Abstract
Inflammatory bowel disease (IBD) is a chronic, relapsing gastrointestinal condition. Ulcerative colitis and Crohn’s disease are types of inflammatory bowel disease. Over many decades, the disease has been a topic of study, with experts still trying to figure out its cause and pathology. Researchers have established many in vivo animal models, in vitro cell lines, and ex vivo systems to understand its cause ultimately and adequately identify a therapy. However, in vivo animal models cannot be regarded as good models for studying IBD since they cannot completely simulate the disease. Furthermore, because species differences are a crucial subject of concern, in vitro cell lines and ex vivo systems can be employed to recreate the condition properly. In vitro models serve as the starting point for biological and medical research. Ex vivo and in vitro models for replicating gut physiology have been developed. This review aims to present a clear understanding of several in vitro and ex vivo models of IBD and provide insights into their benefits and limits and their value in understanding intestinal physiology.
Keywords: Inflammatory bowel disease, In vitro cell lines, Ex vivo systems, Organoids, Caco-2 cell lines, Gut-on-chip
Introduction
Inflammatory bowel disease (IBD) is a type of chronic gastrointestinal inflammatory condition that includes Crohn’s disease (CD) and ulcerative colitis (UC). IBD is marked by periods of stomach discomfort, bloody diarrhea, loss of weight, and infiltration of neutrophils and macrophages that release cytokines, proteolytic enzymes, and reactive species that cause inflammation and ulceration in the intestinal mucosa [1]. The colon and rectum are usually affected by ulcerative colitis. Crohn’s disease affects any region of the gut, although the terminal ileum is the most commonly affected [2, 3]. The incidence of IBD differs widely both within and between geographic areas. Crohn’s disease ranges from 8.9 to 17.45 in Europe, whereas ulcerative colitis has an incidence ranging from 4.1 to 21.47 [4]. The specific cause of IBD is unknown, but growing evidence shows that in genetically predisposed individuals, the development of IBD may be caused by a disruption in the finely controlled equilibrium between host response and gut commensal bacteria in the intestinal epithelium. Environmental variables like antibiotics, dietary components, tobacco, and nicotine may have a role in initiating and recurrence of ulcerative colitis or Crohn’s disease, or both, by modulating host immunological responses [5–9]. Since the specific etiology of IBD is unknown, several in vivo models or animal models have been developed throughout the years to investigate the disease’s pathophysiology. Chemically induced models include dextran sodium sulfate (DSS)-induced, trinitrobenzene sulphonic acid (TNBS)-induced, oxazolone-induced, acetic acid-induced, and carrageenan-induced models of IBD. Bacterial-induced models such as adherent invasive E. coli and salmonella models are also developed. Other in vivo models include genetically engineered, transgenic mice, mutation knock-in, and adoptive transfer models [10].
In vivo animal models are commonly used to simulate IBD. Still, they are too complicated to adjust the multiple IBD factors separately. Moreover, because of the vast inter-species variability between animal models and people, the success of IBD therapy is difficult to predict [11]. As a result of the constraints of using in vivo animal models to understand the pathophysiology of IBD and identify new medicines for treating it, researchers have attempted to establish numerous in vitro and ex vivo models of IBD. In both normal and diseased situations, these in vitro and ex vivo models investigate gastrointestinal physiology, intestinal epithelial function, host-microbiome interaction, absorption of the drug, and cell-cell co-culture.
The current review focuses on several in vitro and ex vivo models of inflammatory bowel disease and their benefits and drawbacks. The review also focuses on the most recent application of each model in research investigations to better understand inflammatory bowel disease.
In vitro models
Caco-2 cell line
Caco-2 cells, also known as cancer-coli-2 cells, are immortalized human colorectal adenocarcinoma cells [12]. Fogh created these cells in 1977 at the Sloan-Kettering Institute for Cancer Research [13]. Caco-2 cells develop independently in culture into a diverse collection of intestinal epithelial cells [12]. Hidalgo and his colleagues discovered the use of Caco-2 cells in research in the late 1980s [14]. While colon cancer produces these cells, they resemble enterocytes that line the intestines [15].
The differentiated Caco-2 cells show features identical to small bowel enterocytes, such as brush-border microvilli, and the production of characteristic digestive enzymes such as peptidases, sucrase-isomaltase, dipeptidyl peptidase IV, lactase, and aminopeptidase N [16, 17]. Caco-2 cells also possess the ability to produce various cytokines, which include interleukin 6, 8, and 15 (IL-6,8,15), tumor necrotic factor-α (TNF-α), and thymic stromal lymphopoietin (TSLP) [18–20]. Thus, the production of these cytokines enables the researchers to utilize the Caco-2 cells in those research involving the study of inflammation such as IBD. Several investigations correlated absorption data to Caco-2 permeability coefficients and found a significant connection, especially for substances carried passively [21–24]. The Dulbecco’s Modified Eagle Medium [25] is routinely used to preserve Caco-2 cell lines.
Caco-2 cell lines, as previously stated, are extremely useful for studying intestinal diseases owing to their close similarity to intestinal epithelial cells; yet, there are numerous restrictions or downsides to utilizing these cell lines. Not only do enterocytes exist in the normal epithelium, but there are many other types of cells as well. When Caco-2 cell lines are being used, mucus and an unstirred layer of water are not present in the solution. A variety of non-cellular factors influence a compound’s absorption in cells. Thus, phospholipids and bile acids have a significant impact on lipophilic component transport, and compound solubility in the mucus layer and the unstirred water layer near the epithelium has a considerable influence on in vivo absorption [12].
Many experts in colitis research have utilized and continue to use these cell lines extensively. Maria-Ferreira et al. conducted in vivo experiments on rhamnogalacturonan and in vitro tests on Caco-2 cells. The findings demonstrated that rhamnogalacturonan enhanced wound healing, reduced epithelial barrier dysfunction, and suppressed IL-1-induced IL-8 production in Caco-2 cells [26]. Chen et al. published research on astragalus polysaccharides revealed that astragalus inhibited ferroptosis in a mouse model of colitis and human Caco-2 cells by disrupting the NRF2/HO-1 cascade [27]. Another study conducted by Song et al. showed Epac-2 expression aided in repairing the intestinal barrier in the LPS-induced cell co-culture environment by increasing TJ protein expression and decreasing Caco-2 cell death [28]. Li et al. investigated the anti-inflammatory impact of allicin on ulcerative colitis induced by trinitrobenzene sulphonic acid. Allicin reduces the phosphorylation of P38 and JNK and the expression of NF-κB p65 in Caco-2 cells, which were raised after IL-1β treatment [29]. Effect of corn protein hydrolysate digests on TNF-α-induced iNOS, COX-2 protein expression, and IL-8 production in Caco-2 cells was studied by Liang et al. [30].
HT29 cell line
HT29, like Caco-2, is a human colon cancer-derived cell line. In 1964, Fogh and Trempe derived it from a 44-year-old Caucasian woman’s primary tumor [31]. Since several human colon cancer cell lines have been developed, these cell lines were initially employed to investigate elements of human cancer biology. These cells drew attention due to their ability to express mature intestinal cell features like enterocytes or mucus generating cells [32]. There are several similarities between Caco-2 and HT29 cells. Similar to Caco-2 cells, HT29 cells differentiate. HT29 cells also release digestive enzymes comparable to Caco-2 cell lines [33].
Previous research revealed that, like Caco-2 cell lines, HT29 cell lines release cytokines comparable to Caco-2 cells [34]. Another significant distinction between Caco-2 and HT29 cells is that HT29 cells could generate mucin at a reasonably high level [35]. The high rate of glucose consumption is the peculiar characteristic of HT29 cells. Hence, a high concentration of glucose is required in the medium. These HT29 cells did not exhibit any characteristics resembling intestinal epithelial cells when exposed to high glucose concentrations. They developed as a multilayer of undifferentiated, unpolarized cells [36]. As a result, the discovery of substituting glucose with galactose was made. Pinto et al. [37] discovered that replacing the media in which HT29 was put with galactose triggered enterocytic differentiation.
Many professionals in colitis studies have and continue to make substantial use of these HT29 cell lines. In a rat model of DSS-induced colitis, Rajendiran et al. used HT29 cells to study the efficacy of Alpinia officinarum extract on cell sustainability and expression of NF-κB and COX-2. The results revealed that increasing the concentration of extract increased cell mortality and lowered the viability of HT29 cells [38]. In another study performed by Lei et al., baicalin reduced LPS-induced HT29 cell death by inhibiting the PI3K/AKT signaling pathway and considerably lowered TNF-α, IL-6, and IL-1β release while increasing the production of IL-10. Studies have also shown that HT29 cells are popularly used in those studies involving adhesion and survival of microorganisms. Wang et al. have performed a similar analysis using the Lactobacillus strain. In that study, four different species and three Lactobacillus strains were utilized to study their adhesion to HT29 cells [39]. Barbosa et al. employed HT29 cells to study goniothalamin’s pro-apoptotic effects on these cells. The researchers discovered that goniothalamin induced apoptosis in HT29 cells, involving the generation of reactive oxygen species (ROS), the activation of MAPK, and caspases [40]. In a recent study on ulcerative colitis, Xiaotian et al. established the in vitro effectiveness of p-hydroxy benzaldehyde derived from a cyanobacterium, Nostoc commune. p-Hydroxy benzaldehyde increased mRNA expression in lipopolysaccharide-stimulated HT29 cells [41]. Another comparable recent work done by Balaji et al. on thymoquinone utilizing HT29 found that thymoquinone lowered pro-inflammatory chemokines such as CXCl-1 and COX-2 production in HT29 cells. The PPAR-γ activity was also investigated using HT29 cells, and it was observed that thymoquinone enhanced their expression [42]. In vitro models of IBD are increasingly being used in research on the involvement of TLR (toll-like receptor) in the IBD. Several researchers have used HT29 cell lines to conduct recent studies on TLR receptors [43–47].
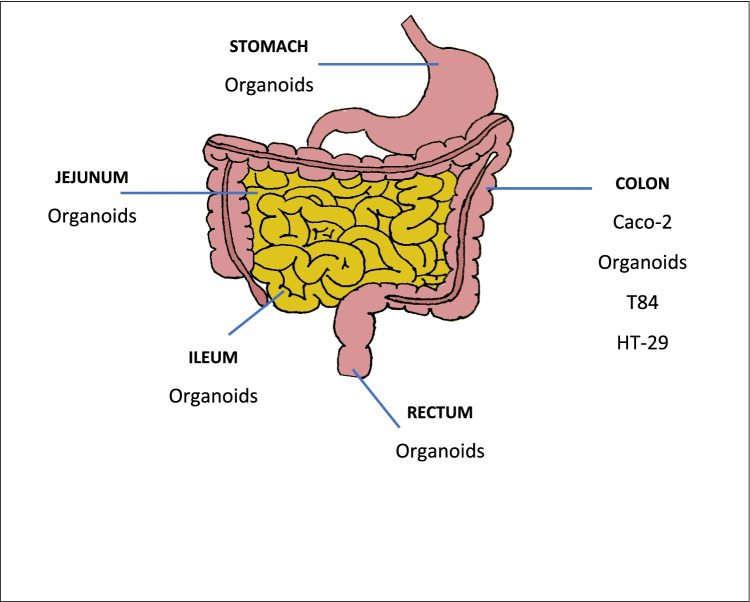
Organoids
Organoids are a type of cell produced from pluripotent or adult tissue stem cells. They are three-dimensional and can change into different kinds of cells to perform the functions of the relevant organs [48–50]. Scientists have been attempting to maintain tissue explants in vitro since 1992 [51, 52]. However, in 2008 and 2009, Eiraku et al. and Sato et al. established the first practical way of producing stem cell-derived structures, which are now known as “organoids” [53, 54]. Sato et al. developed them using Lgr5+ adult stem cells (ASCs), initially isolated from rodents and then human intestinal crypts [54]. Other anatomical regions, such as colonic, esophageal, and gastric tissues, have yielded good organoid cultures [55–57]. Colonoids are organoids that are formed from colonic tissue. Enteroids or small bowel organoids are organoids generated from small intestinal tissue [58]. They may be grown from a small volume of tissue, such as biopsies, and developed into mature enterocytes, tuft cells, goblet cells, and paneth cells [48, 59]. Many of the source tissue processes, including filtration, endocrine, and paracrine secretion molecular transport, contraction, and absorption, are likewise performed by gut organoids [48].
