Abstract
The objective of this study was to evaluate the pharmacokinetics of indinavir in human immunodeficiency virus-infected children as part of a prospective, open, uncontrolled, multicenter study in The Netherlands. Human immunodeficiency virus type 1-infected children were monitored over 6 months of treatment with zidovudine (120 mg/m2 every 8 h [q8h]), lamivudine (4 mg/kg of body weight q12h), and indinavir (33mg/kg of metabolic weight [MW] q8h). Four weeks after the start of treatment, the steady-state pharmacokinetics of indinavir were determined by high-pressure liquid chromatography. If patients had an indinavir area under the concentration-time curve (AUC) of below 10 or above 30 mg/liter · h, a dose increase or a dose reduction was made and pharmacokinetic measurements were repeated 4 weeks later. Nineteen patients started with the dose of 33 mg/kg of MW q8h. The median AUC (range) was 10.5 (2.8 to 51.0) mg/liter · h. The median AUC (range) in 17 children treated with 50 mg/kg of MW q8h was 20.6 (4.1 to 38.7) mg/liter · h. Finally, five patients had a dose increase to 67 mg/kg of MW q8h, resulting in a median AUC (range) of 36.6 (27.2 to 80.0) mg/liter · h. After 6 months of treatment, there were 11 children with an AUC of below 20 mg/liter · h, of whom 5 (45%) had a detectable viral load, while this was the case in none of the 11 children with an AUC of higher than 20 mg/liter · h. We conclude that the optimal dose of indinavir in children to obtain drug exposure similar to that observed in adult patients is 50 mg/kg of MW q8h, which approximates 600 mg/m2 q8h. It would even be better to adjust the indinavir dose based on an AUC of greater than 20 mg/liter · h.
The advent of triple drug therapy, which includes two nucleoside reverse transcriptase inhibitors and one protease inhibitor or two nucleoside reverse transcriptase inhibitors and one nonnucleoside reverse transcriptase inhibitor, has markedly changed therapeutic options for human immunodeficiency virus (HIV)-infected individuals. So far, the large majority of clinical trials have been conducted with HIV type 1 (HIV-1)-infected adults, whereas the use of triple drug combination therapy in children has only recently been reported (8, 11, 13, 14, 17).
Differences in pharmacokinetics between children and adults should warn investigators that successful medical treatment in adults does not necessarily imply that this therapy will also be of benefit in children. Therefore, the use of new agents, such as the HIV-1 protease inhibitors, should be guided by detailed pharmacokinetic and pharmacodynamic evaluations when given for the first time to children. The goal of this approach is that efficacy and toxicity data should be similar to those reported in adults, or even better, if possible. With regard to HIV infection, suboptimal therapy should be detected as soon as possible, and interventions (e.g., dose modifications) should be applied immediately to prevent the emergence of drug resistance. We here report the pharmacokinetics of the HIV protease inhibitor indinavir in children participating in a prospective, open, uncontrolled clinical trial. A detailed analysis of the clinical, immunological, and virological effects is presented elsewhere (16).
MATERIALS AND METHODS
Patients.
HIV-1-infected children between the age of 3 months and 18 years with a viral load of greater than 5,000 copies/ml (Roche Amplicor) and/or a CD4 cell count below an age-specific threshold were included between April 1997 and July 1998. The study protocol was approved by the medical ethics committees of all participating hospitals, and written informed consent was obtained from all parents or legal guardians.
Pretreatment with zidovudine, didanosine, and/or zalcitabine was allowed. Patients were monitored over 6 months of treatment with zidovudine (120 mg/m2 every 8 h [q8h]), lamivudine (4 mg/kg of body weight q12h), and indinavir (33 mg/kg of metabolic weight [MW] q8h). The indinavir dose was based on the assumption that the use of MW (MW = body weight0.75) would better reflect the higher body clearance of drugs in children than in adults (9). An average adult weighing 70 kg has an MW of 24 kg (700.75 kg); the usual adult dose of indinavir is 800 mg q8h, which is equal to 33 mg/kg of MW (800 mg/24 kg of MW) q8h.
Indinavir was administered as 200- or 400-mg capsules (Crixivan) or as 150- or 300-mg capsules (prepared by the hospital pharmacy). If patients were not able to swallow the capsules, the indinavir capsules were opened and mixed with 5 to 10 ml of water. Patients and caregivers were instructed to take the indinavir capsules on an empty stomach or with a low-energy meal.
