Abstract
Background:
Cannabis concentrates, including dabs, contain extremely high levels of Δ9-tetrahydrocannabinol (THC). Although these products appear to be gaining popularity among recreational cannabis consumers, little data exists regarding concentrate use in the US. We conducted a national web-based survey to examine patterns of concentrate use, specifically dabbing.
Methods:
4077 respondents completed a survey designed to assess the use of conventional flower cannabis relative to dabs. Individuals provided information about frequency and magnitude of use, and also completed the Marijuana Motives Measure and Severity of Dependence Scale to examine whether dab users have different motives for use and/or demonstrate more severe consequences of use compared to those who only use conventional flower products.
Results:
58% of respondents reported they had tried dabs at least once and 36.5% endorsed regular use (once a month or more). Those who use regularly use dabs were significantly more likely to report using for experimentation (feeling “curious”) relative to reasons for using conventional flower products. Interestingly, motives reflecting positive effects (i.e., coping, sleep problems, relieving social anxiety) were endorsed more highly for flower use. In addition, regular dab users reported being more worried about their use of cannabis products relative to those who had tried dabs but did not use regularly.
Conclusions:
Results indicate that cannabis consumers do not necessarily choose dabs over flower products for positive effects, but rather appear to choose these highly potent products for experimentation. As concentrate use may lead to increased cannabis-related problems, studies directly assessing concentrate users are needed.
Keywords: Marijuana, Cannabis, Concentrates, Dabs, Potency, THC, Survey
1. Introduction
Literature regarding the impact of cannabis use has primarily focused on recreational users who typically choose products with high levels of Δ9-tetrahydrocannabinol (THC), the main psychoactive constituent of cannabis, responsible for the desired “high” or mood-altering effects. Traditionally, most individuals use flower (“bud”) in joint, blunt, bong, spliff, or bowl preparations. Data suggests a significant increase in potency (THC concentration) of flower products, rising from 4% to 12% between 1995 and 2014 (ElSohly et al., 2016). Moreover, there has been a shift toward alternative modes of use and the use of novel products with even higher THC concentrations. These potent products termed concentrates, provide a faster and more intense “high.”
Concentrates are made by extracting THC from dried cannabis flower using a variety of methods (Raber et al., 2015). Non-solvent concentrates include kief, resin, and different types of hash and are made by rubbing plant material or utilizing cold water to separate trichomes from the plant. Solvent-based extraction methods yield a range of products (butane hash oil [BHO], tinctures, etc.), and either require the use of supercritical extraction methods (e.g., CO2 extraction) or chemical solvents including hexane, isopentane, isopropyl alcohol, acetone, propane or butane. While CO2 extraction avoids exposure to potentially harmful chemicals, solvent-based methods remain common. As a result, residual solvents are often detected in concentrates, posing risks to users’ health. In fact, Raber et al. (2015) detected residual solvents in 83.3% of concentrate samples analyzed. Extraction methods yield a variety of concentrated compounds, typically named for the product’s consistency, including shatter, wax and “budder”. Concentrates can be used in a number of ways, including “dabbing”—a process in which concentrates are placed on a boiling surface using a rig that vaporizes a designated amount (a “dab”); the user subsequently inhales the vapor, delivering a single, extremely high dose of THC in a single bolus. Concentrates can also be used with other routes of administration, including vape pens, which allow users to place concentrates (i.e., shatter, wax) directly in the pen’s “tank” to be vaporized or to use cartridges containing concentrated oil. Compared to dabbing, vaporizers provide an opportunity for users to titrate their intake, rather than receiving a single, highly potent ‘hit’ at once.