Even though they are inexpensive and may be created quickly, these organoids cannot recreate the complex environment of an organism [60]. Only one sort of cell may be manufactured. Cell types that are uncommon, such as tuft cells, are difficult to cultivate. Additionally, organoids cannot replicate the mucosal barrier or mucus production, and standardization protocol is not globally accepted [49]. Furthermore, because organoids are formed from malignant cells, they exhibit inherently distinct qualities from those of non-malignant cells, notably adhesion, cell polarity, and epithelial integrity, among other characteristics [61].
Because organoids may imitate the physiology of intestinal epithelial cells, they are great models for demonstrating IBD, as one of the critical features of IBD is abnormalities in epithelial cell activities. It is also feasible to co-culture gut organoids with non-epithelial cell lines such as macrophages and lymphocytes to better understand the intestinal mucosa [62, 63]. In addition to epithelial alterations, host-microbial interactions play an essential role in the pathogenesis of IBD. These organoids may imitate the gut’s microbial ecology, which can help researchers better understand the host-microbial connections that occur in IBD [64–66]. Organoids generated from an adult, and fetal mouse tissues have also been used to investigate the developmental expression profiles of parts of the innate immune system, such as NOD2, TLR4, and TLR5, in the laboratory [67]. Patients with active inflammatory bowel illness can be used to culture intestinal organoids [68–70]. When organoids were stimulated with particular inflammatory cytokines, specific biomarkers of inflammation were upregulated. In research done by Michael et al., interferon-gamma was employed to activate the human-derived organoid. The results revealed that E-cadherin was upregulated [71]. The NF-κB signaling pathway was activated in mouse colonic organoids subjected to chronic inflammatory stimuli, as demonstrated by Hibiya et al. [72]. Another recent study conducted by Verstockt et al. explored the influence of intestinal inflammation on viral intestine invasion mechanisms (SARS-CoV-2), especially ACE2, in IBD. The researchers found that intestinal inflammation changes SARS-CoV-2 coreceptors in the colon and ileum. In the ileum, HNF4A appears to be a critical upstream modulator of ACE2. At the same time, interferon transmission may be dominant in the colon [73]. Some researchers have also made efforts to use organoids produced from pediatric IBD patients to illustrate and understand the pathophysiology of IBD [74, 75].
Consequently, primary organoid cultures from damaged or inflamed tissue appear to be a suitable model for studying the epithelial and mucosal abnormalities in IBD.
Co-culture of Caco-2/HT29-MTX
The HT29 cell line was discussed in the earlier part of this review. According to preliminary findings, researchers have attempted to cultivate HT29 cells in the presence of methotrexate (MTX), according to preliminary results [76]. These were done to investigate if methotrexate affected the ability of HT29 cells to secrete mucus. The scientists discovered that exposing fast-growing HT29 cells to higher doses of MTX caused them to develop into mucus-secreting differentiated cells [76]. Since then, co-cultures of Caco-2 and HT29-MTX have been employed extensively in various research, including microbial adhesion, intestinal absorption, colonic permeability, and intestinal barrier integrity [77–80].
The stability and repeatability of the Caco-2 and HT29-MTX co-culture models are pretty close to that of the monocultures. During the 21-day polarization stage, the cells are cultured together. Between days 21 and 25, the co-cultures must be employed for experimentation [81]. Caco-2 cell lines are derived from absorptive cells in the intestine, whereas HT29-MTX cells are derived from goblet cells [82]. As previously noted, the Caco-2 cell line is of colonic origin. Still, when cultivated in culture, it exhibits traits of small intestine epithelium, such as the presence of a brush border, typical intestinal enzymes, and columnar absorptive cells. However, one significant drawback of the Caco-2 cell line is its inability to generate a mucus layer. Because HT29-MTX cells are derived from goblet cells, they can develop gel-forming MUC5 and membrane-bound MUC1. The co-cultivation of these two cell lines, Caco-2 and HT29-MTX, results in a model consisting of normal epithelium, goblet cells, and enterocytes when these two cell lines are grown together [82]. Walter et al. identified a strong relationship between the two factors in a study to measure the permeability of Caco-2/HT29 co-culture [83].
Caco-2 and HT29-MTX cells are cultured independently. Before seeding, the two cell cultures are combined. The most physiologically appropriate ratios (Caco-2/HT29-MTX) are from 90:10 and 75:25 [84]. This proportion provides the optimal compromise between model responsiveness and the occurrence of a mucus layer. The co-culture is maintained at 37 °C in a 5% concentration of carbon dioxide in Dulbecco’s Modified Eagle Medium (DMEM) containing 10% of heat-denatured juvenile bovine serum, 2 mM concentration of L-glutamine, 1% concentration of non-essential amino acids, and 100 U/ml concentration of penicillin along with 100 g/ml concentration of streptomycin. During 21 days, the culture media is replaced every 2–3 days.
Caco-2/HT29-MTX co-cultures are widely employed in research on IBD, colon cancer, and other disorders affecting intestinal barrier integrity or mucus layer adhesion abnormalities. Rasha et al. used Caco-2/HT29-MTX co-culture in recent work to investigate the pathophysiology of IBD. The study’s rationale was to look into using L-pNIPAM hydrogel to develop a 3D co-culture model under circumstances similar to inflammation [85]. Another recent work has shown that Caco-2/HT29-MTX co-culture may be used to explore the harmful effects of phycotoxins on the intestinal barrier. Reale et al. studied the toxicity of four phycotoxins on Caco-2/HT29-MTX co-cultured cells [86]. Other studies explore the use of Caco-2/HT29-MTX co-culture in colon cancer [87, 88]. The potential of different plants to stabilize barriers has also been investigated using co-cultures of Caco-2 and HT29-MTX cells [20]. Song et al. recently investigated the transcellular permeability of epigallocatechin-3-gallate using Caco-2 and HT29-MTX co-cultures [89].
Cell lines are a good choice since they are widely accessible and quickly produced in a lab setting, assuring excellent model system reproducibility. The system is simple to implement and successful in screening findings. These two cell lines do not generate some of the transporters or carriers found in average healthy epithelia; hence, the production of the necessary molecules should be established in the case of transport investigations. To create a homogenous mucin layer, the ratio of the two cell types is also critical. Even though cell lines are a viable alternative, they have stability and survival challenges.
T84 cell line
The T84 cell line is another often utilized cell line in the study of intestinal research. Murakami et al. developed it in 1980 to study the hormonal regulation of human colon cancer [90]. T84 cells contain microvilli on their surfaces, and when activated by transforming growth factors, they can develop into crypt-like cells [91].
T84 cells, like Caco-2 cells, can develop quickly into an absorptive stratum of epithelial cells. When T84 cells are stimulated by human transforming growth factors and/or mesenchymal factors, they can develop into crypt-like cells [92]. T84 cell lines are typically acceptable and effectively mimic the colon milieu, making them useful for host-microbe research in general [93].
T84 cell lines have been used to investigate mechanisms involving electrolyte transport [94], intestinal permeability [95, 96], and, most importantly, signaling pathways involved in the inflammatory response of the intestines [97, 98], making it one of the most widely used models in the study of inflammatory bowel disease [99–102]. Researchers have been employing these cells to better understand the complicated pathophysiology of inflammatory bowel disease since their discovery. Li et al. proposed that aberrant phosphorylation of colonic claudins might be linked to alterations in intestinal barrier function in a study that examined the influence of LPS on claudin phosphorylation in T84 colonic cells [103]. Manzini et al. used T84 cells in their research. They found that administering the energy drink to the cells lowered the release of the pro-inflammatory cytokines interleukin-6 and tumor necrosis factor-α [104]. Yueying et al. recently used T84 cells in a novel study. Their goal was to use cDNA microarray probe genomics to investigate the function of long coding RNAs in UC [105]. T84 cells can also be employed in studies involving a primary IBD pathophysiology [106–109].
T84 cell lines are one of the models used in research involving the colon. Still, they can also be utilized in general studies regarding inflammatory bowel disease. However, the T84 cell line, like Caco-2 and HT29 cell lines, has limitations. Because of its malignant origin and lack of epithelium-specific activity exhibited in vivo, the T84 cell line has drawbacks similar to Caco-2 and HT29 cell lines [92].
Intestinal-immunological cultures
Researchers created 2D co-cultures as gut inflammation models to improve simple cellular models. The interaction between intestinal and immune cells was used to create these models. Primary cells such as human peripheral blood mononuclear cells (PBMCs) [110] and macrophage cell lines from either human (THP-1) [111] or murine origin (RAW 246.7) are the principal immune cells employed to generate the various co-culture systems with intestinal cell lines.
PBMC
Human PBMCs are obtained from healthy donors’ or buffy coats’ peripheral blood and utilized to study the effects of dietary bioactive on immune cells. Dendritic cells, lymphocytes, and monocytes make up PBMC. These cells are stimulated by polyclonal activators, which cause them to release cytokines [112]. As a result, these cells are acceptable for IBD research involving immune responses [113–116]. Though PBMC is a convenient source of human immune cells, they have a fundamental drawback: phenotypic variations exist between immune cells and cells of the intestinal mucosa [112].
THP-1
THP-1 cell lines are human leukemia cell lines initially obtained from a patient with acute monocytic leukemia. Tsuchiya et al. were the first to create it in 1980 [117]. THP-1 cells are similar to primary monocytes and macrophages in terms of differentiation. They transform into macrophages after being exposed to PMA (phorbol-12-myristate-13-acetate) [118]. These cells may be maintained in vitro for approximately 3 months (passage 25) without loss of sensitivity or activity. This cell line has been used to research ROS generation and inflammation. It has been described as a model for immunological regulation [119, 120]. THP-1 cells have high reproducibility in studies and low variability of cellular phenotypes due to their homogeneous genetic background. THP-1 is more suited and efficient than PBMC cell lines due to this property [91]. Another benefit of THP-1 cells over other primary monocytes is that siRNA allows for easier down-regulation of the expression of particular proteins [121]. The most often utilized media for storing THP-1 cell lines is RPMI 160 medium [121]. THP-1 cell lines are now being used in inflammatory bowel disease research due to their high vitality, extended storage period, and ability to accurately simulate inflammation [122–126].
RAW 246.7
The RAW 246.7 cell line was obtained from a mouse tumor using the Abelson leukemia virus [127]. RAW 246.7 cell lines are frequently co-cultured with Caco-2 cells [128, 129]. In terms of pattern recognition receptors and reactivity to microbial ligands, including TLR, these cells have been demonstrated to imitate murine bone marrow-derived macrophages [130]. RAW 246.7 cells are often utilized in studies of intestinal inflammation [131–133]. Recent studies have also revealed that these cells are widely employed in inflammatory bowel disease research due to their capacity to accurately simulate the gut environment and their ability to successfully mimic TLRs, which play a key role in the pathogenesis of IBD [134–138]. One of the key pathologies implicated in IBD is the host-microbiome interactions. The RAW 246.7 cell lines have simulated host-microbiome interactions in studies [139–142]. Despite the widespread use of these cells in numerous fields of study, the authors concluded that when utilizing RAW 246.7 cells, caution should be exercised when interpreting the data due to alterations during continuous culture. Various cross-reactions should also be considered when merging human and mouse cells (e.g., co-culture of Caco-2/RAW 246.7) [143].
Ex vivo models
Ussing chamber
Hans Ussing, a Danish zoologist, invented the Ussing chamber in 1950. It was created to understand better the mechanics driving active transport in ex vivo intestinal tissue [144]. The usage of a Ussing chamber is commonly employed to evaluate ion transport in tissues such as the gut mucosa [145]. The discovery of the sodium-potassium ATPase pump was aided by the usage of this chamber [146].
