-making if legally authorized.18 One common cause of impaired capacity in the inpatient setting is delirium. Some suggest that the presence of hospital visitors may protect against delirium development, but this notion was challenged in recent studies.19 , 20 A retrospective cohort study of adults who underwent emergency hospital admissions in Japan (N = 6264) found greater odds for developing delirium after pandemic visitor restrictions as compared with unrestricted visitor policies (adjusted odds ratio [AOR] for delirium incidence 3.79, 95% confidence interval [CI], 2.70-5.31).21 Similarly, patients in inpatient psychiatric facilities also represent a vulnerable population because of their often limited autonomy and potentially diminished capacity and were negatively impacted by visitor restrictions.22 In 1 study of 24 patients in Norway, 80% reported difficulty with not having loved ones present and expressed a need for visitors, 64% believed staff would prevent them from becoming infected with COVID-19, and 88% overall felt safe at the ward. On the contrary, of 140 staff members surveyed at the same facility, 57% feared bringing home COVID-19 from work and 69% were satisfied with measures to mitigate risk of infection (including visitor restrictions).23 Two additional potentially vulnerable populations include pediatrics and peripartum patients, which are discussed in the Supplemental Materials, available online.
Table 1.
Summary of Included Studies Focused on the Inpatient Ward Setting*
| First Author | Location | Design | Sample size | Participants | Visitor Policy |
|---|---|---|---|---|---|
| Dieset I23 | Norway | Cross-sectional survey | 24 | Psychiatric inpatient (female: 69%) | No visitors |
| 140 | Staff in an acute psychiatric inpatient unit (nurses: 67%, physicians or psychologists: 26%, other staff: 7%) | ||||
| Kandori K21 | Japan | Retrospective cohort | 6264 | Adult emergency admissions inpatients (median age: 74, female: 47%%) | No visitors |
| Onwuteaka-Philipsen BD24 | Netherlands | Cross-sectional survey | 241 | Health care professionals (female: 49%) regarding patients who died | Some restriction |
| Feder S26 | United States | Cross-sectional survey | 328 | Next of kin of veterans who died in an inpatient unit (mean age: 76, female: 7%) | No visitors |
| Maaskant JM25 | Netherlands | Cross-sectional survey | 9 | Bedside nurses of inpatient COVID-19 hospital wards (median age: 32, female: 89%) | Some restriction |
COVID-19 = coronavirus disease 2019.
The “No visitors” designation was reserved for studies that explicitly stated no visitors were allowed under any circumstances, per hospital policy. Gender and mean or median age reported as available.
Several studies also concerned end-of-life care. A cross-sectional survey of health care providers regarding deceased patients in the Netherlands found sufficient emotional support was less common for patients for whom there had been restricted (AOR 0.46, 95% CI 0.29-0.75) or no visitors (AOR 0.23, 95% CI 0.12-0.45).24 Spiritual care was also less sufficient for patients who were not allowed visitors in the last 2 days of life (AOR 0.21, 95% CI 0.10-0.42). A small focus group (N = 9) of nurses discussed how the need for family involvement increases during end-of-life care, which can strain personnel who are tasked with communicating with families remotely.25 Similarly, a cross-sectional survey of 328 next of kin of veterans who died in an inpatient unit found themes of “anguish and despair” from not being allowed to see patients.26
Overall, the COVID-19 pandemic and visitor restrictions were associated with negative emotions among most inpatients and their families in the studies reviewed, especially in the context of end-of-life care. There was evidence of moral distress for health care providers caring for dying patients; however, some responded positively to visitor restrictions from the perspective of limiting their occupational exposure to the COVID-19 virus.
Adult ICUs
End-of-life care and vulnerable population discussions are especially pertinent to the ICU setting (Table 2 ). A large cross-sectional survey (N = 1058) of health care providers in France reported that 31.5% regretted restricted visitation policies that were associated with symptoms of anxiety (odds ratio 1.39; 95% CI 1.03-1.86) and depression (odds ratio 1.49; 95% CI, 1.09-2.04).27 Clinicians in the UK also expressed dissent with restricting visitors and raised concerns about the detrimental effect on patients, their families, and staff.28
Table 2.
