Abstract
Acute exposure to air pollution is associated with an increasing risk of death and cardiovascular disorders. Nonetheless, the impact of chronic exposure to air pollution on the circulatory system is still debated. Here, we review the links of chronic exposure to outdoor air pollution with mortality and most common cardiovascular diseases, in particular during the coronavirus disease 2019 event (COVID-19). We found that recent studies provide robust evidence for a causal effect of chronic exposure to air pollution and cardiovascular mortality. In terms of mortality, the strongest relationship was noted for fine particulate matter, nitrogen dioxide, and ozone. There is also increasing evidence showing that exposure to air pollution, mainly fine particulate matter and nitrogen dioxide, is associated with the development of atherosclerosis, hypertension, stroke, and heart failure. However, available scientific evidence is not strong enough to support associations with cardiac arrhythmias and coagulation disturbances. Noteworthy, for some pollutants, the risk of negative health effects is high for concentrations lower than the limit values recommended by the European Union and Word Health Organization. Efforts to diminish exposure to air pollution and to design optimal methods of air pollution reduction should be urgently intensified and supported by effective legislation and interdisciplinary cooperation.
Keywords: Air pollution, Chronic exposure, Mortality, Coronary artery disease, Hypertension, Stroke
Introduction
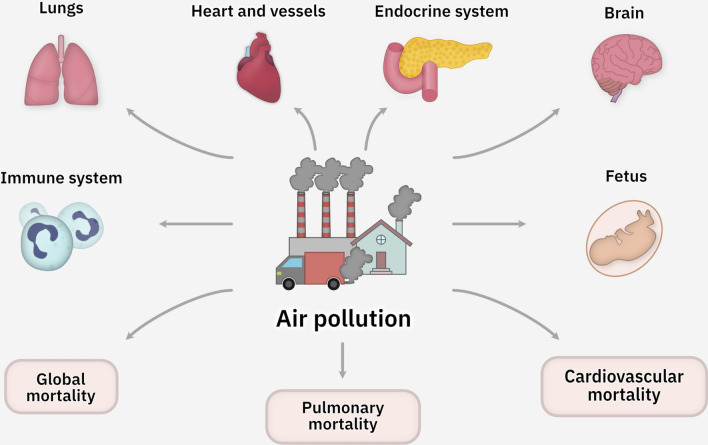
Most cardiovascular diseases have a multifactorial etiopathogenesis combining genetic predisposition, aging, lifestyle, infections, and environmental factors. There is growing evidence that air pollution not only exacerbates the course of cardiovascular diseases, but also contributes to their development. In addition to cardiovascular complications, air pollution has been implicated in a broad spectrum of other clinical entities, with previous studies reporting links with an increased incidence of respiratory diseases, malignancies, immune dysfunction, endocrine and neurodegenerative disorders, and fetal complications (Almetwally et al 2020). In particular, humans with known cardiovascular disease, diabetes, patients with pulmonary disorders, the elderly, and pregnant women are vulnerable to the harmful effects of air pollution (Franklin et al 2015).
Furthermore, air pollution is known to increase all-cause and cardiovascular mortality. While the actual number of deaths due to pollutants is difficult to assess, the World Health Organization estimates that at least 7 million premature deaths per year can be attributed to the adverse effects of both outdoor ambient and indoor air pollution (World Health Organization 2020). The vast majority of these deaths are caused by cardiovascular complications (World Health Organization 2020) (Fig. 1).
Fig. 1.
Adverse effects of air pollution on human health
The cardiovascular response to air pollution is modulated by the chemical composition of the pollutants as well as exposure concentration, duration of exposure, comorbidities, individual vulnerability, and changes in atmospheric conditions such as humidity, temperature, and ambient pressure. Moreover, the chemical composition of air pollutants significantly varies by emission source (Konduracka 2019). Importantly, not all air pollutants are being monitored. In fact, there are countless potential pollutants, and new chemicals are constantly emerging as a result of interactions between the existing ones. Therefore, most pollutants have never been assessed for their toxicity and risk to human health (Briggs 2003; Konduracka 2019).
Air pollutants are composed of gaseous components and particulate matter. The most commonly monitored chemicals among gaseous pollutants are nitrogen oxides (i.e., nitric oxide and nitrogen dioxide), sulfur dioxide, carbon monoxide, benzene, and ozone. On the other hand, particulate matter components consist of elemental and organic carbon particles, transition metals, sulfates, nitrates, polycyclic aromatic hydrocarbons, furans, alkanes, alkenes, dioxins, microbes, lipopolysaccharides (endotoxins), and other chemicals (Brook et al. 2010; Newby et al. 2015; Samek et al. 2020). Previous studies have shown that combustion processes and traffic are among the largest sources of air pollution emissions in the world.
This narrative review focuses on the most common cardiovascular diseases that are related to chronic exposure to outdoor air pollution in the adult population. It also discusses the potential mechanisms underlying the observed associations between long-term exposure to air pollutants and clinical outcomes. The article is an abridged version of the chapter published by Konduracka and Rostoff (2021) in the series “Environmental Chemistry for a Sustainable World 65”.
Mechanisms of chronic outdoor exposure to air pollution on the cardiovascular system
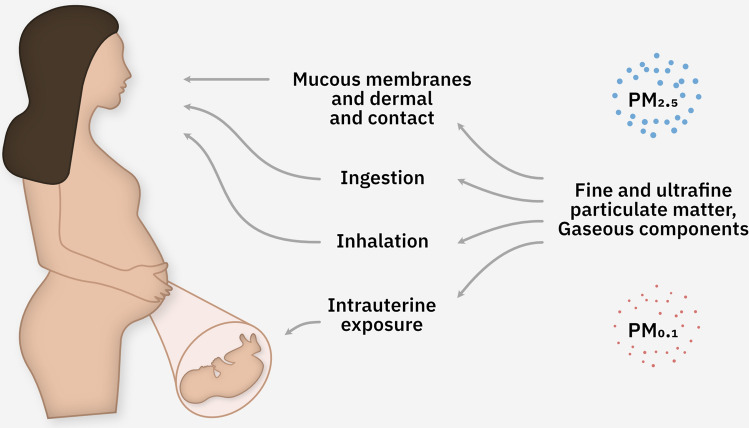
The direct route of exposure to air pollutants is through the respiratory system and eye conjunctiva (Briggs 2003; Brook et al. 2010; De Brouwere et al. 2012; Chin 2015). The gastrointestinal tract may also be involved, although the exact proportion of contaminants that enter the body by this route has not yet been identified (Briggs 2003; Brook et al. 2010; De Brouwere et al. 2012; Chin 2015). Some air pollutants can pass from the air into the water, soil, plants, and animals, thus getting into the human body with food, where they may accumulate and affect the cardiovascular system. The main routes of human exposure to air pollution are shown in Fig. 2.
Fig. 2.
Main routes of human exposure to air pollution. PM2.5: fine inhalable particle matter, with diameter generally 2.5 micrometers and smaller
Although the exact mechanisms of the effects of air pollutants on the cardiovascular system through the respiratory tract are still under investigation, it is currently accepted that a potential mechanism is related to the ability of fine particulate matter (PM2.5, aerodynamic diameter < 2.5 μm), ultrafine particulate matter (aerodynamic diameter ≤ 0.1 μm), and some gaseous chemicals to penetrate from the lungs into the bloodstream (Brook et al. 2010; Newby et al. 2015; Chin 2015). Ultrafine particulate matter is particularly hazardous to health because of its large reactive surface area, greater ability to bind harmful chemicals, very high deposition in the alveoli, its potential to activate inflammatory cells which can enter the bloodstream, and its accumulation in peripheral organs (Ohlwein et al. 2019). Importantly, the ultrafine particulate matter concentration is not routinely measured by all air-quality monitoring stations in the world. Furthermore, air pollutants include also other chemicals that are not routinely evaluated (e.g., endotoxins) and that may interact with particulate matter and gaseous components, making it difficult to assess health effects (Rajagopalan et al. 2018; Miller and Newby 2020).
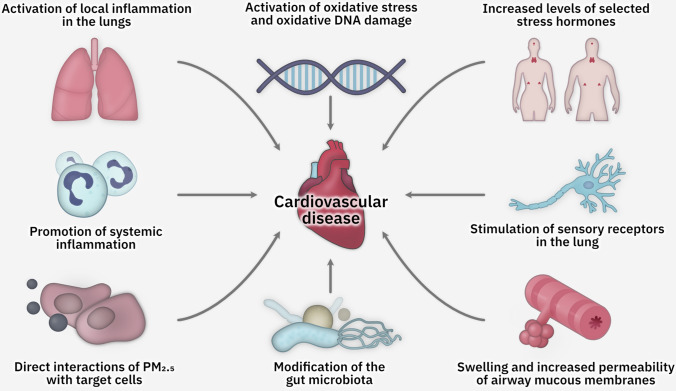
Based on experimental animal and human studies as well as epidemiological studies, the following pathomechanisms are postulated to underlie the unfavorable effects of air pollution on the cardiovascular system:
Activation of local inflammatory responses in the lungs by particulate matter and gaseous pollutants, resulting in cytokine-mediated systemic inflammation (Ghio et al. 2000; Terzano et al. 2010; Brook et al. 2010; Newby et al. 2015; Jiang et al. 2016; Lopez-Campos et al. 2016).
Promotion of systemic inflammation by fine particulate matter and certain gaseous chemicals that can penetrate from the lungs into the bloodstream and activate inflammation, endothelial dysfunction, prothrombotic state, and thrombosis (Brook et al. 2010; Rich et al. 2012; Newby et al. 2015; Hamanaka and Mutlu 2018).
Stimulation of sensory receptors in the lungs, which leads to an imbalance of the autonomic nervous system and predominant sympathetic activation, resulting in vasoconstriction and heart rhythm disturbances. However, there are substantial inconsistencies between studies in terms of the variables analyzed and the results obtained (Brook et al. 2010; Barbosa et al. 2012; Rich et al. 2012; Newby et al. 2015; Buteau and Goldberg 2016; Hamanaka and Mutlu 2018).
Activation of oxidative stress, formation of reactive oxygen species in cells and tissues, and oxidative DNA damage (Sun et al. 2005; Vinzents et al. 2005; Novotna et al. 2007; Rossner Jr et al. 2007; Ha et al. 2007; Araujo et al. 2008; Bai et al. 2011; Min et al. 2011; Lind and Lind 2012; Li et al. 2019).
Direct interactions of fine particulate matter with target cells and tissues (e.g., vessel wall and cardiac tissues), although this pathomechanism remains controversial (Hamanaka and Mutlu 2018).
Elevated levels of selected stress hormones (including epinephrine, norepinephrine, and cortisol) and increased insulin resistance (Li et al. 2017).
Modification of gut microbiota composition, which may promote inflammation, atherosclerosis, and metabolic disorders such as obesity, metabolic syndrome, and diabetes (Zhang et al. 2015; Wang et al. 2018).
Swelling and increased permeability of the respiratory mucosa, which facilitating the penetration of potential cardiotropic micro-organisms into the body.
Figure 3 shows the postulated pathomechanisms underlying the adverse cardiovascular effects of air pollution.
Fig. 3.
Postulated pathomechanisms underlying the adverse cardiovascular effects of air pollution
All of these mechanisms are considered to potentially contribute to the development and progression of atherosclerosis, heart failure, arterial hypertension, stroke, and cardiac arrhythmias, ultimately leading to death. The analysis of the available studies indicates mainly the cardiovascular consequences of exposure to air pollution.
Long-term exposure to air pollution and mortality
Strong epidemiological evidence from available cohort studies conducted primarily in Europe, the USA, and Canada supports the conclusion that there is a causal relationship between long-term exposure to fine particulate matter and all-cause mortality as well as cardiovascular mortality (ISA ES EPA 2019; U.S. EPA. Supplement EPA 2021).
Reevaluation results of the American Cancer Society and Harvard Six 23 Cities cohorts as well as new cohorts consisting of Medicare participants revealed additional evidence of 25 positive associations between long-term PM2.5 exposure and total mortality in areas with annual average concentrations below 20 µg/m3 and, in some cases, below 12 µg/m3 (Pope III et al. 2004; ISA ES EPA 2019). Positive relationships were observed regardless of the exposure assignment with ambient monitors or using modeled or remote sensing data or combination of this methods. Other studies have conducted analyses to examine the impact of confounding pollutants and revealed the relatively unchanged positive associations between long-term PM2.5 exposure and total mortality, particularly for O3, with fewer studies examining NO2 and PM2.5 (2019 PM ISA).
