Abstract
Introduction
Increasingly, older adults are turning to emergency departments (EDs) to address healthcare needs. To achieve these research demands, infrastructure is needed to both generate evidence of intervention impact and advance the development of implementation science, pragmatic trials evaluation and dissemination of findings from studies addressing the emergency care needs of older adults. The Geriatric Emergency Care Applied Research Network (https://gearnetwork.org) has been created in response to these scientific needs—to build a transdisciplinary infrastructure to support the research that will optimise emergency care for older adults and persons living with dementia.
Methods and analysis
In this paper, we describe our approach to developing the GEAR Network infrastructure, the scoping reviews to identify research and clinical gaps and its use of consensus-driven research priorities with a transdisciplinary taskforce of stakeholders that includes patients and care partners. We describe how priority topic areas are ascertained, the process of conducting scoping reviews with integrated academic librarians performing standardised searches and providing quality control on reviews, input and support from the taskforce and conducting a large-scale consensus workshop to prioritise future research topics. The GEAR Network approach provides a framework and systematic approach to develop a research agenda and support research in geriatric emergency care.
Ethics and dissemination
This is a systematic review of previously conducted research; accordingly, it does not constitute human subjects research needing ethics review. These reviews will be prepared as manuscripts and submitted for publication to peer-reviewed journals, and the results will be presented at conferences.
Open Science Framework registered DOI: 10.17605/OSF.IO/6QRYX, 10.17605/OSF.IO/AKVZ8, 10.17605/OSF.IO/EPVR5, 10.17605/OSF.IO/VXPRS.
Keywords: Dementia, accident & emergency medicine, geriatric medicine
Strengths and limitations of this study.
The inclusion of transdisciplinary stakeholder participants as part of the scoping review and consensus process to identify research gaps and priorities.
Cross-coordination with medical librarians of scoping review searches.
Creation of a Health Equity Advisory Board to ensure meaningful inclusion of diverse populations in studies focused on the emergency care of persons living with dementia.
A well-defined search strategy created by a team of academic research librarians to search a broad group of databases.
Small body of published literature in topic areas.
Introduction
Increasingly, older adults are turning to emergency departments (EDs) to address healthcare needs.1 2 Older adults (aged 65 years and older) in the USA visit the ED at a rate of 51.1 per 100 persons per year.3 Recommendations to transform EDs to better care for older adults have included redesigning services and processes.4–6 Geriatric emergency care and geriatric EDs (GEDs) have emerged over the past decade as innovative solutions to better provide emergency care for older adults.4 6–8 However, many of the processes, protocols and care models targeting older patients with emergency care remain untested in the unique ED setting. Consequently, the impact of geriatric emergency care for older adults is unknown.9 10 Furthermore, novel interventions and best practices tailored to the ED setting need to be developed for both older adults and persons living with dementia (PLWD). To achieve these research demands, infrastructure is needed for GEDs to both generate evidence of intervention impact and advance development of implementation science, pragmatic trials evaluation and dissemination of findings from these studies.11
The Geriatric Emergency Care Applied Research (GEAR) Network was created in response to these scientific needs—to build a transdisciplinary infrastructure to support the research that will optimise emergency care for older adults and PLWD.12 The GEAR Network (https://gearnetwork.org) is supported by the National Institute on Aging (NIA) and partner organisations, The Gary and Mary West Health Institute and The John A. Hartford Foundation (jointly on The Geriatric Emergency Department Collaborative grant (award number N/A) with two phased awards: GEAR (R33 AG058926 add dates) and GEAR 2.0—Advancing Dementia Care (GEAR 2.0 ADC) (R61 AG069822 September 2020–June 2022)). In the first phase of both awards, key stakeholders from emergency medicine, geriatrics, nursing, psychiatry, pharmacy, social work, individuals representing healthcare systems, clinicians, researchers, medical specialty organisations, advocacy organisations, caregivers, older adults and PLWD to identify consensus-driven research priorities that will improve the care of older adults (GEAR). GEAR 2.0 ADC added PLWD and care partners to the team. The second phase consists of pilot grant funding to support investigators that advance research priorities identified by stakeholder consensus.
The original GEAR project (hereafter referred to simply as GEAR) is dedicated to improving ED care of the older adult and focused on the priority topics of: care transitions, cognitive impairment—delirium, medication safety, elder abuse and falls. Four of the five GEAR research priorities have already been published using this approach.13–16 GEAR 2.0 ADC is focused on optimising emergency care for PLWD and their care partners in the priority areas of: ED practices, ED care transitions, detection and communication and shared decision-making.
In this paper, we describe the phase I methods used by GEAR 2.0 ADC to identify consensus-driven research priorities, which were based on methods used for GEAR. We describe how we identified the priority topic areas, conducted scoping reviews in each topic area while integrating input from a transdisciplinary stakeholder taskforce, integrated academic librarians in the review process to perform standardised searches and provide quality control and conducted a large-scale consensus conference to prioritise future research. The GEAR Network approach may be valuable for other specialties, disciplines and organisations attempting to identify research and practice gaps, generate evidence, build collaborations, and target high-yield research questions to optimise the care of older adults.
