Abstract
Introduction
Previous studies illustrate significant increases in pelvic fracture incidence; however, there is a paucity of information on the incidence of osteoporotic pelvic ring injuries based on large-scale examinations of geographically and ethnically diverse populations. This study addresses the epidemiology of osteoporotic pubic ramus fractures in the United States and details differences in incidence rates with respect to age, gender, and race.
Materials and Methods
National Electronic Injury Surveillance System (NEISS) data between 2002 and 2019 was gathered for individuals aged 60 and above presenting to U.S. emergency departments with ramus fractures. Incidence rates for ramus injuries were calculated using adjusted U.S. Census Bureau estimates of population. Fracture incidences were calculated for age, gender, and race strata.
Results
The overall incidence rate of pubic ramus fractures in the United States between 2002 and 2019 was 13.47 per 1,000,000 people 60 years and older (95% confidence limit: 9.92-17.01). The incidence of pubic ramus fractures for females in the US was 21.71 (16.08-27.34). Rates of ramus fracture increased overall (P < .001) and for both genders between the ages of 60 and 100, though the rate increase was significantly greater in females than in males (P < .001). In terms of race, incidence was highest Asian females and lowest in Native American and Pacific Islander men.
Discussion/Conclusion
: As the first national study addressing the epidemiology of ramus injuries in the United States, this work reveals these injuries comprise a significant fracture risk in the elderly. In addition, it highlights gender and ethnic strata that are more susceptible to these injuries.
Keywords: national electronic injury surveillance system, pelvic fracture, rami fractures, fragility fracture, epidemiology
Introduction
Current literature of pelvic ring fractures primarily focus on high-energy mechanisms such as motor vehicle accidents; however, over 60% of the pelvic ring are fragility low-energy fractures.1-4 These fractures are associated with significant morbidity and mortality among elderly osteoporotic patients.
Epidemiological evidence suggests that the incidence of pelvic fragility fractures is on a global rise. 5 The sharpest increase has been observed among females and elderly patients, likely attributed to osteoporosis. A 2016 retrospective analysis reported that 75% of patients with fragility pelvic fractures were females and significantly associated with low bone density and vitamin D deficiency. 6 In 1970, 20 of 100,000 people in Finland sustained pelvic ring fractures due to osteoporosis and low-energy trauma. 2 In 1997, the incidence had more than quadrupled to 92 per 100,000 patients. 2 Furthermore, among Netherland’s patients over 65 years of age between 1986 and 2011, rates of osteoporotic pelvic fractures increased by 127%. 5
Previous studies have demonstrated that patients with pubic rami fractures have a reported 1-year mortality rates between 13.3-24.7%, which is significantly higher than the rates observed in age-matched cohorts.3,4,7 Prior work also indicates that 95% of patients who sustain an acute osteoporotic pubic ramus fracture require longer hospitalizations for pain control and physical therapy.2-4,7-9 Ten-year outcomes among 99 patients with isolated pubic rami fractures reported a 20.2% in-hospital complication rate while after discharge, 33% of patients required either temporary or permanent nursing home care. 8 Furthermore, 49% of patients with pubic ramus fragility fractures lost their independent mobility, and 40% of patients did not fully recover. 10
Despite the data illustrating significant increases in pelvic fragility fracture, there is a paucity of incidence data from the United States representative of the large and ethnically diverse populace.1,11 Understanding the implications of fragility fractures is critical given the American Orthopedic Association’s ‘Own the Bone’ program, a national multidisciplinary systems-based fragility fracture prevention initiative. The overall mission of Own the Bone is to reduce the incidence of future fractures while bolstering the impact osteoporosis treatment. Bunta et al reported that the Own the Bone intervention succeeded in improving the behaviors of medical professionals with regards to holistic osteoporosis treatment including: bone mineral density testing, pharmacotherapy management, and coordination of care for patients who sustained a fragility fracture. 12 Therefore, the aims of this study are to calculate the incidence rates and evaluate racial and gender differences among patients with fragility pubic rami fractures presenting to the emergency department.
