Abstract
Preventive health messages are often tailored to reach broad sociodemographic groups. However, within groups, there may be considerable variation in perceptions of preventive health practices, such as colorectal cancer screening. Segmentation analysis provides a tool for crafting messages that are tailored more closely to the mental models of targeted individuals or subgroups. This study used cluster analysis, a psychosocial marketing segmentation technique, to develop a typology of colorectal cancer screening orientation among 102 African American clinic patients between the ages of 50 and 74 years with limited literacy. Patients were from a general internal medicine clinic in a large urban teaching hospital, a subpopulation known to have high rates of colorectal cancer and low rates of screening. Preventive screening orientation variables included the patients’ responses to questions involving personal attitudes and preferences toward preventive screening and general prevention practices. A k-means cluster analysis yielded three clusters of patients on the basis of their screening orientation: ready screeners (50.0%), cautious screeners (30.4%), and fearful avoiders (19.6%). The resulting typology clearly defines important subgroups on the basis of their preventive health practice perceptions. The authors propose that the development of a validated typology of patients on the basis of their preventive health perceptions could be applicable to a variety of health concerns. Such a typology would serve to standardize how populations are characterized and would provide a more accurate view of their preventive health-related attitudes, values, concerns, preferences, and behaviors. Used with standardized assessment tools, it would provide an empirical basis for tailoring health messages and improving medical communication.
Public health campaigns typically target prevention messages to broad sociodemographic groups on the basis of age, race, and ethnicity (Hornik & Ramirez, 2006). However, within these groups, there may be considerable variation in orientation toward preventive health practices such as screening for serious and life-threatening diseases. This may be especially true for African Americans, who have historically had higher morbidity and mortality from chronic disease. R. E. Davis and colleagues (2010) noted that many health communication messages that target African Americans to help address these health disparities often assume the group to be culturally homogenous. Research indicates, however, that African Americans are quite heterogeneous in their attitudes, behavior, and beliefs around health (Radio One & Yankolovic, 2012).
It is clear that the design of more effective health messages is needed to influence preventive health practices, particularly cancer screening behaviors. The research reported here addresses this gap, using a psychosocial marketing segmentation strategy to develop a typology of older African American clinic patients with limited literacy skills, on the basis of their attitudes about preventive practices and health beliefs. These patients represent a subpopulation with particularly high rates of CRC and low rates of screening (Centers for Disease Control and Prevention, 2012). The resulting types of patients are then profiled relative to barriers to CRC screening and health lifestyle factors, which provides insights into the motivations and orientations of this select subgroup of patients and a scientific knowledge base for developing educational interventions designed to increase colonoscopy screening rates.
Background
The use of segmentation approaches to define subgroups with similar characteristics has been a common tool in commercial advertising for many years (Abratt 1993; Berrigan & Finkbeiner, 1992; Croft, 1994; Dickson & Ginter, 1987; Dominguez & Page, 1981; Grover & Srinivasan, 1992; Kumar & Rust, 1989), with the majority of large companies now using consumer segmentation profiles to help define customers and more effectively target particular subgroups (Morris & Schmolze, 2006).
Although the fields of public health and health research have embraced segmentation as an effective marketing tool, most applications have involved large-scale marketing efforts or community focused health campaigns (Albrecht & Bryant, 1996). In these efforts, it is common to see segmentation approaches that use limited demographic, cultural, or health status information to define patient subgroups (Dawson, 1989; Dolinsky & Stinerock, 1998, Cheng, Chang & Liu, 2005). What is often thought to be a relatively homogeneous subgroup, however, may possess important attitudinal, personality, or behavioral variations that, if used in an appeal strategy, could mean the difference between success and failure. Recent segmentation research suggests that applying psychobehavioral segmentation schemes that take into account attitudes, perceptions, and behaviors is more effective in characterizing and influencing patient subgroups than classifying and segmenting them simply on demographic or limited behavioral characteristics (Endresen, 1988; Fletcher et al., 1983; Morrison, Murphy, & Nalder, 2003; Wolff, et al., 2010).
A wide array of segmentation methods have been used to define typologies relative to health care, including typologies of patients relative to cardiovascular risk behaviors (Williams & Flora, 1995), risky sexual behaviors (Carey, Vanable, Senn, Coury-Doniger, & Urban, 2008; Trigg, Peterson, & Meekers, 1997), prescription drug seeking (Morris, Tabak, & Olins, 1992), alcohol use (Slater, Basil, & Maibach, 1999), antihistamine use (Reardon & Pathak, 1990), physical activity and fitness (Brown, 1992; Bull, Kreutner, & Scharff, 1999), health information seeking (Maibach, Weber, Massett, Hancock, & Price, 2006; Risker, 1995; Wahyuningsih, 2008), nonconscious behaviors (Wheeler & Berger, 2007), smoking behaviors (Rose et al., 2007), smoking cessation (Weber et al., 2007), cancer-screening behavior (Scammon, Smith, & Beard, 1991), and fruit and vegetable intake (Della, DeJoy, & Lance, 2009). Despite this, the majority of existing research uses demographics as a means for tailoring health education messages or treats subgroups (e.g., ethnic minorities) as homogenous groups. This restricts the ability to accurately understand differences in perceptions around health behaviors that may exist within subgroups.
Tailoring Messages for Colorectal Cancer Screening
While CRC screening is strongly recommended by the U.S. Preventive Services Task Force (2002) for individuals 50 years of age and older, all CRC screening methods have low rates of use compared with screening for other cancers. It remains lowest for patients with less than a high school education and among racial and ethnic minorities (Centers for Disease Control and Prevention, 2012).
Colonoscopy is a particularly important preventive procedure for African Americans because of their excess rates of CRC mortality, more proximal distribution of cancers and adenomas that are addressed more effectively by this method, and the younger mean age at which they develop CRC (Agrawal et al., 2005). Research has shown that African Americans are particularly likely to remain unscreened even when access to screening is available (American Cancer Society, 2010), and although a number of studies have addressed CRC screening behaviors in broad African American populations (Hornik & Ramirez, 2006; James, Campbell, & Hudson, 2002; Katz et al., 2004; Palmer, Midgette, & Buadoo, 2008), no study has used overall orientations toward preventive health practices as a basis for segmentation. This study addressed that gap by developing a typology of patients on the basis of their preventive health practices.
Method
We recruited 102 African-American patients from a general internal medicine clinic in a large urban teaching hospital that only enrolls patients who have some form of health insurance (predominately Medicaid, Medicare, or a private plan). In the 12 months before the study, reviewed general internal medicine clinic records indicated that patients were 64% female, 78% African American, and most older than 50 years of age. Clinicians and staff regarded the patients as having limited literacy. Pilot studies and focus groups conducted before this study confirmed the low level of literacy in the clinic population (Bass et al., 2011; Wolak, Ruzek, Bass & Gordon, 2009).
