Abstract
Background
There is a variety of techniques for closing the abdominal wall during caesarean section. Some methods may be better in terms of postoperative recovery and other important outcomes.
Objectives
To compare the effects of alternative techniques for closure of the rectus sheath and subcutaneous fat on maternal health and healthcare resource use.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group trials register (September 2003), MEDLINE (1966 to September 2003), EMBASE (1980 to September 2003), CINAHL (1983 to September 2003) and CAB Health (1973 to September 2003), and the reference lists of included articles.
Selection criteria
Randomised trials making any of the following comparisons: (a) any suturing technique or material used for closure of the rectus sheath versus any other; (b) closure versus non‐closure of subcutaneous fat; (c) any suturing technique or material used for closure of the subcutaneous fat versus any other; (d) any type of needle for repair of the abdominal wall in caesarean section versus any other; (e) any other comparison of methods of abdominal wall closure.
Data collection and analysis
Both reviewers evaluated trials for eligibility and methodological quality without consideration of their results.
Main results
Seven studies involving 2056 women were included. The risk of haematoma or seroma was reduced with fat closure compared with non‐closure (relative risk (RR) 0.52, 95% confidence interval (CI) 0.33 to 0.82), as was the risk of 'wound complication' (haematoma, seroma, wound infection or wound separation) (RR 0.68, 95% CI 0.52 to 0.88). No difference in the risk of wound infection alone or other short‐term outcomes was found. No long‐term outcomes were reported. There was no difference in the risk of wound infection between blunt needles and sharp needles in one small study. No studies were found examining suture techniques or materials for closure of the rectus sheath or subcutaneous fat.
Authors' conclusions
Implications for practice Closure of the subcutaneous fat may reduce wound complications but it is unclear to what extent these differences affect the well‐being and satisfaction of the women concerned.
Implications for research Further trials are justified to investigate whether the apparent increased risk of haematoma or seroma with non‐closure of the subcutaneous fat is real. These should use a broader range of short‐ and long‐term outcomes, and ensure that they are adequately powered to detect clinically important differences. Further research comparing blunt and sharp needles is justified, as are trials evaluating suturing materials and suturing techniques for the rectus sheath.
Plain language summary
Techniques and materials for closure of the abdominal wall in caesarean section
There is not enough evidence to say whether particular techniques for closing the abdominal wall during caesarean section are better than others.
Different techniques and suture materials are used in caesarean section for closure of the rectus sheath (fibrous material enclosing the muscles of the abdominal wall). No research has examined whether any technique for closing the rectus sheath is preferable. The subcutaneous fat (between the sheath and the skin) may be left to heal without suturing, or can be closed using a variety of techniques. Closing the subcutaneous fat may reduce the risk of some wound complications (haematoma and seroma) but further research is needed to investigate how these outcomes affect the well‐being and recovery of the women concerned.
Background
Caesarean section is the commonest major operation performed on women in the world. Essentially the operation involves exposing the uterus by entering the abdominal cavity through the abdominal wall. The lining of the abdomen (peritoneum) is opened and the peritoneum covering the uterus is usually also entered. The bladder is reflected away from the uterus to reduce the chance of damage to it during the operation. The uterus is then incised and the baby and placenta delivered. Adequate haemostasis is achieved by closure of the uterine muscle followed by closure of the abdominal wall.
There are many possible ways of performing a caesarean section operation, and operative techniques vary widely. The techniques used may depend on many factors including the clinical situation and the preferences of the operator. For an overview of surgical techniques, indications for caesarean section and postoperative complications, see the protocol for a Cochrane review 'Techniques for caesarean section' (Hofmeyr 2004).
This review summarises randomised controlled trials comparing alternative techniques and materials for closure of the rectus sheath and the superficial (subcutaneous) fat layer of the abdominal wall. The rectus sheath is the fibrous material which encloses the muscles of the abdominal wall. The superficial fat lies between the sheath and the skin.
For closure of the rectus sheath, there are several possible suturing techniques and materials. A survey of techniques used in caesarean section operations by obstetricians in the UK conducted in 1999 (Tully 2002) found that the majority of operators (73%) used a continuous non‐locking suture, 21% used a continuous non‐locking suture with a single central lock, and the remainder used a continuous locking suture (5%), interrupted sutures (less than 1%), or more than one technique. Vicryl was the most commonly used suture material (87%), with small numbers using chromic catgut, plain catgut, dexon, monocryl, or other suture materials. As with other aspects of surgical technique for caesarean section, the methods used in other countries may be very different from those used in the UK.
The subcutaneous fat may be closed (sutured), or left unsutured with the wound being closed by suturing the skin only (seeAlderdice 2003). The theoretical advantage of closing the fat layer is the removal of space under the skin where blood or serous fluid could collect and lead to infection. The theoretical advantages of not closing it include a faster operation, less foreign material in the wound to provide a focus for infection, and greater tissue mobility leading to easier skin closure and a more attractive scar. These theoretical advantages and disadvantages may be perceived differently by operators depending on the thickness of the subcutaneous fat. Some obstetricians would argue that the greater the fat thickness, the more reason for closure (to close a potential empty space). Others would argue that the thinner the fat layer the more reason for closing it in order to bring wound edges together and allow the skin to heal under less tension. In the UK survey (Tully 2002), there was clear variation in practice between obstetricians: 42% stated that they always closed the fat layer, 1% sometimes closed it, 21% never closed it, 28% closed it only if it was thick, and 8% closed it only if it was thin. The thickness of the fat layer under the skin therefore influenced practice. A range of suturing techniques and materials are used. Most UK obstetricians reported using continuous non‐locking (35%) or interrupted (63%) sutures for the subcutaneous fat, and most used plain catgut (56%) or vicryl (30%).