Materials and Methods
Data Acquisition
The National Electronic Injury Surveillance System (NEISS) database was queried between 2002-2019 to identify pubic rami fractures in patients over 60 years of age. NEISS is a validated injury surveillance and tracking system that details de-identified injury data from over 100 emergency departments across the United States selected to represent a probability sample of all 5,000+ U.S. hospitals with emergency departments. Data from each hospital is assigned statistical sample weights. Information collected from January 1, 2002 is available on the online database and searchable by criteria-based queries. Patient age, gender, race, ethnicity, injury diagnosis, anatomic location, and mechanism of action are reported. 13
Variables
To establish the appropriate cohort and identify fragility fractures, all instances of fracture (NEISS diagnosis category = 57) in Trunk, Lower (NEISS body location code = 79) were queried. Narrative fields were coded for inclusion: “rami” or “ramus.” Furthermore, data points yielded by this initial screening were then individually evaluated utilizing the mechanism of injury narrative field for instances of low mechanism among patients over 60 years of age.
Gender, age, and ethnicity were analyzed as categorical variables (Table 1). Age was stratified by half-decade. To accurately identify race, narrative fields were queried for individuals designated as “Other” race. Patients reporting “Hispanic”, “Spanish”, “Latino”, or “Mexican” were re-designated as “Hispanic” in accordance with US census definitions. Similarly, Patients identified as European, Middle Eastern were re-classified as “White”; individuals who identified themselves as coming from East or South Asia were re-designated as “East Asian”; individuals who identified themselves as African, African American, or coming from the West Indians were re-designated as ‘Black or African American”; and individuals who identified themselves as Native American, American Indian, Eskimo, or Alaskan American were re-designated as “Native American”.
Table 1.
Characteristics of pubic ramus fracture patients ages 60-90+ treated in the US, National Electronic Injury Surveillance System 2002-2019.
| Characteristics | Number of Cases N (%) | National Estimates N (%) |
|---|---|---|
| Age groups | — | |
| 60-64 | 297 (11.9%) | 13647 (11.5%) |
| 65-69 | 273 (11.0%) | 12829 (10.8%) |
| 70-74 | 281 (11.3%) | 12639 (10.6%) |
| 75-79 | 368 (14.8%) | 17479 (14.7%) |
| 80-84 | 405 (16.3%) | 19264 (16.2%) |
| 85-89 | 463 (18.6%) | 22367 (18.8%) |
| 90+ | 404 (16.2%) | 20812 (17.5%) |
| Gender | — | |
| Male | 302 (19.2%) | 13840 (18.1%) |
| Female | 1273 (80.8%) | 62463 (81.9%) |
| Race | — | |
| white | 966 (90.1%) | 51554 (92.4%) |
| black or African American | 48 (4.5%) | 1821 (3.3%) |
| Hispanic | 32 (3.0%) | 1304 (2.3%) |
| Asian | 22 (2.1%) | 929 (1.7%) |
| American Indian or Alaska native | 3 (.3%) | 123 (.2%) |
| Native Hawaiian and other Pacific Islander | 1 (.1%) | 93 (.2%) |
| Mechanism of injury | — | |
| fall | 1420 (90.2%) | 69036 (90.5%) |
| Jump | 1 (.1%) | 16 (.0%) |
| Motor vehicle accident | 4 (.3%) | 235 (.3%) |
| Sports | 2 (.1%) | 67 (.1%) |
| Other | 148 (9.4%) | 6948 (9.1%) |
Statistical Analyses
To calculate weighted population estimates of frequency and percent of ramus fractures, the statistical weights provided by the CPSC in the NEISS dataset were utilized. For total national estimates, 95% confidence intervals (CIs) were calculated based on the estimated generalized coefficient of variation for NEISS data provided by the CPSC. Incidence rates and 95% confidence limits per 100,000 person years were then calculated using the weighted estimates relative to the census population estimates. National estimates of ramus fracture related injuries were analyzed using univariate and multivariable logistic regression to assess the independent effects of year, age, gender, race, and mechanism of injury on fragility pubic rami fractures. All tests used a P-value of ≤.05 level of statistical significance. Data analyses were conducted using SPSS v27 (IBM Corp, Armonk, NY, USA).