Research assistants used scheduling records from the hospital clinic to determine eligibility and obtain a convenience sample of patients to participate in the study over an 8-week period in 2008. Enrollment in this study was limited to patients between 50 and 74 years of age, the group regarded most age appropriate for colonoscopy. They were selected from daily patient rosters during regular clinic hours. We recruited equal numbers of men and women to ensure gender balance for analyses. Patients were excluded if they were scheduled for a visit related to a serious, life-threatening or terminal condition that would make participation in a study inappropriate, and these exclusions were made in consultation with each patient’s physician. Patients at the clinic for routine medical care were approached in the waiting room and asked if they would be willing to participate. If willing, patients were consented, evaluated for literacy, and asked survey questions. Interviews took place in a private office before or right after a medical appointment. The protocol took approximately 15 min to complete. All materials and procedures were approved by the institutional review board.
Instruments
The research protocol included two instruments: the Rapid Estimate of Adult Literacy in Medicine–Revised (REALM-R) to measure literacy level and a sociodemographic and patient segmentation survey designed to collect sociodemographic data, preventive health practices, and perceptions of barriers and facilitators for colonoscopy.
REALM-R
Literacy level was measured with the 8-item standardized REALM-R (T. C. Davis et al., 1991), which has a reliability coefficient (Cronbach’s α) of 0.91 (Bass, Wilson, & Griffith, 2003), a test–retest reliability coefficient of .99 (T. C. Davis et al., 1993) and takes less than 2 minutes to administer and score. The part-whole correlation between the REALM-R and the longer version (REALM) is 0.72. Patients are asked to pronounce 11 words, of which the first 3 are not scored. If the patient is unable to pronounce six or more of the remaining eight words, the patient is classified as being at risk of low literacy. Validation studies show that patients who score at or below 6 on the REALM-R are unable to read at a sixth-grade level (Bass, Wilson, & Griffith, 2003).
Sociodemographic and Patient Segmentation Survey
Patients were first asked a series of sociodemographic questions, including the highest level of education they had completed and whether or not they had ever had a screening test for CRC. The patient segmentation questions were developed on the basis of our prior work involving (a) focus groups conducted with low-literacy African American patients (Bass et al., 2011); (b) in-depth interviews with 30 third-year medical residents in internal medicine (Ward et al., 2010); and (c) an extensive review of the available research literature on CRC screening (Ward et al., 2008). The survey questions (see Table 1) covered personal attitudes and preferences regarding preventive health practices (11 questions), perceived barriers to having a colonoscopy (16 questions), and perceptions of colonoscopy (8 questions). Each question was written at or below a sixth-grade reading/comprehension level and pilot-tested with clinic patients. When administered, each question was read aloud by the research assistant who asked the patient to respond by pointing to a graphic scale that rated how much they agreed or disagreed with each of the statements on an 11-point scale ranging from 0 (strongly disagree) to 10 (strongly agree). The graphic scale, using faces at the major scale points, is used widely in clinical settings to assess pain, particularly in populations with limited literacy (Wong & Baker, 1988, 2001). This scale was printed on an sheet and positioned so the participant could point to the face that best represented his/her response.
Table 1.
Survey items, by question theme
| Theme 1: Overall screening and health attitudes/behaviors |
|---|
| 1. Don’t go to doctor unless needed |
| 2. Trust body to tell if testing is needed |
| 3. Don’t get tested unless feel something is wrong |
| 4. Rather not know about cancer |
| 5. Fear of cancer keep from testing |
| 6. Cancer is God’s will |
| 7. Screening tests not good at finding problems |
| 8. Get colonoscopy only if family/friends recommended |
| 9. Get colonoscopy if trusted doctor recommended |
| 10. Feel uncomfortable and embarrassed |
| 11. Colonoscopy is worth effort |
| 12. Screening tests done as way of not getting sick |
| Theme 2: Perceived barriers to colonoscopy |
| 1. Cost is prohibitive |
| 2. No transportation |
| 3. No time off |
| 4. No child care |
| 5. No adult care |
| 6. Too much bother |
| 7. Too unfamiliar |
| 8. Embarrassing |
| 9. Not the best method |
| 10. Scared to know |
| 11. Worry about sedation |
| 12. Worry about pain |
| 13. Worry about complications |
| 14. Women more willing |
| 15. Don’t want rectum probed |
| 16. Seems sexual |
| Theme 3: Perceived facilitators of colonoscopy |
| 1. Most accurate |
| 2. Finds problems early |
| 3. Can remove growths |
| 4. Not done often |
| 5. Provides peace of mind |
| 6. Recommended by doctors |
| 7. If insurance covers, I’ll do it |
| 8. Being sedated is good |
Segmentation Analysis
To establish the typology of patients’ CRC screening orientations, a k-means cluster analysis procedure was used (SPSS 17.0). The variables specified for clustering were responses to the 11 questions involving personal attitudes and preferences toward preventative health practices (see Table 2). After the patient typology subgroups were defined and named, descriptive statistics were computed for all other variables collected in the survey. We then conducted an analysis of variance comparing across the three subgroups on perceived barriers to colorectal cancer screening (Tables 2 and 3) and perceptions of colonoscopy (Table 4).
Table 2.
Personal health attitudes and behaviors, by patient cluster
| Item | Cluster 1: Ready screeners | Cluster 2: Fearful avoiders | Cluster 3: Cautious screeners | p * | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M | SD | n | M | SD | n | M | SD | |||
| I don’t go to doctors | I’m the kind of person who doesn’t go to the doctor unless I really need to. | 51 | 2.45 | 3.04 | 31 | 7.65 | 2.40 | 20 | 5.85 | 3.59 | .000 |
| I trust my body | I trust that my body will let me know when I need to be tested for something. | 51 | 5.94 | 3.36 | 31 | 8.23 | 1.82 | 20 | 5.65 | 3.69 | .002 |
| Don’t like tests | In general, I don’t like to have tests, unless I feel something is wrong. | 51 | 3.22 | 3.38 | 31 | 7.81 | 2.20 | 20 | 4.30 | 3.21 | .000 |
| Rather not know | I’d rather not know if I have cancer. | 51 | 0.57 | 1.65 | 31 | 6.32 | 3.82 | 20 | 1.55 | 2.65 | .000 |
| Fear cancer | My fear of cancer keeps me from getting the tests my doctor recommends. | 51 | 0.82 | 1.87 | 30 | 6.03 | 3.32 | 20 | 1.45 | 2.59 | .000 |
| God’s will | If I get cancer, I accept that it is God’s will. | 51 | 8.61 | 3.18 | 31 | 8.39 | 3.03 | 20 | 3.15 | 3.47 | .000 |
| Tests are not good | I feel many of the screening tests are not very good at finding problems. | 51 | 1.78 | 1.98 | 31 | 3.74 | 2.73 | 20 | 2.25 | 2.25 | .001 |
| Only if family/friends recommend | I would only have a colonoscopy if a family member or friend told me to. | 51 | 0.45 | 1.67 | 31 | 4.29 | 3.95 | 20 | 1.20 | 1.77 | .000 |
| Only if doctor recommends | I would only have a colonoscopy if a doctor I trusted told me to have it. | 51 | 9.65 | 1.48 | 31 | 9.10 | 1.76 | 20 | 4.45 | 4.38 | .000 |
| Worth the effort | Although it may be hard to take the time off and make arrangements to do a colonoscopy, I think it is well worth the effort. | 51 | 9.25 | 1.32 | 31 | 8.19 | 2.72 | 20 | 6.70 | 3.64 | .000 |
| I do screening | I like to avoid getting sick, so I try to do screening tests. | 51 | 9.29 | 1.12 | 31 | 8.06 | 1.93 | 20 | 7.65 | 3.05 | .001 |
Note. Scale base = 0–10; the larger the values, the more agreement with the statement.