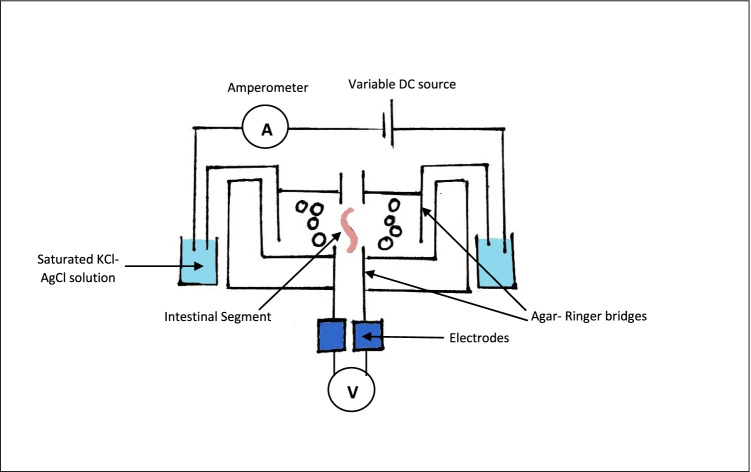
Typically, the Ussing chamber is divided into two compartments, separated by monolayers of cells between them. This chamber contains electrodes, and the voltages and short circuit currents measured by these electrodes may be used to determine the absorption and movement of ions through the epithelium (Figure 1) [147].
Fig. 1.
Ussing chamber
Clinical studies on rectal biopsies of patients with cystic fibrosis have demonstrated that ion transport function may be effectively assessed using the Ussing chamber [148]. Gut integrity and intestinal permeability investigations on mouse and human colon biopsies have also been published [149]. The use of the Ussing chamber also assisted the researchers in determining that in the instance of a human colon, the left colon had more permeability than the right colon [145]. The Ussing chamber’s usage is restricted to investigating intestinal permeability or intestinal barrier integrity. Still, it is also frequently used in the study of host-microbiome interaction, which is an essential factor in the etiology of IBD [150–153]. The first demonstration of enterotoxin from Shigella in rabbits occurred in 1975 when the Ussing chamber was used [154]. Bifico, a commercially available probiotic, was found to increase the epithelial barrier function of the colon in mice that had been deprived of the interleukin-10 (IL-10) cytokine [155]. Another research on the effects of Enterococcus faecalis was conducted in a Ussing chamber, and the results were positive. After doing their study concluded that bacterial translocation in the colon mucosa was caused by an aggregation product produced by Enterococcus faecalis [156]. Using the Ussing chamber, several modern studies have attempted to investigate the physiology of many receptors [157–160].
Although the Ussing chamber has numerous advantages, it also has a few limitations or drawbacks. Long-term experiments are impossible because the ex vivo tissue explants employed in the chamber are only viable for 5 h. Another downside of the chamber is its poor throughput and handling complexity [92].
Everted gut sac
Wilson and Wiseman initially established the everted gut sac model in 1950 to thoroughly understand the kinetics and mechanism of drug absorption [161]. Generally, the everted gut sac model is used to investigate gastrointestinal drug interactions, multidrug resistance, and drug pharmacokinetics and pharmacodynamics [162].
Figure 2 represents the everted gut sac system. The initial step in preparing the gut sac is to segment the chosen region of the intestine (duodenum, jejunum, ileum, or colon) and then evert the segments. The everted parts are then washed with a physiological solution over a glass rod. After that, the sac is filled with Kreb’s solution and transferred to a flask at 37 °Celsius [163].
Fig. 2.
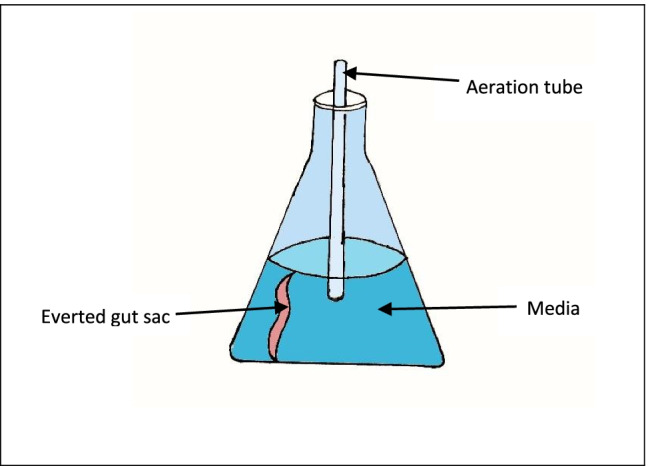
Representation of the everted gut sac system
Few early research employed the everted gut sac model to investigate p-glycoprotein function in rat intestines [164]. It was also utilized to investigate paracellular transport across the small intestine [165]. Since its development, the everted gut sac has been widely used to examine the intestinal permeability of various medications, and in the case of colitis research [166, 167]. Videla et al. conducted a similar trial with polyethylene glycol (PEG) on TNBS-induced colitis. They employed everted colonic sacs to investigate PEG’s intestinal permeability. Pretreatment with PEG resulted in a long-term decrease in epithelial permeability in everted colonic sacs [168]. Recent research on the targeted dual drug administration of 5-aminosalicylic acid and curcumin to inflamed colon has also used the everted gut sac [169].
Although the model closely reflects gastrointestinal tract environments, one of the model’s primary limitations is tissue survivability. Under typical settings, the tissue is only viable for 2 h. Another shortcoming of the system is its sensitivity; the system depends on various conditions. Furthermore, this model is not ideal for using the human intestine; instead, the rat intestine is employed, eliminating the intricacy of the human gut [162, 164].
Microfluidic gut-on-chip
Different in vitro and ex vivo models have previously been detailed in earlier sections of the paper. Still, their usage is limited owing to their drawbacks. For example, the ex vivo models (everted gut sac and Ussing chamber) have a restricted throughput. The in vitro models cannot replicate the intestine’s blood vessels and immune cells.
As a result, a few scientists created the microfluidic gut-on-chip in 2008 and 2009 to overcome the aforementioned restrictions and take in vitro research to the next level. The initial designs of microfluidic gut-on-chip devices were created using a silicon-based polymer, polydimethylsiloxane (PDMS), and had two chambers [170, 171]. In 2009, researchers attempted to change the original model significantly. Sung et al. and Kim et al. created a 3D hydrogel villi microfluidic device using calcium alginate and collagen. Their research indicated that growing Caco-2 cells on this device increased CYP3A4 enzymatic activity [172, 173].
Different organs-on-chip have also been designed based on where the organ is derived. A gut chip based on Caco-2 cells, a duodenum-intestinal chip, a colon-intestinal chip, and a jejunum-intestinal chip have been produced [174–176].
Since its development, the usage of microfluidic gut-on-chip technology in IBD research has been steadily rising over time. Beaurivage et al. used human intestinal cells and monocyte-derived macrophages on a gut-on-chip device to replicate the human intestine. This environment was shown to closely mimic the expression profile of the human colon in vivo. When the model was activated, IEC secreted polarized IL-8, CXCL10, and CCL-20 [177]. Another recent study found that direct interaction between DSS-sensitized mucosa and immune cells increases oxidative stress, with intestinal microbial stimulation eliciting inflammatory cytokines and immune cell recruitment [178]. One research found that the microfluidic technique of the gut-on-chip device may also be used to evaluate the efficacy of colon targeting of dietary fiber, according to the findings of a recent study [179]. Biopsy-derived organoids or induced pluripotent stem cells (iPSCs), which maintain their own diseased morphology ex vivo, are also employed to replicate the IBD phenotype on a microfluidic device [180]. One of the most complicated models of IBD on the chip was developed by Trapecar and colleagues. They built an IBD model that included primary liver and gut cells and circulating immune cells. They evaluated the influence of short-chain fatty acids (SCFAs) on IBD-related inflammation [181]. The microfluidic gut-on-chip is also employed in research to understand better the host-microbiome interaction, which is one of the factors implicated in the pathogenesis of IBD. Jalili-Firoozinezhad et al. have recently attempted to cultivate commensal anaerobic and aerobic bacteria on an intestine-on-chip to understand better the interactions between the host microbiome and the commensal bacteria [182]. Similar experiments employing a colon-on-a-chip technology to explore host-microbiota interactions have recently been described [183, 184].
Thus, microfluidic intestine-on-a-chip devices, which can more precisely imitate in vivo intestinal architecture and environment than standard in vitro culture methods, provide a fresh and more accurate way to study intestinal function and disease. Although the intestine-on-a-chip approach has its pros and cons, there are certain common obstacles. Because cell and organoid-based intestine-on-a-chip technologies lack varied cell types and associated tissue structures, they accurately depict the intestinal wall. Although some researchers have demonstrated that different cell types may be added to a system, their systems are still complex and labor-intensive. Another disadvantage is the chip substance, which can significantly influence drug response bioassays when intestine-on-a-chip models are employed. PDMS is capable of adsorbing a broad spectrum of compounds [185, 186].
Figure 3 depicts the region of origin of several in vitro and ex vivo models.
Fig. 3.
Region of origin of various in vitro and ex vivo models
Conclusion
Over the last few decades, numerous in vitro, in vivo animal models, and ex vivo models have been designed to understand IBD’s pathophysiology and etiology better. In vivo animal models cannot perfectly imitate the condition. Reliability is a challenge due to species differences between humans and animals. As a result, most contemporary research is conducted in cell culture or ex vivo settings. Cell cultures are highly desirable since they allow easy, immediate access to and assessment of tissues. Several models can imitate IBD, but each has its advantages and disadvantages. The review presents a clear understanding of the use of in vitro and ex vivo models of IBD along with their own set of advantages and limitations (Table 1); many of the systems are promising but do not perfectly replicate intestinal function. However, advancements in microfluidic gut-on-chip systems and organoids may provide solutions to those unanswered problems. Each model is distinctive; for example, PBMC, THP-1, or RAW 246.7 cells can be used for immune-related investigations. In crypt-related research, the T84 cell line would be chosen. Because each has its own set of drawbacks, no model is an ideal model for inflammatory bowel disease. As a result, a battery of models is advised to be employed for IBD research. Furthermore, an increased understanding of diverse in vitro and ex vivo models is required to answer outstanding IBD research problems.
Table 1.
Advantages and disadvantages of in vitro and ex vivo models of inflammatory bowel disease.
| Sr. no. | Models/systems | Advantages | Disadvantages |
|---|---|---|---|
| 1. | Caco-2 cell line |
Features identical to small bowel enterocytes (presence of brush-border microvilli) [16]. Produces specific digestive enzymes (e.g., peptidase and lactase) [16]. Ability to produce various cytokines Absorption-related studies are easy to perform |
Presence of other cells other than enterocytes in the epithelium [12]. Mucus and unstirred water are unable to be considered [12]. Various non-cellular factors hinder the study [12]. |
| 2. | HT29 cell line |
Cytokine release pattern similar to Caco-2 cells [34]. Higher mucin production [35]. Cell differentiation pattern similar to Caco-2 cells [33]. Produces typical digestive enzymes (e.g., peptidase and lactase) [33]. |
A longer time of differentiation [33]. High consumption of glucose [36]. Undifferentiated cells even when high glucose concentration is provided [36]. |
| 3. | Organoids |
Imitate physiology of intestinal cells [62, 63]. Co-culturing of gut organoids with non-epithelial cells is also possible. [62, 63] Imitate gut microbial ecology Investigation of innate immune systems possible [67]. Patient-derived organoids can be used |
Lacks specific cells/tissues [49]. Unable to recreate the complex environment of an organism [60]. Uncommon cell types (e.g., tuft cells) are difficult to cultivate [49]. Unable to replicate mucosal barrier [49]. |
| 4. | Caco-2/HT29-MTX co-culture |
Excellent for research involving microbial adhesion, colonic permeability, etc. [81]. Able to generate mucus membranes [82]. Stability and reproducibility similar to monocultures [82]. Increased mucin production [82]. |
Unable to generate some transporters [82]. Perfect ratio between Caco-2 and HT29 cells required for a homogenous mucin layer [82]. Cell viability is challenging [82]. |
| 5. | T84 cell lines | Development into crypt-like cells [92]. | Similar to Caco-2 and HT29 cells [92]. |
| 6. | Intestinal-immunological cultures | Appropriate for use of studying immune-related mechanisms. | Variations between immune cells and intestinal cells. |
| 7. | Ussing chamber |
Presence of two compartments [147]. Presence of electrodes to measure transport of ion [147]. Used to study intestinal permeability [149]. Used to study host-microbiome interactions [151]. Use of both animal and human tissue possible [149]. Physiology of receptors can easily be studied |
Cell viability up to 5 h only [92]. Since viability of cell is less, long-term studies not possible [92]. Poor throughput [92]. Complex handling [92]. |
| 8. | Everted gut sac |
Intestinal tissue is intact [92]. Mucus layer is present [92]. Presence of large surface area [92]. |
Not much relevant to human as it is ideal for rat tissue. System sensitivity depends on a number of factors. Tissue viability is 2 h only [164]. |
| 9. | Microfluidic gut-on-chip |
Location-based organ-on-chip can be developed Co-culturing of cells and macrophages possible [177]. Pluripotent stem cells can also be used [180]. |
Complex system [92]. PDMS used can itself adsorb compounds, hindering the research [185, 186]. High labor intensive [92]. |
Author contribution
The idea for the article, performance of the literature search, drafting, and revision of the work was done by AJ. Final approval for submission of the manuscript as given by AS and SA.
