Abstract
Healthy employee sleep has critical implications for occupational safety, but the mechanisms that explain the relationships among sleep and safety-related behaviors remain unknown. We draw from Crain, Brossoit, and Fisher’s (in press) work, nonwork, and sleep (WNS) framework and Barnes’ (2012) model of sleep and self-regulation in organizations to investigate the influence of construction workers’ self-reported sleep quantity (i.e., duration) and quality (i.e., feeling well-rest upon awakening, ability to fall asleep and remain asleep) on workplace cognitive failures (i.e., lapses in attention, memory, and action at work) and subsequent workplace safety behaviors (i.e., safety compliance and safety participation) and reports of minor injuries. Construction workers from two public works agencies completed surveys at baseline, 6-months, and 12-months. Our results suggest that workers with more insomnia symptoms on average reported engaging in fewer required and voluntary safety behaviors and were at a greater risk for workplace injuries. These effects were mediated by workplace cognitive failures. In addition, workers with greater sleep insufficiency on average reported lower safety compliance, but this effect was not mediated by workplace cognitive failures. These results have implications for future workplace interventions, suggesting that organizations striving to improve safety should prioritize interventions that will reduce workers’ insomnia symptoms and improve their ability to quickly fall asleep and stay asleep throughout the night.
Keywords: sleep, safety behaviors, injuries, workplace cognitive failure, construction
Healthy employee sleep has critical implications for worker safety, as well as broader organizational and societal outcomes. Comprehensive reviews of the sleep literature suggest that people need at least seven hours of sleep per night on average to maintain adequate cognitive functioning (e.g., Watson et al., 2015). Consequently, workers who do not obtain sufficient and high-quality sleep are at a greater risk for workplace accidents and injuries (e.g., Rosekind et al., 2010; Salminen et al., 2010; Uehli et al., 2014; Watson et al., 2015), and are more likely to have a fatal occupational accident (e.g., Akerstedt, Fredlund, Gillberg, & Jansson, 2002). Notably, Leigh (2011) found that fatal and non-fatal workplace accidents cost US organizations $192 billion in 2007. At the larger societal level, Colton and Altevogt (2006) estimate that nationwide sleep problems cost hundreds of billions of dollars annually in medical (e.g., hospital and doctor visits, prescription and over-the-counter medications) and work-related (e.g., absenteeism, workplace accidents) expenses. However, a recent Centers for Disease Control and Prevention (CDC) report found that over one-third of Americans do not obtain sufficient sleep (Liu et al., 2016). In addition, approximately 30% of adults experience insomnia symptoms, which include trouble falling and/or staying asleep throughout the night (e.g., Roth, 2007).
Despite this widespread public health issue (CDC, 2015), specific occupations are likely more affected by a lack of employee sleep. Specifically, construction is one safety-sensitive industry where employee sleep is of concern. The National Institutes of Occupational Safety and Health (NIOSH) has deemed construction work to be especially high-risk for workplace accidents and injuries (NIOSH, 2017). Furthermore, the Occupational Safety and Health Administration (OSHA) reported that the fatal injury rate for the construction industry is above the national average (OSHA, 2015); the construction industry was responsible for 21% of all worker fatalities in 2015 (OSHA, 2016). In Powell and Copping’s (2010) study, construction workers obtained less than 7 hours of sleep per night, and this was associated with an increased risk of having an accident at work. Therefore, in response to calls that recommend identifying ways to improve safety in the construction industry (e.g., Gillen, 2010), we investigate the effects of construction workers’ sleep on safety behavior (i.e., safety compliance and safety participation) and minor workplace injuries to help prevent the occurrence of these accidents in the future.
Sleep quantity is defined as the amount of time someone spends asleep (e.g., Watson et al., 2015). In contrast, consistent with Litwiller, Snyder, Taylor, and Steele’s (2017) meta-analysis on sleep and work outcomes and Crain, Brossoit, and Fisher’s (in press) review, measures of sleep quality include insomnia symptoms (i.e., trouble falling or staying asleep) and sleep insufficiency (i.e., not feeling well-rested upon waking). Insomnia symptoms are regarded as the most commonly used measure of sleep quality in the occupational sciences (Litwiller et al., 2017), though researchers have also considered sleep insufficiency as an indicator of sleep quality (e.g., Buxton et al., 2012; Crain et al., 2014). Prior work has demonstrated that the correlations between sleep quantity and quality are typically small and nonsignificant, and scholars argue that sleep quantity and quality should be assessed as distinct constructs (e.g., Barnes, 2012; Crain et al., in press; Litwiller et al., 2017).
We assess three safety-specific outcomes in relation to sleep. First, safety compliance is a form of safety-specific task performance that involves following mandated workplace safety procedures and conducting one’s work in a safe manner (Neal, Griffin, & Hart, 2000); it has been defined as “the core safety activities that need to be carried out by individuals to maintain workplace safety” (Griffin & Neal, 2000, p. 349). Safety participation reflects contextual, or “extra-role”, safety performance and involves voluntarily promoting safety at work (Griffin & Neal, 2000). Griffin and Neal (2000) identify safety compliance and safety participation as the two key facets of safety performance (i.e., behavior). Minor workplace injuries (e.g., bruises, cuts, sprains) are assessed as an additional safety outcome. Finally, we examine workplace cognitive failures, which are self-reported lapses in attention, memory, and physical action in the workplace (Wallace & Chen, 2005), as a mediating variable connecting employees’ sleep and their safety-related behaviors and injuries at work.
Anticipated Contributions
This work provides theoretical contributions to the existing sleep and organizational science literatures. First, although links between sleep and workplace accidents and injuries have been well-documented (e.g., Rosekind et al., 2010; Uehli et al., 2014), research to date has not evaluated how sleep is associated with intermediary variables (e.g., workplace cognitive failure, safety behavior, minor injuries) that could lead to more serious accidents and injuries. Given well-established links between safety behavior and workplace accidents and injuries (e.g., Christian, Bradley, Wallace, & Burke, 2009), identification of intermediary variables will allow for improved design of future safety interventions. Second, we add to existing theories of sleep in the organizational sciences, including Crain and colleagues’ (in press) work, nonwork, and sleep (WNS) framework and Barnes’ (2012) self-regulation and sleep theory, by studying safety-specific work behaviors. We draw from these models by considering the effects of poor sleep on workplace cognitive failure and subsequent activities that are impacted by reductions in one’s ability to regulate behavior, including safety behavior and injuries at work. Third, organizational scholars (e.g., Barnes, 2012; Crain et al., in press; Mullins, Cortina, Drake, & Dalal, 2014) have noted the possibility that both sleep quantity and sleep quality influence workplace behavior, though past research has typically only evaluated safety outcomes in relation to either sleep quantity or quality (e.g., Shahly et al., 2012; Watson et al., 2015). Identifying which aspects of sleep are associated with safety-related behaviors and outcomes is critical, as intervention efforts can be distinct depending on whether sleep quantity or quality is being targeted. Lastly, Bergman and Jean (2016) highlighted the overrepresentation of managerial, professional, and executive workers in the industrial-organizational psychology literature, so this work instead focuses on hourly labor workers in a safety-sensitive industry.
Theoretical Rationale: Sleep, Self-Regulation, and Enduring Relationships over Time
We draw from Crain and colleagues’ (in press) theoretical framework, which identifies the underlying processes that connect the three key areas of employees’ lives; work, nonwork, and sleep (WNS). The WNS model outlines how employees’ sleep quantity and quality have an influence on attitudes, behaviors, and states at work and at home via energy and time resources. In this model, physical energy is defined as one type of human energy akin to fatigue; “individuals who obtain sufficient and adequate sleep quantity and quality are more likely to possess enough physical energy for waking physical and cognitive activities” (Crain et al., in press, p. 8). We focus on the influence of sleep quantity and quality on work behaviors related to cognitive failures and safety. Though we do not assess physical resources, there is ample evidence that fatigue acts as a mechanism in relationships between sleep and work behaviors (e.g., Crain et al., in press).
Crain and colleagues’ (in press) framework was informed by Barnes’ (2012) model, which integrates self-regulation theory with sleep literature to identify how employees’ sleep impacts the workplace. Self-regulation describes the process of navigating goal-directed activities by controlling one’s thoughts, attention, affect, and/or behavior (e.g., Barnes, 2012; Karoly, 1993). Barnes (2012) suggests that individuals who obtain less sleep and have poorer sleep quality are more likely to experience decreases in alertness and impaired attention, in addition to distortions of risk analyses (i.e., decreased sensitivity to potential loss and engagement in risky decisions) and increases in delay discounting (i.e., impulsively selecting behaviors that result in immediate payoffs rather than behaviors that result in later payoffs). Although Barnes (2012) addresses a number of workplace outcomes that are impacted by these decrements in self-regulatory cognitive performance (e.g., work withdrawal, workplace incivility), we extend this work and evaluate safety behavior and workplace injuries as outcomes that are also contingent on a worker’s ability to self-regulate. Relatedly, in Wallace and Chen’s (2005) validation paper, workplace cognitive failures are conceptualized as a form of self-regulation that occurs at work. They posit that those who struggle to self-regulate are particularly susceptible to cognitive failures (Wallace & Chen, 2005). Therefore, we consider workplace cognitive failure as a self-regulatory behavior that should be influenced by employee sleep.