p value for analysis of variance test of mean differences across types of patients.
Table 3.
Perceived barriers to colorectal cancer screening, by patient cluster
| Item | Cluster 1: Ready screeners | Cluster 2: Fearful avoiders | Cluster 3: Cautious screeners | p * | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M | SD | n | M | SD | n | M | SD | |||
| Cost is prohibitive | The cost of having a colon screening test keeps me from getting one. | 50 | 1.24 | 2.81 | 29 | 3.21 | 4.03 | 20 | 1.20 | 1.99 | .018 |
| No transportation | It would be hard getting someone to take me to and from the testing location. | 51 | 2.08 | 3.22 | 31 | 1.61 | 2.35 | 20 | 1.50 | 2.50 | .660 |
| No time off | It would be hard taking the time off from work to get screened. | 51 | 0.20 | 0.69 | 31 | 1.90 | 3.15 | 20 | 0.45 | 0.83 | .000 |
| No child care | It would be hard finding someone to care for my children. | 51 | 1.02 | 2.34 | 31 | 2.19 | 3.28 | 20 | 0.55 | 1.10 | .045 |
| No adult care | It would be hard finding someone to care for adults I take care of. | 51 | 0.76 | 2.00 | 31 | 2.26 | 3.38 | 20 | 0.90 | 1.55 | 0.24 |
| Too much bother | For me, preparing for the test is too much bother. | 51 | 2.49 | 2.88 | 31 | 4.13 | 2.96 | 20 | 2.50 | 2.56 | .032 |
| Too unfamiliar | For me, the whole screening process is so unfamiliar, I don’t want to do it. | 51 | 2.24 | 3.47 | 31 | 4.39 | 3.73 | 20 | 1.70 | 3.20 | .010 |
| Embarrassing | I would find the screening test to be too embarrassing. | 51 | 1.78 | 3.10 | 30 | 4.53 | 3.63 | 20 | 2.15 | 3.12 | .001 |
| Not best method | I don’t think colonoscopy is the best method for detecting colon problems. | 51 | 1.31 | 1.58 | 31 | 3.55 | 3.48 | 20 | 2.10 | 2.38 | .001 |
| Scared to know | It scares me to think that I might find out I have cancer and this keeps me from having a colon screening. | 51 | 1.98 | 2.71 | 31 | 5.81 | 3.66 | 20 | 1.65 | 3.00 | .000 |
| Worry about sedation | I worry about getting medicine to make me sleepy to have the colonoscopy test. | 51 | 1.41 | 2.72 | 31 | 1.97 | 3.14 | 20 | 2.10 | 3.21 | .577 |
| Worry about pain | I’m concerned that the screening test might be painful. | 51 | 2.69 | 3.64 | 31 | 6.35 | 3.56 | 20 | 3.60 | 3.65 | .000 |
| Worry about complications | Although I know it is very rare, I am worried that I could have a serious complication. | 51 | 3.04 | 3.27 | 31 | 4.94 | 2.86 | 20 | 2.90 | 3.08 | .018 |
| Women more willing | In general, I think women are more willing than men to have a colonoscopy. | 51 | 7.37 | 3.62 | 30 | 7.60 | 3.49 | 20 | 7.70 | 3.51 | .927 |
| Don’t want rectum probe | I wouldn’t want to have a colonoscopy because they would be putting something in my rectum. | 51 | 2.12 | 3.51 | 31 | 5.48 | 4.13 | 20 | 2.50 | 3.55 | .000 |
| Seems sexual | Having a colonoscopy seems sexual. | 50 | 0.34 | 1.64 | 30 | 2.70 | 3.70 | 20 | 0.50 | 1.10 | .000 |
Note. Scale base = 0–10; the larger the values, the more agreement with the statement.
p value for analysis of variance test of mean differences across types of patients.
Table 4.
Perceptions of colonoscopy, by patient cluster
| Item | Cluster 1: Ready screeners | Cluster 2: Fearful avoiders | Cluster 3: Cautious screeners | p * | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | M | SD | n | M | SD | N | M | SD | |||
| Most accurate | Colonoscopy is the most accurate way to check for colon cancer. | 49 | 9.41 | 1.58 | 28 | 8.29 | 1.84 | 20 | 9.05 | 1.64 | .021 |
| Finds problems easy | Having the test is a good way to find colon or rectal cancer very early. | 49 | 9.14 | 1.68 | 28 | 8.50 | 1.97 | 20 | 8.80 | 1.64 | .301 |
| Can remove growths | During the test the doctor can remove growth before they become cancer. | 49 | 8.80 | 1.73 | 28 | 8.04 | 1.86 | 20 | 8.15 | 2.06 | .164 |
| Not done often | A colonoscopy doesn’t have to be done as often as other screenings. | 49 | 7.43 | 2.26 | 28 | 6.57 | 2.28 | 20 | 7.05 | 2.69 | .311 |
| Provides peace mind | For me, the peace of mind that comes with knowing about my health is a good reason for having the test. | 49 | 9.51 | 1.39 | 28 | 9.23 | 1.52 | 20 | 9.00 | 2.18 | .462 |
| Recommended by doctors | I like the fact that the test is recommended by most doctors. | 49 | 9.43 | 1.47 | 28 | 8.93 | 1.55 | 20 | 8.80 | 1.85 | .220 |
| If insurance covers, I’ll do it | If my health insurance covers the cost of the test, I feel I should have one. | 49 | 8.86 | 1.86 | 28 | 8.83 | 1.93 | 20 | 9.30 | 1.22 | .597 |
| Being sedated is good | I think getting medicine to make me sleepy and not feel uncomfortable during the colonoscopy test is a plus. | 49 | 9.33 | 1.93 | 28 | 9.27 | 1.31 | 20 | 8.55 | 1.93 | .237 |
Note. Scale base = 0–10; the larger the values, the more agreement with the statement.
p value for analysis of variance test of mean differences across types of patients.
