Summary
Background
Low- and middle-income countries (LMICs) bear a disproportionately higher burden of Cardiovascular Disease (CVD). Team-based care approach adds capacity to improve blood pressure (BP) control. This updated review aimed to test team-based care efficacy at different levels of hypertension team-based care complexity.
Methods
We searched PubMed, Embase, Cochrane, and CINAHL for newer articles on task-sharing interventions to manage hypertension in LMICs. Levels of tasks complexity performed by healthcare workers added to the clinical team in hypertension control programs were categorized as administrative tasks (level 1), basic clinical tasks (level 2), and/or advanced clinical tasks (level 3). Meta-analysis using an inverse variance weighted random-effects model summarized trial-based evidence on the efficacy of team-based care on BP control, compared with usual care.
Findings
Forty-three RCT articles were included in the meta-analysis: 31 studies from the previous systematic review, 12 articles from the updated search. The pooled mean effect for team-based care was a -4.6 mm Hg (95% CI: -5.8, -3.4, I2 = 80.2%) decrease in systolic BP compared with usual care. We found similar comparative reduction among different levels of team-based care complexity, i.e., administrative and basic clinical tasks (-4.7 mm Hg, 95% CI: -6.8, -2.2; I2 = 79.8%); and advanced clinical tasks (-4.5 mmHg, 95%CI: -6.1, -3.3; I2 = 81%). Systolic BP was reduced most by team-based care involving pharmacists (-7.3 mm Hg, 95% CI: -9.2, -5.4; I2 = 67.2%); followed by nurses (-5.1 mm Hg, 95% CI: -8.0, -2.2; I2 = 72.7%), dieticians (-4.7 mmHg, 95%CI: -7.1, -2.3; I2 = 0.0%), then community health workers (-3.3 mm Hg, 95% CI: -4.8, -1.8; I2 = 77.3%).
Interpretation
Overall, team-based hypertension care interventions consistently contributed to lower systolic BP compared to usual care; the effect size varies by the clinical training of the healthcare team members.
Funding
Resolve To Save Lives (RTSL) Vital Strategies, Danielle Cazabon, Andrew E. Moran, Yvonne Commodore-Mensah receive salary support from Resolve to Save Lives, an initiative of Vital Strategies. Resolve to Save Lives is jointly supported by grants from Bloomberg Philanthropies, the Bill & Melinda Gates Foundation, and Gates Philanthropy Partners, which is funded with support from the Chan Zuckerberg Foundation.
Keywords: Hypertension, LMIC, Team-based care
Research in context.
Evidence before this study
Studies have reported team-based care as an effected strategy that responds to physician shortages and improves hypertension care management outcomes. Team-based care has consistently been efficacious in lowering population mean blood pressure (BP) and improving its control. Based on these consistent findings in the literature, we developed a team-based care conceptual framework based on the World Health Organization (WHO) HEARTS Team-based care technical package “T” (team-based care) Module for implementation of team-based care interventions in member countries, especially Low-and Middle-Income Countries (LMICs). For this meta-analyses, we updated an existing review. We searched PubMed, Embase, Cochrane, and CINAHL until July 30, 2020, including reports from randomized control trials only. A meta-analysis using an inverse variance weighted random-effects model was used to summarize trial-based evidence on the efficacy of team-based care on BP control, compared with usual care.
Added value of this study
The inclusion of a Task Sharing Complexity Framework developed by our team is a novel contribution to the literature. To our knowledge, our study is the first to propose a framework for team-based hypertension care and applied to assess for differences in team-based care effect on BP-lowering according to the complexity of tasks being performed by healthcare workers. WHO published the HEARTS Team-based care technical package “T” (team-based care) Module, a technical package and module for implementing the intervention in member countries, particularly LMICs. Consequently, our study assessed the uptake and efficacy of team-based hypertension care and examined the validity of the newly developed Task Sharing Complexity Framework following the WHO recommendations.
Implications of all the available evidence
Team-based care interventions for hypertension lower systolic BP more than usual care. This effect appears to be slightly stronger when the team member added is more highly trained. Studies, including the current one, have reported that team-based care involving pharmacists as the new team member was associated with the most significant reduction in mean systolic BP.
Alt-text: Unlabelled box
Introduction
Globally, the prevalence of hypertension is increasing, particularly in low- and middle-income countries.1 Like other chronic diseases, treatment for hypertension is lifelong and requires a robust primary health care system to provide sustained treatment services to many patients for their remaining lifetimes. While the demand for hypertension services is increasing, the world is simultaneously facing a shortage of trained health workers. Healthcare worker density is higher in countries with a higher gross domestic product (GDP), while the contrasting state of severe shortage of workers in low-and-middle-income countries has become a pressing global health issue.2
Team-based care is a strategy that responds to physician shortages. Team-based care allocates service delivery efficiently at the community or primary care level among healthcare workers with diverse skills and training requirements3. It can involve shifting tasks from higher-level healthcare providers such as physicians to lower-level clinical staff or lay workers or expanding the levels of healthcare providers who can appropriately deliver specific health services.4,5 Sharing tasks with lower-level cadres of trained health care workers enables physicians to spend more time using their specialized training and skills, leading to expanded access to treatment interventions at the primary health care and community levels, and provide high-quality, cost-effective care to all patients according to need.4,6,7 Team-based care requires training healthcare workers such as nurses, community health workers, pharmacists, and dieticians to take on a number of services, including medication prescriptions and refills, algorithm-based treatment management, education and counseling, follow-up care, and organization of care. Task shifting is consistently efficacious in lowering population mean BP and improving BP control.8
In this study, we aimed to: 1) summarize the evidence on the efficacy of team-based care on BP control, compared with usual care, by updating a prior systematic review8, and 2) assess for differences in team-based care effect on BP-lowering according to the complexity of tasks being performed by healthcare workers and according to the training and job category of the new team member added.
Methods
Development of task sharing complexity framework
A team-based care conceptual framework was developed based on the World Health Organization(WHO) HEARTS Team-based care technical package “T” (team-based care) Module.19 The conceptual framework was peer-reviewed by clinical hypertension experts at Johns Hopkins University, the University of Alberta, Resolve to Save Lives, and the WHO. The framework aimed to outline three progressively more complex and training-intensive team-based care levels, describing tasks assigned to the new team member added to the health care team: administrative tasks only, basic clinical tasks with or without administrative tasks, and advanced clinical tasks with or without administrative and basic clinical tasks.