Crain and colleagues (in press) theorize that the processes connecting employee sleep and work outcomes occur intra-individually (i.e., within people) and inter-individually (i.e., between people) and note that changes can happen both immediately after sleep and over time based on average levels of sleep. Accordingly, they note that relationships should be examined day-to-day and across time intervals of months and years (Crain et al., in press). Specific to cognition, past research has also found that sleep has an immediate and long-term influence on cognitive functioning. For example, there is meta-analytic evidence that sleep deprivation in laboratory studies results in immediate impairments in cognitive variables like attention and vigilance (e.g., Lim & Dinges, 2010). However, a complimentary area within the sleep literature, informed by traditional laboratory research, suggests that sleep influences cognitive variables due to changes in the brain that occur over longer, substantial time periods (e.g., Abel, 2013; Castronovo et al., 2014). This work informs our decision to consider the enduring relationships among sleep, cognitive failure, and safety outcomes over 6-month time lags.
Research in the area of cognitive neuroscience has begun to elucidate the role of sleep in facilitating long-term adaptive changes in the brain (e.g., Abel, 2013; Shaffer, 2016; Walker & Stickgold, 2006). In contrast to the idea of age-related cognitive declines, there is evidence that individuals can maintain and even improve cognitive functioning over time. Long-term brain changes (i.e., neuroplasticity) can occur in brain cells, anatomical structures, grey matter volume, neural pathways, and synapses – all of which can influence human cognition and behavior (e.g., Kolb, 1995; Kolb & Gibb, 2014). Further, obtaining adequate sleep activates brain regions associated with cognitive processes (e.g., the hippocampus) and stimulates neurogenesis (i.e., growth of new brain cells) in these areas (e.g., Joo, Kim, Suh, & Hong, 2014; Goel, Rao, Durmer, & Dinges, 2009). In a similar vein, research in clinical populations has demonstrated that successful treatment of sleep disorders leads to changes in brain structures and partial recovery of cognitive processes like memory and attention (e.g., Castronovo et al., 2014; Rosenzweig et al., 2016). These effects have been detected over time intervals ranging from days to one year (e.g., Castronovo et al., 2014; Rosenzweig et al., 2016; Turkington, Sircar, Saralaya, & Elliot, 2004), though more substantial changes are found over longer time lags (Castronovo et al., 2014). This work lends evidence to sleep-dependent neuroplasticity and suggests that improved sleep can have both immediate and long-term impacts on cognition.
We choose to explore the longitudinal relationships between baseline sleep quantity and quality on workplace cognitive failures 6-months later, in line with Crain and colleagues (in press) suggestion to investigate enduring relationships over time and consistent with past research on sleep and long-term changes in the brain. Prior work has demonstrated that individuals with disturbed sleep experience more accidents at work and at home (e.g., Garbarino, Guglielmi, Sanna, Mancardi, & Magnavita, 2016; Leger et al., 2014; Uehli et al., 2014), though this work has relied on cross-sectional reports of accidents and has not explored these effects longitudinally. Therefore, we consider the impact of baseline sleep and 6-month cognitive failures on 12-month workplace safety outcomes (i.e., safety compliance, safety participation, and minor injuries). Over time, we expect that workers without sufficient sleep quantity and quality will lack physical energy resources needed to effectively self-regulate, resulting in more unintended and unsafe behaviors and injuries at work.
Sleep and Cognitive Failures
Cognitive failures are errors in cognitive processing which occur during tasks that people should normally be able to complete (Martin, 1983; Wallace & Chen, 2005). Workplace cognitive failure, for example, may occur when an employee experiences lapses in memory for work-related tasks and procedures, reduced attention to work-related information, and/or exhibits unintended behaviors at work (Wallace & Chen, 2005). Past research also suggests that sleep influences cognitive processing and performance. Reviews and meta-analyses, which have primarily included laboratory studies, indicate that sleep restriction (i.e., reduced sleep duration) and deprivation (i.e., total lack of sleep) have detrimental effects on cognitive performance variables, like vigilance, reaction time, reasoning, attention, and working memory (e.g., Banks & Dinges, 2007; Durmer & Dinges, 2005; Lim & Dinges, 2010; Pilcher & Huffcut, 1996; Short & Banks, 2014; Walker, 2009; Watson et al., 2015). Further, a CDC-sponsored report found that the most prevalent difficulties for people who sleep less than 7 hours per night include trouble concentrating and remembering things (CDC, 2011).
The effects of sleep on cognitive components of self-regulation have been studied in field settings with working populations, as well. For example, people who experience insomnia symptoms report more work-related cognitive problems, such as poor concentration and organization (Swanson et al., 2011). Another study found that poor sleep quality and fatigue are correlated with being more distracted at work and having lower work situation awareness (Sneddon, Mearns, & Flin, 2013). These studies suggest that employee sleep is associated with work-related cognitive functioning, but less is known about how sleep is related to workplace cognitive failures. One exception includes a study which found that self-reported sleep problems were positively associated with a single-item measure of workplace cognitive failures (Simpson, Wadsworth, Moss, & Smith, 2005). The present study instead considers these relationships longitudinally in a field setting with a safety-sensitive sample, assesses both sleep quantity and quality, and uses a multiple-item measure of workplace cognitive failures.
We predict that construction workers with greater sleep quality and quantity will have more available physical energy resources and experience fewer workplace cognitive failures. For example, workers who obtain adequate sleep, feel well-rested in the morning, and do not have trouble falling or staying asleep will have adequate physical energy resources and should therefore be less likely to experience decrements in cognitive components of self-regulation, such as forgetting work procedures or becoming distracted on-the-job. In line with Crain and colleagues’ (in press) and Barnes’ (2012) theoretical frameworks, and findings from past research, we hypothesize the following:
Hypothesis 1:
Sleep quantity and quality will negatively affect workplace cognitive failure.
Cognitive Failure and Safety Outcomes
Prior work has shown that cognitive failures are related to safety-related outcomes. For example, general measures of cognitive failure have been found to be significantly and positively related to self-reports of unsafe behaviors and workplace accidents (e.g., Larson, Alderton, Neideffer, & Underhill, 1997; Wallace & Vodanovich, 2003). Wallace and Chen (2005) found that workplace cognitive failures were positively related to self-reported unsafe behaviors (i.e., low safety compliance), micro-accidents at work (i.e., a combination of minor and major accidents), and organizational OSHA records of injuries, lost work days, and restricted work days due to injuries. Further, Wallace and Chen (2005) found that workplace cognitive failure predicted these effects over and above general cognitive failure.
Other studies have also investigated the influence of workplace cognitive failure on safety at work. For example, a single-item measure of workplace cognitive failure was associated with self-reports of accidents and minor workplace injuries (Simpson et al., 2005). Another study found that nurses who experienced frequent workplace cognitive failures were more likely to have patient safety incidents (Park & Kim, 2013). Elfering, Grebner, and Ebener (2015) found that workplace cognitive failures in action (e.g., unintentionally pressing control switches on a machine) mediated the association between safety compliance and near-accidents. However, Elfering and colleagues (2015) only considered cognitive failures specific to action-based behaviors at work, so we use a more comprehensive measure of workplace cognitive failure.
Lapses in cognitive performance aspects of self-regulation (i.e., cognitive failure) should inhibit employees’ ability to be compliant toward safety protocols, voluntarily put in extra effort to carry out their work in a safe manner, and increase their experiences of workplace injuries. Indeed, Barnes (2012) describes that cognitive aspects of self-regulation, such as being distracted and unable to control attention, can impede on goal-directed activities. We argue that construction workers who experience cognitive failure at work will be less inclined and/or able to complete work tasks in adherence with safety protocols, voluntarily try to improve workplace safety, and maintain their personal safety on-the-job. For example, workers will not be able to correctly follow work procedures and complete their job tasks in a safe manner if they are distracted or do not remember what the procedures entail. In light of the evidence that cognitive failure is related to employees’ safety at work, we hypothesize the following:
Hypothesis 2a:
Workplace cognitive failure will negatively affect safety compliance.
Hypothesis 2b:
Workplace cognitive failure will negatively affect safety participation.
Hypothesis 2c:
Workplace cognitive failure will positively affect minor workplace injuries.
Cognitive Failure as a Mediator
Previous research has provided extensive evidence that work-related safety outcomes – such as accidents and injuries – are influenced by employees’ sleep quantity and quality (e.g., Barnes & Wagner, 2009; Kao, Spitzmueller, Cigularov, & Wu, 2016; Kling, McLeod, & Koehoorn, 2010; Rosekind et al., 2010; Salminen et al., 2010; Uehli et al., 2014; Watson et al., 2015). Prior work has also found that sleep duration predicts greater extra role behaviors (Barnes, Ghumman, & Scott, 2013), and safety participation is a type of extra role behavior that is specific to safety. Furthermore, findings from Uehli and colleagues’ (2014) meta-analysis suggests that approximately 13% of work-related injuries can be attributed to problems in employees’ sleep quantity and sleep quality. These authors also call for future research that uncovers the underlying mechanisms that connect sleep problems with workplace injuries (Uehli et al., 2014). Safety-specific behaviors are not theorized by Crain and colleagues (in press) or Barnes (2012). However, Crain and colleagues (in press) describe the importance of considering safety-sensitive industries, and we argue that workers’ ability to be compliant towards safety procedures, voluntarily promote the safety program in their organization, and avoid workplace injuries is contingent on their levels of physical resources and self-regulatory capacity, which are contingent on sleep.