Results
Participant Characteristics
Participants self-identified as 94.9% African American and 5.1% mixed race; 96% considered themselves to be non-Hispanic, 3% Hispanic, and 1% were unsure. We stratified by gender to ensure having equal numbers of men (n = 51) and women (n = 51), with a mean age of 69 years (range = 50 to 74 years). This subset of clinic patients was similar in age and ethnicity to the total population of patients who use the general internal medicine clinic. Of the 101 patients who self-reported the highest grade of school completed, 51% (n = 52) completed less than high school; and 48% (n = 49) graduated from high school, had earned a GED, or had some college. One participant did not respond.
Literacy Levels
REALM-R scores were obtained for 98 patients. Four refused to take the test, saying that they did not have their glasses or could not see the text—common statements patients make to hide low literacy. Of these, three reported less than high school education; one reported having graduated from high school or equivalent. For analysis, those with less than high school were assigned the REALM-R mean score (2.90) of the 98 patients with less than high school who took the REALM-R; similarly, the one participant with a high school education was assigned the mean score (4.05) for those who took the test and had also graduated from high school. These four patients are included in the results.
Overall, 91% of all patients (n = 92) scored 0–6, and were classified as having low literacy. Nine patients scored 7–8, above the low literacy cutoff point of 6. REALM-R scores differed by education. For those with less than high school graduation, the mean score was 2.93 (SD = 2.07). For those who had graduated from high school, had a GED, or some college, the mean score was 4.29 (SD = 2.34). To assess the potential effect of the patients who reported some college (n = 8), we initially calculated the mean score for this subgroup alone (M = 5.0, SD = 2.67). Because patients with a high school degree or GED and those with some college scored on average below 6, meaning unable to read at the sixth-grade level, we combined these patients in our analyses of literacy within and between groups in the cluster analysis.
Patient Clusters on the Basis of Preventive Orientation
The cluster analysis procedure was highly successful in producing three distinct clusters that differed significantly across all of the variables, labeled ready screeners (50.0%), fearful avoiders (30.4%), and cautious screeners (19.6%). Figure 1 presents the mean values for the clusters in graphic form to aid comparison across the 11 cluster variables used to create the groupings. Table 2 presents the mean values for each of the clustering variables across the three groups including the tests of statistical significance from the analysis of variance procedure.
Figure 1.
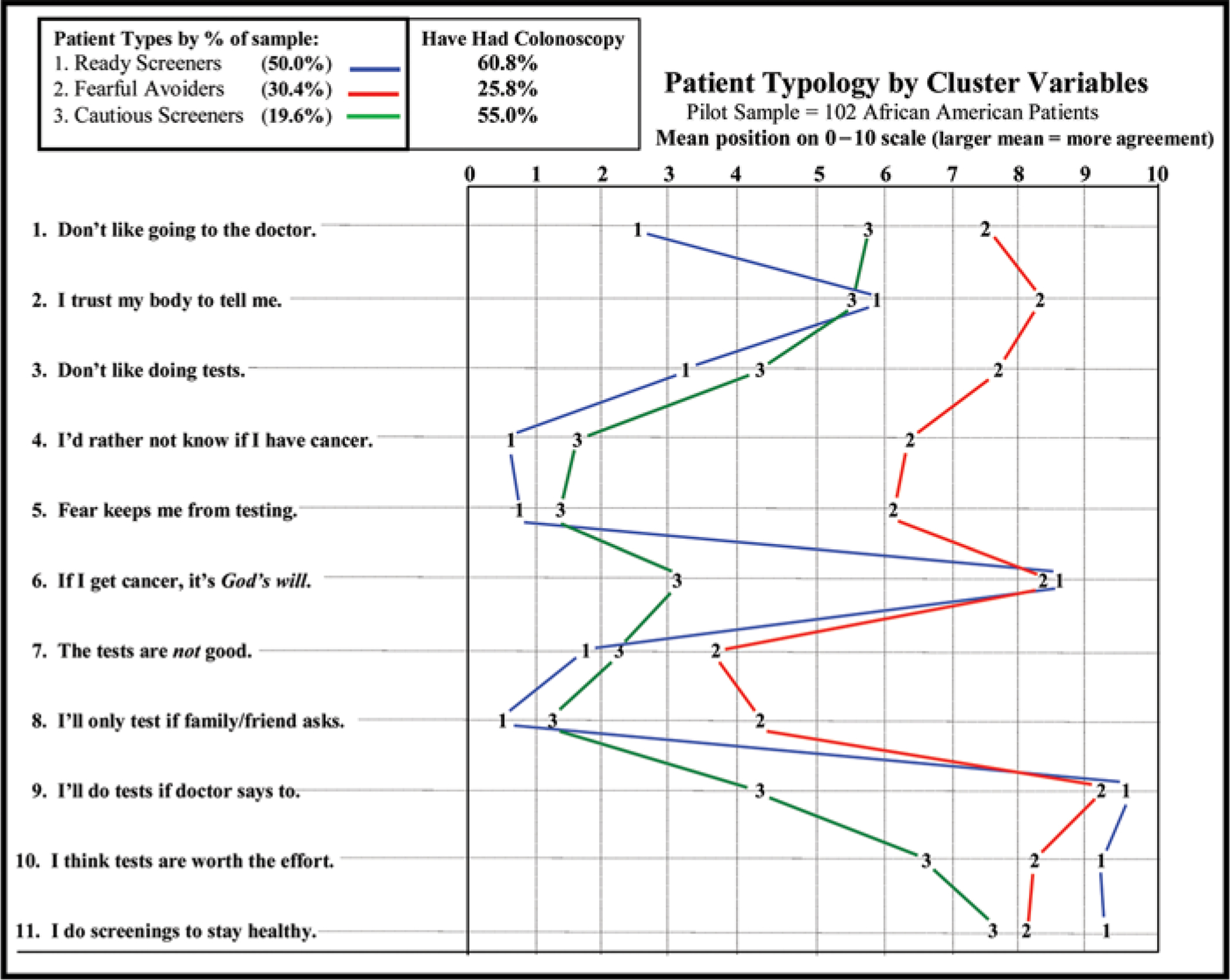
Mean scores for patient types, by cluster variables.