This review incorporates the Cochrane review 'Closure of camper fascia at caesarean section' (CCPC 1995). We combined the results of studies addressing closure of Camper's fascia with the results of studies addressing fat closure. This decision was taken because Camper's fascia is defined as the fatty outer layer of the connective tissue between the skin and the rectus sheath and therefore closure of the subcutaneous fat would incorporate this layer.
'Blunt' needles which are designed to penetrate tissue while being less likely to penetrate skin have been advocated in areas where there is a high risk of blood‐borne infections such as HIV and Hepatitis B. The theoretical advantage of blunt needles is that they reduce the chance of transmission of infection from operator to patient or vice versa through inadvertent needle‐stick injury to the operator. The theoretical disadvantages of blunt needles include the fact that they may lead to more tissue trauma and therefore a worse outcome for the patient.
Objectives
To compare, using the best available evidence, the effects of alternative techniques for closure of the rectus sheath and subcutaneous fat at caesarean section on maternal health and the use of healthcare resources.
Methods
Criteria for considering studies for this review
Types of studies
We aimed to examine all published, unpublished and ongoing randomised controlled trials comparing techniques and materials for closure of the rectus sheath or subcutaneous fat. No unpublished or ongoing randomised controlled trials were identified. We planned to exclude quasi‐randomised trials (e.g. those randomised by date of birth or hospital number) from the analysis but none were identified. Studies reported only in abstract form were considered for inclusion in the review. We planned to list them under 'studies awaiting assessment ' if they did not report sufficient details of their methodology or results while we contacted the authors. This did not prove to be necessary.
Types of participants
Women undergoing a caesarean section.
Types of interventions
Trials were included in the review if they made any of the following comparisons: (a) any suturing technique or material used for closure of the rectus sheath versus any other; (b) closure versus non‐closure of subcutaneous fat or Camper's fascia; (c) any suturing technique or material used for closure of the subcutaneous fat or Camper's fascia versus any other; (d) any type of needle for repair of the abdominal wall in caesarean section versus any other; (e) any other comparison of methods of abdominal wall closure.
Examples of possible suturing techniques include: continuous non‐locking (with or without single central lock), continuous locking and interrupted. Examples of possible suturing materials include: chromic catgut, plain catgut, vicryl, dexon, monocryl and others. Examples of types of needles include: blunt, sharp, round‐bodied, cutting, hand‐held and others.
Types of outcome measures
Short‐term outcomes (up to six months after hospital discharge)
Postoperative febrile morbidity (as defined by trial authors) Postoperative analgesia (as defined by trial authors) Postoperative pain (visual analogue scale score) Blood transfusion Postoperative anaemia (as defined by trial authors) Wound infection (as defined by trial authors) Wound complications (including operative procedures carried out on the wound and wound haematoma) Breastfeeding (at discharge or as defined by trial authors) Voiding problems (as defined by trial authors) Duration of surgery Thromboembolism Need for re‐laparotomy Maternal death or admission to intensive care unit
Long‐term outcomes (more than six months after discharge)
Long‐term wound complications e.g. numbness, keloid formation, incisional hernia Fertility problems (e.g. secondary infertility due to adhesion formation) Complications in future pregnancy (e.g. placenta praevia, uterine rupture) Complications at future surgery (e.g. adhesion formation)
Health service use
Length of postoperative hospital stay Re‐admission to hospital
Only outcomes with available data were included in the analysis table. We planned to appropriately label any outcome data that were not prespecified by the reviewers but which were reported by the authors. No data on outcomes that were not prespecified were provided.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group trials register (September 2003).
The Cochrane Pregnancy and Childbirth Group's trials register is maintained by the Trials Search Co‐ordinator and contains trials identified from: 1. quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL); 2. monthly searches of MEDLINE; 3. handsearches of 30 journals and the proceedings of major conferences; 4. weekly current awareness search of a further 37 journals.
Details of the search strategies for CENTRAL and MEDLINE, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the 'Search strategies for identification of studies' section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
Trials identified through the search activities described above are given a code (or codes) depending on the topic. The codes are linked to review topics. The Trials Search Co‐ordinator searches the register for each review using these codes rather than keywords.
In addition, we searched MEDLINE (1966 to September 2003), EMBASE (1980 to September 2003), CINAHL (1983 to September 2003) and CAB Health (1973 to September 2003) using a combination of the following key words: c?esarean or c?eserean; 'Cesarean‐Section' (all subheadings); c?esarian or c?serian; Pfannenstiel; Joel Cohen or Joel‐Cohen; Lower segment near c?es?r?an;
Searching other resources
We also conducted a manual search of the reference lists of all identified papers.
Data collection and analysis
Trials were evaluated for appropriateness for inclusion and methodological quality without consideration of their results. This was done by both review authors according to the prestated eligibility criteria.
We assessed eligible trials using the following criteria for quality: 1. generation of random allocation sequence: adequate, inadequate, unclear; 2. allocation concealment: A = adequate, B = unclear, C = inadequate; 3. blinding of participants: yes, no, inadequate, no information; 4. blinding of caregivers: yes, no, inadequate, no information; 5. blinding of outcome assessment: yes, no, inadequate or no information; 6. completeness of follow‐up data (including any differential loss of participants from each group): A = less than 3% of participants excluded B = 3% to 9.9% of participants excluded C = 10% to 19.9% excluded D = 20% or more excluded E = unclear; 7. analysis of participants in randomised groups.
If a publication did not report analysis of participants in their randomised groups, we attempted to restore them to the correct group.
Both reviewers extracted data from the original publications onto data extraction forms. We resolved differences of opinion about eligibility or quality by discussion.