Overall, there is empirical and theoretical evidence that suggests that employees’ sleep has an impact on their work-related safety outcomes. However, to our knowledge, no prior work has investigated the effects of workers’ sleep on their subsequent compliance with safety procedures, willingness to put in extra effort to improve safety at work, and experiences of workplace injuries. Moreover, research that explores the mechanisms which explain the relationship between sleep and safety-related outcomes is sparse. One exception is Kao and colleagues’ (2016) study, which found that the effects of insomnia on injuries at work was explained by safety behavior. In summary, we expect that construction workers who have shorter sleep durations and poorer sleep quality on average will report being less compliant with safety protocols, less willing to promote the safety program in their organization, and more likely to experience minor injuries because they experience a greater frequency of cognitive failures (i.e., decrements in self-regulatory ability) at work.
Hypothesis 3a:
Workplace cognitive failure will mediate the effects of sleep quantity and quality on safety compliance.
Hypothesis 3b:
Workplace cognitive failure will mediate the effects of sleep quantity and quality on safety participation.
Hypothesis 3c:
Workplace cognitive failure will mediate the effects of sleep quantity and quality on minor workplace injuries.
Method
Procedure and Participants
Data were collected as part of a larger health and safety intervention study. Specifically, construction workers on day shifts from two public works agencies in a U.S. metropolitan area completed surveys at baseline (n = 329–470), 6-months (n = 377), and 12-months (n = 318–325). Of the substantive study variables, sleep quantity and quality and all safety-related variables (i.e., compliance, participation, and injuries) were assessed at each time-point, and workplace cognitive failure was assessed at 6-months and at 12-months. As such, our analyses are based on baseline reports of sleep, 6-month reports of cognitive failure, and 12-month reports of compliance, participation, and injuries. Final analyses reported in the results section are based on a total of 222 responses across all time points. Participants received $25 as an incentive at each time point.
Participants were primarily male (66%), white (56%), and were on average 44.50 years old (SD = 9.58). In terms of education, 2% completed some high school, 26% graduated from high school, 33% completed some college, 8% graduated from college, and 1% had attended some graduate school. Most participants were married or living with a partner (74%) and 39% had children living in their home. Additionally, participants worked an average of 41.89 hours per week (SD = 5.92) and had worked in their current job an average of 10.54 years (SD = 8.14).
Measures
Mean imputation of missing scores was used for all scales with four or more items when at least 75% of the data were present. Otherwise, listwise deletion was used to construct scale scores.
Sleep quantity and quality.
Baseline sleep quantity was measured using two items from the Pittsburgh Sleep Quality Index (PSQI; Buysse, Reynolds, Monk, Berman, & Kupfer, 1989): “During the past month, when have you usually gone to bed?” and “During the past month, when have you usually gotten up in the morning?” These items were used to calculate participants’ typical sleep duration. Baseline sleep quality was assessed with measures of sleep insufficiency and insomnia symptoms. Sleep insufficiency was measured with a single-item (Buxton et al., 2009; Buxton et al., 2012): “During the past month, how often did you get enough sleep to feel rested upon waking?” Scores range from 1 to 4 (1 = Three or more times a week; 4 = Never), in which higher scores represent greater sleep insufficiency. Insomnia symptoms were measured with two items on the PSQI (Buysse et al., 1989): “During the past month, how often could you not get to sleep within 30 minutes?” and “During the past month, how often did you wake in the middle of the night or early morning?” Participants rated both items on a 1 to 4 scale (1 = Never; 4 = Three or more times a week), in which higher scores represent greater insomnia symptoms. These two items were averaged to compute an aggregated insomnia symptoms score.
Workplace cognitive failure.
6-month workplace cognitive failure was measured with a 13-item measure (Cronbach’s α = .85) asking about the frequency an individual engages in specific behaviors (Wallace & Chen, 2005). Example items include “cannot remember what materials are required to complete a particular task” and “do not focus full attention on work activities.” Scores range from 1 to 5 (1 = Never; 5 = Very Often), in which higher scores represent greater workplace cognitive failure. Items 7 (“Do not fully listen to instruction”) and 11 (“Accidentally drop objects or things”) were dropped from the original 15-item scale as a result of low factor loadings; the majority of participants reported that these behaviors were never or rarely experienced, thus limiting variance in each item.
Safety compliance.
12-month safety compliance was measured with a 3-item measure adapted from Neal and colleagues’ (2000) safety behavior scale (Cronbach’s α = .92). The instructors prompted participants to think about the past 4 weeks. An example item is “I use all the necessary safety equipment to do my job.” Scores range from 1 to 5 (1 = Strongly Disagree; 5 = Strongly Agree), in which higher scores represent greater safety compliance.
Safety participation.
12-month safety participation was measured with a 3-item measure also adapted from Neal and colleagues’ (2000) safety behavior scale (Cronbach’s α = .89). Participants were asked to think about the past 4 weeks. An example item is “I put in extra effort to improve the safety of the workplace”. Scores range from 1 to 5 (1 = Strongly Disagree; 5 = Strongly Agree), in which higher scores represent greater safety participation.
Minor workplace injuries.
12-month minor workplace injuries were measured with the following single-item measure, as used in prior work (e.g., Bodner, Kraner, Bradford, Hammer, & Truxillo, 2014): “In the past 6 months, have you had any minor injuries at work that did NOT require you to miss work on following shifts? (minor cuts, bruises, or sprains requiring first aid or no treatment)”. Response options were dichotomized (0 = No minor injuries experienced in the past 6 months; 1 = At least one minor injury experienced in the past 6 months).
Control variables.
Control variables were selected according to theory and past research as described in Spector and Brannick’s (2011) discussion of the use of statistical control variables. Accordingly, control variables that are potentially related to variables of interest were selected as a way to control for alternative (i.e., spurious) explanations of relationships in the model. Specifically, we included age, race, gender, and average work hours per day as control variables, as prior work has demonstrated that these are related to sleep. For example, Caucasians, women, younger adults, and those with fewer work hours tend to have better sleep compared to racial and ethnic minorities, men, older adults, and employees with a greater number of work hours (e.g., Adenekan et al., 2013; Burgard & Ailshire, 2013; Carskadon & Dement, 2017; Hale & Do, 2007; Landrigan et al., 2008; Neikrug & Ancoli-Israel, 2010). Additionally, because participants in this study were recruited from two different organizations, industry was also controlled for. Further, this study was part of a larger intervention study, so we accounted for the treatment indicator in our analyses because we were not substantively interested in the intervention for the purposes of this paper.
Lastly, because safety motivation has been shown to predict safety behaviors (e.g., Neal, Griffin, & Hart, 2000), 12-month motivation to comply and motivation to participate were controlled for. Based on theory and past research, we would not expect that workplace cognitive failures and/or safety behaviors would predict motivation to comply or motivation to participate, which is why it is included as a covariate instead of a substantive variable in the model. Motivation to comply was controlled for with a 5-item measure from Neal and colleagues’ (2000) safety behavior scale (Cronbach’s α = .93). An example item is “I feel that adhering to safety procedures is worthwhile.” Motivation to participate was controlled for with a 6-item measure from Neal and colleagues’ (2000) safety behavior scale (Cronbach’s α = .85). An example item is “I feel that it is worthwhile to volunteer for safety-related tasks”. Scores for both safety motivation measures range from 1 to 5 (1 = Strongly Disagree; 5 = Strongly Agree), in which higher scores represent greater motivation to comply and participate.1
Results
All analyses were conducted in Mplus Version 8. Because employees were nested within 12 workgroups across the two different organizations, intraclass correlations (ICCs) were calculated to determine the degree of dependency within workgroups. Values for workplace cognitive failure and all safety outcomes were less than .010. Thus, multilevel modeling was not used in the final analyses. See Table 1 for means, standard deviations, and bivariate correlations of all variables.
Table 1.