Ready Screeners (50.0%)
This group has a positive orientation toward the medical establishment in general, and toward screening specifically. A majority (65%) self-report that they had had a colonoscopy (an outcome variable not used to create the clusters). In general, ready screeners are willing to go to the doctor, do not mind having preventive testing such as colonoscopy, and feel that screening in general is a good way to find medical problems early, making screening “worth the effort.” They believe that screening is a good way to stay healthy. This group also feels that if they had cancer they would want to know, and their fear of having cancer is not an impediment to being tested. They would readily be screened if a doctor recommended it, without being pushed by family or friends. At the same time, this cluster group agreed with the statement that if they got cancer it is “God’s will.” Overall, the ready screeners reflect a high degree of self-control, are positive about the benefits of screening, and report fewer barriers to doing colonoscopy compared with the other groups.
Fearful Avoiders (30.4%)
Almost a third of participants (30.4%) were fearful avoiders. This cluster distinctly differs from the first group in that their orientation toward doctors and medical procedures is negative. Only 24.3% of the group self-reported having had a colonoscopy.
The fearful avoiders not only dislike organized medicine but also profess to trust their bodies to tell them if there is a problem, and feel that screening is unnecessary. Their trust in their own bodies appears to mask an overall fear of having medical tests and the potentially negative diagnosis that might result. The majority of fearful avoiders say they would rather not know if they have cancer. They did acknowledge that screening tests are “worth the effort” and that such tests should be done to stay healthy, especially if a doctor recommends the screening. However, as noted above, few of them have actually acted on that recommendation. Similar to the ready screeners, fearful avoiders believe that getting cancer is “God’s will.”
Cautious Screeners (19.6%)
This group’s orientation is somewhat like the ready screeners but with key differences. The majority of cautious screeners would rather know if they had cancer and do not mind going to the doctor. They see the benefits of screening tests, feeling these tests are “worth the effort.” They also strongly believe that screenings help a person “stay healthy.” More than half of the cluster group (57.6%) self-reported having had a colonoscopy. This group differs from the ready screeners, however, in that they would not feel overly influenced by a doctor’s recommendation or pressure from family and friends to be screened. They are cautious in that they feel they want to make their own decisions regarding health issues. In addition, this cluster is the only group that disagreed with the statement, “Getting cancer is God’s will.”
Perceptions of Barriers to CRC Screening, by Patient Cluster
Once participants had been identified as belonging to one of the three patient-types described earlier, the clusters were analyzed for similarities and/or differences in perceptions of barriers and facilitators to screening and perceptions of colonoscopy. These variables, which were not used to establish the clusters, are summarized in Tables 3 and 4.
Table 3 presents the means and significance tests by cluster for perceived barriers to colonoscopy. Transportation, taking time off from work, and arranging childcare and/or care for older family members, are rated low as barriers to getting screened by all patient-types (<2.3 on the 0–10 scale). Cost was an issue only for fearful avoiders, who rate cost as a concern significantly higher than do the other types of patients (3.2 vs. 1.24 and 1.20; p = .018). There were nine perceived barriers that did show very significant differences. Four were specific to colonoscopy. Fearful avoiders were significantly more likely to indicate “too much bother” as a barrier than either Ready screeners or cautious screeners (M = 4.13 vs. 2.49 and 2.50; p = .032), as well as colonoscopy a too unfamiliar (M = 4.39 vs. 2.24 and 1.70; p = .010), embarrassing (M = 4.53 vs. 1.78 and 2.15; p = .001), and not the best method of screening (M = 3.55 vs. 1.31 and 2.10; p = .001). While fear of finding out that they might have cancer is not a barrier to screening for the ready screeners and the cautious screeners (M = 1.98 and M = 1.65, respectively), this concern is significantly higher for the fearful avoiders (M = 5.81; p = .000). Worry variables related to pain (M = 6.35 vs. 2.69 and 3.60; p = 000) and complications (M = 4.94 vs. 3.04 and 2.90; p = .018) and also significantly higher in the fearful avoiders.
Last, there were also significant differences related to having a probe inserted into the rectum and the idea that colonoscopy was “sexual.” Fearful avoiders were most likely to indicate fear of a rectal probe (M = 5.48 vs. 2.12 and 2.50; p = .000) and having the perception of the probe being “sexual” (M = 2.70 vs. 0.34 and 0.50; p = .000).
Perceptions of Colonoscopy as a Method for CRC Screening
There is a high degree of agreement across all clusters that colonoscopy is the superior technique for colorectal cancer screening. All groups rated it highly as a form of screening, indicating it is the most accurate, most effective at finding growths early and removing them, has to be done least often, is the most recommended by doctors, is covered by insurance, and produces the most peace of mind (see Table 4). Comparing results for all eight variables across the clusters, there was a statistically significant difference on only one variable (colonoscopy being the most accurate). Fearful avoiders rated this slightly lower (M = 8.29 vs. 9.41 and 9.05; p = .021).
Distribution of Literacy Levels Across Clusters
To assess the possibility that literacy was differentially associated with preventive health practices and beliefs, we did an analysis of variance. There were no statistically significant differences between cluster groups’ REALM-R mean scores as determined by one-way analysis of variance (F [df = 99] = 1.415; p = .248). Because mean REALM-R scores were higher for participants with more education, we also examined the distribution of patients with the highest level of education. Of the 8 who reported some college, 4 were cautious screeners, 1 a ready screener, and 3 fearful avoiders, indicating a distribution of these participants across cluster groups.
Discussion
The cluster analysis used to establish the typology in this sample of African Americans with limited literacy produced clear distinctions among patient types on the basis of their attitudes and health maintenance preferences. Differences were also evident in perceptions of barriers to colonoscopy and self-reported screening outcomes. The resulting typology clearly demonstrates that there are important subgroups related to orientation toward preventive health within what is sometimes misperceived as a relatively homogeneous sociodemographic population. For example, ready screeners who have a positive orientation toward the medical establishment, see screening tests as well worth the effort, and would rather know if they have cancer. This is validated by the fact that of the three clusters, the ready screeners have the highest percentage of individuals who have already had a colonoscopy (65%). On the other extreme, the fearful avoiders, who have a negative orientation, score lower on these attributes and are the least likely to have had a colonoscopy (24.3%).
One of the most striking findings from the typology is the existence and size of the fearful avoiders group. This group differed significantly from the ready screeners and cautious screeners in their perceptions of the medical establishment, their hesitancy to be screened, their belief that if they get sick it is “God’s will,” and if they get cancer, they would “rather not know.” Because the fearful avoiders are 30.4% of the sample, they represent a very important target group for preventive screening messages. It should also be recognized that because participants in this study were recruited from a health care setting, and because fearful avoiders are prone to stay away from such settings, it is highly likely that the size of this group is substantially larger than 30%. This is a likelihood that must be addressed in follow-up studies. In addition, reversing what has become a stereotypical view of African Americans as being disinterested in preventive health practices, CRC screening in particular, could alter physicians’ assumptions about how to communicate effectively with the two thirds of this population that has a more positive orientation toward being screened. Taken together, these changes in understanding could be used to increase screening rates in all groups and could have a dramatic effect on the burden of colorectal cancer in the African American community.