Methods/Design
GEAR 2.0 ADC design and structure
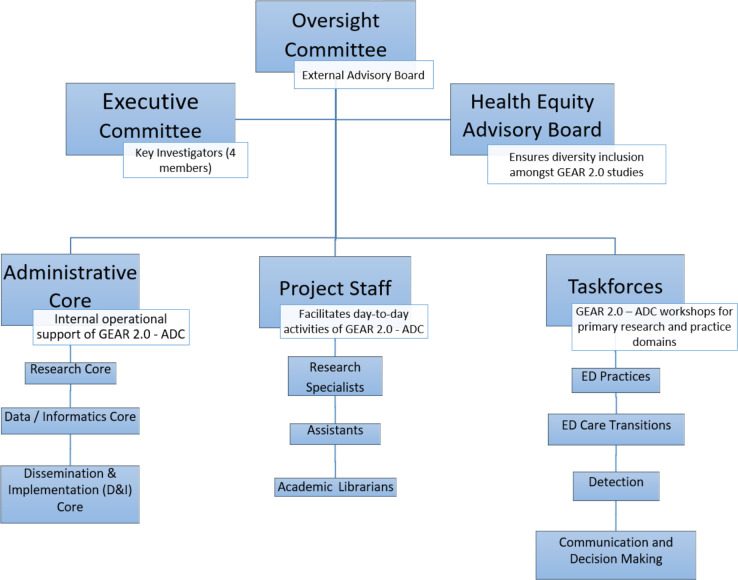
Like GEAR, GEAR 2.0 ADC is a phased programme that provides infrastructure to support the mission of increasing transdisciplinary research to improve emergency care for PLWD and their care partners. The organisational structure of GEAR 2.0 ADC (figure 1) consists of committees that guide operations, a taskforce of stakeholder members that join workgroups and participate in the consensus conference during the first phase (2 years) and Cores that support training and expert consultation for pilot studies that will be conducted during the second phase (3 years). GEAR 2.0 ADC is from 1 June 2020 to 31 May 2025.
Figure 1.
Geriatric Emergency Care Applied Research (2.0) Network - Advancing Dementia Care (GEAR 2.0 ADC) organisational structure. ED, emergency department.
The executive committee
GEAR 2.0 ADC is operationally coordinated by the executive committee that oversees and guides the programme and activities in both phases. The executive committee is led by geriatric emergency medicine investigators who also lead one of the four priority topic workgroups. Each of these leads were selected based on geriatric emergency medicine expertise and the concurrent engagement of local Alzheimer’s Disease Research Center faculty at their sites. These investigators supervise the GEAR 2.0 ADC efforts and meet virtually on a biweekly basis.
The oversight committee
The oversight committee consists of content experts in geriatrics, emergency medicine, and Alzheimer’s disease and related disorders (ADRD) that provides high-level guidance to the executive committee during quarterly meetings. Representatives from the NIA also participate in these meetings to hear updates and progress of GEAR 2.0 ADC activities. The oversight committee provides interdisciplinary guidance on the project direction, content and research approaches and future directions to address cross-disciplinary gaps highlighted by the American Geriatrics Society conference series.17
Health Equity Advisory Board
To address the need for greater equity in emergency care research in geriatrics and dementia care both with regard to PLWD, care partners and researchers, a Health Equity Advisory Board (HEAB) was created. The HEAB provides guidance and feedback on GEAR 2.0 ADC activities, to ensure meaningful inclusion of diverse populations based on race, gender, ethnic/religious affiliation, sex identification, along with the impact of social determinants of health in studies focused on the emergency care of PLWD. HEAB members include PLWD, their caregiver and care partners, advocates and stakeholders all from under-represented populations or groups. Current board members include individuals that are African American, Hispanic, Asian and lesbian. The HEAB will follow the NIA Health Disparities Research Framework18 approach and will work with partner organisations like the Imbedded Pragmatic Alzheimer’s disease and AD-Related Dementias Clinical Trials Collaboratory, an organisation that is developing strategies to address diversity and inclusion in studies focused on PLWD.19 This includes addressing the four key levels of analyses related to the NIA health disparities priorities of environmental, sociocultural, behavioural and biological disparities in health for older minority populations. We will incorporate the lifecourse perspective, which is a ‘multidisciplinary approach to understanding the mental, physical and social health of individuals, which incorporates both life span and life stage concepts that determine health trajectory and influence population-level health disparities’.18
Project team staff
GEAR 2.0 ADC activities are supported by smaller project teams where each of the executive committee leads are located. Local project team members include a research coordinator and academic medical school librarian to facilitate GEAR 2.0 ADC activities, the bulk of which includes conducting the scoping reviews. Additional activities of the research coordinators include coordinating communication with all members, and organising meetings (including presentations, recordings, minute preparation).
Patient and public involvement
Throughout the methods, the involvement, inclusion and representation of patients, and public partners are described. The GEAR 2.0 ADC taskforce and workgroups are transdisciplinary groups of stakeholders committed to improve the emergency care of PLWD. Members were identified to participate based on content expertise, their positions in partner organisations and referrals from other invited members. The executive committee invited participants to ensure diversity of background and expertise while ensuring a manageable group size. They include emergency physicians, geriatricians, neurologists, psychiatrists, neuropsychologists, nurses, social workers, pharmacists, physical therapists, patient advocates and most importantly PLWD and their care partners.
