Abstract
Background
Adverse childhood experiences have a significant impact on different mental disorders.
Objective
To compare differences in adverse childhood experiences among those with different mental disorders and their relationships in a cross-disorder manner.
Methods
The study included 1513 individuals aged ≥18 years : 339 patients with substance use disorders, 125 patients with schizophrenia, 342 patients with depression, 136 patients with bipolar disorder, 431 patients with obsessive-compulsive disorder (OCD), and 140 healthy controls. The Early Trauma Inventory Self Report-Short Form was used to investigate childhood traumatic experiences, and the Addiction Severity Index, Positive and Negative Syndrome Scale, Hamilton Depression Scale, Young Mania Rating Scale, and Yale-Brown Obsessive-Compulsive Scale were used to assess mental disorder severity. Correlation and multivariate logistic regression were analysed between adverse childhood experiences and clinical features.
Results
Levels of adverse childhood experiences were significantly different among different mental disorders. Moreover, 25.8% of patients with substance use disorders reported childhood trauma, which was significantly higher than found in the other four psychiatric disorder groups. Emotional abuse scores were positively correlated with disease severity: the higher the total trauma score, the more severe the mental disorder.
Conclusions
Adverse childhood experiences are a common phenomenon in those with mental disorders, and the level of trauma affects mental disorder severity. Emotional abuse is closely related to many mental disorders. The incidence or severity of mental disorders can be reduced in the future by reducing the incidence of adverse childhood experiences or by timely intervention in childhood trauma.
Keywords: child psychiatry
Key messages.
What is already known on this topic
Adverse childhood experiences are closely related to the occurrence and development of many mental disorders.
Adverse childhood experiences have negative effects on an individual’s physiology, cognition, behaviour and psychology, and increase the risk of developing severe mental disorders.
Cumulative childhood trauma exposure increases the risk of developing psychopathology in adulthood as well as poor social functioning.
What this study adds
Childhood trauma is a common phenomenon in those with mental disorders, and the level of trauma affects mental disorder severity.
Emotional abuse scores had the trend to be positively correlated with disease severity in the schizophrenia, depression and bipolar group, and it was a major risk factors for obsessive-compulsive disorder (OCD) severity.
The age at assessment and chronological background are important for the evaluation of trauma.
How this study might affect research, practice or policy
The incidence or severity of mental disorders can be reduced in the future by reducing the incidence of adverse childhood experiences or by timely intervention in childhood trauma.
Introduction
Adverse childhood experiences (ACEs) are closely related to the occurrence and development of many mental disorders. Different subtypes of ACEs may have different effects on the occurrence of these disorders. At present, few studies have analysed the influence of childhood trauma on different types of mental disorders. This study compared differences in ACEs among those with different mental disorders and their relationships in a cross-disorder manner.
ACEs include child abuse (emotional, physical or sexual), child neglect (emotional or physical), and household dysfunction (domestic violence, substance abuse, mental illness, criminal activity, or parental absence). Recent studies have shown that ACEs have negative effects on an individual’s physiology, cognition, behaviour and psychology,1 and increase the risk of developing severe mental disorders.2 ACEs were associated with severe clinical symptoms, such as severe positive symptoms of psychosis,3 greater rates of suicidality,4 increased prevalence of substance use,5 pronounced perceptual disturbances and affective symptoms,6 diminished neuropsychological performance,7 more frequent insomnia,8 and a more refractory and prolonged illness course.9 ACEs10 have been considered by some scholars as a potential risk factor for both non-suicidal self-injury and suicidal behaviour. The increased vulnerability to suicidal behaviour seems to be, at least partially, related to experiences of childhood traumatic experiences.
There are robust associations between accumulated exposures to ACEs and health risks—including substance use disorders (SUDs) and co-occurring psychopathology—throughout the lifespan.11 12 A recent large prospective study found that cumulative childhood trauma exposure increases the risk of developing psychopathology in adulthood as well as poor social functioning.13 Physical abuse, sexual abuse and physical neglect were significantly associated with reduced scores in working memory, executive function and verbal tasks.14
As a severe neuropsychiatric disorder, schizophrenia was considered to have significant associations with ACEs.15 Many scholars have even considered that ACEs are a potential risk factor for schizophrenia and suggest a causal relationship between them.16 The literature suggests that the greater the severity of ACEs, the greater the severity of the schizophrenia symptoms.17 ACEs have been repeatedly shown to negatively impact ‘recovery’ among patients with schizophrenia.18 Among the latter, the most frequent subtype of trauma was emotional neglect, but rates of physical abuse and physical neglect were also significantly increased.19 20
It must be noted that the effects of ACEs are not specific to schizophrenia. SUDs are among the most commonly occurring disorders in the USA.21 Some evidence has suggested that sexual abuse,22 23 physical abuse,24 and emotional abuse25 were associated with SUDs. In patients with SUD, severe sexual and physical abuse experiences were significantly associated with lifetime heroin use, whereas lifetime cocaine use appeared to be associated only with severe physical abuse.26
ACEs are also associated with the development of emotional disorders.27 Major depressive disorder (MDD) has been associated with changes in biological stress systems.28 ACEs enhanced the risk for MDD and may lead to permanent changes in biological stress regulation systems, including cortisol levels, and cognitive functions.29 Childhood sexual abuse and physical abuse were related to high levels of depression in adults.30 Emotional abuse and neglect and physical and sexual abuse were related to depressive symptoms in female samples.31 In addition, patients with bipolar disorder had a higher prevalence of ACEs; they also had poorer response to treatment,32 higher numbers of psychiatric hospitalisations,33 and lower premorbid functioning levels.34
Some evidence suggests that ACEs may not only cause the emergence of obsessive-compulsive disorder (OCD), but also influence individuals to show disease progression, increase in intensity and / or frequency, and changes in content.35 ACEs have been associated with severe symptoms, higher suicide probability,36 and resistance to treatment37 in patients with OCD. ACEs, specifically emotional abuse and neglect, significantly increase the odds of having OCD.38
Some studies have shown that ACEs also increased the incidence of smoking behaviour.39 Substance abuse seems to mediate ACEs and multiple mental disorders, and the abuse of substances with psychoactive properties, such as alcohol, amphetamines, cannabis, cocaine, and hallucinogens, has been associated with a greater risk for psychotic experiences in the general population.40 There is a significant interaction between childhood sexual abuse and cannabis use, and this may contribute to the development of schizophrenia. Prior studies have found that mood and anxiety disorders (eg, MDD) usually precede the onset of SUDs, and mood and anxiety disorders partially mediate the relationship between ACEs and lifetime diagnoses of SUDs.41 People who have experienced abuse tend to become depressed more frequently and, thus, may more often use cannabis to alleviate depressive symptoms or more likely develop dysfunctional coping strategies such as self-medication to reduce trauma-related stress.42
The five mental disorders included in this paper—SUD, schizophrenia, depression, bipolar disorder, and OCD—cover four different directions of the International Classification of Diseases, 10th Revision classification of mental and behavioural disorders. The above research suggests that ACEs have different degrees of influence on the development of multiple psychiatric disorders, but the severity of symptoms varies among individuals who experience ACEs, and the extent to which emotional abuse or physical trauma affects disorders is not yet known. Therefore, this study intends to include groups with different clinical descriptions and diagnostic orientations of the five types of mental disorders to compare differences in ACEs.