In addition to concerns regarding residual solvents, concentrates have significantly higher levels of THC relative to conventional flower products, which may have negative implications for consumers. Recent analyses of concentrate products reported average THC levels of 60.3% (Raber et al., 2015) to 68.7% (Smart et al., 2017); however, some concentrates have been shown to approach 75–80% (Stogner and Miller, 2015), and those sold at dispensaries frequently list even higher THC potencies on packaging (> 90% THC). Use of concentrates is potentially concerning as THC has been associated with adverse physiological (i.e., increased heart rate) (Zuurman et al., 2009) and psychological effects; paranoia, anxiety, and hallucinations have been observed in those administered high doses of THC (Bhattacharyya et al., 2010; D’Souza et al., 2004; Fusar-Poli et al., 2009; Winton-Brown et al., 2011). Further, acute administration studies suggest that higher doses of THC have a negative impact on cognition. For example, D’Souza et al. (2004) reported that THC administration produced acute decrements in cognitive performance, including poorer word recall and impaired performance on measures assessing distractibility, verbal fluency and working memory which appeared to be dose-dependent. Similarly, Ramaekers et al. (2006) administered placebo, 4% THC and 10% THC “marijuana cigarettes” to recreational cannabis consumers. Participants performed most poorly after administration of the higher potency product across measures of motor control, executive function, and impulsivity. In addition, increased severity of dependence (Freeman and Winstock, 2015) and reduced creativity (Kowal et al., 2015) have also been observed with higher potency THC. Only one study thus far has examined the effect of cannabis potency on brain structure; Rigucci et al. (2016) observed alterations in corpus callosum white matter microstructure in self-reported high-potency cannabis users compared to low-potency users and controls. Finally, some studies note an increased risk of psychosis among self-reported high-potency cannabis users relative to low potency users (Large and Nielssen, 2017) and non-users (Di Forti et al., 2015), and two case reports have documented psychosis following concentrate use (Keller et al., 2016; Pierre et al., 2016).
In a recent study which analyzed tweets about concentrate use, Cavazos-Rehg et al. (2016) reported that common themes included mentions of extreme effects and the intense high resulting from use. Concentrate users also tweeted about negative physiological consequences, including passing out, respiratory effects (e.g., coughing, lung pain), nausea/vomiting, and loss of bodily control. Despite these negative experiences, some report a preference for concentrates. In the first known survey of concentrate users (specifically those who dab), Loflin and Earleywine (2014) found that the most common reasons reported for dabbing were to create a different kind of high, a stronger intoxicating effect, and because fewer hits are necessary to achieve desired effects. Although analyses did not support the hypothesis that dabbing resulted in more problems, accidents, or greater negative side effects relative to conventional flower use, increased self-reported tolerance and withdrawal were noted among dab users (Loflin and Earleywine, 2014). Further, in a survey of college students, Meier (2017) found that more frequent use of BHO was related to higher levels of physical dependence. Using an international survey, Chan et al. (2017) reported that BHO use was related to higher self-reported depression and anxiety, weaker positive effects and stronger negative effects compared to conventional flower use. Despite the increased popularity of concentrate products, few studies have examined rates of concentrate use within the US. In a preliminary study, Zhang et al. (2016) analyzed Google data to examine the extent of online searches focused on dabbing between 2004 and 2015. Dab-focused searches increased over time, suggesting greater public interest. Searches were performed more often in western states than other regions, and the total number of searches was higher in states with legal medical and recreational cannabis than those with only medical cannabis or states without any legalization. Similarly, another study reported that dab-related tweets were highest in states with legalized medical or recreational cannabis and lowest in states where cannabis use is prohibited (Daniulaityte et al., 2015). Regarding the scope of concentrate use, in a US-based survey of 673 cannabis users recruited from a web-forum focused on drug-related experiences, 66% of respondents reported concentrate use (Daniulaityte et al., 2017). Further, authors reported that living in states with less restrictive cannabis policies, being male, being younger, using other drugs, using flower cannabis daily, and lower perceived risk of cannabis use all conferred a greater risk of using concentrates. Finally, some studies have specifically assessed concentrate use in Washington State, one of the first states to legalize recreational cannabis. Carlini et al. (2017) reported that concentrate sales increased 770% from 2014–2015 to 2015–2016 in Washington while flower products, edibles, and cannabis drinks increased 400–488%. Similarly, Smart et al. (2017) reported that although cannabis flower remains the most frequently purchased product type in Washington, concentrate sales increased 145.8% over two years (October 2014–September 2016), accounting for 21% of product sales.