Two trials (Allaire 2000; Magann 2002) randomised women to three groups: suturing of subcutaneous fat, subcutaneous drain, or neither. For comparing suturing of fat with no suturing, we have combined the drain and no suture groups. This was done for dichotomous outcomes by summing the events and denominators for these two groups, and for continuous outcomes by calculating the combined means and standard deviations for the two groups.
We used fixed effect meta‐analysis for combining study data if trials were sufficiently similar for this to be reasonable. We performed the meta‐analysis using relative risks as the measure of effect size for binary outcomes, and weighted mean differences for continuous outcome measures. If trials used different ways of measuring the same continuous outcome (for example pain), we used standardised mean differences if possible. We investigated heterogeneity by calculating I2 statistics (Higgins 2002). If this had identified a high level of heterogeneity among the trials included in an analysis, a random effects meta‐analysis would have been preferred for an overall summary. If we had found a high level of heterogeneity, we would have explored it by the prespecified subgroup analyses. We would also have performed sensitivity analyses excluding the trials most susceptible to bias based on the quality assessment: those with inadequate allocation concealment (B or C); high levels of postrandomisation losses or exclusions (D); or unblinded outcome assessment, or blinding of outcome assessment uncertain.
Planned subgroup analyses were: (1) first versus repeat caesarean section versus mixed or undefined (trials that recruited both first and repeat caesareans or provide no information will be included in the mixed or undefined category); (2) prelabour versus intrapartum caesarean section versus mixed or undefined; (3) preterm versus term caesarean section versus mixed or undefined; (4) general versus regional anaesthesia versus mixed or undefined; (5) for comparison of closure versus non‐closure of superficial fat: obese versus non‐obese women.
Investigation of heterogeneity would have used the methods of Deeks 2001 to assess differences between the subgroups if this had been required.
Results
Description of studies
Seven studies met the inclusion criteria for the review. Five randomised controlled trials compared closure versus non‐closure of the subcutaneous fat, one compared closure versus non‐closure of Camper's fascia, and one compared blunt‐tipped versus sharp‐tipped needles for abdominal closure (Stafford 1998). In this review, the study addressing closure of Camper's fascia is combined with the studies addressing fat closure. We felt this was reasonable because Camper's fascia is defined as the fatty outer layer of the connective tissue between the skin and the rectus sheath and therefore closure of the subcutaneous fat would incorporate this layer.
All studies recruited women having either first or repeat caesarean sections, and all recruited both prelabour and intrapartum caesareans. Both transverse and vertical skin incisions were included in four of the seven studies. Cetin 1997 and Stafford 1998 only included transverse incisions, and Allaire 2000 did not specify the type of skin incision.
Of the six trials comparing closure versus non‐closure of subcutaneous fat, two were three‐armed studies that randomised women to suturing of subcutaneous fat, subcutaneous wound drain, or neither (Allaire 2000; Magann 2002). For comparison of suturing versus non‐suturing of the fat layer, the drain and no treatment groups have been combined in this review. In the other included studies, two specified that drains were not used (Cetin 1997; Chelmow 2002) and the extent of drain‐use in the remaining two is not known (Del Valle 1992; Naumann 1995).
Three studies restricted entry to women with 2 cm or more of subcutaneous fat (Allaire 2000; Magann 2002; Naumann 1995). One of these studies randomised women before surgery, and excluded them from the analysis if subcutaneous fat thickness was found during surgery to be less than 2 cm (Magann 2002). Allaire 2000 and Naumann 1995 randomised during surgery, after measurement of subcutaneous fat thickness. In addition, in Del Valle 1992 the mean body mass index of both groups exceeded 30, although the study was not stated to be restricted to obese women.
The timescale over which outcomes were recorded varied between the studies comparing suturing versus non‐suturing of the subcutaneous fat. All studies followed up all the women until discharge from hospital, but they varied in the way in which outcomes after discharge were recorded. Two studies did not attempt to follow up all women systematically (Cetin 1997; Del Valle 1992); instead they stated that "women were instructed to return if they developed problems". Another study performed a chart review (timing not stated) to detect outcomes after discharge (Allaire 2000). It is likely that in these three studies some outcomes were missed because women who developed problems may have been treated elsewhere. Magann and Naumann attempted to contact all women two to six weeks after discharge, failing to reach 24% and 22% respectively. The rates of loss to follow up were therefore relatively high. The final trial attempted to follow up all women until six weeks after surgery (Chelmow 2002) and women were only included in the analysis if they had at least one postpartum visit. The rate of loss to follow up was 15%.
Stafford 1998 randomised women to the use of 45 mm blunt‐tipped or sharp‐tipped needles for the suturing of uterine muscle, parietal and visceral peritoneum, rectus muscle (if sutured), rectus sheath and fat (optional).
Risk of bias in included studies
Randomisation and allocation concealment
Five studies used opaque sealed envelopes to randomise women (Allaire 2000; Chelmow 2002; Magann 2002; Naumann 1995; Stafford 1998). Four of these used a computer‐generated randomisation schedule to produce the randomised allocations contained within the envelopes. The fifth (Stafford 1998) placed equal numbers of blunt‐tipped and sharp‐tipped needles in envelopes, which were then "mixed in a random order". None of the studies mentioned numbering of envelopes or any other methods for ensuring that all of them could be accounted for. It is therefore unknown whether any envelopes were opened and their allocations not used, and hence whether there is any suspicion that randomisation may have been subverted.