Materials and methods
Subjects
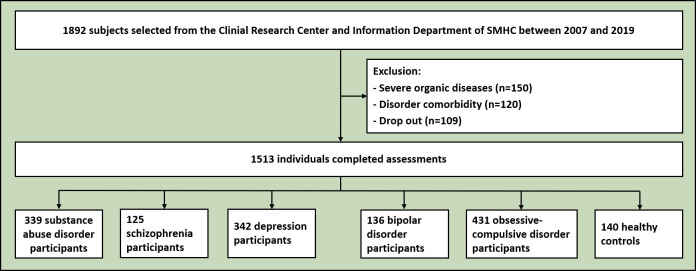
All subjects recruited were older than 18 years and had at least a junior high school education level. They were screened using the Mini-International Neuropsychiatric Interview (MINI) to assess whether there was a history of any Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) psychiatric disorder. 1892 subjects were selected from the Shanghai Mental Health Center (SMHC) between 2007 and 2019. Data from patients and healthy volunteers in this retrospective study were gathered from the Clinical Research Center and Information Department of SMHC. A total of 1513 individuals completed the assessment. All participants signed informed consent for data recollection. Among them, patients need to meet the inclusion criteria for 5 disorders in the DSM-IV. Exclusion criteria were the presence of (a) severe organic diseases requiring urgent treatment at baseline assessment, (b) severe cognitive, motor or visual impairment, (c) any DSM-IV psychiatric disorder other than substance abuse, schizophrenia, depression, bipolar disorder or OCD (MINI assessment screening), or (d) any Axis I psychiatric disorder comorbidity. The subjects were divided into six groups as follows: Group 1 was the substance abuse group (n=339), including 122 males and 217 females, with a mean age of 32.0 (26.0, 36.0) years. Group 2 was the schizophrenia group (n=125), including 68 males and 57 females, with a mean age of 33.0 (25.0, 60.0) years. Group 3 was the depression group (n=342), including 128 males and 214 females, with a mean age of 31.5 (24.3, 48.0) years. Group 4 was the bipolar disorder group (n=136), including 69 males and 67 females, with a mean age of 29.5 (22.8, 45.0) years. Group 5 was the OCD group (n=431), including 252 males and 179 females, with a mean age of 27.0 (22.0, 34.0) years. Group 6 was the healthy control (HC) group (n=140), of which 75 were male and 65 were female, and the mean age was 27.0 (24.0, 34.0) years. One hundred and forty HCs were recruited from volunteers. Individuals who had any psychiatric history or family history were excluded. The flow chart is shown in figure 1.
Figure 1.
Flowchart of participant recruitment. SMHC, Shanghai Mental Health Center.
Tools
Five scales were used to assess the severity of disease. (a) The Addiction Severity Index43 was used to identify and assess seven potential problem areas in the substance abuse group: medical condition, employment/support status, alcohol use, drug use, legal issues, family/social issues, and psychiatric symptoms. (b) The Positive and Negative Syndrome Scale (PANSS)44 is a medical scale used to measure the severity of symptoms in patients with schizophrenia. It is widely used in the research of antipsychotics. Positive and negative refer to the two sets of symptoms of schizophrenia, with positive symptoms referring to the excess of distortion in normal functioning, such as hallucinations and delusions, and negative symptoms referring to the loss of normal function. In the schizophrenia group, total PANSS scores of 30–58 were considered normal; 58–75, mild; 75–95, moderate; 95–116, severe; and 116–210, extremely severe. (c) The Hamilton Depression Scale (HAMD)45 was developed by Hamilton in 1960 and is the most commonly used scale for the clinical assessment of depression. The HAMD was administered to patients who were independently assessed after the interview and observation, and were assessed before and after treatment by two trained raters. This scale can evaluate the severity of the disease and the effects of treatment. In the depression group, HAMD total scores of <7 were considered normal; 7–17, mild; 17–24, moderate; and >24, severe. (d) The Young Mania Rating Scale (YMRS)46 is an 11-item scale used to assess the severity of mania in patients diagnosed with bipolar disorder. In the bipolar disorder group, total YMRS scores of 0–5 were considered normal; 6–12, mild; 13–19, moderate; 20–29, severe; and>30, extreme. (e) The Yale-Brown Obsessive-Compulsive Scale (Y-BOCS)47 is one of the most widely used clinical scales for OCD. In the OCD group, total Y-BOCS scores of 0–7 were considered normal; 8–16, mild; 17–25, moderate; 26–32, severe; and >33, extremely severe.Besides, the Early Trauma Inventory Self Report-Short Form (ETISR-SF)48 was used to evaluate four types of ACEs before the age of 18 and their severity with 27 items, including 11 items for general trauma, 5 items for physical trauma, 5 items for emotional abuse, and 6 items for sexual trauma. All the scores were summed for a total score. The higher the individual’s score, the more severe the effects of ACEs.