This segmentation analysis also allowed for further elucidation of barriers to CRC screening and colonoscopy, showing that barriers were different for different clusters of patients, and that some barriers that are widely believed to pertain to African Americans as a group were not issues for many in the ready screeners and cautious screener groups. For example, studies have indicated that lack of trust in the health care system and health providers is a significant barrier for African Americans in pursuing preventive health care, such as CRC screening (Carcaise-Edinboro & Bradley, 2008; Greiner, Born, Nollen, & Ahluwalia, 2005; James et al., 2002; Katz et al., 2004). This cluster analysis clearly shows that more than 50% of the total sample, the ready screeners, were quite trustful of their doctors and highly regarded their advice on screening. Also, though both the ready screeners and fearful avoiders indicated that getting cancer was “God’s will,” it was only significantly associated with CRC screening in the fearful avoiders group, despite other studies indicating African Americans have fatalistic beliefs regarding whether screening is needed because the future is in “God’s hands” (Green & Kelly, 2004; Greiner et al., 2005).
The fact that the cautious screeners were the least likely to agree that getting cancer is God’s will, raises an interesting question about whether their religious beliefs differ significantly from those of the other two groups. If so, this could be valuable information in the development of intervention strategies for this group. Future studies must clarify this possibility. Overall, it is clear that assumptions about the pervasiveness of fatalism as a barrier to preventive care may inadvertently lead to lower investment in enrolling African Americans in screening programs.
Likewise, studies have indicated that African Americans do not get screened for CRC because it is “embarrassing” (Greiner et al., 2005; McAlearney et al., 2008). In our study this was only a significant barrier for fearful avoiders, again indicating that a majority of African Americans in this study did not find being embarrassed a significant barrier to CRC screening. Last, many studies have indicated that cost is a significant barrier in African American populations (Peterson et al., 2008; Taylor et al., 2003). This was seen as a significant barrier in only the fearful avoiders group, likely a reflection of recent changes to Medicare/Medicaid reimbursement of colonoscopy. A major goal of this research was to demonstrate the value of having a well-defined typology of a target audience on the basis of their preventive orientation. The typology reported here is valuable in that it (a) verifies that important subgroups exist in populations that are assumed to be or that appear to be relatively homogeneous; (b) provides rich profiles of each type of individual, revealing useful comparisons and a better understanding of important differences that exist across types of individuals; (c) makes tailoring of communication strategies for each subtype feasible and potentially more accurate; (d) makes it possible to identify and better understand the most vulnerable types of individuals, allowing resources to be focused effectively; and (e) reduces potential stereotyping of all African Americans on the basis of findings specific only to a subgroup.
Although the clear distinctions among the three types of patients detailed in this study provide a solid theoretical argument for approaching these segments differently, the question of clinical application and/or clinical significance necessitates a way to identify patients by their screening orientation. An important next-step will be to develop instrumentation that can be quickly and easily administered in a clinical setting. Once administered, the typology scoring and/or characterization could become a valuable addition to the patient’s record.
Last, the results of this research also raise important questions about the way in which we approach the task of increasing screening rates in vulnerable populations through community health campaigns and health education programs. If orientation toward preventive health care is a strong predictor of actual behavior, our strategies might shift from a focus on targeting screening for individual diseases to broader health campaigns designed to change beliefs, values, and perceptions of medical care, and preventive care in general. To do this would also require a commitment to removing the types of system barriers that may be at the root of many fearful avoiders’ reluctance to embrace preventive health practices.
Limitations
This study used a convenience sample of 102 African Americans between the ages of 50 and 74 years for whom the usual source of care is a large, urban, hospital clinic who all had some form of insurance. As such, our results cannot be generalized beyond this study population. Given that interviewing was done in an available room within the clinic, it is possible that being in the clinic setting, while judging medical services and screening options, could potentially have biased patient responses toward a more positive orientation than had the study been done in a community setting. However, given that the clinic setting involved in this research is the patients’ primary location for medical services, and that they are familiar with and accustomed to addressing health-related issues in this setting, it is unlikely that the setting biased their responses.
In testing the literacy level of each patient, we were aware that participants might be uncomfortable about being asked to read the words on the REALM-R literacy instrument. Following standard procedure, we stopped asking patients to read after a second word could not be read. It is possible, however, that difficulty with this task could have put some participants into a defensive or negative frame of mind that could have biased some of their responses on the survey instrument. To minimize their discomfort if they did not know the words on the REALM-R, we framed the literacy testing by saying we understood that people have difficulty with medical language and that we were trying to understand which words were difficult.
Although there were no statistically significant differences in mean scores on the REALM-R across clusters, the inclusion of patients who were able to pronounce six or more words (i.e., could read at or above the sixth-grade level) potentially could have biased the results. However, the fact that these patients were distributed across all clusters suggests that literacy per se is not the underlying factor in preventive health behavior. In addition, given that these patients had only slightly better than a sixth-grade reading level as defined by the REALM-R, it is very likely that their inclusion had no significant effect on the final cluster results.
Conclusions
Overall, this project successfully defined a typology of limited literacy African American patients on the basis of their attitudes and preferences toward preventative health practices — rather than on their sociodemographic characteristics. The three resulting types of patients were then profiled on perceptions of barriers to CRC screening, and perceptions of colonoscopy as a specific method for colorectal cancer screening. Because patients in the sample have a stable usual source of care and insurance, they were likely to have had the opportunity to be screened. The relatively high rate of self-reported screening confirms this and lends further credence to our view that patient orientations, rather than system barriers, account for lack of screening.
Because the clustering variables in this study dealt with African American patients’ general attitudes toward preventive health practices in general, this typology potentially could be applied to other health-related areas where screening is encouraged. Having such a tool would facilitate assessments in these areas of study while simultaneously enhancing cross-study comparisons. In addition, segmentation would allow for more uniquely targeted and tailored health messages. The development of a validated typology of patient orientations constructed to be applicable to a variety of health conditions would thus serve to standardize how selected populations are characterized, and would detail their health-related attitudes, values, concerns, preferences, and behaviors. Having such a typology, used with standardized assessment tools or as a basis for development of health messages, could dramatically enhance the ability of clinicians to communicate with their patients and would permit public health practitioners to better target and tailor materials for the public. In addition, a standardized typology could help guide the development of larger scale communication campaigns, allowing for tracking of perceptions by subtypes across time, across geographic regions, and across socioeconomic contexts. This would be invaluable for understanding changing perceptions regarding health-protecting behaviors such as CRC screening and allow for refinement of messages across a variety of sociodemographic groups.
In conclusion, this study strongly supports the argument that understanding the heterogeneity that exists within sociodemographic subgroups can provide a broader canvas on which to paint more effective health messages. Also, it can provide health care clinicians and public health practitioners with valuable insights into the motivations and behaviors of at-risk populations.