Pharmacokinetics.
Four weeks after the start of treatment, patients were admitted to the day-care unit of each hospital to determine the steady-state pharmacokinetics of indinavir. Patients took indinavir on an empty stomach, and blood samples were collected just before and 0.5, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 7, and 8 h after ingestion. Plasma was separated by centrifugation, and samples were stored at −20°C until analysis. Indinavir concentrations in plasma were determined by high-pressure liquid chromatography, as previously reported (1). In brief, 100 μl of plasma and 10 μl of an internal standard (125 μg of methylindinavir per ml dissolved in acetonitrile) were added to 400 μl of acetonitrile. Each cup was vortexed for 1 min and subsequently centrifuged for 5 min at 10,500 × g. The supernatant was evaporated to dryness. The residue was dissolved in the eluent, which consisted of acetonitrile-water (40:60, vol/vol). The water phase contained 50 mM phosphate buffer (pH 6) and 4 g of tetramethylammonium chloride per liter. The analytical column was an Inertsil ODS-2 C18 column. UV absorption was monitored at 210 nm. With this assay plasma indinavir concentrations of between 0.05 and 12.5 mg/liter can be measured. If the concentration in plasma was higher than 12.5 mg/liter, the sample was diluted 1:1 with drug-free plasma and reanalyzed. This dilution protocol was validated. At an indinavir concentration of approximately 1 mg/liter the accuracy of the assay is 97.7%, with an inter- and intraassay variations of 3.1 and 4.8%, respectively.
Pharmacokinetic parameters were calculated with Microsoft Excel 97 by non compartmental methods (5). The highest observed concentration in plasma was defined as Cmax, with the corresponding sampling time as Tmax. The terminal, log-linear period (log C versus T) was defined by the last data points (n > 2) by visual inspection. The absolute value of the slope (β/ln10) was calculated by least-squares analysis. The elimination half-life (t1/2) was calculated using the equation t1/2 = ln2/β. The area under the C-versus-T curve (AUC) was calculated by using the trapezoidal rule for t0 to t8. The target AUC0–8 of indinavir was based on adult values of 20 ± 10 mg/liter · h (Crixivan product manual, Merck & Co., Rahway, N.J.; unpublished observations). If patients had an indinavir AUC outside this range, a dose modification of 50 to 200% was made and pharmacokinetic measurements were repeated 4 weeks later.
Pharmacokinetic parameters in the children were compared to those in a population of 15 HIV-1-infected adults treated at the University Hospital Nijmegen. These patients had been using indinavir (800 mg q8h) as part of a triple-drug regimen for at least 4 weeks. The patients were randomly selected from the outpatient population to assess the population pharmacokinetics of indinavir in adults. Patients took 800 mg of indinavir on an empty stomach, and blood samples were collected just before and 0.5, 1, 1.5, 2, 2.5, 3, 4, 5, 6, 7, and 8 h after ingestion.
Pharmacokinetic-pharmacodynamic relationships.
The relationship between the concentrations of indinavir in plasma and its therapeutic effect was investigated in patients who completed the 6-month study. For those patients the last recorded AUC was related to the viral load response at 6 months. The group of patients was divided in two, based on an indinavir AUC higher or lower than the median value observed in adults (approximately 20 mg/liter · h), and for each group the number of patients who had an undetectable viral load (<500 copies/ml) was counted.
Statistics.
All statistical tests were performed using SPSS for Windows version 8.0 (SPSS Inc., Chicago, Ill.). The Mann-Whitney U test and Pearson's chi-square test were used for comparison of pharmacokinetic parameters between subgroups.
RESULTS
Inclusion.
A total of 27 patients were included in the prospective clinical trial. An 8-h pharmacokinetic curve was recorded at least once for 25 of them (12 males and 13 females). Two of the children stopped taking indinavir before a pharmacokinetic curve could be recorded at week 4. The median age of the 25 children was 6.0 years (range, 3 months to 16 years).
Pharmacokinetics of indinavir.
