Abstract
Background
The Clinical Frailty Scale (CFS) is increasingly used for clinical decision making in acute care but little is known about frailty after COVID-19.
Objectives
To investigate frailty and the CFS for post-COVID-19 follow-up.
Methods
This prospective multicentre cohort study included COVID-19 survivors aged ≥50 years presenting for a follow-up visit ≥3 months after the acute illness. Nine centres retrospectively collected pre-COVID-19 CFS and prospectively CFS at follow-up. Three centres completed the Frailty Index (FI), the short physical performance battery (SPPB), 30 s sit-to-stand test and handgrip strength measurements. Mixed effect logistic regression models accounting for repeated measurements and potential confounders were used to investigate factors associated with post-COVID-19 CFS. Criterion and construct validity were determined by correlating the CFS to other concurrently assessed frailty measurements and measures of respiratory impairment, respectively.
Results
Of the 288 participants 65% were men, mean (SD) age was 65.1 (9) years. Median (IQR) CFS at follow-up was 3 (2–3), 21% were vulnerable or frail (CFS ≥4). The CFS was responsive to change, correlated with the FI (r=0.69, p<0.001), the SPPB score (r=−0.48, p<0.001) (criterion validity) and with the St George’s Respiratory Questionnaire score (r=0.59, p<0.001), forced vital capacity %-predicted (r=−0.25, p<0.001), 6 min walk distance (r=−0.39, p<0.001) and modified Medical Research Council (mMRC) (r=0.59, p<0.001). Dyspnoea was significantly associated with a higher odds for vulnerability/frailty (per one mMRC adjusted OR 2.01 (95% CI 1.13 to 3.58), p=0.02).
Conclusions
The CFS significantly increases with COVID-19, and dyspnoea is an important risk factor for post-COVID-19 frailty and should be addressed thoroughly.
Keywords: COVID-19, respiratory infection
Key messagegs.
What is already known on this topic
Frailty increases the risk for adverse health outcomes and the Clinical Frailty Scale (CFS) is used to allocate heathcare resources in COVID-19, however determinants of post-COVID-19 frailty are unknown.
What this study adds
The CFS is a valid and responsive tool to assess post-COVID-19 frailty, and dyspnoea is the most important driver of post-COVID-19 frailty.
How this study might affect research, practice and/or policy
This study supports the implementation of the easy to administer CFS for post-COVID-19 care, and hopefully increases awareness for frailty in the post-COVID-19 setting.
Introduction
The pandemic caused by SARS CoV-2 is still the most critical ongoing global healthcare challenge. COVID-19 poses a risk for severe disease, hospitalisation and death particularly for older adults and individuals with chronic diseases.1 2 In addition to the acute threat of COVID-19, evidence on residual symptoms, impairment of pulmonary and physical function several months after COVID-19 is emerging.3 4
Frailty reflects a persons’ functional age, which correlates with the propensity for adverse health outcomes when faced with an acute stressor.5 In the general population and in patients with chronic diseases, frailty is associated with poor quality of life and an increased risk for frequent hospitalisations and early mortality.6–8 Several tools for the assessment of frailty are available but no consensus exists on an established reference standard for clinical practice.9 The Clinical Frailty Scale (CFS) has been discussed as a potential tool to allocate healthcare resources, and has been integrated in decision trees, for example, for intensive care admission in older patients with COVID-19.10 The CFS predicts in-hospital mortality in patients of all ages with COVID-19,11 12 and specifically in older adults the CFS was associated with 30-day mortality independent of age, sex, social deprivation and ethnicity.13
While previous studies have established the role of the CFS to estimate short-term outcomes of acute COVID-19, the CFS has not been validated for post-COVID-19 follow-up yet.
We aimed to investigate the impact of COVID-19 on frailty, identify determinants of post-COVID-19 frailty and assess validity of the CFS in a prospective observational cohort of COVID-19 survivors presenting for follow-up ≥3 months after acute COVID-19.
Methods
Study design and participants
The national, multicentre, observational Swiss COVID-19 lung study is a prospective cohort study that includes adults who survived acute COVID-19 and presented with residual symptoms for follow-up assessments 3, 6 and 12 months after first COVID-19 symptoms. For practical reasons, it was not possible to adhere precisely to the follow-up schedule, and participants presenting for their first follow-up visit later than 3 months were still allowed to participate. Given the recruitment pattern of the study, more participants were hospitalised for COVID-19 and a smaller proportion were treated as outpatients. Details on the study have been published previously.3 For the current study, participants aged ≥50 years were included. The CFS was collected in all nine participating centres, while three centres recruited patients for a more extensive frailty assessment, which included the cumulative Frailty Index (FI) and the short physical performance battery (SPPB).