Declarations
Conflict of interest
The authors declare no competing interests.
References
- 1.Guan Q. A comprehensive review and update on the pathogenesis of inflammatory bowel disease. J Immunol Res. Hindawi. 2019;2019:e7247238. doi: 10.1155/2019/7247238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Head KA, Jurenka JS. Inflammatory bowel disease Part 1: ulcerative colitis—pathophysiology and conventional and alternative treatment options. Altern Med Rev. United States. 2003;8:247–283. [PubMed] [Google Scholar]
- 3.Head K, Jurenka JS. Inflammatory bowel disease Part II: Crohn’s disease—pathophysiology and conventional and alternative treatment options. Altern Med Rev United States. 2004;9:360–401. [PubMed] [Google Scholar]
- 4.Mak WY, Zhao M, Ng SC, Burisch J. The epidemiology of inflammatory bowel disease: east meets west. J Gastroenterol Hepatol. Australia. 2020;35:380–389. doi: 10.1111/jgh.14872. [DOI] [PubMed] [Google Scholar]
- 5.Zhao M, Burisch J. Impact of genes and the environment on the pathogenesis and disease course of inflammatory bowel disease. Dig Dis Sci. 2019;64:1759–1769. doi: 10.1007/s10620-019-05648-w. [DOI] [PubMed] [Google Scholar]
- 6.Yue B, Luo X, Yu Z, Mani S, Wang Z, Dou W. Inflammatory bowel disease a potential result from the collusion between gut microbiota and mucosal immune system. Microorganisms Multidiscip Digital Publish Inst. 2019;7:440. doi: 10.3390/microorganisms7100440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nguyen LH, Örtqvist AK, Cao Y, Simon TG, Roelstraete B, Song M, et al. Antibiotic use and the development of inflammatory bowel disease: a national case-control study in Sweden. lancet Gastroenterol Hepatol. Elsevier. 2020;5:986–995. doi: 10.1016/S2468-1253(20)30267-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicolaides S, Vasudevan A, Long T, Van Langenberg D. The impact of tobacco smoking on treatment choice and efficacy in inflammatory bowel disease. Intest Res Korean Assoc Stud Intest Dis. 2021;19:158. doi: 10.5217/ir.2020.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chiba M, Nakane K, Komatsu M. Westernized diet is the most ubiquitous environmental factor in inflammatory bowel disease. The Permanente Journal. Kaiser Permanente; 2019;23. [DOI] [PMC free article] [PubMed]
- 10.Goyal N, Rana A, Ahlawat A, Bijjem KRV, Kumar P. Animal models of inflammatory bowel disease: a review. Inflammopharmacology. Springer. 2014;22:219–233. doi: 10.1007/s10787-014-0207-y. [DOI] [PubMed] [Google Scholar]
- 11.Barone M, Chain F, Sokol H, Brigidi P, Bermúdez-Humarán LG, Langella P, et al. A versatile new model of chemically induced chronic colitis using an outbred murine strain. Frontiers in Microbiology [Internet]. 2018;9. Available from: https://www.frontiersin.org/article/10.3389/fmicb.2018.00565 [DOI] [PMC free article] [PubMed]
- 12.Lea T. Caco-2 Cell Line. In: Verhoeckx K, Cotter P, López-Expósito I, Kleiveland C, Lea T, Mackie A, et al., editors. The impact of food bioactives on health: in vitro and ex vivo models [Internet]. Cham: Springer International Publishing; 2015. p. 103–11. Available from: 10.1007/978-3-319-16104-4_10 [PubMed]
- 13.Fogh J, Fogh JM, Orfeo T. One hundred and twenty-seven cultured human tumor cell lines producing tumors in nude mice 23. JNCI J National Cancer Inst. 1977;59:221–6. doi: 10.1093/jnci/59.1.221. [DOI] [PubMed] [Google Scholar]
- 14.Hidalgo IJ, Raub TJ, Borchardt RT. Characterization of the human colon carcinoma cell line (Caco-2) as a model system for intestinal epithelial permeability. Gastroenterology. United States. 1989;96:736–749. [PubMed] [Google Scholar]
- 15.Kucki M, Diener L, Bohmer N, Hirsch C, Krug HF, Palermo V, et al. Uptake of label-free graphene oxide by Caco-2 cells is dependent on the cell differentiation status. J Nanobiotechnol. 2017;15:46. doi: 10.1186/s12951-017-0280-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lozoya-Agullo I, Araújo F, González-Álvarez I, Merino-Sanjuán M, González-Álvarez M, Bermejo M, et al. Usefulness of Caco-2/HT29-MTX and Caco-2/HT29-MTX/Raji B coculture models to predict intestinal and colonic permeability compared to Caco-2 monoculture. Mol Pharm. United States. 2017;14:1264–1270. doi: 10.1021/acs.molpharmaceut.6b01165. [DOI] [PubMed] [Google Scholar]
- 17.Primavera R, Palumbo P, Celia C, Cinque B, Carata E, Carafa M, et al. An insight of in vitro transport of PEGylated non-ionic surfactant vesicles (NSVs) across the intestinal polarized enterocyte monolayers. Eur J Pharm Biopharm. Netherlands. 2018;127:432–442. doi: 10.1016/j.ejpb.2018.03.013. [DOI] [PubMed] [Google Scholar]
- 18.Borgonetti V, Cocetta V, Biagi M, Carnevali I, Governa P, Montopoli M. Anti-inflammatory activity of a fixed combination of probiotics and herbal extract in an in vitro model of intestinal inflammation by stimulating Caco-2 cells with LPS-conditioned THP-1 cells medium. Minerva Pediatr. Italy; 2020 [DOI] [PubMed]
- 19.Andrews C, McLean MH, Durum SK. Cytokine tuning of intestinal epithelial function. Front Immunol. 2018;9:1270. doi: 10.3389/fimmu.2018.01270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weber L, Kuck K, Jürgenliemk G, Heilmann J, Lipowicz B, Vissiennon C. Anti-inflammatory and barrier-stabilising effects of myrrh, coffee charcoal and chamomile flower extract in a co-culture cell model of the intestinal mucosa. Biomolecules. 2020;10. [DOI] [PMC free article] [PubMed]
- 21.Lanevskij K, Didziapetris R. Physicochemical QSAR analysis of passive permeability across Caco-2 monolayers. J Pharm Sci. United States. 2019;108:78–86. doi: 10.1016/j.xphs.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 22.Jarc T, Novak M, Hevir N, Rižner TL, Kreft ME, Kristan K. Demonstrating suitability of the Caco-2 cell model for BCS-based biowaiver according to the recent FDA and ICH harmonised guidelines. J Pharm Pharmacol. England. 2019;71:1231–1242. doi: 10.1111/jphp.13111. [DOI] [PubMed] [Google Scholar]
- 23.Xu R, Zhu H, Hu L, Yu B, Zhan X, Yuan Y, et al. Characterization of the intestinal absorption of morroniside from Cornus officinalis Sieb. et Zucc via a Caco-2 cell monolayer model. PLoS One. 2020;15:e0227844. doi: 10.1371/journal.pone.0227844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akiyama Y, Matsumura N, Ono A, Hayashi S, Funaki S, Tamura N, et al. Prediction of oral drug absorption in rats from in vitro data. Pharm Res. United States; 2022; [DOI] [PubMed]
- 25.Dulbecco R, Freeman G. Plaque production by the polyoma virus. Virology. 1959;8:396–397. doi: 10.1016/0042-6822(59)90043-1. [DOI] [PubMed] [Google Scholar]
- 26.Maria-Ferreira D, Nascimento AM, Cipriani TR, Santana-Filho AP, da Watanabe P, de Mello GonçalesSant´Ana D, et al. Rhamnogalacturonan, a chemically-defined polysaccharide, improves intestinal barrier function in DSS-induced colitis in mice and human Caco-2 cells. Scientific Rep. 2018;8:12261. doi: 10.1038/s41598-018-30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chen Y, Wang J, Li J, Zhu J, Wang R, Xi Q, et al. Astragalus polysaccharide prevents ferroptosis in a murine model of experimental colitis and human Caco-2 cells via inhibiting NRF2/HO-1 pathway. Eur J Pharmacol. 2021;911:174518. doi: 10.1016/j.ejphar.2021.174518. [DOI] [PubMed] [Google Scholar]
- 28.Song X, Wen H, Zuo L, Geng Z, Nian J, Wang L, et al. Epac-2 ameliorates spontaneous colitis in Il-10−/− mice by protecting the intestinal barrier and suppressing NF-κB/MAPK signalling. Journal of Cellular and Molecular Medicine [Internet]. John Wiley & Sons, Ltd; 2021 [cited 2021 Dec 30];n/a. Available from: 10.1111/jcmm.17077 [DOI] [PMC free article] [PubMed]
- 29.Li C, Lun W, Zhao X, Lei S, Guo Y, Ma J, et al 2015 Allicin alleviates inflammation of trinitrobenzenesulfonic acid-induced rats and suppresses P38 and JNK pathways in Caco-2 cells. Agrawal A, editor. Mediators of Inflammation. Hindawi Publishing Corporation 2015:434692. [DOI] [PMC free article] [PubMed]
- 30.Liang Q, Ren X, Chalamaiah M, Ma H. Simulated gastrointestinal digests of corn protein hydrolysate alleviate inflammation in Caco-2 cells and a mouse model of colitis. J Food Sci Technol. 2020;57:2079–2088. doi: 10.1007/s13197-020-04242-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fogh J, Trempe G. New human tumor cell lines. Human tumor cells in vitro. Springer; 1975. p. 115–59.
- 32.Martínez-Maqueda D, Miralles B, Recio I, et al. HT29 cell line. In: Verhoeckx K, Cotter P, López-Expósito I, Kleiveland C, Lea T, Mackie A, et al., editors. The impact of food bioactives on health: in vitro and ex vivo models. Cham (CH): Springer; 2015. pp. 113–124. [PubMed] [Google Scholar]
- 33.Zweibaum A, Laburthe M, Grasset E, Louvard D. Use of cultured cell lines in studies of intestinal cell differentiation and function. Comprehensive physiology. Wiley Online Library; 2010;223–55.