Summary of Included Studies Focused on the ICU Setting*
| First author | Location | Design | Sample size | Participants | Visitor Policy |
|---|---|---|---|---|---|
| Azoulay E27 | France | Cross-sectional survey | 1058 | Frontline health care providers (median age: 33, female: 71%) | Some restriction |
| Azad TD29 | Maryland, United States | Retrospective cohort | 940 | Adult decedents | Some restriction |
| Piscitello GM30 | Illinois, United States | Retrospective cohort | 61 | Patients lacking medical decision-making capacity | Some restriction |
| Cattelan J31 | France | Prospective cohort | 88 | Reference persons of patients referred to ICU for COVID-19 (female: 65%, first-degree relatives of the patient: 92%) | No visitors |
| Chen C32 | New York, United States | Cross-sectional survey | 10 | Family members of adult patients with COVID-19 in the ICU | No visitors |
| Creutzfeldt CJ33 | Washington, United States | Cross-sectional survey | 19 | Family members of patients with severe acute brain injury (female: 59%) | No visitors |
| Kennedy NR34 | Pennsylvania, United States | Qualitative interview | 21 | Family members cardiothoracic and neurologic ICU patients (mean age: 56, female: 76%) | Some restriction |
| 14 | Treating clinicians of cardiothoracic and neurologic ICU patients (female: 36%) | ||||
| Sasangohar F35 | Texas, United States | Cross-sectional survey | 230 | Family members of intensive care unit patients | No visitors |
| Jeyabraba S36 | UK | Retrospective survey | 24 | Families affected by the visitor restrictions during the coronavirus period | No visitors |
| Rose L37 | UK | Cross-sectional survey | 117 ICUs | 217 UK hospitals with at least 1 ICU | Mixed |
| Azoulay E27 | France | Cross-sectional survey | 1058 | Frontline health care providers (median age: 33, female: 71%) | Some restriction |
| Boulton AJ28 | UK | Cross-sectional survey | 134 | ICUs with patients with COVID-19 | Some restriction |
COVID-19 = coronavirus disease 2019; ICU = intensive care unit.
The “No visitors” designation was reserved for studies that explicitly stated no visitors were allowed under any circumstances, per hospital policy. Gender and mean or median age reported as available.
Video conferencing is becoming a common means of communicating with families remotely; however, it is uncertain whether this can fully substitute for physical presence. A retrospective cohort of 940 patients with adult descendant subjects found that patient admission after restrictive visitor policy implementation was associated with a significantly longer time to first do not resuscitate, do not intubate, or comfort care order (adjusted hazard ratio, 2.2; 95% CI, 1.6-3.1).29 Another retrospective cohort study of patients lacking medical decision-making capacity found more frequent changes in patient goals of care for in-person meetings than by video (36% vs 11%, P = .0006), implying a potential differential effect of communication modality on outcome.30 A prospective cohort of 88 families of ICU patients in France assessed the impact of remote communication on reference persons (RPs)—family members as designated points of contact for communication from health care providers. All RPs surveyed described a specific type of “responsibility” with being an RP in a remote-only context, leading RPs to restrict communication to extended family members (67%). Thirty percent of RPs related the situation to a prior traumatic experience.31 Among all the studies assessed here, restriction of visitors in the ICU setting was associated with distress among patients and their health care providers. A prominent challenge in this environment was navigating goals of care discussions and it seems that mode of communication may influence the decision-making outcome.
Patients in the Postoperative Period
Two studies covered the postoperative patient population (Table 3 ). A retrospective cohort study of 117 postoperative patients who were not allowed visitors found that those in the no-visitor cohort were less likely to report complete satisfaction with the hospital experience (80.7% vs 66%, P = .044), timely receipt of medications (84.5% vs 69%, P = .048), and assistance getting out of bed (70.7% vs 51.7%, P = .036).38 Qualitative analysis of patient responses highlighted the consistent psychosocial support provided by visitors after surgery (84.5%), and patients in the no-visitor cohort reported social isolation due to lack of psychosocial support (50.8%). A similar study of 541 postoperative patients in Italy, however, found a unique benefit of pandemic precautions for postoperative patients.39 The measures to reduce the severe acute respiratory coronavirus 2 spread (ie, surgical mask wearing and no visitors allowed) were independently associated with the reduction of all surgery site infections (AOR: 0.316, 95% CI: 0.103-0.970). It seems that psychosocial stress results from limiting visitor access may be somewhat offset by reducing infection risk in the postoperative setting. Interestingly, the transmission of COVID-19 infection was still not assessed.
Table 3.
Summary of Included Studies Focused on the Postoperative Setting*
| First Author | Location | Design | Sample size | Participants | Visitor Policy |
|---|---|---|---|---|---|
| Zeh RD38 | Ohio, United States | Retrospective cohort | 117 | Postoperative surgery patients (mean age: 57.5, female: 56.4%) | No visitors |
| Losurdo P39 | Italy | Retrospective cohort | 541 | Surgical patients (mean age: 62, female: 59.8%) | No visitors |
The “No visitors” designation was reserved for studies that explicitly stated no visitors were allowed under any circumstances, per hospital policy. Demographic information reported as available.