Search strategy and selection criteria
An electronic literature search strategy was developed based on a systematic review completed in 2019 on the effects of task-sharing on BP control8 (Supplementary material). The original review searched PubMed, Embase, Cochrane Library, and CINAHL with terms related to CVD, task sharing, and LMICs. The search covered the period from the inception of each database until December 28, 2018. For this study, the same search criteria were used in the updated database search in PubMed, Embase, CINAHL, and Cochrane databases between December 1, 2018, and July 30, 2020. This updated systematic review used similar inclusion and exclusion criteria as the 2019 systematic review; the criteria have been reported elsewhere.8 This updated search included only randomized control trials, whereas the original study included experimental studies in general (including randomized controlled trials, cluster randomized trials, quasi-experimental studies, and before-and-after designs).
Review and data extraction
A screening and data extraction tool, Covidence,9 was used to review data from the articles identified by the updated search criteria. One author conducted the initial title and abstract screening (O.O). For the next steps of the review process (full-text review, data extraction, risk of bias analysis), five articles were reviewed by three authors (with two authors serving as one reviewer) (A.A., D.C., O.O) to achieve concordance on article inclusion, data extraction and risk of bias assessment. Following the pilot at each step, the same three authors completed the reviews, and any discrepancies were discussed and resolved by a fourth reviewer (A.E.M.).
Once full-text screening was complete, data on country, region, study type, age group, intervention and control group descriptions, type of healthcare worker, and tasks performed were extracted from both pre-identified articles and the additional articles identified through the updated search.
The peer-reviewed conceptual framework (Figure 1) was used to categorize levels of team-based care for each of the study interventions. Interventions were categorized into three levels of team-based care: administrative tasks (level 1), basic clinical tasks (level 2), and/or advanced clinical tasks (level 3). Task sharing levels were dichotomized: all interventions that had tasks reaching level 2 were categorized into group 0 (i.e., interventions had tasks in level 2 only, or both levels 1 and 2), while group 1 contained interventions with tasks that reached level 3 (i.e., tasks in level 3 only, tasks in levels 2 and 3, and tasks in levels 1, 2 and 3).
Figure 1.
Team-based care conceptual framework for hypertension management.
Quality assessment
The quality and risk for bias and certainty of evidence were assessed using the Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) tool.10 The tool contains the following domains: risk of bias, indirectness of evidence, inconsistency, publication bias, the magnitude of effect, dose-response gradient, and assessment of plausible confounding. The overall GRADE certainty level was be rated as “very low”, “low”, “moderate”, or “high”.
Statistical analysis
For all included articles, summary descriptive statistics were estimated. A meta-analysis summarized BP-lowering effect across the trials using an inverse variance weighted random-effects model with calculated weights for each study. The overall average estimates of mean difference in systolic BP change and 95% confidence intervals(CIs) were calculated.11,12 Net BP was obtained by calculating a difference in BP estimates between baseline and last follow-up time points for intervention and control groups, and then a difference of the BP changes between team-based care intervention and usual care groups (difference in differences). Variability across studies attributable to heterogeneity was characterized using I2 statistics. Cochran's Q statistic was used to tests subgroup interaction, and the chi-squared test was used to test differences in groups in the subgroup analyses. Statistical significance was set at p<0.05.
To assess for sources of heterogeneity, sensitivity analyses were performed by stratifying the articles by team-based care levels, healthcare worker cadre, sample size, WHO region, and follow-up duration. Using the leave-one-out method, the contribution of each study to the overall heterogeneity was assessed. The pooled mean systolic BP changes across all the studies, and the individual study effects were visualized using forest plots. Publication bias in the meta-analysis was detected qualitatively by visual inspection of funnel plots and quantitatively by the Egger linear regression test.13,14 To account for some of the publication bias detected in the subgroup analyses, the non-parametric trim-and-fill model was explored when there were at least 3 articles for pooling.15
To assess the effect of team-based care on BP-lowering after adjustment for study-level variables, meta-regression analyses were conducted. First, a univariable meta-regression was conducted to explore a dose-response relationship between progressively more complex team-based care level and mean systolic BP difference. Then, a multivariable meta-regression was conducted, adding potential causes of study-level variance, including average age, follow-up duration, baseline BP, and healthcare worker cadre as moderators in the model.16 The 10 data points per variable rule were applied for the univariable model and 20 per variable in the multivariable models in the meta-regression.17 All analyses were conducted in Stata Stata/IC 16.1.18
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of this manuscript.
Results
Conceptual framework
Following expert review and consensus, a final version of the conceptual framework was derived (Figure 1). The framework outlines three levels of complexity of hypertension tasks for healthcare workers: administrative tasks, basic clinical tasks, and advanced clinical tasks. The tasks in the framework are listed in order of complexity for health care workers such as nurses, pharmacists, or community health workers. Administrative tasks, such as scheduling and medication delivery, can be completed with limited clinical knowledge. Basic clinical tasks require a higher degree of clinical knowledge but can be performed independently of direct physician supervision or additional support. Advanced clinical tasks require the highest level of clinical knowledge and supervision or support. For example, a nurse could use a standard treatment protocol to initiate a patient on treatment or could use a phone application to video call a physician for advice on medication titration.
