Abstract
The COVID-19 pandemic heightened the psychosocial impact of a cancer diagnosis as patients face concerns about the risk of infection and serious disease and uncertainties about the impact on their treatment. We conducted an online survey (n = 317) and focus groups (n = 19) with patients to examine their experiences with cancer care during the pandemic. Most survey respondents (68%) reported one or more disruptions or delays in care, including appointments switched to telehealth (49%). Patients perceived both benefits (e.g., convenience) and drawbacks (e.g., more impersonal) to telehealth. For many patients, COVID-19-related restrictions on bringing family members to support them during appointments was a major concern and left them feeling alone and vulnerable during treatment. Patients’ self-reported coping during the pandemic was positively associated with age, education, and income (P < .05 for each) and better communication with their doctors during telehealth sessions (P < .001). Study findings highlight the importance of patient-centered care and communication to help patients cope with the challenges of the pandemic. Further research is needed to develop guidelines for use of telehealth as part of patient-centered cancer care.
Keywords: patient experience, cancer, coping, COVID-19 pandemic, distress and anxiety, patient-centered care, psycho-oncology, psychosocial distress, telehealth
Introduction
A cancer diagnosis can lead to anxiety, fear, and feelings of uncertainty about treatment options and prognosis (1,2). The COVID-19 pandemic has heightened the psychosocial impact of cancer as patients face additional concerns about the risk of COVID-19 infection and serious disease (3–10). Adding to distress and uncertainty, patients also have experienced disruptions and delays in cancer care as healthcare systems established safety protocols, postponed or canceled nonurgent care, and prioritized COVID-19 efforts (11,12). International (13) and US-based studies (14–18) have found pandemic-related delays and disruptions in cancer care across all treatment modalities and changes to treatment plans, such as longer intervals between treatments or switching to oral chemotherapy (19). Additionally, to reduce both their own and patients’ risk of infection, cancer care teams have rapidly shifted some aspects of care from in-person to telehealth, thereby changing how patients interact with their cancer care providers (15,18–23).
Patient-centered cancer care can help patients cope with living with cancer and undergoing care during a pandemic. Patient-centered care refers to care that is respectful of and responsive to individuals’ preferences, needs, and values (24). High-quality communication between patients and their cancer care team—a critical component of patient-centered care—provides important information, fosters healing relationships, helps patients manage uncertainty and difficult feelings, and supports self-care (25), all of which are especially important during the pandemic.
To learn more about the impact of the COVID-19 pandemic on cancer patients, we conducted a mixed-methods study addressing the following research questions: (1) To what extent have patients experienced delays and disruptions in their care and changes to their treatment plans? (2) What do patients perceive as the most important impact of the pandemic on their cancer care? (3) How often are patients using telehealth, and what are their perceptions of its benefits and drawbacks? (4) What are patients’ perceptions of healthcare professionals’ communication via telehealth? and (5) How are patients coping with cancer care during the pandemic?
Methods
We conducted an online survey (n = 317) and virtual focus group discussions (n = 5 groups, with a total of 19 participants) with cancer patients in the United States who had received treatment during the pandemic. The survey was conducted from October to December 2020 and the focus groups from November 2020 to January 2021. Eligibility criteria for both the survey and focus groups included having a cancer diagnosis (any cancer type), aged 18 or older, English speaking, and having received any type of cancer treatment in 2020.
The study protocol was reviewed by the [anonymized] Institutional Review Board (IRB) and determined to meet the criteria for exemption from IRB review. A consent process was implemented as part of the focus groups and survey. Focus group participants were sent a consent form prior to the discussions. The facilitator met with each potential participant individually by phone prior to the group discussion, reviewed the consent form, asked if they agreed to participate, and recorded their response. The survey included consent information followed by a question asking if they agreed to participate.
Survey
The survey involved a convenience sample, recruited in partnership with two nonprofit cancer support organizations, Fight Colorectal Cancer and Cancer Support Community, and a market research firm for additional recruitment support. The Cancer Support Community recruited patients through its Cancer Experience Registry, a registry of cancer patients and caregivers who have expressed interest in research participation, and both organizations promoted the research opportunity to their networks via social media. The market research firm recruited participants through its consumer panel, which includes individuals diagnosed with cancer. Survey participants were offered the chance to win a $75 gift card (a total of 20 survey respondents were randomly selected).
The survey included questions about patients’ experiences with cancer care during the pandemic, including delays, disruptions, and changes to care; use of telehealth; communication with healthcare providers; and coping during the pandemic. Open-ended questions asked about the impact of the pandemic on their cancer care (see the survey instrument in the Supplemental Material). Survey questions related to disruptions in care, coping, and telehealth experience and were informed by a patient survey conducted by Fight Colorectal Cancer at the onset of the pandemic (unpublished) and insights gained from both cancer support organizations’ interactions with patients, such as through helplines and support groups, during this time. The communication items parallel key functions in the National Cancer Institute's conceptual model of patient-centered communication in cancer care, such as showing care and support via the function of Fostering Healing Relationships. We conducted survey analysis using SAS v9.4, using chi-square tests to examine bivariate relationships and differences across participant subgroups.