Video Conferencing
In lieu of in-person visits, video calls are increasingly prevalent in hospitals. A retrospective survey of families (N = 24) in the UK who received video calls were more likely to be satisfied with the frequency (83%) and quality (83%) of communication.34 All reported that video calls helped them to stay connected with the patient and health care team. Although another valence-based and manual sentiment analysis of family members of ICU patients found mostly positive responses to video visits, 44% of respondents (25 out of 57) found it challenging to communicate with patients due to being either intubated or undergoing procedures, a pertinent consideration for the critically ill patient population.35 A small (N = 10) cross-sectional qualitative survey of family members of ventilated patients highlighted this challenge.36 This group struggled to feel informed, had difficulty understanding information, and found video calls unhelpful. Commonly reported benefits for those patients who could participate in virtual visits across 117 ICUs in the UK included reducing patient psychological distress (78%) and reorientation of delirious patients (47%).37
Qualitative interviews with ICU physicians yielded different results.38 This study found that telehealth increased clinician workload, technical difficulties limited effective communication, and clinicians struggled to engage family members because of discomfort with technology use and less apparent social cues. Clinicians also were concerned about ability to convey empathy remotely. Family member participants, however, felt empathy was relayed successfully via phone and video. In this same study, respondents viewed phone and video communication as somewhat effective but inferior to in-person communication.38 Common barriers to virtual visiting included challenges associated with family member ability to use videoconferencing technology or having access to a device.37 Communication strategies suggested by families and clinicians for productive remote interactions include identifying a family point person to receive updates, frequently assessing family understanding, positioning the camera so that family can see the patient, and allowing time for the family and patient to interact without clinician presence.38 Interestingly, this model is in contrast to the study in France that reported high levels of stress among RPs who were to field provider calls and updates.31 Overall, judicious use of video conferencing may be beneficial in some settings. Optimizing communication strategies is important from the provider standpoint. Technical issues and access to technology may limit effective implementation of video conferencing.
Study Quality
The authors found the included studies were of limited quality (Table 4 ). Qualitative studies, of which there were several (Figure 2B), were evaluated using the Critical Appraisal Skills Program appraisal tool.15 Here, the authors found inconsistent use of validated formal assessment measures for coding of subject interviews. Globally, this contributed to substantial heterogeneity, limiting the ability to synthesize data. Furthermore, the nature of the secondary research questions has a tendency toward qualitative studies which, by nature, precludes most quantitative analyses. Given the uncertain potential risks and benefits of allowing hospital visitors, it might be argued that a randomized controlled trial is justified in this situation to provide further clarity, as was done for a study assessing impact of visitor presence on delirium prevalence in patients in the ICU.19
Table 4.
Evaluation of Study Quality*
| First Author | Location | Design | Modified OCEM Rating | ROBINS-I Score or CASP Rank |
|---|---|---|---|---|
| Ashini A40 | Libya | Cross-sectional survey | 4 | 10 (CASP) |
| Azad TD29 | United States | Retrospective cohort | 3 | 3 (ROBINS-I) |
| Azoulay E27 | France | Cross-sectional survey | 4 | 3 (CASP) |
| Bembich S41 | Italy | Cross-sectional survey | 4 | 6 (CASP) |
| Boulton AJ 28 | UK | Cross-sectional survey | 4 | 9 (CASP) |
| Bradfield Z42 | Australia | Cross-sectional survey | 4 | 3 (CASP) |
| Cattelan J31 | France | Prospective cohort | 3 | 3 (CASP) |
| Chen C32 | United States | Cross-sectional survey | 4 | 2 (CASP) |
| Creutzfeldt CJ33 | United States | Cross-sectional survey | 4 | 9 (CASP) |
| Cullen S43 | Ireland | Cross-sectional survey | 4 | 6 (CASP) |
| Dieset I23 | Norway | Cross-sectional survey | 4 | 7 (CASP) |
| Feder S26 | United States | Cross-sectional survey | 4 | 3 (CASP) |
| Jeyabraba S36 | UK | Retrospective survey | 4 | 6 (CASP) |
| Kandori K21 | Japan | Retrospective cohort | 3 | 1 (CASP) |
| Kennedy NR34 | United States | Qualitative interview | 4 | 1 (CASP) |
| Losurdo P39 | Italy | Retrospective cohort | 3 | 2 (ROBINS-I) |
| Maaskant JM25 | Netherlands | Cross-sectional survey | 4 | 1(CASP) |
| Mayopoulos G44 | United States | Cross-sectional survey | 4 | 3 (CASP) |
| Muniraman H45 | UK | Cross-sectional survey | 4 | 3 (CASP) |
| Onwuteaka-Philipsen BD24 | Netherlands | Cross-sectional survey | 4 | 6 (CASP) |
| Piscitello GM30 | United States | Retrospective cohort | 3 | 3 (ROBINS-I) |
| Romano-Keeler J46 | United States | Prospective cohort | 3 | 8 (CASP) |
| Rose L37 | UK | Cross-sectional survey | 4 | 4 (CASP) |
| Sasangohar F35 | United States | Cross-sectional survey | 4 | 5 (CASP) |
| Wiener L47 | United States | Cross-sectional survey | 4 | 1 (CASP) |
| Zeh RD38 | United States | Retrospective cohort | 3 | 2 (ROBINS-I) |
CASP = Critical Appraisal Skills Programme; OCEM = Oxford Centre for Evidence-based Medicine; ROBINS-I = Risk Of Bias In Nonrandomized Studies of Interventions.