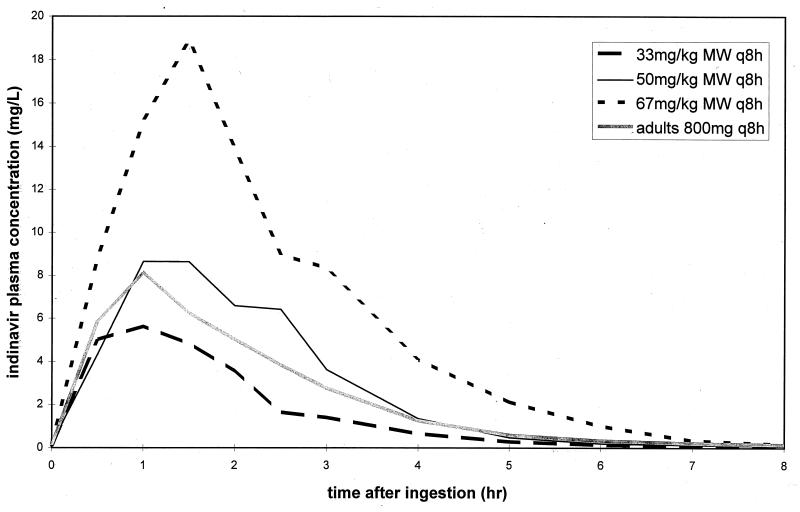
Nineteen patients started with the dose of 33 mg/kg of MW q8h. The median AUC0–8 (range) was 10.5 (2.8 to 51.0) mg/liter · h. Other pharmacokinetic parameters are listed in Table 1. For comparison, average values from a population of 15 HIV-infected adults receiving 800 mg of indinavir q8h are also listed in Table 1. Because the AUC was below 10 mg/liter · h in 11 of the children, the indinavir dose was increased to 50 mg/kg of MW q8h in these patients (150% dose). In addition, six other children started treatment with this higher dose. The median AUC0–8 (range) in these 17 children was 20.6 (4.1 to 38.7) mg/liter · h (Table 1). Finally, five patients had a dose increment to 67 mg/kg of MW q8h (200% dose), resulting in a median AUC0–8 (range) of 36.6 (27.2 to 80.0) mg/liter · h. The mean concentrations of indinavir in plasma in the three dosing groups of children as well as the reference data for adults are depicted in Fig. 1.
TABLE 1.
Pharmacokinetic parameters of indinavira
| Parameterb | Value for:
|
|||
|---|---|---|---|---|
| Children | Adults | |||
| Indinavir dose (q8h) | 33 mg/kg of MW | 50 mg/kg of MW | 67 mg/kg of MW | 800 mg |
| n | 19 | 17 | 5 | 15 |
| AUC0–8 (mg/liter · h) | 10.5 (2.8–51.0) | 20.6 (4.1–38.7) | 36.6 (27.2–80.0) | 19.1 (8.5–33.3) |
| CL/F [liters/(h · kg)] | 1.1 (0.3–4.6) | 0.9 (0.5–4.7) | 0.6 (0.4–1.2) | 0.6 (0.4–1.4) |
| V/F (liters/kg) | 2.3 (0.5–11.5) | 1.7 (0.5–6.8) | 1.1 (0.3–1.7) | 1.3 (0.6–3.2) |
| Cmax (mg/liter) | 6.4 (2.1–19.5) | 9.7 (2.3–17.0) | 17.1 (15.0–29.0) | 8.7 (3.6–15.8) |
| Tmax (h) | 1.0 (0.5–2.0) | 1.0 (0.5–2.5) | 0.8 (0.4–1.6) | 1.0 (0.5–2.0) |
| Cmin (mg/liter) | 0.04 (<0.02–0.26) | 0.07 (0.02–0.21) | 0.17 (0.05–0.38) | 0.13 (0.03–0.29) |
Data are median values, with ranges in parentheses.
CL, clearance; F, bioavailability; V, volume of distribution.
FIG. 1.
Mean concentrations of indinavir in plasma versus time for the three dose levels and adult data for comparison.