- 34.Zhou G, Kong W-S, Li Z-C, Xie R-F, Yu T-Y, Zhou X. Effects of Qing Chang Suppository powder and its ingredients on IL-17 signal pathway in HT-29 cells and DSS-induced mice. Phytomed Germany. 2021;87:153573. doi: 10.1016/j.phymed.2021.153573. [DOI] [PubMed] [Google Scholar]
- 35.Adamczak MI, Hagesaether E, Smistad G, Hiorth M. An in vitro study of mucoadhesion and biocompatibility of polymer coated liposomes on HT29-MTX mucus-producing cells. Int J Pharm. Netherlands. 2016;498:225–233. doi: 10.1016/j.ijpharm.2015.12.030. [DOI] [PubMed] [Google Scholar]
- 36.Zweibaum A, Pinto M, Chevalier G, Dussaulx E, Triadou N, Lacroix B, et al. Enterocytic differentiation of a subpopulation of the human colon tumor cell line HT-29 selected for growth in sugar-free medium and its inhibition by glucose. J Cell Physiol. United States. 1985;122:21–29. doi: 10.1002/jcp.1041220105. [DOI] [PubMed] [Google Scholar]
- 37.Pinto M. Enterocyte-like differentiation and polarization of the human colon cancer cells by replacement of glucose by galactose in the medium. Biol Cell. 1983;44:193–196. [Google Scholar]
- 38.Rajendiran V, Natarajan V, Devaraj SN. Anti-inflammatory activity of Alpinia officinarum hance on rat colon inflammation and tissue damage in DSS induced acute and chronic colitis models. Food Sci Human Wellness. 2018;7:273–281. doi: 10.1016/j.fshw.2018.10.004. [DOI] [Google Scholar]
- 39.Wang G, Liu Y, Lu Z, Yang Y, Xia Y, Lai PFH, et al. The ameliorative effect of a Lactobacillus strain with good adhesion ability against dextran sulfate sodium-induced murine colitis. Food & Function. Royal Soc Chem. 2019;10:397–409. doi: 10.1039/c8fo01453a. [DOI] [PubMed] [Google Scholar]
- 40.Vendramini-Costa DB, Alcaide A, Pelizzaro-Rocha KJ, Talero E, Ávila-Román J, Garcia-Mauriño S, et al. Goniothalamin prevents the development of chemically induced and spontaneous colitis in rodents and induces apoptosis in the HT-29 human colon tumor cell line. Toxicol Appl Pharmacol. 2016;300:1–12. doi: 10.1016/j.taap.2016.03.009. [DOI] [PubMed] [Google Scholar]
- 41.Xu X, Wei C, Yang Y, Liu M, Luo A, Song H, et al. New discovery of anti-ulcerative colitis active ingredients of Nostoc commune: p-Hydroxy benzaldehyde. J Function Foods. 2021;77:104327. doi: 10.1016/j.jff.2020.104327. [DOI] [Google Scholar]
- 42.Venkataraman B, Almarzooqi S, Raj V, Alhassani AT, Alhassani AS, Ahmed KJ, et al. Thymoquinone, a dietary bioactive compound, exerts anti-inflammatory effects in colitis by stimulating expression of the colonic epithelial PPAR-γ transcription factor. Nutrients [Internet]. 2021;13. Available from: https://www.mdpi.com/2072-6643/13/4/1343 [DOI] [PMC free article] [PubMed]
- 43.Damoogh S, Vosough M, Hadifar S, Rasoli M, Gorjipour A, Falsafi S, et al. derived metabolites in modulating key mediator genes of the TLR signaling pathway. BMC Res Notes. 2021;14:156. doi: 10.1186/s13104-021-05568-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Park YS, Kim SW, Cheon JH. P041 Melatonin controls microbiota in colitis through toll-like receptor 4 signalling. J Crohn’s Colitis. 2020;14:S153–4. doi: 10.1093/ecco-jcc/jjz203.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jin B-R, Chung K-S, Hwang S, Hwang SN, Rhee K-J, Lee M, et al. Rosmarinic acid represses colitis-associated colon cancer: a pivotal involvement of the TLR4-mediated NF-κB-STAT3 axis. Neoplasia. 2021;23:561–573. doi: 10.1016/j.neo.2021.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Park G-B, Jeong J-Y, Kim D. Modified TLR-mediated downregulation of miR-125b-5p enhances CD248 (endosialin)-induced metastasis and drug resistance in colorectal cancer cells. Mol Carcinog. 2020;59:154–167. doi: 10.1002/mc.23137. [DOI] [PubMed] [Google Scholar]
- 47.Sugitani Y, Nishida A, Inatomi O, Ohno M, Imai T, Kawahara M, et al. Sodium absorption stimulator prostasin (PRSS8) has an anti-inflammatory effect via downregulation of TLR4 signaling in inflammatory bowel disease. J Gastroenterol. 2020;55:408–417. doi: 10.1007/s00535-019-01660-z. [DOI] [PubMed] [Google Scholar]
- 48.O’Connell L, Winter DC, Aherne CM. The role of organoids as a novel platform for modeling of inflammatory bowel disease. Frontiers in Pediatrics [Internet]. 2021;9. Available from: https://www.frontiersin.org/article/10.3389/fped.2021.624045 [DOI] [PMC free article] [PubMed]
- 49.Kim J, Koo B-K, Knoblich JA. Human organoids: model systems for human biology and medicine. Nat Rev Mol Cell Biol. 2020;21:571–584. doi: 10.1038/s41580-020-0259-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kar SK, Wells JM, Ellen ED, te Pas MFW, Madsen O, Groenen MAM, et al. Organoids: a promising new in vitro platform in livestock and veterinary research. Vet Res. 2021;52:43. doi: 10.1186/s13567-021-00904-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fukamachi H. Proliferation and differentiation of fetal rat intestinal epithelial cells in primary serum-free culture. Journal of cell science. Company of Biologists The Company of Biologists, Bidder Building, 140 Cowley …; 1992;103:511–9. [DOI] [PubMed]
- 52.Evans GS, Flint N, Somers AS, Eyden B, Potten CS. The development of a method for the preparation of rat intestinal epithelial cell primary cultures. Journal of cell science. Company of Biologists The Company of Biologists, Bidder Building, 140 Cowley …; 1992;101:219–31. [DOI] [PubMed]
- 53.Eiraku M, Watanabe K, Matsuo-Takasaki M, Kawada M, Yonemura S, Matsumura M, et al. Self-organized formation of polarized cortical tissues from ESCs and its active manipulation by extrinsic signals. Cell Stem Cell. 2008;3:519–532. doi: 10.1016/j.stem.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 54.Sato T, Vries RG, Snippert HJ, van de Wetering M, Barker N, Stange DE, et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262–265. doi: 10.1038/nature07935. [DOI] [PubMed] [Google Scholar]
- 55.Múnera JO, Sundaram N, Rankin SA, Hill D, Watson C, Mahe M, et al. Differentiation of human pluripotent stem cells into colonic organoids via transient activation of BMP signaling. Cell Stem Cell. 2017;21:51–64.e6. doi: 10.1016/j.stem.2017.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li X, Francies H, Miremadi A, Grantham A, Grehan N, Devonshire G, et al. Su2042—derivation of oesophageal organoids to recapitulate the heterogeneity of primary tumours and provide a model system for precision therapeutics. Gastroenterology. 2019;156:S-696.
- 57.Dotti I, Salas A. Potential use of human stem cell–derived intestinal organoids to study inflammatory bowel diseases. Inflamm Bowel Dis Oxford Univ Press US. 2018;24:2501–9. doi: 10.1093/ibd/izy275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zachos NC, Kovbasnjuk O, Foulke-Abel J, In J, Blutt SE, de Jonge HR, et al. Human enteroids/colonoids and intestinal organoids functionally recapitulate normal intestinal physiology and pathophysiology. J Biol Chem. 2016;291:3759–3766. doi: 10.1074/jbc.R114.635995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Takahashi T, Fujishima K, Kengaku M. Modeling intestinal stem cell function with organoids. Int J Mol Sci. 2021;22. [DOI] [PMC free article] [PubMed]
- 60.O’Connell L, Winter DC. Organoids: past learning and future directions. Stem Cells Dev. United States. 2020;29:281–289. doi: 10.1089/scd.2019.0227. [DOI] [PubMed] [Google Scholar]
- 61.Goldhammer N, Kim J, Timmermans-Wielenga V, Petersen OW. Characterization of organoid cultured human breast cancer. Breast Cancer Res. 2019;21:141. doi: 10.1186/s13058-019-1233-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nozaki K, Mochizuki W, Matsumoto Y, Matsumoto T, Fukuda M, Mizutani T, et al. Co-culture with intestinal epithelial organoids allows efficient expansion and motility analysis of intraepithelial lymphocytes. J Gastroenterol. 2016;51:206–213. doi: 10.1007/s00535-016-1170-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Noel G, Baetz NW, Staab JF, Donowitz M, Kovbasnjuk O, Pasetti MF, et al. A primary human macrophage-enteroid co-culture model to investigate mucosal gut physiology and host-pathogen interactions. Sci Rep. 2017;7:45270. doi: 10.1038/srep45270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Poletti M, Arnauts K, Ferrante M, Korcsmaros T. Organoid-based models to study the role of host-microbiota interactions in IBD. J Crohns Colitis. 2021;15:1222–1235. doi: 10.1093/ecco-jcc/jjaa257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bartfeld S. Modeling infectious diseases and host-microbe interactions in gastrointestinal organoids. Dev Biol. 2016;420:262–270. doi: 10.1016/j.ydbio.2016.09.014. [DOI] [PubMed] [Google Scholar]
- 66.Dutta D, Clevers H. Organoid culture systems to study host–pathogen interactions. Curr Opin Immunol. 2017;48:15–22. doi: 10.1016/j.coi.2017.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kayisoglu O, Weiss F, Niklas C, Pierotti I, Pompaiah M, Wallaschek N, et al. Location-specific cell identity rather than exposure to GI microbiota defines many innate immune signalling cascades in the gut epithelium. Gut. 2021;70:687–697. doi: 10.1136/gutjnl-2019-319919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ojo BA, VanDussen KL, Rosen MJ. The promise of patient-derived colon organoids to model ulcerative colitis. Inflammatory Bowel Diseases. 2021;izab161. [DOI] [PMC free article] [PubMed]
- 69.Lee C, Hong S-N, Kim E-R, Chang D-K, Kim Y-H. Epithelial regeneration ability of Crohn’s disease assessed using patient-derived intestinal organoids. Int J Mol Sci Multidiscip Dig Publish Inst. 2021;22:6013. doi: 10.3390/ijms22116013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Varani J, McClintock SD, Aslam MN. Organoid culture to study epithelial cell differentiation and barrier formation in the colon: bridging the gap between monolayer cell culture and human subject research. In Vitro Cellular & Developmental Biology-Animal. Springer; 2021;1–17. [DOI] [PMC free article] [PubMed]
- 71.Workman MJ, Troisi E, Targan SR, Svendsen CN, Barrett RJ. Modeling intestinal epithelial response to interferon-γ in induced pluripotent stem cell-derived human intestinal organoids. Int J Mol Sci Multidiscip Dig Publish Inst. 2021;22:288. doi: 10.3390/ijms22010288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hibiya S, Tsuchiya K, Hayashi R, Fukushima K, Horita N, Watanabe S, et al. Long-term inflammation transforms intestinal epithelial cells of colonic organoids. J Crohns Colitis. England. 2017;11:621–630. doi: 10.1093/ecco-jcc/jjw186. [DOI] [PubMed] [Google Scholar]