The procedure used by Magann of randomising before surgery, and excluding women from the analysis if their subcutaneous fat thickness was less than 2 cm could cause problems (Magann 2002). Firstly, a strict intention to treat analysis was not carried out because a large proportion of those randomised were known not to be eligible (374/964). Secondly, assessment of eligibility once the woman's randomised group was already known could potentially introduce bias. Surgeons' decisions about eligibility in cases where the subcutaneous fat thickness was close to 2 cm may have been influenced, consciously or unconsciously, by the random assignment. However, no differences between the groups in baseline characteristics were apparent.
Del Valle 1992 stated that randomisation was via a computer‐generated list kept in the delivery unit. This suggests that the list was open and that there was no allocation concealment.
Cetin 1997 gave no information about either generation of the random sequence or how women were assigned to groups.
Blinding
Blinding of surgeons (caregivers) was not possible in any of the trials. One study (Chelmow 2002) stated that the women participating were blind to their randomisation group. It is likely that in the other trials women were also unaware of the group they had been assigned to but this was not documented. Four studies attempted to have blinding of outcome assessment. Two trials stated that doctors assessing outcomes were 'encouraged not to refer to the randomisation list' (Cetin 1997; Del Valle 1992). It is not recorded whether these doctors were actually aware of women's allocations when assessing outcomes. Chelmow stated that outcome assessment was "effectively blinded", as the trial allocations were not recorded in patients' charts, and would not normally be available. Naumann stated that postoperative care providers were blinded, which implies blinding of outcome assessment. Allaire and Magann did not state whether outcome assessors were blinded to the randomised allocations or not.
Exclusions and ITT analysis
Two studies that attempted long‐term follow up at two to six weeks reported high levels of loss to long‐term follow up, although there was short‐term assessment of outcomes in all the women recruited (Magann 2002; Naumann 1995). The results reported in these papers did not refer only to those women who were successfully followed up, but included data from earlier time points when all women were examined. Thus, it would not be correct to use the number of women followed up as the denominator, as some of those who had outcomes may not have had a follow‐up examination. The denominator used in the review is therefore the number of women with some outcome information. The same denominator was used for each outcome in each individual trial. Stafford 1998 may have had a high level of postrandomisation exclusions. The report states that "all women undergoing caesarean delivery [at their hospital] between October 1994 and December 1995 were randomised", and that an unspecified number of patients were not included in the analysis because they were discharged before their wound could be assessed. If it is true that all women who had caesarean delivery were randomised over a 14 month period, several hundred must have been randomised, but only 204 women were included in the published paper.
Other studies reported low numbers of postrandomisation exclusions.
Effects of interventions
A total of seven studies involving 2056 women were included in the review.
Six randomised controlled trials with a total of 1853 women examined the effects of closure versus non‐closure of subcutaneous tissue at caesarean section on maternal outcomes (Allaire 2000; Cetin 1997; Chelmow 2002; Del Valle 1992; Magann 2002; Naumann 1995). One randomised controlled trial with a total of 203 women examined the effects of blunt needles versus sharp needles for closure of all layers at caesarean section on maternal outcome (Stafford 1998). No trials were found looking at different techniques or materials for closing the rectus sheath or the subcutaneous tissues.
Closure versus non‐closure of the subcutaneous tissue (fat and/or camper fascia)
These trials reported wound infection and various wound complications such as haematoma, seroma and wound separation as their outcomes. None of the trials reported long‐term outcomes and many of the trials were not clear about the time‐point at which complications were identified and whether all the women had been followed up for the same length of time. All the trials gave definitions of the outcomes of interest but these definitions varied between studies.
Allaire 2000 reported the incidences of wound infection, haematoma, seroma and wound separation separately and then gave a combined 'wound complication' outcome in which each woman was counted only once. Cetin 1997, Magann 2002 and Naumann 1995 reported the incidences of wound infection, haematoma and seroma as mutually exclusive diagnoses. Chelmow 2002 reported the incidences of wound infection, wound separation and of haematoma/seroma separately, and then gave a combined 'wound complication' outcome in which each woman was counted only once. Del Valle 1992 did not report the results by randomised group. The only result we could extract was the incidence of 'superficial wound disruption' which included infection, haematoma and seroma. In addition, Magann 2002 reported the incidence of endometritis, mean blood loss at surgery and mean duration of surgery. Naumann 1995 also reported duration of surgery and readmission to hospital but it was not possible to distinguish which of these were in the non‐closure group and which were in the closure group.
The meta‐analysis demonstrated no difference in wound infection risk between the closure group and the non‐closure group (relative risk (RR) 1.02, 95% confidence interval (CI) 0.69 to 1.50). Haematoma and/or seroma was less common in the closure group (RR 0.52, 95% CI 0.33 to 0.82). The aggregate outcome of 'wound complication' (which included one or more of wound infection, wound separation, haematoma and seroma) was significantly less frequent in the closure group (RR 0.68, 95% CI 0.52 to 0.88).
Magann 2002 found no difference in the incidence of endometritis between the closure and non‐closure groups (RR 0.77, 95% CI 0.46 to 1.28). There was also no difference in this study between the closure and the 'no drain or closure' groups for mean duration of surgery or mean blood loss.
Blunt needles versus sharp needles for closure of all layers at caesarean section
Stafford 1998 reported the incidence of wound infection only. This was reported in all women four days after surgery. At six weeks 36 out of 97 women (37%) had been lost to follow up in the blunt needle group. Thirty‐five out of 106 women (33%) were lost to follow‐up at six weeks in the sharp needle group. Four days after surgery there was no significant difference in the incidence of wound infection between the blunt needle group and the sharp needle group (RR 2.73, 95% CI 0.54 to 13.76).