Ratings based on Modified OCEM, ROBINS-I, and CASP scoring systems. For ROBINS-I, 0 = not needed, 1 = very low, 2 = low, 3 = moderate, 4 = high assessment of study quality.
Discussion
Risk-benefit assessment is the cornerstone of medical and policy decision-making. As our systematic review has shown, there are inadequate studies of sufficient quality to determine whether restrictive policies have been effective in potentially limiting the spread of COVID-19. Although it might be reasonable to speculate that these policies slow spread based on mechanistic understanding of disease, this must be weighed against the potential harms of limiting hospital visitors. Our study highlights the complexity associated with the numerous factors and stakeholders impacted by hospital visitor policies. A review of literature surrounding hospital visitor policies after the 2003 severe acute respiratory syndrome (SARS) outbreak concluded that there should be a tailored approach to visitor policies depending on the clinical scenario. For example, reasonable exceptions include allowing visitors for the labor and delivery unit, adults with disabilities, children, and dying individuals.7 Similarly, recommendations from 7 interdisciplinary German palliative care societies argue for making palliative care and dying patients exempt from hospital visitor bans.48 Specifically, the authors advocate for a patient-centered guidance of visitor policies.49 Together, this argues for a nuanced approach to hospital visitor policymaking, taking into account clinical setting, patient population, visitor use of personal protective equipment, screening measures, community prevalence, and immunization status.12 Exceptional circumstances should be included, and policies should be clearly articulated with transparent communication to the public.7 , 50
The CDC now provides visitor recommendations for a variety of scenarios (eg, vaccinated versus unvaccinated status, symptomatic vs asymptomatic, and specific facilities, such as dialysis centers); however, end-of-life care is not addressed.6 The CDC also recommends using alternative methods of staying connected with patients, such as video calls. Although our findings suggest that increasing availability of video conferencing may be beneficial in certain situations, consideration should be given to how this practice may be practically and equitably applied. Exclusive reliance on technology may differentially impact those at an economic or resource disadvantage. The origin of this potential disparity harkens back to the infancy of hospital visitor policies when only paying patients were allowed to have visitors.1
Finally, there is a paucity of reporting for COVID-19 transmission in the context of altering hospital visitor policies and the body of literature is mostly of limited quality. Further retrospective, but importantly prospective or randomized studies, are needed to clarify the risks and benefits associated with limiting hospital visitors. In the meantime, it is prudent to take a patient-centered and thoughtful approach to hospital visitor policies with freedom given to practicing physicians to grant exemptions as opposed to blanket rulings produced by administrators.
Strengths and Limitations
Strengths of our study include a systematic investigation of the available literature at a period of high policy turnover during the COVID-19 pandemic. Study parameters were prespecified in the protocol to reduce the risk of bias in accordance with accepted systematic review guidelines. Multiple authors independently completed each step to reduce noise among the otherwise heterogenous data. The most notable limitation was the inability to assess our primary outcome: the impact of visitor policies on COVID-19 transmission. Only 1 included study reported COVID-19 transmission, which was in the context of transmission from mother to newborn.46 Therefore, it is difficult to comment on whether restriction of hospital visitors significantly reduced the spread of COVID-19 infection. Second, our analysis was limited by the lack of reporting of COVID-19 status in study participants and pertinent details about the visitor policies in place. This may be due to fluid policies in the face of a rapidly evolving pandemic; however, a few investigators used this as an advantage to perform cohort studies. Notably, these retrospective cohort studies compared groups of patients pre- and postimplementation of visitor policy.21 , 29 , 30 , 38 Potential downsides to these retrospective studies include biases related to the selection of subjects, recall bias, and confounding factors given lack of randomization.51 Additionally, 2 prospective cohort studies had relatively small sample sizes and only 1 assessed COVID-19 transmission.31 , 46 Finally, the ROBINS-I tool was used, and all authors agreed that these studies were of low quality.16 Together, the data reflect an early, developing literature exploring the efficacy of policy changes in the face of a challenging pandemic.
Acknowledgments
The authors thank Jeanette Iness and Martin Iness for their comments.
Footnotes
Funding: Virginia Commonwealth University C. Kenneth and Dianne Wright Fellowship for Translational Research (ANI, 2020-2021), National Cancer Institute of the National Institutes of Health (NIH) Ruth L. Kirschstein National Research Service Award F30 Fellowship F30CA221004 (ANI, 2018-2021) and 5F30AR076221-02 (JOA, 2020-2023), Arnold Ventures (VP).