Results
Among patients 60 years or older, 73,994 lower trunk injuries were identified, of which 1,575 (2.1%) were pubic rami fractures. The mean patient age was 81.3 (range: 60-103)). 302 (19.2%) were males and 1273 (80.8%) were females, respectively. Among all patients between 2002-2019, a total calculated national estimate of 76,303 (95% confidence limit: 61,658 – 90,949) rami fracture cases were observed, in which 69,036 (90.5%) were caused by falls Table 1. The calculated overall incidence rate of 13.5 per 1,000,000 person-years (95% confidence limit: 9.92-17.01). With regards to race, over ninety percent of patients identified as white. Additionally, 90.2% of pubic rami fractures were due to a fall from standing height. Table 1 details the number of cases and national estimates of ramus fractures by age group, gender, race/ethnicity, and mechanism of injury.
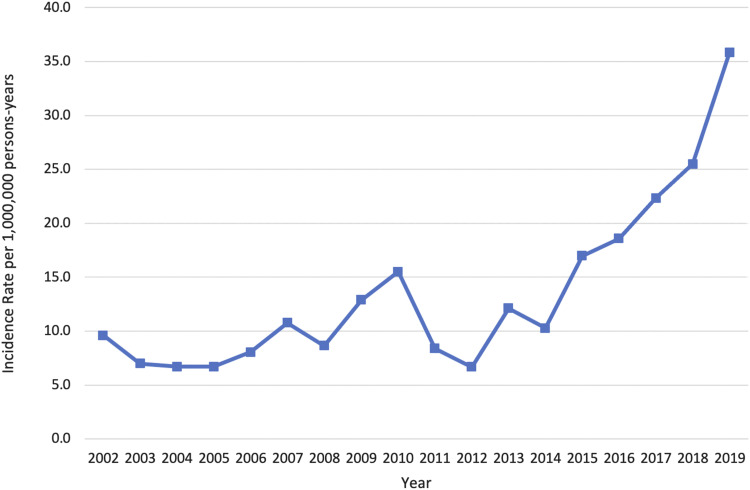
Figure 1 reports the annual incidence rates of pubic rami fractures between 2002-2019. The largest increase in incidence (48.9%) occurred between 2018- 2019 (P < .001). Multivariable logistic regression demonstrated that the relative risk of osteoporotic pubic rami fractures increases 10% per year Table 2.
Figure 1.
Incidence of ramus fractures in the US by year from 2002 to 2019.
Table 2.
Multivariable logistic regression assessing independent variables associated with fragility pubic rami fractures.
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| Independent Variable | OR | 95% CI | P-Value | OR | 95% CI | P-Value |
| Age groups | — | |||||
| 60-64 | Ref | Ref | Ref | Ref | Ref | Ref |
| 65-69 | 1.1 | 1.0-1.1 | <.001 | 1.0 | 1.0-1.1 | .699 |
| 70-74 | 1.6 | 1.6-1.7 | <.001 | 1.4 | 1.3-1.4 | <.001 |
| 75-79 | 2.5 | 2.4-2.6 | <.001 | 2.1 | 2.1-2.2 | <.001 |
| 80-84 | 3.2 | 3.1-3.3 | <.001 | 2.3 | 2.2-2.4 | <.001 |
| 85-89 | 4.3 | 4.2-4.5 | <.001 | 3.2 | 3.1-3.3 | <.001 |
| 90+ | 5.7 | 5.5-5.9 | <.001 | 3.4 | 3.3-3.6 | <.001 |