Subgroup analyses
No subgroup analyses were performed because the results were not reported in the subgroups prespecified by us. One study reported results for obese (at least 2 cm fat) and non‐obese women (less than 2 cm fat) (Cetin 1997). There was no evidence of a different effect of fat closure on wound infection in the obese group when compared with the non‐obese group (at least 2 cm fat RR 0.31, 95% CI 0.03 to 2.89; less than 2 cm fat RR 1.89, 95% CI 0.18 to 19.83; interaction test p = 0.28). The other trials which recruited women regardless of their degree of obesity did not provide the data with a non‐obese subgroup to compare with the trials of obese women only.
Discussion
The methodology of the seven trials identified appeared to be generally satisfactory. However, many of the reports omitted important information, which meant that their susceptibility to bias could not be assessed adequately. Moreover, some of the trial reports were unclear about the number of women assessed for each outcome, which meant that assumptions were necessary to make the review possible.
Very few immediate outcomes and no long‐term outcomes were reported. The results suggest however that closure of the subcutaneous fat at caesarean section may lead to a reduction in wound complications in general, and haematomas and seromas in particular. However the effects on haematoma and seroma may not be robust because of the potentially subjective nature of these diagnoses and the fact that wound infection rates were found to be similar in the two groups. 'Seroma' in particular, which was the commonest complication found, appeared to be an extremely subjective diagnosis which may not have caused pathology or influenced the well‐being or satisfaction of the women concerned. The repercussions of the diagnoses were not reported. It is also possible that the assessment of these outcomes may have been influenced by knowledge of the women's randomised group.
There was no evidence to show that the risk of wound infection was different in the fat closure group or the non‐closure group.
A major problem with the findings is that the reported outcomes were diagnosed at different times following surgery using different criteria. It is not clear from some of the studies whether all the women were followed up for the same length of time. In those that simply invited women to return to hospital if they had any complications, adverse outcomes may easily have been missed by women going elsewhere for treatment.
The single small trial of blunt needles versus sharp needles found no difference in wound infection between the two groups (Stafford 1998). This was however a small trial with no power calculation and a wide confidence interval around the estimate of effect. It is therefore difficult to know what to conclude from this finding. As the use of blunt needles may potentially protect both patients and operators from the transmission of blood‐borne infections, and as they are already widely used in countries such as South Africa, further research to determine the outcomes with blunt needle use is justified.
No subgroup analyses were carried out because the data were not presented in a way which made this possible. Given that British obstetricians reported using different techniques depending on the amount of subcutaneous fat present (Tully 2002), it is important to determine whether obesity made a difference to the outcomes with fat closure or non‐closure.
Authors' conclusions
Implications for practice.
It is hard to draw conclusions from the small trials included in this review. The results suggest that closure of the subcutaneous fat may reduce wound haematoma and seroma but it is unclear to what extent these differences affect the well‐being and satisfaction of the women concerned.
Implications for research.
Further trials are justified using blinded outcome assessment to investigate whether the apparent increased risk of haematoma or seroma with non‐closure of the subcutaneous fat is real.
It is important to investigate whether the interventions and the outcomes reported lead to a different postoperative recovery experience for the women concerned. It is also important to know whether the interventions and outcomes reported lead to a difference in rates of medical interventions such as antibiotics, further surgery or prolonged admission. Trials looking at a broader range of immediate outcomes and at longer‐term outcomes, using an adequate power calculation to calculate the sample size required would be helpful.
Blunt needles may protect operators and patients from blood‐borne infections although more evidence is needed to confirm this. As they are already widely used in countries such as South Africa, further research to determine if the outcomes for women are unchanged with blunt needle use is justified.
There are currently no published trials looking at different suture techniques or materials for closure of the rectus sheath or subcutaneous fat at caesarean section.
What's new
| Date | Event | Description |
|---|---|---|
| 13 August 2008 | Amended | Converted to new review format. |
Acknowledgements
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), one or more members of the Pregnancy and Childbirth Group's international panel of consumers and the Group's Statistical Adviser.
Data and analyses
Comparison 1. Closure of subcutaneous tissue versus non‐closure of subcutaneous tissue.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Wound infection | 5 | 1348 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.69, 1.50] |
| 2 Haematoma +/‐ seroma | 5 | 1348 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.33, 0.82] |
| 3 Aggregate wound complications (infection, wound separation, haematoma or seroma) | 6 | 1786 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.52, 0.88] |
| 4 Endometritis | 1 | 590 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.46, 1.28] |
| 5 Duration of surgery (minutes) | 1 | 590 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [‐2.29, 3.49] |
| 6 Mean blood loss (ml) | 1 | 590 | Mean Difference (IV, Fixed, 95% CI) | 9.0 [‐24.29, 42.29] |
1.1. Analysis.
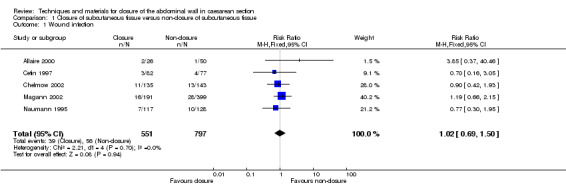
Comparison 1 Closure of subcutaneous tissue versus non‐closure of subcutaneous tissue, Outcome 1 Wound infection.
1.2. Analysis.
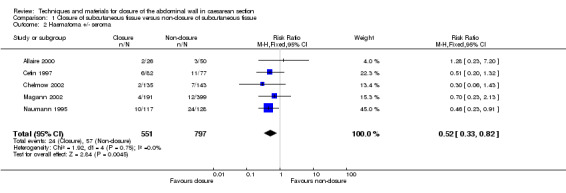
Comparison 1 Closure of subcutaneous tissue versus non‐closure of subcutaneous tissue, Outcome 2 Haematoma +/‐ seroma.