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Measurements
Clinical Frailty Scale
The CFS has been developed in geriatric medicine to estimate prognosis and to set care goals by summarising overall fitness or frailty. The 9-point scale ranges from 1 (very fit) to 4 (vulnerable/living with very mild frailty) to 9 (terminally ill).14 Physicians or nurses allocated CFS scores based on the clinical routine interviews with patients and caregivers using clinical judgement.10 15 Participants and their caregivers were asked about the participant’s activity and ability to function and move independently before COVID-19, and at the time of follow-up. Even though the concept of frailty and the CFS originate from geriatric medicine and the CFS is most frequently applied in the old and very old population, the importance of frailty is increasingly recognised in middle-aged adults suffering from chronic diseases that can accelerate functional ageing.6 16 17 The CFS has been previously validated for retrospective use in the context of older hospitalised patients.18
Frailty Index
The cumulative FI is a 40-item index assessing the presence or absence of 40 deficits related to independence and self-care or comorbidities. The FI is calculated as the proportion of items present divided by the total number of assessed items, expressed as a continuous variable between 0 and 1. An FI >0.21 denominates frail, 0.1–0.21 prefrail.8 19 The FI has been widely studied in the general elderly population, with a good prognostic validity in patients with age-related chronic lung diseases.6
Short physical performance battery
Physical frailty was assessed by the SPPB, which is a three-component test battery of lower extremity performance. Usual gait speed is assessed measuring the time needed to walk 4 m, lower extremity strength by the time needed to complete 5-repetition sit-to-stand (5R STS) and balance is tested in side-by-side, in semi-tandem and in tandem stand. A score from 0 to 4 is allocated to each measurement to a total score ranging from 0 to 12. A lower SPPB score signifies more severe physical frailty. An individual with SPPB ≤7 is considered physically frail, SPPB 8–9 signifies prefrailty and individuals with SPPB ≥10 are not physically frail. The SPPB is a widely accepted frailty assessment tool.20
Other measurements
Additional features of physical frailty were assessed by the 30 s sit-to stand test (30 s STS) and the measurement of handgrip strength. Furthermore, participants completed the St George’s Respiratory Questionnaire (SGRQ), the Fatigue Severity Scale (FSS), the Medical Research Council (mMRC) dyspnoea scale and a cough visual analogue scale (VAS). Further details are provided in the online supplemental material. Pulmonary functional tests, measurement of carbon monoxide diffusing capacity (DLCO) and 6 min walk tests were performed using established protocols.21–24
Assessment of validity
The ability of the CFS to respond to a specific health change was established by comparing CFS before COVID-19 and at the time of post-COVID-19 follow-up. Previously, the threshold for an observable change in health status has been estimated at 0.03 for the FI and at one-point for the CFS, respectively,15 however differences are more likely clinically significant for the distinction between fit (CFS <4) and vulnerable or frail (CFS ≥4) individuals.25 Criterion validity refers to the extent to which the CFS agrees with other measures of frailty. This was determined by correlating the CFS with other concurrently assessed frailty measurements (FI, SPPB total score, 4 m gait speed, 5R STS test, 30 s STS and handgrip strength). Construct validity reflects the expected behaviour of the CFS in context of other patient characteristics. Convergent validity was determined by correlating the CFS with 6 min walk distance (6MWD), partial pressure of oxygen in arterial blood (PaO2), pulmonary function tests, fatigue, cough, dyspnoea and health-related quality of life. Discriminant validity was investigated assuming that the CFS does not correlate with chronological age but adds an additional layer to ageing. Lastly, clinical validity was investigated by identification of clinical features associated with post-COVID-19 CFS.
Statistical analysis
Participant characteristics are reported as number (per cent), mean (SD) or median (IQR) depending on the distribution of the data.
To determine criterion and construct validity, the association between CFS and other measures of frailty as well as patient characteristics was assessed by Wilcoxon signed rank tests for categorical variables and by Spearman’s correlation for continuous variables. Pre-COVID-19 and post-COVID-19 CFS were compared using paired Wilcoxon signed rank tests.
Mixed effect logistic regression models were used to determine factors associated with post-COVID-19 CFS accounting for multiple follow-ups. In addition to the random effect for patient, fixed effects were added to adjust for potential confounders with conceptual importance. The internal consistency of the 40 items of the FI was evaluated using Cronbach’s alpha, a value of >0.70 indicates an appropriate degree of internal consistency.26 A two-sided p<0.05 indicated statistical significance for all comparisons. Data were analysed using R V.4.1.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Participant characteristics and frailty at the first post-COVID-19 follow-up visit
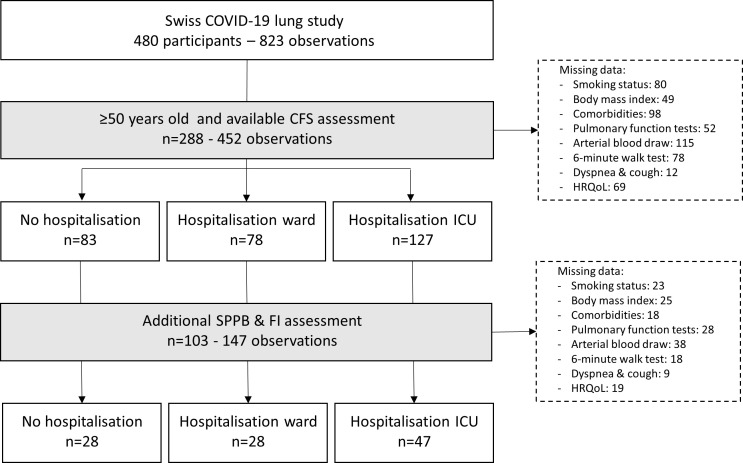
From 1 May 2020 to 1 July 2021, 480 participants were recruited to the Swiss COVID-19 lung study, of those 288 were included in the current CFS analyses, with 103 participants from 3 centres completing additional frailty assessments (FI and SPPB) (figure 1, table 1). Median (IQR) time from first COVID-19 symptoms to the first follow-up visit was 3.9 (3.2–5) months. One, two and three visits were available in 156, 100 and 32 participants, respectively. Of the 288 participants, 78 (27%) and 127 (44%) were hospitalised for COVID-19 on the ward and on the intensive care unit (ICU), respectively. The subgroup of participants who were hospitalised on the ICU included more men (72% vs 66% in the ward and 51% in the non-hospitalised subgroup) and more ever smokers (52% vs 33% in the ward and 17% in the non-hospitalised subgroup). Patients with ward hospitalisations were slightly older (mean 66.2 years) compared with patients with ICU hospitalisations (mean 64.9 years) and no hospitalisations (64.4 years). Patients who were hospitalised on the ICU had a higher body mass index (BMI), more frequent comorbidities, poorer lung function and physical performance, more dyspnoea, slightly worse quality of life at the first follow-up visit (online supplemental table S1).
Figure 1.