Acknowledgments
The authors thank Karen Lin, M.D., M.P.H., and Brian Meyer, M.D., M.P.H., for their help in developing the project; and Johnson Britto, M.B.B.S., M.P.H., and Zanaib Ibrihim, M.P.H., for their contributions in collecting data for the study.
Funding
This research was supported by the National Cancer Institute (grant number 1R21CA120122).
Contributor Information
THOMAS F. GORDON, Department of Psychology, University of Massachusetts Lowell, Lowell, Massachusetts, USA
SARAH BAUERLE BASS, Department of Public Health, Temple University, Philadelphia, Pennsylvania, USA.
SHERYL B. RUZEK, Department of Public Health, Temple University, Philadelphia, Pennsylvania, USA
CAITLIN WOLAK, Department of Public Health, Temple University, Philadelphia, Pennsylvania, USA.
MICHAEL J. ROVITO, Department of Health Professions, University of Central Florida, Orlando, Florida, USA
DOMINIQUE G. RUGGIERI, Interdisciplinary Health Services, Saint Joseph’s University, Philadelphia, Pennsylvania, USA
STEPHANIE WARD, Bravo Health Advanced Care Center, Philadelphia, Pennsylvania, USA.
ANURADHA PARANJAPE, Department of General Internal Medicine, Temple University School of Medicine, Philadelphia, Pennsylvania, USA.
JUDITH GREENER, Department of Public Health, Temple University, Philadelphia, Pennsylvania, USA.
References
- Abratt R (1993). Market segmentation practices of industrial marketers. Industrial Marketing Management, 22, 79–84. [Google Scholar]
- Agrawal S, Bhupinderjit A, Bhutani MS, Boardman L, Nguyen C, Romero Y, … Figueroa-Moseley C (2005). Colorectal cancer in African Americans. American Journal of Gastroenterology, 100, 515–523. [DOI] [PubMed] [Google Scholar]
- Albrecht TL, & Bryant C (1996). Advances in segmentation modeling for health communication and social marketing campaigns. Journal of Health Communication, 1, 656–680. [DOI] [PubMed] [Google Scholar]
- American Cancer Society. (2010). Colorectal cancer facts & figures 2008–2010. Retrieved from http://www.cancer.org/downloads/STT/F861708_finalforweb.pdf
- Bass SB, Gordon TF, Ruzek SR, Wolak C, Ward S, Paranjape A, … Ruggieri D (2011). Perceptions of colorectal cancer screening in urban African American clinic patients: Differences by gender and screening status. Journal of Cancer Education, 26, 121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass PF, Wilson JF, & Griffith CH (2003). A shortened instrument for literacy screening. Journal of General Internal Medicine, 18, 1036–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrigan J, & Finkbeiner C (1992). Segmentation marketing: New methods for capturing business markets. New York, NY: Harper Business. [Google Scholar]
- Brown JD (1992). Benefit segmentation of the fitness market. Health Marketing Quarterly, 9, 19–28. [DOI] [PubMed] [Google Scholar]
- Bull FC, Kreuter MW, & Scharff DP (1999). Effects of tailored, personalized, and general health messages on physician activity. Patient Education and Counseling, 36, 181–192. [DOI] [PubMed] [Google Scholar]
- Carcaise-Edinboro P, & Bradley CJ (2008). Influence of patient–provider communication on colorectal cancer screening. Medical Care, 46, 738–745. [DOI] [PubMed] [Google Scholar]
- Carey MP, Vanable PA, Senn TE, Coury-Doniger P, & Urban MA (2008). Evaluating a two-step approach to sexual risk reduction in a publically-funded STI clinic: Rationale, design, and baseline data from the Health Improvement Project–Rochester (HIP-R). Contemporary Clinical Trials, 29, 569–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control & Prevention. (2012). Cancer screening—United States, 2010. Morbidity and Mortality Weekly Report, 61, 41–45. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6103a1.htm [PubMed] [Google Scholar]
- Cheng B, Chang C, & Liu I (2005). Enhancing care services quality of nursing homes using data mining. Total Quality Management & Business Excellence, 16, 575–596. [Google Scholar]
- Croft MJ (1994). Market segmentation. London, England: Routledge. [Google Scholar]
- Cross WE Jr. (1991). Shades of black: Diversity in African-American identity. Philadelphia, PA: Temple University Press. [Google Scholar]
- Davis RE, Alexander G, Calvi J, Wiese C, Greene S, Nowak M, … Resnicow K (2010). A new audience segmentation tool for African Americans: The Black Identity Classification Scale. Journal of Health Communication, 15, 532–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis TC, Crouch MA, Long SW, Jackson RH, Bates P, George RB, & Bairnsfather LE (1991). Rapid assessment of literacy levels of adult primary care patients. Family Medicine, 23, 433–435. [PubMed] [Google Scholar]
- Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, & Crouch MA (1993). Rapid estimate of adult literacy in medicine: A shortened screening instrument. Family Medicine, 25, 391–395. [PubMed] [Google Scholar]
- Dawson S (1989). Health care consumption and consumer social class: A different look at the patient. Journal of Health Care Marketing, 9, 15–25. [PubMed] [Google Scholar]
- Della LJ, DeJoy DM, & Lance CE (2009). Explaining fruit and vegetable intake using a consumer marketing tool. Health Education & Behavior, 36, 895–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickson PR, & Ginter JL (1987). Market segmentation, product differentiation, and marketing strategy. Journal of Marketing, 51, 1–10. [Google Scholar]
- Dolinsky AL, & Stinerock R (1998). Cultural affiliation and the importance of health care Attributes: Marketers can develop segmentation strategies for targeted patient groups. Marketing Health Services, 18, 28–37. [PubMed] [Google Scholar]
- Dominguez LV, & Page AL (1981). Stratification in consumer behavior research: An examination. Journal of the Academy of Marketing Science, 9, 250–271. [Google Scholar]
- Endresen KW (1988). Psychographic segmentation for marketing success: Health-related attitudes and lifestyles are the key. Healthcare Executive, 3, 26–29. [PubMed] [Google Scholar]
- Fletcher RH, O’Malley M, Earp JA, Littleton TA, Fletcher SW, Greganti MA, … Taylor J (1983). Patient priorities for medical care. Medical Care, 21, 234–242. [DOI] [PubMed] [Google Scholar]
- Green PM, & Kelly BA (2004). Colorectal cancer knowledge, perceptions, and behaviors in African Americans. Cancer Nursing, 27, 206–215. [DOI] [PubMed] [Google Scholar]
- Greiner KA, Born W, Nollen N, & Ahluwalia JS (2005). Knowledge and perceptions of colorectal cancer screening among urban African Americans. Journal of General Internal Medicine, 20, 977–983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover R, & Srinivasan V (1992). Reflections on a simultaneous approach to market segmentation and market structuring. Journal of Marketing Research, 29, 474–476. [Google Scholar]