1.3. Analysis.
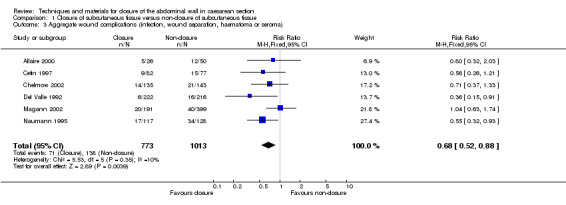
Comparison 1 Closure of subcutaneous tissue versus non‐closure of subcutaneous tissue, Outcome 3 Aggregate wound complications (infection, wound separation, haematoma or seroma).
1.4. Analysis.
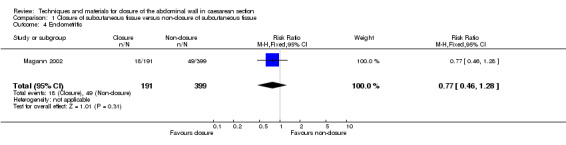
Comparison 1 Closure of subcutaneous tissue versus non‐closure of subcutaneous tissue, Outcome 4 Endometritis.
1.5. Analysis.
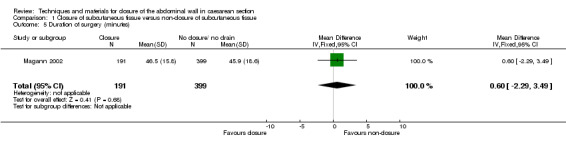
Comparison 1 Closure of subcutaneous tissue versus non‐closure of subcutaneous tissue, Outcome 5 Duration of surgery (minutes).
1.6. Analysis.
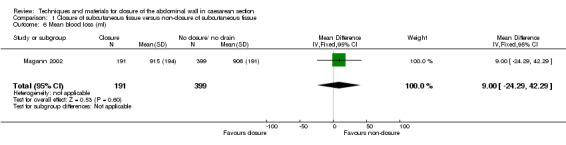
Comparison 1 Closure of subcutaneous tissue versus non‐closure of subcutaneous tissue, Outcome 6 Mean blood loss (ml).
Comparison 2. Blunt needles versus sharp needles for closure at caesarean section.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Wound infection | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.73 [0.54, 13.76] |
2.1. Analysis.
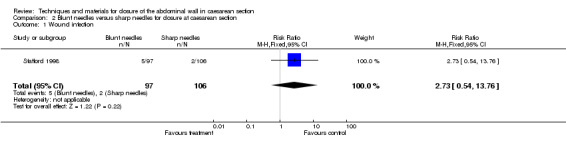
Comparison 2 Blunt needles versus sharp needles for closure at caesarean section, Outcome 1 Wound infection.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allaire 2000.
| Methods | Randomised controlled trial. Randomisation by computer generated random number sequence, after fat depth had been measured. Numbers kept in opaque envelopes. No information on whether all envelopes were accounted for. Caregivers (surgeons) not blinded. No information on whether participants or outcome assessors were blinded. | |
| Participants | 76 women undergoing caesarean section with more than 2 cm of subcutaneous fat.
26 women in the closure group and 50 women in the non‐closure group. Excluded if no time for adequate consent. Included if: first or repeat caesarean; prelabour or intrapartum caesarean. The type of skin incision was not described. |
|
| Interventions | Treatment group: closure of the subcutaneous tissue.
Control group for this review: non‐closure of the subcutaneous tissue (with or without subcutaneous drain). Three randomised groups: closure of subcutaneous tissue; subcutaneous drain used; no closure of subcutaneous tissue or use of subcutaneous drain. |
|
| Outcomes | Wound infection and wound complication incidence available on all randomised women.
No loss to follow up documented.
No significant difference in complications between the closure and the non‐closure groups. Wounds assessed prior to discharge and at staple removal (7 to 10 days postpartum). Further complications identified by retrospective chart review (timing not stated). |
|
| Notes | USA. 1995 to 1997. 1109 women delivered by caesarean section; 76 enrolled in the study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Cetin 1997.
| Methods | Randomised controlled trial. Randomised from a 'list' in theatre. No information on allocation concealment. Caregivers (surgeons) not blinded. No information on whether participants were blinded. Outcome assessors not blinded but were "encouraged not to refer to the randomisation list" until after assessing the wound. | |
| Participants | 164 women undergoing caesarean section.
It is not clear how many women were in the closure group and how many were in the non‐closure group. Excluded if prescribed antibiotics in the two weeks prior to caesarean, or if given antibiotics for cardiac prophylaxis. Included if: first or repeat caesarean; prelabour or intrapartum caesarean; obese or 'non‐obese'. All women in the trial had transverse skin incisions and no wound drains were used. |
|
| Interventions | Treatment group: closure of the subcutaneous fat. Control group: non‐closure of the subcutaneous fat. | |
| Outcomes | Wound infection and wound complication incidence available on 82 women in the closure group and 77 women in the non‐closure group.
Loss to follow up: 5 women. It is not clear from the paper which randomised group they were from.
No significant difference in complications between the closure and the non‐closure groups. Wounds assessed during hospital admission. Women were asked to return to the hospital "if they developed any problems". |
|
| Notes | Turkey. 1995 to 1997. Two groups of results reported; women with < 2 cm fat and women with > 2 cm fat. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Chelmow 2002.
| Methods | Randomised controlled trial. Randomisation by computer‐generated 'permuted blocks' at the time of caesarean section. Numbers kept in opaque envelopes. No information on whether all envelopes were accounted for. Caregivers (surgeons) not blinded. Participants blinded. Outcome assessors were 'effectively' blinded because the allocation was not recorded in the notes, but some dictated operative reports may have been available. | |
| Participants | 327 women undergoing caesarean section.