The weight-corrected apparent oral clearance of indinavir in children receiving the dose of 33 mg/kg of MW qh8 was used to investigate factors that were related to the huge variation in the AUC values (coefficient of variation, 85%). The median apparent oral clearance of indinavir (range) in the 19 children who started receiving indinavir at the dose of 33 mg/kg of MW q8h was 1.1 (0.3 to 4.6) liters/(h · kg). There was no statistically significant difference between boys (n = 8) and girls (n = 11) [1.6 (0.3 to 4.6) versus 1.1 (0.6 to 4.1) liters/(h · kg) (P = 0.96, Mann-Whitney U test)]. Although the variation in clearance values was much larger in younger children than in older children, children below the median age of 6 years (n = 9) had a significantly higher apparent oral clearance of indinavir than children 6 years and older (n = 10) [2.5 versus 1.0 liters/(h · kg) (P = 0.03, Mann-Whitney U test)]. The average adult value is 0.6 liter/(h · kg). There were no medications that were concomitantly used with indinavir that are known or suspected to have an influence on indinavir clearance.
Pharmacokinetic-pharmacodynamic relationships.
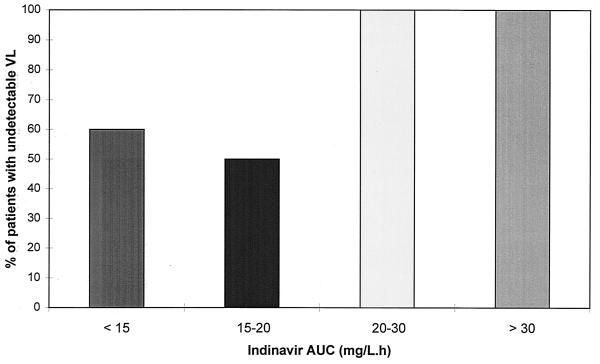
The relationship between the concentration of indinavir in plasma and the antiviral effect of the treatment regimen was investigated for the 22 children who completed 6 months of treatment and for whom the pharmacokinetic parameters were available for the dose that they were using at that time point. There was no statistically significant difference between the AUC, the Cmax, or the Cmin values in the patients who responded to therapy (defined as having a viral load of below 500 copies/ml) and those who did not respond to therapy (defined as having a viral load of above 500 copies/ml). However, there were 11 children with an AUC below 20 mg/liter · h, of whom 5 (45%) had a detectable viral load after 6 months of treatment, while this was the case in none of the 11 children with an AUC higher than 20 mg/liter · h (P = 0.01, Pearson chi-square test) (Fig. 2).
FIG. 2.
Relationship between the AUC of indinavir and the virological response after 6 months of treatment. The numbers of patients in the AUC groups are as follows: five, <15 mg/liter · h; six, 15 to 20 mg/liter · h; seven, 20 to 30 mg/liter · h; four, >30 mg/liter · h. VL, viral load.
DISCUSSION
The optimal dose of indinavir for HIV-infected children has not yet been established. The first phase I/II study was performed using three different formulations: two kinds of suspensions of indinavir base and dry-filled capsules of indinavir. Because of the poor absorption of indinavir from the suspensions, further research was conducted only with the capsules containing indinavir sulfate, now marketed as Crixivan capsules (8, 13, 17; R. P. Nelson, J. Sleasman, J. Cervia, G. Scott, R. Rutstein, R. McKinney, M. Nessly, L. Hawe, and B.-Y. Nguyen, Program Abstr. 6th Conf. Retroviruses Opportun. Infect., abstr. 425, 1999). Most children have been treated with an indinavir dose of 500 mg/m2 q8h, although this dose had to be reduced to 350 mg/m2 q8h in the phase I/II study because of a high incidence of nephrolithiasis in children receiving the higher dose (13).
We have evaluated three dose levels of indinavir in this study. We started with a dose of 33 mg/kg of MW q8h, but this resulted in low AUC values in a substantial proportion of the children. A dose increment to 50 mg/kg of MW q8h resulted in AUC values that were comparable to values observed in adults. Five children received the highest indinavir dose of 67 mg/kg of MW qh8, but this led to large increases in plasma indinavir concentrations and serious toxicity (nausea and vomiting) in these children. Therefore, the optimal dose appeared to be 50 mg/kg of MW q8h. After 6 months of treatment, 16 of the 25 patients still on indinavir treatment were now receiving this dose. Seventy percent of these children had reached the goal of an undetectable viral load (<500 copies/ml).