Study flow chart. CFS, Clinical Frailty Scale; FI, Frailty Index; HRQoL, health-related quality of life; ICU, intensive care unit; SPPB, short physical performance battery.
Table 1.
Participant characteristics at first COVID-19 follow-up in the entire cohort and in patients with extensive frailty assessment
| Entire cohort (CFS) (n=288) |
Extensive frailty assessment (n=103) | |
| Number (%), mean (SD) | ||
| Sex, men | 187 (65%) | 63 (61%) |
| Age, years | 65.1 (9) | 63 (8.7) |
| Ever smokers % | 109 (38%) | 40 (39%) |
| Smoked pack years* | 20 (10–31) | 20 (8–30) |
| Body mass index, kg/m2 | 28.7 (5.2) | 27.7 (5.2) |
| Hospitalisation for COVID-19 | ||
| No hospitalisation | 83 (29%) | 28 (27%) |
| Hospitalisation ward | 78 (27%) | 28 (27%) |
| Hospitalisation ICU | 127 (44%) | 47 (46%) |
| Comorbidities | ||
| Interstitial lung disease | 5 (1.7%) | 4 (4%) |
| COPD | 10 (3.5%) | 5 (5%) |
| Asthma | 29 (10%) | 11 (11%) |
| Diabetes | 40 (14%) | 13 (13%) |
| Pulmonary embolism | 8 (2.8%) | 5 (5%) |
| Pulmonary hypertension | 4 (1.4%) | 3 (3%) |
| Arterial hypertension | 106 (37%) | 43 (42%) |
| Gastro-oesophageal reflux | 22 (7.6%) | 11 (11%) |
| Cancer | 23 (8%) | 12 (12%) |
| Functional tests | ||
| TLC, L | 5.6 (1.5) | 5.8 (1.5) |
| TLC, %-predicted | 89 (19) | 93 (19) |
| FVC, L | 3.5 (1) | 3.7 (1) |
| FVC, %-predicted | 90 (18) | 92 (18) |
| FEV1, L | 2.8 (0.75) | 2.9 (0.75) |
| FEV1, %-predicted | 92.8 (18) | 92.8 (16) |
| DLCO, %-predicted | 78 (21) | 84 (23) |
| PaO2, mm Hg | 79 (13) | 82 (14) |
| 6MWD, m | 484 (110) | 507 (104) |
| 6MWD, %-predicted | 79.1 (13) | 95.7 (17) |
| O2 nadir on 6MWT | 90.3 (5.1) | 91.7 (5.3) |
| Symptoms | ||
| mMRC | 1.0 (0.9) | 0.91 (0.9) |
| Cough VAS | 0 (0–1) | 0 (0–1) |
| SGRQ total | 33.0 (20) | 34.4 (18) |
| SGRQ impact | 22.1 (20) | 21.7 (17) |
| SGRQ activity | 48.1 (26) | 49.8 (25) |
| SGRQ symptoms | 38.4 (24) | 39.4 (22) |
| Frailty | ||
| CFS pre-COVID-19 | 2 (1–2) | 2 (1.5–2) |
| CFS post-COVID-19 | 3 (2–3) | 3 (2–3.25) |
Data are presented as mean (SD), median (IQR) or frequency (percentage).
*Smoked pack years in ever smokers
CFS, Clinical Frailty Scale; COPD, chronic obstructive pulmonary disease; DLCO, diffusing capacity of the lung for carbon monoxide; FEV1, forced vital capacity in 1 min; FI, Frailty Index; FVC, forced vital capacity; ICU, intensive care unit; mMRC, modified Medical Research Council; 6MWD, 6 min walk distance; 6MWT, 6 min walk test; PaO2, partial pressure of oxygen in arterial blood; SGRQ, St George’s Respiratory Questionnaire; SPPB, short physical performance battery; TLC, total lung capacity; VAS, visual analogue scale.
bmjresp-2022-001227supp001.pdf (233.8KB, pdf)
The individual items of the FI are listed in the online supplemental table S2. Cronbach’s alpha of the 40 items of the FI was 0.82 (95% CI 0.87 to 0.93). The median (IQR) FI was 0.10 (0.05–0.18), 49% of the participants were not frail, 32% were prefrail and 19% were frail. The median (IQR) SPPB was 12 (10.2–12), accordingly 84% of the participants were not physically frail, 11% were prefrail and 5% were frail. Median (IQR) 4 m gait speed was 1.3 (1–1.3) m/s, mean (SD) grip strength was 36.4 (14.7) kg, the mean (SD) time for 5R STS was 10.9 (3.4) s and in 30 s a mean (SD) of 16 (7) STS repetitions were achieved.
The CFS showed criterion validity with correlations between the CFS and other measures of frailty at first post-COVID-19 follow-up (online supplemental figure S1). There was a strong correlation between the CFS and the FI (r=0.69, p<0.001), with a moderate correlation between the CFS and the SPPB score (r=−0.48, p<0.001), 4 m gait speed (r=−0.45, p<0.001) and 5R STS (r=0.48, p<0.001), and a week correlation with the 30 s STS (r=−0.33, p=0.005). CFS was not significantly correlated with grip strength (r=−0.16, p=0.22).