Among the numerous cohort studies, it is worth mentioning the results of the multicenter European study of cohorts of air pollution effects (ESCAPE), a 13-nation project involving 367,251 participants, which demonstrated an increased hazard ratio for all-cause mortality of 1.07 (95% confidence interval, 1.02–1.13) for every 5 μg/m3 increase in PM2.5 concentrations (Beelen et al. 2014). In this study, the effect of PM2.5 on all-cause mortality was about twice as large as in previous estimates. The link between PM2.5 levels and mortality remained significant even when PM2.5 concentrations were lower than the European annual mean limit value of 25 μg/m3 (hazard ratio, 1.06; 95% confidence interval, 1.00–1.12) and even when they were below 20 μg/m3 (hazard ratio 1.07; 95% confidence interval, 1.01–1.13). Interestingly, the study showed no significant association with cardiovascular mortality (Beelen et al. 2014).
A number of epidemiological studies found a positive relationship between long-term exposure to fine particulate matter and cardiovascular mortality. Most of these studies included a wide spectrum of potential confounders, and the observed results remained unchanged or even increased in co-pollutant models adjusted for NO2, ozone, or SO2.
In the time-series analysis in 272 major cities in China, Liu et al. (2018) revealed an association between carbon monoxide concentrations and cardiovascular mortality and did not find a concentration below which carbon monoxide exposure had no effect on cardiovascular system.
In the Woman’s Health Initiative study of nearly 66,000 healthy postmenopausal women from 36 cities in the USA, a 10 μg/m3 increase in long-term fine particulate matter exposure was related to a 24% (hazard ratio, 1.24; 95% confidence interval, 1.09–1.41) and 76% (hazard ratio, 1.76; 95% confidence interval, 1.25–2.47) increase in the risk of cardiovascular events and cardiovascular mortality, respectively (Miller et al. 2007).
Another large Canadian national-level cohort study demonstrated that long-term PM2.5 exposure was associated with cardiovascular mortality (Crouse et al. 2012). The estimated hazard ratio for ischemic heart disease-related mortality was 1.31 (95% confidence interval, 1.27–1.35) for each increase in PM2.5 by 10 μg/m3. These associations were observed with exposure to PM2.5 at concentrations that were mostly lower (mean, 8.7 μg/m3) than those reported previously (Crouse et al. 2012). Similar findings were reported in the 2001 Canadian Census Health and Environment Cohort study (Pinault et al. 2017). In this study, the hazard ratio for mortality due to cardiovascular disorders was 1.25 (95% confidence interval, 1.19–1.31); ischemic heart disease, 1.36 (95% confidence interval, 1.28–1.44); cardiometabolic disease, 1.27 (95% confidence interval, 1.21–1.33); and chronic obstructive pulmonary disease, 1.24 (95% confidence interval, 1.11–1.39).
On the other hand, the NIH-AARP Diet and Health Study of 517,043 people—a collaboration between the National Institutes of Health (NIH) and AARP (formerly known as the American Association of Retired Persons)—showed that a chronic fine particulate matter exposure was associated with higher cardiovascular mortality by 10% (per 100 μg/m3 increase), despite low fine particulate matter concentrations (10–13 μg/m3) (Thurston et al. 2016). This study also demonstrated that long-term exposure to fine particulate matter was significantly related to all-cause (hazard ratio, 1.03; 95% confidence interval, 1.00–1.05) and cardiovascular (hazard ratio 1.10; 95% confidence interval, 1.05–1.15) mortality.
Similarly, the Aphekom-improving knowledge and communication for decision making on air pollution and health in Europe project confirmed that the major health burden in 25 European cities can be attributed to the effects of long-term exposure to PM2.5 (Pascal et al. 2013). It is estimated that the adherence to the World Health Organization guidelines for PM2.5 (annual mean < 10 μg/m3) would result in a median increase in life expectancy at the age of 30 years of 5.8 months.
A meta-analysis by Hoek et al. (2013) demonstrated that a 10-μg/m3 increase in the annual PM2.5 concentration results in an average increase in all-cause mortality by 6% (95% confidence interval, 4–8) and in cardiovascular mortality by 11% (95% confidence interval, 5–16). Another meta-analysis by Bourdrel et al. (2017) showed that air pollution with PM2.5 most strongly correlated with mortality associated with coronary artery disease (Bourdrel et al. 2017).
Kioumourtzoglou et al. (2016) were the first to demonstrate a positive relationship between the effects of temperature, chronic PM2.5 exposure, and mortality. A study of a large population of more than 35 million Medicare enrollees from 207 American cities found a stronger relationship between long-term PM2.5 exposure and mortality in cities with higher average temperatures. Furthermore, the authors found that temperature may indicate varying particle composition, because it influences the size and composition of particulate matter in urban air. In addition to PM2.5, long-term exposure to gaseous co-pollutants was also shown to be related to all-cause and cardiovascular mortality.
Hoek et al. (2013) demonstrated that all-cause mortality was significantly associated with ambient air nitrogen dioxide concentrations (pooled estimate per 10 μg/m3, 5%; 95% confidence interval, 3–8). A meta-analysis by Faustini et al. (2014) found that long-term exposure to nitrogen dioxide also significantly impacts all-cause mortality, independently of PM2.5 levels. They reported a 13% increase in cardiovascular mortality related to a 10-μg/m3 increase in annual nitrogen dioxide concentrations (Faustini et al. 2014). The detrimental effects of chronic exposure to ozone appear to be less evident (Bourdrel et al. 2017). Several studies showed a modest increase in cardiopulmonary mortality in response to chronic exposure to ozone; however, this was observed only during the warm season and not in the annual analysis (Bourdrel et al. 2017; Atkinson et al. 2016). This can be partly explained by the fact that ozone pollution tends to occur on warm and sunny days, because its formation requires photochemical reactions (Bourdrel et al. 2017). It was shown that for every 10-ppb increase in chronic warm-season exposure to ozone, the hazard ratios for cardiovascular and respiratory deaths were 1.01 (95% confidence interval, 1.00–1.02) and 1.03 (95% confidence interval, 1.01–1.05), respectively (Atkinson et al. 2016). Finally, long-term exposure to sulfur dioxide was strongly related to respiratory mortality, but the results for the effect on cardiovascular deaths were inconclusive (Bourdrel et al. 2017).
The present cohort studies extend our knowledge about the relationship between long-term exposure to ozone and cardiovascular mortality; however, the study results are inconsistent (US EPA. ISA for Ozone and Related Photochemical Oxidants, 2020). The strongest evidence for this relationship was reported in a cohort study published by Jerrett et al. (2009); Turner et al. (2016).
There is insufficient evidence on the health effects of exposure to pollutant concentrations lower than the current limits set by the European Union and World Health Organization guidelines. A recent meta-analysis of six large European administrative cohorts within the effects of low-level air pollution: a study in Europe (ELAPSE) project, including almost 27 million participants contributing more than 240 million person-years, revealed that exposure to PM2.5, nitrogen dioxide, and black carbon was significantly positively associated with natural, respiratory, cardiovascular, and lung cancer mortality. These associations remained significant at low levels: below 10 μg/m3 for PM2.5 and below 20 μg/m3 for nitrogen dioxide. Two-pollutant models with black carbon and nitrogen dioxide remained significantly associated with mortality in two-pollutant models with PM2.5 and ozone. The PM2.5 hazard ratio reduced two-pollutant model with nitrogen dioxide (Rodopoulou et al. 2021).
Air pollution and coronary artery disease
There is growing evidence that chronic exposure to air pollutants contributes to the pathogenesis of coronary artery disease. The current state of knowledge indicates that among air pollutants, PM2.5 and nitrogen oxides play the most important role in the pathophysiology of coronary disease (Brook et al. 2010; Newby et al. 2015; Robertson and Miller 2018; Integrated Science Assessment for Particulate Matter 2019. United States Environment Protection Agency website; Health Canada. Human health risk assessment for coarse particulate matter 2016).
A number of epidemiological studies showed that chronic exposure to air pollution, particularly to PM2.5, favors premature atherosclerosis and is associated with cardiovascular events (Cesaroni et al. 2014; Kaufman et al. 2016; Bourdrel et al. 2017; Ljungman et al. 2019).
A prospective 10 years cohort study of Kaufman et al. (2016), which included 6795 participants of the multi-ethnic study of atherosclerosis and air pollution (MESA Air study) in six metropolitan areas in the USA, found that exposure to PM2.5 and traffic-related air pollutants was associated with an increased coronary artery calcium score. It was demonstrated that an elevation in PM2.5 levels by every 5 μg/m3 increased the coronary calcium score by 4.1 Agatston units per year (95% CI, 1.4–6.8). Moreover, an increase in nitrogen oxide concentrations by every 40-ppb enhanced the coronary calcium score by 4.8 Agatston units per year (95% CI, 0.9–8.7) (Kaufman et al. 2016). Similar results has been presented in another cohort study (Hoffmann et al. 2007) and cross-sectional analysis of the Heinz Nixdorf Recall study (Kälsch et al. 2014).
In turn, Tonne et al. (2012) reported that exposure to coarse particulate matter was related to a 5.0% (95% confidence interval, 1.9%–8.3%) increase in carotid intima-media thickness even after adjustment for covariates. However, it should be noted that none of those studies found a relationship between chronic exposure to outdoor air pollution (including PM2.5, coarse particulate matter, and gaseous co-pollutants) and subclinical atherosclerosis (Kim et al. 2014; Perez et al. 2015; Dorans et al. 2016).
There is strong evidence for a significant association of chronic exposure to air pollution with the risk of acute myocardial infarction (Bourdrel et al. 2017; Rajagopalan et al. 2018). Many studies, but not all, have shown the effect of chronic exposure to various air pollutants on the increased incidence of acute coronary syndromes, including acute myocardial infarction.
A longitudinal cohort study of all physical workers in the Swedish National Census of 1,725,671 subjects demonstrated that occupational exposure to both small (adjusted hazard ratio, 1.12; 95% confidence interval, 1.09–1.15) and to large (adjusted hazard ratio, 1.14; 95% confidence interval, 1.10–1.18) particles was related to the incidence of acute myocardial infarction (Wiebert et al. 2012). The risk associated with exposure to small particles (< 1 μm) was increased in women (hazard ratio, 1.30; 95% confidence interval, 1.12–1.51) compared with men (hazard ratio, 1.10; 95% confidence interval, 1.07–1.14).
A previous longitudinal cohort study of Seoul residents, which used data from 136,094 health insurance claims, found that chronic exposure to PM2.5 (adjusted hazard ratio, 1.36; 95% confidence interval, 1.19–1.56 per 1 μg/m3), coarse particulate matter (adjusted hazard ratio, 2.14; 95% confidence interval, 2.02–2.27 per 1 μg/m3), nitrogen dioxide (adjusted hazard ratio, 1.81; 95% confidence interval, 1.46–2.25 per 18.4 ppb), sulfur dioxide (adjusted hazard ratio, 1.82; 95% confidence interval, 1.52–2.19 per 2.54 ppb), and carbon monoxide (adjusted HR, 2.12; 95% confidence interval, 1.72–2.61 per 0.25 ppm), but not ozone, was related to the occurrence of myocardial infarction (Kim et al. 2017).
A prospective cohort study and meta-analysis of 11 European cohorts from the European study of cohorts for air pollution effects (ESCAPE) revealed that an annual increase of 5 μg/m3 in PM2.5 concentrations and of 10 μg/m3 in coarse particulate matter concentrations was associated with an increase in the risk of acute myocardial infarction of 13% (hazard ratio, 1.13, 95% confidence interval, 0.98–1.30) and 12% (HR, 1.12, 95% confidence interval, 1.01–1.25), respectively (Cesaroni et al. 2014). Of note, the relationships observed in this study were also present at air pollutant concentrations below the current annual European threshold of 25 μg/m3 for PM2.5 (hazard ratio, 1.18; 95% confidence interval, 1.01–1.39 for a 5-μg/m3 increase in PM2.5) and below the threshold of 40 μg/m3 for coarse particulate matter (hazard ratio, 1.12; 95% confidence interval, 1.00–1.27 for a 10-μg/m3 increase in coarse particulate matter).
Finally, the results of a pooled analysis of six European cohorts within the effects of low-level air pollution: a study in Europe (ELAPSE) of 137,148 participants with a mean age at baseline of 54 years and median follow-up of 17.2 years indicated that the incidence of coronary artery disease was associated with exposure to nitrogen dioxide (hazard ratio, 1.04; 95% confidence interval, 1.01–1.07) but not to PM2.5. Concentration–response curves revealed no evidence of a threshold below which air pollutant concentrations are save for health. Negative effect estimates for nitrogen dioxide were elevated even for concentrations lower than the European Union limit values of 40 μg/m3 (Wolf et al. 2021).
Effect of chronic air pollution on blood pressure and arterial hypertension
In the latest years, a numerous studies have shown that exposure to higher concentrations of PM2.5 and some gaseous air pollutants (nitrogen oxides, sulfur dioxide, and ozone) can also result in arterial hypertension and increased blood pressure (ISA ES EPA 2019; U.S. EPA. Supplement EPA 2021; ISA ED EPA for ozone 2020; US. EPA. ISA for Oxides of Nitrogen 2016).