- 73.Verstockt B, Verstockt S, Abdu Rahiman S, Ke B-J, Arnauts K, Cleynen I, et al. Intestinal receptor of SARS-CoV-2 in inflamed IBD tissue seems downregulated by HNF4A in ileum and upregulated by interferon regulating factors in colon. J Crohns Colitis. 2021;15:485–498. doi: 10.1093/ecco-jcc/jjaa185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Howell KJ, Kraiczy J, Nayak KM, Gasparetto M, Ross A, Lee C, et al. DNA methylation and transcription patterns in intestinal epithelial cells from pediatric patients with inflammatory bowel diseases differentiate disease subtypes and associate with outcome. Gastroenterology. 2018;154:585–598. doi: 10.1053/j.gastro.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Niklinska-Schirtz BJ, Venkateswaran S, Anbazhagan M, Kolachala VL, Prince J, Dodd A, et al. Ileal derived organoids from Crohn’s disease patients show unique transcriptomic and secretomic signatures. medRxiv. Cold Spring Harbor Laboratory Press; 2021; [DOI] [PMC free article] [PubMed]
- 76.Lesuffleur T, Barbat A, Dussaulx E, Zweibaum A. Growth adaptation to methotrexate of HT-29 human colon carcinoma cells is associated with their ability to differentiate into columnar absorptive and mucus-secreting cells. Cancer Res. United States. 1990;50:6334–6343. [PubMed] [Google Scholar]
- 77.Krausova G, Hynstova I, Svejstil R, Mrvikova I, Kadlec R. Identification of synbiotics conducive to probiotics adherence to intestinal mucosa using an in vitro Caco-2 and HT29-MTX cell model. Processes [Internet]. 2021;9. Available from: https://www.mdpi.com/2227-9717/9/4/569
- 78.Wu C, Gao Y, Li S, Huang X, Bao X, Wang J, et al. Modulation of intestinal epithelial permeability and mucin mRNA (MUC2, MUC5AC, and MUC5B) expression and protein secretion in Caco-2/HT29-MTX co-cultures exposed to aflatoxin M1, ochratoxin A, and zearalenone individually or collectively. Toxicol Lett. 2019;309:1–9. doi: 10.1016/j.toxlet.2019.03.010. [DOI] [PubMed] [Google Scholar]
- 79.Barnett AM, Roy NC, Cookson AL, McNabb WC. Metabolism of caprine milk carbohydrates by probiotic bacteria and Caco-2: HT29–MTX epithelial co-cultures and their impact on intestinal barrier integrity. Nutrients Multidiscip Dig Publish Inst. 2018;10:949. doi: 10.3390/nu10070949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cai Y, Liu L, Xia M, Tian C, Wu W, Dong B, et al. SEDDS facilitate cinnamaldehyde crossing the mucus barrier: the perspective of mucus and Caco-2/HT29 co-culture models. International Journal of Pharmaceutics. Elsevier; 2022;121461 [DOI] [PubMed]
- 81.Pan F, Han L, Zhang Y, Yu Y, Liu J. Optimization of Caco-2 and HT29 co-culture in vitro cell models for permeability studies. International Journal of Food Sciences and Nutrition. 2015;66. [DOI] [PubMed]
- 82.Kleiveland CR. Co-cultivation of Caco-2 and HT-29MTX. In: Verhoeckx K, Cotter P, López-Expósito I, Kleiveland C, Lea T, Mackie A, et al., editors. The impact of food bioactives on health: in vitro and ex vivo models [Internet]. Cham: Springer International Publishing; 2015. p. 135–40. Available from: 10.1007/978-3-319-16104-4_13
- 83.Walter E, Janich S, Roessler BJ, Hilfinger JM, Amidon GL. HT29-MTX/Caco-2 co-cultures as an in vitro model for the intestinal epithelium: in vitro–in vivo correlation with permeability data from rats and humans. J Pharmaceutic Sci. Elsevier. 1996;85:1070–1076. doi: 10.1021/js960110x. [DOI] [PubMed] [Google Scholar]
- 84.Mahler GJ, Shuler ML, Glahn RP. Characterization of Caco-2 and HT29-MTX co-cultures in an in vitro digestion/cell culture model used to predict iron bioavailability. J Nutr Biochem. United States. 2009;20:494–502. doi: 10.1016/j.jnutbio.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 85.Dosh RH, Jordan-Mahy N, Sammon C, Le Maitre CL. Long-term in vitro 3D hydrogel co-culture model of inflammatory bowel disease. Sci Rep. 2019;9:1812. doi: 10.1038/s41598-019-38524-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Reale O, Huguet A, Fessard V. Co-culture model of Caco-2/HT29-MTX cells: a promising tool for investigation of phycotoxins toxicity on the intestinal barrier. Chemosphere. 2021;273:128497. doi: 10.1016/j.chemosphere.2020.128497. [DOI] [PubMed] [Google Scholar]
- 87.Berger E, Nassra M, Atgié C, Plaisancié P, Géloën A. Oleic acid uptake reveals the rescued enterocyte phenotype of colon cancer Caco-2 by HT29-MTX cells in co-culture mode. International Journal of Molecular Sciences [Internet]. 2017;18. Available from: https://www.mdpi.com/1422-0067/18/7/1573 [DOI] [PMC free article] [PubMed]
- 88.Castiaux V, Laloux L, Schneider Y-J, Mahillon J. Screening of cytotoxic B. cereus on differentiated Caco-2 cells and in co-culture with mucus-secreting (HT29-MTX) cells. Toxins. 2016;8. [DOI] [PMC free article] [PubMed]
- 89.Song H, He A, Guan X, Chen Z, Bao Y, Huang K. Fabrication of chitosan-coated epigallocatechin-3-gallate (EGCG)-hordein nanoparticles and their transcellular permeability in Caco-2/HT29 co-cultures. Int J Biol Macromol. 2022;196:144–150. doi: 10.1016/j.ijbiomac.2021.12.024. [DOI] [PubMed] [Google Scholar]
- 90.Murakami H, Masui H. Hormonal control of human colon carcinoma cell growth in serum-free medium. Proceed Natl Acad Sci Proceed Natl Acad Sci. 1980;77:3464–8. doi: 10.1073/pnas.77.6.3464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Del Carmen Ponce de León-Rodríguez M, Guyot JP, Laurent-Babot C. Intestinal in vitro cell culture models and their potential to study the effect of food components on intestinal inflammation null. Taylor & Francis. 2019;59:3648–66. doi: 10.1080/10408398.2018.1506734. [DOI] [PubMed] [Google Scholar]
- 92.Rahman S, Ghiboub M, Donkers JM, van de Steeg E, van Tol EAF, Hakvoort TBM, et al. The progress of intestinal epithelial models from cell lines to gut-on-chip. Int J Mol Sci. 2021;22. [DOI] [PMC free article] [PubMed]
- 93.Devriese S, Van den Bossche L, Van Welden S, Holvoet T, Pinheiro I, Hindryckx P, et al. T84 monolayers are superior to Caco-2 as a model system of colonocytes. Histochem Cell Biol. Germany. 2017;148:85–93. doi: 10.1007/s00418-017-1539-7. [DOI] [PubMed] [Google Scholar]
- 94.Sawasvirojwong S, Kittayaruksakul S. Constitutive androstane receptor inhibits Ca2+-dependent Cl− secretion in intestinal epithelial cells. J Physiol. 2019;32:47–52. [Google Scholar]
- 95.Jennis M, Cavanaugh CR, Leo GC, Mabus JR, Lenhard J, Hornby PJ. Microbiota-derived tryptophan indoles increase after gastric bypass surgery and reduce intestinal permeability in vitro and in vivo. Neurogastroenterol Motility Wiley Online Library. 2018;30:e13178. doi: 10.1111/nmo.13178. [DOI] [PubMed] [Google Scholar]
- 96.Franco YL, Da Silva L, Cristofoletti R. Navigating through cell-based in vitro models available for prediction of intestinal permeability and metabolism: are we ready for 3D? AAPS J. 2021;24:2. doi: 10.1208/s12248-021-00665-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wongkrasant P, Pongkorpsakol P, Ariyadamrongkwan J, Meesomboon R, Satitsri S, Pichyangkura R, et al. A prebiotic fructo-oligosaccharide promotes tight junction assembly in intestinal epithelial cells via an AMPK-dependent pathway. Biomedicine & Pharmacotherapy. 2020;129:110415. doi: 10.1016/j.biopha.2020.110415. [DOI] [PubMed] [Google Scholar]
- 98.Yin A, Sun Y. Downregulation of HSF2 inhibits inflammation in human intestinal epithelial cells by regulating IL-6/STAT3 signaling pathway. International Journal of Clinical and Experimental Medicine. E-Century Publishing Corp 40 White Oaks LN, Madison, WI 53711 USA; 2020;13:1068–74.
- 99.Ohno M, Imai T, Chatani M, Nishida A, Inatomi O, Kawahara M, et al. The anti-inflammatory and protective role of interleukin-38 in inflammatory bowel disease. J Clin Biochem Nutri Soc Radical Res Japan. 2022;70:64. doi: 10.3164/jcbn.21-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hall CHT, Lee JS, Murphy EM, Gerich ME, Dran R, Glover LE, et al. Creatine transporter, reduced in colon tissues from patients with inflammatory bowel diseases, regulates energy balance in intestinal epithelial cells, epithelial integrity, and barrier function. Gastroenterology. 2020;159:984–998.e1. doi: 10.1053/j.gastro.2020.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Guo Z, Cai X, Guo X, Xu Y, Gong J, Li Y, et al. Let-7b ameliorates Crohn’s disease-associated adherent-invasive E. coli induced intestinal inflammation via modulating toll-like receptor 4 expression in intestinal epithelial cells. Biochem Pharmacol. 2018;156:196–203. doi: 10.1016/j.bcp.2018.08.029. [DOI] [PubMed] [Google Scholar]
- 102.Soroosh A, Rankin CR, Polytarchou C, Lokhandwala ZA, Patel A, Chang L, et al. miR-24 is elevated in ulcerative colitis patients and regulates intestinal epithelial barrier function. Am J Pathol. 2019;189:1763–1774. doi: 10.1016/j.ajpath.2019.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Li J, Li Y-X, Chen M-H, Li J, Du J, Shen B, et al 2015 Changes in the phosphorylation of claudins during the course of experimental colitis. Int J Clin Exp Pathol. e-Century Publishing Corporation 8:12225–33. [PMC free article] [PubMed]
- 104.Manzini R, Schwarzfischer M, Bircher A, Niechcial A, Vavricka SR, Atrott K, et al. Energy drink administration ameliorates intestinal epithelial barrier defects and reduces acute DSS colitis. Inflamm Bowel Dis. 2021;27:1139–1152. doi: 10.1093/ibd/izaa328. [DOI] [PubMed] [Google Scholar]
- 105.Chen Y, Li H, Lai L, Huang Y, Shen J. Discovery of new long noncoding RNAs associated with ulcerative colitis with a novel general microarray expression data. Life Sciences. 2021;287:120090. [DOI] [PubMed]
- 106.Beterams A, De Paepe K, Maes L, Wise IJ, De Keersmaecker H, Rajkovic A, et al. Versatile human in vitro triple co-culture model coincubated with adhered gut microbes reproducibly mimics pro-inflammatory host-microbe interactions in the colon. The FASEB Journal. 2021;35:e21992. [DOI] [PubMed]
- 107.Grosheva I, Zheng D, Levy M, Polansky O, Lichtenstein A, Golani O, et al. High-throughput screen identifies host and microbiota regulators of intestinal barrier function. Gastroenterology. 2020;159:1807–1823. doi: 10.1053/j.gastro.2020.07.003. [DOI] [PubMed] [Google Scholar]
- 108.Alexeev EE, Lanis JM, Kao DJ, Campbell EL, Kelly CJ, Battista KD, et al. Microbiota-derived indole metabolites promote human and murine intestinal homeostasis through regulation of interleukin-10 receptor. Am J Pathol. 2018;188:1183–1194. doi: 10.1016/j.ajpath.2018.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ghyselinck J, Verstrepen L, Moens F, Abbeele PV den, Said J, Smith B, et al. A 4-strain probiotic supplement influences gut microbiota composition and gut wall function in patients with ulcerative colitis. International Journal of Pharmaceutics. 2020;587:119648. [DOI] [PubMed]
- 110.Jessen B, Rodriguez-Sillke Y, Sonnenberg E, Schumann M, Kruglov A, Freise I, et al. Level of tumor necrosis factor production by stimulated blood mononuclear cells can be used to predict response of patients with inflammatory bowel diseases to infliximab. Clin Gastroenterol Hepatol. 2021;19:721–731.e1. doi: 10.1016/j.cgh.2020.03.066. [DOI] [PubMed] [Google Scholar]