| Gender | — | |||||
| Male | Ref | Ref | Ref | Ref | Ref | Ref |
| Female | 2.9 | 2.8-2.9 | <.001 | 2.4 | 2.3-2.4 | <.001 |
| Race | — | |||||
| white | Ref | Ref | Ref | Ref | Ref | Ref |
| black or African American | 0.4 | .4-0.4 | <.001 | 0.4 | .4-0.5 | <.001 |
| Hispanic | 0.8 | .7-0.8 | <.001 | 0.8 | .8-0.9 | <.001 |
| Asian | 1.2 | 1.2-1.3 | <.001 | 1.2 | 1.1-1.2 | <.001 |
| American Indian or Alaska native | 1.0 | .8-1.2 | .904 | 0.9 | .8-1.1 | .553 |
| Native Hawaiian and other Pacific Islander | 2.7 | 2.2-2.3 | <.001 | 2.2 | 1.8-2.7 | <.001 |
| Mechanism of injury | — | |||||
| fall | 4.8 | 4.7-4.9 | <.001 | 3.3 | 3.2-3.4 | <.001 |
| Jump | 0.6 | .4-1.0 | .048 | — | ||
| Motor vehicle accident | 3.8 | 3.3-4.2 | <.001 | 3.7 | 3.2-4.4 | <.001 |
| Sports | 0.3 | .3-0.4 | <.001 | 0.6 | .5-0.8 | <.001 |
| Other | Ref | Ref | Ref | Ref | Ref | Ref |
| Year | 1.05 | 1.05-1.05 | <.001 | 1.10 | 1.09-1.10 | <.001 |
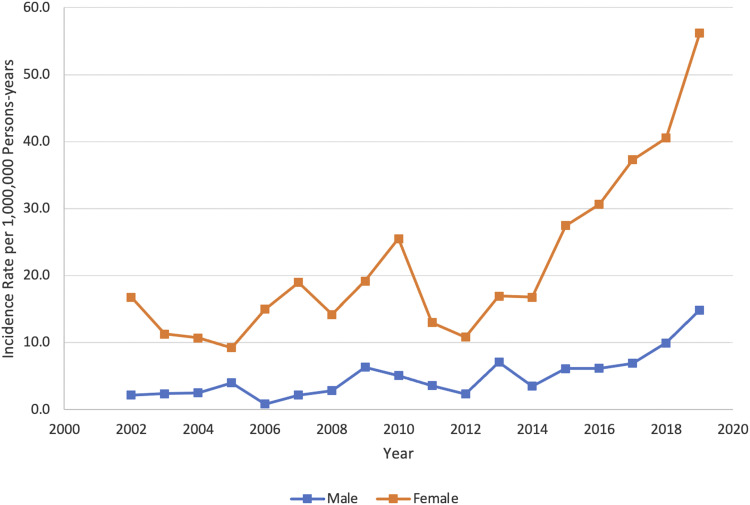
To further assess sub-group trends, Figure 2 displays the incidence rates of pubic rami fractures among males and females. In terms of national estimates, 13,840 (18.1%) and 62,463 (81.9%) of patients with pubic rami fracture were male and female, respectively. Multivariable logistic regression demonstrated that females have a 2.4 (95% CI: 2.3-2.4; P < .001) increased relative risk of fragility pubic rami fractures when compared to males controlling for age, race, year, and mechanism of injury Table 2. Figure 3 demonstrates that the incidence of fragility pubic rami fractures have a statistically significant increased trajectory per decade for both males and females. The incidence rate of pubic rami fractures is significantly greater for females than males (P<.001).
Figure 2.
Incidence of ramus fractures in the US: by gender, 2002 to 2019.
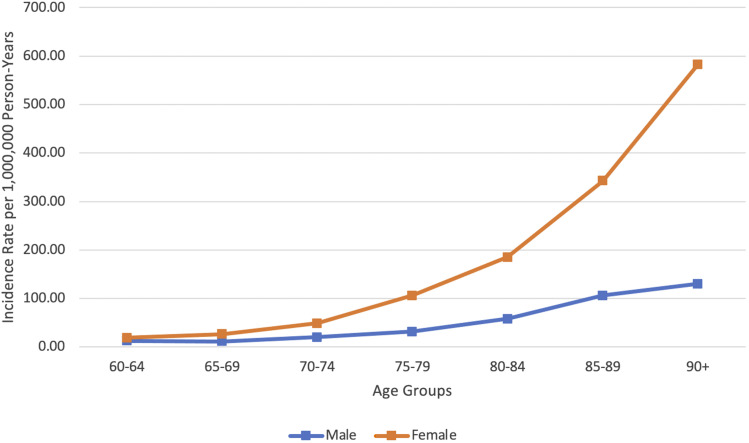
Figure 3.
Incidence of ramus fractures in the US: by age groups and gender, 2002 to 2019.