Conflicts of Interest: VP reports research funding from Arnold Ventures; royalties from Johns Hopkins Press, MedPage, YouTube, and Substack; consulting fees from Optum Health; and Plenary Session podcast has individual Patreon donors. ANI, JOA, WS, CMI, MD, JC report none.
Authorship: All authors had access to the data and a role in writing this manuscript.
Supplementary Data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amjmed.2022.04.005.
Supplementary Material
Pediatric ICUs and Neonatal ICUs
As with adult populations, similar negative associations with visitor restrictions are present in the pediatric population. A cross-sectional survey of pediatric palliative care team members from 80 cities within 39 states in the United States found a high incidence of moral distress among health care providers. This distress was attributed to an inability to provide a desired level of care with existing rules and policies (21 of the reviewed open-ended responses) as well as bearing witness to patient and family suffering enhanced by the pandemic (18 responses). Finally, 6 responses described moral uncertainty and distress with medical decision-making in context of new rules and policies.47
Parent-infant closeness is also an integral aspect of newborn care (Supplementary Table 2 , available online). Skin-to-skin contact between parents and their newborns is known to positively impact parent well-being and infant development.52 , 53 Likewise, NICUs were historically associated with increased access of hospital visitors.2 This typical practice was called into question during the COVID-19 pandemic, especially when babies were born to mothers who tested positive for COVID-19. A prospective cohort study of this population (N = 21) found no COVID-19 transmission from mother to infant when separated after delivery. However, this came at the detriments of increased length of hospital stay and decreased breastmilk use.46 A cross-sectional survey of parents of newborns in a NICU in Italy found 54.5% of coded answers expressed dysphoric emotions, in particular sadness and anger associated with restrictive visitor policies. Another 25.5% expressed relational suffering, both as separation from the partner and newborn. A total of 20% of responses reflected adaptation strategies.41
Supplementary Table 2.
Summary of Included Studies Focused on the NICU and Peripartum Settings*
| First Author | Location | Design | Sample Size | Participants | Visitor Policy |
|---|---|---|---|---|---|
| NICU and PICU | |||||
| Romano-Keeler J46 | Illinois, United States | Prospective cohort | 21 | Newborns in the NICU, born to mothers who were COVID-19 positive | No visitors |
| Bembich S41 | Italy | Cross-sectional survey | 10 | Parents of newborns in the NICU (mothers: 90%) | Some restriction |
| Muniraman H45 | United States, UK | Cross-sectional survey | 224 | Parents of newborns in the NICU (mean age: 32, mothers: 70%) | Some restriction |
| Ashini A40 | Libya | Cross-sectional survey | 41 | Parents of neonate(s) in the NICU (mean age: 32, mothers: 75.5%) | Some restriction |
| Wiener L47† | United States | Cross-sectional survey | 207 | Pediatric palliative care team members from 80 cities within 39 states | Mixed |
| Peripartum/Labor and Delivery | |||||
| Cullen S43 | Ireland | Cross-sectional survey | 422 | Antenatal or postpartum patients | Some restriction |
| Mayopoulos G44 | Massachusetts, United States | Cross-sectional survey | 136 | Postpartum women (mean age: 32, 68 COVID-19 positive, suspected, or confirmed and 68 COVID-19 negative) | Some restriction |
| Bradfield Z42 | Australia | Cross-sectional survey | 620 | Midwives (age ≥18, female: 98.5%) | Mixed |
COVID-19 = coronavirus disease 2019; ICU = intensive care unit; NICU = neonatal intensive care unit; PICU = pediatric intensive care unit.
The “No visitors” designation was reserved for studies that explicitly stated no visitors were allowed under any circumstances, per hospital policy. Demographic information reported as available.
Study included both inpatient ward and ICU settings.
A larger-scale international (United States and UK) cross-sectional survey of 224 parents of newborns yielded similar findings.45 Here, a policy of one visitor restricted to a limited duration was associated with a higher proportion of concerns for lack of bonding and inability to participate in care. A policy of one visitor and unrestricted visit duration was associated with a lower proportion of concerns (P < .02). Respondents subject to policy restrictions of one parent for a limited time were more likely to perceive a mild or severe impact compared with those facing less austere restrictions (P = .02). Respondents from centers with more restrictive policies reported more negative impacts on breast feeding (P = .01). A survey from Libya (N = 41) echoed similar findings regarding breastfeeding and addressed some additional concerns.40 Almost half of parents (46.3%) did not receive status updates about their child, and 7 (17.1%) reported facing difficulties in bringing milk and other supplies to the hospital. Most mothers (85.4%) scored >10 on the Edinburgh Postnatal Depression Scale, which suggested a minor or major depression. Notably, 4 (9.8%) participants reported suicidal ideation.