We have chosen to use the MW of a child to calculate the indinavir dose. The use of MW instead of normal body weight is based on the assumption that metabolic clearance in children is higher than that in adults, even when corrected for body weight. Although we had anticipated this higher oral clearance of indinavir in children, we made the incorrect assumption that we should use an adult of 70 kg to calculate the indinavir dose of 33 mg/kg of MW (800 mg/700.75 kg). For most medications, children 10 to 12 years old already receive the adult dose. In retrospect, it would have been better to use an estimated body weight of 45 kg of an 12-year-old child to calculate the indinavir dose: the MW is then 17.3 kg, and 800 mg divided by 17.3 kg of MW results in an indinavir dose of 46 mg/kg of MW q8h. This is close to the 50 mg/kg of MW that we have found in this study to be the optimal dose of indinavir. This dose results in a median AUC value of 20.6 mg/liter · h, which is just above the median adult value of 19 mg/liter · h. An indinavir dose of 500 mg/m2 q8h is now under investigation in a phase III clinical trial (Nelson et al., Program Abstr. 6th Conf. Retroviruses Opportun. Infect.). The two methods used to calculate pediatric doses, i.e., MW and body surface area, are based on similar physiological mechanisms. Because pediatricians are more familiar with dosing based on body surface area, this may be preferred over dosing based on MW. The 50 mg/kg of MW q8h that we found to be the optimal dose approximates a dose of 600 mg/m2 q8h.
A higher metabolic clearance of indinavir in children is not the only factor that may have caused the differences in clearance values between children and adults. Because indinavir is administered orally, impaired absorption of the drug may result in higher apparent oral clearances of indinavir. The reasons for possible malabsorption may be variable, but one of the mechanisms may be reduced solubility of indinavir at relatively high gastric pH values (10). It is known that children younger than 3 years have reduced gastric acid secretion (3), and this may result in lower indinavir exposure. However, peak concentrations of indinavir were achieved rapidly and were often higher than what is seen in adults. Furthermore, dose increments would not lead to increased concentrations of indinavir in plasma if drug solubility is problematic. In contrast, more-than-proportional increases in Cmax and AUC were seen (Table 1). This makes impaired absorption due to increased gastric pH unlikely.
Yet another possible explanation of lower plasma indinavir levels may be an increased volume of distribution. Young children have more total body water (80 to 90% of body weight) than adults (55 to 60% of body weight) (3), so water-soluble drugs, such as indinavir, will have a larger apparent volume of distribution in children than in adults (Table 1).
In adults there are a number of observations showing that the concentration of indinavir in plasma is related to the antiviral response (2, 6, 15). Therefore, instead of using a fixed dose regimen for each child, it seems logical to monitor the levels of indinavir in plasma shortly after the start of an indinavir-containing regimen and adjust the indinavir dose if necessary. For adults a trough level of 0.1 mg/liter has been proposed as the minimum effective concentration, which is equal to 75% of an average population value (2, 7). These values can be extrapolated to an AUC value of approximately 15 mg/liter · h (75% of 20), but our data show that for children this will not be enough. The AUC threshold in children appears to be 20 mg/liter · h, because none of the children with an AUC higher than 20 mg/liter · h had a detectable viral load after 6 months of treatment (Fig. 2). Not all of the children with an AUC below this threshold of 20 mg/liter · h can be considered nonresponders, but it is clear that the risk of virological failure is much greater with these lower AUC values. The fact that a higher AUC of indinavir is needed in children than in adults to have a virological response may be explained by the faster clearance of the drug in children than in adults. Table 1 illustrates that with similar AUCs in a child and an adult, a higher peak level and a lower trough level of indinavir are observed in the child. Therefore, if trough levels are important to obtain a durable antiviral response (2, 6, 15), children will need higher AUC values than adults to obtain similar trough levels. It is remarkable that in this group of pediatric patients the success of combination antiretroviral therapy can be explained to a large extent by the plasma concentrations of only one of the three components of the drug regimen. A similar observation was made for adults (2). Because the majority of children used zidovudine plus lamivudine as the nucleoside background and this may have influenced the observed relationship between indinavir AUC and virological outcome, it cannot be concluded from our data that the target AUC of indinavir is also valid for other nucleoside combinations.