With regards to age, Figure 3 demonstrates the general incidence of ramus fractures stratified by half-decade and gender. The incidence of fragility pubic rami fracture approximately doubles itself at 5 year intervals starting at 70 years of age for women and 1.5 times for men. Female patients older than 90 years reported a 31.0 times increased incidence of fragility pubic rami fractures compared to patients 60-65 years old (582.4 vs 18.8 per 1,000,000 person-years). Male patients older than 90 years reported a 10.0 times increased incidence compared to patients 60-65 years old (129.9 vs 13.0 per 1,000,000 person-years).
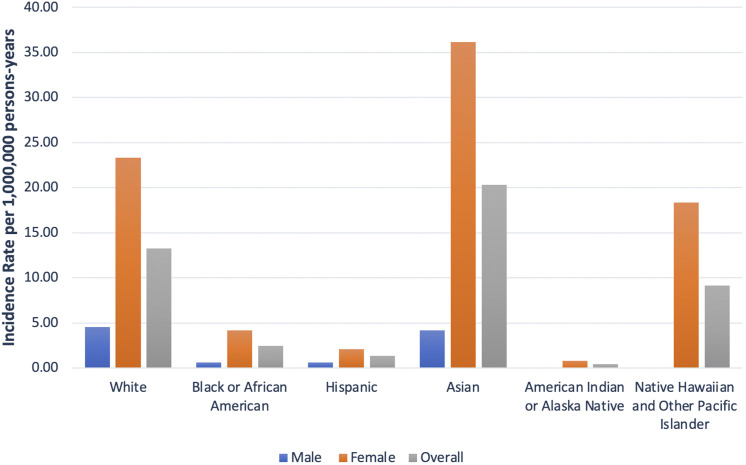
Evaluation of pubic rami fractures by ethnic groups demonstrated considerable variation. The overall incidence rate was highest in Asian group (36.18 per 1,000,000 females and 4.19 per 1,000,000 men), followed by white (23.35 per 1,000,000 females and 4.53 per 1,000,000 men) and Native-American groups (18.38 per 1,000,00 females and 0 per 1,000,000 men). Multivariable logistic regression demonstrated that Asians and Native Hawaiians report a 1.2 (95% CI: 1.1-1.2; P < 0001) and 2.1 (95% CI: 1.7-2.6; P < 0001) increased relative risk compared to whites controlling for age, race, year, and mechanism of injury, respectively. This trend remains consistent among females; however, among males, Whites reported the highest overall incidence rate (4.53 per 1,000,000 men), followed by Asians (4.19 per 1,000,000 men) and Hispanics (.65 per 1,000,000 men) Figure 4. Finally, the estimated incidence rates of ramus fractures found in Native American and Native Hawaiian males are virtually zero based on this sample collection.
Figure 4.
Incidence of ramus fractures in the US: by race and gender, 2002 to 2019.
Discussion
The aims of this study were to calculate the incidence rates and evaluate racial and gender differences among patients with fragility pubic rami fractures presenting to the emergency department. Our results indicate that overall incidence of fragility pubic rami fractures presenting to the emergency department was 13.47 per 1,000,000 people. Interestingly, pubic rami fractures among the elderly in the U.S. declined slightly between 2002 and 2012, then steadily increased from 2012 to 2019. This corresponds with trends in previous work that suggests incidence of osteoporotic pelvic ring fractures are steadily rising.2,14,15 From 2012-2019, fragility pubic rami fracture rates in males and females increased 7 and 5-fold, respectively. Furthermore, previous studies have demonstrated a 24% increase in pelvic ring fractures among elderly individuals has been observed in the US between 1993-2010 with a concurrent 20.5 and 31.6% age-adjusted decrease in hip fractures among men and women, respectively.16,17
Of note, the rise of fragility fractures has been associated with large health care cost burden. Williams et al reported $30,000 all-cause total healthcare costs in the 12 months following a sustained fragility fracture. Among those patients, 6.6% of patients sustained an additional fragility fracture. To control both the rise of preventable fragility fracture incidence and cost, initiatives such as the American Orthopaedic Association’s Own the Bone program have been developed. Bunta et al demonstrated a positive effect among the behaviors of medical professionals with regards to holistic coordinated osteoporosis workup and management among patients who sustained a fragility fracture. 12 Furthermore, Gardner et al conducted a randomized control trial and observed a significant increase in patient osteoporosis management compliance following the introduction of a perioperative osteoporosis patient education program. 18