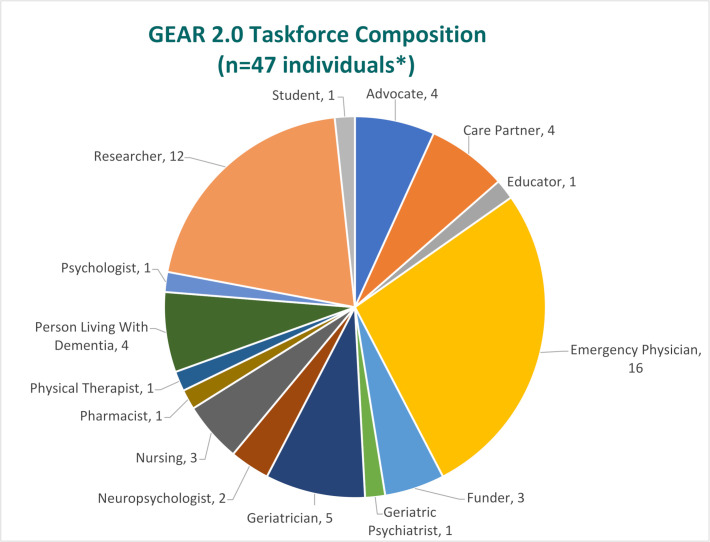
GEAR 2.0 ADC taskforce and workgroups
The GEAR 2.0 ADC taskforce is a transdisciplinary group of stakeholders committed to improve the emergency care of PLWD. Members were identified to participate based on content expertise, their positions in partner organisations and referrals from other invited members. The executive committee invited participants to ensure diversity of background and expertise while ensuring a manageable group size. This included 47 individuals who identified themselves as emergency physicians, geriatricians, neurologists, psychiatrists, neuropsychologists, nurses, social workers, pharmacists, physical therapists, patient advocates and most importantly PLWD and their care partners (figure 2).
Figure 2.
Geriatric Emergency Care Applied Research (2.0) Network - Advancing Dementia Care (GEAR 2.0 ADC)taskforce composition. *Identification categories not mutually exclusive.
Taskforce members participated on one or more workgroups that represented research and clinical practice priorities in four topics (see below Priority domain determination section for how these topics were chosen):
Optimal ED care practices for PLWD and their caregivers (ED practices).
Optimal ED care transitions for PLWD and their caregivers (ED care transitions).
Approaches to identify ED PLWD (diagnosed and undiagnosed ADRD) (detection).
Approaches to communication and shared decision-making in ED treatment and disposition for PLWD and their caregivers (communication and decision making).
Approach
GEAR 2.0 ADC operational overview
During the first phase, GEAR 2.0 ADC identified and prioritised research by completing scoping reviews in each of the priority topics and then held a 2-day consensus conference of key stakeholders who discussed and voted on research priorities to optimise emergency care for PLWD. The GEAR Network consensus conference approach is modelled after the Cornell Institute for Translational Research on Aging (CITRA) process for developing stakeholder-based translational research agendas in ageing.20 Unlike CITRA, the GEAR Network approach has more extensive preparatory work prior to the consensus conference that includes completion of scoping reviews in preselected priority areas prior to the consensus conference. Completion of the scoping review required: (1) proposing initial research priorities in each of the domains; (2) using a Population, Intervention, Comparison, Outcome (PICO) framework for the research questions to conduct structured literature searches with academic librarians to identify publications related to the domains (round 1 priority research questions); (3) summarising the most recent scientific reviews of ED-based trials, observational and/or retrospective studies (if any) that address the priority area; (4) extracting major conclusions from relevant literature identified or other systematic reviews related to the PICO question. The results of the scoping reviews were then used as the basis for discussion and considerations of research priorities at the consensus conference.
During the second phase, GEAR 2.0 ADC will fund pilot studies that encourage transdisciplinary collaboration to address the research priorities ranked by the stakeholders from the first phase.
Priority domain determination
GEAR 2.0 ADC taskforce members ranked priority topics in December 2019 during the grant proposal preparation process. The executive committee proposed the multiple priority topics which the taskforce ranked. These were then emailed as a survey to taskforce members to rank the importance of each topic and the top ones were selected to be the focus of GEAR 2.0 ADC activities. Based on past experience in GEAR, the decision was made to limit efforts to four workgroups based on capacity and workload.
Workgroup preconference activities
Each workgroup was led by an executive committee member lead and supported by the project team staff. At the study kickoff meeting, taskforce members were invited to participate in any of the four workgroups representing research and practice priority domains. Taskforce members joined workgroups based on their interests and expertise, noting their preferences through an online survey. Although most requests were honoured, some respondents were assigned to non-primary choices to ensure diversity of background and maintain workable group sizes of 12–14 participants. While participants were encouraged to only engage with one group, a number engaged in multiple groups.
Each workgroup’s leader developed a charter document that consisted of a description of the workgroup’s topic, goals, meeting dates, membership list as well as expectations of both group leadership and participants. All workgroups met monthly for 1 hour, while work continued asynchronously through emails moderated by the group leadership. Files were accessible through cloud-based file sharing tools and servers to provide a single source of information for all members. These workgroup meetings served to review the progress of the project, to discuss and reflect on project findings and to frame project directions. Workgroups particularly had extensive discussions to develop key questions and identify research gaps using the PICO approach.21
Phase I: scoping review process
In preparation for the GEAR 2.0 ADC consensus conference, scoping reviews were conducted in the four domains. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses-scoping review—scoping review checklist process to explore both the breadth of literature in this area and identify the knowledge and practice gaps.22 Scoping reviews are preferred for this type of work as they incorporate a wider range of literature than systematic reviews and can provide more synthesised ideas for future systematic reviews.22 23
Development of PICO research questions
Each workgroup brainstormed potential PICO questions within their domains. The workgroups iteratively refined and reviewed the questions and then submitted them to the executive committee for review. Each workgroup had approximately 20 questions. The executive committee, through joint discussion among the workgroup leads, ensured that questions were distinct. The full taskforce ranked questions for each workgroup via an online survey (Qualtrics). A respondent weighting system was used to identify the top research questions with workgroup members’ ranking weighted double that of other taskforce members. The top two questions were then formatted using the PICO approach21 (tables 1–4).