Respondents were 65% female, 34.4% male, 69.3% non-Hispanic White, 15.8% Hispanic, 9.8% non-Hispanic Black, and 5.1% other racial/ethnic groups. Most of the respondents were diagnosed with colorectal cancer (37.9%) and breast cancer (22.4%) (see participant characteristics in Supplementary Table S1).
Focus Groups
A final survey question asked participants if they were interested in additional Cancer Support Community research opportunities. Fight Colorectal Cancer recruited additional participants through social media promotion. Based on patient characteristics from the survey and screening, we recruited a mix of participants in terms of demographic characteristics, time since diagnosis (prior to or during the pandemic), and the use of telehealth. With patient consent, the research team emailed patients to provide information about the focus groups and arrange for a prefocus—group telephone call to gather background information, such as cancer type, treatments, and basic demographic information, and address concerns or questions.
We conducted each 60-minute focus group virtually using a videoconference platform. An experienced qualitative researcher led the discussions, using a semistructured guide that covered experiences with cancer care, telehealth, and communication with healthcare providers. A second researcher took notes and we audio-recorded and transcribed the discussions with participant permission. Participants were provided a $75 Amazon e-gift card.
A majority of participants were female (n = 14), White (n = 16), aged 45–64 (n = 12), and had a 4-year college degree or higher (n = 10). Their cancer diagnoses were colorectal (n = 7); breast (n = 6); ovarian (n = 3); liver (n = 3); lung (n = 2); and oral/throat, skin, fallopian, prostate, and Hodgkin’s lymphoma (n = 1 each). Five participants were diagnosed in 2020, during the pandemic, and others had been diagnosed previously and were still in treatment during 2020. Telehealth experience ranged from 5 or fewer sessions (n = 11) to 6 to 10 sessions (n = 4), and more than 10 sessions (n = 2).
We performed a thematic analysis of the focus group data (26). We used notes and verbatim transcripts from the discussions organized by interview questions and participants to arrive at themes in each group and across the five focus groups. Two researchers with training in qualitative data analysis (RM and LA) reviewed the notes and verbatim abstracts and identified emerging themes. Two senior researchers (KT and RS) reviewed the themes and discussed with the team to reach a consensus. Responses to four open-ended survey questions also were analyzed qualitatively for themes, context for the closed-ended survey response, and for illustrative quotes.
Results
Disruptions, Delays, and Changes to Treatment Plan
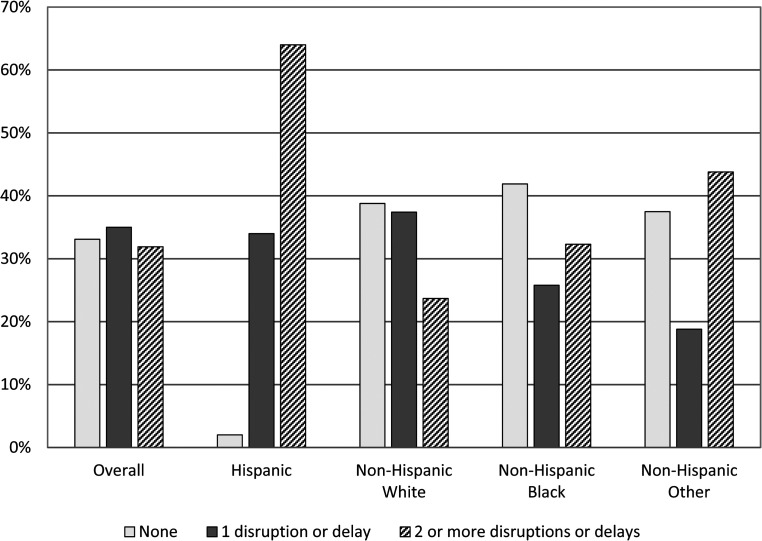
Survey participants were asked if they had experienced different types of delays or disruptions in their cancer care because of the pandemic. Overall, 68.1% of survey respondents reported one or more disruptions or delays in care (Figure 1). The most frequent response was that some appointments had been changed from in-person to telehealth (49.5%), followed by delayed treatment (27.4%) and canceled or rescheduled appointments (24.3%). Respondents also were asked if there had been any changes in their cancer care (or treatment) plan. Participants were most likely to report a change in treatment frequency (17.4%) and type (15.5%), such as change from intravenous to oral chemotherapy. About 14% of participants said that their doctors had recommended a significant change to their cancer care plan (13.6%) (data are not shown).
Figure 1.
Disruptions or delays in care overall and by racial/ethnic group.
Hispanic patients were significantly more likely to report two or more delays or disruptions in care (64.0%) compared with all non-Hispanic groups (e.g., non-Hispanic Whites, non-Hispanic Blacks, and other non-Hispanic respondents) (P < .001) and were significantly more likely to report two or more treatment changes (62.0%) compared with all non-Hispanic groups (P < .001). The percentage of respondents reporting two or more delays/disruptions decreased with age; from 52% among participants aged 18–34 to 19% among participants aged 65 or older (P < .001). There were no significant differences in delays/disruptions by gender or education. The pattern of responses by age group was similar for changes to treatment (P < .001).