Updated literature search results
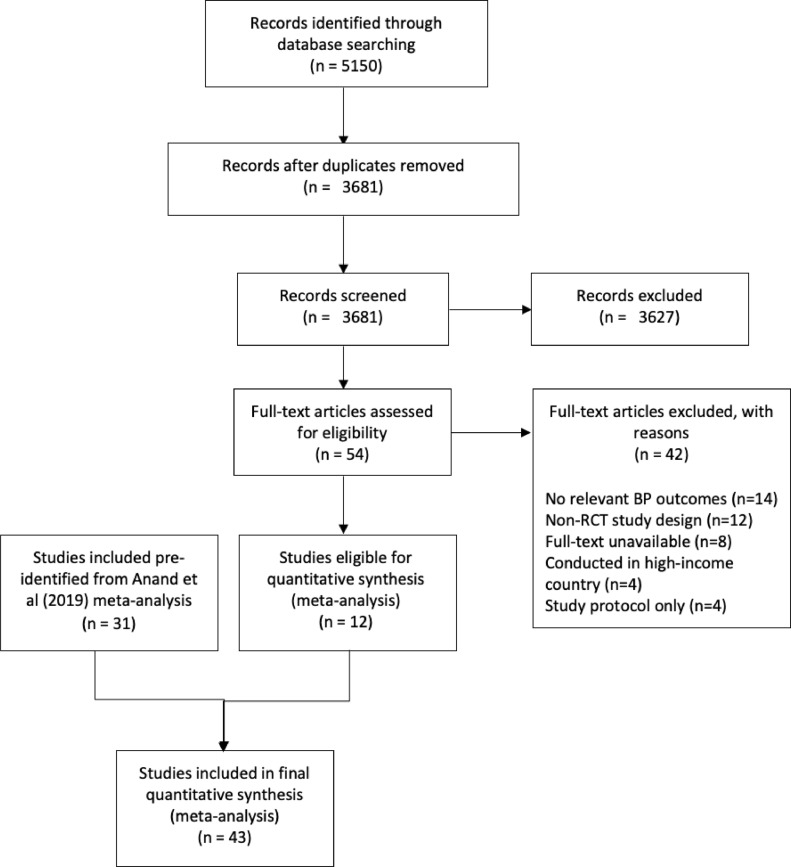
The meta-analysis of systolic BP included thirty-one articles selected in a previous systematic review,8 the search covered the period from the inception of each database until December 28, 2018. From the updated database search, which covered the period December 1, 2018, and July 30, 2020, 5,150 new articles were identified, and after removing duplicates, 3,691 titles and abstracts were screened for inclusion. Following title and abstract screening, 3,681 articles were excluded, and 54 studies were assessed for full-text eligibility screening. Full-text articles (n=42) were excluded for various reasons, which resulted in 12 new full-text articles included in the meta-analysis from the updated search (Figure 2). Forty-three articles were included in the updated meta-analysis; 31 studies from the previous systematic review and 12 articles from the updated search. We assessed the quality of evidence using the GRADE tool, 29 of the articles were judged to have a high level of evidence, while 14 of the articles were judged to have moderate evidence quality.
Figure 2.
PRISMA flowchart showing search results and article selection.
Note: BP- Blood Pressure; RCT- Randomized Controlled Trials
Study characteristics
Of the forty-three individual randomized controlled trials were included in the meta-analysis (Table 1), 11 (26%) of the studies were conducted in the Southeast Asia region, 8 (19%) in the Western Pacific region, 9 (21%) in Africa, 5 (12%) in the Americans, 1 (2%) in Europe, 4 (9%) in the Eastern Mediterranean region, and 5 (12%) in multiple countries and regions. Most studies were conducted in primary or community healthcare facilities (n=15). The articles were published between 2003 and 2020, and 19 (44%) were conducted in urban or suburban settings. Team-based care interventions for hypertension were delivered by community health workers in 16 (42%) of the studies, 4 (9%) were delivered by dieticians, 13 (30%) by nurses, and 8 (19%) by pharmacists. The mean intervention time was 9 (±6) months, ranging from two weeks to 24 months. The sample sizes for the individual studies ranged from 32 to 8642, with a total sum of 31,895 participants. The mean age of the participants was 57.4 (±6.1) years. Across the studies, mean baseline systolic BP was 142.3 (±11.3) mmHg.
Table 1.
Summary of Individual Randomized Controlled Trials Included in the Meta-analysis, by Intervention Levels based on the Team-Based Hypertension Care Framework.
| Author, year | Country | Type of health center or setting | Team-based care intervention intensity level |
Health worker type | Mean diff between SBP change in intervention and control groups (95% CI) | ||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | |||||
| Ali, 201620 | India & Pakistan | Outpatient diabetes clinics | Dietician | -5.4 (-8.22, -2.58) | |||
| Xavier, 201621 | India | Private, government, and non-profit hospitals | CHW | -2.4 (-5.77, 0.97) | |||
| Chao, 201222 | China | Community Health Centers | CHW | -3.95 (-5.18, -2.72) | |||
| Cappuccio, 200623 | Ghana | Villages | CHW | -3.1 (-8.65, 2.45) | |||
| de Souza, 201724 | Brazil | Primary Health Unit | CHW | -5 (-13.14, 3.14) | |||
| Saffi, 201325 | Brazil | Teaching Hospital | Nurse | -15 (-25.97, -4.03) | |||
| Zhu, 201826 | China | Community Health Center | Nurse | -5.5 (-12.26, 1.26) | |||
| Azami, 201827 | Iran | Hospital | Nurse | −2.30 (-5.84, 1.24) | |||
| Prabhakara, 201828 | India | Community Health Center | Nurse | 2.5 (-0.03, 5.03) | |||
| Hammad, 201129 | Jordan | Hospital | Pharmacist | -5.2 (-10.03, -0.37) | |||
| Jarab, 201230 | Jordan | Hospital | Pharmacist | -6.9 (-9.81, -3.99) | |||
| Jafar II, 202031 | Bangladesh, Pakistan & Sri-Lanka | Household and Government clinics | CHW | -0.70 (-2.04, 0.64) | |||
| Peiris, 201932 | India | Primary Healthcare Center | CHW | -0.17 (-1.61, 1.27) | |||
| Vedanthan, 201933 | Kenya | Community Health center | CHW | -3.40 (-6.26, -0.54) | |||
| Jain, 201834 | India | Tertiary Healthcare facility (Teaching Hospital) | CHW | 0.55 (-5.71, 6.81) | |||
| Wahab, 201735 | Nigeria | Tertiary Healthcare facility (Teaching Hospital) | Nurse | 4.03 (-17.29, 25.35) | |||
| Mendis, 201036 | China & Nigeria | Primary Health Center | CHW | -3.86 (-5.94, -1.78) | |||
| Neupane, 201837 | Nepal | Primary healthcare center, Subhealth posts, Urban healthcare centers | CHW | -3.62 (-8.76, 1.52) | |||
| Plaster, 201238 | Brazil | Community Health Center | Pharmacist | -10 (-11.73, -8.27) | |||
| Sookaneknun, 200439 | Thailand | Community pharmacy | Pharmacist | -5.65 (-10.3, -1) | |||
| Jayasuriya, 201540 | Sri Lanka | Primary Care center | Nurse | -7.70 (-17.18, 1.78) | |||
| Cakir, 200641 | Turkey | Hospital | Nurse | −10.10 (-12.76, -7.44) | |||
| Ma, 201442 | China | Community Health Center | Nurse | −7·81 (-15.58, -0.04) | |||