Descriptive Statistics and Correlations Among Study Variables
| Variable | N | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | 345 | 44.45 | 9.56 | - | ||||||||||||||
| 2. Race | 341 | 0.77 | 0.42 | −.01 | - | |||||||||||||
| 3. Gender | 345 | 0.90 | 0.30 | −.03 | .06 | - | ||||||||||||
| 4. Work Hours Per Day | 329 | 8.58 | 1.02 | −.01 | .01 | .06 | - | |||||||||||
| 5. Treatment | 470 | 0.60 | 0.49 | −.08 | .02 | .11* | .09 | - | ||||||||||
| 6. Organization | 470 | 0.42 | 0.49 | −.16** | −.04 | −.02 | .42*** | .08 | - | |||||||||
| 7. Motiv. to Comply (12m) | 320 | 4.33 | 0.51 | −.02 | −.03 | −.15* | .06 | −.09 | .09 | - | ||||||||
| 8. Motiv. to Participate (12m) | 320 | 4.10 | 0.55 | .00 | −.10 | −.15* | .12 | −.03 | .08 | .78*** | - | |||||||
| 9. Sleep Insufficiency (B) | 346 | 1.80 | 0.91 | −.02 | −.04 | −.04 | .04 | −.01 | .11* | .15* | .10 | - | ||||||
| 10. Insomnia Symptoms (B) | 340 | 2.69 | 0.81 | .04 | −.08 | −.04 | .02 | −.15** | .06 | −.05 | −.03 | .09 | - | |||||
| 11. Sleep Duration (B) | 342 | 7.05 | 0.97 | .05 | .06 | −.15** | −.21*** | −.08 | −.07 | .04 | .03 | −.22*** | .10 | - | ||||
| 12. Cognitive Failure (6m) | 377 | 1.85 | 0.45 | .05 | .03 | .06 | .06 | −.10* | .13 | −.07 | −.07 | .06 | .19** | .05 | - | |||
| 13. Safety Compliance (12m) | 320 | 4.17 | 0.64 | −.07 | −.07 | −.13* | .05 | −.08 | .07 | .80*** | .64*** | .03 | −.09 | .02 | −.21*** | - | ||
| 14. Safety Participation (12m) | 318 | 3.70 | 0.83 | −.02 | −.07 | −.08 | .06 | .02 | .00 | .58*** | .69*** | .06 | −.05 | .04 | −.20*** | .58*** | - | |
| 15. Minor Injuries (12m) | 325 | 0.31 | 0.46 | −.08 | .00 | −.00 | −.03 | −.04 | .04 | −.00 | .00 | .02 | .07 | .08 | .15* | −.06 | −.05 | - |
Note: Race (0 = Non-white; 1 = White); Gender (0 = Female; 1 = Male); Organization (0 = Organization 1; 1 = Organization 2); Treatment (0 = Control, 1 = Intervention). Motiv. = Motivation. Minor Injuries (0 = No minor injuries experienced in the past 6 months; 1 = At least one minor injury experienced in the past 6 months). B = baseline; 6m = 6-months, 12m = 12-months.
< p < .05.
p < .01.
p < .001.
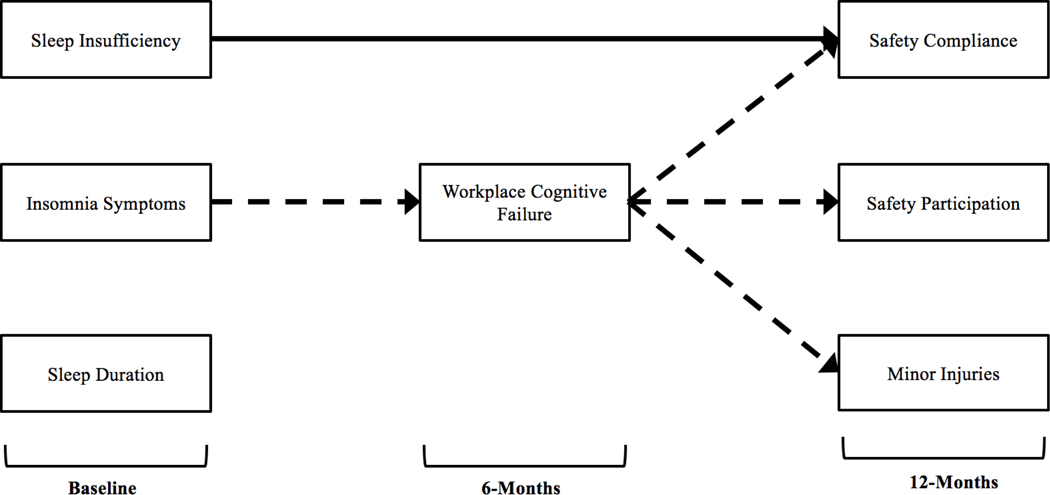
Using path modeling, we next tested hypotheses 1–3 to determine whether relationships between sleep and safety were mediated by cognitive failure, controlling for industry, treatment indicator, age, gender, ethnicity, hours worked, and safety motivation. Linear regressions were used to test the effects of sleep and workplace cognitive failure on safety compliance and safety participation, and logistic regressions were used to test the effects of sleep and workplace cognitive failure on reports of minor workplace injuries. A fully saturated path model was specified with all study variables included. Bootstrapping with 1,000 bootstrapped samples was used and significance was determined by asymmetrical confidence intervals that did not include 0. See Table 2 for results and Figure 1 for the model that was tested.
Table 2.
Direct Regression Effects of Sleep on Workplace Cognitive Failure, Safety Compliance, Safety Participation, and Minor Injuries
| Outcome | Outcome | Outcome | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| 6m Cognitive Failure | 12m Safety Compliance | 12m Safety Participation | 12m Minor Injuries | ||||||
|
|
|||||||||
| Predictor | B | SE B | B | SE B | B | SE B | B | SE B | OR |
| Intercept | 1.50** | 0.56 | 0.93* | 0.44 | −0.48 | 0.61 | −1.85 | 1.74 | |
| Age | 0.00 | 0.00 | −0.00 | 0.00 | −0.00 | 0.00 | −0.02 | 0.01 | 0.97 |
| Race | 0.01 | 0.07 | −0.04 | 0.05 | 0.00 | 0.09 | −0.02 | 0.24 | 0.99 |
| Gender | 0.06 | 0.11 | −0.01 | 0.10 | 0.13 | 0.14 | 0.03 | 0.33 | 1.07 |
| Work Hours Per Day | −0.00 | 0.05 | −0.00 | 0.03 | 0.00 | 0.03 | −0.04 | 0.12 | 0.94 |
| Treatment | −0.09 | 0.06 | −0.00 | 0.05 | 0.04 | 0.08 | −0.02 | 0.20 | 0.95 |
| Organization | 0.14 | 0.08 | 0.03 | 0.06 | −0.05 | 0.08 | −0.06 | 0.23 | 0.90 |
| Motivation to Comply (12m) | 0.02 | 0.10 | 0.94*** | 0.08 | 0.21 | 0.14 | 0.01 | 0.33 | 1.02 |
| Motivation to Participate (12m) | −0.09 | 0.09 | 0.05 | 0.09 | 0.91*** | 0.12 | 0.05 | 0.30 | 1.10 |
| Sleep Insufficiency (B) | 0.00 | 0.04 | −0.06* | 0.03 | −0.03 | 0.05 | 0.06 | 0.12 | 1.10 |
| Insomnia Symptoms (B) | 0.09* | 0.04 | −0.02 | 0.03 | 0.03 | 0.05 | 0.04 | 0.14 | 1.08 |
| Sleep Duration (B) | 0.03 | 0.04 | −0.03 | 0.03 | 0.02 | 0.04 | 0.13 | 0.11 | 1.24 |
| Cognitive Failure (6m) | −0.26*** | 0.06 | −0.32*** | 0.08 | 0.55* | 0.23 | 2.52 | ||
Note: Race (0 = Non-white; 1 = White); Gender (0 = Female, 1 = Male); Organization (0 = Organization 1; 1 = Organization 2); Treatment (0 = Control, 1 = Intervention). Minor Injuries (0 = No minor injuries experienced in the past 6 months; 1 = At least one minor injury experienced in the past 6 months). OR = Odds Ratio. B = baseline; 6m = 6-months, 12m = 12-months.
< p < .05.
p < .01.
p < .001.
Figure 1.
Empirical result of baseline sleep on 6-month workplace cognitive failure and 12-month safety compliance, safety participation, and minor injuries process model. Control variables (i.e., age, race, gender, work hours, treatment, organization, and 12-month motivation to comply and motivation to participate) not shown for parsimony. Bold arrows depict significant direct effects and bold dashed arrows depict significant indirect effects.
Direct effects.
Controlling for all other variables in the model, a significant positive association was found between insomnia symptoms and workplace cognitive failure (B = 0.09, p < .05). However, sleep insufficiency (B = 0.00, p = 0.92) and sleep duration (B = 0.03, p = 0.40) were not related to workplace cognitive failure. Furthermore, a significant negative relationship was found between workplace cognitive failure and safety compliance (B = −0.26, p < 0.001), and safety participation (B = −0.32, p < 0.001), controlling for all other variables in the model. In addition, there was a significant positive relationship between workplace cognitive failure and minor workplace injuries (B = 0.55, p < 0.05). It is also important to note that the covariates of motivation to comply and motivation to participate were not significantly associated with workplace cognitive failure, but motivation to comply was significantly and positively associated with safety compliance, and motivation to participate was significantly and positively associated with safety participation, controlling for all other variables in the model. Thus, hypothesis 1 was partially supported, and hypotheses 2a-2c were supported.
Indirect effects.