- 111.Kaur H, Erickson A, Moreau R. Divergent regulation of inflammatory cytokines by mTORC1 in THP-1–derived macrophages and intestinal epithelial Caco-2 cells. Life Sciences. 2021;284:119920. [DOI] [PubMed]
- 112.Kleiveland CR. Peripheral Blood Mononuclear Cells. In: Verhoeckx K, Cotter P, López-Expósito I, Kleiveland C, Lea T, Mackie A, et al., editors. The impact of food bioactives on health: in vitro and ex vivo models [Internet]. Cham: Springer International Publishing; 2015. p. 161–7. Available from: 10.1007/978-3-319-16104-4_15 [PubMed]
- 113.Yoshimura T, Mitsuyama K, Sakemi R, Takedatsu H, Yoshioka S, Kuwaki K, et al. Evaluation of serum leucine-rich alpha-2 glycoprotein as a new inflammatory biomarker of inflammatory bowel disease. Fröde TS, editor. Mediators of Inflammation. Hindawi; 2021;2021:8825374. [DOI] [PMC free article] [PubMed]
- 114.Morita T, Mitsuyama K, Yamasaki H, Mori A, Yoshimura T, Araki T, et al. Gene expression of transient receptor potential channels in peripheral blood mononuclear cells of inflammatory bowel disease patients. Journal of Clinical Medicine [Internet]. 2020;9. Available from: https://www.mdpi.com/2077-0383/9/8/2643 [DOI] [PMC free article] [PubMed]
- 115.Ye Y-L, Yin J, Hu T, Zhang L-P, Wu L-Y, Pang Z. Increased circulating circular RNA_103516 is a novel biomarker for inflammatory bowel disease in adult patients. World J Gastroenterol. Baishideng Publishing Group Inc; 2019;25:6273–88. [DOI] [PMC free article] [PubMed]
- 116.Ju JK, Cho Y-N, Park K-J, Kwak HD, Jin H-M, Park S-Y, et al. Activation, deficiency, and reduced IFN-γ production of mucosal-associated invariant T cells in patients with inflammatory bowel disease. J Innate Immun. 2020;12:422–434. doi: 10.1159/000507931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Tsuchiya S, Yamabe M, Yamaguchi Y, Kobayashi Y, Konno T, Tada K. Establishment and characterization of a human acute monocytic leukemia cell line (THP-1) Int J Cancer. United States. 1980;26:171–176. doi: 10.1002/ijc.2910260208. [DOI] [PubMed] [Google Scholar]
- 118.Baxter EW, Graham AE, Re NA, Carr IM, Robinson JI, Mackie SL, et al. Standardized protocols for differentiation of THP-1 cells to macrophages with distinct M(IFNγ+LPS), M(IL-4) and M(IL-10) phenotypes. Journal of Immunological Methods. 2020;478:112721. [DOI] [PubMed]
- 119.Cong L, Gao Z, Zheng Y, Ye T, Wang Z, Wang P, et al. Electrical stimulation inhibits Val-boroPro-induced pyroptosis in THP-1 macrophages via sirtuin3 activation to promote autophagy and inhibit ROS generation. Aging (Albany NY). 2020;12:6415–6435. doi: 10.18632/aging.103038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Li H, Wang Y, Song Y. MicroRNA-26b inhibits the immune response to Mycobacterium tuberculosis (M.tb) infection in THP-1 cells via targeting TGFβ-activated kinase-1 (TAK1), a promoter of the NF-κB pathway. Int J Clin Exp Pathol. 2018;11:1218–27. [PMC free article] [PubMed]
- 121.Chanput W, Mes JJ, Wichers HJ. THP-1 cell line: an in vitro cell model for immune modulation approach. Int Immunopharmacol. 2014;23:37–45. doi: 10.1016/j.intimp.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 122.Wang T, Liu W, Li C, Si G, Liang Z, Yin J. Mist1 promoted inflammation in colitis model via K+-ATPase NLRP3 inflammasome by SNAI1. Pathology - Research and Practice. 2021;224:153511. [DOI] [PubMed]
- 123.Li Q, cheng H, Liu Y, Wang X, He F, Tang L. Activation of mTORC1 by LSECtin in macrophages directs intestinal repair in inflammatory bowel disease. Cell Death & Disease. 2020;11:918. [DOI] [PMC free article] [PubMed]
- 124.Zhang ZZ, Zhang Y, He T, Sweeney CL, Baris S, Karakoc-Aydiner E, et al. Homozygous IL37 mutation associated with infantile inflammatory bowel disease. Proceedings of the National Academy of Sciences. 2021;118:e2009217118. [DOI] [PMC free article] [PubMed]
- 125.Trefzer R, Elpeleg O, Gabrusskaya T, Stepensky P, Mor-Shaked H, Grosse R, et al. Characterization of a L136P mutation in Formin-like 2 (FMNL2) from a patient with chronic inflammatory bowel disease. PLOS ONE. Public Library of Science. 2021;16:1–17. doi: 10.1371/journal.pone.0252428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Park HJ, Kim J, Saima FT, Rhee K-J, Hwang S, Kim MY, et al. Adipose-derived stem cells ameliorate colitis by suppression of inflammasome formation and regulation of M1-macrophage population through prostaglandin E2. Biochem Biophys Res Commun. 2018;498:988–995. doi: 10.1016/j.bbrc.2018.03.096. [DOI] [PubMed] [Google Scholar]
- 127.Raschke WC, Baird S, Ralph P, Nakoinz I. Functional macrophage cell lines transformed by Abelson leukemia virus. Cell. United States. 1978;15:261–267. doi: 10.1016/0092-8674(78)90101-0. [DOI] [PubMed] [Google Scholar]
- 128.Aly E, López-Nicolás R, Darwish AA, Ros-Berruezo G, Frontela-Saseta C. In vitro effectiveness of recombinant human lactoferrin and its hydrolysate in alleviating LPS-induced inflammatory response. Food Res Int. 2019;118:101–107. doi: 10.1016/j.foodres.2017.12.029. [DOI] [PubMed] [Google Scholar]
- 129.Liu H, Ye H, Sun C, Xi H, Ma J, Lai F, et al. Antioxidant activity in HepG2 cells, immunomodulatory effects in RAW 264.7 cells and absorption characteristics in Caco-2 cells of the peptide fraction isolated from Dendrobium aphyllum. International Journal of Food Science & Technology. 2018;53:2027–36. doi: 10.1111/ijfs.13783. [DOI] [Google Scholar]
- 130.Zhang X, Wang S, Cai Y, He W, Yang Q, Li C. Regulatory mechanism of microRNA-9 / long non-coding RNA XIST expression on mouse macrophage RAW264.7 apoptosis induced by oxidized low density lipoprotein. Bioengineered Taylor & Francis. 2022;13:3537–50. doi: 10.1080/21655979.2021.2018978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gao R, Shu W, Shen Y, Sun Q, Bai F, Wang J, et al. Sturgeon protein-derived peptides exert anti-inflammatory effects in LPS-stimulated RAW2647 macrophages via the MAPK pathway. J Function Foods. 2020;72:104044. doi: 10.1016/j.jff.2020.104044. [DOI] [Google Scholar]
- 132.Cheng C, Zou Y, Peng J. Oregano essential oil attenuates RAW264.7 cells from lipopolysaccharide-induced inflammatory response through regulating NADPH oxidase activation-driven oxidative stress. Molecules [Internet]. 2018;23. Available from: https://www.mdpi.com/1420-3049/23/8/1857 [DOI] [PMC free article] [PubMed]
- 133.Wang H, Zhang L, Xu S, Pan J, Zhang Q, Lu R. Surface-layer protein from Lactobacillus acidophilus NCFM inhibits lipopolysaccharide-induced inflammation through MAPK and NF-κB signaling pathways in RAW2647 cells. J Agric Food Chem Am Chem Soc. 2018;66:7655–62. doi: 10.1021/acs.jafc.8b02012. [DOI] [PubMed] [Google Scholar]
- 134.Zhen D, Xuan T, Hu B, Bai X, Fu D, Wang Y, et al. Pteryxin attenuates LPS-induced inflammatory responses and inhibits NLRP3 inflammasome activation in RAW264.7 cells. Journal of Ethnopharmacology. 2022;284:114753. doi: 10.1016/j.jep.2021.114753. [DOI] [PubMed] [Google Scholar]
- 135.Krajewska JB, Długosz O, Sałaga M, Banach M, Fichna J. Silver nanoparticles based on blackcurrant extract show potent anti-inflammatory effect in vitro and in DSS-induced colitis in mice. Int J Pharm. 2020;585:119549. doi: 10.1016/j.ijpharm.2020.119549. [DOI] [PubMed] [Google Scholar]
- 136.Yokota Y, Shikano A, Kuda T, Takei M, Takahashi H, Kimura B. Lactobacillus plantarum AN1 cells increase caecal L reuteri in an ICR mouse model of dextran sodium sulphate-induced inflammatory bowel disease. Int Immunopharmacol. 2018;56:119–27. doi: 10.1016/j.intimp.2018.01.020. [DOI] [PubMed] [Google Scholar]
- 137.Lin W-C, Pan W-Y, Liu C-K, Huang W-X, Song H-L, Chang K-S, et al. In situ self-spray coating system that can uniformly disperse a poorly water-soluble H2S donor on the colorectal surface to treat inflammatory bowel diseases. Biomaterials. 2018;182:289–298. doi: 10.1016/j.biomaterials.2018.07.044. [DOI] [PubMed] [Google Scholar]
- 138.Kim Y, Lim HJ, Jang H-J, Lee S, Jung K, Lee SW, et al. Portulaca oleracea extracts and their active compounds ameliorate inflammatory bowel diseases in vitro and in vivo by modulating TNF-α, IL-6 and IL-1β signalling. Food Res Int. 2018;106:335–343. doi: 10.1016/j.foodres.2017.12.058. [DOI] [PubMed] [Google Scholar]
- 139.Qu L, Lin X, Liu C, Ke C, Zhou Z, Xu K, et al. Atractylodin attenuates dextran sulfate sodium-induced colitis by alleviating gut microbiota dysbiosis and inhibiting inflammatory response through the MAPK pathway. Front Pharmacol. 2021;12:665376. doi: 10.3389/fphar.2021.665376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Shibayama J, Kuda T, Shikano A, Fukunaga M, Takahashi H, Kimura B, et al. Effects of rice bran and fermented rice bran suspensions on caecal microbiota in dextran sodium sulphate-induced inflammatory bowel disease model mice. Food Biosci. 2018;25:8–14. doi: 10.1016/j.fbio.2018.07.002. [DOI] [Google Scholar]
- 141.Tang X, Wang W, Hong G, Duan C, Zhu S, Tian Y, et al. Gut microbiota-mediated lysophosphatidylcholine generation promotes colitis in intestinal epithelium-specific Fut2 deficiency. J Biomed Sci. 2021;28:20. doi: 10.1186/s12929-021-00711-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Li H, Christman LM, Li R, Gu L. Synergic interactions between polyphenols and gut microbiota in mitigating inflammatory bowel diseases. Food Funct Royal Soc Chem. 2020;11:4878–91. doi: 10.1039/D0FO00713G. [DOI] [PubMed] [Google Scholar]
- 143.Berghaus LJ, Moore JN, Hurley DJ, Vandenplas ML, Fortes BP, Wolfert MA, et al. Innate immune responses of primary murine macrophage-lineage cells and RAW 2647 cells to ligands of toll-like receptors 2, 3, and 4. Comp Immunol Microbiol Infect Dis. 2010;33:443–54. doi: 10.1016/j.cimid.2009.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ussing HH, Zerahn K. Active transport of sodium as the source of electric current in the short-circuited isolated frog skin. Acta Physiol Scand. 1951;23:110–127. doi: 10.1111/j.1748-1716.1951.tb00800.x. [DOI] [PubMed] [Google Scholar]
- 145.Thomson A, Smart K, Somerville MS, Lauder SN, Appanna G, Horwood J, et al. The Ussing chamber system for measuring intestinal permeability in health and disease. BMC Gastroenterol. 2019;19:98. doi: 10.1186/s12876-019-1002-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Skou JC. The identification of the sodium pump. Bioscience reports. Portland Press Ltd. 1998;18:155–169. doi: 10.1023/A:1020196612909. [DOI] [PubMed] [Google Scholar]
- 147.Michiba K, Maeda K, Kurimori K, Enomoto T, Shimomura O, Takeuchi T, et al. Characterization of the human intestinal drug transport with Ussing chamber system incorporating freshly isolated human jejunum. Drug Metabol Disposition Am Soc Pharmacol Exp Therapeutics. 2021;49:84–93. doi: 10.1124/dmd.120.000138. [DOI] [PubMed] [Google Scholar]