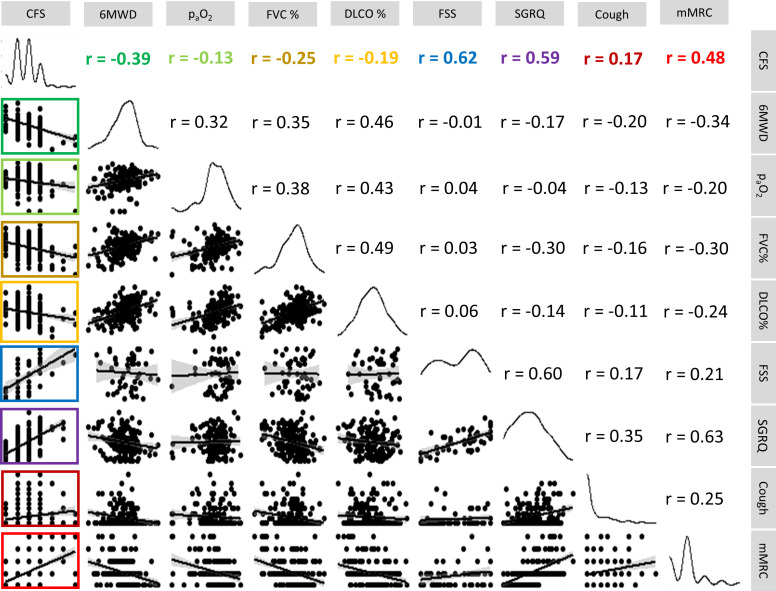
Figure 2 shows construct validity with correlations between the CFS and measures of respiratory and general impairment at first post-COVID-19 follow-up. The strongest correlations were observed between the CFS and the FSS (r=0.62, p<0.001), SGRQ score (r=0.59, p<0.001) and the mMRC dyspnoea scale (r=0.48, p<0.001). There was also a weak to moderate correlation with 6MWD (r=−0.39, p<0.001), forced vital capacity (FVC) and DLCO %-predicted (r=−0.25, p<0.001 and r=−0.19, p=0.008, respectively), and a weak correlation with PaO2 (r=−0.13, p=0.1) and cough VAS (r=0.17, p=0.006). Age was not correlated with the CFS (r=0.01, p=0.86).
Figure 2.
Construct validity of the Clinical Frailty Scale (CFS). DLCO %, diffusing capacity of the lung for carbon monoxide %-predicted; FSS, Fatigue Severity Scale; FVC %, forced vital capacity %-predicted; mMRC, modified Medical Research Council; PaO2, arterial partial pressure of oxygen in arterial blood; SGRQ, St George’s Respiratory Questionnaire; 6MWD, 6 min walk distance.
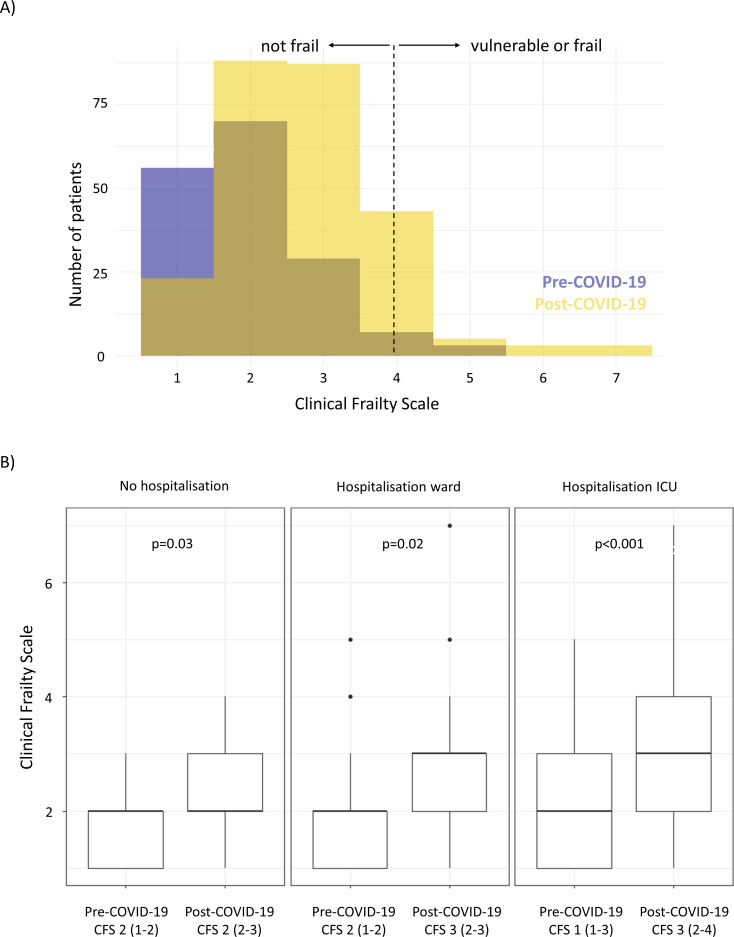
Change of the CFS from pre-COVID-19 to post-COVID-19
Overall, the median (IQR) pre-COVID-19 CFS was 2 (1–2), and at post-COVID-19 follow-up the median (IQR) CFS was 3 (2–3), with 6% and 21% of participants being considered vulnerable or frail (CFS ≥4) pre-COVID-19 and post-COVID-19, respectively (figure 3A). There was a slight but significant increase in frailty from the pre-COVID-19 state to the CFS at post-COVID-19 follow-up (median (IQR) 2 (1–2) to 2 (2–3), p=0.03) in participants without hospitalisation, with a larger CFS increase in participants who were hospitalised on the ward (pre-COVID-19 2 (1–2) to post-COVID-19 3 (2–3), p=0.02), or on the ICU (pre-COVID-19 1 (1–3) to post-COVID-19 3 (2–4), p<0.001) (figure 3B).
Figure 3.
Clinical Frailty Scale (CFS) pre-COVID-19 and post-COVID-19. Distribution of the CFS pre-COVID-19 and post-COVID-19 in the entire cohort (A) and change of the CFS stratified by hospitalisation (B). ICU, intensive care unit.