Table 1.
Communication and decision-making PICO research questions
| Preliminary PICO questions | Final two PICO questions |
|
Question 1: How does communication and decision-making differ for persons with dementia compared with persons without dementia? Question 2: Are there specific medical communication strategies (such as ‘Teach Back’ or next day telephone follow-up) that improve the process or outcomes of ED care in persons with dementia? |
ED, emergency department; PICO, Population, Intervention, Comparison, Outcome.
Table 2.
Detection/Identification of dementia/cognitive impairment PICO research questions
| Preliminary PICO questions | Final two PICO questions |
|
Question 1: How can the ED best identify cognitive impairment? (Best in terms of sensitivity, specificity, reliability, practicality, easy and speed of completion, etc) Are there differences by race or ethnicity? Question 2: Are there pragmatic cognitive impairment screening tools that can identify patients at risk of dementia? (Pragmatic in terms of ease of use, training, quickness to complete, etc) |
ED, emergency department; PICO, Population, Intervention, Comparison, Outcome.
Table 3.
Care transitions PICO research questions
| Preliminary PICO questions | Final two PICO questions |
|
Question 1: What interventions delivered to ED patients with impaired cognition and their care partners improve ED discharge transitions? Question 2: What measures of quality ED discharge transitions are important to varying groups of ED patients with impaired cognition and their care partners? |
ED, emergency department; PICO, Population, Intervention, Comparison, Outcome; PLWD, persons living with dementia.
Table 4.
Optimal ED practices PICO research questions
| Preliminary PICO questions | Final two PICO questions |
|
Question 1: What components of emergency department care improve patient-centred outcomes for persons with dementia? Question 2: How do emergency care needs for persons with dementia differ from other patients in the emergency department? |
ED, emergency department; PICO, Population, Intervention, Comparison, Outcome; PLWD, persons living with dementia.
Medical librarian collaboration
Medical librarians from each workgroup leads institution working together developed a standardised core search strategy for the workgroups, as well as topic specific modifications for the scoping reviews. Prior studies have demonstrated this collaboration style creates higher quality search strategies and minimises review bias.24–26 To confirm the search strategies developed would capture the articles sought after, exemplar articles were identified. The searches were reviewed to ensure inclusion of these articles. The only exclusion filter applied to the search was to limit the focus to an adult patient population. No other publication type, language or date filters were applied.
The librarians worked together to identify relevant bibliographic databases to maximise capture of relevant articles while limiting duplication. Databases searched included MEDLINE (Ovid), Embase, Cochrane Central Register of Controlled Trials, CINAHL, PsychINFO, PubMed Central, Web of Science and ProQuest Theses and Dissertations. For a list of databases used by the workgroups, see table 5. Each site librarian conducted the literature search, identified article duplication and uploaded the results to Covidence, a systematic review software (Veritas Health Innovation, Melbourne, Australia; available at www.covidence.org). Search strategies began at the earliest year databases began indexing until March 2021 and focused on emergency care and the scoping reviews for each group are registered on Open Science Framework.27–30
Table 5.
Databases searched by workgroups
| Database searched | Workgroup | |||
| Detection | Communication | Practices | Transitions | |
| MEDLINE (Ovid) | X | X | X | X |
| Embase | X | X | X | X |
| Cochrane Central Register of Controlled Trials | X | X | X | X |
| CINAHL (Ebsco) | X | X | X | X |
| PsycINFO (Ebsco) | X | X | X | |
| PubMed Central | X | X | X | X |
| Web of Science | X | X | X | X |
| ProQuest Theses and Dissertations | X | |||
The workgroup lead and a trained research associate from each workgroup independently screened the titles and abstracts of all articles uploaded into Covidence for relevance. Each workgroup created unique inclusion and exclusion criteria based on workgroup consensus. Future publications will present the findings of the workgroups. The reviewers adjudicated any disagreements. If they did not agree, a third-party reviewer made the final decision. The full text of articles identified as potentially relevant were then reviewed in the same manner. Data were abstracted from the articles deemed relevant. To ensure consistency in the conduct of the scoping reviews, workgroup leads and project team members discussed progress at the biweekly meetings and communicated frequently through email correspondence.
Phase I: GEAR 2.0 ADC consensus conference
The culmination of the scoping review process resulted in presentations of these synthesised results from each domain at a 2-day consensus conference of the full GEAR 2.0 ADC taskforce in September 2021. At the conference, taskforce members were mixed and distributed across smaller groups to discuss the findings of the scoping reviews. The goal of these small groups was to provide stakeholder insight and recommendations on the current knowledge base and to provide suggestions for future research and pilot grants. After small group discussion, there was an opportunity for shared debrief of these breakout sessions. Each workgroup then incorporated the feedback and themes heard from the small group discussion to prepare five research priorities, based on the scoping review results and transdisciplinary stakeholder recommendations. The full taskforce then ranked these research priorities using an online survey (Polleverywhere.com). Taskforce members unable to attend the conference were asked to vote asynchronously, for 100% participation by all taskforce and HEAB members. Results of each scoping reviews, their search methodology, data from included manuscripts and ranked research priorities will be published separately.