| Zhang, 201743 | China | Hospital | Nurse | −9·70 (-13.28, -6.12) | |||
| Sarfo, 201844 | Ghana | Hospital | Nurse | -1.50 (17.09, 14.09) | |||
| Sartorelli, 200745 | Brazil | Primary health care center | Dietician | -3.9 (-9.86, 2.06) | |||
| Mash, 201446 | South Africa | Community Health Centers | CHW | -6 (-13.45, 1.45) | |||
| Muchiri, 201647 | South Africa | Nurse managed clinics (PHC) | Dietician | 1.5 (-12.17, 15.7) | |||
| Goldhaber-Fiebert, 200348 | Costa Rica | Primary clinics | Dietician | -1 (-10.83, 8.83) | |||
| Huang, 201749 | China | Community Health Service (CHS) | Nurse | -5.28(-13.64, 3.08) | |||
| Khetan, 201950 | India | Household | CHW | -5.90 (-10.97, -0.83) | |||
| Zhai, 202051 | China | Community Health center | Pharmacist | -2.30 (-7.34, 2.74) | |||
| Wal, 201352 | India | Hospital | Pharmacist | -12.24 (-16.13, -8.35) | |||
| Jafar I, 200953 | Pakistan | Communities | CHW | 1 (-4.46, 6.46) | |||
| Tian, 201554 | China & India | Healthcare center | CHW | -2.7 (-5.08, -0.32) | |||
| He, 201755 | Nigeria | Community pharmacies | Pharmacist | -6.6 (-8.58, -4.62) | |||
| Jiang, 200756 | China | Hospital-initiated/Home-based | Nurse | -1.49 (-7.37, 4.39) | |||
| Joshi, 201957 | India | Primary Healthcare Center | CHW | -0.70 (-2.56, 1.16) | |||
| Schwalm, 201958 | Colombia & Malaysia | Community Health center | CHW | -11.40 (-14.89, -7.91) | |||
| Ojji, 202059 | Nigeria | Primary Healthcare Center | CHW | -5.00 (-13.07, 3.07) | |||
| Gamage, 202060 | India | Villages/Wards | CHW | -6.60 (-9.96, -3.24) | |||
| Zhao, 201261 | China | Hospital | Pharmacist | -6.6 (-10.65, -2.55) | |||
| Ogedegbe, 201862 | Ghana | Community Health Centers | Nurse | -3.30 (-7.92, 1.32) | |||
CHW – Community Health Workers.
95% CI: 95% Confidence Intervals.
Intervention Levels: Blue level: Administrative tasks that can be completed with limited clinical knowledge; Orange level: Tasks that require higher degree of clinical knowledge that can be performed mostly independently from direct physician supervision or additional support; Green level: Tasks that require the highest level of clinical knowledge, and supervision or support (e.g., standard treatment protocol, or phone call with a physician).
We examined components of the team-based hypertension care interventions and stratified these based on the team-based care framework. None of the studies included a level 1 only intervention (team-based care adding sharing of only administrative tasks). The majority of the intervention conducted were multilevel; twenty of the articles (46.5%) included both levels 1 & 2 team-based care tasks, 12 articles (28%) had team-based care level 2 tasks only, 5 articles (12%) included all three team-based care task levels (levels 1,2,3), and 4 articles (9%) had interventions comprising of team-based care task levels 2 & 3.
Meta-analysis
From the random-effects meta-analysis, the overall mean change in systolic BP with team-based care was -4.6 mm Hg (95% CI: -5.8, -3.4) compared with usual care (Figure 3; Z= -7.57, p< 0.001). We observed moderated to high heterogeneity across the included studies in the pooled analysis based on the I2 statistic (80.2%). The test of homogeneity of study-specific effect sizes was rejected (Chi2=236.4, p<0.001).
Figure 3.
Changes in Systolic Blood Pressure comparing team-based hypertension intervention group to usual care. Note: SBP – Systolic Blood Pressure; DBP – Diastolic Blood Pressure.
Meta-analysis by subgroup: levels of team-based care intervention
Since no studies included only level 1 interventions, two groups were created for comparison: studies that included team-based care levels 1 and 2 in varying combinations (i.e., levels 1 & 2 only, and 2 only), and studies that included level 3 team-based care tasks, with or without levels 1-2 (i.e., levels 1, 2, &3, and levels 2 & 3. After stratifying by team-based care intervention levels, the pooled mean systolic BP changes for studies that included team-based care levels 1 and 2 in various combinations was -4.7 mm Hg (95%CI: -6.8, -2.2; I2 = 79.8%) (Figure 4). For studies that included level 3 team-based care tasks, with or without levels 1-2, mean systolic blood pressure change was -4.5 mmHg (95%CI: -6.1, -3.3; I2 = 81%). The systolic BP reduction were similar between the team-based care complexity groups (Chi2=0.01, p=0.90).
Figure 4.
Subgroup analysis comparing Team-Based Hypertension Care by team-base care framework levels.
Note: SBP – Systolic Blood Pressure; DBP – Diastolic Blood Pressure.
Meta-analysis by subgroup: cadre of healthcare worker
Larger systolic BP reductions were seen when pharmacists delivered the intervention (-7.3mmHg, 95% CI: -9.2, -5.4; I2 = 67.2%); followed by nurses (-5.1 mm Hg, 95% CI: -8.0, -2.2; I2 = 72.7%), then dieticians (-4.9 mmHg, 95%CI: -7.1, -2.3; I2 = 0.0%), then CHW (-3.3 mm Hg, 95% CI: -4.8, -1.8; I2 = 77.3%) (Supplemental material).