Chronic exposure to particulate matter
Several studies showed a positive association between chronic PM2.5 exposure and either systolic or diastolic blood pressure or both. (Chuang et al. 2011; Dong et al. 2013).
In contrast, a meta-analysis by Fuks et al. (2014), which included 113,926 participants from 15 international cohorts of the European study of cohorts for air pollution effects (ESCAPE), found no significant association between PM2.5 concentrations and blood pressure. Similar conclusions were drawn from a meta-analysis by Cai et al. (2016), who also found no relationship between chronic PM2.5 exposure and the risk of hypertension.
Few years later in new meta-analysis, involving seven cohorts from the European study of cohorts for air pollution effects (ESCAPE), Fuks et al. (2017) found a significant association between higher PM2.5 levels and the incidence of self-reported hypertension (relative risk, 1.22; 95% confidence interval, 1.08–1.37 per each 5 μg/m3 increase).
In a cross-sectional study of 13,975 population, Liu et al. (2017) observed that systolic blood pressure increased by 0.60 mmHg (95% confidence interval, 0.05–1.15) per 41.7 μg/m3 increase in PM2.5 levels. The annual average exposure to PM2.5 for all study participants was 72.8 μg/m3. In contrast, in a cross-sectional study of 2552 subjects, Pitchika et al. (2017) demonstrated an increase in diastolic blood pressure by 0.7% (95% confidence interval, 0.2–1.2) per a 1 μg/m3 increase in PM2.5 levels.
In a study by Liu et al. (2017), the odds ratio of hypertension per a 41.7 μg/m3 increase in chronic average PM2.5 levels was 1.11 (95% confidence interval, 1.05–1.17). It was also found that an interquartile range increase in the annual average PM2.5 concentration (by 1 μg/m3) was significantly associated with a 15% higher prevalence of arterial hypertension (95% confidence interval, 2.5–28.0).
A recent large prospective cohort study—the China prediction for atherosclerotic cardiovascular disease risk (China-PAR) project involving 119,388 individuals—provided the first evidence that chronic exposure to PM2.5 was independently associated with the occurrence of hypertension at relatively high levels of ambient PM2.5 (mean annual concentrations, 58.4 μg/m3) (Huang et al. 2019). Study participants in the highest quartile of PM2.5 levels had an increased risk of hypertension with a hazard ratio of 1.77 (95% confidence interval, 1.56–2.00), compared with those in the lowest quartile. Each 10 μg/m3 increase in the PM2.5 level resulted in an 11% increased risk of hypertension (hazard ratio 1.11; 95% confidence interval, 1.05–1.17) (Huang et al. 2019).
Long-term exposure to ozone
Few cohort studies showed an association between chronic exposure to ozone and elevation of blood pressure or the prevalence of hypertension (Chuang et al. 2011; Dong et al. 2013).
A significant relation between ozone concentrations and hypertension was also found by Coogan et al. (2017). In this study, the estimated hazard ratio of arterial hypertension per a 6.7 ppb increase in ozone levels was 1.09 (95% confidence interval, 1.00–1.18).
However, the strength of the association between chronic ozone exposure and blood pressure remains unclear. Scientific evidence are suggestive of, but not sufficient to infer, a causal relationship. (Integrated Science Assessment for Ozone and Related Photochemical Oxidants, 2020; https://www.epa.gov/isa/integrated-science-assessment-isa-ozone-and-related-photochemical-oxida).
Long-term exposure to nitrogen dioxide
The impact of chronic exposure to nitrogen dioxide on blood pressure was evaluated in the study by Chuang et al. (2011), which showed that a 12.83 ppb increase in nitrogen dioxide concentrations was related to an increase in systolic blood pressure by 14.40 mmHg (95% confidence interval, 10.98–17.82) and diastolic blood pressure by 12.43 mmHg (95% confidence interval, 10.63–14.23). The similar positive relationship between exposure to nitric oxide and nitrogen dioxide and elevation of diastolic blood pressure was shown in a Chinese cross-sectional study on a cohort of 27,752 participants aged > 65 years (Chen et al. 2015). The average annual levels of nitric oxide and nitrogen dioxide in this study were 38.4 ± 15.3 and 23.7 ± 5.8 μg/m3, respectively. However, other single studies (Sorensen et al. 2012; Dong et al. 2013; Fuks et al. 2014; Pitchika et al. 2017) and large multi-cohort meta-analyses of the European study of cohorts for air pollution effects (ESCAPE) (Fuks et al. 2014, 2017) did not confirm the relationship between nitrogen dioxide levels and elevation of blood pressure.
Long-term exposure to sulfur dioxide
There are a limited number of studies evaluating the effects of sulfur dioxide on blood pressure or arterial hypertension (Chuang et al. 2011; Dong et al. 2013). Chuang et al. (2011) showed a significant positive relationship between an increase in sulfur dioxide concentrations by 20 μg/m3 and an elevation in systolic blood pressure by 0.80 mmHg (95% confidence interval, 0.46–1.14) and diastolic blood pressure by 0.31 mmHg (95% confidence interval, 0.10–0.51). In this study, the odds ratio for hypertension was 1.11 (95% confidence interval, 1.04–1.18). In contrast, no association between increased mean sulfur dioxide levels (54.42 ± 14.33 mg/m3) and elevated blood pressure was found by Dong et al. (2013). Similarly, no such relationship was observed in a Serbian study (Stanković et al. 2018).
While most of the cited studies showed a positive link between ambient air pollutants (particularly PM2.5) and blood pressure or hypertension, it should be noted that they were not without limitations. First, in the majority of the studies, there was no appropriate adjustment for confounding or effect modification by other variables (including treatment of hypertension and other comorbidities, emotional/psychosocial stress, diet, obesity, temperature, traffic noise, and the synergistic effect of a mixture of pollutants). Furthermore, some of the confounding factors are difficult to measure. The studies used various lag patterns of exposure to assess immediate, delayed, or late effects of exposure. They also differed in their statistical analysis and methods of blood pressure measurement (Wang et al. 2017). In addition, most studies did not evaluate individual exposure to ambient air pollutants and had different methods of measurement of pollutants. In estimating the health effects of chronic long-term exposure, detailed information is needed on past and lifetime exposure levels, the age at which exposure occurred, and pre-exposure health status, whereas most studies did not have such information. Finally, although all those studies suggested that long-term exposure to ambient air pollution is associated with alterations in blood pressure in distinct subpopulations, the results remain conflicting and inconclusive.
Effect of chronic exposure to air pollution on heart failure
Several studies showed a positive relationship of long-term exposure to particulate matter and selected gaseous pollutants with the risk of death or hospitalization from heart failure. There is a general consensus that the pathomechanisms underlying heart failure worsening associated with exposure to air pollution have not been fully elucidated. It is possible that chemical pollutants irritate the lower airways, consequently enhancing pulmonary vasoconstriction and increasing right ventricular diastolic filling pressures. This, in turn, can result in pressure overload, which may be which may be fundamental for the deterioration of heart failure. Moreover, when selected pollutants enter the bloodstream, they can increase peripheral vascular resistance and blood pressure, thus leading to increased cardiac afterload, prothrombotic state, and secondary hypoxia. All of these pathomechanisms can contribute to the exacerbation of heart failure.
The relationship between long-term exposure to ambient air pollution and heart failure has been confirmed in several, mostly cohort, studies. In a large cohort of 836,557 patients aged 40–89 years and registered in general practices in England, Atkinson et al. (2013) found a positive correlation between air pollutant exposure and incidence of heart failure. After adjusting for confounders, a 3 μg/m3 increase in coarse particulate matter and a 10.7 μg/m3 increase in nitrogen dioxide resulted in a hazard ratio for heart failure of 1.06 (95% confidence interval, 1.01–1.11). Of note, the study follow-up was 5 years, and the mean 1 year average concentrations of coarse particulate matter and nitrogen dioxide were 19.7 and 22.5 μg/m3, respectively (Atkinson et al. 2013).
The association between long-term exposure to ultrafine particulate matter and nitrogen dioxide and an increased incidence of heart failure was also reported in another cohort study by Bai et al. (2019a). The authors found that each interquartile range increase in exposure to ultrafine particulate matter, nitrogen dioxide was related to an increased incidence of heart failure (hazard ratio, 1.03; 95% confidence interval, 1.02–1.05 and hazard ratio, 1.04; 95% confidence interval, 1.03–1.06, respectively). Danesh Yazdi et al. (2019), in a large cohort of 11,084,660 subjects from the USA aged 65 years or older, showed that chronic exposure to PM2.5 and ozone led to a higher rate of hospitalizations for exacerbation of preexisting heart failure. In this study, each 1-μg/m3 increase in PM2.5 concentration resulted in a 5.3% increase in first hospital admissions for heart failure. The hazard ratio for hospitalization due to heart failure was 1.053 (95% confidence interval, 1.052–1.054) for long-term exposure to PM2.5 and 1.023 (95% confidence interval, 1.022–1.024) for ozone. There were also substantial health effects for average annual PM2.5 concentrations below 12 μg/m3 and ozone concentrations below 70 ppm. However, an important limitation of the study was the method used to estimate the time of exposure to air pollutants, as exposure was imputed using the participant’s zip code, which could result in a measurement error depending on how much time the participant spent in a certain area. In addition, the study did not assess the effect of other confounders, primarily the risk factors of heart failure exacerbation. In a large cohort study of 5,000,000 population conducted in Canada, Bai et al. (2019b) also found a significant association between chronic exposure to PM2.5, nitrogen dioxide, and ozone and the occurrence of heart failure and acute myocardial infarction. Each interquartile range increase in exposure to PM2.5, nitrogen dioxide, and ozone was related to a higher incidence of heart failure (hazard ratio, 1.05; 95% confidence interval, 1.04–1.05 for PM2.5; hazard ratio, 1.02; 95% confidence interval, 1.01–04 for nitrogen dioxide; and hazard ratio, 1.03; 95% confidence interval, 1.02–1.03 for ozone) (Bai et al. 2019b). A more recent analysis of data on female nurses from the Danish Nurse Cohort (aged > 44 years) performed by Lim et al (2021) revealed an enhanced risk of heart failure incidence in persons exposed to high levels of two pollutants (PM2.5, nitrogen dioxide) and concomitant road traffic noise during the mean time exposure of about 3 years. The hazard ratios were 1.17 (95% confidence interval, 1.01–1.36), 1.10 (95% confidence interval, 0.99–1.22), and 1.12 (95% confidence interval, 0.99–1.26) per an increase of 5.1 µg/m3 in PM2.5, 8.6 µg/m3 in nitrogen dioxide, and 9.3 dB in road traffic noise, respectively. The associations were more evident in smokers and nurses with hypertension.
It is important to note that the majority of studies showing an association between chronic exposure to ambient air pollution and the risk of hospitalization and death due to heart failure have a number of limitations. Data on the diagnosis of heart failure were derived from death certificates, autopsy documentation, or hospital discharge records, in which heart failure was very frequently listed as a secondary and direct cause of death, regardless of the primary cause. However, even in patients with a previous diagnosis of chronic heart failure, it is often challenging to identify the cause of heart failure exacerbation and death (e.g., progression of myocardial ischemia, coexisting infection, overexertion, or excessive salt and fluid intake). In the above studies, none of these confounders were included in the analysis. Furthermore, these studies did not reflect individual exposure to air pollutants. Therefore, all these ambiguities and limitations caused by the misclassification of exposure as well as the presence of confounders make interpretation of the available evidence difficult.
Chronic exposure to air pollution and stroke
Data from the World Health Organization show that approximately 20% of air pollution-related deaths are due to ischemic stroke (www.who.int/health-topics/air-pollution). Another report revealed a downward trend in the mortality rate from ischemic stroke attributed to exposure to air pollution; however, the data varied by region of the world (Babatola 2018). The link between chronic exposure to air pollution and stroke incidence or stroke-related mortality has been assessed predominantly in cohort studies. Most of them showed a positive relationship, although the results were not consistent.
Yuan et al. (2019) conducted a meta-analysis of 16 cohort studies from Europe, North America, and Asia, involving more than 2.2 million participants and more than 49,149 endpoint events. They investigated the association between chronic PM2.5 exposure and incident stroke and stroke-related death. The pooled hazard ratio for each 5 μg/m3 increase in PM2.5 levels was 1.11 (95% confidence interval, 1.05–1.17) for incident stroke and 1.11 (95% confidence interval, 1.05–1.17) for stroke-related death. Of note, a significant relationship between PM2.5 levels and incident stroke was found in Europe (hazard ratio, 1.07; 95% confidence interval, 1.05–1.10) and North America (hazard ratio, 1.09; 95% confidence interval, 1.05–1.14), whereas the pooled result for Asia was not significant (hazard ratio, 2.31, 95% confidence interval, 0.49–10.95). Surprisingly, the results among current smokers were not significant, although smoking is an independent risk factor for all cardiovascular diseases.