Regarding participant perceptions of the most important effect of the pandemic on their cancer care, focus group participants and survey respondents shared their anxieties about delays in care, such as having canceled or postponed surgeries and having long appointment waits.
“I was getting a scan and there was a spot that had come up on my liver. I ended up having to wait a month to see my oncologist for them to read it. I was calling to try and get answers…. When you get those scans, you’re just a nervous wreck.”
(FG participant)
“I was very worried about one of my surgeries this year being delayed and that added a lot of stress…the rules change each day.”
(Survey respondent)
More than half (51.4%) of survey respondents were moderate to very seriously concerned that family or friends could not accompany them at appointments, which was echoed in focus groups as a primary concern. Focus group participants most often discussed the difficulty of attending in-person appointments and treatment alone, the corresponding anxiety and vulnerability, and the difficult switch to telehealth. Participants missed the emotional support afforded when accompanied during chemotherapy sessions or in the waiting room prior to surgery—having someone to listen, ask questions, advocate for them, and help them process information when they got home.
“My husband is not allowed to come into appointments with me and that is very frustrating. I have had to do my last rounds of chemo alone. I felt very isolated and alone and depressed. I had the nurses and my oncologist, but your significant other is a huge support system.”
(FG participant)
Some participants found it helpful to have a support person participate in appointments virtually, by phone or video call.
“My sister, who is a stage III cancer survivor, was my main support person. Whenever I had a consult with any of the doctors, I would try to have her in on the call…. When I went in for my in-person appointments, I had her on FaceTime.”
(FG participant)
Use of Telehealth
Survey participants were asked whether they had any telehealth visits for their cancer care since the pandemic, with telehealth defined as “medical appointments with your doctors or healthcare providers by video (for example, using Facetime, Zoom or another video platform) or phone.” Overall, 71.6% of survey respondents reported at least one telehealth session. As shown in Table 1, there were significant differences in telehealth use by gender, age, race/ethnicity, and cancer stage at diagnosis. Respondents aged 65 or older were least likely to report telehealth use, with more than half (50.8%) reporting no telehealth sessions (P < .001). Hispanic patients were most likely to report telehealth use compared with all non-Hispanic groups, with 64% reporting six or more sessions (P < .001). Respondents diagnosed at Stage 0/1 were least likely to report any telehealth use, with 42.2% reporting no telehealth sessions (P < .001). There were no significant differences by income, education, or time since diagnosis (data are not shown).
Table 1.
Survey Participants use of Telehealth.
| Number of Telehealth Sessions | ||||
|---|---|---|---|---|
| N (%) | P-value c | |||
| Characteristic | None | 1–5 times | 6 + times | |
| Overall | 90 (28.4%) | 151 (47.6%) | 76 (24.0%) | |
| Gender a | ||||
| Female | 57 (27.7%) | 109 (52.9%) | 40 (19.4%) | .0110 |
| Male | 32 (29.4%) | 41 (37.6%) | 36 (33.0%) | |
| Other | 0 (0.0%) | 1 (100.0%) | 0 (0.0%) | |
| Prefer not to answer | 1 (100.0%) | 0 (0.0%) | 0 (0.0%) | |
| Age | ||||
| 18–4 | 5 (20.0%) | 5 (20.0%) | 15 (60.0%) | <.001 |
| 35–49 | 16 (16.2%) | 48 (48.5%) | 35 (35.4%) | |
| 50–64 | 37 (28.5%) | 73 (56.2%) | 20 (15.4%) | |
| 65 + | 32 (50.8%) | 25 (39.7%) | 6 (9.5%) | |
| Race/Ethnicity b | ||||
| Hispanic | 3(6%) | 15 (30%) | 32 (64%) | <.001 |
| Non-Hispanic White | 73 (33.3%) | 111 (50.7%) | 35 (16.0%) | |
| Non-Hispanic Black | 9 (29.0%) | 17 (54.8%) | 5 (16.1%) | |
| Other Non-Hispanic/ multiracial/other | 5 (31.3%) | 7 (43.8%) | 4 (25.0%) | |
| Cancer stage at diagnosis | ||||
| Stage 0/1 | 19 (42.2%) | 25 (55.6%) | 1 (2.2%) | <.001 |
| Stage II | 15 (23.4%) | 28 (43.8%) | 21 (32.8%) | |
| Stage III | 14 (17.1%) | 40 (48.8%) | 28 (34.1%) | |
| Stage IV | 21 (23.6%) | 46 (51.7%) | 22 (24.7%) | |
| Don't know/other | 21 (56.8%) | 12 (32.4%) | 4 (10.8%) | |
Note: aAnswers other than male and female were excluded for statistical testing.
For statistical testing, categories were collapsed into three categories: (1) Hispanic, (2) Non-Hispanic White, and (3) Non-Hispanic Black/Asian, American Indian, Native Hawaiians and Pacific Islanders/Other/Multiracial.
Statistical tests conducted were chi-square tests.