Overall, data suggest a significant, rapid increase in concentrate use across the nation. Despite growing popularity, little data exists regarding concentrate use, including prevalence, patterns of use, and other related variables. Given the paucity of data and increasing use of these products, we developed a comprehensive, internet-based survey to examine concentrate use, specifically the use of dabs, among US cannabis users consumers. The survey assessed frequency and magnitude of use, product selection, motives for use and consequences of use.
2. Material and methods
2.1. Sample selection
Potential participants aged 18 and older were recruited via self-selection by responding to Facebook advertisements for an online survey about cannabis use. Advertisements were generated through the site’s proprietary marketing algorithms and targeted those who had “liked” pages associated with cannabis use or pro-cannabis interest (e.g. High Times, NORML). The total reach estimated by Facebook was 202,921. Additionally, links were posted on the Cognitive and Clinical Neuroimaging Core’s Facebook page (@MJBrainStudy), Twitter (@CCNCBrainStudy), and on the “Cannabis Extracts” Reddit forum (https://www.reddit.com/r/CannabisExtracts/).
Prior to entering the survey, participants were presented with an informed consent page approved by Partners Healthcare; only respondents who gave consent to participate were directed to the survey. Compensation was not provided for participation. Automatic data collection procedures were disabled to preserve anonymity except for spam deterrence features (e.g., preventing multiple responses from the same IP address). Study procedures were reviewed and approved by the Partners Institutional Review Board.
2.2. Survey content
The Internet survey took approximately 20 min to complete and was hosted on SurveyMonkey.com, with data collected over a 64-day period (12/20/2016–2/22/2017). Survey content included questions addressing demographics, general substance use history, and cannabis use history, which included a subset of questions designed to specifically assess current and former concentrate use, namely dabs. In addition, individuals who endorsed cannabis use completed a modified version of the Marijuana Motives Measure (MMM) (Simons et al., 1998), which assesses motives/reasons for use (only 15 of the original 25-items from the MMM were chosen for the survey based on factor loading scores, and an additional question was added to query about the use of cannabis for medical symptoms). Participants were asked to complete the MMM to assess motives for conventional flower use and additionally, individuals who endorsed dabbing completed the MMM a second time to assess motives for dabbing. Participants also completed the Severity Dependence Scale (SDS), a five-item questionnaire assessing problematic cannabis use (Piontek et al., 2008).
2.3. Data analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS) version 24 (IBM Corp., Armonk, NY). Descriptive statistics were performed on the entire sample and to better assess cannabis use patterns across the US, descriptive statistics were also performed on three discrete groups. Survey respondents were subdivided by legal status of cannabis at the time of the survey (2016): 8 states and DC with legalized recreational (and medical) cannabis, 20 states with full medical cannabis programs, and 22 states which prohibited cannabis. Notably, the latter group also included states only allowing access to CBD products, as concentrates are illegal in these states. Chi-square tests were utilized to assess nominal (e.g., gender) and ordinal data (e.g., income). In addition, analyses of variance (ANOVAs) were used to assess scalar data (e.g., age) or, if homogeneity of variance was unequal between groups, non-parametric, Kruskal-Wallis tests were used. Wilcoxon signed rank tests were performed on the MMM data for individuals reporting use of both flower and concentrate products in order to compare differences in the ordinal ranking for motives of use between products. Two-tailed t-tests were used (α = .05) and bootstrapped 95% confidence intervals were calculated using 1000 samples, which were not bias-corrected or accelerated. For the SDS, regular dab users were divided into current and former users; chi-square tests were used for the ordinal SDS rankings, while ANOVAs were used for total SDS scores, which were considered scalar.
3. Results
3.1. Sample characteristics and participation rate
As noted in Fig. 1, a total of 6819 individuals clicked on the survey link; of these, 5412 provided consent. Among those who consented and began the survey, 4077 (75.33% participation rate) completed demographics questions and provided information about their cannabis use and were therefore included in data analyses. Demographic information (age, gender, ethnicity, income, and education) are provided in Table 1, and basic information regarding patterns of cannabis, alcohol, and other drug use are provided in Table 2. Notably, the majority of participants who began the survey completed the entire survey (3674 participants; 67.89% of the total number of individuals who provided consent).