Limitation of visitors, particularly parents, to the NICU is associated with negative impacts on parent-infant bonding and breastfeeding, overall counter to the well-being of the family unit. Only 1 of the included studies assessed COVID-19 transmission, and it was centered on vertical passage from mother to infant.46 It remains uncertain whether limiting parental visitation brings enough benefit via curbing COVID-19 transmission to offset the known detrimental effects of parent-child separation, especially with parents who are asymptomatic and negative for COVID-19 infection.54
Peripartum Period
Focusing on the maternal aspect of the mother-child unit, a cross-sectional survey of 422 women in Ireland investigated the impact of visitor restrictions on the peripartum experience (Supplementary Table 2, available online).43 Most (86.5%) women desired that their partner be permitted to visit while on antenatal ward. However, most (84.7%) also said they had enough staff support on postnatal ward. In contrast, a survey of 620 midwives in Australia revealed that 61.9% thought social distancing impacted their ability to care for mothers and endorsed feeling distressed by seeing women without support of their partners.42 However, some midwives expressed support for limited visitation because the lack of distraction by visitors gave them more dedicated time with new mothers to work on breastfeeding, for example. Finally, a cross-sectional survey (N = 136) specifically assessed the impact of visitor limitations on postpartum mothers with COVID-19 infection.44 Women positive for COVID-19 were 11 times as likely to have no visitors than women who were negative for COVID-19 and reported higher levels of pain in delivery, lower newborn weights, and more infant admissions to the NICU. Those with no visitors were 6 times as likely to report clinical acute stress in birth than women who were COVID positive and had visitors. Overall, the theme of frustration and sadness of limited access of hospital visitors is continued in the peripartum space.
References
- 1.The care of strangers: the rise of America's hospital system. Ann Intern Med. 1988 doi: 10.7326/0003-4819-109-11-931_2. [DOI] [Google Scholar]
- 2.Giganti AW. Families in pediatric critical care: the best option. Pediatr Nurs. 1998;24:261–265. [PubMed] [Google Scholar]
- 3.Peluso AM, Harnish BA, Miller NS, Cooper ER, Fujii AM. Effect of young sibling visitation on respiratory syncytial virus activity in a NICU. J Perinatol. 2015;35:627–630. doi: 10.1038/jp.2015.27. [DOI] [PubMed] [Google Scholar]
- 4.Vain NE. Nosocomial respiratory viral infection in the neonatal intensive care unit. Am J Perinatol. 2020;37:S22–S25. doi: 10.1055/s-0040-1714081. [DOI] [PubMed] [Google Scholar]
- 5.Bridges CB, Kuehnert MJ, Hall CB. Transmission of influenza: implications for control in health care settings. Clin Infect Dis. 2003;37:1094–1101. doi: 10.1086/378292. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC). Managing health care operations during COVID-19. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/facility-planning-operations.html. Accessed December 22, 2020.
- 7.Antommaria AHM, Monhollen L, Schaffzin JK. An ethical analysis of hospital visitor restrictions and masking requirements during the COVID-19 pandemic. J Clin Ethics. 2021;32:38–47. [PubMed] [Google Scholar]
- 8.Kemp CL. #MoreThanAVisitor: Families as “Essential” Care Partners During COVID-19. Gerontologist. 2021;61:145–151. doi: 10.1093/geront/gnaa161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daubman BR, Black L, Goodman A. Recognizing moral distress in the COVID-19 pandemic: lessons from global disaster response. J Hosp Med. 2020;15:696–698. doi: 10.12788/jhm.3499. [DOI] [PubMed] [Google Scholar]
- 10.Anderson-Shaw LK, Zar FA. COVID-19, moral conflict, distress, and dying alone. J Bioeth Inq. 2020;17:777–782. doi: 10.1007/s11673-020-10040-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Houghton C, Meskell P, Delaney H, et al. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;4 doi: 10.1002/14651858.CD013582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Munshi L, Evans G, Razak F. The case for relaxing no-visitor policies in hospitals during the ongoing COVID-19 pandemic. CMAJ. 2021;193:E135–E137. doi: 10.1503/cmaj.202636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- 14.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.CASP. Critical Appraisal Skills Programme (CASP). Available at: www.casp-uk.net. Accessed August 22, 2021.