Experiences with Patient-Provider Communication via Telehealth
Survey participants were asked about their communication with doctors and other healthcare professionals during telehealth sessions for their cancer care (strongly disagree to strongly agree). Most respondents agreed or strongly agreed that their healthcare providers “communicate well during telehealth sessions” (91.2%), “are caring and supportive during telehealth sessions” (92.9%), and “share the information I need during telehealth sessions” (92.5%). Respondents reporting five or fewer telehealth visits were more likely to strongly agree that doctors communicated well during telehealth visits compared with respondents reporting six or more visits (47% vs. 30.3%; P < .05) (data are not shown).
Focus group participants and survey respondents described the benefits and drawbacks of telehealth sessions (Table 2). Benefits included the convenience and comfort of home, the fact that family members and loved ones can easily participate, and the perception that it is safer during the pandemic. Drawbacks included that it is more impersonal and thus harder to build rapport, and it is absent both physical assessment and a comforting touch.
Table 2.
Perceptions About Benefits and Drawbacks of Telehealth.
| Benefits | |
|---|---|
| Convenience and comfort of home |
I enjoy televisits. It consumes less time and keeps me safe! Doctors tend to stay on schedule easier. – Survey respondent I thought it was great, because you didn't have to go in and it was quick, especially for the issue that I had, I didn't want to have to wait, make an appointment, go in a week later, I didn't really have that time. – Focus group participant |
| Family members and loved ones can easily participate |
I started to like telemed. I adapted. I would have my husband around the table, my oldest son, who is in nursing school who would sit there and he would just absorb everything – Focus group participant |
| Safer during pandemic |
Telehealth is working during this tough time. It's not as great as in-person appointments but it keeps me safe. – Survey respondent |
| Drawbacks | |
| Harder to build rapport, impersonal |
It's been difficult to build rapport through telehealth. Communication doesn't just take place through verbal means and it's often those nonverbal parts of communication that help us connect and find comfort. – Survey respondent It's just impersonal sometimes. I just don't think I would ask nearly as many questions as I would if I could see them face to face. – Focus group participant |
| Absence of comforting touch |
I’ll reference back the hug that my oncologist always gave me and how I miss that. It's kind of an isolating feeling right now. You’re already nervous about the pandemic and contracting it, and the ‘what ifs’ if you do because of your cancer status. And then at a time when I really feel like I need a hug the most, it's not there. – Focus group participant |
| Lack of physical assessment |
There is something about seeing your doctor face-to-face…. It just sets you more at ease. You’re there. They can see you. If you’re like, “Oh, I have this pain here,” they can touch your liver and be like, “Oh, that's this.” – Focus group participant So I physically want them to see me, I physically want to have those tests done and be present for all of that where I don't think over the phone or tele visit they wouldn't be able to really see the things that I’d want them to see. – Focus group participant |
Coping During the Pandemic
Participants were asked, “Overall, how would you say you are coping during the coronavirus pandemic?” About 14% of respondents said they were not coping very well during the pandemic, 60.3% were coping fairly well, and 25.9% were coping very well (Table 3). Coping very well was positively associated with age (P < .01), education (P < .01), and income (P < .05). Hispanic respondents were most likely to report they were not coping well compared with all non-Hispanic groups (P < .01). There were no significant differences by gender (data are not shown).
Table 3.
Coping During the Pandemic.
| N (%) | |||||
|---|---|---|---|---|---|
| I am not coping very well | I am coping fairly well | I am coping very well | P-value b | ||
| Overall | 44 (13.9%) | 191 (60.3%) | 82 (25.9%) | ||
| Age | |||||
| 18–34 | 4 (16.0%) | 19 (76.0%) | 2 (8.0%) | .0022 | |
| 35–49 | 17 (17.2%) | 60 (60.6%) | 22 (22.2%) | ||
| 50–64 | 20 (15.4%) | 75 (57.7%) | 35 (26.9%) | ||
| 65 + | 3 (4.8%) | 37 (58.7%) | 23 (36.5%) | ||
| Race/Ethnicity a | |||||
| Hispanic | 11 (22.0%) | 36 (72.0%) | 3 (6.0%) | .0010 | |
| Non-Hispanic White | 24 (11.0%) | 125 (57.1%) | 70 (32.0%) | ||
| Non-Hispanic Black | 6 (19.4%) | 20 (64.5%) | 5 (16.1%) | ||
| Other Non-Hispanic/multiracial/other | 3 (18.8%) | 10 (62.5%) | 3 (18.8%) | ||
| Education | |||||
| High school graduate/GED or less | 11 (32.4%) | 17 (50.0%) | 6 (17.6%) | .0011 | |
| Some college | 11 (19.0%) | 36 (62.1%) | 11 (19.0%) | ||
| Associate/or technical degree | 6 (9.4%) | 41 (64.1%) | 17 (26.6%) | ||
| College or advanced degree | 16 (9.9%) | 97 (60.2%) | 48 (29.8%) | ||
| Income | |||||
| Less than $20,000 | 3 (11.5%) | 16 (61.5%) | 7 (26.9%) | .0344 | |
| $20,001–$40,000 | 13 (31.7%) | 25 (61.0%) | 3 (7.3%) | ||
| $20,001–$40,000 | 11 (22.0%) | 28 (56.0%) | 11 (22.0%) | ||
| $60,001–$80,000 | 2 (5.0%) | 28 (70.0%) | 10 (25.0%) | ||
| $80,001–$100,000 | 4 (11.4%) | 21 (60.0%) | 10 (28.6%) | ||
| More than $100,001 | 10 (9.9%) | 60 (59.4%) | 31 (30.7%) | ||
| Don't know/Not sure/Prefer not to answer | 1 (4.2%) | 13 (54.2%) | 10 (41.7%) | ||
Note: aFor statistical testing, categories were collapsed into three categories: Hispanic, Non-Hispanic White, and Non-Hispanic Black/Asian, American Indian, Native Hawaiian or Pacific Islander/Other/Multiracial.