Fig. 1.
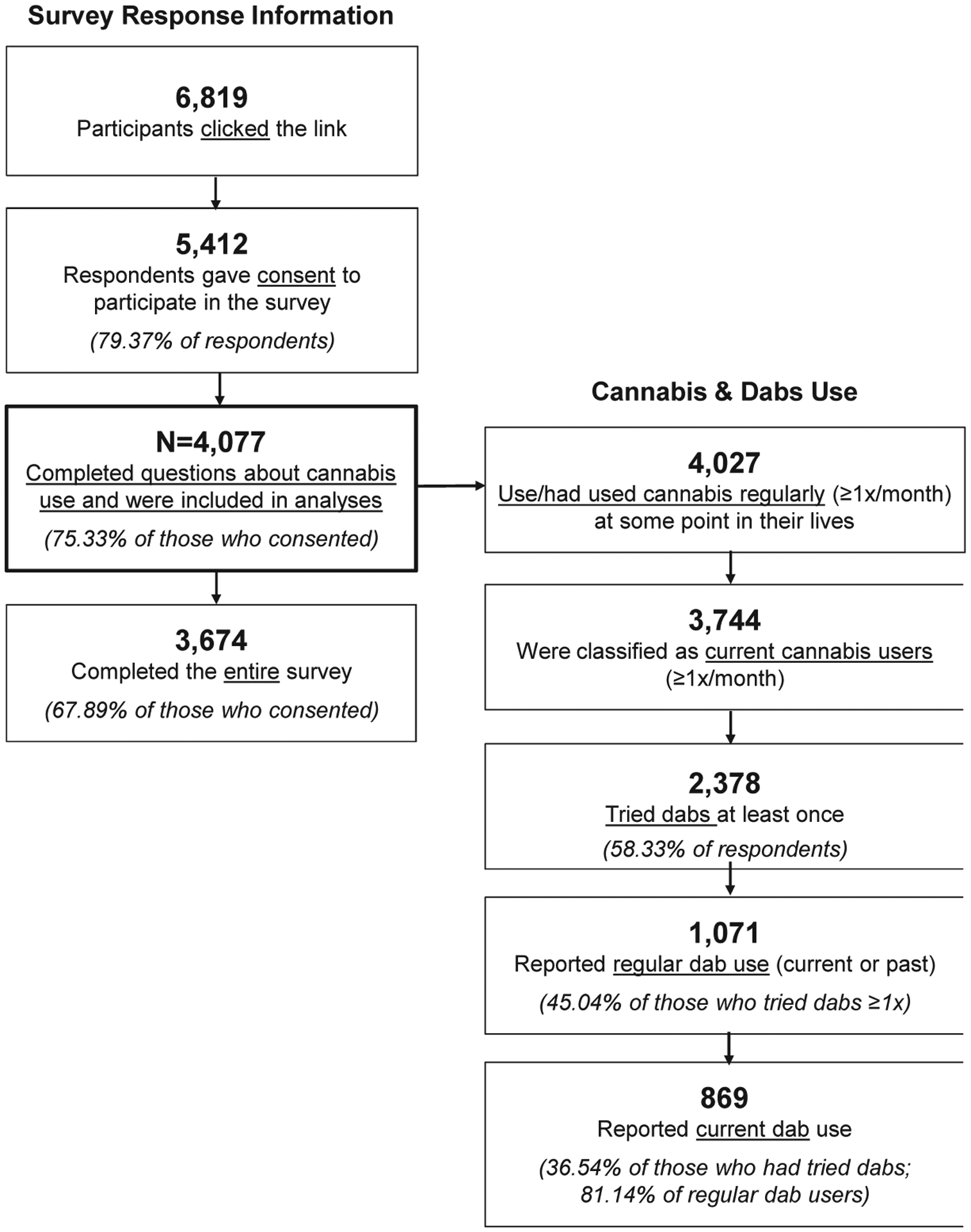
Schematic classifying individuals based on degree of survey completion and cannabis and dabs use status.
Table 1.