Results indicate a significant indirect effect, controlling for all other variables in the model, of insomnia symptoms on safety compliance through workplace cognitive failure (indirect effect = −0.02, 95% CI [−0.5, −.004]). Associations between sleep insufficiency (indirect effect = −0.00, 95% CI [−.02, .01]) and duration (indirect effect = −0.01, 95% CI [−.03, .01]) and safety compliance were not significantly mediated by cognitive failure. Interestingly, a significant negative association between sleep insufficiency and safety compliance was found (B = −0.06, p < .05), controlling for all other variables in the model, suggesting that other unmeasured mediators played a role in this association. Next, there was a significant indirect effect of insomnia symptoms on safety participation through workplace failure (indirect effect = −.03, 95% CI [−.07, −.01]), after controlling for all other variables in the model. However, associations between sleep insufficiency (indirect effect = −.00, 95% CI [−.03, .03]) and duration (indirect effect = −.01, 95% CI [−.04, .01]) and safety participation were not significantly mediated by cognitive failure. Finally, after controlling for all other variables in the model, there was a significant indirect effect of insomnia symptoms on minor workplace injuries through workplace cognitive failure (indirect effect = .05, 95% CI [.00, .14]). Associations between sleep insufficiency (indirect effect = .00, 95% CI [−.05, .05]) and duration (indirect effect = .02, 95% CI [−.02, .08]) and minor workplace injuries were not significantly mediated by cognitive failure. No significant direct effects of insomnia symptoms on safety compliance, safety participation, or minor injuries were found simultaneously in the path model, suggesting that these relationships were fully mediated by cognitive failure. Thus, hypotheses 3a-3c were partially supported.2,3
Discussion
We examined the effects of construction workers’ sleep duration, sleep insufficiency, and insomnia symptoms on safety compliance, safety participation, and minor injuries and mediating effects of workplace cognitive failure. We found that construction workers with more insomnia symptoms on average experienced more frequent cognitive failures at work, and this predicted less compliance with safety protocols and procedures, less voluntary willingness to promote the safety program within the organization, and higher rates of minor injuries at work. Additionally, construction workers who reported not feeling well-rested upon awakening on average had lower safety compliance, but this effect was not mediated by workplace cognitive failures. No effects were found among sleep duration and any of the safety-related outcomes. These results suggest that organizations should be concerned with their employees’ sleep quality in order to prevent downstream unsafe behaviors and workplace accidents and injuries.
Our results lend support to Crain and colleagues’ (in press) and Barnes’ (2012) frameworks as employee sleep predicted self-regulatory behaviors at work. Specifically, insomnia symptoms predicted the frequency of workplace cognitive failures and later safety behaviors and minor injuries at work, suggesting that workers’ sleep influences work behaviors via cognitive components of their self-regulation. These findings are aligned with past research that has found effects of insomnia symptoms on safety-related outcomes, including workplace injuries (e.g., Kao et al., 2016; Swanson et al., 2011). We extend this prior work by considering safety compliance and participation as specific safety-related behavioral constructs, and workplace cognitive failure as a self-regulatory mechanism in this process. Further, in line with Crain and colleagues’ (in press) theorization and past work examining the effects of sleep on long-term brain changes, we found enduring associations across 6-month time lags. This suggests that the relationship between adequate sleep quality and improved cognitive functioning at work (i.e., reduced experiences of cognitive failures) endures over time. In addition, the effects we found are less likely due to common method bias given that measures were collected at different points in time. (e.g., Podsakoff, MacKenzie, Lee, & Podsakoff, 2003). Moreover, assessing relations between variables over time reduces measurement error and, consequently, increases the validity of our statistical conclusions (e.g., Wang et al., 2017).
Surprisingly, although there was a direct effect of baseline sleep insufficiency on safety compliance, this effect was not mediated by workplace cognitive failure, and similar effects were not found between sleep insufficiency and safety participation or minor injuries. Therefore, the mechanism(s) that explain the relationship between sleep insufficiency and safety compliance currently remain unknown. It is possible that different aspects of self-regulation explain this relationship. Barnes (2012) theorizes that poor sleep is related to defection in social dilemmas, in which workers put their own self-interests above the interests of coworkers or the organization as a whole. For example, workers who are not well-rested may neglect to use required safety equipment (e.g., PPE) or adhere to safety procedures in attempts to complete their work tasks at a faster rate. Although this could be of personal benefit to them, it could threaten the safety of their coworkers and disrupt the overall safety climate within their organization. This example reflects a different type of self-regulatory ability, which would not be explained by experiences of workplace cognitive failure. In this case, lack of safety compliance could be attributed to an impaired ability to assess risk, or the desire to seek immediate payoffs (Barnes, 2012), or could be due to sleepiness that has manifested into the deviant behavior of not adhering to workplace safety procedures (Mullins et al., 2014). It is also possible that symptoms of insomnia are a more powerful predictor of cognitive functioning and safety-related outcomes because they could reflect a more chronic or persistent problem than insufficiency (e.g., Bhaskar, Hemavathy, & Prasad, 2016). Future work should consider potential mediators that explain the relationship between sleep insufficiency and non-compliance with workplace safety procedures.
In addition, we did not find effects of sleep duration on workplace cognitive failure or any of the safety-related outcomes. This is discrepant from past research, which has found that restricted or deprived sleep quantity is associated with reduced cognitive performance outcomes (e.g., Lim & Dinges, 2010; Short & Banks, 2014; Watson et al., 2015), and that sleep duration predicts safety outcomes, like workplace injuries (e.g., Uehli et al., 2014). However, the majority of studies evaluating sleep duration in relation to human performance have been conducted in laboratory settings with strong sleep restriction or sleep deprivation manipulations and simple neurobehavioral test batteries (e.g., psychomotor vigilance tasks), which do not necessarily generalize to all on-the-job behaviors. In contrast, our study uses a more externally valid work-specific measure of cognitive failure, which encompasses failure to carry out typical work-related tasks. Also of note is that employees in our sample reported an average of 7.05 hours of sleep, thereby meeting the recommended criteria for healthy sleep duration that would not be expected to result in frequent cognitive failures (e.g., Watson et al., 2015).
Practical Implications
Our findings indicate that organizations concerned with employee safety behaviors and injuries at work should prioritize workplace practices and policies that would influence employees’ ability to get high quality sleep. In particular, organizations hoping to improve safety behaviors and injury rates should prioritize efforts that are likely to improve insomnia symptoms, or employees’ ability to quickly initiate sleep and maintain sleep throughout the night. Given well-established associations between stressors and insomnia symptoms, organizations could attempt to alleviate employee strain, for example, by targeting work demands, resources, and social support (e.g., Jansson & Linton, 2006; Linton, 2004). Intervening on stress-related variables could improve sleep quality by reducing ruminative thoughts before bedtime and increasing employees’ ability to unwind, quickly fall asleep, and maintain sleep throughout the night (e.g., Cropley, Dijk, & Stanley, 2006). Additionally, prior work has found that workplace mindfulness-based training interventions have improved participants’ sleep and reduced insomnia symptoms (e.g., Crain, Schonert-Reichl, & Roeser, 2017). Further, there is evidence that psychological detachment from work mediates the relationships between mindfulness and sleep quality (Hülsheger et al., 2014) and can benefit workplace cognitive failures (e.g., Lapierre, Hammer, Truxillo, & Murphy, 2012), so refraining from work-related thoughts (i.e., psychologically detaching) while at home could also indirectly relate to safer workplace behaviors. Finally, Barnes, Miller, and Bostock (2017) implemented an effective online cognitive behavioral therapy training intervention for workers with insomnia, in which participants were taught about how to change their thoughts and behaviors to improve sleep.
More general interventions could also improve both sleep quantity and sleep quality. For example, providing people with actigraphic (i.e., sleep-tracking through wristwatch devices) sleep feedback has also been shown to improve sleep quantity and quality (Adler, Guina, Bliese, Kim, & LoPresti, 2017). Further, training employees on sleep hygiene behaviors (e.g., avoiding caffeine and alcohol, reducing bedroom noise, maintaining consistent sleep schedules) could also improve multiple aspects of sleep, as prior work has shown that hygiene behaviors influence both sleep quantity and quality (e.g., Irish, Kline, Gunn, Buysse, & Hall, 2015). However, the effectiveness of sleep hygiene interventions in healthy, non-clinical populations is limited, so future research is needed in this area (e.g., Irish, et al., 2015). Although we do not find parallel effects among the different measures of sleep (i.e., sleep quantity, insufficiency, and insomnia symptoms), general sleep interventions could be beneficial for all of these constructs. Further, though most effects on workplace safety were predicted by insomnia symptoms, we do find a direct effect of sleep insufficiency on safety compliance, suggesting that more general interventions could have positive implications for workplace safety, as well.
Limitations and Future Research
There are a number of limitations of this study and avenues for future research. First, although it is a strength of our study to examine workers in the construction industry, which has been characterized as being hazardous (e.g., NIOSH, 2017; OSHA, 2016), this work should be replicated in other safety-sensitive industries and operational settings where it is especially important to avoid workplace cognitive failures (e.g., agriculture, healthcare, and manufacturing). In addition, this work was conducted with a sample of day shift construction workers who received an adequate average sleep duration of about 7 hours per night. Therefore, future work should consider a sample of night shift workers or rotating shift workers who are more likely to experience short sleep durations and misalignment between their highest propensity for sleep based on their circadian rhythm (i.e., the biological night) and the available window of time to sleep (i.e., often during the day). Similarly, this sample also reported relatively low levels of workplace cognitive failure (i.e., an average of 1.85 on a 5-point scale), so future work should explore populations that may be particularly susceptible to cognitive failure at work. Workers with frequently changing shift schedules (e.g., nurses) or who are required to sustain attention and respond quickly (e.g., control room operators) may be more at risk for workplace cognitive failures.