Statistical tests conducted were chi-square tests.
For telehealth participants, those who reported better communication with their doctors during telehealth sessions reported better coping, with positive associations between coping and agreement with these statements: “My doctors and other healthcare professionals communicate well during telehealth sessions” (P < .001); “My doctors and other healthcare professionals are caring and supportive during telehealth sessions” (P < .05); and “My doctors and other healthcare professionals share the information I need during telehealth sessions” (P < .001). These relationships were assessed using a Cochran–Mantel–Haenszel test, which tests for linear trend as opposed to a general association among items. We combined these items into a scale, with high internal consistency (Cronbach's alpha = 0.89) and found a significant positive relationship between the composite measure of communication with doctors and coping (P < .001).
We asked focus group participants what was most important for their cancer care team to understand about the experience of receiving cancer treatment during the pandemic. Participants wanted their doctors to be aware that they are feeling anxious, scared, isolated, depressed, and missing the social and emotional support they might otherwise have. They shared feelings of being overwhelmed with worries about COVID-19 in addition to their cancer diagnosis.
“COVID has really…just added a whole other level of fear for some people, depression for some people.”
“During this time, the doctors need to be really mindful of how nervous their patients are and how overwhelmed we are and how depressed we might be getting. Because on so many levels, it is just a recipe for becoming depressed, being sick with a terrible disease and being afraid of this COVID and being alone and isolated.”
Discussion
This study highlights the uncertainties and stress for patients receiving cancer treatment during the COVID-19 pandemic. They have had to adjust to disruptions and delays in care, changes to their treatment plans, not having loved ones with them during in-person appointments, and changes in communication with providers as many appointments transitioned to telehealth. Similar to other studies (11,12,15,19,23), we found that many patients experienced delays and disruptions in their care during the pandemic. While patients generally understood the need for extra precautions, delays and disruptions increased their stress and anxiety. Similarly, Sokas and colleagues (27) found that patients were not surprised by and generally accepted delays in care. Yet they had persistent delay-related worries. Our study findings highlight differences in the extent of delays and disruptions in care experienced by patient subgroups, with racial and ethnic minority groups more likely to report disruptions and delays. The COVID-19 pandemic may have exacerbated preexisting differences in social determinants of health, such as employment and health insurance status, which contribute to disparities in the quality of cancer care (28). Further research is needed to identify and address the factors underlying these differences.
Study participants reported that one major impact of the pandemic was not being able to bring a support person to appointments or treatment sessions. Our mixed-methods findings expand and confirm the findings from a small prior study (n = 7) that found that a key patient difficulty during the pandemic was attending treatment and appointments alone (29). This finding aligns with our understanding of the critical role family members and other loved ones play in cancer care. Patients rely on others for both instrumental (e.g., transportation to appointments) and emotional support (25,30). Bringing a companion to appointments facilitates the exchange of information and understanding between physicians and patients (31–36). Some participants used phone and videoconference to connect family members during in-person consultations, but they missed the physical presence and emotional support provided by a companion.
Patients understood the need to change in-person visits to telehealth visits to reduce exposure to COVID-19. As previously documented (22,37), patients appreciated the convenience of being able to participate from home and the ability to involve family members and other loved ones who would not ordinarily be able to join in-person appointments. They felt telehealth was more appropriate when they had a preexisting relationship with the doctor, relative to consulting with a new doctor. Conversely, participants cited the difficulty of building rapport with their doctor, missing comforting touch, and lacking confidence in their doctors’ assessments without seeing them face to face. Other studies have found that telehealth may not be an appropriate modality for diagnosis and treatment of symptomatic patients or for communicating complex treatment recommendations or bad news, and that it can be more difficult for doctors to express caring and concern (37–39). Despite the drawbacks, many patients and healthcare professionals would like telehealth to remain an option in post-pandemic cancer care (22,38–40).
About 28% of the survey respondents had never used telehealth for their cancer care, with significantly less use among older patients. We did not ask the reasons why they did not use telehealth; consequently, further research is warranted to understand the reasons why some cancer patients do not use telehealth, which may include doctors did not offer this option, patient preference, and/or technological barriers (41).
Only about one-quarter of survey respondents reported coping very well during the pandemic with worse coping across several sociodemographic groups. Several other studies assessed the psychosocial impact of the COVID-19 pandemic on cancer patients, such as fear and social isolation, but not overall coping (4,8,10,42). For example, Lou and colleagues’ (4) cross-sectional survey found significantly higher levels of concern about contracting COVID-19, serious illness, and not being able to get needed healthcare (for COVID-19 or other serious illness) among respondents with cancer.