A recent analysis of a prospective cohort of 4,105 subjects aged 45–76 at baseline, including 52.5% of women, from the Heinz Nixdorf Recall study conducted in Germany revealed that exposure to traffic-specific particulate matter had a more potent effect on the risk of stroke than industry-specific PM2.5 during 14 years follow-up (hazard ratio, 2.53; 95% confidence interval, 1.07–5.97 and hazard ratio, 1.27; 95% confidence interval, 1.03–1.56, respectively, per 1 μg/m3 increase) (Rodins et al. 2020). This study included numerous confounders, which improves its quality.
The analysis of six European cohorts within the effects of low-level air pollution: a study in Europe (ELAPSE) project showed that long-term exposure to air pollution was associated with stroke occurrence even at pollutant concentrations lower than the current limit values (Wolf et al 2021). Importantly, the definition of stroke in this study comprised the principal diagnosis of ischemic, hemorrhagic, or unspecified stroke and out-of-hospital deaths from cerebrovascular diseases. The incidence of stroke was associated with PM2.5 (hazard ratio, 1.10; 95% confidence interval, 1.01–1.21 per 5 μg/m3 increase), nitrogen dioxide (hazard ratio, 1.08; 95% confidence interval, 1.04–1.12 per 10 μg/m3 increase), and black carbon (hazard ratio, 1.06; 95% confidence interval, 1.02–1.10 per 0.5 10−5/m increase). The results of the effects of low-level air pollution: a study in Europe (ELAPSE) project support the role of nitrogen dioxide or correlated pollutants as an important risk factor for stroke (Wolf et al 2021).
The assessment of the above cohort studies and meta-analyses suggests that among the evaluated air pollutants, particulate matter and nitrogen dioxide have the strongest association with the risk of stroke. This particularly concerns subjects over 60 years of age. However, there are some discrepancies between the studies related to geographical region. In addition, most investigators focused on ischemic stroke failed to provide a clear distinction between the different types of stroke (hemorrhagic vs. ischemic), or provided an incorrect definition of stroke. The studies underestimated the major confounders of stroke, and the authors themselves indicated a misclassification of exposure and substantial heterogeneity for most pollutants. Thus, the existing evidence on the association between air pollution and stroke is insufficient and requires further research.
Air pollution and the coagulation system
The effects of air pollutants on coagulation disorders are still under investigation. The vast majority of studies focused on the direct or indirect ability of particulate matter to activate coagulation and impair fibrinolytic activity. However, most studies investigated short-term exposure, and more data are required on the effects of chronic exposure.
Studies on long-term exposure to air pollution did not find a significant relationship between ambient air pollution and fibrinogen levels (Dadvand et al. 2014; Viehmann et al. 2015). Of note, studies described in previous sections also provided conflicting results with regard to changes in plasma levels of coagulation factors other than fibrinogen.
Results from several experimental studies suggested a link between hypercoagulability and exposure to PM2.5 and an immediate effect of soluble metal compounds (e.g., sulfate and nitrates) that can activate a number of human prothrombotic factors (Sangani et al. 2010; Gray et al. 2015; Pun et al. 2015; Tinkov et al. 2018; Signorelli et al. 2019). All metal sulfates except nickel were proven to shorten the whole-blood coagulation time. Another possible pathomechanism of hypercoagulability is the induction of gene hypomethylation resulting in inflammation and secondary venous thrombosis (Tarantini et al. 2013).
Tang et al. (2016) conducted a meta-analysis of eight prospective cohort, case-crossover, case–control, and time-series studies performed in Western countries, where the median PM2.5 level is lower than 20 μg/m3, in contrast to Central and Eastern Europe as well as Asia, where the median PM2.5 levels are much higher. The analysis of long-term exposure did not confirm a positive association between traffic-related air pollutants (particulate matter, carbon monoxide, sulfur dioxide, ozone, and nitrogen dioxide) and the risk of incident venous thromboembolism. Therefore, the relationship between ambient air pollution and venous thromboembolism cannot be confirmed as yet.
Chronic exposure to air pollution and cardiac arrhythmias
The association between air pollution and cardiac arrhythmias is still under investigation. The available papers report conflicting results depending on the study design, the strength of statistical relationships between the investigated air pollutants, the levels of air pollutants at which a harmful health effect is observed, and definition of outcomes.
In their paper, Tsai et al (2009) described a significant positive relationship between a single pollutant model of long-term exposure to nitrogen dioxide, ozone, and particulate matter regardless of air temperature and emergency room visits for arrhythmias in inhabitants of a subtropical city in Taiwan. For a two-pollutant model, the results were significant for ozone and nitrogen dioxide. The results of another cohort study—the Danish diet cancer and health study involving 57,053 participants aged 50–64 years—also showed a proarrhythmic effect of long exposure to nitrogen dioxide and nitrogen oxides and higher risk of atrial fibrillation (Monrad et al. 2017). Some investigators suggested that nitrogen dioxide is a surrogate for PM2.5 rather than exerting a causal direct effect on the heart (Billionnet et al. 2012).
Some studies indicated positive associations between long-term exposure to PM2.5 and increased risk of supraventricular arrhythmias. A nationwide cohort study of 432,587 population from the Korean National Health Insurance Service National Sample Cohort reported a link between long-term exposure to air pollution and atrial fibrillation. A 10-μg/m3 increase of PM2.5 was associated with a 17.9% increase in the risk of atrial fibrillation (p < 0.001). Effects were more profound in men, obese individuals, participants aged ≥ 60 years, and those with previous myocardial infarction (Kim et al. 2019).
Another cohort study of 5,071,956 subjects aged 35–85 years conducted in Canada demonstrated that long-term exposure to PM2.5 was positively associated with the incidence of atrial fibrillation even at very low levels (Shin et al. 2019). On the other hand, Kwon et al. (2019) revealed no significant evidence for a link between ambient air pollution and cardiac arrhythmias in long-term exposure.
Although most of these studies included potential confounding factors (such as weather conditions or the presence of coronary artery disease and hypertension), they are not without limitations. First, they did not consider all substrates for arrhythmia or the severity of arrhythmia and concomitant pharmacotherapy. Furthermore, they failed to assess triggers of arrhythmia such as recurrent myocardial ischemia, physical exertion, emotional stress, electrolyte imbalance, elevation in blood pressure, alcohol consumption, or tobacco smoking. Although the assessment of arrhythmia triggers is difficult in everyday practice, particularly in retrospective studies, both substrates and triggers are more important contributors to arrhythmia than ambient air pollution. Some patients with atrial fibrillation or nonsustained ventricular tachycardia can be asymptomatic, and some arrhythmic events may go unnoticed in the absence of an arrhythmia monitoring device. A number of studies did not require independent confirmation by a cardiologist that cardioverter-defibrillators were activated by ventricular tachycardia (i.e., appropriate interventions). Finally, all these studies are inherently limited by an individual exposure estimation error. In summary, the existing evidence is insufficient to support a strong effect of ambient air pollution on the incidence of cardiac arrhythmias.
Associations between chronic ambient air pollution and cardiovascular diseases in the era of COVID-19
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) first appeared in December 2019 in Wuhan, China, and then spread worldwide within 2–3 months, causing the COVID-19 pandemic, the largest pandemic on record since 1918 (Chen et al. 2021; Dutta et al. 2021; Han et al. 2020; Khan et al. 2021; Parczewski and Ciechanowicz 2021; Sławiński and Lewicka 2020). Data from the World Health Organization indicate that as of December 27, 2021, nearly 280 million COVID-19 cases and more than 5 million COVID-19 deaths have been documented worldwide (WHO 2021a).
There is an increasing evidence for an association between chronic air pollution, SARS-CoV-2 infection, and cardiovascular diseases. Because we are still in the midst of the COVID-19 pandemic at the time of writing this paper (December 2021), it is challenging to draw definitive conclusions on how COVID-19-related changes in air pollution have affected cardiovascular morbidity and mortality. The effect of COVID-19 on the relationship between ambient air pollution and cardiovascular diseases appears to be bidirectional. On the one hand, there are reports that both indoor and outdoor air pollution increase the risk of SARS-CoV-2 infection and its cardiovascular complications (Ali and Islam 2020). On the other hand, there is evidence that preventive measures to reduce the spread of SARS-CoV-2 can be a source of environmental pollution, including air pollution, and have adverse health effects (Akter et al. 2021; Ufnalska and Lichtfouse 2021).
The SARS-CoV-2 transmission can occur via direct, indirect, or close contact with infected individuals, through infected secretions including saliva and respiratory secretions or their respiratory droplets (> 5–10 μm in diameter) that are expelled when an infected patient coughs, sneezes, talks, or sings (WHO 2021b). Despite some previous controversy (WHO 2021b; Chen et al. 2021; Wang Q et al. 2021), airborne transmission has recently been confirmed as a possible route of COVID-19 transmission.
It was postulated that ambient air pollution may play an important role in the airborne transmission of SARS‐CoV‐2 (Ali et al. 2020). The studies by Setti et al. provided the first evidence that SARS-CoV-2 RNA can be present on outdoor particulate matter under some conditions of atmospheric stability and at elevated coarse particulate matter levels (Setti et al. 2020). In several countries, the presence of SARS-CoV-2 in the air was directly correlated with the presence of high particulate matter concentrations, which resulted in increased mortality (Dutta et al. 2021). Although studies on the association between long-term exposure to PM2.5 and COVID-19 infections as well as COVID-19-related deaths have been limited and their results was inconsistent, it has been shown that PM2.5 exposure impairs host defenses and, in particular, alters macrophage function, which facilitates respiratory infection by SARS-CoV-2 (U.S. EPA. 2021). There is also evidence that exposure to PM2.5 may lead to decreases in an individual’s immune response, which in turn may promote replication of many respiratory viruses, probably including SARS-CoV-2 (Bourdrel et al. 2021; U.S. EPA. 2021). However, these studies have some methodological limitations (e.g., studies performed during an ongoing pandemic before COVID-19 had reached many parts of the country, failing to account for other key factors that could have a major impact on the spread of SARS-CoV-2); therefore, their results should be interpreted with caution.
The relationship between long-term exposure to PM2.5 and COVID-19 outcomes, including COVID-19-related deaths, has recently been evaluated in several large, primarily ecological studies (Chakrabarty et al. 2021; Liang et al. 2020; Stieb et al. 2020; Wu et al. 2020). Although positive associations have been observed in some of these studies, there is limited evidence at this stage of the COVID-19 pandemic to conclude whether long-term exposure to PM2.5 or other air pollutants significantly affects the spread of SARS-CoV-2 or susceptibility to infection in humans (U.S. EPA. 2021).
The possible association of long-term exposure to air pollution, including high concentrations of nitrogen dioxide and particulate matter, with high rates of SARS-CoV-2 infection in some patient populations may be partly explained by air pollution-induced overexpression of angiotensin-converting enzyme 2, an 805 amino-acid transmembrane monocarboxypeptidase, on human airway epithelial cell surfaces (Paital and Agrawal 2020). In addition to its key physiological role in the renin–angiotensin–aldosterone system and regulation of the plasma kallikrein-kinin system, angiotensin-converting enzyme 2 serves as a host receptor for coronaviruses that is recognized by the S protein of the SARS-CoV-2, which enables fusion of the virus with the cell membrane of the infected cell and subsequent viral life cycle. Such overexpression of angiotensin-converting enzyme 2 has been proven to occur under chronic exposure to ambient air pollutants such as nitrogen dioxide and PM2.5 (Paital and Agrawal 2020). Paital and Agrawal (2020) demonstrated a relationship between nitrogen dioxide emissions, PM2.5 levels, angiotensin-converting enzyme 2 expression and the severity of COVID-19 infection.
Finally, there is increasing evidence that preventive measures to limit the spread of SARS-CoV-2, which are used widely during the COVID-19 pandemic, have direct and indirect effects on the environment (Akter et al. 2021; Boroujeni et al. 2021; Gorrasi et al. 2020). This has been shown to occur through various mechanisms including:
reductions in fossil fuel consumption, resource depletion, and waste disposal; reductions in transport and industrial activity; and reductions in tourism as a result of lockdowns, travel restrictions, and slowed economic activities;
an increase in medical and municipal waste, haphazard disposal of personal protective equipment, hindered recycling activities due to the widespread use of personal protective equipment and pressure in hospitals;
an increment in energy consumption and increased liquid and solid waste from large-scale use of vaccinations (Akter et al. 2021; Ufnalska and Lichtfouse 2021).
An indirect beneficial effect of the COVID‐19 lockdown in 2020 was a substantial reduction in the emission of air pollutants and improvement in air quality globally. This was particularly noticeable in India, China, and Europe, where PM2.5 concentrations decreased by 64.7, 30, and 17%, respectively (Wolhuter et al. 2021). The cumulative effects of the lockdown have resulted in a 20–30% reduction in the global emission of nitrogen dioxide, the main product of fossil fuel combustion (Wolhuter et al. 2021). Despite this, a regional severe haze was still observed in some areas of the world (Li et al. 2021a, b). Furthermore, during the strict lockdown resulting in a 30% reduction in PM2.5 levels in China, PM2.5 concentrations in 95 Chinese cities, although lower than before the pandemic, were still fourfold higher than those considered safe by the World Health Organization (Wolhuter et al. 2021).