Statistical analysis
Independent sample t-tests (or non-parametric tests) and χ2 tests were used to compare the differences between the groups. R V4.0 was used as the statistical tool. For multifactor comparisons, ordered multiclassification logistic regression was used. Comparison between five mental disorder groups (multigroup comparison) with disease severity as the dependent variable and trauma scores were used as independent variables for ordered multiple classification logistic regression. Kruskal-Wallis H test was used for measurement data, and RxC contingency table χ2 was used for counting data between multigroup comparisons. Since substance use cannot be characterised by the rank conversion of disease severity, multivariate regression was compared between only the other four disease groups.
Results
The total scores for childhood trauma differed significantly among different mental disorders (χ2=39.845, p<0.001, figure 2). The y-coordinate, ETI_Tot, represents the total score of the Early Trauma Inventory Self Report-Short Form. The horizontal coordinate represents the comparison of differences in substance abuse, schizophrenia, depression, bipolar disorder and OCD. Table 1 shows that there are significant differences in the total scores for childhood trauma and the subdivisions of each dimension of trauma between the multigroup comparisons of the five disorders.
Figure 2.
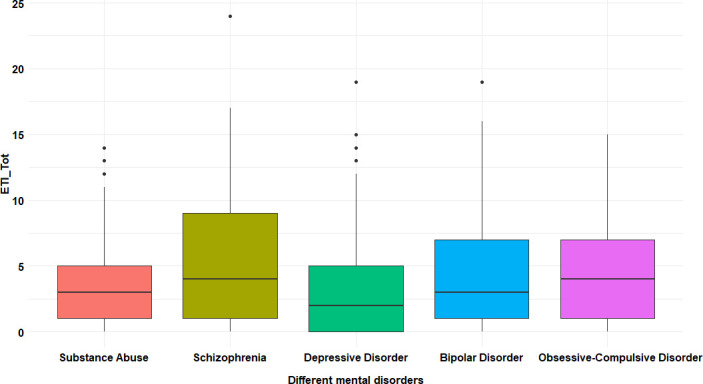
Total childhood trauma scores in patients with different mental disorders. ETI-Tot: total score of the Early Trauma Inventory Self Report-Short Form.
Table 1.
Comparative analysis of trauma scores between five groups with mental disorders
| Substance abuse (n=339) |
Schizophrenia (n=125) |
Depression (n=342) |
Bipolar disorder (n=136) |
OCD (n=431) |
Kruskal-Wallis test | ||
| H | P value | ||||||
| ETI, median (Q1, Q3) | |||||||
| I | 1 (0, 2) | 1 (0, 2) | 0 (0, 1) | 1 (0, 2) | 1 (0, 2) | 15.152 | 0.004 |
| II | 1 (0, 2) | 1 (0, 2) | 0 (0, 1) | 0.5 (0, 2) | 1 (0, 3) | 51.861 | <0.001 |
| III | 0 (0, 1) | 1 (0, 3) | 0 (0, 2) | 1 (0, 3) | 1 (0, 3) | 79.953 | <0.001 |
| IV | 0 (0, 1) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 0 (0, 0) | 18.655 | <0.001 |
| Total | 3 (1, 5) | 4 (1, 9) | 2 (0, 5) | 3 (1, 7) | 4 (1, 7) | 39.845 | <0.001 |
I, general trauma; II, physical trauma; III, emotional abuse; IV, sexual trauma.
ETI, ETISR-SF scores; OCD, obsessive-compulsive disorder.
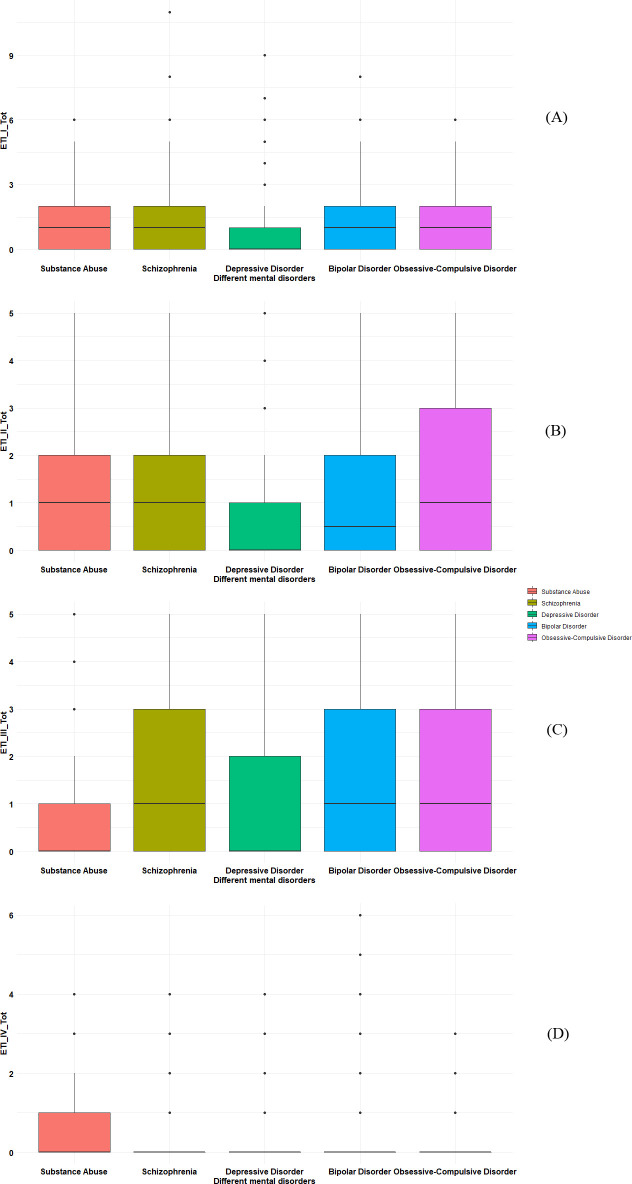
In the substance abuse group, 25.8% of patients reported experiencing sexual trauma in childhood. ETI_I_Tot, ETI_II_Tot, ETI_III_Tot and ETI_IV_Tot, respectively, represent the total scores of the childhood general trauma, childhood physical trauma, childhood emotional abuse and childhood sexual trauma.