Among the three-quarters of survey respondents who had used telehealth, there were significant positive correlations between ratings of provider communication via telehealth and coping during the pandemic. Although it is feasible that provider communication supported patient coping, the cross-sectional nature of our data limits our ability to draw causal inferences. Nevertheless, evidence from other research supports the importance of the role of patient-centered communication in the context of the pandemic. We are not aware of prior studies examining patient-provider communication via telehealth and patient coping or other outcomes. A few studies provide insight into the importance of high-quality patient-provider communication generally in the context of the pandemic. Rossi and colleagues (7) found that empathetic and clear communication buffered the adverse effects of COVID-19 -related fear on cancer patients’ hopelessness. Two studies identified the importance of patient-provider communication related to delays and disruptions in treatment in terms of increasing patient understanding and acceptance and reducing distress (27,43).
Lessons learned from the rapid adoption of telehealth during the pandemic can inform guidelines for integrating telehealth as an option in future patient-centered cancer care. Additional research is warranted to better understand the perspectives of patients, families, and healthcare providers concerning when and how telehealth should be integrated; for example, at which points in the cancer care continuum and for which services and patients. From a patient-centered care perspective, understanding and respecting patients’ preference regarding in-person or virtual visits is paramount. To support such care, patients will require support from healthcare systems to identify and address barriers (where possible) to telehealth use and provide adequate training for healthcare providers.
Clinical Implications
The pandemic compounded cancer patients’ psychosocial distress as they faced uncertainties about their risks and the impact on their care, coupled with social isolation. The need for patient-centered communication—a critical component of high-quality cancer care across the care continuum—was highlighted in our findings, as better coping during the pandemic was associated with higher ratings of clinician communication. Through steps such as asking patients about and validating their experiences during the pandemic, sharing up-to-date information, acknowledging the uncertainties of cancer care and helping patients deal with these uncertainties during an evolving pandemic, and offering emotional support, healthcare professionals may be able to help patients cope.
Learning from the experience of widespread use of telehealth during the pandemic, cancer care providers can strengthen patient-centered care by offering telehealth as an option (when clinically appropriate), discussing the pros and cons of telehealth with patients and families, respecting their preferences, and providing technological support as needed. As mentioned, many patients and healthcare professionals would like telehealth to remain an option in post-pandemic cancer care (22,38–40).
Study Limitations
This study involved a convenience sample of cancer patients recruited through two patient advocacy groups and a research recruitment firm. While diverse with respect to age, cancer stage, and time since diagnosis, the sample was disproportionally non-Hispanic White, college educated, and female. Consequently, the results are not generalizable to all cancer patients who received treatment during the pandemic.
Conclusion
This study provides insight into patients’ experiences with cancer care during the pandemic. Most respondents experienced significant delays or disruptions in care, but they also had positive assessments of telehealth. However, respondents also expressed concerns that communication quality might suffer, particularly with respect to a supportive connection in the clinician–patient relationship.
Supplemental Material
Supplemental material, sj-docx-1-jpx-10.1177_23743735221092567 for Patients’ Experiences with Cancer Care: Impact of the COVID-19 Pandemic by Katherine Treiman, Elissa C. Kranzler, Rebecca Moultrie, Laura Arena, Nicole Mack, Erica Fortune, Reese Garcia and Richard L Street in Journal of Patient Experience
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Patient-Centered Outcomes Research Institute (grant number EADI_14460).
Ethical Approval: The study was reviewed by RTI International's Institutional Review Board (IRB). The IRB determined that the protocol meets the criteria for exempt research.
ORCID iDs: Katherine Treiman https://orcid.org/0000-0001-9589-2491
Richard L Street https://orcid.org/0000-0001-7392-9927
Statement of Human and Animal Rights: All procedures in this study were conducted in accordance with the RTI IRB ethical standards. The IRB determined that the protocol meets the criteria for exempt research.
Statement of Informed Consent: Informed consent was obtained from patients (written for survey respondents and verbal for focus group participants) for participation in the study and reporting of anonymized information.