Copies of the GEAR and GEAR 2.0 ADC consensus conference summaries are available on the GEAR website: https://gearnetwork.org/manuscripts-publications/
Phase II: GEAR 2.0 ADC pilot funding
During the second phase, pilot funding opportunities will be made available to investigators. Proposals for pilot studies must address the research priorities recommended by the GEAR 2.0 ADC taskforce and HEAB members from the GEAR 2.0 ADC consensus conference. During this phase, the GEAR 2.0 ADC Cores will become active and support early research addressing research gaps and priorities recommended by the GEAR 2.0 ADC taskforce. In addition to pilot funding, the Research Core, Data and Informatics Core and Dissemination and Implementation Core will provide guidance to pilot awardees as they conduct their studies, including training sessions to enhance and increase transdisciplinary collaboration within and across the GEAR 2.0 ADC Network. These will be held as virtual training webinars, conferences and office hours, and bimonthly research progress meetings where awardees will have the opportunity to share their study progress with each other.
GEAR 2.0 ADC pilot funding opportunities can be found on the GEAR website: https://gearnetwork.org/grants-and-funding-opportunities/
Discussion
In this paper, we present a framework establishing an infrastructure to advance geriatric emergency medicine research. The value of this framework, and more importantly the representation of key stakeholders, is unique and critical to guide optimally future research addressing practice gaps that matter to all those engaged in all facets of emergency care for PLWD and their care partners. It differs from other previous agenda setting processes directed at geriatric emergency care31–34 in the following ways: (1) the inclusion of stakeholder participation as part of the scoping review and consensus process to identify research gaps and priorities; (2) cross-coordination with medical librarians of scoping review searches; (3) creation of a HEAB to ensure meaningful inclusion of diverse populations in studies focused on the emergency care of PLWD; (4) provision of pilot funding to initiate research in the recommended consensus research priorities.
A significant strength of the GEAR Network approach is the inclusion of patients, individuals that use the healthcare system and care partners as part of the process. It is a priority of the GEAR Network to include their experiences and perspectives and to learn what matters to them about the emergency care they receive. Furthermore, GEAR Network strives to share with these stakeholders’ reasons why health and medical care occurs the way it does, to enable them to engage meaningfully and to integrate their critical feedback and recommendations on the topics throughout the entire GEAR Network approach. For GEAR 2.0 ADC, this has even greater relevance coupled with challenges faced by PLWD, all of whom have cognitive impairment with varying degrees of severity. While the PLWD who participate in GEAR 2.0 ADC are in the early stages of dementia and remain high functioning, they, along with care partners and many other stakeholders who are not researchers nor clinicians, are not as familiar with taskforce or agenda setting research processes.
Preparatory background steps by the GEAR 2.0 ADC Project Team with these non-research and non-clinical stakeholders are necessary to support their full engagement. Following the empowering partnership principles of and working with the Livewell Dementia Specialists organisation,35 GEAR 2.0 ADC set up several working sessions with the non-researchers and non-clinicians taskforce members, including separate preparatory video conferences, providing printed folders of all conference materials in advance of the meeting, and providing opportunities for feedback about conference format and to address any questions they might have prior to the conference. There was also an additional debrief session after the GEAR 2.0 ADC consensus conference to gather additional suggestions and feedback about the conference from these individuals. When working with PLWD with early to middle stage dementia, it is important to recognise there may be varying degrees of cognitive function that may impact tasks and activities. For example, the survey ranking many potential questions initially proposed by workgroups required significant mental focus to complete for individuals of all levels of cognitive function. This was even more challenging for some PLWD members who found the survey format difficult to comprehend fully. To incorporate their input, once the top four choices were identified, their thoughts on each were discussed separately with them. Concurrently, other PLWD members did not express any difficulty with the survey. It is important that researchers consider the potential limitations of PLWD in research engagement and find ways to enable their full participation.
Another innovative feature of the scoping review process in GEAR 2.0 ADC was the collaboration of research librarians from four different institution sites and their inclusion early in PICO question development. Each workgroup’s assigned librarian participated in meetings when PICO question development was occurring. This provided unique insight and understanding as to the group’s thought process that allowed the librarian to craft the appropriate search strategy. It was decided that the four librarians would develop a standardised search for the elements consistent between the groups and then tailor the remaining elements for their specific groups. By cooperating on core search development, the librarians were quickly able to develop a highly effective search strategy, minimising bias.26 The standardisation of the common elements helped ensure consistency in articles identified between groups.25
As part of its mission, GEAR 2.0 ADC has also prioritised addressing equity through diversity and inclusion in its research agenda. The concern is multifactorial as it includes the diversity and composition of the workgroups, the defining of the questions and implementation in the future pilot grants to be offered by GEAR 2.0 ADC. Despite continuous efforts to increase diversity of the taskforce and while equally split in member gender, the workgroups and PLWD representatives are overwhelmingly Caucasian. This is a challenge for many organisations attempting to increase diversity in representation and health equity with research, especially for PLWD. Within the workgroups, diversity equity and inclusion was discussed in terms of the patients seen in the ED. The discussions included race, gender, ethnic/religious affiliation, sex identification, along with the impact of social determinants of health. Identifying additional workgroup members whose participation would broaden the groups’ diversity would have taken more time than the groups had, thus the decision was made to create a HEAB of members from under-represented and disenfranchised groups to review and provide input on the output of the workgroups and GEAR 2.0 ADC processes. The GEAR 2.0 ADC Principal Investigators along with the workgroup leads have developed a framework for the board that includes quarterly meetings that preview consensus conference materials to incorporate feedback before the conference and sharing materials and will involve the HEAB when selecting GEAR 2.0 ADC pilot studies to fund.