162 women in the closure group and 165 women in the non‐closure group. Excluded if delayed primary closure or drain insertion was planned preoperatively. Included if: first or repeat caesarean; prelabour or intrapartum caesarean; obese or 'non‐obese'; longitudinal or transverse skin incision. No wound drains were used. |
|
| Interventions | Treatment group: closure of the subcutaneous fat. Control group: non‐closure of the subcutaneous fat. | |
| Outcomes | Wound infection and wound complication incidence available on 135 in the closure group and 143 in the non‐closure group.
Loss to follow up: 27 women in the closure group; 22 women in the non‐closure group.
No significant difference in complications between the closure and the non‐closure groups. Outcomes assessed at a postpartum visit (4 to 8 weeks postpartum). |
|
| Notes | USA. 1995 to 1997. 631 women delivered by caesarean section; 327 enrolled in the study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Del Valle 1992.
| Methods | Randomised controlled trial. Randomisation by computer‐generated list of numbers kept in delivery suite. No information on allocation concealment. Caregivers (surgeons) not blinded. No information on whether participants were blinded. Outcome assessors were not blinded but were "encouraged not to look at the randomisation list until after assessing the wound". | |
| Participants | 451 women undergoing caesarean section.
It is not clear how many women were randomised to the closure group and how many women were randomised to the non‐closure group. No stated exclusion criteria. Included if: first or repeat caesarean; prelabour or intrapartum; longitudinal or transverse skin incision. No information on whether the women were obese or 'non‐obese'. Mean body mass index in both groups was greater than 30 kg/m2. No information on wound drain use. |
|
| Interventions | Treatment group: closure of the camper fascia. Control group: non‐closure of the camper fascia. | |
| Outcomes | Superficial wound disruption incidence (including wound infection, haematoma or seroma) available on 222 women in the closure group and 216 women in the non‐closure group.
Loss to follow up: 13 women. It is not clear from the paper which randomised groups they were from.
There were fewer wound complications in the closure group compared with the non‐closure group. Wounds assessed during hospital admission. Women were asked to return to the hospital "if they developed any problems". A chart review was also carried out at six weeks postpartum. |
|
| Notes | USA. 1991 to 1992. Results were not reported by randomised group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Magann 2002.
| Methods | Randomised controlled trial. Randomisation by random number. Numbers kept in opaque envelopes. No information on whether all envelopes were accounted for. Caregivers (surgeons) not blinded. No information on whether participants or outcome assessors were blind to the randomised allocations. | |
| Participants | 964 women undergoing caesarean section were randomised preoperatively.
590 women undergoing caesarean section were deemed eligible intra‐operatively because they had more than 2 cm of subcutaneous fat.
191 women in the closure group and 399 women in the non‐closure group Excluded if: no time for adequate consent; less than 2 cm of subcutaneous fat (when measured intraoperatively). Included if: first or repeat caesarean; prelabour or intrapartum caesarean; vertical or transverse skin incision. |
|
| Interventions | Treatment group: closure of the subcutaneous tissue.
Control group for this review: non‐closure of the subcutaneous tissue (with or without subcutaneous drain). Three randomised groups: closure of subcutaneous tissue; subcutaneous drain used; no closure of subcutaneous tissue or use of subcutaneous drain. |
|
| Outcomes | Wound infection, wound complication and endometritis incidence available on all randomised women at staple removal (7 to 10 days postpartum).
Mean blood loss and mean duration of operation also available.
No loss to follow up documented at discharge from hospital.
No significant difference in complications between the closure and the non‐closure groups. Unclear at which point in the follow up the recorded outcomes were diagnosed. |
|
| Notes | USA. 1998 to 2001. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Naumann 1995.
| Methods | Randomised controlled trial. Randomisation by computer generated random number sequence at time of surgery. Numbers kept in sealed envelopes. No information on whether all envelopes were accounted for. Caregivers (surgeons) not blinded. No information on whether participants were blinded. Outcome assessors were blind to the randomised allocations. | |
| Participants | 245 women undergoing caesarean section with more than 2 cm of subcutaneous fat.
117 women in the closure group and 128 women in the non‐closure group. No stated exclusion criteria. Included if: first or repeat caesarean; prelabour or intrapartum caesarean, longitudinal or transverse skin incision. No information on wound drain use. |
|
| Interventions | Treatment group: closure of the subcutaneous fat. Control group: non‐closure of the subcutaneous fat. | |
| Outcomes | Wound infection and wound complication incidence available on all randomised women. Outcomes assessed at hospital discharge, and at staple removal (7 to 10 days postnatally). There were significantly fewer wound complications in the closure group than in the non‐closure group. |
|
| Notes | USA. 1991 to 1993. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Stafford 1998.
| Methods | Randomised controlled trial. Randomisation by shuffling sealed envelopes containing needles. No information on whether all envelopes were accounted for. Caregivers (surgeons) not blind. No information on whether participants or outcome assessors were blind to the randomised allocations. | |
| Participants | 204 women undergoing caesarean section.
97 women in the blunt needle group and 106 women in the sharp needle group. 1 woman excluded ‐ allocation not known. No stated exclusion criteria. Included if: first or repeat caesarean; prelabour or intrapartum caesarean. The caesarean sections were consecutive and used a transverse skin incision. No information on obesity of patients or wound drain use. |
|
| Interventions | Treatment group: closure of the uterus, peritoneum and rectus sheath using dexon with blunt needles (fat closure optional).