- 16.Sterne JAC, Hernán MA, Reeves BC, et al. Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I): detailed guidance. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oxford Center for Evidence-Based Medicine. Levels of evidence. Available at: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009. Accessed December 22, 2020
- 18.Fritsch J, Petronio S, Helft PR, Torke AM. Making decisions for hospitalized older adults: ethical factors considered by family surrogates. J Clin Ethics. 2013;24:125–134. [PMC free article] [PubMed] [Google Scholar]
- 19.Rosa RG, Falavigna M, da Silva DB, et al. Effect of flexible family visitation on delirium among patients in the intensive care unit. JAMA. 2019;322:216–228. doi: 10.1001/jama.2019.8766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nassar AP, Besen BAMP, Robinson CC, Falavigna M, Teixeira C, Rosa RG. Flexible versus restrictive visiting policies in ICUs: A systematic review and meta-analysis. Crit Care Med. 2018;46:1175–1180. doi: 10.1097/CCM.0000000000003155. [DOI] [PubMed] [Google Scholar]
- 21.Kandori K, Okada Y, Ishii W, Narumiya H, Maebayashi Y, Iizuka R. Association between visitation restriction during the COVID-19 pandemic and delirium incidence among emergency admission patients: a single-center retrospective observational cohort study in Japan. J Intensive Care. 2020;8:90. doi: 10.1186/s40560-020-00511-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jeste DV, Eglit GML, Palmer BW, Martinis JG, Blanck P, Saks ER. Supported decision making in serious mental illness. Psychiatry. 2018;81:28–40. doi: 10.1080/00332747.2017.1324697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dieset I, Løvhaug L, Selle M, Kolseth A, Smeland OB, Færden A. Lessons learned from a cross-sectional survey among patients and staff in an acute psychiatric unit during an ongoing pandemic outbreak. Psychiatry Res. 2021;298 doi: 10.1016/j.psychres.2021.113779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Onwuteaka-Philipsen BD, Pasman HRW, Korfage IJ, et al. Dying in times of the coronavirus: An online survey among healthcare professionals about end-of-life care for patients dying with and without COVID-19 (the CO-LIVE study) Palliat Med. 2021;35:830–842. doi: 10.1177/02692163211003778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maaskant JM, Jongerden IP, Bik J, et al. Strict isolation requires a different approach to the family of hospitalised patients with COVID-19: a rapid qualitative study. Int J Nurs Stud. 2021;117 doi: 10.1016/j.ijnurstu.2020.103858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feder S, Smith D, Griffin H, et al. “Why couldn't I go in to see him?” Bereaved families’ perceptions of end-of-life communication during COVID-19. J Am Geriatr Soc. 2021;69:587–592. doi: 10.1111/jgs.16993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Azoulay E, Cariou A, Bruneel F, et al. Symptoms of anxiety, depression, and peritraumatic dissociation in critical care clinicians managing patients with COVID-19 a cross-sectional study. Am J Respir Crit Care Med. 2020;202:1388–1398. doi: 10.1164/rccm.202006-2568OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boulton AJ, Jordan H, Adams CE, Polgarova P, Morris AC, Arora N. Intensive care unit visiting and family communication during the COVID-19 pandemic: a UK survey. J Intensive Care Soc. 2021 doi: 10.1177/17511437211007779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Azad TD, Al-Kawaz MN, Turnbull AE, Rivera-Lara L. Coronavirus disease 2019 policy restricting family presence may have delayed end-of-life decisions for critically ill patients. Crit Care Med. 2021;49:e1037–e1039. doi: 10.1097/CCM.0000000000005044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Piscitello GM, Fukushima CM, Saulitis AK, et al. Family meetings in the intensive care unit during the coronavirus disease 2019 pandemic. Am J Hosp Palliat Med. 2021;38:305–312. doi: 10.1177/1049909120973431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cattelan J, Castellano S, Merdji H, et al. Psychological effects of remote-only communication among reference persons of ICU patients during COVID-19 pandemic. J Intensive Care. 2021;9:5. doi: 10.1186/s40560-020-00520-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen C, Wittenberg E, Sullivan SS, Lorenz RA, Chang YP. The experiences of family members of ventilated covid-19 patients in the intensive care unit: a qualitative study. Am J Hosp Palliat Med. 2021;38:869–876. doi: 10.1177/10499091211006914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Creutzfeldt CJ, Schutz REC, Zahuranec DB, Lutz BJ, Curtis JR, Engelberg RA. Family presence for patients with severe acute brain injury and the influence of the COVID-19 pandemic. J Palliat Med. 2021;24:743–746. doi: 10.1089/jpm.2020.0520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kennedy NR, Steinberg A, Arnold RM, et al. Perspectives on telephone and video communication in the intensive care unit during COVID-19. Ann Am Thorac Soc. 2021;18:838–847. doi: 10.1513/AnnalsATS.202006-729OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sasangohar F, Dhala A, Zheng F, Ahmadi N, Kash B, Masud F. Use of telecritical care for family visitation to ICU during the COVID-19 pandemic: an interview study and sentiment analysis. BMJ Qual Saf. 2021;30:715–721. doi: 10.1136/bmjqs-2020-011604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jeyabraba S. Optimising family communication during a pandemic: do video calls have a role? Intensive Care Med Exp. 2020 [Google Scholar]