Meta-analysis by subgroup: WHO regions
In the subgroup analyses by WHO regions, we observed a systolic blood pressure decrease of -2.88mm Hg (95% CI: -5.70, -0.06) for studies conducted in the Eastern Meditarranean; -4.43mm Hg (95% CI: -6.71, -2.15) for studies conducted in Southeast Asia; -5.08mm Hg (95% CI: -7.37, -2.78) for studies conducted in Africa; -5.85mm Hg (95% CI: -9.45, -2.24) for studies conducted in multiple regions; -8.22mm Hg (95% CI: -12.12, -4.32) for studies conducted in the Americas; and -10.10mm Hg (95% CI: -12.76, -7.44) for studies conducted in Europe (Supplemental material).
Meta-regression
In the univariable random effects meta-regression, we observed a decrease in mean systolic BP of -4.67mm Hg (95% CI: -6.08, -3.25; p<0.001; I2 = 80.1%) for interventions comprised of team-based care levels 1-2, and a -4.50 mm Hg (95% CI: -6.85, -2.14; p<0.001) decrease for interventions inclusive of team-based care levels 3. The mean difference in systolic BP decrease between these team-based care complexity levels was similar (p=0.976). For healthcare worker cadre, in comparison to community health workers, we observed a decrease of -3.81mm Hg in systolic blood pressure (95% CI: -6.60, -1.02; p=0.007; I2 = 75.6%) for interventions pharmacist-led interventions, and -1.55mm Hg systolic blood pressure decrease (95% CI: -4.31, 1.21; p=0.271) for nurse-led interventions.
After including potential effect measure modifiers of average age, follow-up duration, baseline BP, and healthcare cadre in the multivariable meta-regression analyses, mean systolic BP change for interventions inclusive of team-based levels 1-2 was -2.62 mm Hg (95% CI: -17.11, 22.34; p=0.795; I2 = 72.9%). For studies with intervention inclusive of task level 3, mean systolic BP change was -2.79 mm Hg (95% CI: -17.52, 23.10; p=0.788).
Assessment of publication bias
In the overall meta-analysis, the funnel plots for publication bias showed no evidence of bias based on the Egger regression-based test (Z =0.06, p=0.95) (Supplementary material). Within each group of team-based care levels, the funnel plots showed some asymmetry; however, the Egger's regression test did not indicate bias (Z=0.19, p=0.85) (Supplementary material). Similarly, in the subgroup analyses by healthcare worker cadre, there was some asymmetry in the funnel plots; however, the Egger's regression test did not indicate bias (Z=0.08, p=0.94) (Supplementary material). The asymmetry of the funnel plot in the subgroup analysis may be due to the presence of between-study variability rather than publication bias.
Discussion
Team-based care interventions for hypertension lower systolic BP more than usual care. Team-based care involving pharmacists as the new team member was associated with the largest reduction in mean systolic BP. In contrast, team-based care interventions involving CHWs had the smallest reduction in systolic BP. These results are consistent with the findings from the previous review and meta-analysis.8 There was no dose-response relationship between the level of increasing task complexity and BP reduction.
The overall results indicate that when team-based care is added to usual care, BP is further reduced in patients with hypertension. The lack of dose-response related to increasing non-physician health worker task complexity suggests that even when basic tasks are redistributed to a new non-physician team member, this, in turn, increases the capacity of more specialized members of the team to focus on the more complex tasks they are trained to do. For example, if a CHW receives training to measure the BP of patients, the nurse in that facility may have more time to take on titrating hypertension medications as per a treatment protocol, leaving the physician to focus on complex tasks managing complicated hypertension cases. The results suggest that increasing capacity in the team and sharing tasks, regardless of the complexity level, contributes positively to hypertension care. Alternately, the task complexity scale in the conceptual framework may be an overly simplistic construct; one cannot assess the function of the team by assessing the scope of tasks performed by one member of the team.
In contrast, we found a more robust effect on BP change when team-based care interventions were delivered by pharmacists, followed by nurses, dieticians, and CHWs. The dose-response observed based on healthcare worker cadre suggests that the addition of or redistribution of tasks to healthcare workers with more advanced training and experience of autonomy may be more effective in treating hypertension. This finding suggests that when more highly trained healthcare workers are added to a team or given additional responsibilities, it may tax the physician members of the team less because of less need for supervision of the new team members.
This meta-analysis has some limitations. First, there was a moderate to high heterogeneity in patient population, location, healthcare worker training, availability of supervision, intervention type, and primary outcomes of the articles reviewed. This heterogeneity limits quantitive comparison of the team-based care intervention levels by the effect sizes. Second, our conceptual framework could be limited in its utility for evaluating team-based care interventions or programs, since interventions components may overlap the intervention levels in the framework. Third, the original RCTs were not designed to compare effect sizes based on the categories of team-based care intervention level, as featured on our analysis; hence we recognize indirect comparisons as a limitation of our meta-analysis. Fourth, the pooled mean difference and our analysis may not have taken into account unmeasured confounders from the individual studies, however, we included average age, baseline BP, follow-up duration as potential effect measure modifiers in the models. In addition, the protocol for this updated review was not registered in a systematic review protocol registry. Despite these limitations, this study has several strengths. First, to our knowledge, this is the first study to propose a conceptual framework to be applied to team-based hypertension care. Between the time of publication of the previous review and now, the WHO published the HEARTS Team-based care technical package “T” (team-based care) Module, a technical package and module for implementation of the intervention in member countries, particularly LMICs.19 Our conceptual framework was developed in congruence with the WHO HEARTS module. Second, this study adds value to the literature on team-based care based; this meta-analysis is based on an existing review. Third, the analytic approach was a restrictive and inclusive meta-analysis that included meta-regression analyses to explore sources of heterogeneity and effect measure modification. Importantly, the subgroup meta-analysis was based on a comparison of the pooled effect sizes between the intervention levels of the conceptual framework, which was not the focus of the previously published review.
Team-based care succeeds beyond usual care in lowering BP in patients living with hypertension. This effect appears to be slightly stronger when the team member added is more highly trained. However, these well-trained healthcare personnel are often expensive. Effectiveness studies and economic evaluations of team-based care are needed to justify investment in the healthcare worker training and salary allocations needed to support team-based care on a broader scale.