In an exploratory analysis, factors associated with an increase in CFS ≥1 were determined (online supplemental table S3). Comparable to the below findings from the cross-sectional analysis, more severe dyspnoea (higher mMRC) was significantly associated with a higher risk for CFS increase on unadjusted analysis (OR 1.95 (95% CI 1.24 to 3.07), p=0.004), and with adjustement for age, sex, follow-up time, hospitalisation, smoking status and BMI (OR 2.11 (95% CI 1.13 to 3.94), p=0.02). Furthermore, there was a significantly lower risk for CFS increase in patients with a higher 6MWD (OR 0.98 (95% CI 0.95 to 1.00), p=0.02). FVC %-predicted (OR 0.98 (95% CI 0.96 to 1.00), p=0.11) and other pulmonary function parameters were not significantly associated with CFS increase.
Determinants of post-COVID-19 CFS
For the investigation of post-COVID-19 determinants of CFS, all 452 follow-up observations (3–12 months after first COVID-19 symptoms) of the 288 patients were considered.
Clinical variables associated with vulnerability or frailty (CFS ≥4) at post-COVID-19 follow-up are shown in table 2. Patients who were hospitalised for COVID-19 had 4 times the odds for vulnerability/frailty (OR 4.01 (95% CI 0.98 to 16.3), p=0.05). Compared with women, men had 57% lower odds for frailty/vulnerability (OR 0.43 (95% CI 0.16 to 1.18)). Age and the most frequent comorbidities showed no significant association with vulnerability/frailty, whereas higher BMI was a risk factor for vulnerability/frailty (OR 1.10 (95% CI 0.99 to 1.21), p=0.05).
Table 2.
Unadjusted associations with vulnerability/frailty (CFS ≥4) post-COVID-19
| Unadjusted analysis* | ||
| OR (95% CI) | P value | |
| Sex, men | 0.43 (0.16 to 1.18) | 0.10 |
| Age, years | 1.01 (0.95 to 1.06) | 0.83 |
| Body mass index, kg/m2 | 1.10 (0.99 to 1.21) | 0.05 |
| Ever smokers % | 1.34 (0.45 to 4.02) | 0.60 |
| Hospitalisation | 4.01 (0.98 to 16.3) | 0.05 |
| Follow-up time, months | 0.94 (0.81 to 1.08) | 0.39 |
| Diabetes | 2.53 (0.56 to 11.4) | 0.23 |
| Arterial hypertension | 1.11 (0.41 to 3.05) | 0.84 |
| FVC, %-predicted | 0.96 (0.94 to 0.98) | 0.002 |
| DLCO, %-predicted | 0.96 (0.93 to 0.99) | 0.005 |
| 6MWD, %-predicted | 0.92 (0.88 to 0.96) | <0.001 |
| PaO2, mm Hg | 0.95 (0.90 to 1.00) | 0.046 |
| mMRC | 3.64 (2.20 to 6.03) | <0.001 |
| SGRQ, total | 1.11 (1.05 to 1.19) | <0.001 |
| Fatigue Severity Scale | 1.13 (0.99 to 1.29) | 0.08 |
For example, every 1% increase in FVC %-predicted is associated with a 4% lower odds and every one-point increase in mMRC is associated with 3.64 times the odds for vulnerability/frailty.
*Individual models accounting for multiple follow-up visits per patient (random effect)
6 min walk distance; CFS, Clinical Frailty Scale; DLCO, diffusing capacity of the lung for carbon monoxide; FVC, forced vital capacity; mMRC, modified Medical Research Council; PaO2, partial pressure of oxygen in arterial blood; SGRQ, St George’s Respiratory Questionnaire.
Higher FVC %-predicted, DLCO %-predicted, 6MWD %-predicted and PaO2 were significantly associated with lower risk for vulnerability/frailty in the analyses only accounting for multiple follow-ups per patient (table 2), and with adjustment for the potential confounders age, sex, BMI, smoking, hospitalisation for COVID-19 and follow-up time (table 3). Dyspnoea (mMRC) was significantly associated with vulnerability/frailty, which was robust to adjustment for the above confounders and additionally for FVC %-predicted and 6MWD %-predicted (fully adjusted OR 2.01 (95% CI 1.13 to 3.58), p=0.02). Similarly, the SGRQ was associated with vulnerability/frailty including with adjustment for above confounders (OR 1.06 (95% CI 1.03 to 1.10), p<0.001).
Table 3.
Adjusted associations with vulnerability/frailty (CFS ≥4) post-COVID-19
| OR (95% CI) | P value | |
| Adjusted for age, sex, BMI, smoking, hospitalisation and follow-up time* | ||
| FVC, %-predicted | 0.95 (0.92 to 0.98) | <0.001 |
| DLCO, %-predicted | 0.96 (0.93 to 0.99) | 0.005 |
| 6MWD, %-predicted | 0.92 (0.88 to 0.95) | <0.001 |
| PaO2, mm Hg | 0.93 (0.87 to 1.00) | 0.043 |
| mMRC | 3.73 (2.12 to 6.58) | <0.001 |
| SGRQ, total | 1.12 (1.05 to 1.19) | <0.001 |
| Additional adjustment for FVC %-predicted and 6MWD %-predicted† | ||
| mMRC | 2.01 (1.13 to 3.58) | 0.02 |
| SGRQ, total | 1.06 (1.03 to 1.10) | <0.001 |
For example, every 1% increase in FVC %-predicted is associated with a 5% lower odds and every one-point increase in mMRC is associated with 2 times the odds for vulnerability/frailty after accounting for the listed confounders.
*Individual models with random effect: patient; fixed effects: age, sex, follow-up time, hospitalisation, BMI, smoking.
†Random effect: patient; fixed effects: age, sex, follow-up time, hospitalisation, BMI, smoking, FVC %-predicted, 6MWD %-predicted.
6 min walk distance; CFS, Clinical Frailty Scale; DLCO, diffusing capacity of the lung for carbon monoxide; FVC, forced vital capacity; mMRC, modified Medical Research Council; PaO2, partial pressure of oxygen in arterial blood; SGRQ, St George’s Respiratory Questionnaire.