Finally, perhaps the most significant and unique feature of the GEAR Network research infrastructure is its provision of pilot funding for the research priorities generated by its consensus stakeholder process. Support is directed to build preliminary research and evidence in clinical and research gaps identified by scoping review processes that were voted by transdisciplinary members of the field and by patients and their care partners. This novel approach targets funding for stated and ranked priorities by ‘putting money where our mouth is’. It is hoped that the funding from these pilot studies will foster interest and research in needed areas of geriatric-related and dementia-related emergency care, increase and diversify the pool and foci of researchers and generate preliminary evidence and data for larger scale study proposals that are critically needed to advance the science of geriatric emergency care.
In summary, the GEAR Network approach provides a framework and systematic approach to review the literature for research and practice gaps. Furthermore, the GEAR Network approach gives insight as to how to engage key stakeholders from all facets of caring for older adults and PLWD to define and state what research priorities matter. This approach may be used by other disciplines, professions and specialties to advance research priorities in ageing.
Supplementary Material
Footnotes
Twitter: @GeriatricEDNews, @nowroozpoor
Collaborators: GEAR Network consists of: M Fernando Bellolio, Kevin Biese, Christine Binkley, Nicolas Bott, Abraham Brody, Christopher Carpenter, Sunday Clark, Scott Dresden, Savannah Forester, Cameron Gettel, Elizabeth Goldberg, Allyson Greenberg, Nada Hammouda, Jin Han, Nicole S Hastings, Teresita Hogan, William Hung, Ula Hwang, Jay Kayser, Maura Kennedy, Kelly Ko, Adriane Lesser, Elizabeth Linton, Shan Liu, Aaron Malsch, Don Melady, Carmen Morano, Nancy Morrow-Howell, Denise Nassisi, Lori Nerbonne, Sylvie Nyamu, Ugochi Ohuabunwa, Timothy Platts-Mills, Luna Ragsdale, Lynne Richardson, Thom Ringer, Anthony Rosen, Mark Rosenberg, Manish Shah, Rachel Skains, Stephanie Skees, Kimberly Souffront, Laura Stabler, Connor Sullivan, Joseph Suyama, Samuel Vargas, E Camille Vaughan, Corrine Voils and Daniel Wei. GEAR 2.0 Network consists of: Heather Allore, Amy Aloysi, Michael Belleville, M Fernanda Bellolio, Marian Betz, Kevin Biese, Cynthia Brandt, Ryan Carnahan, Christopher Carpenter, David Carr, Jennie Chin-Hansen, Morgan Daven, Nida Degesys, Scott Dresden, Jeffrey Dussetschleger, Michael Ellenbogen, Marcus Escobedo, Jason Falvey, Cameron Gettel, Angela Gifford, Andrea Gilmore-Bykovskyi, Elizabeth Goldberg, Jin Han, James Hardy, Susan (Nicki) Hastings, Jon Mark Hirshon, Teresita Hogan, William Hung, Ula Hwang, Eric Isaacs, Kathleen Kelly, Maura Kennedy, Amy JH Kind, Jesseca Leggett, Caitlin Malicki, Michael Malone, Richard Marottoli, Michelle Moccia, Vincent Mor, John Morris, Nancy Morrow Howell, Armin Nowroozpoor, Ugochi Ohuabunwa, Brenda Oiyemhonlan, William Perry, Maria Raven, Kristin Rising, Mary Sano, Manish Shah, Laura Stabler, Conor Sullivan, Joe Suyama, Jeremy Swartzberg, Zachary Taylor, Vaishal Tolia, Allan Vann, Sandra Weintraub and Susan Zieman.
Contributors: All authors read and approved the final manuscript. CC conceived the approach, provided methodological guidance, oversaw the implementation and operations of the approach and provided review and edits in the writing. SD organised the implementation and operations of the approach and was a major contributor in writing. JD organised the implementation and operations of the research approach and was a major contributor in writing the manuscript. AG organised the implementation and operations of the research approach and was a major contributor in writing the manuscript. LH organised the implementation and operations of the research approach and was a major contributor in writing the manuscript. UH secured funding, conceived the approach, organised the infrastructure and partnerships, organised the implementation and operations of the approach, was a major contributor in writing and overseeing the manuscript. JL organised the implementation and operations of the research approach and was a major contributor in writing the manuscript. AN organised the implementation and operations of the research approach and was a major contributor in writing the manuscript. MS secured funding, conceived the approach, organised the infrastructure and partnerships, organised the implementation and operations of the approach, was a major contributor in writing and overseeing the manuscript. ZT organised the implementation and operations of the research approach and was a major contributor in writing the manuscript.