The results showed that childhood emotional abuse had a significant impact on the severity of the disease in the schizophrenia and OCD groups.
The relationship of the severity of the five mental disorders and childhood trauma was assessed with multiple factor regression (figure 3, table 2). As a risk factor, the higher the childhood trauma score, the more serious the mental disorder. The total ETISR-SF score level indicated a level of risk (OR=1.04, p=0.012, table 3).
Figure 3.
Childhood trauma scores across mental disorders. (A) Childhood general trauma scores. (B) Childhood physical trauma scores. (C) Childhood emotional abuse scores. (D) Childhood sexual trauma scores. ETI_I_Tot, Childhood general trauma scores; ETI_II_Tot, Childhood physical trauma scores; ETI_III_Tot, Childhood emotional abuse scores; ETI_IV_Tot, Childhood sexual trauma scores.
Table 2.
Multiple regression between the severity of disorders and childhood trauma
| ETI | Schizophrenia | Depression | Bipolar disorder | OCD | ||||||||
| OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | OR | 95% CI | P value | |
| I | 0.98 | 0.80 to 1.19 | 0.824 | 0.85 | 0.72 to 1.01 | 0.069 | 1.00 | 0.75 to 1.32 | 0.996 | 0.93 | 0.79 to 1.09 | 0.350 |
| II | 1.07 | 0.80 to 1.43 | 0.639 | 1.10 | 0.92 to 1.32 | 0.306 | 1.06 | 0.75 to 1.48 | 0.750 | 1.03 | 0.90 to 1.17 | 0.694 |
| III | 1.29 | 1.00 to 1.68 | 0.049 | 1.16 | 0.99 to 1.35 | 0.064 | 1.12 | 0.88 to 1.43 | 0.351 | 1.20 | 1.06 to 1.36 | 0.004 |
| IV | 0.69 | 0.39 to 1.18 | 0.180 | 1.36 | 0.93 to 1.98 | 0.108 | 1.27 | 0.83 to 1.92 | 0.253 | 1.08 | 0.74 to 1.58 | 0.681 |
I, general trauma; II, physical trauma; III, emotional abuse; IV, sexual trauma.
ETI, ETISR-SF scores; OCD, obsessive-compulsive disorder.
Table 3.
The severity of different mental disorders and childhood trauma by demographic characteristics
| OR | 95% CI | P value | |
| Gender | |||
| Male | Ref | ||
| Female | 0.87 | 0.70 to 1.09 | 0.226 |
| Age | |||
| ≤30 years | Ref | ||
| 30–50 years | 0.93 | 0.68 to 1.26 | 0.624 |
| >50 years | 0.54 | 0.37 to 0.78 | 0.001 |
| Marriage | |||
| Divorced | 0.69 | 0.41 to 1.16 | 0.159 |
| Married | Ref | ||
| Single | 0.80 | 0.59 to 1.06 | 0.120 |
| ETI_Tot | 1.04 | 1.01 to 1.07 | 0.012 |
CI, confidence interval; ETI_Tot, total score of the Early Trauma Inventory Self Report-Short Form; OR, odds ratio.
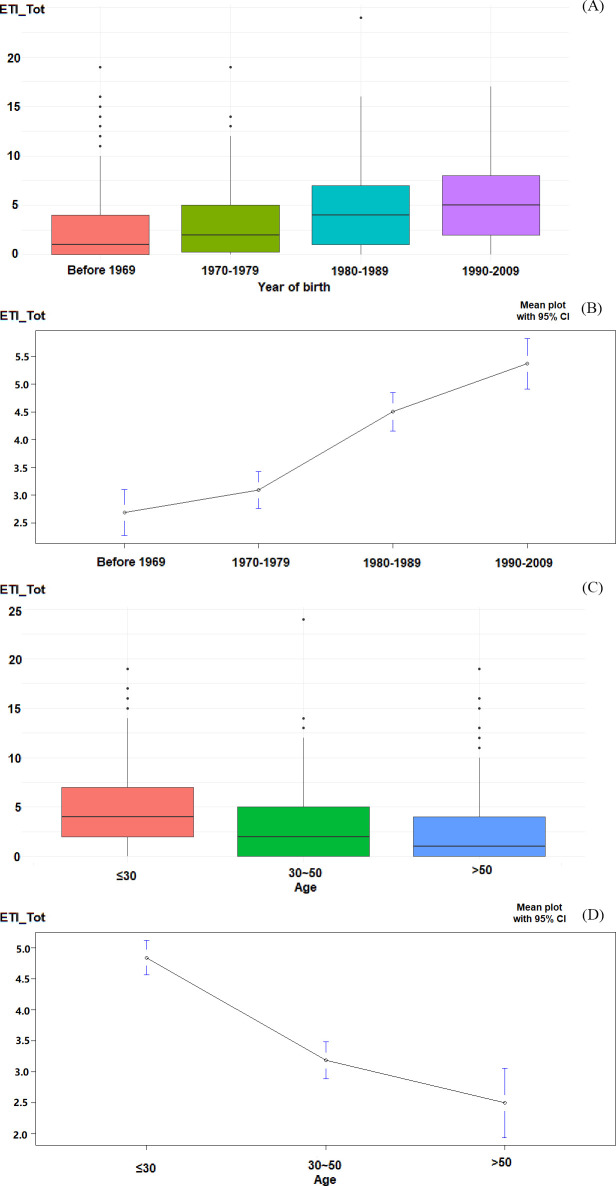
The more recent the date of birth, the higher the trauma score (p<0.001); the younger the age at assessment, the higher the trauma score (p<0.001, figure 4).