To better identify patients at high risk pubic rami fragility fracture patients who could benefit from a perioperative osteoporotic management program, our study reported that females have a 4.4 increased odds of fragility pubic rami fractures when compared to men. Furthermore, the national average estimate calculations demonstrated females to have a 4.5-increased odds of reporting a fragility pubic rami when compared to men. The literature has consistently reported the correlation bone mineral density with osteoporotic fracture risk. 19 In particular, older females have a 2-3-fold increased risk of hip fracture compared to males due to the abrupt estrogen decline and subsequent increased risk in osteoporosis following menopause. 20
Among males and females, fragility pubic rami fracture incidence rates varied by reported race. Among males, our study demonstrated highest rates of fragility pubic rami fractures were observed in Asian and white men. No osteoporotic pubic ramus fractures were observed in Pacific Islander or Native American men. Interestingly, no strong consensus exists with regards to race and fracture risk among elderly men.21-23
Among females, Asian females exhibited the highest fracture rate, followed by white and black females. Our finding corresponds with recent studies that report black females to have lower risk of osteoporosis compared to white and Asian females. 24 Pothiwala et al evaluated disparities amongst ethnic groups with regard to access to healthcare, effectiveness of medications, screening for osteoporosis, nutrition, and physical activity. 25 It was observed that black females have a greater bone mineral density than age- and size-matched white females.
Furthermore, studies have reported that Native American females have similar rates of osteoporosis to white females.20,24-26 Barrett-Connor et al evaluated 197,848 black, Asian, Hispanic, and Native American post-menopausal females sampled from the National Osteoporosis Risk Assessment (NORA) database. and observed that black females had the highest average bone mineral density (BMD) followed by Hispanic females, and Asians, Native Americans, and Whites had the lowest.24,27
Osteoporotic pubic ramus fractures are almost always associated with concurrent posterior pelvic ring injuries. The osteoporotic sacrum is highly susceptible to fracture at physiologic loads, but previous work describes the unreliability of diagnosing posterior pelvic ring injuries on standard AP pelvis roentgenograms.28,29 Beckmann et al reported that sacral fractures were reported in up to 60% of pelvic trauma patients. Longitudinal fractures were almost always associated with additional pelvic ring injuries. 30 Furthermore, Berg et al observed that 47% injuries to the sacrum, the sacroiliac joints, and injuries to the posterior ilium that were observed on CT scan, yet missed on standard radiographs. 31 Additionally, Cosker et al reported 90% of patients presenting with pubic rami fractures also sustained sacral fractures identified on MRI. 32 Populations that exhibit higher rates of pubic rami fractures may thus particularly benefit from routine advanced imaging when these fractures are initially identified by conventional radiographs.
Although this is the largest evaluation of fragility pubic rami fractures presenting to the emergency room, limitations must be addressed. Our study was principally limited by lack of information regarding medication and comorbidity history. Substantial literature has been reported with regards to the use of bisphosphonates and other anti-osteoporotic agent for osteoporotic fragility fracture prevention. The meta-analysis performed by Eastell et al identifies the role of bisphosphonates in increasing bone mineral density and decreasing the risk of hip and vertebral fractures by up to 42% and 56%, respectively, in a 5 year period. 33 Therefore, future studies are required to evaluate the role of these medications in the setting of fragility pubic rami fractures.