Contributors
AEM, DC, YCM conceived the idea for the study; DC drafted the protocol. OO conducted the updated literature search. OO, DC, AA conducted the quality assessment, data extraction, and results synthesis, with AEM providing guidance through the process. OO conducted the meta-analysis, with guidance from AEM and YCM. DC, AA, OO drafted the initial draft of the manuscript; AEM, YCM provided substantial contribution and critical evaluation of the draft. PJ conceived the previous systematic review which was updated, reviewed manuscript draft and provided critical feedback. All authors contributed to the design, results interpretations, and critical revision of the manuscripts. All authors approved the final version for submission.
Data Sharing
Study data are available upon reasonable request.
Funding
Resolve To Save Lives (RTSL) Vital Strategies, Danielle Cazabon, Andrew E. Moran, Yvonne Commodore-Mensah receive salary support from Resolve to Save Lives, an initiative of Vital Strategies. Resolve to Save Lives is jointly supported by grants from Bloomberg Philanthropies, the Bill & Melinda Gates Foundation, and Gates Philanthropy Partners, which is funded with support from the Chan Zuckerberg Foundation. Panniyammakal Jeemon is supported by a DBT-Wellcome Trust India Alliance (IA) Senior Fellowship (IA/CPHS/20/1/505229).
Declaration of interests
The authors declare no conflict of interest.
Acknowledgments
We would like to acknowledge the following reviewers of the team-based care conceptual framework: Dr. Lawrence Appel, Dr. Yvonne Commodore-Mensah, Dr. George Pariyo, Dr. Kunihiro Matsushita, Dr. Cheryl R. Dennison Himmelfarb, and Dr. Anbrasi Edward; Johns Hopkins University; Dr. Norm Campbell, University of Calgary, Alberta; Dr. Doris Mugrditchian, World Health Organization. We also acknowledge Dr. Di Zhao, Johns Hopkins University School of Public Health, for providing feedback on the statistical analysis plan.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2022.101388.
Appendix. Supplementary materials
References
- 1.Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nature Reviews Nephrology. 2020:1–15. doi: 10.1038/s41581-019-0244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . No Health Without a Workforce; Geneva: 2013. A Universal Truth. [Google Scholar]
- 3.World Health Organization . workforce 2030; 2016. Global strategy on human resources for health. [Google Scholar]
- 4.World Health Organization . WHO; Geneva: 2017. Task sharing to improve access to Family Planning/Contraception. [Google Scholar]
- 5.World Health Organization . Geneva; 2008. Operations manual for delivery of HIV prevention, care and treatment at primary health centres in high-prevalence, resource-constrained settings: Edition 1 for fieldtesting and country adaptation. [PubMed] [Google Scholar]
- 6.Callaghan M, Ford N, Schneider H. A systematic review of task- shifting for HIV treatment and care in Africa. Hum Resour Health. 2010;8:8. doi: 10.1186/1478-4491-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . Geneva; 2008. Task Shifting Global Recommendations and Guidelines. [Google Scholar]
- 8.Anand TN, Joseph LM, Geetha AV, Prabhakaran D, Jeemon P. Task sharing with non-physician health-care workers for management of blood pressure in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Glob Health. 2019;7(6):e761–ee71. doi: 10.1016/S2214-109X(19)30077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Covidence systematic review software. Veritas Health Innovation. Melbourne, Australia.
- 10.Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction–GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology. 2011;64(4):383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 11.StataCorp . A Stata Press Publication StataCorp LLC; College Station, Texas: 2019. Stata Meta-Analysis Reference Manual. Release 16. [Google Scholar]
- 12.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 13.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Comparison of two methods to detect publication bias in meta-analysis. JAMA. 2006;295(6):676–680. doi: 10.1001/jama.295.6.676. [DOI] [PubMed] [Google Scholar]
- 15.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 16.Hox JJ MM, van de Schoot R. Routledge; Abingdon, UK: 2018. Multilevel Analysis: Techniques and Applications. Third ed. [Google Scholar]
- 17.Higgins JPT. Wiley-Blackwell; Hoboken, NJ: 2020. Cochrane Collaboration. Cochrane handbook for systematic reviews of interventions. Second edition. ed.pages cm p. [Google Scholar]
- 18.StataCorp. Stata . StataCorp LLC; TX: 2021. Release 16. Statistical Software. College Station. [Google Scholar]
- 19.World Health Organisation HEARTS: technical package for cardiovascular disease management in primary health care: team-based care. Geneva. 2018 [Google Scholar]
- 20.Ali MK, Singh K, Kondal D, et al. Effectiveness of a Multicomponent Quality Improvement Strategy to Improve Achievement of Diabetes Care Goals: A Randomized, Controlled Trial. Ann Intern Med. 2016;165(6):399–408. doi: 10.7326/M15-2807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xavier D, Gupta R, Kamath D, et al. Community health worker-based intervention for adherence to drugs and lifestyle change after acute coronary syndrome: a multicentre, open, randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4(3):244–253. doi: 10.1016/S2213-8587(15)00480-5. [DOI] [PubMed] [Google Scholar]
- 22.Chao J, Wang Y, Xu H, et al. The effect of community-based health management on the health of the elderly: a randomized controlled trial from China. BMC Health Serv Res. 2012;7;12:449. 10.1186/1472-6963-12-449. PMID: 23217036; PMCID: PMC3537545. [DOI] [PMC free article] [PubMed]