A study by Zheng et al. (2021) comparing air pollution data in Wuhan from 2020 with previous years showed that particulate matter and nitrogen dioxide levels were strongly reduced, carbon monoxide levels were less reduced owing to ongoing power industries, sulfur dioxide levels first decreased and then increased to exceed the 2018–2019 values due to coal combustion, and, finally, ozone concentrations were even higher as a result of lower nitrogen oxide air pollution and the weekend effect. Similarly, Wang et al. (2020) showed that during the lockdown, the average daily concentrations in urban areas decreased by 47.9% for coarse particulate matter, 42.7% for PM2.5, 58.4% for nitrogen dioxide, 28.6% for sulfur dioxide, and 22.3% for carbon monoxide as compared to the same period in 2019.
There are also interesting findings from epidemiological studies conducted in Italy. The COVID-19 pandemic had dramatic consequences for the population of the industrialized and economically developed northern part of Italy, while it did not heavily affect the inhabitants of the southern regions. Roviello and Roviello (2020) found that pandemic severity was generally lower in the evergreen-rich southern regions, especially those with more than 0.3 hectares of forest per capita.
In conclusion, although the association between chronic exposure to air pollution and cardiovascular diseases is well-established, further studies are needed to delineate the precise mechanistic relationship between ambient air pollution and the course of SARS-CoV-2 infection with its serious cardiovascular complications and to explain the effect of long-term exposure to air pollution on differences in COVID-19-related outcomes.
Conclusion
Data from the literature show that exposure to fine particulate matter and some gaseous pollutants is a major contributor to cardiovascular mortality and morbidity. The strongest evidence exists for the effects of air pollution on all-cause and cardiovascular mortality. An alarmingly increasing number of studies indicates that negative health impact of air pollution persists even at pollutant concentrations lower than the limits set by the European Union and World Health Organization. This suggests a wide range of individual susceptibility in the global population to exposure to emerging contaminants present in air. However, studies vary in terms of data reliability and provide inconsistent results. Discrepancies among studies are due to the variety of physical and chemical properties of particulate matter (size, mass, reactivity), emission sources, and concomitant gaseous pollutants. Moreover, studies differ in population and statistical methods, exposure assessment, and adjustment for confounding or modifying factors. It is also challenging to assess general individual exposure and susceptibility, whereas these seem to be the most important factors determining response to environmental pollution. Furthermore, because there is a vast spectrum of individual susceptibility, for many air pollutants there is no evidence on a safe level below which no unfavorable health effects occur. Other challenges involve the reliability of the methods used to analyze the relationships between ambient air pollutants and adverse health effects; the necessity to identify the causal pathways that can help establish preventive strategies; the need to evaluate the properties of air pollutants that change over time and space and to determine the consequences of these variations for the human population; the identification of individuals who are particularly vulnerable to air pollution; defining the extent to which confounding factors mask the actual health effects of air pollution; and assessing whether the interventions taken to improve air quality have beneficial health effects.
Healthcare professionals should play a key role in educating politicians and citizens about the harmful effects of air pollution. It is also essential to combine the existing knowledge with practical opportunities to control emission sources. Only interdisciplinary collaboration can help protect the environment, ensure the human right to preserve health, and develop the optimal methods for reducing air pollution with subsequent evaluation of the achieved outcomes.
Methods
The available literature published over the preceding 30 years was reviewed to evaluate the relationships of chronic outdoor air pollution with cardiovascular morbidity and mortality, and to summarize the potential mechanisms underlying these associations identified in experimental and human studies. Publications were found by searching PubMed, EBSCO, Cochrane, and Science Direct databases, using the following MESH terms: air pollution, chronic or long-time exposure, particulate matter, and gaseous air pollutants. In addition, the following keywords were used: all-cause mortality, cardiovascular mortality, coronary artery disease, cardiac arrhythmias, hypertension, stroke, and coagulation system. Our eligibility criteria were defined following the PECOS approach: population, adults chronically exposed to single or cumulative outdoor air pollutants (i.e., particulate matter and gaseous pollutants); comparator, unexposed individuals; outcome, all-cause mortality, cardiovascular morbidity and mortality; and study design, experimental studies if available (controlled human exposure and/or animal studies), epidemiological studies including cohort, case-cohort, case–control, and cross-sectional studies, intervention studies, and meta-analyses and systematic reviews published (or accepted for publication, i.e., in press) between January 1990 and October 2021 in peer-reviewed journals and written in English. Studies involving children and those focusing on indoor exposure and exposure to persistent organic chemicals, gray literature, conference abstracts, conference papers, notes, editorials, letters, and unpublished data were excluded from the analysis. After the initial analysis of about 540 articles, 123 articles were included in the review.
Author contributions
All authors contributed to the study conception and design, material preparation, data collection and analysis, writing of the original draft, its review and editing. All authors read and approved the final manuscript.
Funding
This work was supported by the Polish National Science Centre (Grant number 2016/21/B/NZ7/01747 to E.K.).
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ewa Konduracka, Email: ekonduracka@interia.eu.
Paweł Rostoff, Email: pawel.rostoff@uj.edu.pl.
References
- Akter S, Zakia MA, Mofijur M, Ahmed SF, Vo DN, Khandaker G, Mahlia TMI. SARS-CoV-2 variants and environmental effects of lockdowns, masks and vaccination: a review. Environ Chem Lett. 2021;2021:1–12. doi: 10.1007/s10311-021-01323-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali N, Islam F. The effects of air pollution on COVID-19 infection and mortality-a review on recent evidence. Front Public Health. 2020;8:580057. doi: 10.3389/fpubh.2020.580057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almetwally AA, Bin-Jumah M, Allam AA. Ambient air pollution and its influence on human health and welfare: an overview. Environ Sci Pollut Res. 2020;27:24815–24830. doi: 10.1007/s11356-020-09042-2. [DOI] [PubMed] [Google Scholar]
- Araujo JA, Barajas B, Kleinman M, Wang X, Bennett BJ, Gong KW, Navab M, Harkema J, Sioutas C, Lusis AJ, Nel AE. Ambient particulate pollutants in the ultrafine range promote early atherosclerosis and systemic oxidative stress. Circ Res. 2008;102:589–596. doi: 10.1161/CIRCRESAHA.107.164970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson RW, Carey IM, Kent AJ, van Staa TP, Anderson HR, Cook DG. Long-term exposure to outdoor air pollution and incidence of cardiovascular diseases. Epidemiology. 2013;24:44–53. doi: 10.1097/EDE.0b013e318276ccb8. [DOI] [PubMed] [Google Scholar]
- Atkinson RW, Butland BK, Dimitroulopoulou C, Heal MR, Stedman JR, Carslaw N, Jarvis D, Heaviside C, Vardoulakis S, Walton H, Anderson HR. Long-term exposure to ambient ozone and mortality: a quantitative systematic review and meta-analysis of evidence from cohort studies. BMJ Open. 2016;6:e009493. doi: 10.1136/bmjopen-2015-009493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babatola SS. Global burden of diseases attributable to air pollution. J Public Health Afr. 2018;9:813. doi: 10.4081/jphia.2018.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai N, Kido T, Suzuki H, Yang G, Kavanagh TJ, Kaufman JD, Rosenfeld ME, van Breemen C, Eeden SF. Changes in atherosclerotic plaques induced by inhalation of diesel exhaust. Atherosclerosis. 2011;216:299–306. doi: 10.1016/j.atherosclerosis.2011.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bai L, Weichenthal S, Kwong JC, Burnett RT, Hatzopoulou M, Jerrett M, van Donkelaar A, Martin RV, Van Ryswyk K, Lu H, Kopp A, Chen H. Associations of long-term exposure to ultrafine particles and nitrogen dioxide with increased incidence of congestive heart failure and acute myocardial infarction. Am J Epidemiol. 2019;188:151–159. doi: 10.1093/aje/kwy194. [DOI] [PubMed] [Google Scholar]
- Bai L, Shin S, Burnett RT, Kwong JC, Hystad P, van Donkelaar A, Goldberg MS, Lavigne E, Copes R, Martin RV, Kopp A, Chen H. Exposure to ambient air pollution and the incidence of congestive heart failure and acute myocardial infarction: a population-based study of 5.1 million Canadian adults living in Ontario. Environ Int. 2019;132:105004. doi: 10.1016/j.envint.2019.105004. [DOI] [PubMed] [Google Scholar]
- Barbosa CM, Terra-Filho M, de Albuquerque AL, Di Giorgi D, Grupi C, Negrão CE, Rondon MU, Martinez DG, Marcourakis T, dos Santos FA, Braga AL, Zanetta DM, Santos Ude P. Burnt sugarcane harvesting – cardiovascular effects on a group of healthy workers. Brazil Plos One. 2012;7:e46142. doi: 10.1371/journal.pone.0046142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beelen R, Raaschou-Nielsen O, Stafoggia M, et al. Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet. 2014;383:785–795. doi: 10.1016/S0140-6736(13)62158-3. [DOI] [PubMed] [Google Scholar]
- Billionnet C, Sherrill D, Annesi-Maesano I. Estimating the health effects of exposure to multi-pollutant mixture. Ann Epidemiol. 2012;22:126–141. doi: 10.1016/j.annepidem.2011.11.004. [DOI] [PubMed] [Google Scholar]
- Boroujeni M, Saberian M, Li J. Environmental impacts of COVID-19 on Victoria, Australia, witnessed two waves of Coronavirus. Environ Sci Pollut Res Int. 2021;28(11):14182–14191. doi: 10.1007/s11356-021-12556-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourdrel T, Bind MA, Béjot Y, Morel O, Argacha JF. Cardiovascular effects of air pollution. Arch Cardiovasc Dis. 2017;110:634–642. doi: 10.1016/j.acvd.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourdrel T, Annesi-Maesano I, Alahmad B, Maesano CN, Bind MA. The impact of outdoor air pollution on COVID-19: a review of evidence from in vitro, animal, and human studies. Eur Respir Rev. 2021;30(159):200242. doi: 10.1183/16000617.0242-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs D. Environmental pollution and the global burden of disease. Br Med Bull. 2003;68:1–24. doi: 10.1093/bmb/ldg019. [DOI] [PubMed] [Google Scholar]
- Brook RD, Rajagopalan S, Pope CA, III, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC, Jr, Whitsel L, Kaufman JD. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- Buteau S, Goldberg MS. A structured review of panel studies used to investigate associations between ambient air pollution and heart rate variability. Environ Res. 2016;148:207–247. doi: 10.1016/j.envres.2016.03.013. [DOI] [PubMed] [Google Scholar]
- Cai Y, Zhang B, Ke W, Feng B, Lin H, Xiao J, Zeng W, Li X, Tao J, Yang Z, Ma W, Liu T. Associations of short-term and long-term exposure to ambient air pollutants with hypertension. Hypertension. 2016;68:62–70. doi: 10.1161/HYPERTENSIONAHA.116.07218. [DOI] [PubMed] [Google Scholar]