Funding: This work and the GEAR Networks are funded and supported by the following organisations, each of which fosters and supports the development of research infrastructures to promote studies that address the research and clinical gaps in the ageing process and related health fields through: (1) research performed and proposed through contracts; (2) a programme of research grants and individual and institutional pilot awards; (3) cooperation and collaboration with other departmental agencies, voluntary organisations and other institutions and (4) collection and dissemination of the findings of ageing and dementia-related studies. National Institute on Aging (R33 AG058926 (UH)). National Institute on Aging (R61 AG069822 (UH, MS)). Emergency Medicine Foundation (N/A). The Gary and Mary West Health Institute (The Geriatric Emergency Department Collaborative). The John A. Hartford Foundation (The Geriatric Emergency Department Collaborative).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the 'Methods/Design' section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
The GEAR* and GEAR 2.0** Networks:
M Fernando Bellolio, Kevin Biese, Christine Binkley, Nicolas Bott, Abraham Brody, Christopher Carpenter, Sunday Clark, Scott Dresden, Savannah Forester, Cameron Gettel, Elizabeth Goldberg, Allyson Greenberg, Nada Hammouda, Jin Han, Nicole S Hastings, Teresita Hogan, William Hung, Ula Hwang, Jay Kayser, Maura Kennedy, Kelly Ko, Adriane Lesser, Elizabeth Linton, Shan Liu, Aaron Malsch, Carmen Morano Don Melady, Nancy Morrow-Howell, Denise Nassisi, Lori Nerbonne, Sylvie Nyamu, Ugochi Ohuabunwa, Timothy Platts-Mills, Luna Ragsdale, Lynne Richardson, Thom Ringer, Anthony Rosen, Mark Rosenberg, Manish Shah, Rachel Skains, Stephanie Skees, Kimberly Souffront, Laura Stabler, Connor Sullivan, Joseph Suyama, Samuel Vargas, E Camille Vaughan, Corrine Voils, Daniel Wei, Heather Allore, Amy Aloysi, Michael Belleville, M Fernanda Bellolio, Marian Betz, Kevin Biese, Cynthia Brandt, Ryan Carnahan, David Carr, Jennie Chin-Hansen, Morgan Daven, Nida Degesys, Michael Ellenbogen, Marcus Escobedo, Jason Falvey, Thomas Gill, Andrea Gilmore-Bykovskyi, Elizabeth Goldberg, Jin Han, James Hardy, Susan Hastings, Jon Mark Hirshon, Teresita Hogan, William Hung, Eric Isaacs, Kathleen Kelly, Maura Kennedy, Amy JH Kind, Caitlin Malicki, Michael Malone, Richard Marottoli, Michelle Moccia, Vincent Mor, John Morris, Nancy Morrow Howell, Armin Nowroozpoor, Ugochi Ohuabunwa, Brenda Oiyemhonlan, William Perry, Maria Raven, Kristin Rising, Mary Sano, Laura Stabler, Conor Sullivan, Joe Suyama, Jeremy Swartzberg, Vaishal Tolia, Allan Vann, Sandra Weintraub, Susan Zieman, Jeffrey Dussetschleger, Angela Gifford, Jesseca Leggett, Armin Nowroozpoor, and Zachary Taylor
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. National Center for Health Statistics . Health, United States, 2015: with special feature on racial and ethnic disparities. Hyattesville, MD: U.S. Centers for Disease Control & Prevention, 2015. [PubMed] [Google Scholar]
- 2. Tang N, Stein J, Hsia RY, et al. Trends and characteristics of US emergency department visits, 1997-2007. JAMA 2010;304:664–70. 10.1001/jama.2010.1112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ukkonen M, Jämsen E, Zeitlin R, et al. Emergency department visits in older patients: a population-based survey. BMC Emerg Med 2019;19:20. 10.1186/s12873-019-0236-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hwang U, Morrison RS. The geriatric emergency department. J Am Geriatr Soc 2007;55:1873–6. 10.1111/j.1532-5415.2007.01400.x [DOI] [PubMed] [Google Scholar]
- 5. Hwang U, Shah MN, Han JH, et al. Transforming emergency care for older adults. Health Aff 2013;32:2116–21. 10.1377/hlthaff.2013.0670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. American College of Emergency Physicians, American Geriatrics Society, Emergency Nurses Association, et al. Geriatric emergency department guidelines. Ann Emerg Med 2014;63:e7–25. 10.1016/j.annemergmed.2014.02.008 [DOI] [PubMed] [Google Scholar]
- 7. Schumacher JG, Hirshon JM, Magidson P, et al. Tracking the rise of geriatric emergency departments in the United States. J Appl Gerontol 2020;39:871–9. 10.1177/0733464818813030 [DOI] [PubMed] [Google Scholar]
- 8. Kennedy M, Lesser A, Israni J, et al. Reach and adoption of a geriatric emergency department accreditation program in the United States. Ann Emerg Med 2022;79:367-373. 10.1016/j.annemergmed.2021.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wilber ST. Geriatric Emergency Medicine. In: Solomon D, LoCicero J, Rosenthal R, eds. New frontiers in geriatric research. New York, NY: American Geriatric Society, 2004: 53–83. [Google Scholar]
- 10. Carpenter CR, Banerjee J, Keyes D, et al. Accuracy of dementia screening instruments in emergency medicine: a diagnostic meta-analysis. Acad Emerg Med 2019;26:226–45. 10.1111/acem.13573 [DOI] [PubMed] [Google Scholar]
- 11. Hogan TM, Olade TO, Carpenter CR. A profile of acute care in an aging America: Snowball sample identification and characterization of United States geriatric emergency departments in 2013. Acad Emerg Med 2014;21:337–46. 10.1111/acem.12332 [DOI] [PubMed] [Google Scholar]
- 12. GEAR Network . Geriatric emergency care applied research, 2022. Available: https://gearnetwork.org/ [Accessed 10 Sep 2021].