Discussion
This multicentre observational study demonstrates the CFS as a valid tool for the assessment of vulnerability and frailty at post-COVID-19 follow-up. With the clinically relevant increase in CFS from the pre-COVID-19 state to follow-up ≥3 months post-COVID-19, the CFS showed responsiveness, particularly to severe COVID-19 requiring hospitalisation. Furthermore, we demonstrate criterion validity of the CFS in reference to other frailty measurements, and construct validity when correlated with the severity of symptoms and pulmonary function impairment. Low FVC %-predicted, DLCO %-predicted, 6MWD %-predicted and PaO2 were significantly associated with post-COVID-19 vulnerability and frailty, with dyspnoea (mMRC) and SGRQ as the factors with the strongest association, independent from demographics, hospitalisation, and pulmonary function.
One-fifth of participants 4 months after acute COVID-19 were vulnerable or frail (CFS ≥4), in contrast two-thirds of elderly patients (mean age 80 years) who were in hospital for COVID-19 at the time of CFS assessment had a CFS ≥4.27 According to the FI, 19% of our population was frail and an additional 32% was prefrail. Using an equation derived from a representative Canadian general population, the median FI of 0.1 in this post-COVID-19 population corresponds to a biological age of 67 years, which is only slightly above this cohort’s chronological mean age of 63 years.28 In contrast, a cohort of patients with interstitial lung disease (mean age 69 years) had a median FI of 0.2.29 Overall, in this cohort only slightly more individuals were vulnerable or frail compared with the general population and frailty was less common than in patients with chronic respiratory disease.
Different frailty assessment tools typically cover different aspects of frailty,30 and in our study the CFS showed a stronger correlation with the FI than with the SPPB score. This confirms the CFS, like the FI, as a higher-level measure of functionality compared with the SPPB, which specifically measures physical frailty. Although the FI provides more granularity and has established prognostic validity across different populations,5 6 the CFS is simple to administer and easy to implement in clinical practice.31 Respiratory impairment is increasingly recognised at post-COVID-19 follow-up,3 with several variables of respiratory limitation showing a significant association with the CFS in this cohort. Previous findings suggest that dyspnoea is an important determinant of frailty in patients with chronic lung disease,32 and this study similarly shows double the odds of vulnerability or frailty with every one-point increase in mMRC, in a model adjusting for demographics, common risk factors, pulmonary function and physical performance. Furthermore, participants with a CFS increase from pre-COVID-19 to post-COVID-19 were also more likely to suffer from dyspnoea at post-COVID-19 follow-up. This relationship between dyspnoea and frailty emphasises the importance of assessing dyspnoea post-COVID-19. Hospitalisation is a risk factor for the progression of frailty.33 34 We confirm that COVID-19 survivors who were hospitalised had a CFS increase of one point on average, which is considered clinically meaningful.15 Together with the less pronounced CFS increase in those without hospitalisation, this shows that the CFS responds to major health issues as expected.
This study has some limitations. The Swiss lung COVID-19 cohort is not a representative sample of the population but includes COVID-19 survivors who were still symptomatic at least 3 months after the acute disease. Consequently, our proportion of frail individuals does not reflect post-COVID-19 prevalence of frailty in the general population. However, the validation of the CFS in individuals with and without hospitalisation for acute COVID-19 ensures generalisability of our findings to populations of different COVID-19 severities. The pre-COVID-19 CFS assessment was retrospective, and although this approach has been validated previously,18 there is a potential for recall bias. Unfortunately, the number of missing CFS information pre-COVID-19 was high, and consequently our analysis of determinants of pre-COVID-19/post-COVID-19 change was only exploratory. We choose the FI and SPPB as reference standards for the CFS validation, even though the comprehensive geriatric assessment is considered the gold standard for frailty assessment. However, a comprehensive geriatric assessment is time-consuming and considered not feasible in the typical clinical research scenario.35 We customised a 40-item FI for the current study with applications in German and French. The concept of the cumulative deficit accumulation allows for a collection of deficits that can vary between studies, with the assumption that the individual items are correlated with one another as well as with additional unmeasured deficits. A high internal consistency is therefore an important feature of the FI. With a Cronbach’s alpha of 0.87 (0.88 for the German FI, 0.80 for the French FI), this was demonstrated for this current FI.
In recent years, the CFS has been increasingly used in different populations and clinical contexts. By quantifying the clinicians overall ‘gestalt’ of the patient, the CFS can provide a valuable tool to communicate risks associated with decreasing physiological reserves.36 Particularly in old and very old patients, the CFS has been demonstrated to be reliable, valid and of high prognostic importance.37 38 Studies looking at the validity of the CFS in middle-aged adults are more sparse, but evidence is emerging that the CFS predicts outcomes also in patients younger than 50 years.39 Overall, considering chronological and biological and functional age is appropriate for risk assessments and management decisions in acute and chronic care settings.36 39–41 We found that age was not a determinant of post-COVID-19 frailty, which supports the added value of frailty also in the post-COVID-19 context. The COVID-19 pandemic has a large impact on day-to-day life of the general population, and particularly older adults experience the consequences of limited access to healthcare, social isolation and reduced physical activity.12 42 If frailty is identified, patients can benefit from comprehensive geriatric assessments, nutrition and physical activity interventions, mobile health-assisted interventions and pulmonary rehabilitation.43–47 Since frailty is a potentially preventable and reversible state, early detection of frailty is important, and particularly in the high-volume low-resource context of COVID-19 simple screening tools such as the CFS are urgently needed.
In summary, dyspnoea is the most important driver of post-COVID-19 frailty and should be addressed thoroughly, especially after severe COVID-19. The CFS shows validity and is responsive to hospitalisation for COVID-19. We hope that this study raises awareness of frailty in the post-COVID-19 setting and fosters the implementation of the CFS in clinical practice.