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Mehnert A, Hartung TJ, Friedrich M, et al. One in two cancer patients is significantly distressed: prevalence and indicators of distress. Psychooncology. 2018;27:75‐82. doi: 10.1002/pon.4464 [DOI] [PubMed] [Google Scholar]
- 2.Peters L, Brederecke J, Franzke A, et al. Psychological distress in a sample of inpatients with mixed cancer—a cross-sectional study of routine clinical data. Front Psychol. 2020;11:591771. 2020/12/18. DOI: 10.3389/fpsyg.2020.591771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ciazynska M, Pabianek M, Szczepaniak K, et al. Quality of life of cancer patients during coronavirus disease (COVID-19) pandemic. Psychooncology. 2020;29:1377‐9. doi: 10.1002/pon.5434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lou E, Teoh D, Brown K, et al. Perspectives of cancer patients and their health during the COVID-19 pandemic. PLOS One. 2020;15:e0241741. doi: 10.1371/journal.pone.0241741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miaskowski C, Paul SM, Snowberg K, et al. Stress and symptom burden in oncology patients during the COVID-19 pandemic. J Pain Symptom Manage. 2020;60:e25‐34. doi: 10.1016/j.jpainsymman.2020.08.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schellekens MPJ, van der Lee ML. Loneliness and belonging: exploring experiences with the COVID-19 pandemic in psycho-oncology. Psychooncology. 2020;29:1399‐401. doi: 10.1002/pon.5459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rossi AA, Marconi M, Taccini F, et al. From fear to hopelessness: the buffering effect of patient-centered communication in a sample of oncological patients during COVID-19. Behavioral Sciences. 2021;11:87. doi: 10.3390/bs11060087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caston NE, Lawhon VM, Smith KL, et al. Examining the association among fear of COVID-19, psychological distress, and delays in cancer care. Cancer Med. 2021;10:8854‐65. doi: 10.1002/cam4.4391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leach CR, Kirkland EG, Masters M, et al. Cancer survivor worries about treatment disruption and detrimental health outcomes due to the COVID-19 pandemic. J Psychosoc Oncol. 2021;39:347‐65. doi: 10.1080/07347332.2021.1888184 [DOI] [PubMed] [Google Scholar]
- 10.Salehi O, Alarcon SV, Vega EA, et al. COVID-19’s impact on cancer care: increased emotional stress in patients and high risk of provider burnout. J Gastrointest Surg. 2022;26:1‐12. doi: 10.1007/s11605-021-05032-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Papautsky EL, Hamlish T. Patient-reported treatment delays in breast cancer care during the COVID-19 pandemic. Breast Cancer Res Treat. 2020;184:249‐54. doi: 10.1007/s10549-020-05828-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patt D, Gordan L, Diaz M, et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO clinical Cancer Informatics. 2020;4:1059‐71. doi: 10.1200/cci.20.00134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riera R, Bagattini AM, Pacheco RL, et al. Delays and disruptions in cancer health care due to COVID-19 pandemic: systematic review. JCO Glob Oncol. 2021;7:311‐23. doi: 10.1200/GO.20.00639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dilawari A, Rentscher KE, Zhai W, et al. Medical care disruptions during the first six-months of the COVID19 pandemic: the experience of older breast cancer survivors. Res Sq. 2021. doi: 10.21203/rs.3.rs-416077/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hui JYC, Yuan J, Teoh D, et al. Cancer management during the COVID-19 pandemic in the United States: results from a national physician cross-sectional survey. Am J Clin Oncol. 2020;43:679‐84. doi: 10.1097/COC.0000000000000757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nakayama J, Wang GM, Cioffi G, et al. The negative impact of the COVID-19 pandemic on oncology care at an academic cancer referral center. Oncology (Williston Park). 2021;35:462‐70. doi: 10.46883/ONC.2021.3508.0462 [DOI] [PubMed] [Google Scholar]
- 17.Perkons NR, Kim C, Boedec C, et al. Quantifying the impact of the COVID-19 pandemic on gastrointestinal cancer care delivery. Cancer Rep (Hoboken). 2021:e1427. doi: 10.1002/cnr2.1427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rodriguez GM, Ferguson JM, Kurian A, et al. The impact of COVID-19 on patients with cancer: a national study of patient experiences. Am J Clin Oncol. 2021;44:580‐7. doi: 10.1097/COC.0000000000000865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Powis M, Milley-Daigle C, Hack S, et al. Impact of the early phase of the COVID pandemic on cancer treatment delivery and the quality of cancer care: a scoping review and conceptual model. Int J Qual Health Care. 2021;33:mzab088. doi: 10.1093/intqhc/mzab088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lonergan PE, Washington Iii SL, Branagan L, et al. Rapid utilization of telehealth in a comprehensive cancer center as a response to COVID-19: cross-sectional analysis. J Med Internet Res. 2020;22:e19322. doi: 10.2196/19322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Doroshow D, Schmidt AL, Bakouny Z, et al. Disparities in cancer during the COVID-19 pandemic: COVID-19 and cancer outcomes study (CCOS). Ann Oncol. 2020;31:S1204. doi: 10.1016/j.annonc.2020.08.2315 [DOI] [Google Scholar]
- 22.Patt D, Wilfong L, Toth S, et al. Telemedicine in community cancer care: how technology helps patients with cancer navigate a pandemic. JCO oncology Practice. 2021;17:e11‐5. doi: 10.1200/op.20.00815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tang A, Neeman E, Vuong B, et al. Care in the time of COVID-19: impact on the diagnosis and treatment of breast cancer in a large, integrated health care system. Breast Cancer Res Treat. 2022;191:665–675. doi: 10.1007/s10549-021-06468-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Institute of Medicine. Delivering high-quality cancer care: charting a new course for a system in crisis. http://www.nap.edu/catalog/18359/delivering-high-quality-cancer-care-charting-a-new-course-for (2013, accessed April 7, 2016)