- 37.Rose L, Yu L, Casey J, et al. Communication and virtual visiting for families of patients in intensive care during the COVID-19 pandemic: a UK national survey. Ann Am Thorac Soc. 2021;18:1658–1692. doi: 10.1513/AnnalsATS.202012-1500OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zeh RD, Santry HP, Monsour C, et al. Impact of visitor restriction rules on the postoperative experience of COVID-19 negative patients undergoing surgery. Surgery. 2020;168:770–776. doi: 10.1016/j.surg.2020.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Losurdo P, Paiano L, Samardzic N, et al. Impact of lockdown for SARS-CoV-2 (COVID-19) on surgical site infection rates: a monocentric observational cohort study. Updates Surg. 2020;762:1263–1271. doi: 10.1007/s13304-020-00884-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ashini A, Alsoufi A, Elhadi M. Parental perception of neonatal ICU visitation during the COVID-19 pandemic. Int J Gynecol Obstet. 2021;153:554–555. doi: 10.1002/ijgo.13650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bembich S, Tripani A, Mastromarino S, Di Risio G, Castelpietra E, Risso FM. Parents experiencing NICU visit restrictions due to COVID-19 pandemic. Acta Paediatr Int J Paediatr. 2021;110:940–941. doi: 10.1111/apa.15620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bradfield Z, Hauck Y, Homer CSE, et al. Midwives’ experiences of providing maternity care during the COVID-19 pandemic in Australia. Women and Birth. 2022;35:262–271. doi: 10.1016/j.wombi.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cullen S, Doherty J, Brosnan M. Women's views on the visiting restrictions during COVID-19 in an Irish maternity hospital. Br J Midwifery. 2021;29 doi: 10.12968/bjom.2021.29.4.216. [DOI] [Google Scholar]
- 44.Mayopoulos G, Ein-Dor T, Li K, Chan S, Dekel S. Giving birth under hospital visitor restrictions: heightened acute stress in childbirth in COVID-19 positive women [preprint]. Res Sq. doi:10.21203/rs.3.rs-112882/v1, accessed June 12, 2021.
- 45.Muniraman H, Ali M, Cawley P, et al. Parental perceptions of the impact of neonatal unit visitation policies during COVID-19 pandemic. BMJ Paediatr Open. 2020;4 doi: 10.1136/bmjpo-2020-000899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Romano-Keeler J, Fiszbein D, Zhang J, et al. Center-based experiences implementing strategies to reduce risk of horizontal transmission of sars-cov-2: potential for compromise of neonatal microbiome assemblage. Gastroenterology. 2021 doi: 10.1016/s0016-5085(21)01299-3. [DOI] [Google Scholar]
- 47.Wiener L, Rosenberg AR, Pennarola B, Fry A, Weaver M. Navigating the terrain of moral distress: experiences of pediatric end-of-life care and bereavement during COVID-19. Palliat Support Care. 2021;19:129–134. doi: 10.1017/S1478951521000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Münch U, Müller H, Deffner T, et al. Recommendations for the support of suffering, severely ill, dying or grieving persons in the corona pandemic from a palliative care PERSPECTIVE: RECOMMENDATIONS of the German Society for Palliative Medicine (DGP), the German Interdisciplinary Association. Schmerz. 2020;34:303–313. doi: 10.1007/s00482-020-00483-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smith L, Medves J, Harrison MB, Tranmer J, Waytuck B. The impact of hospital visiting hour policies on pediatric and adult patients and their visitors. JBI Libr Syst Rev. 2009;7:38–79. doi: 10.11124/jbisrir-2009-181. [DOI] [PubMed] [Google Scholar]
- 50.Weiner HS, Firn JI, Hogikyan ND, et al. Hospital visitation policies during the SARS-CoV-2 pandemic. Am J Infect Control. 2021;49:516–520. doi: 10.1016/j.ajic.2020.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Geneletti S, Richardson S, Best N. Adjusting for selection bias in retrospective, case-control studies. Biostatistics. 2009;10:17–31. doi: 10.1093/biostatistics/kxn010. [DOI] [PubMed] [Google Scholar]
- 52.Flacking R, Lehtonen L, Thomson G, et al. Closeness and separation in neonatal intensive care. Acta Paediatr Int J Paediatr. 2012;101:1032–1037. doi: 10.1111/j.1651-2227.2012.02787.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.He FB, Axelin A, Ahlqvist-Björkroth S, Raiskila S, Löyttyniemi E, Lehtonen L. Effectiveness of the close collaboration with parents intervention on parent-infant closeness in NICU. BMC Pediatr. 2021;21:28. doi: 10.1186/s12887-020-02474-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Murray PD, Swanson JR. Visitation restrictions: is it right and how do we support families in the NICU during COVID-19? J Perinatol. 2020;40:1576–1581. doi: 10.1038/s41372-020-00781-1. [DOI] [PMC free article] [PubMed] [Google Scholar]