- 23.Cappuccio FP, Kerry SM, Micah FB, Plange-Rhule J, Eastwood JB. A community programme to reduce salt intake and blood pressure in Ghana [ISRCTN88789643] BMC Public Health. 2006;6:13. doi: 10.1186/1471-2458-6-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Souza CF, Dalzochio MB, Zucatti ATN, et al. Efficacy of an education course delivered to community health workers in diabetes control: A randomized clinical trial. Endocrine. 2017;57(2):280–286. doi: 10.1007/s12020-017-1352-z. [DOI] [PubMed] [Google Scholar]
- 25.Saffi MA, Polanczyk CA, Rabelo-Silva ER. Lifestyle interventions reduce cardiovascular risk in patients with coronary artery disease: a randomized clinical trial. Eur J Cardiovasc Nurs. 2014;13(5):436-43. 10.1177/1474515113505396. Epub 2013 Sep 10. PMID: 24021286. [DOI] [PubMed]
- 26.Zhu X, Wong FKY, Wu CLH. Development and evaluation of a nurse-led hypertension management model: A randomized controlled trial. Int J Nurs Stud. 2018;77:171–178. doi: 10.1016/j.ijnurstu.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 27.Azami G, Soh KL, Sazlina SG, et al. Effect of a Nurse-Led Diabetes Self-Management Education Program on Glycosylated Hemoglobin among Adults with Type 2 Diabetes. J Diabetes Res. 2018;2018:4930157. 10.1155/2018/4930157. PMID: 30225268; PMCID: PMC6129337. [DOI] [PMC free article] [PubMed]
- 28.Prabhakaran D, Jha D, Prieto-Merino D, et al. Effectiveness of an mHealth-Based Electronic Decision Support System for Integrated Management of Chronic Conditions in Primary Care: The mWellcare Cluster-Randomized Controlled Trial. Circulation. 2018 doi: 10.1161/CIRCULATIONAHA.118.038192. [DOI] [PubMed] [Google Scholar]
- 29.Hammad EA, Yasein N, Tahaineh L, Albsoul-Younes AM. A randomized controlled trial to assess pharmacist- physician collaborative practice in the management of metabolic syndrome in a university medical clinic in Jordan. J Manag Care Pharm. 2011;17(4):295-303. 10.18553/jmcp.2011.17.4.295. PMID: 21534640. [DOI] [PMC free article] [PubMed]
- 30.Jarab AS, Alqudah SG, Mukattash TL, Shattat G, Al-Qirim T. Randomized controlled trial of clinical pharmacy management of patients with type 2 diabetes in an outpatient diabetes clinic in Jordan. J Manag Care Pharm. 2012;18(7):516–526. doi: 10.18553/jmcp.2012.18.7.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jafar TH, Gandhi M, de Silva HA, et al. A Community-Based Intervention for Managing Hypertension in Rural South Asia. N Engl J Med. 2020;382(8):717–726. doi: 10.1056/NEJMoa1911965. [DOI] [PubMed] [Google Scholar]
- 32.Peiris D, Praveen D, Mogulluru K, et al. SMARThealth India: A stepped-wedge, cluster randomised controlled trial of a community health worker managed mobile health intervention for people assessed at high cardiovascular disease risk in rural India. PLoS One. 2019;14(3) doi: 10.1371/journal.pone.0213708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vedanthan R, Kamano JH, DeLong AK, et al. Community Health Workers Improve Linkage to Hypertension Care in Western Kenya. Journal of the American College of Cardiology. 2019;74(15):1897–1906. doi: 10.1016/j.jacc.2019.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jain V, Joshi R, Idiculla J, Xavier D. Community health worker interventions in type 2 diabetes mellitus patients: Assessing the feasibility and effectiveness in Rural Central India. Journal of Cardiovascular Disease Research. 2018;9(3):127–133. [Google Scholar]
- 35.Wahab KW, Owolabi M, Akinyemi R, et al. Short-term pilot feasibility study of a nurse-led intervention to improve blood pressure control after stroke in Nigeria. J Neurol Sci. 2017;377:116–120. doi: 10.1016/j.jns.2017.04.005. [DOI] [PubMed] [Google Scholar]
- 36.Mendis S, Johnston SC, Fan W, Oladapo O, Cameron A, Faramawi MF. Cardiovascular risk management and its impact on hypertension control in primary care in low-resource settings: a cluster-randomized trial. Bull World Health Organ. 2010;88(6):412–419. doi: 10.2471/BLT.08.062364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Neupane D, McLachlan CS, Mishra SR, et al. Effectiveness of a lifestyle intervention led by female community health volunteers versus usual care in blood pressure reduction (COBIN): an open-label, cluster-randomised trial. Lancet Glob Health. 2018;6(1):e66-e73. 10.1016/S2214-109X(17)30411-4. PMID: 29241617. [DOI] [PubMed]
- 38.Plaster C, Melo D, Boldt V, Cassaro K, Lessa F, Boëchat G, et al. Reduction of cardiovascular risk in patients with metabolic syndrome in a community health center after a pharmaceutical care program of pharmacotherapy follow-up. Brazilian Journal of Pharmaceutical Sciences. 2012;48:435–446. [Google Scholar]
- 39.Sookaneknun P, Richards RM, Sanguansermsri J, Teerasut C. Pharmacist involvement in primary care improves hypertensive patient clinical outcomes. Ann Pharmacother. 2004;38(12):2023–2028. doi: 10.1345/aph.1D605. [DOI] [PubMed] [Google Scholar]
- 40.Jayasuriya R, Pinidiyapathirage MJ, Jayawardena R, et al. Translational research for diabetes self-management in Sri Lanka: a randomized controlled trial. Prim Care Diabetes. 2015;9(5):338-45. 10.1016/j.pcd.2015.01.014. Epub 2015 Feb 26. PMID: 25733343. [DOI] [PubMed]
- 41.Cakir H, Pinar R. Randomized controlled trial on lifestyle modification in hypertensive patients. West J Nurs Res. 2006;28(2):190-209; discussion 210-5. 10.1177/0193945905283367. PMID: 16513919. [DOI] [PubMed]
- 42.Ma C, Zhou Y, Zhou W, Huang C. Evaluation of the effect of motivational interviewing counselling on hypertension care. Patient Educ Couns. 2014;95(2):231–237. doi: 10.1016/j.pec.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 43.Zhang P, Hu YD, Xing FM, Li CZ, Lan WF, Zhang XL. Effects of a nurse-led transitional care program on clinical outcomes, health-related knowledge, physical and mental health status among Chinese patients with coronary artery disease: A randomized controlled trial. Int J Nurs Stud. 2017;74:34-43. 10.1016/j.ijnurstu.2017.04.004. Epub 2017 Apr 14. PMID: 28601691. [DOI] [PubMed]