- 13. Kayser J, Morrow-Howell N, Rosen TE, et al. Research priorities for elder abuse screening and intervention: a geriatric emergency care applied research (GEAR) network scoping review and consensus statement. J Elder Abuse Negl 2021;33:123–44. 10.1080/08946566.2021.1904313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Carpenter CR, Hammouda N, Linton EA, et al. Delirium prevention, detection, and treatment in emergency medicine settings: a geriatric emergency care applied research (GEAR) network scoping review and consensus statement. Acad Emerg Med 2021;28:19–35. 10.1111/acem.14166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hammouda N, Carpenter CR, Hung WW, et al. Moving the needle on fall prevention: a geriatric emergency care applied research (GEAR) network scoping review and consensus statement. Acad Emerg Med 2021;28:1214–27. 10.1111/acem.14279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gettel CJ, Voils CI, Bristol AA, et al. Care transitions and social needs: a geriatric emergency care applied research (GEAR) network scoping review and consensus statement. Acad Emerg Med 2021;28:1430–9. 10.1111/acem.14360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Carpenter CR, McFarland F, Avidan M, et al. Impact of cognitive impairment across specialties: summary of a report from the U13 conference series. J Am Geriatr Soc 2019;67:2011–7. 10.1111/jgs.16093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Health Disparities Framework . National Institute on aging, 2018. Available: https://www.nia.nih.gov/research/osp/framework [Accessed 11 Dec 2021].
- 19. Health Equity Team . Nia impact Collaboratory transforming dementia care, 2022. Available: https://impactcollaboratory.org/about-us/cores-and-teams/health-equity-team/ [Accessed 12 Dec 2021].
- 20. Sabir M, Breckman R, Meador R, et al. The CITRA research-practice consensus-workshop model: exploring a new method of research translation in aging. Gerontologist 2006;46:833–9. 10.1093/geront/46.6.833 [DOI] [PubMed] [Google Scholar]
- 21. Schardt C, Adams MB, Owens T, et al. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak 2007;7:16. 10.1186/1472-6947-7-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 23. Chambers D, Simpson L, Hill-Briggs F. Proceedings of the 8th Annual Conference on the Science of Dissemination and Implementation : Washington, DC, USA. 14-15 December 2015. Implement Sci 2016;11 Suppl 2:100. 10.1186/s13012-016-0452-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Peters MDJ, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13:141–6. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- 25. Rethlefsen ML, Farrell AM, Osterhaus Trzasko LC, et al. Librarian co-authors correlated with higher quality reported search strategies in general internal medicine systematic reviews. J Clin Epidemiol 2015;68:617–26. 10.1016/j.jclinepi.2014.11.025 [DOI] [PubMed] [Google Scholar]
- 26. Aamodt M, Huurdeman H, Strømme H. Librarian Co-Authored systematic reviews are associated with lower risk of bias compared to systematic reviews with acknowledgement of librarians or no participation by librarians. Evid Based Libr Inf Pract 2019;14:103–27. 10.18438/eblip29601 [DOI] [Google Scholar]
- 27. Brackett AL, Shah MN. Geriatric Emergency Care Applied Research Network 2.0 – Advancing Dementia Care (GEAR 2.0 ADC) - Care Transitions Work Group. Open Science Framework 2021. [Google Scholar]
- 28. Brackett AL, Carpenter CR. Geriatric Emergency Care Applied Research Network 2.0 – Advancing Dementia Care (GEAR 2.0 ADC) – Communication & Decision Making Workgroup. Open Science Framework 2021;2021. [Google Scholar]
- 29. Brackett AL, Hwang U. Geriatric Emergency Care Applied Research Network 2.0 – Advancing Dementia Care (GEAR 2.0 ADC) - Detection and Identification Work Group. June 30 ed: Open Science Framework, 2021. [Google Scholar]
- 30. Brackett AL, Dresden S. Geriatric emergency care applied research network 2.0 – advancing dementia care (GEAR 2.0 ADC) – emergency department practices Workgroup. June 30 ED: open science framework, 2021. [Google Scholar]
- 31. Wilber ST. Geriatric Emergency Medicine. In: Solomon D, LoCicero J, Rosenthal R, eds. New frontiers in geriatric research. New York, NY: American Geriatrics Society, 2004: 53–83. [Google Scholar]
- 32. Carpenter CR, Gerson LW. Geriatric Emergency Medicine. In: Solomon D, LoCicero J, Rosenthal R, eds. New frontiers in geriatric research. New York, NY: American Geriatrics Society, 2008. [Google Scholar]
- 33. Carpenter CR, Heard K, Wilber S, et al. Research priorities for high-quality geriatric emergency care: medication management, screening, and prevention and functional assessment. Acad Emerg Med 2011;18:644–54. 10.1111/j.1553-2712.2011.01092.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Carpenter CR, Shah MN, Hustey FM, et al. High yield research opportunities in geriatric emergency medicine: prehospital care, delirium, adverse drug events, and falls. J Gerontol A Biol Sci Med Sci 2011;66:775–83. 10.1093/gerona/glr040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Empowering Partnerships . LiveWell dementia specialists, 2019. Available: https://livewell.org/empoweringpartners/ [Accessed 5 Jan 2022].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.