There has been some concern that the risk of indinavir-induced nephrological toxicity (kidney stones, hematuria, and flank pain) in children may be higher than in adults. As noted above, for that reason the maximum indinavir dose was originally reduced to 350 mg/m2 in the first phase I/II trial of indinavir in the United States (13). Because urological toxicity is the result of precipitation of indinavir crystals and this is correlated with the level of indinavir in plasma (4), one would expect a high incidence of urological toxicity in our study because most children received an indinavir dose that is even higher than 500 mg/m2. However, this was not the case. None of the children developed kidney stones, and only three children developed hematuria, which resolved after dose interruption. An explanation of this low incidence of urological toxicity in our children cannot be given, but differences in the amount of fluid intake and climatological influences (higher temperatures in the United States than in The Netherlands) are some of the possible reasons.
In conclusion, we found that the optimal dose of indinavir in children to obtain drug exposure similar to that observed in adult patients is 50 mg/kg of MW q8h, which approximates 600 mg/m2 q8h. Using this dose, 70% of the children reached the goal of an undetectable viral load (<500 copies/ml) after 6 months of treatment, without the occurrence of serious adverse events. We also found that it would be even better to adjust the indinavir dose based on an AUC0–8 greater than 20 mg/liter · h, because in that situation 100% of the children could be regarded as responders.
ACKNOWLEDGMENTS
We thank Jackie Droste, Marga de Graaff, Mikel Maas, and Corrien Verwey for performing the indinavir analyses. Clementien Vermont, Gwenda Verweel, Menno Gaakeer, and Esther de Kleijn helped with blood sampling.
The clinical study was financially supported by the Dutch AIDS Foundation, Merck Sharp & Dohme, The Netherlands, and Glaxo Wellcome, The Netherlands.
Appendix
Members of the Dutch Study Group for Children with HIV-1 Infection are as follows: H. J. Scherpbier and F. de Wolf (Academic Medical Center, Amsterdam), F. Miedema and M. T. L. Roos (Central Laboratory of the Red Cross Blood Transfusion Service, Amsterdam); A. J. P. Veerman (Academic Hospital Free University, Amsterdam); J. J. M. Vossen (Leiden University Medical Center, Leiden); J. J. P. Schrander (Academic Hospital Maastricht, Maastricht); D. M. Burger and C. Weemaes (University Hospital Nijmegen, Nijmegen); R. de Groot, N. G. Hartwig, H. Hooijkaas, H. G. M. Niesters, A. D. M. E. Osterhaus, A. M. C. van Rossum, W. A. T. Slieker, M. H. Suur, and A. G. Vulto (Erasmus Medical Center Rotterdam, Rotterdam); and C. A. B. Boucher, S. P. M. Geelen, E. R. de Graeff-Meeder, T. F. W. Wolfs, and J. M. Zegers (Academic Hospital Utrecht, Utrecht).
REFERENCES
- 1.Burger D M, de Graaff M, Wuis E W, Koopmans P P, Hekster Y A. Determination of indinavir, an HIV-protease inhibitor, in human plasma by reversed-phase high-performance liquid chromatography. J Chromatogr B. 1997;703:235–241. doi: 10.1016/s0378-4347(97)00421-0. [DOI] [PubMed] [Google Scholar]
- 2.Burger D M, Hoetelmans R M W, Hugen P W H, Mulder J W, Meenhorst P L, Koopmans P P, Brinkman K, Keuter M, Dolmans W, Hekster Y A. Low plasma concentrations of indinavir are related to virological treatment failure in HIV-1 infected patients on indinavir-containing triple therapy. Antivir Ther. 1998;3:215–220. [PubMed] [Google Scholar]
- 3.Butler D R, Kuhn R J, Chandler M H H. Pharmacokinetics of anti-infective agents in paediatric patients. Clin Pharmacokinet. 1994;26:374–395. doi: 10.2165/00003088-199426050-00005. [DOI] [PubMed] [Google Scholar]
- 4.Dieleman J P, Gyssens I C, van der Ende M E, de Marie S, Burger D M. Urological complaints in relation to indinavir plasma concentrations in HIV-infected patients. AIDS. 1999;13:473–478. doi: 10.1097/00002030-199903110-00005. [DOI] [PubMed] [Google Scholar]