- 44.Sarfo FS, Treiber F, Gebregziabher M, et al. Phone-based intervention for blood pressure control among Ghanaian stroke survivors: A pilot randomized controlled trial. Int J Stroke. 2019;14(6):630-638. 10.1177/1747493018816423. Epub 2018 Nov 22. PMID: 30465630. [DOI] [PubMed]
- 45.Sartorelli DS, Sciarra EC, Franco LJ, Cardoso MA. Beneficial effects of short-term nutritional counselling at the primary health-care level among Brazilian adults. Public Health Nutr. 2005;8(7):820-5. 10.1079/phn2005737. PMID: 16277797. [DOI] [PubMed]
- 46.Mash RJ, Rhode H, Zwarenstein M, et al. Effectiveness of a group diabetes education programme in under-served communities in South Africa: a pragmatic cluster randomized controlled trial. Diabet Med. 2014;31(8):987-93. 10.1111/dme.12475. Epub 2014 May 20. PMID: 24766179; PMCID: PMC4232864. [DOI] [PMC free article] [PubMed]
- 47.Muchiri JW, Gericke GJ, Rheeder P. Effect of a nutrition education programme on clinical status and dietary behaviours of adults with type 2 diabetes in a resource-limited setting in South Africa: a randomised controlled trial. Public Health Nutr. 2016;19(1):142–155. doi: 10.1017/S1368980015000956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goldhaber-Fiebert JD, Goldhaber-Fiebert SN, Tristan ML, Nathan DM. Randomized controlled community-based nutrition and exercise intervention improves glycemia and cardiovascular risk factors in type 2 diabetic patients in rural Costa Rica. Diabetes Care. 2003;26(1):24–29. doi: 10.2337/diacare.26.1.24. [DOI] [PubMed] [Google Scholar]
- 49.Huang YJ, Parry M, Zeng Y, Luo Y, Yang J, He GP. Examination of a Nurse-led Community-based Education and Coaching Intervention for Coronary Heart Disease High-risk Individuals in China. Asian Nurs Res (Korean Soc Nurs Sci) 2017;11(3):187–193. doi: 10.1016/j.anr.2017.07.004. [DOI] [PubMed] [Google Scholar]
- 50.Khetan A, Zullo M, Rani A, et al. Effect of a Community Health Worker-Based Approach to Integrated Cardiovascular Risk Factor Control in India: A Cluster Randomized Controlled Trial. Glob Heart. 2019;14(4):355–365. doi: 10.1016/j.gheart.2019.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhai P, Hayat K, Ji W, et al. Efficacy of Text Messaging and Personal Consultation by Pharmacy Students Among Adults With Hypertension: Randomized Controlled Trial. Journal of Medical Internet Research. 2020;22(5) doi: 10.2196/16019. N.PAG-N.PAG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wal P, Wal A, Bhandari A, Pandey U, Rai AK. Pharmacist involvement in the patient care improves outcome in hypertension patients. J Res Pharm Pract. 2013;2(3):123–129. doi: 10.4103/2279-042X.122386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jafar TH, Hatcher J, Poulter N, et al. Hypertension Research Group. Community-based interventions to promote blood pressure control in a developing country: a cluster randomized trial. Ann Intern Med. 2009;151(9):593-601. 10.7326/0003-4819-151-9-200911030-00004. PMID: 19884620. [DOI] [PubMed]
- 54.Tian M, Ajay VS, Dunzhu D, et al. A Cluster-Randomized, Controlled Trial of a Simplified Multifaceted Management Program for Individuals at High Cardiovascular Risk (SimCard Trial) in Rural Tibet, China, and Haryana, India. Circulation. 2015;132(9):815-24. 10.1161/CIRCULATIONAHA.115.015373. Epub 2015 Jul 17. PMID: 26187183; PMCID: PMC4558306. [DOI] [PMC free article] [PubMed]
- 55.He J, Irazola V, Mills KT, Poggio R, Beratarrechea A, Dolan J, et al. Effect of a Community Health Worker-Led Multicomponent Intervention on Blood Pressure Control in Low-Income Patients in Argentina: A Randomized Clinical Trial. JAMA. 2017;318(11):1016–1025. doi: 10.1001/jama.2017.11358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jiang X, Sit JW, Wong TK. A nurse-led cardiac rehabilitation programme improves health behaviours and cardiac physiological risk parameters: evidence from Chengdu, China. J Clin Nurs. 2007;16(10):1886-97. 10.1111/j.1365-2702.2007.01838.x. PMID: 17880478. [DOI] [PubMed]
- 57.Joshi R, Agrawal T, Fathima F, et al. Cardiovascular risk factor reduction by community health workers in rural India: A cluster randomized trial. Am Heart J. 2019;216:9–19. doi: 10.1016/j.ahj.2019.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Schwalm JD, McCready T, Lopez-Jaramillo P, et al. A community-based comprehensive intervention to reduce cardiovascular risk in hypertension (HOPE 4): a cluster-randomised controlled trial. Lancet. 2019;394(10205):1231–1242. doi: 10.1016/S0140-6736(19)31949-X. [DOI] [PubMed] [Google Scholar]
- 59.Ojji DB, Baldridge AS, Orji AI, et al. Feasibility and effect of community health worker support and home monitoring for blood pressure control in Nigeria: a randomised pilot trial. Cardiovascular journal of Africa. 2020;31(3):e4–e6. doi: 10.5830/CVJA-2019-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gamage DG, Riddell MA, Joshi R, et al. Effectiveness of a scalable group-based education and monitoring program, delivered by health workers, to improve control of hypertension in rural India: A cluster randomised controlled trial. PLoS Med. 2020;17(1) doi: 10.1371/journal.pmed.1002997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhao P-X, Wang C, Qin L, et al. Effect of clinical pharmacist's pharmaceutical care intervention to control hypertensive outpatients in China. Afr J Pharm Pharmacol. 2012;6 [Google Scholar]
- 62.Ogedegbe G, Plange-Rhule J, Gyamfi J, et al. Health insurance coverage with or without a nurse-led task shifting strategy for hypertension control: A pragmatic cluster randomized trial in Ghana. PLoS Med. 2018;15(5):e1002561. 10.1371/journal.pmed.1002561. PMID: 29715303; PMCID: PMC5929500. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.