Figure 4.
The date of birth and the age at assessment across mental disorders. (A)The date of birth across mental disorders. (B) Analysis of the date of birth influencing adverse childhood experiences (ACEs). (C) The age at assessment across mental disorders. (D) Analysis of the age at assessment influencing ACEs. CI, confidence interval; ETI_Tot, total score of the Early Trauma Inventory Self Report-Short Form.
Discussion
Main findings
By assessing the level of ACEs in patients with five mental disorders, namely substance use, schizophrenia, depression, bipolar disorder and OCD, this study confirmed that ACE is an important risk factor for mental disorders in Chinese culture and further found that trauma of different types may exert varying effects on the severity of mental disorders.
According to the self-development theory, childhood and adolescence are two important stages of rapid physical and mental development. However, due to the immaturity of physical and mental development, weak resistance to stress, poor adaptability and tolerance in childhood, children are most vulnerable to trauma. Meanwhile, the events experienced during this period of trauma can exert profound and lasting impacts on the individual. In general, children having experienced abuse or neglect tend to show low self-esteem and negative self-evaluation, so that it is difficult for them to construct a correct and positive self-concept support system. According to many previous studies,49 50 childhood trauma is an important risk factor for mental disorders. This study found that the type of ACEs an individual experienced had different effects on the severity of various mental disorders. For example, there was no significant difference in the total ETISR-SF score between the depressed and healthy individuals, but the severity of physical trauma, emotional abuse, and sexual trauma was significantly higher in depressed persons than in HCs, and only general trauma did not differ between the two groups. In other words, general trauma may not be the main factor affecting depression, but physical trauma, emotional abuse, and sexual trauma, which are not common in healthy individuals, can significantly increase the incidence of depression. It is generally accepted that depression is more likely to be influenced by social and environmental factors such as stress. Beyond that, general trauma is a common experience with a high prevalence in the general population.51 52 Therefore, even if the ETISR-SF score is not significant, the effect of ACEs on depressed patients cannot be denied. According to the results, the individual’s subjective evaluation of the ACEs may be a relatively more important factor in the onset of depression than just the traumatic event itself, and individuals are more likely to have negative perceptions of infrequent events such as physical trauma, emotional abuse, and sexual trauma, which in turn can lead to the onset of illness.
According to findings from the present study, the levels of ACEs were generally higher in patients with schizophrenia, bipolar disorder, and OCD. Also, there are significant differences in trauma levels, specifically the levels of general trauma, emotional abuse, and sexual trauma, between the HCs and groups with mental disorders. As suggested by some studies, physical trauma is strongly associated with bipolar disorder, but others have reported conflicting results.53 54 That is to say, physical trauma may not be a key factor. The present study clearly supports the latter conclusion. Due to the fact that there are elements of shared genetic susceptibility to schizophrenia, bipolar disorder, and OCD, epigenetic and DNA methylation alterations of genes are considered as potential pathophysiological factors. Biological experiments55 have demonstrated that the glucocorticoid receptor mRNA expression in the hippocampus is decreased and the NR3C1 gene promoter methylation levels are increased in suicidal individuals who suffered ACEs. In addition, stressful stimuli and traumatic events experienced early in life will significantly affect the physiological and behavioural patterns of the organism and can be transmitted across generations.56 The results of this study strongly indicate that more severe negative experiences in childhood predict more severe psychopathic distress in adulthood in these patients. Therefore, clinicians should pay more attention to the impact of negative early childhood experiences on adult mental health and illness.
Sexual trauma from ACEs was significantly more common in substance abuse patients (25.8%) than in other patients. Meanwhile, compared with HCs, no significant difference was found in other dimensions of trauma or the total ETISR-SF scores except for the level of sexual trauma.57 The incidence of sexual trauma in China is 8%, which is much lower than the incidence of other types of trauma. However, sexual trauma is a significant traumatic event, regardless of the age when it occurs, and individuals having experienced it in childhood are more likely to use addictive drugs and alcohol than those who have not. The study found58 59 that as many as 68% of women with substance abuse disorders (including addictive drugs and alcohol) experienced childhood sexual trauma, and the rate of substance abuse or dependence was significantly higher among women who experienced childhood sexual trauma than among those who did not. As revealed by pathophysiological studies,60 altered secretion in the hypothalamic-pituitary-adrenocortical system is the possible mechanism by which negative childhood experiences increase the risk of substance abuse. In addition, substance abuse patients often also have post-traumatic stress disorder, and patients with comorbid substance abuse and post-traumatic stress disorder are more difficult to treat with conventional therapies. Therefore, negative childhood experiences may predict the occurrence of substance abuse or dependence, and it is necessary to provide additional psychological interventions and treatment measures for patients with comorbid substance abuse and other disorders. It was found that the emotional abuse scores were positively correlated with disease severity in the depression, bipolar disorder and compulsive disorder groups, and clinical interventions should be considered for patients who have experienced emotional abuse.
As shown by some studies,61 patient's present age and the age when the trauma occurred are important for the evaluation of trauma. The background of cultural norms and the age at assessment are associated with differences in patients’ understanding and tolerance of negative childhood experiences, which usually result in severe trauma. This study found that the younger the patient, the higher the trauma scores. With the development of society and improved cultural awareness, the general population is no longer ashamed to talk about ACEs, and adolescents, unlike the older people, are more likely to recognize that it is wrong because of the changes to society over the years. Meanwhile, the corresponding exacerbation of ACEs will lead to higher scores of trauma in adolescents. The higher levels of childhood trauma in young adults than in older adults were analysed, and the relationship between ACE scores and the severity of psychiatric disorders was also explored.