- 5.Gibaldi M. Biopharmaceutics and clinical pharmacokinetics. Philadelphia, Pa: Lea & Febiger; 1999. [Google Scholar]
- 6.Harris M, Durakovic C, Rae S, Raboud J, Fransen S, Shillington A, Conway B, Montaner J S G. A pilot study of nevirapine, indinavir and lamivudine among patients with advanced human immunodeficiency virus disease who have had failure of combination nucleoside therapy. J Infect Dis. 1998;177:1514–1520. doi: 10.1086/515317. [DOI] [PubMed] [Google Scholar]
- 7.Hsu A, Granneman G R, Cao G, Carothers L, Japour A, El-Shourbagy T, Dennis S, Berg J, Erdman K, Leonard J M, Sun E. Pharmacokinetic interaction between ritonavir and indinavir in healthy volunteers. Antimicrob Agents Chemother. 1998;42:2784–2791. doi: 10.1128/aac.42.11.2784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kline M W, Fletcher C V, Harris A T, Evans K D, Brundage R C, Remmel R P, Calles N R, Kirkpatrick S B, Simon C. A pilot study of combination therapy with indinavir, stavudine (d4T), and didanosine (ddI) in children infected with human immunodeficiency virus. J Pediatr. 1998;132:543–546. doi: 10.1016/s0022-3476(98)70039-3. [DOI] [PubMed] [Google Scholar]
- 9.Lave T, Coassolo C, Reigner B. Prediction of hepatic metabolic clearance based on interspecies allometric scaling techniques and in vitro-in vivo correlations. Clin Pharmacokinet. 1999;36:211–231. doi: 10.2165/00003088-199936030-00003. [DOI] [PubMed] [Google Scholar]
- 10.Lin J H, Chen I-W, Vastag K J, Ostovic D. pH-dependent oral absorption of L-735,524, a potent HIV protease inhibitor, in rats and dogs. Drug Metab Disp. 1995;23:730–735. [PubMed] [Google Scholar]
- 11.Melvin A J, Mohan K M, Arcuino L A, Edelstein R E, Frenkel L M. Clinical, virological and immunological responses of children with advanced human immunodeficiency virus type 1 disease treated with protease inhibitors. Pediatr Infect Dis J. 1997;16:968–974. doi: 10.1097/00006454-199710000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Monpoux F, Sirvent N, Cottalorda J, Mariani R, Lefbvre J C. Stavudine, lamivudine and indinavir in children with advanced HIV-1 infection: preliminary experience. AIDS. 1997;11:1523–1525. [PubMed] [Google Scholar]
- 13.Mueller B U, Sleasman J, Nelson R P, Smith S, Deutsch P, Ju W, Steinberg S M, Balis F M, Jarosinski P F, Brouwers P, Mistry G, Winchell G, Zwerski S, Sei S, Wood L V, Zeichner S, Pizzo P A. A phase I/II study of the protease inhibitor indinavir in children with HIV infection. Pediatrics. 1998;102:101–109. doi: 10.1542/peds.102.1.101. [DOI] [PubMed] [Google Scholar]
- 14.Rutstein R, Feingold A, Meislich D, Word B, Rudy B. Protease inhibitor therapy in children with perinatally acquired HIV infection. AIDS. 1997;11:F107–F111. doi: 10.1097/00002030-199712000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Stein D S, Fish D G, Bilello J A, Preston S L, Martineau G L, Drusano G L. A 24-week open-label phase I/II evaluation of the HIV-protease inhibitor MK-39 (indinavir) AIDS. 1996;10:485–492. doi: 10.1097/00002030-199605000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Van Rossum A M C, Niesters H G M, Geelen S P M, Scherpbier H J, Hartwig N G, Weemaes C M, Veerman A J P, Suur M H, De Graeff-Meeder E R, Slieker W A T, Hop W C J, Osterhaus A D M E, Burger D M, de Groot R. Clinical and virologic response to combination treatment with indinavir, zidovudine, and lamivudine in children with human immunodeficiency virus-1 infection: a multicentre study in The Netherlands. J Pediatr. 2000;136:780–788. doi: 10.1067/mpd.2000.106234. [DOI] [PubMed] [Google Scholar]
- 17.Wintergerst U, Hoffmann F, Solder B, Notheis G, Petropoulou T, Eberle J, Gurtzler L, Belohradsky B H. Comparison of two antiretroviral triple combinations including the protease inhibitor indinavir in children infected with human immunodeficiency virus. Pediatr Infect Dis J. 1998;17:495–499. doi: 10.1097/00006454-199806000-00012. [DOI] [PubMed] [Google Scholar]