Conclusion
Osteoporotic pubic rami fractures are a common injury presenting to emergency departments in the United States. This is the first large-scale study in the United States to investigate the national epidemiology of osteoporotic pubic ramus fractures. Incidence data by age, gender, and ethnicity were stratified identifying white females and Asian males at increased risk for fragility pubic rami fractures. Further prospective investigation is required to confirm these study findings.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Ryan M Kong https://orcid.org/0000-0001-8493-799X
Olivia C Tracey https://orcid.org/0000-0002-3563-6696
Zachary Mallon https://orcid.org/0000-0003-2868-7134
References
- 1.Cooper C, Campion G, Melton LJ, 3rd. Hip fractures in the elderly: A world-wide projection. Osteoporos Int. 1992;2:285-289. DOI: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 2.Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M. Epidemiology of osteoporotic pelvic fractures in elderly people in Finland: Sharp increase in 1970-1997 and alarming projections for the new millennium. Osteoporos Int. 2000;11:443-448. DOI: 10.1007/s001980070112. [DOI] [PubMed] [Google Scholar]
- 3.Rollmann MF, Herath SC, Kirchhoff F, et al. Pelvic ring fractures in the elderly now and then - A pelvic registry study. Arch Gerontol Geriatr. 2017;71:83-88. DOI: 10.1016/j.archger.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 4.Soles GLS, Ferguson TA. Fragility fractures of the pelvis. Current Reviews in Musculoskeletal Medicine. 2012;5:222-228. DOI: 10.1007/s12178-012-9128-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nanninga GL, de Leur K, Panneman MJM, van der Elst M, Hartholt KA. Increasing rates of pelvic fractures among older adults: The Netherlands, 1986-2011. Age Ageing. 2014;43:648-653. DOI: 10.1093/ageing/aft212. [DOI] [PubMed] [Google Scholar]
- 6.Maier GS, Kolbow K, Lazovic D, et al. Risk factors for pelvic insufficiency fractures and outcome after conservative therapy. Arch Gerontol Geriatr. 2016;67:80-85. DOI: 10.1016/j.archger.2016.06.020. [DOI] [PubMed] [Google Scholar]
- 7.Hill RMF, Robinson CM, Keating JF. Fractures of the pubic rami. J Bone Joint Surg. 2001;83-B:1141-1144. DOI: 10.1302/0301-620x.83b8.11709. [DOI] [PubMed] [Google Scholar]
- 8.van Dijk WA, Poeze M, van Helden SH, Brink PRG, Verbruggen JPAM. Ten-year mortality among hospitalised patients with fractures of the pubic rami. Injury. 2010;41:411-414. DOI: 10.1016/j.injury.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 9.Koval KJ, Aharonoff GB, Schwartz MC, et al. Pubic rami fracture: A benign pelvic injury? J Orthop Trauma. 1997;11:7-9. DOI: 10.1097/00005131-199701000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Loggers SAI, Joosse P, Jan Ponsen K. Outcome of pubic rami fractures with or without concomitant involvement of the posterior ring in elderly patients. Eur J Trauma Emerg Surg. 2019;45:1021-1029. DOI: 10.1007/s00068-018-0971-2. [DOI] [PubMed] [Google Scholar]
- 11.Leslie MP, Baumgaertner MR. Osteoporotic pelvic ring injuries. Orthop Clin N Am. 2013;44:217-224. DOI: 10.1016/j.ocl.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Bunta AD, Edwards BJ, Macaulay WB, et al. Own the bone, a system-based intervention, improves osteoporosis care after fragility fractures. J Bone Joint Surg. 2016;98:e109. DOI: 10.2106/JBJS.15.01494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Electronic Injury Surveillance System (NEISS) | CPSC.Gov n.D, ■■■. https://www.cpsc.gov/Research--Statistics/NEISS-Injury-Data (accessed August 27, 2021). [Google Scholar]
- 14.Prieto-Alhambra D, Avilés FF, Judge A, et al. Burden of pelvis fracture: A population-based study of incidence, hospitalisation and mortality. Osteoporos Int. 2012;23:2797-2803. DOI: 10.1007/s00198-012-1907-z. [DOI] [PubMed] [Google Scholar]
- 15.Kannus P, Palvanen M, Parkkari J, Niemi S, Järvinen M. Osteoporotic pelvic fractures in elderly women. Osteoporos Int. 2005;16:1304-1305. DOI: 10.1007/s00198-005-1941-1. [DOI] [PubMed] [Google Scholar]