Limitations
Despite some meaningful findings in this study, there are a few limitations. First, the effects of education on trauma and disease severity were weakened by the generally higher level of education in the sample of patients with OCD. Second, the multifactorial analysis of disease severity was incomplete when the study of the relationship between trauma and disease severity failed to include indicators such as time of onset, duration of illness, and duration of untreated psychosis in a stepwise fashion. It is hoped that the relevant information can be explored more deeply in a subsequent single-illness analysis to elucidate the factors affecting disease severity. Third, since this group of patients came from a single centre, we could not analyse these issues across regions, races, and multiple centres or effectively represent the overall patient population in China. Therefore, it is necessary to interpret the conclusions with caution. Fourth, the intelligence of the participants might not be adequately represented by their educational level, so future studies should assess the IQ.
Implications
Despite these limitations, our findings reveal associations between ACEs, particularly emotional abuse, and five psychiatric disorders: substance abuse, schizophrenia, depression, bipolar disorder, and OCD.
Biography
Wenjie Gu received a bachelor's degree from Hefei University of Technology in 2012 and a master's degree in bioinformatics from Tongji University in 2015. Since 2015, she has worked at the Shanghai Mental Health Center and served as an information engineer in the Statistics Department. She worked as a contact person at the Shanghai Shenkang Hospital Development Center and correspondent to the China Hospital Network Information Conference. Her research interests include statistical analysis and data governance, including text mining and meta-analysis. Currently, she is responsible for hospital information systems management, software design and functional review. She has participated in several academy-level projects and a consulting research project for the Chinese Academy of Engineering.

Footnotes
Contributors: WG:guarantor. QZ: investigation. ZW: obsessive-compulsive disorder conceptualisation. MZ: substance abuse conceptualisation. ZY: schizophrenia conceptualisation. CY: depression and bipolar disorder conceptualisation.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants and was approved by the Ethics Committee of Shanghai Mental Health Center IRB (IORG number: IORG0002202; ethics approval ID: 2008-23, 2013-21, 2017-19R, 2013-23). Participants gave informed consent to participate in the study before taking part.
References
- 1.Shonkoff JP, Garner AS, Committee on Psychosocial Aspects of Child and Family Health, et al. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012;129:e232–46. 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- 2.Croft J, Heron J, Teufel C, et al. Association of trauma type, age of exposure, and frequency in childhood and adolescence with psychotic experiences in early adulthood. JAMA Psychiatry 2019;76:79. 10.1001/jamapsychiatry.2018.3155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Falukozi E, Addington J. Impact of trauma on attenuated psychotic symptoms. Psychosis 2012;4:203–12. 10.1080/17522439.2011.626867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vos Cde, Thompson A, Paul A. The relationship between childhood trauma and clinical characteristics in ultrahigh risk for psychosis youth. Psychosis 2019;11:1–14. 10.1080/17522439.2019.1582686 [DOI] [Google Scholar]
- 5.Tomassi S, Tosato S, Mondelli V, et al. Influence of childhood trauma on diagnosis and substance use in first-episode psychosis. Br J Psychiatry 2017;211:151–6. 10.1192/bjp.bp.116.194019 [DOI] [PubMed] [Google Scholar]
- 6.Loewy RL, Corey S, Amirfathi F, et al. Childhood trauma and clinical high risk for psychosis. Schizophr Res 2019;205:10–14. 10.1016/j.schres.2018.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Üçok A, Kaya H, Uğurpala C, et al. History of childhood physical trauma is related to cognitive decline in individuals with ultra-high risk for psychosis. Schizophr Res 2015;169:199–203. 10.1016/j.schres.2015.08.038 [DOI] [PubMed] [Google Scholar]
- 8.Laskemoen JF, Aas M, Vaskinn A, et al. Sleep disturbance mediates the link between childhood trauma and clinical outcome in severe mental disorders. Psychol Med 2021;51:1–10. 10.1017/S0033291720000914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aas M, Andreassen OA, Aminoff SR, et al. A history of childhood trauma is associated with slower improvement rates: findings from a one-year follow-up study of patients with a first-episode psychosis. BMC Psychiatry 2016;16:126. 10.1186/s12888-016-0827-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Serafini G, Canepa G, Adavastro G, et al. The relationship between childhood maltreatment and non-suicidal self-injury: a systematic review. Front Psychiatry 2017;8:149. 10.3389/fpsyt.2017.00149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campbell JA, Walker RJ, Egede LE. Associations between adverse childhood experiences, high-risk behaviors, and morbidity in adulthood. Am J Prev Med 2016;50:344–52. 10.1016/j.amepre.2015.07.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Larkin H, Aykanian A, Dean E, et al. Adverse childhood experiences and substance use history among vulnerable older adults living in public housing. J Gerontol Soc Work 2017;60:01634372.2017.1362091 10.1080/01634372.2017.1362091 [DOI] [PubMed] [Google Scholar]