Acknowledgments
We thank our study coordinator Kurt De Jaegere, all study nurses and other staff who worked on this project, and all participants for their contribution.
Footnotes
Contributors: SG, MM, IM and MF-C designed the study. IM, MM, AR, P-OB, MHB, CC, CG, AL, BN, SO, LP, MP, Y-AQ, PMS, CvG, TKG, MF-C, SG contributed to data acquisition. IM, MM, MF-C and SG contributed to analysis of the data and drafting of the manuscript. All authors critically revised and finally approved the manuscript. SG is the guarantor of the study.
Funding: Lungenliga Bern Switzerland, the Johanna Dürmüller-Bol Foundation, Bern Centre for Precision Medicine of the University of Bern (Grant numbers not applicable).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study was approved by Swiss Ethics Committee (KEK 2020-00799). Participants gave informed consent to participate in the study before taking part.
References
- 1.Geng J, Yu X, Bao H, et al. Chronic diseases as a predictor for severity and mortality of COVID-19: a systematic review with cumulative meta-analysis. Front Med 2021;8:588013. 10.3389/fmed.2021.588013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020;584:430–6. 10.1038/s41586-020-2521-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guler SA, Ebner L, Aubry-Beigelman C, et al. Pulmonary function and radiological features 4 months after COVID-19: first results from the National prospective observational Swiss COVID-19 lung study. Eur Respir J 2021;57:2003690. 10.1183/13993003.03690-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sonnweber T, Sahanic S, Pizzini A, et al. Cardiopulmonary recovery after COVID-19: an observational prospective multicentre trial. Eur Respir J 2021;57:2003481. 10.1183/13993003.03481-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal 2001;1:323–36. 10.1100/tsw.2001.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guler SA, Kwan JM, Leung JM, et al. Functional ageing in fibrotic interstitial lung disease: the impact of frailty on adverse health outcomes. Eur Respir J 2020;55:1900647. 10.1183/13993003.00647-2019 [DOI] [PubMed] [Google Scholar]
- 7.Galizia G, Cacciatore F, Testa G, et al. Role of clinical frailty on long-term mortality of elderly subjects with and without chronic obstructive pulmonary disease. Aging Clin Exp Res 2011;23:118–25. 10.1007/BF03351076 [DOI] [PubMed] [Google Scholar]
- 8.Rockwood K, Song X, Mitnitski A. Changes in relative fitness and frailty across the adult lifespan: evidence from the Canadian national population health survey. CMAJ 2011;183:E487–94. 10.1503/cmaj.101271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blodgett J, Theou O, Kirkland S, et al. Frailty in NHANES: comparing the frailty index and phenotype. Arch Gerontol Geriatr 2015;60:464–70. 10.1016/j.archger.2015.01.016 [DOI] [PubMed] [Google Scholar]
- 10.Rockwood K, Theou O. Using the clinical frailty scale in allocating scarce health care resources. Can Geriatr J 2020;23:254–9. 10.5770/cgj.23.463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sablerolles RSG, Lafeber M, van Kempen JAL, et al. Association between clinical frailty scale score and hospital mortality in adult patients with COVID-19 (comet): an international, multicentre, retrospective, observational cohort study. Lancet Healthy Longev 2021;2:e163–70. 10.1016/S2666-7568(21)00006-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hewitt J, Carter B, Vilches-Moraga A, et al. The effect of frailty on survival in patients with COVID-19 (cope): a multicentre, European, observational cohort study. Lancet Public Health 2020;5:e444–51. 10.1016/S2468-2667(20)30146-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aw D, Woodrow L, Ogliari G, et al. Association of frailty with mortality in older inpatients with Covid-19: a cohort study. Age Ageing 2020;49:915–22. 10.1093/ageing/afaa184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173:489–95. 10.1503/cmaj.050051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Theou O, van der Valk AM, Godin J, et al. Exploring clinically meaningful changes for the frailty index in a longitudinal cohort of hospitalized older patients. J Gerontol A Biol Sci Med Sci 2020;75:1928–34. 10.1093/gerona/glaa084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lorenz DR, Mukerji SS, Misra V, et al. Predictors of transition to frailty in middle-aged and older people with HIV: a prospective cohort study. J Acquir Immune Defic Syndr 2021;88:518–27. 10.1097/QAI.0000000000002810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Venado A, Kolaitis NA, Huang C-Y, et al. Frailty after lung transplantation is associated with impaired health-related quality of life and mortality. Thorax 2020;75:669–78. 10.1136/thoraxjnl-2019-213988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stille K, Temmel N, Hepp J, et al. Validation of the clinical frailty scale for retrospective use in acute care. Eur Geriatr Med 2020;11:1009–15. 10.1007/s41999-020-00370-7 [DOI] [PubMed] [Google Scholar]
- 19.Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal 2001;1:323–36. 10.1100/tsw.2001.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994;49:M85–94. 10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- 21.Graham BL, Steenbruggen I, Miller MR, et al. Standardization of spirometry 2019 update. An official American thoracic Society and European respiratory Society technical statement. Am J Respir Crit Care Med 2019;200:e70–88. 10.1164/rccm.201908-1590ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Graham BL, Brusasco V, Burgos F, et al. 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur Respir J 2017;49:1600016. 10.1183/13993003.00016-2016 [DOI] [PubMed] [Google Scholar]
- 23.Holland AE, Spruit MA, Troosters T, et al. An official European respiratory Society/American thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J 2014;44:1428–46. 10.1183/09031936.00150314 [DOI] [PubMed] [Google Scholar]