- Cesaroni G, Forastiere F, Stafoggia M, Andersen ZJ, Badaloni C, Beelen R, Caracciolo B, de Faire U, Erbel R, Eriksen KT, Fratiglioni L, Galassi C, Hampel R, Heier M, Hennig F, Hilding A, Hoffmann B, Houthuijs D, Jöckel KH, Korek M, Lanki T, Leander K, Magnusson PK, Migliore E, Ostenson CG, Overvad K, Pedersen NL, Juha Pekkanen J, Penell J, Pershagen G, Pyko A, Raaschou-Nielsen O, Ranzi A, Ricceri F, Sacerdote C, Salomaa V, Swart W, Turunen AW, Vineis P, Weinmayr G, Wolf K, de Hoogh K, Hoek G, Brunekreef B, Peters A. Long term exposure to ambient air pollution and incidence of acute coronary events: prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ. 2014;348:f7412. doi: 10.1136/bmj.f7412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrabarty RK, Beeler P, Liu P, Goswami S, Harvey RD, Pervez S, van Donkelaar A, Martin RV. Ambient PM2.5 exposure and rapid spread of COVID-19 in the United States. Sci Total Environ. 2021;760:143391. doi: 10.1016/j.scitotenv.2020.143391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen SY, Wu CF, Lee JH, Hoffmann B, Peters A, Brunekreef B, Chu DC, Chan CC. Associations between long-term air pollutant exposures and blood pressure in elderly residents of taipei city: a cross-sectional study. Environ Health Perspect. 2015;123:779–784. doi: 10.1289/ehp.1408771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen B, Jia P, Han J. Role of indoor aerosols for COVID-19 viral transmission: a review. Environ Chem Lett. 2021;2021:1–18. doi: 10.1007/s10311-020-01174-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin MT. Basic mechanisms for adverse cardiovascular events associated with air pollution. Heart. 2015;101:253–256. doi: 10.1136/heartjnl-2014-306379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang KJ, Yan YH, Chiu SY, Cheng TJ. Long-term air pollution exposure and risk factors for cardiovascular diseases among the elderly in Taiwan. Occup Environ Med. 2011;68:64–68. doi: 10.1136/oem.2009.052704. [DOI] [PubMed] [Google Scholar]
- Coogan PF, White LF, Yu J, Brook RD, Burnett RT, Marshall JD, Bethea TN, Rosenberg L, Jerrett M. Long-term exposure to NO2 and ozone and hypertension incidence in the black women’s health study. Am J Hypertens. 2017;30:367–372. doi: 10.1093/ajh/hpw168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouse DL, Peters PA, van Donkelaar A, Goldberg MS, Villeneuve PJ, Brion O, Khan S, Atari DO, Jerrett M, Pope CA, Brauer M, Brook JR, Martin RV, Stieb D, Burnett RT. Risk of nonaccidental and cardiovascular mortality in relation to long-term exposure to low concentrations of fine particulate matter: a Canadian national-level cohort study. Environ Health Perspect. 2012;120:708–714. doi: 10.1289/ehp.1104049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dadvand P, Nieuwenhuijsen MJ, Agustí À, de Batlle J, Benet M, Beelen R, Cirach M, Martinez D, Hoek G, Basagana X, Ferrer A, Ferrer J, Rodriguez-Roisin R, Sauleda J, Guerra S, Antó JM, Garcia-Aymerich J. Air pollution and biomarkers of systemic inflammation and tissue repair in COPD patients. Eur Respir J. 2014;44:603–613. doi: 10.1183/09031936.00168813. [DOI] [PubMed] [Google Scholar]
- Danesh Yazdi M, Wang Y, Di Q, Zanobetti A, Schwartz J. Long-term exposure to PM2.5 and ozone and hospital admissions of Medicare participants in the Southeast USA. Environ Int. 2019;130:104879. doi: 10.1016/j.envint.2019.05.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Brouwere K, Buekers J, Cornelis C, Schlekat CE, Oller AR. Assessment of indirect human exposure to environmental sources of nickel: oral exposure and risk characterization for systemic effects. Sci Total Environ. 2012;419:25–36. doi: 10.1016/j.scitotenv.2011.12.049. [DOI] [PubMed] [Google Scholar]
- Dong GH, Qian ZM, Xaverius PK, Trevathan E, Maalouf S, Parker J, Yang L, Liu MM, Wang D, Ren WH, Ma W, Wang J, Zelicoff A, Fu Q, Simckes M. Association between long-term air pollution and increased blood pressure and hypertension in China. Hypertension. 2013;61:578–584. doi: 10.1161/HYPERTENSIONAHA.111.00003. [DOI] [PubMed] [Google Scholar]
- Dorans KS, Wilker EH, Li W, Rice MB, Ljungman PL, Schwartz J, Coull BA, Kloog I, Koutrakis P, D’Agostino RB, Sr, Massaro JM, Hoffmann U, O’Donnell CJ, Mittleman MA. Residential proximity to major roads, exposure to fine particulate matter, and coronary artery calcium: the Framingham heart study. Arterioscler Thromb Vasc Biol. 2016;36:1679–1685. doi: 10.1161/ATVBAHA.116.307141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutta D, Arya S, Kumar S, Lichtfouse E. Electronic waste pollution and the COVID-19 pandemic. Environ Chem Lett. 2021;2021:1–4. doi: 10.1007/s10311-021-01286-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faustini A, Rapp R, Forastiere F. Nitrogen dioxide and mortality: review and meta-analysis of long-term studies. Eur Respir J. 2014;44:744–753. doi: 10.1183/09031936.00114713. [DOI] [PubMed] [Google Scholar]
- Franklin BA, Brook R, Pope CA., III Air pollution and cardiovascular disease. Curr Probl Cardiol. 2015;40:207–238. doi: 10.1016/j.cpcardiol.2015.01.003. [DOI] [PubMed] [Google Scholar]
- Fuks KB, Weinmayr G, Foraster M, Dratva J, Hampel R, Houthuijs D, Oftedal B, Oudin A, Panasevich S, Penell J, Sommar JN, Sorensen M, Tiittanen P, Wolf K, Xun WW, Aguilera I, Basagana X, Beelen R, Bots ML, Brunekreef B, Bueno-de-Mesquita HB, Caracciolo B, Cirach M, de Faire U, de Nazelle A, Eeftens M, Elosua R, Erbel R, Forsberg B, Fratiglioni L, Gaspoz JM, Hilding A, Jula A, Korek M, Krämer U, Künzli N, Lanki T, Leander K, Magnusson PK, Marrugat J, Nieuwenhuijsen MJ, Ostenson CG, Pedersen NL, Pershagen G, Phuleria HC, Probst-Hensch NM, Raaschou-Nielsen O, Schaffner E, Schikowski T, Schindler C, Schwarze PE, Sogaard AJ, Sugiri D, Swart WJ, Tsai MY, Turunen AW, Vineis P, Peters A, Hoffmann B. Arterial blood pressure and long-term exposure to traffic-related air pollution: an analysis in the European study of cohorts for air pollution effects (ESCAPE) Environ Health Perspect. 2014;122:896–905. doi: 10.1289/ehp.1307725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuks KB, Weinmayr G, Basagana X, Gruzieva O, Hampel R, Oftedal B, Sorensen M, Wolf K, Aamodt G, Aasvang GM, Aguilera I, Becker T, Beelen R, Brunekreef B, Caracciolo B, Cyrys J, Elosua R, Eriksen KT, Foraster M, Fratiglioni L, Hilding A, Houthuijs D, Korek M, Künzli N, Marrugat J, Nieuwenhuijsen M, Östenson CG, Penell J, Pershagen G, Raaschou-Nielsen O, WJR S, Peters A, Hoffmann B (2017) Long-term exposure to ambient air pollution and traffic noise and incident hypertension in seven cohorts of the European study of cohorts for air pollution effects (ESCAPE). Eur Heart J 38:983–990. 10.1093/eurheartj/ehw413 [DOI] [PubMed]
- Ghio AJ, Kim C, Devlin RB. Concentrated ambient air particles induce mild pulmonary inflammation in healthy human volunteers. Am J Respir Crit Care Med. 2000;162:918–981. doi: 10.1164/ajrccm.162.3.9911115. [DOI] [PubMed] [Google Scholar]
- Gorrasi G, Sorrentino A, Lichtfouse E. Back to plastic pollution in COVID times. Environ Chem Lett. 2020;2020:1–4. doi: 10.1007/s10311-020-01129-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray DL, Wallace LA, Brinkman MC, Buehler SS, La Londe C. Respiratory and cardiovascular effects of metals in ambient particulate matter: a critical review. Rev Environ Contam Toxicol. 2015;234:135–203. doi: 10.1007/978-3-319-10638-0-3. [DOI] [PubMed] [Google Scholar]
- Ha MH, Lee DH, Jacobs DR. Association between serum concentrations of persistent organic pollutants and self-reported cardiovascular disease prevalence: results from the national health and nutrition examination survey, 1999–2002. Environ Health Perspect. 2007;115:1204–1209. doi: 10.1289/ehp.10184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamanaka RB, Mutlu GM. Particulate matter air pollution: effects on the cardiovascular system. Front Endocrinol. 2018;9:680. doi: 10.3389/fendo.2018.00680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han J, Zhang X, He S, Jia P. Can the coronavirus disease be transmitted from food? A review of evidence, risks, policies and knowledge gaps. Environ Chem Lett. 2020;2020:1–12. doi: 10.1007/s10311-020-01101-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Canada. Human health risk assessment for coarse particulate matter (2016) https://www.canada.ca/en/health-canada/services/publications/healthy-living/human-health-risk-assessment-coarse-particulate-matter-executive-summary.html
- Hoek G, Krishnan RM, Beelen R, Peters A, Ostro B, Brunekreef B, Kaufman JD. Long-term air pollution exposure and cardio-respiratory mortality: a review. Environ Health. 2013;12:43. doi: 10.1186/1476-069X-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann B, Moebus S, Möhlenkamp S, Stang A, Lehmann N, Dragano N, Schmermund A, Memmesheimer M, Mann K, Erbel R, Jöckel KH, Heinz Nixdorf Recall Study Investigative Group (2007) Residential exposure to traffic is associated with coronary atherosclerosis. Circulation 116:489–496. 10.1161/CIRCULATIONAHA.107.693622 [DOI] [PubMed]
- Huang K, Yang X, Liang F, Liu F, Li J, Xiao Q, Chen J, Liu X, Cao J, Shen C, Yu L, Lu F, Wu X, Zhao L, Wu X, Li Y, Hu D, Huang J, Liu Y, Lu X, Gu D. Long-term exposure to fine particulate matter and hypertension incidence in China. Hypertension. 2019;73:1195–1201. doi: 10.1161/HYPERTENSIONAHA.119.12666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerrett M, Burnett RT, Pope CA, III, Ito K, Thurston G, Krewski D, Shi Y, Calle E, Thun M. Long-term ozone exposure and mortality. N Engl J Med. 2009;360:1085–1095. doi: 10.1056/NEJMoa0803894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang XQ, Mei XD, Feng D. Air pollution and chronic airway diseases: what should people know and do? J Thorac Dis. 2016;8:E31–E40. doi: 10.3978/j.issn.2072-1439.2015.11.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kälsch H, Hennig F, Moebus S, Möhlenkamp S, Dragano N, Jakobs H, Memmesheimer M, Erbel R, Jöckel KH, Hoffmann B. Are air pollution and traffic noise independently associated with atherosclerosis: the Heinz Nixdorf recall study. Eur Heart J. 2014;35:853–860. doi: 10.1093/eurheartj/eht426. [DOI] [PubMed] [Google Scholar]
- Kaufman JD, Adar SD, Barr RG, Budoff M, Burke GL, Curl CL, Daviglus ML, Diez Roux AV, Gassett AJ, Jacobs DR, Jr, Kronmal R, Larson TV, Navas-Acien A, Olives C, Sampson PD, Sheppard L, Siscovick DS, Stein JH, Szpiro AA, Watson KE. Association between air pollution and coronary artery calcification within six metropolitan areas in the USA (the Multi-Ethnic Study of Atherosclerosis and Air Pollution): a longitudinal cohort study. Lancet. 2016;388:696–704. doi: 10.1016/S0140-6736(16)00378-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan AH, Tirth V, Fawzy M, Mahmoud AED, Khan NA, Ahmed S, Ali SS, Akram M, Hameed L, Islam S, Das G, Roy S, Dehghani MH. COVID-19 transmission, vulnerability, persistence and nanotherapy: a review. Environ Chem Lett. 2021;2021:1–15. doi: 10.1007/s10311-021-01229-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim SY, Sheppard L, Kaufman JD, Bergen S, Szpiro AA, Larson TV, Adar SD, Diez Roux AV, Polak JF, Vedal S. Individual-level concentrations of fine particulate matter chemical components and subclinical atherosclerosis: a cross-sectional analysis based on 2 advanced exposure prediction models in the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2014;180:718–728. doi: 10.1093/aje/kwu186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, Kim J, Kim S, Kang SH, Kim HJ, Kim H, Heo J, Yi SM, Kim K, Youn TJ, Chae IH. Cardiovascular effects of long-term exposure to air pollution: a population-based study with 900 845 person-years of follow-up. J Am Heart Assoc. 2017;6:e007170. doi: 10.1161/JAHA.117.007170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim IS, Yang PS, Lee J, Yu HT, Kim TH, Uhm JS, Pak HN, Lee MH, Joung B. Long-term exposure of fine particulate matter air pollution and incident atrial fibrillation in the general population: a nationwide cohort study. Int J Cardiol. 2019;283:178–183. doi: 10.1016/j.ijcard.2018.12.048. [DOI] [PubMed] [Google Scholar]