- 13.Copeland WE, Shanahan L, Hinesley J, et al. Association of childhood trauma exposure with adult psychiatric disorders and functional outcomes. JAMA Netw Open 2018;1:e184493-e 10.1001/jamanetworkopen.2018.4493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aas M, Steen NE, Agartz I, et al. Is cognitive impairment following early life stress in severe mental disorders based on specific or general cognitive functioning? Psychiatry Res 2012;198:495–500. 10.1016/j.psychres.2011.12.045 [DOI] [PubMed] [Google Scholar]
- 15.Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull 2012;38:661–71. 10.1093/schbul/sbs050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morgan C, Gayer-Anderson C. Childhood adversities and psychosis: evidence, challenges, implications. World Psychiatry 2016;15:93–102. 10.1002/wps.20330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heins M, Simons C, Lataster T, et al. Childhood trauma and psychosis: a case-control and case-sibling comparison across different levels of genetic liability, psychopathology, and type of trauma. Am J Psychiatry 2011;168:1286–94. 10.1176/appi.ajp.2011.10101531 [DOI] [PubMed] [Google Scholar]
- 18.Alameda L, Golay P, Baumann PS, et al. Mild depressive symptoms mediate the impact of childhood trauma on long-term functional outcome in early psychosis patients. Schizophr Bull 2017;43:1027–35. 10.1093/schbul/sbw163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Larsson S, Andreassen OA, Aas M, et al. High prevalence of childhood trauma in patients with schizophrenia spectrum and affective disorder. Compr Psychiatry 2013;54:123–7. 10.1016/j.comppsych.2012.06.009 [DOI] [PubMed] [Google Scholar]
- 20.Uyan TT, Baltacioglu M, Hocaoglu C. Relationships between childhood trauma and dissociative, psychotic symptoms in patients with schizophrenia: a case-control study. Gen Psychiatr 2022;35:e100659. 10.1136/gpsych-2021-100659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Merikangas KR, He J-P, Burstein M, et al. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 2010;49:980–9. 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quinn K, Boone L, Scheidell JD. The relationships of childhood trauma and adulthood prescription pain reliever misuse and injection drug use. Drug Alcohol Depend 2016;169:190–8. 10.1016/j.drugalcdep.2016.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wickersham JA, Loeliger KB, Marcus R, et al. Patterns of substance use and correlates of lifetime and active injection drug use among women in Malaysia. Am J Drug Alcohol Abuse 2016;42:98–110. 10.3109/00952990.2015.1101467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marotta PL. Childhood adversities and substance misuse among the incarcerated: implications for treatment and practice in correctional settings. Subst Use Misuse 2017;52:717–33. 10.1080/10826084.2016.1261899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abajobir AA, Kisely S, Williams G, et al. Gender-based differences in injecting drug use by young adults who experienced maltreatment in childhood: findings from an Australian birth cohort study. Drug Alcohol Depend 2017;173:163–9. 10.1016/j.drugalcdep.2016.12.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tomassi S, Tosato S, Mondelli V, et al. Influence of childhood trauma on diagnosis and substance use in first-episode psychosis. Br J Psychiatry 2017;211:bjp.bp.116.194019:151–6. 10.1192/bjp.bp.116.194019 [DOI] [PubMed] [Google Scholar]
- 27.Serafini G, Gonda X, Canepa G, et al. Extreme sensory processing patterns show a complex association with depression, and impulsivity, alexithymia, and hopelessness. J Affect Disord 2017;210:249–57. 10.1016/j.jad.2016.12.019 [DOI] [PubMed] [Google Scholar]
- 28.Maletic V, Eramo A, Gwin K, et al. The role of norepinephrine and its α-adrenergic receptors in the pathophysiology and treatment of major depressive disorder and schizophrenia: a systematic review. Front Psychiatry 2017;8:42. 10.3389/fpsyt.2017.00042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mohammed AA, Moustafa HA, Nour-Eldein H, et al. Association of anxiety-depressive disorders with irritable bowel syndrome among patients attending a rural family practice center: a comparative cross-sectional study. Gen Psychiatr 2021;34:e100553. 10.1136/gpsych-2021-100553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lindert J, von Ehrenstein OS, Grashow R, et al. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. Int J Public Health 2014;59:359–72. 10.1007/s00038-013-0519-5 [DOI] [PubMed] [Google Scholar]
- 31.O'Mahen HA, Karl A, Moberly N, et al. The association between childhood maltreatment and emotion regulation: two different mechanisms contributing to depression? J Affect Disord 2015;174:287–95. 10.1016/j.jad.2014.11.028 [DOI] [PubMed] [Google Scholar]
- 32.Marchand WR, Wirth L, Simon C. Adverse life events and pediatric bipolar disorder in a community mental health setting. Community Ment Health J 2005;41:67–75. 10.1007/s10597-005-2600-x [DOI] [PubMed] [Google Scholar]
- 33.Carballo JJ, Harkavy-Friedman J, Burke AK, et al. Family history of suicidal behavior and early traumatic experiences: additive effect on suicidality and course of bipolar illness? J Affect Disord 2008;109:57–63. 10.1016/j.jad.2007.12.225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Conus P, Cotton S, Schimmelmann BG, et al. Pretreatment and outcome correlates of past sexual and physical trauma in 118 bipolar I disorder patients with a first episode of psychotic mania. Bipolar Disord 2010;12:244–52. 10.1111/j.1399-5618.2010.00813.x [DOI] [PubMed] [Google Scholar]
- 35.Huh HJ, Kim KH, Lee H-K, et al. The relationship between childhood trauma and the severity of adulthood depression and anxiety symptoms in a clinical sample: the mediating role of cognitive emotion regulation strategies. J Affect Disord 2017;213:44–50. 10.1016/j.jad.2017.02.009 [DOI] [PubMed] [Google Scholar]