The present study is the first to assess the relations among sleep, workplace cognitive failure, and safety-related outcomes in a time-lagged design, though we were unable to analyze more serious or objective safety-specific outcomes. We collected data related to reported major injuries (i.e., those requiring employees to miss work due to recovery time and medical treatment) and workers’ compensation claims. However, we could not empirically assess these outcomes in our model because of the low base rate of these reports; 8.6% of our sample reported experiencing a major injury and 6.8% of our sample filed a workers’ compensation claim. Future research should examine how sleep and workplace cognitive failures are related to additional long-term rates of accidents, injuries, and near-misses. This information could be obtained via self-reports on surveys, OSHA 300 logs, or workers’ compensation claims. Additionally, as Barnes (2012) theorized that poor sleep should predict distorted risk analysis, future work would benefit by examining risk-taking behaviors at work, such as rule violations, corner-cutting, and safety workarounds.
Although this study identifies how average levels of sleep, workplace cognitive failures, and safety outcomes are associated over time, it would be fruitful to evaluate this model in a within-person framework using experience sampling or daily diary methodology. For example, participants could report their experiences of cognitive failures and safety-specific behaviors (e.g., safety behaviors, near-misses, rule violations) at multiple pre-determined times throughout a workday. Then, these daily experiences could be examined alongside daily reports of sleep quantity and quality or with actigraphic devices (see Ohly, Sonnentag, Niessen, & Zapf, 2010 for a review of diary studies in organizational research and Beal, 2015 for a review of experience sampling methodology in organizational research). This would provide insight into how daily fluctuations in employees’ sleep influence the amount of workplace cognitive failures they experience, and how this relates to whether they engage in safe behaviors and avoid injuries at work. Indeed, as suggested by Crain and colleagues (in press), there are likely intra-individual (i.e., within-person) and inter-individual (i.e., between-person) effects. For example, intra-individually, workers may have days when they are more fatigued and less able to pay attention at work, such as after a night of staying awake with a newborn baby. Alternatively, some groups of people may have lower energy and/or be more distractible than others, or may work in environments with stronger safety climates (i.e., inter-individual effects). Future work would benefit by exploring these relationships at different levels of analysis.
Finally, future studies could also measure sleep with alternative methods, such as using objective measures of sleep quantity and quality in addition to self-reports. For example, actigraphy is a validated tool to measure sleep; wristwatch devices (i.e., actigraphs) contain accelerometers to measure movement, which allows for the distinction between sleep and wake cycles (e.g., Ganster, Crain, & Brossoit, 2018; Marino et al., 2013). Further, although the self-reported measures of sleep duration and insomnia symptoms used in the present study are from the PSQI, which is the most commonly used questionnaire to assess sleep characteristics (e.g., Grandner, Kripke, Yoon, & Youngstedt, 2006), new measures of sleep could be considered. For instance, Yu and colleagues (2012) developed the Patient-Reported Outcomes Measurement Information System (PROMIS) measures of sleep disturbance and sleep-related impairment. These authors used item-response theory techniques to compare the PROMIS sleep measures to other common measures of sleep, including the PSQI, and concluded that the PROMIS measures provide the greatest test information. Therefore, future work should consider incorporating objective measures of sleep as well as updated and validated self-reported measures.
Conclusion
In summary, this is the first study to test workplace cognitive failure as a mechanism connecting workers’ sleep and safety compliance, safety participation, and minor injuries in a safety-sensitive industry. As numerous studies in the sleep literature have evaluated relations between sleep and basic laboratory tests of cognitive functioning, this study extends our understanding of how deficient sleep manifests into actual safety behaviors and minor injuries in the workplace, while also expanding upon current organizational theories related to sleep.
Acknowledgments
Funding for this project was through the Oregon Healthy Workforce Center (www.ohsu.edu/ohwc), a National Institute for Occupational Safety and Health Total Worker Health Center of Excellence (Grant: U19OH010154). Rebecca M. Brossoit’s work on this manuscript was supported by the Grant T42OH009229, funded by the Centers for Disease Control and Prevention. The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services. The authors declare no conflicts of interest.
Footnotes
All analyses were conducted with and without control variables and results do not substantively differ (i.e., all significant direct and indirect effects are retained). Due to some moderate skewness on sleep insufficiency, cognitive failure, and safety compliance, all analyses were also conducted with and without transformed variables. However, because results did not differ, we report the untransformed variables for ease of interpretability.
In their original validation paper, Wallace and Chen (2005) found evidence of a three-factor model with a higher order cognitive failure factor and argue for future studies to evaluate both the superordinate cognitive failure construct, in addition to a three-factor construct. We also found support for this three-factor model, so we ran additional path analyses that simultaneously accounted for attention-, action-, and memory-related cognitive failure as mediators. However, no mediation effects were found in this model, likely as a result of the strong correlations among the three dimensions. For additional information and results of these analyses, please contact the authors.
Three additional models were conducted in which earlier levels of the outcome variables (i.e., baseline and 6-month safety compliance, safety participation, and minor injuries) were controlled for. In theory, these analyses should account for variance resulting from common method bias and stability of the variables over time. However, we did not collect measures of workplace cognitive failure at baseline and therefore could not control for earlier levels of workplace cognitive failure, so these supplemental results should be interpreted provisionally. The significant indirect effect of baseline insomnia symptoms predicting 12-month safety compliance through 6-month workplace cognitive failure was retained, though no other indirect effects were significant after controlling for earlier levels of the outcome variables. Given theory and empirical work indicating that sleep results in long-term changes in cognitive functioning as described previously, the remaining significant indirect effect with the safety compliance outcome is expected. Safety participation and minor injuries on the other hand, may be more subject to stability over time as a result of other enduring workplace factors, like safety climate or engineered safety protections in the workplace, thus resulting in less fluctuation in these outcomes in response to sleep and cognitive failure when earlier levels of the variables are controlled for.
References
- Abel T, Havekes R, Saletin JM, & Walker MP (2013). Sleep, plasticity and memory from molecules to whole-brain networks. Current Biology, 23, R774–R788. doi: 10.1016/j.cub.2013.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adenekan B, Pandey A, McKenzie S, Zizi F, Casimir GJ, & Jean-Louis G. (2013). Sleep in America: role of racial/ethnic differences. Sleep Medicine Reviews, 17, 255–262. doi: 10.1016/j.smrv.2012.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler AB, Gunia BC, Bliese PD, Kim PY, & LoPresti ML (2017). Using actigraphy feedback to improve sleep in soldiers: an exploratory trial. Sleep Health, 3, 126–131. doi: 10.1016/j.sleh.2017.01.001 [DOI] [PubMed] [Google Scholar]
- Akerstedt T, Fredlund P, Gillberg M, & Jansson B. (2002). A prospective study of fatal occupational accidents–relationship to sleeping difficulties and occupational factors. Journal of Sleep Research, 11, 69–71. doi: 10.1046/j.1365-2869.2002.00287.x [DOI] [PubMed] [Google Scholar]
- Banks S, & Dinges DF (2007). Behavioral and physiological consequences of sleep restriction. Journal of Clinical Sleep Medicine, 3(5), 519–528. [PMC free article] [PubMed] [Google Scholar]
- Barnes CM (2012). Working in our sleep: Sleep and self-regulation in organizations.Organizational Psychology Review, 2, 234–257. doi: 10.1177/2041386612450181 [DOI] [Google Scholar]
- Barnes CM, Ghumman S, & Scott BA (2013). Sleep and organizational citizenship behavior: The mediating role of job satisfaction. Journal of Occupational Health Psychology, 18, 16–26. doi: 10.1037/a0030349 [DOI] [PubMed] [Google Scholar]