- 25.Epstein RM, Street RL, Jr. Patient-centered communication in cancer care: Promoting healing and reducing suffering. Report no. NIH Publications No. 07-6225, 2007. Bethesda, MD: National Cancer Institute
- 26.Kiger ME, Varpio L. Thematic analysis of qualitative data: AMEE Guide No. 131. Med Teach. 2020;42:846‐54. doi: 10.1080/0142159X.2020.1755030 [DOI] [PubMed] [Google Scholar]
- 27.Sokas C, Kelly M, Sheu C, et al. Cancer in the shadow of COVID: early-stage breast and prostate cancer patient perspectives on surgical delays due to COVID-19. Ann Surg Oncol. 2021;28:8688‐96. doi: 10.1245/s10434-021-10319-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Acquati C, Chen TA, Martinez Leal I, et al. The impact of the COVID-19 pandemic on cancer care and health-related quality of life of non-Hispanic Black/African American, Hispanic/Latina and non-Hispanic White women diagnosed with breast cancer in the U.S.: a mixed-methods study protocol. Int J Environ Res Public Health. 2021;18. doi: 10.3390/ijerph182413084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moran HK, Brooks JV, Spoozak L. Undergoing active treatment for gynecologic cancer during COVID-19: a qualitative study of the impact on healthcare and social support. Gynecol Oncol Rep. 2020;34:100659. doi: 10.1016/j.gore.2020.100659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laidsaar-Powell R, Butow P, Bu S, et al. Attitudes and experiences of family involvement in cancer consultations: a qualitative exploration of patient and family member perspectives. Support Care Cancer. 2016;24:4131‐40. doi: 10.1007/s00520-016-3237-8 [DOI] [PubMed] [Google Scholar]
- 31.Wolff JL, Guan Y, Boyd CM, et al. Examining the context and helpfulness of family companion contributions to older adults’ primary care visits. Patient Educ Couns. 2017;100:487‐94. doi: 10.1016/j.pec.2016.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lum Y, Colburn J, Christmas C. Involvement of visit companions in internal medicine resident clinic visits: perspectives of patients, companions, and internal medicine residents. J Am Geriatr Soc. 2013;61:S208‐9. doi: 10.1111/jgs.12263 [DOI] [Google Scholar]
- 33.Rosland AM, Piette JD, Choi H, et al. Family and friend participation in primary care visits of patients with diabetes or heart failure: patient and physician determinants and experiences. Med Care. 2011;49:37‐45. doi: 10.1097/MLR.0b013e3181f37d28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sheehan OC, Graham-Phillips AL, Wilson JD, et al. Non-spouse companions accompanying older adults to medical visits: a qualitative analysis. BMC Geriatr. 2019;19:84. doi: 10.1186/s12877-019-1098-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Laidsaar-Powell R, Butow PN, Bu S, et al. Physician-patient-companion communication and decision-making: a systematic review of triadic medical consultations. Patient Educ Couns. 2013;91:3‐13. DOI: 10.1016/j.pec.2012.11.007 [DOI] [PubMed] [Google Scholar]
- 36.Otto AK, Reblin M, Harper FWK, et al. Impact of patients’ companions on clinical encounters between black patients and their non-black oncologists. JCO Oncology Practice. 2021;17(5):e676–e685. doi: 10.1200/op.20.00820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heyer A, Granberg RE, Rising KL, et al. Medical oncology professionals’ perceptions of telehealth video visits. JAMA Netw Open. 2021;4:e2033967. doi: 10.1001/jamanetworkopen.2020.33967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang PJ, Jay GM, Kalpakjian C, et al. Patient and provider-reported satisfaction of cancer rehabilitation telemedicine visits during the COVID-19 pandemic. PM & R : The Journal of Injury, Function, and Rehabilitation. 2021;13(12):1362–1368. doi: 10.1002/pmrj.12552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang H, Cha EE, Lynch K, et al. Radiation oncologist perceptions of telemedicine from consultation to treatment planning: a mixed-methods study. Int J Radiat Oncol Biol Phys. 2020;108:421‐9. doi: 10.1016/j.ijrobp.2020.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zimmerman BS, Seidman D, Berger N, et al. Patient perception of telehealth services for breast and gynecologic oncology care during the COVID-19 pandemic: a single center survey-based study. J Breast Cancer. 2020;23:542‐52. doi: 10.4048/jbc.2020.23.e56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.BrintzenhofeSzoc K, Krok-Schoen JI, Pisegna JL, et al. Survey of cancer care providers’ attitude toward care for older adults with cancer during the COVID-19 pandemic. J Geriatr Oncol. 2021;12:196‐205. doi: 10.1016/j.jgo.2020.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhao F, Henderson TO, Cipriano TM, et al. The impact of coronavirus disease 2019 on the quality of life and treatment disruption of patients with breast cancer in a multiethnic cohort. Cancer. 2021;127:4072‐80. doi: 10.1002/cncr.33798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Soriano EC, Perndorfer C, Otto AK, et al. Psychosocial impact of cancer care disruptions in women with breast cancer during the COVID-19 pandemic. Front Psychol. 2021;12:662339. doi: 10.3389/fpsyg.2021.662339 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-jpx-10.1177_23743735221092567 for Patients’ Experiences with Cancer Care: Impact of the COVID-19 Pandemic by Katherine Treiman, Elissa C. Kranzler, Rebecca Moultrie, Laura Arena, Nicole Mack, Erica Fortune, Reese Garcia and Richard L Street in Journal of Patient Experience