- 36.Ay R, Erbay LG. Relationship between childhood trauma and suicide probability in obsessive-compulsive disorder. Psychiatry Res 2018;261:132–6. 10.1016/j.psychres.2017.12.054 [DOI] [PubMed] [Google Scholar]
- 37.Semiz UB, Inanc L, Bezgin CH. Are trauma and dissociation related to treatment resistance in patients with obsessive-compulsive disorder? Soc Psychiatry Psychiatr Epidemiol 2014;49:1287–96. 10.1007/s00127-013-0787-7 [DOI] [PubMed] [Google Scholar]
- 38.Hemmings SMJ, Lochner C, van der Merwe L, et al. BDNF Val66Met modifies the risk of childhood trauma on obsessive-compulsive disorder. J Psychiatr Res 2013;47:1857–63. 10.1016/j.jpsychires.2013.08.012 [DOI] [PubMed] [Google Scholar]
- 39.Ford ES, Anda RF, Edwards VJ, et al. Adverse childhood experiences and smoking status in five states. Prev Med 2011;53:188–93. 10.1016/j.ypmed.2011.06.015 [DOI] [PubMed] [Google Scholar]
- 40.Kelleher I, Cannon M. Psychotic-like experiences in the general population: characterizing a high-risk group for psychosis. Psychol Med 2011;41:1–6. 10.1017/S0033291710001005 [DOI] [PubMed] [Google Scholar]
- 41.Strine TW, Dube SR, Edwards VJ, et al. Associations between adverse childhood experiences, psychological distress, and adult alcohol problems. Am J Health Behav 2012;36:408–23. 10.5993/AJHB.36.3.11 [DOI] [PubMed] [Google Scholar]
- 42.Houston JE, Murphy J, Shevlin M, et al. Cannabis use and psychosis: re-visiting the role of childhood trauma. Psychol Med 2011;41:2339–48. 10.1017/S0033291711000559 [DOI] [PubMed] [Google Scholar]
- 43.McLellan AT, Luborsky L, Cacciola J, et al. New data from the Addiction Severity Index. Reliability and validity in three centers. J Nerv Ment Dis 1985;173:412–23. 10.1097/00005053-198507000-00005 [DOI] [PubMed] [Google Scholar]
- 44.Kay SR, Opler LA, Lindenmayer JP. The positive and negative syndrome scale (PANSS): rationale and standardisation. Br J Psychiatry Suppl 1989;155:59–65. 10.1192/S0007125000291514 [DOI] [PubMed] [Google Scholar]
- 45.Bech P, Allerup P, Gram LF, et al. The Hamilton depression scale. Evaluation of objectivity using logistic models [J]. Acta Psychiatri Scand 1981;63:290–9. [DOI] [PubMed] [Google Scholar]
- 46.Gracious BL, Youngstrom EA, Findling RL, et al. Discriminative validity of a parent version of the young mania rating scale. J Am Acad Child Adolesc Psychiatry 2002;41:1350–9. 10.1097/00004583-200211000-00017 [DOI] [PubMed] [Google Scholar]
- 47.Kim SW, Dysken MW, Kuskowski MA. The Yale-Brown obsessive-compulsive scale. Psychiatry Res 1990;51:203. [DOI] [PubMed] [Google Scholar]
- 48.Park S. Reliability and validity of the early trauma inventory self report-short form among Korean adolescents. J Korean Acad Child Adolesc Psychiatry 2018;29:2–6. 10.5765/jkacap.2018.29.1.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stanton KJ, Denietolis B, Goodwin BJ, et al. Childhood trauma and psychosis: an updated review. Child Adolesc Psychiatr Clin N Am 2020;29:115–29. 10.1016/j.chc.2019.08.004 [DOI] [PubMed] [Google Scholar]
- 50.McKay MT, Cannon M, Chambers D, et al. Childhood trauma and adult mental disorder: a systematic review and meta-analysis of longitudinal cohort studies. Acta Psychiatr Scand 2021;143:189–205. 10.1111/acps.13268 [DOI] [PubMed] [Google Scholar]
- 51.Bremner JD, Bolus R, Mayer EA. Psychometric properties of the early trauma Inventory-Self report. J Nerv Ment Dis 2007;195:211–8. 10.1097/01.nmd.0000243824.84651.6c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.World Health Organization, International Society for Prevention of Child Abuse and Neglect . Preventing child maltreatment: a guide to taking action and generating evidence. Geneva: World Health Organization, 2006. [Google Scholar]
- 53.Dualibe AL, Osório FL. Bipolar disorder and early emotional trauma: a critical literature review on indicators of prevalence rates and clinical outcomes. Harv Rev Psychiatry 2017;25:198–208. 10.1097/HRP.0000000000000154 [DOI] [PubMed] [Google Scholar]
- 54.Citak C, Erten E. Impact of childhood trauma and attachment on resilience in remitted patients with bipolar disorder. J Affect Disord 2021;280:219–27. 10.1016/j.jad.2020.11.025 [DOI] [PubMed] [Google Scholar]
- 55.Segura AG, Mitjans M, Jiménez E, et al. Association of childhood trauma and genetic variability of CRH-BP and FKBP5 genes with suicidal behavior in bipolar patients. J Affect Disord 2019;255:15–22. 10.1016/j.jad.2019.05.014 [DOI] [PubMed] [Google Scholar]
- 56.McGowan PO, Sasaki A, D'Alessio AC, et al. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat Neurosci 2009;12:342–8. 10.1038/nn.2270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chan KL, Yan E, Brownridge DA, et al. Associating child sexual abuse with child victimization in China. J Pediatr 2013;162:1028–34. 10.1016/j.jpeds.2012.10.054 [DOI] [PubMed] [Google Scholar]
- 58.Shin SH, Hong HG, Hazen AL. Childhood sexual abuse and adolescent substance use: a latent class analysis. Drug Alcohol Depend 2010;109:226–35. 10.1016/j.drugalcdep.2010.01.013 [DOI] [PubMed] [Google Scholar]
- 59.Mendoza-Meléndez Miguel Ángel, Cepeda A, Frankeberger J, et al. History of child sexual abuse among women consuming illicit substances in Mexico City. J Subst Use 2018;23:520–7. 10.1080/14659891.2018.1489478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang A, Price JL, Leonard D, et al. Alcohol use disorder masks the effects of childhood adversity, lifetime trauma, and chronic stress on hypothalamic-pituitary-adrenal axis reactivity. Alcohol Clin Exp Res 2020;44:1192–203. 10.1111/acer.14334 [DOI] [PubMed] [Google Scholar]
- 61.Croft J, Heron J, Teufel C, et al. Association of trauma type, age of exposure, and frequency in childhood and adolescence with psychotic experiences in early adulthood. JAMA Psychiatry 2019;76:79–86. 10.1001/jamapsychiatry.2018.3155 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request.