- Barnes CM, Miller JA, & Bostock S. (2017). Helping employees sleep well: Effects of cognitive behavioral therapy for insomnia on work outcomes. Journal of Applied Psychology, 102, 104–113. doi: 10.1037/apl0000154 [DOI] [PubMed] [Google Scholar]
- Barnes CM, & Wagner DT (2009). Changing to daylight saving time cuts into sleep and increases workplace injuries. Journal of Applied Psychology, 94, 1305–1317. doi: 10.1037/a0015320 [DOI] [PubMed] [Google Scholar]
- Beal DJ (2015). ESM 2.0: State of the art and future potential of experience sampling methods in organizational research. Annual Review of Organizational Psychology and Organizational Behavior, 2, 383–407. doi: 10.1146/annurev-orgpsych-032414-111335 [DOI] [Google Scholar]
- Bergman ME, & Jean VA (2016). Where have all the “workers” gone? A critical analysis of the unrepresentativeness of our samples relative to the labor market in the industrial–organizational psychology literature. Industrial and Organizational Psychology, 9, 84–113. doi: 10.1017/iop.2015.70 [DOI] [Google Scholar]
- Bhaskar S, Hemavathy D, & Prasad S. (2016). Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. Journal of Family Medicine and Primary Care, 5, 780–784. doi: 10.4103/2249-4863.201153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodner T, Kraner M, Bradford B, Hammer L, & Truxillo D. (2014). Safety, health, and well-being of municipal utility and construction workers. Journal of Occupational and Environmental Medicine, 56, 771–778. doi: 10.1097/JOM.0000000000000178. [DOI] [PubMed] [Google Scholar]
- Burgard SA, & Ailshire JA (2013). Gender and time for sleep among U.S. adults. American Sociological Review, 78, 51–69. doi: 10.1177/0003122412472048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buxton OM, Karen Hopcia NP, Sembajwe G, Porter JH, Dennerlein JT, Kenwood C, & Sorensen G. (2012). Relationship of sleep deficiency to perceived pain and functional limitations in hospital patient care workers. Journal of Occupational and Environmental Medicine/American College of Occupational and Environmental Medicine, 54, 851–858. doi: 10.1097/jom.0b013e31824e6913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buxton OM, Quintiliani LM, Yang MH, Ebbeling CB, Stoddard AM, Pereira LK, & Sorensen G. (2009). Association of sleep adequacy with more healthful food choices and positive workplace experiences among motor freight workers. American Journal of Public Health, 99, 636–643. doi: 10.2105/ajph.2008.158501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, & Kupfer DJ (1989). The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Research, 28, 193–213. doi: 10.1016/j.psychres.2012.03.045 [DOI] [PubMed] [Google Scholar]
- Carskadon MA & Dement WC (2017). Normal Human Sleep: An Overview. In Kryger MH, Roth T, & Dement WC (Eds.), Principles and Practices of Sleep Medicine, 6th Edition (1516–1563). Philadelphia, PA: Elsevier. doi: 10.1016/b978-0-323-24288-2.00002-7 [DOI] [Google Scholar]
- Castronovo V, Scifo P, Castellano A, Aloia MS, Iadanza A, Marelli S, . . .Falini A. (2014). White matter integrity in obstructive sleep apnea before and after treatment. Sleep, 37, 1465–1475. doi: 10.5665/sleep.3994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2011) Effect of Short Sleep Duration on Daily Activities – United States, 2005–2008. Centers for Disease Control and Prevention Morbidity and Mortality Weekly Report, 60, 239–242. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/21368739 [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2015). Insufficient Sleep is a Public Health Problem. Retrieved from http://www.cdc.gov/features/dssleep/
- Christian MS, Bradley JC, Wallace JC, & Burke MJ (2009). Workplace safety: a meta-analysis of the roles of person and situation factors. Journal of Applied Psychology, 94, 1103–1127. doi: 10.1037/a0016172 [DOI] [PubMed] [Google Scholar]
- Colton HR, & Altevogt BM (2006). Functional and economic impact of sleep loss and sleep-related disorders. In Colton HR & Altevogt BM (Eds.) Sleep disorders and sleep deprivation: An unmet public health problem (pp. 137–172). Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Crain TL, Brossoit RM, & Fisher GG (in press). Work, nonwork, and sleep (WNS): A review and conceptual framework. Journal of Business and Psychology. doi: 10.1007/s10869-017-9521-x [DOI] [Google Scholar]
- Crain TL, Hammer LB, Bodner T, Kossek EE, Moen P, Lilienthal R, & Buxton OM (2014). Work–family conflict, family-supportive supervisor behaviors (FSSB), and sleep outcomes. Journal of Occupational Health Psychology, 19, 155–167. doi: 10.1037/a0036010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crain TL, Schonert-Reichl KA, & Roeser RW (2017). Cultivating teacher mindfulness: Effects of a randomized controlled trial on work, home, and sleep outcomes. Journal of Occupational Health Psychology, 22, 138–1152. doi: 10.1037/ocp0000043 [DOI] [PubMed] [Google Scholar]
- Cropley M, Dijk DJ, & Stanley N. (2006). Job strain, work rumination, and sleep in school teachers. European Journal of Work and Organizational Psychology, 15, 181–196. doi: 10.1080/13594320500513913 [DOI] [Google Scholar]
- Durmer JS, & Dinges DF (2005). Neurocognitive consequences of sleep deprivation. Seminars in Neurology, 25, 117–129. doi: 10.1055/s-2005-867080 [DOI] [PubMed] [Google Scholar]
- Elfering A, Grebner S, & Ebener C. (2015). Workflow interruptions, cognitive failure and near-accidents in health care. Psychology, Health & Medicine, 20, 139–147. doi: 10.1080/13548506.2014.913796 [DOI] [PubMed] [Google Scholar]
- Ganster DC, Crain TL, & Brossoit RM (2018). Physiological Measurement in I/O and OB: A Review and Recommendations for Future Use. Annual Review of Organizational Psychology and Organizational Behavior, 5, 267–293. 10.1146/annurev-orgpsych-032117-104613 [DOI] [Google Scholar]
- Garbarino S, Guglielmi O, Sanna A, Mancardi GL, & Magnavita N. (2016). Risk of occupational accidents in workers with obstructive sleep apnea: Systematic review and meta-analysis. Sleep, 39, 1211–1218. doi: 10.5665/sleep.5834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillen M. (2010). The NIOSH Construction Program: Research to practice, impact, and developing a National Construction Agenda. Journal of Safety Research, 41, 289–299. doi: 10.1016/j.jsr.2010.04.002 [DOI] [PubMed] [Google Scholar]
- Goel N, Rao H, Durmer J, & Dinges D. (2009). Neurocognitive consequences of sleep deprivation. Seminars in Neurology, 29, 320–339. doi: 10.1055/s-0029-1237117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner MA, Kripke DF, Yoon IY, & Youngstedt SD (2006). Criterion validity of the Pittsburgh Sleep Quality Index: Investigation in a non‐clinical sample. Sleep and Biological Rhythms, 4, 129–136. doi: 10.1111/j.1479-8425.2006.00207.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin MA, & Neal A. (2000). Perceptions of safety at work: A framework for linking safety climate to safety performance, knowledge, and motivation. Journal of Occupational Health Psychology, 5, 347–358. doi: 10.1037/l1076-8998.5.3.347 [DOI] [PubMed] [Google Scholar]
- Hale L, & Do DP (2007). Racial differences in self-reports of sleep duration in a population-based study. Sleep, 30, 1096–1103. doi: 10.1093/sleep/30.9.1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hülsheger UR, Lang JWB, Depenbrock F, Fehrmann C, Zijlstra FRH, & Alberts HJEM (2014). The power of presence: The role of mindfulness at work for daily levels and change trajectories of psychological detachment and sleep quality. Journal of Applied Psychology, 99, 1113–1128. doi: 10.1037/a0037702 [DOI] [PubMed] [Google Scholar]
- Irish LA, Kline CE, Gunn HE, Buysse DJ, & Hall MH (2015). The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Medicine Reviews, 22, 23–36. doi: 10.1016/j.smrv.2014.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansson M, & Linton SJ (2006). Psychosocial work stressors in the development and maintenance of insomnia: A prospective study. Journal of Occupational Health Psychology, 11, 241–248. doi: 10.1037/1076-8998.11.3.241 [DOI] [PubMed] [Google Scholar]
- Joo EY, Kim H, Suh S, & Hong SB (2014). Hippocampal substructural vulnerability to sleep disturbance and cognitive impairment in patients with chronic primary insomnia: Magnetic resonance imaging morphometry. Sleep, 37, 1189–1198. doi: 10.5665/sleep.3836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kao KY, Spitzmueller C, Cigularov K, & Wu H. (2016). Linking insomnia to workplace injuries: A moderated mediation model of supervisor safety priority and safety behavior. Journal of Occupational Health Psychology, 21, 91–104. doi: 10.1037/a0039144 [DOI] [PubMed] [Google Scholar]
- Karoly P. (1993). Mechanisms of self-regulation: A systems view. Annual Review of Psychology, 44, 23–52. doi: 10.1146/annurev.psych.44.1.23 [DOI] [Google Scholar]
- Kling RN, McLeod CB, & Koehoorn M. (2010). Sleep problems and workplace injuries in Canada. Sleep, 33, 611–618. doi: 10.1093/sleep/33.5.611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolb B, & Gibb R. (2014). Searching for the principles of brain plasticity and behavior. Cortex, 58, 251–260. doi: 10.1016/j.cortex.2013.11.012 [DOI] [PubMed] [Google Scholar]
- Kolb B, (1995). Brain Plasticity and Behavior. Mahwah, NJ: Lawrence Erlbaum Associates, Inc., Publishers. [Google Scholar]
- Landrigan CP, Rothschild JM, Cronin JW, Kaushal R, Burdick E, Katz JT, . . .Czeisler CA (2004). Effect of reducing interns’ work hours on serious medical errors in intensive care units. New England Journal of Medicine, 351, 1838–1848. doi: 10.1056/NEJMoa041406 [DOI] [PubMed] [Google Scholar]