- Kioumourtzoglou MA, Schwartz J, James P, Dominici F, Zanobetti A. PM2.5 and mortality in 207 US Cities: modification by temperature and city characteristics. Epidemiology. 2016;27:221–227. doi: 10.1097/EDE.0000000000000422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konduracka E. A link between environmental pollution and civilization disorders: a mini review. Rev Environ Health. 2019;34:227–233. doi: 10.1515/reveh-2018-0083. [DOI] [PubMed] [Google Scholar]
- Konduracka E, Rostoff P (2021) Relationships Between Outdoor Ambient Air Pollution and Cardiovascular Disorders. In: Morin-Crini N, Lichtfouse E, Crini G (eds). Emerging Contaminants, Occurrence and Impact. 1:261–305. Cham: Springer International Publishing. 10.1007/978-3-030-69079-3_5
- Kwon OK, Kim SH, Kang SH, Cho Y, Oh IY, Yoon CH, Kim SY, Kim OJ, Choi EK, Youn TJ, Chae IH. Association of short- and long-term exposure to air pollution with atrial fibrillation. Eur J Prev Cardiol. 2019;26:1208–1216. doi: 10.1177/2047487319835984. [DOI] [PubMed] [Google Scholar]
- Li H, Cai J, Chen R, Zhao Z, Ying Z, Wang L, Chen J, Hao K, Kinney PL, Chen H, Kan H. Particulate matter exposure and stress hormone levels: a randomized, double-blind, crossover trial of air purification. Circulation. 2017;136:618–627. doi: 10.1161/CIRCULATIONAHA.116.026796. [DOI] [PubMed] [Google Scholar]
- Li J, Zhou C, Xu H, Brook RD, Liu S, Yi T, Wang Y, Feng B, Zhao M, Wang X, Zhao Q, Chen J, Song X, Wang T, Liu S, Zhang Y, Wu R, Gao J, Pan B, Pennathur S, Rajagopalan S, Huo Y, Zheng L, Huang W. Ambient air pollution is associated with HDL (high-density lipoprotein) dysfunction in healthy adults. Arterioscler Thromb Vasc Biol. 2019;39:513–522. doi: 10.1161/ATVBAHA.118.311749. [DOI] [PubMed] [Google Scholar]
- Li H, Huang K, Fu Q, Lin Y, Chen J, Deng C, Tian X, Tang Q, Song Q, Wei Z. Airborne black carbon variations during the COVID-19 lockdown in the Yangtze River Delta megacities suggest actions to curb global warming. Environ Chem Lett. 2021;2021:1–10. doi: 10.1007/s10311-021-01327-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z, Yu S, Li M, Chen X, Zhang Y, Li J, Jiang Y, Liu W, Li P, Lichtfouse E. Non-stop industries were the main source of air pollution during the 2020 coronavirus lockdown in the North China Plain. Environ Chem Lett. 2021;2021:1–11. doi: 10.1007/s10311-021-01314-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang D, Shi L, Zhao J, Liu P, Sarnat JA, Gao S, Schwartz J, Liu Y, Ebelt ST, Scovronick N, Chang HH. Urban Air Pollution May Enhance COVID-19 Case-Fatality and Mortality Rates in the United States. Innovation (n y) 2020;1(3):100047. doi: 10.1016/j.xinn.2020.100047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim YH, Jorgensen JT, So R, Cole-Hunter T, Mehta AJ, Amini H, Bräuner EV, Westendorp RGJ, Liu S, Mortensen LH, Hoffmann B, Loft S, Ketzel M, Hertel O, Brandt J, Jensen SS, Backalarz C, Simonsen MK, Tasic N, Maric M, Andersen ZJ. Long-Term Exposure to Air Pollution, Road Traffic Noise, and Heart Failure Incidence: The Danish Nurse Cohort. J Am Heart Assoc. 2021;10:e021436. doi: 10.1161/JAHA.121.021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lind L, Lind PM. Can persistent organic pollutants and plastic-associated chemicals cause cardiovascular disease? J Intern Med. 2012;271:537–553. doi: 10.1111/j.1365-2796.2012.02536. [DOI] [PubMed] [Google Scholar]
- Liu C, Chen R, Zhao Y, Ma Z, Bi J, Liu Y, Meng X, Wang Y, Chen X, Li W, Kan H. Associations between ambient fine particulate air pollution and hypertension: a nationwide cross-sectional study in China. Sci Total Environ. 2017;584–585:869–874. doi: 10.1016/j.scitotenv.2017.01.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C, Yin P, Chen R, Meng X, Wang L, Niu Y, Lin Z, Liu Y, Liu J, Qi J, You J, Kan H, Zhou M. Ambient carbon monoxide and cardiovascular mortality: a nationwide time-series analysis in 272 cities in China. Lancet Planet Health. 2018;2:e12–e18. doi: 10.1016/S2542-5196(17)30181. [DOI] [PubMed] [Google Scholar]
- Ljungman PLS, Andersson N, Stockfelt L, Andersson EM, Nilsson Sommar J, Eneroth K, Gidhagen L, Johansson C, Lager A, Leander K, Molnar P, Pedersen NL, Rizzuto D, Rosengren A, Segersson D, Wennberg P, Barregard L, Forsberg B, Sallsten G, Bellander T, Pershagen G. Long-term exposure to particulate air pollution, black carbon, and their source components in relation to ischemic heart disease and stroke. Environ Health Perspect. 2019;127:107012. doi: 10.1289/EHP4757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Campos JL, Marquez-Martin E, Soriano JB. The role of air pollution in COPD and implications for therapy. Expert Rev Respir Med. 2016;10:849–859. doi: 10.1080/17476348.2016.1191356. [DOI] [PubMed] [Google Scholar]
- Miller MR, Newby DE. Air pollution and cardiovascular disease: car sick. Cardiovasc Res. 2020;116:279–294. doi: 10.1093/cvr/cvz228. [DOI] [PubMed] [Google Scholar]
- Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, Kaufman JD. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. 2007;356:447–458. doi: 10.1056/NEJMoa054409. [DOI] [PubMed] [Google Scholar]
- Min JY, Cho JS, Lee KJ, Park JB, Park SG, Kim JY, Min KB. Potential role for organochlorine pesticides in the prevalence of peripheral arterial diseases in obese persons: results from the national health and nutrition examination survey 1999–2004. Atherosclerosis. 2011;218:200–206. doi: 10.1016/j.atherosclerosis.2011.04.044. [DOI] [PubMed] [Google Scholar]
- Monrad M, Sajadieh A, Christensen JS, Ketzel M, Raaschou-Nielsen O, Tjonneland A, Overvad K, Loft S, Sorensen M. Long-Term Exposure to Traffic-Related Air Pollution and Risk of Incident Atrial Fibrillation: A Cohort Study. Environ Health Perspect. 2017;125:422–427. doi: 10.1289/EHP392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby DE, Mannucci PM, Tell GS, Baccarelli AA, Brook RD, Donaldson K, Forastiere F, Franchini M, Franco OH, Graham I, Hoek G, Hoffmann B, Hoylaerts MF, Künzli N, Mills N, Pekkanen J, Peters A, Piepoli MF, Rajagopalan S, Storey RF. Expert position paper on air pollution and cardiovascular disease. Eur Heart J. 2015;36:83–93. doi: 10.1093/eurheartj/ehu458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novotna B, Topinka J, Solansky I, Chvatalova I, Lnenickova Z, Sram RJ. Impact of air pollution and genotype variability on DNA damage in Prague policemen. Toxicol Lett. 2007;172:37–47. doi: 10.1016/j.toxlet.2007.05.013. [DOI] [PubMed] [Google Scholar]
- Ohlwein S, Kappeler R, Kutlar Joss M, Kunzli N, Hoffmann B. Health effects of ultrafine particles: a systematic literature review update of epidemiological evidence. Int J Public Health. 2019;64:547–559. doi: 10.1007/s00038-019-01202-7. [DOI] [PubMed] [Google Scholar]
- Paital B, Agrawal PK. Air pollution by NO2 and PM2.5 explains COVID-19 infection severity by overexpression of angiotensin-converting enzyme 2 in respiratory cells: a review. Environ Chem Lett. 2020;2020:1–18. doi: 10.1007/s10311-020-01091-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parczewski M, Ciechanowicz A. Molecular epidemiology of SARS-CoV-2: a review of current data on genetic variability of the virus. Pol Arch Intern Med. 2020;131(1):63–69. doi: 10.20452/pamw.15550. [DOI] [PubMed] [Google Scholar]
- Pascal M, Corso M, Chanel O, Declercq C, Badaloni C, Cesaroni G, Henschel S, Meister K, Haluza D, Martin-Olmedo P, Medina S, Aphekom group (2013) Assessing the public health impacts of urban air pollution in 25 European cities: results of the Aphekom project. Sci Total Environ 449:390–400. 10.1016/j.scitotenv.2013.01.077 [DOI] [PubMed]
- Perez L, Wolf K, Hennig F, Penell J, Basagaña X, Foraster M, Aguilera I, Agis D, Beelen R, Brunekreef B, Cyrys J, Fuks KB, Adam M, Baldassarre D, Cirach M, Elosua R, Dratva J, Hampel R, Koenig W, Marrugat J, de Faire U, Pershagen G, Probst-Hensch NM, de Nazelle A, Nieuwenhuijsen MJ, Rathmann W, Rivera M, Seissler J, Schindler C, Thiery J, Hoffmann B, Peters A, Künzli N. Air pollution and atherosclerosis: a cross-sectional analysis of four European cohort studies in the ESCAPE study. Environ Health Perspect. 2015;123:597–605. doi: 10.1289/ehp.1307711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinault LL, Weichenthal S, Crouse DL, Brauer M, Erickson A, Donkelaar AV, Martin RV, Hystad P, Chen H, Finès P, Brook JR, Tjepkema M, Burnett RT. Associations between fine particulate matter and mortality in the 2001 Canadian census health and environment cohort. Environ Res. 2017;159:406–415. doi: 10.1016/j.envres.2017.08.037. [DOI] [PubMed] [Google Scholar]
- Pitchika A, Hampel R, Wolf K, Kraus U, Cyrys J, Babisch W, Peters A, Schneider A. Long-term associations of modeled and self-reported measures of exposure to air pollution and noise at residence on prevalent hypertension and blood pressure. Sci Total Environ. 2017;593–594:337–346. doi: 10.1016/j.scitotenv.2017.03.156. [DOI] [PubMed] [Google Scholar]
- Pope CA, III, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, Godleski JJ. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation. 2004;109:71–77. doi: 10.1161/01.CIR.0000108927.80044.7F. [DOI] [PubMed] [Google Scholar]
- Pun VC, Kabrhel C, Camargo CA, Jr, Baccarelli AA, Laden F. Prospective study of ambient particulate matter exposure and risk of pulmonary embolism in the nurses’ health study cohort. Environ Health Perspect. 2015;123:1265–1270. doi: 10.1289/ehp.1408927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajagopalan S, Al-Kindi SG, Brook RD. Air pollution and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2018;72:2054–2070. doi: 10.1016/j.jacc.2018.07.099. [DOI] [PubMed] [Google Scholar]
- Rich DQ, Kipen HM, Huang W, Wang G, Wang Y, Zhu P, Ohman-Strickland P, Hu M, Philipp C, Diehl SR, Lu SE, Tong J, Gong J, Thomas D, Zhu T, Zhang JJ. Association between changes in air pollution levels during the Beijing Olympics and biomarkers of inflammation and thrombosis in healthy young adults. JAMA. 2012;307:2068–2078. doi: 10.1001/jama.2012.3488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson S, Miller MR. Ambient air pollution and thrombosis. Part Fibre Toxicol. 2018;15:1. doi: 10.1186/s12989-017-0237-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodins V, Lucht S, Ohlwein S, Hennig F, Soppa V, Erbel R, Jöckel KH, Weimar C, Hermann DM, Schramm S, Moebus S, Slomiany U, Hoffmann B. Long-term exposure to ambient source-specific particulate matter and its components and incidence of cardiovascular events – the Heinz Nixdorf recall study. Environ Int. 2020;142:105854. doi: 10.1016/j.envint.2020.105854. [DOI] [PubMed] [Google Scholar]
- Rodopoulou S, Stafoggia M, Chen J, de Hoogh K, Bauwelinck M, Mehta AJ, Klompmaker JO, Oftedal B, Vienneau D, Janssen NAH, Strak M, Andersen ZJ, Renzi M, Cesaroni G, Nordheim CF, Bekkevold T, Atkinson R, Forastiere F, Katsouyanni K, Brunekreef B, Samoli E, Hoek G. Long-term exposure to fine particle elemental components and mortality in Europe: Results from six European administrative cohorts within the ELAPSE project. Sci Total Environ. 2021;809:152205. doi: 10.1016/j.scitotenv.2021.152205. [DOI] [PubMed] [Google Scholar]
- Rossner P, Jr, Svecova V, Milcova A, Lnenickova Z, Solansky I, Santella RM, Sram RJ. Oxidative and nitrosative stress markers in bus drivers. Mutat Res. 2007;617:23–32. doi: 10.1016/j.mrfmmm.2006.11.033. [DOI] [PubMed] [Google Scholar]