- Hornik RC, & Ramirez AS (2006). Racial/ethnic disparities and segmentation in communication campaigns. American Behavioral Scientist, 49, 868–884. [Google Scholar]
- James AS, Campbell MK, & Hudson MA (2002). Perceived barriers and benefits to colon cancer screening among African Americans in North Carolina: How does perception relate to screening behavior? Cancer Epidemiology Biomarkers & Prevention, 11, 529–534. [PubMed] [Google Scholar]
- Katz ML, James AS, Pignone MP, Hudson MA, Jackson E, Oates V, & Campbell MK (2004). Colorectal cancer screening among African American church members: A qualitative and quantitative study of patient–provider communication. BMC Public Health, 4, 62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar RV, & Rust RT (1989). Market segmentation by visual inspection. Journal of Advertising Research, 29, 23–30. [Google Scholar]
- Maibach EW, Weber D, Massett H, Hancock GR, & Price S (2006). Understanding consumers’ health information preferences: Development and validation of a brief screening instrument. Journal of Health Communication, 11, 717–736. [DOI] [PubMed] [Google Scholar]
- McAlearney AS, Reeves KW, Dickinson SL, Kelly KM, Tatum C, Katz ML, & Paskett ED (2008). Racial differences in colorectal cancer screening practices and knowledge within a low-income population. Cancer, 112, 391–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris L, & Schmolze R (2006). Consumer archetypes: A new approach to developing consumer understanding frameworks. Journal of Advertising Research, 46, 289–300. [Google Scholar]
- Morris L, Tabak E, & Olins NJ (1992). A segmentation analysis of prescription drug information seeking motives among the elderly. Journal of Public Policy and Marketing, 11, 115–125. [Google Scholar]
- Morrison M, Murphy T, & Nalder C (2003). Consumer preferences for general practitioner services. Health Marketing Quarterly, 20, 3–19. [DOI] [PubMed] [Google Scholar]
- Palmer RC, Midgette LA, & Buadoo I (2008). Colorectal cancer screening and African Americans: Findings from a qualitative study. Cancer Control, 15, 72–79. [DOI] [PubMed] [Google Scholar]
- Peterson NB, Murff HJ, Fowke JH, Cui Y, Hargreaves M, Signorello LB, & Blot WJ (2008). Use of colonoscopy and flexible sigmoidoscopy among African Americans and Whites in a low-income population. Preventing Chronic Disease, 5, 1–4. [PMC free article] [PubMed] [Google Scholar]
- Radio One & Yankolovic. (2012). Black American Study. Retrieved from http://www.blackamericastudy.com/index.htm
- Reardon G, & Pathak DD (1990). Segmenting the antihistamine market: An investigation of consumer preferences. Journal of Health Care Marketing, 10, 22–33. [PubMed] [Google Scholar]
- Risker DC (1995). A segmentation analysis of consumer uses of health information. Health Marketing Quarterly, 12, 39–48. [DOI] [PubMed] [Google Scholar]
- Rose JS, Chassin L, Presson C, Sherman SJ, Stein MD, & Col N (2007). A latent class typology of young women smokers. Addiction, 102, 1310–1319. [DOI] [PubMed] [Google Scholar]
- Scammon DL, Smith JA, & Beard T (1991). Mammography screening services: Market segments and messages. Journal of Ambulatory Care Marketing, 4, 1–16. [DOI] [PubMed] [Google Scholar]
- Slater MD, Basil MD, & Maibach EW (1999). A cluster analysis of alcohol-related attitudes and behaviors in the general population. Journal of Studies on Alcohol & Drugs, 60, 667–74. [DOI] [PubMed] [Google Scholar]
- Taylor V, Lessler D, Mertens K, Tu S, Hart A, Chan N, Shu J, & Thompson B (2003). Colorectal cancer screening among African Americans: The importance of physician recommendation. Journal of the National Medical Association, 95, 806–812. [PMC free article] [PubMed] [Google Scholar]
- Trigg D, Peterson K, & Meekers D (1997). Psychographic predictors of risky sexual practice. Safaids News: Southern Africa AIDS Information Dissemination Service Bulletin, 5, 13–15. [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force. (2002). Screening for colorectal cancer: Recommendations and rationale. Retrieved from http://www.ahrq.gov/clinic/3rduspstf/colorectal/colorr.htm
- Wahyuningsih TJ (2008). A study on customer satisfaction across information search behavior typology. Gadjah Mada. International Journal of Business, 10, 25–46. [Google Scholar]
- Ward SH, Lin K, Meyer B, Bass SB, Parameswaran L, Gordon TF, & Ruzek SB (2008). Increasing colorectal cancer screening among African Americans, linking risk perception to interventions targeting patients, communities and clinicians. Journal of the National Medical Association, 100, 748–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward SH, Parameswaran L, Bass SB, Paranjape A, Gordon TF, & Ruzek SB (2010). Resident physicians’ perceptions of barriers and facilitators to colorectal cancer screening for African Americans. Journal of the National Medical Association, 102, 303–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weber D, Wolff LS, Orleans T, Mockenhaupt RE, Massett HA, & Vose KK (2007). Smokers’ attitudes and behaviors related to consumer demand for cessation counseling in the medical care setting. Nicotine & Tobacco Research, 9, 571–580. [DOI] [PubMed] [Google Scholar]
- Wheeler SC, & Berger J (2007). Same prime, different effects: Segmentation in nonconscious behavior. Advances in Consumer Research—North American Conference Proceedings, 34, 155–156. [Google Scholar]
- Williams JE, & Flora JA (1995). Health behavior segmentation and campaign planning to reduce cardiovascular disease risk among Hispanics. Health Education Quarterly, 22, 36–48. [DOI] [PubMed] [Google Scholar]
- Wolak CN, Ruzek SB, Bass SB, & Gordon TF (2009, October). Assessing literacy in a low-income African American clinic population to facilitate improving health education interventions. Paper presented at the National Health Literacy Conference, Washington, D.C. [Google Scholar]
- Wolff LS, Massett HA, Maibach EW, Weber D, Hassmiller S, & Mockenhaupt RE (2010). Validating a health consumer segmentation model: Behavioral and attitudinal differences in disease prevention-related practices. Journal of Health Communication, 15, 167–188. [DOI] [PubMed] [Google Scholar]
- Wong DL, & Baker CM (1988). Pain in children: Comparison of assessment scales. Pediatric Nursing, 14, 9–17. [PubMed] [Google Scholar]
- Wong DL, & Baker CM (2001). Smiling face as anchor for pain intensity scales. Pain, 89, 295–297. [DOI] [PubMed] [Google Scholar]