- Lapierre LM, Hammer LB, Truxillo DM, & Murphy LA (2012). Family interference with work and workplace cognitive failure: The mitigating role of recovery experiences. Journal of Vocational Behavior, 81, 227–235. 10.1016/j.jvb.2012.07.007 [DOI] [Google Scholar]
- Larson GE, Alderton DL, Neideffer M, & Underhill E. (1997). Further evidence on dimensionality and correlates of the Cognitive Failures Questionnaire. British Journal of Psychology, 88, 29–38. doi: 10.1111/j.2044-8295.1997.tb02618.x [DOI] [Google Scholar]
- Leger D, Bayon V, Ohayon MM, Philip P, Ement P, Metlaine A, . . . Faraut B. (2014). Insomnia and accidents: Cross-sectional study (EQUINOX) on sleep-related home, work and car accidents in 5293 subjects with insomnia from 10 countries. Journal of sleep research, 23, 143–152. doi: 10.1111/jsr.12104 [DOI] [PubMed] [Google Scholar]
- Leigh J. (2011). Economic burden of occupational injury and illness in the United States. The Milbank Quarterly, 89, 728–772. doi: 10.1111/j.1468-0009.2011.00648.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim J, & Dinges DF (2010). A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychological Bulletin, 136, 375–389. doi: 10.1037/a0018883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linton SJ (2004). Does work stress predict insomnia? A prospective study. British Journal of Health Psychology, 9, 127–136. doi: 10.1348/135910704773891005 [DOI] [PubMed] [Google Scholar]
- Litwiller B, Snyder LA, Taylor WD, & Steele LM (2017). The relationship between sleep and work: A meta-analysis. Journal of Applied Psychology, 102, 682–699. doi: 10.1037/apl0000169 [DOI] [PubMed] [Google Scholar]
- Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft J. (2016). Prevalence of healthy sleep duration among adults – United States, 2014. Centers for Disease Control and Prevention Morbidity and Mortality Weekly Report. 65, 137–141. doi: 10.15585/mmwr.mm6506a1 [DOI] [PubMed] [Google Scholar]
- Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, . . . Buxton OM (2013). Measuring sleep: Accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep, 36, 1747–1755. doi: 10.5665/sleep.3142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin M. (1983). Cognitive failure: Everyday and laboratory performance. Bulletin of the Psychonomic Society, 21, 97–100. doi: 10.3758/BF03329964 [DOI] [Google Scholar]
- Mullins HM, Cortina JM, Drake CL, & Dalal RS (2014). Sleepiness at work: A review and framework of how the physiology of sleepiness impacts the workplace. Journal of Applied Psychology, 99, 1096–1112. doi: 10.1037/a0037885 [DOI] [PubMed] [Google Scholar]
- National Institute for Occupational Safety and Health. (2017). Construction Safety and Health. Retrieved from: https://www.cdc.gov/niosh/construction/default.html
- Neal A, Griffin MA, & Hart PM (2000). The impact of organizational climate on safety climate and individual behavior. Safety Science, 34, 99–109. doi: 10.1016/S09257535(00)00008-4 [DOI] [Google Scholar]
- Neikrug AB, & Ancoli-Israel S. (2010). Sleep disorders in the older adult – A mini-review. Gerontology, 56, 181–189. doi: 10.1159/000236900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Occupational Safety and Health Administration (2015). Commonly Used Statistics. Retrieved from www.osha.gov/oshstats/commonstats.html
- Occupational Safety and Health Administration (2016). Worker Safety Series – Construction. Retrieved from https://www.osha.gov/Publications/OSHA3252/3252.html
- Ohly S, Sonnentag S, Niessen C, & Zapf D. (2010). Diary studies in organizational research. Journal of Personnel Psychology, 9, 79–93. doi: 10.1027/1866-5888/a000009 [DOI] [Google Scholar]
- Park YM, & Kim SY (2013). Impacts of job stress and cognitive failure on patient safety incidents among hospital nurses. Safety and Health at Work, 4, 210–215. doi: 10.1016/j.shaw.2013.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilchur JJ, & Huffcut AI (1996). Effects of sleep deprivation on performance: A meta-analysis. Sleep, 19, 318–326. doi: 10.1093/sleep/19.4.318 [DOI] [PubMed] [Google Scholar]
- Podsakoff PM, MacKenzie SB, Lee JY, & Podsakoff NP (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology, 88, 879–903. doi: 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- Powell R, & Copping A. (2010). Sleep deprivation and its consequences in construction workers. Journal of Construction Engineering and Management, 136, 1086–1092. doi: 10.1061/(asce)co.1943-7862.0000211 [DOI] [Google Scholar]
- Rosekind MR, Gregory KB, Mallis MM, Brandt SL, Seal B, & Lerner D. (2010). The cost of poor sleep: Workplace productivity loss and associated costs. Journal of Occupational and Environmental Medicine, 52, 91–98. doi: 10.1097/JOM.0b013e3181c78c30 [DOI] [PubMed] [Google Scholar]
- Rosenzweig I, Glasser M, Crum WR, Kempton MJ, Milosevic M, McMillan A, . . . Morrell MJ (2016). Changes in neurocognitive architecture in patients with obstructive sleep apnea treated with continuous positive airway pressure. EBioMedicine, 7, 221–229. doi: 10.1016/j.ebiom.2016.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth T. (2007). Insomnia: definition, prevalence, etiology, and consequences. Journal of Clinical Sleep Medicine, 3(5 Suppl), S7–S10. [PMC free article] [PubMed] [Google Scholar]
- Salminen S, Oksanen T, Vahtera J, Sallinen M, Härmä M, Salo P, & Kivimäki M. (2010). Sleep disturbances as a predictor of occupational injuries among public sector workers. Journal of Sleep Research, 19, 207–213. doi: 10.1111/j.1365-2869.2009.00780.x [DOI] [PubMed] [Google Scholar]
- Shaffer J. (2016). Neuroplasticity and clinical practice: Building brain power for health. Frontiers in Psychology, 7, 1–12. doi: 10.3389/fpsyg.2016.01118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahly V, Berglund PA, Coulouvrat C, Fitzgerald T, Hajak G, Roth T, . . .Kessler RC (2012). The associations of insomnia with costly workplace accidents and errors: results from the America Insomnia Survey. Archives of General Psychiatry, 69, 1054–1063. doi: 10.1001/archgenpsychiatry.2011.2188 [DOI] [PubMed] [Google Scholar]
- Short MA, & Banks S. (2014). The functional impact of sleep deprivation, sleep restriction, and sleep fragmentation. Sleep Deprivation and Disease, 13–26. doi: 10.1007/978-1-4614-9087-6_2 [DOI] [Google Scholar]
- Simpson SA, Wadsworth EJ, Moss SC, & Smith AP (2005). Minor injuries, cognitive failures and accidents at work: Incidence and associated features. Occupational Medicine, 55, 99–108. doi: 10.1093/occmed/kqi035 [DOI] [PubMed] [Google Scholar]
- Sneddon A, Mearns K, & Flin R. (2013). Stress, fatigue, situation awareness and safety in offshore drilling crews. Safety Science, 56, 80–88. doi: 10.1016/j.ssci.2012.05.027 [DOI] [Google Scholar]
- Spector PE, & Brannick MT (2011). Methodological urban legends: The misuse of statistical control variables. Organizational Research Methods, 14, 287–305. doi: 10.1177/1094428110369842 [DOI] [Google Scholar]
- Swanson LM, Arnedt J, Rosekind MR, Belenky G, Balkin TJ, & Drake C. (2011). Sleep disorders and work performance: Findings from the 2008 National Sleep Foundation Sleep in America poll. Journal of Sleep Research, 20, 487–494. doi: 10.1111/j.1365-2869.2010.00890.x [DOI] [PubMed] [Google Scholar]
- Turkington PM, Sircar M, Saralaya D, & Elliott MW (2004). Time course of changes in driving simulator performance with and without treatment in patients with sleep apnoea hypopnoea syndrome. Thorax, 59, 56–59. [PMC free article] [PubMed] [Google Scholar]
- Uehli K, Mehta AJ, Miedinger D, Hug K, Schindler C, Holsboer-Trachsler E, . . Künzli N. (2014). Sleep problems and work injuries: A systematic review and meta-analysis. Sleep Medicine Reviews, 18, 61–73. doi: 10.1016/j.smrv.2013.01.004 [DOI] [PubMed] [Google Scholar]
- Walker MP, & Stickgold R. (2006). Sleep, memory, and plasticity. Annual Review of Psychology, 57, 139–166. doi: 10.1146/annurev.psych.56.091103.070307 [DOI] [PubMed] [Google Scholar]
- Wallace JC, & Chen G. (2005). Development and validation of a work-specific measure of cognitive failure: Implications for occupational safety. Journal of Occupational and Organizational Psychology, 78, 615–632. doi: 10.1348/096317905X37442 [DOI] [Google Scholar]
- Wallace JC, & Vodanovich SJ (2003). Workplace safety performance: Conscientiousness, cognitive failure, and their interaction. Journal of Occupational Health Psychology, 8, 316–327. doi: 10.1037/1076-8998.8.4.316 [DOI] [PubMed] [Google Scholar]
- Wang M, Beal DJ, Chan D, Newman DA, Vancouver JB, & Vandenberg RJ (2017). Longitudinal research: A panel discussion on conceptual issues, research design, and statistical techniques. Work, Aging and Retirement, 3, 1–24. doi: 10.1093/workar/waw033 [DOI] [Google Scholar]
- Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, . . . Malhotra RK (2015). Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep, 38, 843–844. doi: 10.5665/sleep.4716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L, Buysse DJ, Germain A, Moul DE, Stover A, Dodds NE, . . .Pilkonis PA (2012). Development of short forms from the PROMIS™ sleep disturbance and sleep-related impairment item banks. Behavioral Sleep Medicine, 10, 6–24. doi: 10.1080/15402002.2012.636266 [DOI] [PMC free article] [PubMed] [Google Scholar]