- Roviello V, Roviello GN. Lower COVID-19 mortality in Italian forested areas suggests immunoprotection by Mediterranean plants. Environ Chem Lett. 2020;2020:1–12. doi: 10.1007/s10311-020-01063-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samek L, Stegowski Z, Styszko K, Furman L, Zimnoch M, Skiba A, Kistler M, Kasper-Giebl A, Rożański K, Konduracka E. Seasonal variations of chemical composition of PM2.5 fraction in the urban area of Krakow, Poland: PMF source attribution. Air Quality Atmosphere Health. 2020;13:89–96. doi: 10.1007/s11869-019-00773-x. [DOI] [Google Scholar]
- Sangani RG, Soukup JM, Ghio AJ. Metals in air pollution particles decrease whole-blood coagulation time. Inhal Toxicol. 2010;22:621–626. doi: 10.3109/08958371003599037. [DOI] [PubMed] [Google Scholar]
- Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, Palmisani J, Di Gilio A, Torboli V, Fontana F, Clemente L, Pallavicini A, Ruscio M, Piscitelli P, Miani A. SARS-Cov-2RNA found on particulate matter of Bergamo in Northern Italy: first evidence. Environ Res. 2020;188:109754. doi: 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin S, Burnett RT, Kwong JC, Hystad P, van Donkelaar A, Brook JR, Goldberg MS, Tu K, Copes R, Martin RV, Liu Y, Kopp A, Chen H. Ambient air pollution and the risk of atrial fibrillation and stroke: a population-based cohort study. Environ Health Perspect. 2019;127:87009. doi: 10.1289/EHP4883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Signorelli SS, Oliveri Conti G, Zanobetti A, Baccarelli A, Fiore M, Ferrante M. Effect of particulate matter-bound metals exposure on prothrombotic biomarkers: a systematic review. Environ Res. 2019;177:108573. doi: 10.1016/j.envres.2019.108573. [DOI] [PubMed] [Google Scholar]
- Sławiński G, Lewicka E (2020) What should a cardiologist know about coronavirus disease 2019?. Kardiol Pol 24 78(4):278–283. 10.33963/KP.15302 [DOI] [PubMed]
- Sorensen M, Hoffmann B, Hvidberg M, Ketzel M, Jensen SS, Andersen ZJ, Tjønneland A, Overvad K, Raaschou-Nielsen O. Long-term exposure to traffic-related air pollution associated with blood pressure and self-reported hypertension in a Danish cohort. Health Perspect. 2012;120:418–424. doi: 10.1289/ehp.1103631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanković A, Bogdanović D, Nikolić M, Anđelković Apostolović M. Does short-term air pollution exposure have effects on blood pressure and heart rate in healthy women in the city of Niš, Serbia? Cent Eur J Public Health. 2018;26:310–315. doi: 10.21101/cejph.a5104. [DOI] [PubMed] [Google Scholar]
- Stieb DM, Evans GJ, To TM, Brook JR, Burnett RT. An ecological analysis of long-term exposure to PM2.5 and incidence of COVID-19 in Canadian health regions. Environ Res. 2020;191:110052. doi: 10.1016/j.envres.2020.110052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun Q, Wang A, Jin X, Natanzon A, Duquaine D, Brook RD, Aguinaldo JG, Fayad ZA, Fuster V, Lippmann M, Chen LC, Rajagopalan S. Long-term air pollution exposure and acceleration of atherosclerosis and vascular inflammation in an animal model. JAMA. 2005;294:3003–3010. doi: 10.1001/jama.294.23.3003. [DOI] [PubMed] [Google Scholar]
- Tang L, Wang QY, Cheng ZP, Hu B, Liu JD, Hu Y. Air pollution and venous thrombosis: a meta-analysis. Sci Rep. 2016;6:32794. doi: 10.1038/srep32794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarantini L, Bonzini M, Tripodi A, Angelici L, Nordio F, Cantone L, Apostoli P, Bertazzi PA, Baccarelli AA. Blood hypomethylation of inflammatory genes mediates the effects of metal-rich airborne pollutants on blood coagulation. Occup Environ Med. 2013;70:418–425. doi: 10.1136/oemed-2012-101079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terzano C, Di Stefano F, Conti V, Graziani E, Petroianni A. Air pollution ultrafine particles: toxicity beyond the lung. Eur Rev Med Pharmacol Sci. 2010;14:809–821. [PubMed] [Google Scholar]
- Thurston GD, Ahn J, Cromar KR, Shao Y, Reynolds HR, Jerrett M, Lim CC, Shanley R, Park Y, Hayes RB. Ambient particulate matter air pollution exposure and mortality in the NIH-AARP Diet and Health cohort. Environ Health Perspect. 2016;124:484–490. doi: 10.1289/ehp.1509676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinkov AA, Filippini T, Ajsuvakova OP, Skalnaya MG, Aaseth J, Bjørklund G, Gatiatulina ER, Popova EV, Nemereshina ON, Huang PT, Vinceti M, Skalny AV. Cadmium and atherosclerosis: a review of toxicological mechanisms and a meta-analysis of epidemiologic studies. Environ Res. 2018;162:240–260. doi: 10.1016/j.envres.2018.01.008. [DOI] [PubMed] [Google Scholar]
- Tonne C, Yanosky JD, Beevers S, Wilkinson P, Kelly FJ. PM mass concentration and PM oxidative potential in relation to carotid intima-media thickness. Epidemiology. 2012;23:486–494. doi: 10.1097/EDE.0b013e31824e613e. [DOI] [PubMed] [Google Scholar]
- Tsai SS, Chiu HF, Wu TN, Yang CY. Air pollution and emergency room visits for cardiac arrhythmia in a subtropical city: Taipei. Taiwan Inhal Toxicol. 2009;21:1113–1118. doi: 10.3109/08958370902758939. [DOI] [PubMed] [Google Scholar]
- Turner MC, Jerrett M, Pope CA, III, Krewski D, Gapstur SM, Diver WR, Beckerman BS, Marshall JD, Su J, Crouse DL, Burnett RT. Long-term ozone exposure and mortality in a large prospective study. Am J Respir Crit Care Med. 2016;193:1134–1142. doi: 10.1164/rccm.201508-1633OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. EPA. Integrated Science Assessment (ISA) for Oxides of Nitrogen – Health Criteria (2016). U.S. Environmental Protection Agency, Washington, DC, EPA/600/R-15/068
- U.S. EPA. Integrated Science Assessment (ISA) for Ozone and Related Photochemical Oxidants (2020). U.S. Environmental Protection Agency, Washington, DC, EPA/600/R-20/012
- U.S. EPA. Integrated Science Assessment (ISA) for Particulate Matter (2019). U.S. Environmental Protection Agency, Washington, DC, EPA/600/R-19/188 [PubMed]
- U.S. EPA. Supplement to the 2019 Integrated Science Assessment for Particulate Matter (2021). U.S. Environmental Protection Agency, Washington, DC, EPA/600/R-21/198 [PubMed]
- Ufnalska S, Lichtfouse E. Unanswered issues related to the COVID-19 pandemic. Environ Chem Lett. 2021;2021:1–2. doi: 10.1007/s10311-021-01249-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Integrated Science Assessment for Particulate Matter (2019) United States Environment Protection Agency website. https://www.epa.gov/isa/integrated-science-assessment-isa-particulate-matter [PubMed]
- Integrated Science Assessment for Ozone and Related Photochemical Oxidants (2020) United States Environment Protection Agency website. https://www.epa.gov/isa/integrated-science-assessment-isa-ozone-and-related-photochemical-oxida
- Viehmann A, Hertel S, Fuks K, Eisele L, Moebus S, Möhlenkamp S, Nonnemacher M, Jakobs H, Erbel R, Jöckel KH, Hoffmann B. Long-term residential exposure to urban air pollution, and repeated measures of systemic blood markers of inflammation and coagulation. Occup Environ Med. 2015;72:656–663. doi: 10.1136/oemed-2014-102800. [DOI] [PubMed] [Google Scholar]
- Vinzents P, Moller P, Sorensen M, Knudsen LE, Hertel O, Jensen FP, Schibye B, Loft S. Personal exposure to ultrafine particles and oxidative DNA damage. Environ Health Perspect. 2005;113:1485–1490. doi: 10.1289/ehp.7562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q, Li C, Guo Y, Barnett AG, Tong S, Phung D, Chu C, Dear K, Wang X, Huang C. Environmental ambient temperature and blood pressure in adults: a systematic review and meta-analysis. Sci Total Environ. 2017;575:276–286. doi: 10.1016/j.scitotenv.2016.10.019. [DOI] [PubMed] [Google Scholar]
- Wang W, Zhou J, Chen M, Huang X, Xie X, Li W, Cao Q, Kan H, Xu Y, Ying Z. Exposure to concentrated ambient PM2.5 alters the composition of gut microbiota in a murine model. Part Fibre Toxicol. 2018;15:17–20. doi: 10.1186/s12989-018-0252-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Li M, Yu S, Chen X, Li Z, Zhang Y, Jiang L, Xia Y, Li J, Liu W, Li P, Lichtfouse E, Rosenfeld D, Seinfeld JH. Unexpected rise of ozone in urban and rural areas, and sulfur dioxide in rural areas during the coronavirus city lockdown in Hangzhou, China: implications for air quality. Environ Chem Lett. 2020;2020:1–11. doi: 10.1007/s10311-020-01028-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q, Han J, Chang H, Wang C, Lichtfouse E. Society organization, not pathogenic viruses, is the fundamental cause of pandemics. Environ Chem Lett. 2021;2021:1–7. doi: 10.1007/s10311-021-01346-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiebert P, Lönn M, Fremling K, Feychting M, Sjögren B, Nise G, Kauppinen T, Plato N, Gustavsson P. Occupational exposure to particles and incidence of acute myocardial infarction and other ischaemic heart disease. Occup Environ Med. 2012;69:651–657. doi: 10.1136/oemed-2011-100285. [DOI] [PubMed] [Google Scholar]
- Wolf K, Hoffmann B, Andersen ZJ, Atkinson RW, Bauwelinck M, Bellander T, Brandt J, Brunekreef B, Cesaroni G, Chen J, de Faire U, de Hoogh K, Fecht D, Forastiere F, Gulliver J, Hertel O, Hvidtfeldt UA, Janssen NAH, Jørgensen JT, Katsouyanni K, Ketzel M, Klompmaker JO, Lager A, Liu S, MacDonald CJ, Magnusson PKE, Mehta AJ, Nagel G, Oftedal B, Pedersen NL, Pershagen G, Raaschou-Nielsen O, Renzi M, Rizzuto D, Rodopoulou S, Samoli E, van der Schouw YT, Schramm S, Schwarze P, Sigsgaard T, Sørensen M, Stafoggia M, Strak M, Tjønneland A, Verschuren WMM, Vienneau D, Weinmayr G, Hoek G, Peters A, Ljungman PLS. Long-term exposure to low-level ambient air pollution and incidence of stroke and coronary heart disease: a pooled analysis of six European cohorts within the ELAPSE project. Lancet Planet Health. 2021;5:e620–e632. doi: 10.1016/S2542-5196(21)00195-9. [DOI] [PubMed] [Google Scholar]
- Wolhuter K, Arora M, Kovacic JC. Air pollution and cardiovascular disease: can the Australian bushfires and global COVID-19 pandemic of 2020 convince us to change our ways? BioEssays. 2021;43(9):e2100046. doi: 10.1002/bies.202100046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2020) Air pollution. World Health Organization. http://who.int/health-topics/air-pollution
- World Health Organization (2021a) Transmission of SARS-CoV-2: implications for infection prevention precautions. https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions. (Accessed on 28 December 2021a)
- World Health Organization (2021b) WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/?gclid=Cj0KCQiAwMP9BRCzARIsAPWTJ_Hjhep5qv-AvH0RG2ssFAeoKmTIsrq-_W1wjzQSyh0gBXo1v1aK4r4aAgNwEALw_wcB (Accessed on 28 December 2021b)
- Wu X, Nethery RC, Sabath MB, Braun D, Dominici F. Air pollution and COVID-19 mortality in the United States: strengths and limitations of an ecological regression analysis. Sci Adv. 2020 doi: 10.1126/sciadv.abd4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan S, Wang J, Jiang Q, He Z, Huang Y, Li Z, Cai L, Cao S. Long-term exposure to PM2.5 and stroke: a systematic review and meta-analysis of cohort studies. Environ Res. 2019;177:108587. doi: 10.1016/j.envres.2019.108587. [DOI] [PubMed] [Google Scholar]
- Zhang L, Nichols RG, Correll J, Murray IA, Tanaka N, Smith PB, Hubbard TD, Sebastian A, Albert I, Hatzakis E, Gonzalez FJ, Perdew GH, Patterson AD. Persistent organic pollutants modify gut microbiota-host metabolic homeostasis in mice through aryl hydrocarbon receptor activation environ. Health Perspect. 2015;123:679–688. doi: 10.1289/ehp.1409055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng S, Fu Y, Sun Y, Zhang C, Wang Y, Lichtfouse E. High resolution mapping of nighttime light and air pollutants during the COVID-19 lockdown in Wuhan. Environ Chem Lett. 2021;2021:1–9. doi: 10.1007/s10311-021-01222-x. [DOI] [PMC free article] [PubMed] [Google Scholar]