- 24.Wanger J, Clausen JL, Coates A, et al. Standardisation of the measurement of lung volumes. Eur Respir J 2005;26:511–22. 10.1183/09031936.05.00035005 [DOI] [PubMed] [Google Scholar]
- 25.Kastora S, Kounidas G, Perrott S, et al. Clinical frailty scale as a point of care prognostic indicator of mortality in COVID-19: a systematic review and meta-analysis. EClinicalMedicine 2021;36:100896. 10.1016/j.eclinm.2021.100896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika 1951;16:297–334. 10.1007/BF02310555 [DOI] [Google Scholar]
- 27.Collins JT, Short R, Carter B, et al. The clinical frailty scale: estimating the prevalence of frailty in older patients hospitalised with COVID-19. The cope study. Geriatrics 2020;5:58. 10.3390/geriatrics5030058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mitnitski AB, Graham JE, Mogilner AJ, et al. Frailty, fitness and late-life mortality in relation to chronological and biological age. BMC Geriatr 2002;2:1. 10.1186/1471-2318-2-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guler SA, Kwan JM, Winstone TA, et al. Severity and features of frailty in systemic sclerosis-associated interstitial lung disease. Respir Med 2017;129:1–7. 10.1016/j.rmed.2017.05.012 [DOI] [PubMed] [Google Scholar]
- 30.Xue Q-L, Tian J, Walston JD, et al. Discrepancy in frailty identification: move beyond predictive validity. J Gerontol A Biol Sci Med Sci 2020;75:387–93. 10.1093/gerona/glz052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chin M, Voduc N, Huang S, et al. Practical lessons in implementing frailty assessments for hospitalised patients with COPD. BMJ Open Qual 2020;9:e000782. 10.1136/bmjoq-2019-000782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Milne KM, Kwan JM, Guler S, et al. Frailty is common and strongly associated with dyspnoea severity in fibrotic interstitial lung disease. Respirology 2017;22:728–34. 10.1111/resp.12944 [DOI] [PubMed] [Google Scholar]
- 33.Kojima G, Taniguchi Y, Iliffe S, et al. Transitions between frailty states among community-dwelling older people: a systematic review and meta-analysis. Ageing Res Rev 2019;50:81–8. 10.1016/j.arr.2019.01.010 [DOI] [PubMed] [Google Scholar]
- 34.Medina-Mirapeix F, Bernabeu-Mora R, García-Guillamón G, et al. Patterns, trajectories, and predictors of functional decline after hospitalization for acute exacerbations in men with moderate to severe chronic obstructive pulmonary disease: a longitudinal study. PLoS One 2016;11:e0157377. 10.1371/journal.pone.0157377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reflection paper on physical frailty: instruments for baseline characterisation of older populations in clinical trials. Available: https://www.ema.europa.eu/en/physical-frailty-instruments-baseline-characterisation-older-populations-clinical-trials [Accessed 12 Apr 2021].
- 36.Church S, Rogers E, Rockwood K, et al. A scoping review of the clinical frailty scale. BMC Geriatr 2020;20:393. 10.1186/s12877-020-01801-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Flaatten H, Guidet B, Andersen FH, et al. Reliability of the clinical frailty scale in very elderly ICU patients: a prospective European study. Ann Intensive Care 2021;11:22. 10.1186/s13613-021-00815-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haas LEM, Boumendil A, Flaatten H, et al. Frailty is associated with long-term outcome in patients with sepsis who are over 80 years old: results from an observational study in 241 European ICUs. Age Ageing 2021;50:1719–27. 10.1093/ageing/afab036 [DOI] [PubMed] [Google Scholar]
- 39.Darvall JN, Bellomo R, Paul E, et al. Routine frailty screening in critical illness: a population-based cohort study in Australia and New Zealand. Chest 2021;160:1292–303. 10.1016/j.chest.2021.05.049 [DOI] [PubMed] [Google Scholar]
- 40.Hewitt J, Moug SJ, Middleton M, et al. Prevalence of frailty and its association with mortality in general surgery. Am J Surg 2015;209:254–9. 10.1016/j.amjsurg.2014.05.022 [DOI] [PubMed] [Google Scholar]
- 41.Leclerc T, Donat N, Donat A, et al. Prioritisation of ICU treatments for critically ill patients in a COVID-19 pandemic with scarce resources. Anaesth Crit Care Pain Med 2020;39:333–9. 10.1016/j.accpm.2020.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yamada M, Kimura Y, Ishiyama D, et al. Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: a cross-sectional online survey. J Nutr Health Aging 2020;24:948–50. 10.1007/s12603-020-1501-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gephine S, Saey D, Grosbois J-M, et al. Home-Based pulmonary rehabilitation is effective in frail COPD patients with chronic respiratory failure. Chronic Obstr Pulm Dis 2022;9:15–25. 10.15326/jcopdf.2021.0250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nord M, Lyth J, Alwin J, et al. Costs and effects of comprehensive geriatric assessment in primary care for older adults with high risk for hospitalisation. BMC Geriatr 2021;21:263. 10.1186/s12877-021-02166-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Diamond JM, Courtwright AM, Balar P, et al. Mobile health technology to improve emergent frailty after lung transplantation. Clin Transplant 2021;35:e14236. 10.1111/ctr.14236 [DOI] [PubMed] [Google Scholar]
- 46.Negm AM, Kennedy CC, Thabane L, et al. Management of frailty: a systematic review and network meta-analysis of randomized controlled trials. J Am Med Dir Assoc 2019;20:1190–8. 10.1016/j.jamda.2019.08.009 [DOI] [PubMed] [Google Scholar]
- 47.Ng TP, Feng L, Nyunt MSZ, et al. Nutritional, physical, cognitive, and combination interventions and frailty reversal among older adults: a randomized controlled trial. Am J Med 2015;128:1225–36. 10.1016/j.amjmed.2015.06.017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjresp-2022-001227supp001.pdf (233.8KB, pdf)
Data Availability Statement
Data are available on reasonable request.