Control group: closure of the uterus, peritoneum and rectus sheath using dexon with sharp needles (fat closure optional). One woman excluded because unable to use dexon throughout the operation. |
|
| Outcomes | Wound infection incidence available on 97 women in the blunt needle group and on 106 women in the sharp needle group at discharge (four days postnatally).
Loss to follow up: 1 woman excluded at surgery. No other loss to follow up at discharge.
Follow up at six weeks achieved for 61 women in the blunt needle group and 71 women in the sharp needle group. No significant difference in complications between the blunt needle and the sharp needle groups. Wounds assessed at discharge. |
|
| Notes | UK. 1994 to 1995. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Contributions of authors
Both reviewers contributed to writing the protocol.
E Anderson (EA) conducted the literature search. EA and S Gates both reviewed all the included papers and co‐wrote the review.
Declarations of interest
The National Perinatal Epidemiology Unit, where both reviewers work, is in the early stages of planning and seeking funding for an international randomised controlled trial which will evaluate materials for suturing rectus sheath as one of a number of interventions of interest. The CAESAR study which is evaluating closure versus non‐closure of the peritoneum, single versus double layer closure of the uterus and the use of a sub‐sheath drain at caesarean section is also being coordinated at the National Perinatal Epidemiology Unit.
Edited (no change to conclusions)
References
References to studies included in this review
Allaire 2000 {published data only}
- Allaire A, Fisch J, McMahon M. A prospective randomized trial of subcutaneous drain versus subcutaneous suture in obese women undergoing cesarean section. American Journal of Obstetrics and Gynecology 1998;178(1 Pt 2):S78. [Google Scholar]
- Allaire AD, Fisch J, McMahon MJ. Subcutaneous drain vs. suture in obese women undergoing cesarean delivery: a prospective, randomized trial. Journal of Reproductive Medicine 2000;45(4):327‐31. [PubMed] [Google Scholar]
Cetin 1997 {published data only}
- Cetin A, Cetin M. Superficial wound disruption after cesarean delivery: effect of the depth and closure of subcutaneous tissue. International Journal of Gynecology & Obstetrics 1997;57(1):17‐21. [DOI] [PubMed] [Google Scholar]
Chelmow 2002 {published data only}
- Chelmow D, Huang E, Strohbehn K. Closure of the subcutaneous dead space and wound disruption after cesarean delivery. Journal of Maternal‐Fetal & Neonatal Medicine 2002;11(6):403‐8. [DOI] [PubMed] [Google Scholar]
Del Valle 1992 {published data only}
- Valle GO, Combs P, Qualls C, Curet LB. Does closure of camper fascia reduce the incidence of post‐cesarean superficial wound disruption?. Obstetrics & Gynecology 1992;80(6):1013‐6. [PubMed] [Google Scholar]
Magann 2002 {published data only}
- Magann EF, Chauhan SP, Rodts‐Palenik S, Bufkin L, Martin Jr JN, Morrison JC. Subcutaneous stitch closure versus subcutaneous drain to prevent wound disruption after cesarean delivery: a randomized clinical trial. American Journal of Obstetrics and Gynecology 2002;186(6):1119‐23. [DOI] [PubMed] [Google Scholar]
Naumann 1995 {published data only}
- Naumann RW, Hauth JC, Owen J, Hodgkins P, Lincoln T. Approximation of the subcutaneous tissue lowers the incidence of wound complications after cesarean section. American Journal of Obstetrics and Gynecology 1994;170(1 Pt 2):341. [Google Scholar]
- Naumann RW, Hauth JC, Owen J, Hodgkins PM, Lincoln T. Subcutaneous tissue approximation in relation to wound disruption after cesarean delivery in obese women. Obstetrics & Gynecology 1995;85(3):412‐6. [DOI] [PubMed] [Google Scholar]
Stafford 1998 {published data only}
- Stafford M, Nanthakumaran H, Pitman M, Smith J. A randomised controlled study of wound morbidity comparing the use of blunt‐tipped versus sharp‐tipped needles. 27th British Congress of Obstetrics and Gynecology; 1995 July 4‐7; Dublin. 1995:420.
- Stafford MK, Pitman MC, Nanthakumaran N, Smith JR. Blunt‐tipped versus sharp‐tipped needles: wound morbidity. Journal of Obstetrics and Gynaecology 1998;18:18‐9. [DOI] [PubMed] [Google Scholar]
Additional references
Alderdice 2003
- Alderdice F, McKenna D, Dornan J. Techniques and materials for skin closure in caesarean section (Cochrane Review). The Cochrane Library 2003, Issue 4. [DOI] [PubMed] [Google Scholar]
Deeks 2001
- Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta‐analysis. In: Egger M, Davey Smith G, Altman DG editor(s). Systematic reviews in health care: meta‐analysis in context. London: BMJ Books, 2001. [Google Scholar]
Higgins 2002
- Higgins J, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21:1539‐58. [DOI] [PubMed] [Google Scholar]
Hofmeyr 2004
- Hofmeyr GJ, Mathai M. Techniques for caesarean section (Protocol for a Cochrane Review). The Cochrane Library 2004, Issue 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tully 2002
- Tully L, Gates S, Brocklehurst P, McKenzie‐McHarg K, Ayers S. Surgical techniques used during caesarean section operations: results of a national survey of practice in the UK. European Journal of Obstetrics & Gynecology and Reproductive Biology 2002;102:120‐6. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
CCPC 1995
- Enkin MW. Closure of Camper fascia at Caesarean section. In: Enkin MW, Keirse MJNC, Renfrew MJ, Neilson JP (eds.) Pregnancy and Childbirth Module of The Cochrane Database of Systematic Reviews, 1995 [updated 24 February 1995]. Available from BMJ Publishing Group: London.