- 148.Silva IAL, Duarte A, Marson FAL, Centeio R, Doušová T, Kunzelmann K, et al. Assessment of distinct electrophysiological parameters in rectal biopsies for the choice of the best diagnosis/prognosis biomarkers for cystic fibrosis. Front Physiol. 2020;11:604580. doi: 10.3389/fphys.2020.604580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Fart F, Salihović S, McGlinchey A, Gareau MG, Orešič M, Halfvarson J, et al. Perfluoroalkyl substances are increased in patients with late-onset ulcerative colitis and induce intestinal barrier defects ex vivo in murine intestinal tissue null. Taylor & Francis. 2021;56:1286–95. doi: 10.1080/00365521.2021.1961306. [DOI] [PubMed] [Google Scholar]
- 150.Lomasney KW, Hyland NP. The application of Ussing chambers for determining the impact of microbes and probiotics on intestinal ion transport. Can J Physiol Pharmacol NRC Res Press. 2013;91:663–70. doi: 10.1139/cjpp-2013-0027. [DOI] [PubMed] [Google Scholar]
- 151.Bhattarai Y, Williams BB, Battaglioli EJ, Whitaker WR, Till L, Grover M, et al. Gut microbiota-produced tryptamine activates an epithelial G-protein-coupled receptor to increase colonic secretion. Cell Host Microbe. 2018;23:775–785.e5. doi: 10.1016/j.chom.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Rude KM, Pusceddu MM, Keogh CE, Sladek JA, Rabasa G, Miller EN, et al. Developmental exposure to polychlorinated biphenyls (PCBs) in the maternal diet causes host-microbe defects in weanling offspring mice. Environmental Pollution. Elsevier. 2019;253:708–721. doi: 10.1016/j.envpol.2019.07.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Libertucci J, Dutta U, Kaur S, Jury J, Rossi L, Fontes ME, et al. Inflammation-related differences in mucosa-associated microbiota and intestinal barrier function in colonic Crohn’s disease. American Journal of Physiology-Gastrointestinal and Liver Physiology. American Physiological Society Bethesda, MD; 2018;315:G420–31. [DOI] [PubMed]
- 154.Donowitz M, Keusch GT, Binder HJ. Effect of Shigella enterotoxin on electrolyte transport in rabbit ileum. Gastroenterol. United States. 1975;69:1230–1237. [PubMed] [Google Scholar]
- 155.Shi C-Z, Chen H-Q, Liang Y, Xia Y, Yang Y-Z, Yang J, et al. Combined probiotic bacteria promotes intestinal epithelial barrier function in interleukin-10-gene-deficient mice. World J Gastroenterol. 2014;20:4636–4647. doi: 10.3748/wjg.v20.i16.4636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Isenmann R, Schwarz M, Rozdzinski E, Marre R, Beger HG. Aggregation substance promotes colonic mucosal invasion of Enterococcus faecalis in an ex vivo model. J Surg Res. United States. 2000;89:132–138. doi: 10.1006/jsre.1999.5813. [DOI] [PubMed] [Google Scholar]
- 157.Kato S, Sato T, Fujita H, Kawatani M, Yamada Y. Effects of GLP-1 receptor agonist on changes in the gut bacterium and the underlying mechanisms. Scientific Rep. Nature Publishing Group. 2021;11:1–13. doi: 10.1038/s41598-021-88612-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Peiris M, Aktar R, Reed D, Cibert-Goton V, Zdanaviciene A, Halder W, et al. Decoy bypass for appetite suppression in obese adults: role of synergistic nutrient sensing receptors GPR84 and FFAR4 on colonic endocrine cells. Gut: BMJ Publishing Group; 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Al-Sadi R, Nighot P, Nighot M, Haque M, Rawat M, Ma TY. Lactobacillus acidophilus induces a strain-specific and toll-like receptor 2–dependent enhancement of intestinal epithelial tight junction barrier and protection against intestinal inflammation. Am J Pathol. Elsevier. 2021;191:872–884. doi: 10.1016/j.ajpath.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Feddersen UR, Hendel SK, Berner-Hansen MA, Jepps TA, Bindslev N, Berner-Hansen M. Nanomolar EP4 receptor potency and expression of eicosanoid-related enzymes in normal appearing colonic mucosa from patients with colorectal neoplasia. 2021 [DOI] [PMC free article] [PubMed]
- 161.Wilson TH, Wiseman G. The use of sacs of everted small intestine for the study of the transference of substances from the mucosal to the serosal surface. J Physiol. 1954;123:116–125. doi: 10.1113/jphysiol.1954.sp005036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Fang Y, Cao W, Xia M, Pan S, Xu X. Transport and interactions of co-incubated bi-functional flavonoids through inhibiting the function of P-glycoprotein (P-gp) using KB/multidrug-resistant (MDR) cells and rat everted gut sacs. J Agric Food Chem Am Chem Soc. 2022;70:1923–33. doi: 10.1021/acs.jafc.1c07694. [DOI] [PubMed] [Google Scholar]
- 163.Ranjan R, Sawal Rk, Ranjan A, Patil Nv. Comparison of calcium absorption from nano- and micro-sized calcium salts using everted gut sac technique [Internet]. 2019th-03–22nd ed. The Indian Journal of Animal Sciences. 2019. Available from: https://epubs.icar.org.in/ejournal/index.php/IJAnS/article/view/88101
- 164.Yaghoobian M, Haeri A, Bolourchian N, Shahhosseini S, Dadashzadeh S. An investigation into the role of P-glycoprotein in the intestinal absorption of repaglinide: assessed by everted gut sac and Caco-2 cell line. Iran J Pharm Res. 2019;18:102–110. [PMC free article] [PubMed] [Google Scholar]
- 165.Surampalli G, Nanjwade BK, Patil PA. Safety evaluation of naringenin upon experimental exposure on rat gastrointestinal epithelium for novel optimal drug delivery. Drug Deliv. England. 2016;23:512–524. doi: 10.3109/10717544.2014.923957. [DOI] [PubMed] [Google Scholar]
- 166.He R, Xu Y, Peng J, Ma T, Li J, Gong M. The effects of 18β-glycyrrhetinic acid and glycyrrhizin on intestinal absorption of paeoniflorin using the everted rat gut sac model. J Nat Med. 2017;71:198–207. doi: 10.1007/s11418-016-1049-2. [DOI] [PubMed] [Google Scholar]
- 167.AU - Mateer SW, AU - Cardona J, AU - Marks E, AU - Goggin BJ, AU - Hua S, AU - Keely S. Ex vivo intestinal sacs to assess mucosal permeability in models of gastrointestinal disease. JoVE. MyJoVE Corp; 2016;e53250. [DOI] [PMC free article] [PubMed]
- 168.Videla S, Lugea A, Vilaseca J, Guarner F, Treserra F, Salas A, et al. Polyethylene glycol enhances colonic barrier function and ameliorates experimental colitis in rats. Int J Colorectal Dis. 2007;22:571–580. doi: 10.1007/s00384-006-0232-4. [DOI] [PubMed] [Google Scholar]
- 169.Duan H, Lü S, Gao C, Bai X, Qin H, Wei Y, et al. Mucoadhesive microparticulates based on polysaccharide for target dual drug delivery of 5-aminosalicylic acid and curcumin to inflamed colon. Colloids Surf, B. 2016;145:510–519. doi: 10.1016/j.colsurfb.2016.05.038. [DOI] [PubMed] [Google Scholar]
- 170.Kimura H, Yamamoto T, Sakai H, Sakai Y, Fujii T. An integrated microfluidic system for long-term perfusion culture and on-line monitoring of intestinal tissue models. Lab Chip. England. 2008;8:741–746. doi: 10.1039/b717091b. [DOI] [PubMed] [Google Scholar]
- 171.Imura Y, Asano Y, Sato K, Yoshimura E. A microfluidic system to evaluate intestinal absorption. Anal Sci. Japan. 2009;25:1403–1407. doi: 10.2116/analsci.25.1403. [DOI] [PubMed] [Google Scholar]
- 172.Sung JH, Yu J, Luo D, Shuler ML, March JC. Microscale 3-D hydrogel scaffold for biomimetic gastrointestinal (GI) tract model. Lab Chip Royal Soc Chem. 2011;11:389–92. doi: 10.1039/C0LC00273A. [DOI] [PubMed] [Google Scholar]
- 173.Kim SH, Lee JW, Choi I, Kim Y-C, Lee JB, Sung JH. A microfluidic device with 3-D hydrogel villi scaffold to simulate intestinal absorption. J Nanosci Nanotechnol. 2013;13:7220–7228. doi: 10.1166/jnn.2013.8088. [DOI] [PubMed] [Google Scholar]
- 174.Kasendra M, Tovaglieri A, Sontheimer-Phelps A, Jalili-Firoozinezhad S, Bein A, Chalkiadaki A, et al. Development of a primary human small intestine-on-a-chip using biopsy-derived organoids. Sci Rep. 2018;8:2871. doi: 10.1038/s41598-018-21201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Apostolou A, Panchakshari RA, Banerjee A, Manatakis DV, Paraskevopoulou MD, Luc R, et al. A Micro-engineered human colon intestine-chip platform to study leaky barrier. bioRxiv. 2020;2020.08.28.271759.
- 176.Yin J, Sunuwar L, Kasendra M, Yu H, Tse C-M, Talbot CCJ, et al. Fluid shear stress enhances differentiation of jejunal human enteroids in intestine-chip. Am J Physiol Gastrointest Liver Physiol. 2021;320:G258–G271. doi: 10.1152/ajpgi.00282.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Beaurivage C, Kanapeckaite A, Loomans C, Erdmann KS, Stallen J, Janssen RAJ. Development of a human primary gut-on-a-chip to model inflammatory processes. Sci Rep. 2020;10:21475. doi: 10.1038/s41598-020-78359-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Shin W, Kim HJ. Intestinal barrier dysfunction orchestrates the onset of inflammatory host–microbiome cross-talk in a human gut inflammation-on-a-chip. Proceed Natl Acad Sci Natl Acad Sci. 2018;115:10539–47. doi: 10.1073/pnas.1810819115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Ren Y, Xu A, Tang Q, Yuan X. Dietary fiber-derived microparticles from microfluidic for drug delivery in treating inflammatory bowel disease. Mater Express. 2021;11:452–460. [Google Scholar]
- 180.Shin YC, Shin W, Koh D, Wu A, Ambrosini YM, Min S, et al. Three-dimensional regeneration of patient-derived intestinal organoid epithelium in a physiodynamic mucosal interface-on-a-chip. Micromachines [Internet]. 2020;11. Available from: https://www.mdpi.com/2072-666X/11/7/663 [DOI] [PMC free article] [PubMed]
- 181.Trapecar M, Communal C, Velazquez J, Maass CA, Huang Y-J, Schneider K, et al. Gut-liver physiomimetics reveal paradoxical modulation of IBD-related inflammation by short-chain fatty acids. Cell Systems. Elsevier. 2020;10:223–239.e9. doi: 10.1016/j.cels.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Jalili-Firoozinezhad S, Gazzaniga FS, Calamari EL, Camacho DM, Fadel CW, Bein A, et al. A complex human gut microbiome cultured in an anaerobic intestine-on-a-chip. Nature Biomed Eng. 2019;3:520–531. doi: 10.1038/s41551-019-0397-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Gazzaniga FS, Camacho DM, Wu M, Silva Palazzo MF, Dinis ALM, Grafton FN, et al. Harnessing colon chip technology to identify commensal bacteria that promote host tolerance to infection. Frontiers in Cellular and Infection Microbiology [Internet]. 2021;11. Available from: https://www.frontiersin.org/article/10.3389/fcimb.2021.638014 [DOI] [PMC free article] [PubMed]
- 184.Ryan FJ, Ahern AM, Fitzgerald RS, Laserna-Mendieta EJ, Power EM, Clooney AG, et al. Colonic microbiota is associated with inflammation and host epigenomic alterations in inflammatory bowel disease. Nat Commun. 2020;11:1512. doi: 10.1038/s41467-020-15342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Toepke MW, Beebe DJ. PDMS absorption of small molecules and consequences in microfluidic applications. Lab on a chip Royal Soc Chem. 2006;6:1484–6. doi: 10.1039/b612140c. [DOI] [PubMed] [Google Scholar]
- 186.Wang JD, Douville NJ, Takayama S, ElSayed M. Quantitative analysis of molecular absorption into PDMS microfluidic channels. Ann Biomed Eng. Springer. 2012;40:1862–1873. doi: 10.1007/s10439-012-0562-z. [DOI] [PubMed] [Google Scholar]