- 16.Wang Z, Bhattacharyya T. Trends in incidence of subtrochanteric fragility fractures and bisphosphonate use among the US elderly, 1996-2007. J Bone Miner Res. 2011;26:553-560. DOI: 10.1002/jbmr.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sullivan MP, Baldwin KD, Donegan DJ, Mehta S, Ahn J. Geriatric fractures about the hip: divergent patterns in the proximal femur, acetabulum, and pelvis. Orthopedics. 2014;37:151-157. DOI: 10.3928/01477447-20140225-50. [DOI] [PubMed] [Google Scholar]
- 18.Gardner MJ, Brophy RH, Demetrakopoulos D, et al. Interventions to improve osteoporosis treatment following hip fracture. J Bone Joint Surg. 2005;87:3-7. DOI: 10.2106/JBJS.D.02289. [DOI] [PubMed] [Google Scholar]
- 19.Van der Klift M, Pols HAP, Geleijnse JM, Van der Kuip DAM, Hofman A, De Laet CEDH. Bone mineral density and mortality in elderly men and women: The Rotterdam study. Bone. 2002;30:643-648. 10.1016/S8756-3282(02)00670-1. [DOI] [PubMed] [Google Scholar]
- 20.Evers SE, Orchard JW, Haddad RG. Bone density in postmenopausal North American Indian and Caucasian females. Hum Biol. 1985;57:719-726. [PubMed] [Google Scholar]
- 21.Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res. 2011;469:1913-1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shin M-H, Zmuda JM, Zmuda JM, et al. Race/ethnic differences in associations between bone mineral density and fracture history in older men. Osteoporos Int. 2014;25:837-845. DOI: 10.1007/s00198-013-2503-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu LH, Chandra M, Gonzalez JR, Lo JC. Racial and ethnic differences in hip fracture outcomes in men. Am J Manag Care. 2017;23:560-564. [PubMed] [Google Scholar]
- 24.Thu WPP, Logan SJS, Cauley JA, Kramer MS, Yong EL. Ethnic differences in bone mineral density among midlife women in a multi-ethnic Southeast Asian cohort. Archives of Osteoporosis. 2019;14:80. DOI: 10.1007/s11657-019-0631-0. [DOI] [PubMed] [Google Scholar]
- 25.Pothiwala P, Evans EM, Chapman-Novakofski KM. Ethnic variation in risk for osteoporosis among women: a review of biological and behavioral factors. J Wom Health. 2006;15:709-719. DOI: 10.1089/jwh.2006.15.709. [DOI] [PubMed] [Google Scholar]
- 26.Frech T, Ma K-n., Ferrucci ED, Lanier AP, McFadden M, Tom-Orme L, et al. Prevalence of fracture and osteoporosis risk factors in American Indian and Alaska Native people. J Health Care Poor Underserved. 2012;23:1157-1173. DOI: 10.1353/hpu.2012.0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kellie SE, Brody JA. Sex-specific and race-specific hip fracture rates. Am J Publ Health. 1990;80:326-328. DOI: 10.2105/ajph.80.3.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Waites MD, Mears SC, Mathis JM, Belkoff SM. The strength of the osteoporotic sacrum. Spine. 2007;32:E652-E655. DOI: 10.1097/BRS.0b013e318158c552. [DOI] [PubMed] [Google Scholar]
- 29.Rommens PM, Dietz SO, Ossendorf C, Pairon P, Wagner D, Hofmann A. Fragility fractures of the pelvis: Should they be fixed? Acta Chir Orthop Traumatol Cech. 2015;82:101-112. [PubMed] [Google Scholar]
- 30.Beckmann N, Cai C. CT characteristics of traumatic sacral fractures in association with pelvic ring injuries: Correlation using the Young-Burgess classification system. Emerg Radiol. 2017;24:255-262. DOI: 10.1007/s10140-016-1476-0. [DOI] [PubMed] [Google Scholar]
- 31.Berg EE, Chebuhar C, Bell RM. Pelvic trauma imaging. J Trauma Inj Infect Crit Care. 1996;41:994-998. DOI: 10.1097/00005373-199612000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Cosker TDA, Ghandour A, Gupta SK, Tayton KJJ. Pelvic ramus fractures in the elderly. Acta Orthop. 2005;76:513-516. DOI: 10.1080/17453670510044634. [DOI] [PubMed] [Google Scholar]
- 33.Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D. Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab. 2019;104:1595-1622. DOI: 10.1210/jc.2019-00221. [DOI] [PubMed] [Google Scholar]