Demographic Data: total sample, current flower users, and current dab users.
| Demographic Variable | Total Sample (N = 4077) M (SD) or n (%) |
Current Flower Users (N = 3744) M (SD) or n (%) |
Current Dab Users (N = 869) M (SD) or n (%) |
|---|---|---|---|
| Age | 44.09 (13.84) | 43.71 (13.73) | 38.20 (13.48) |
| Gender | |||
| Male | 2459 (60.31%) | 2266 (60.52%) | 617 (71.00%) |
| Female | 1599 (39.22%) | 1460 (39.00%) | 248 (28.54%) |
| Other | 13 (0.32%) | 13 (0.35%) | 4 (0.46%) |
| Non-Response | 6 (0.15%) | 5 (0.13%) | 0 (0.00%) |
| Race | |||
| American Indian | 273 (6.70%) | 259 (6.92%) | 56 (6.44%) |
| Asian | 29 (0.71%) | 28 (0.75%) | 10 (1.15%) |
| Black/African American | 193 (4.73%) | 183 (4.89%) | 20 (2.30%) |
| Hawaiian/Pacific Islander | 22 (0.54%) | 20 (0.53%) | 7 (0.81%) |
| White | 3590 (88.05%) | 3291 (87.90%) | 780 (89.76%) |
| Multiracial | 211 (5.18%) | 255 (6.81%) | 64 (7.36%) |
| Prefer not to answer | 268 (6.57%) | 194 (5.18%) | 51 (5.87%) |
| Ethnicity | |||
| Non-Hispanic | 3175 (77.88%) | 2908 (77.67%) | 675 (77.68%) |
| Hispanic | 273 (6.70%) | 256 (6.84%) | 61 (7.02%) |
| Unknown | 329 (8.07%) | 313 (8.36%) | 71 (8.17%) |
| Prefer Not to Answer | 300 (7.36%) | 267 (7.13%) | 62 (7.13%) |
| Annual Income | |||
| $0–$29,999 | 1844 (45.23%) | 1694 (45.25%) | 343 (39.47%) |
| $30,000–$39,999 | 608 (14.91%) | 558 (14.90%) | 139 (16.00%) |
| $40,000–$49,999 | 406 (9.96%) | 380 (10.15%) | 86 (9.90%) |
| $50,000–$59,999 | 304 (7.46%) | 280 (7.48%) | 71 (8.17%) |
| $60,000–$69,999 | 239 (5.86%) | 216 (5.77%) | 58 (6.67%) |
| $70,000–$79,999 | 182 (4.46%) | 165 (4.41%) | 47 (5.41%) |
| $80,000–$89,999 | 118 (2.89%) | 112 (2.99%) | 32 (3.68%) |
| $90,000–$99,999 | 96 (2.35%) | 87 (2.32%) | 25 (2.88%) |
| $100,000–$149,999 | 180 (4.42%) | 161 (4.30%) | 43 (4.95%) |
| $150,000+ | 100 (2.45%) | 91 (2.43%) | 25 (2.88%) |
| Non-Response | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) |
| Education | |||
| Partial High Schoola | 338 (8.29%) | 317 (8.47%) | 62 (7.13%) |
| High School Diplomab | 1304 (31.98%) | 1175 (31.38%) | 254 (29.23%) |
| Associate’s Degreec | 832 (20.41%) | 772 (20.62%) | 193 (22.21%) |
| Partial College | 991 (24.31%) | 919 (24.55%) | 233 (26.81%) |
| Bachelor’s Degree | 340 (8.34%) | 311 (8.31%) | 78 (8.98%) |
| Master’s Degree | 92 (2.26%) | 84 (2.24%) | 21 (2.42%) |
| Doctoral Degree | 22 (0.54%) | 21 (0.56%) | 5 (0.58%) |
| Other | 14 (0.34%) | 12 (0.32%) | 2 (0.23%) |
| Non-Response | 144 (3.53%) | 133 (3.55%) | 0 (0.00%) |
Partial/Currently Enrolled in High School/GED.
High School Diploma or Equivalent (GED/HiSET, Vocational High School).
Associate’s Degree/Specialized Training/Vocational Training Program.
Table 2.
Substance Use Data: Total Sample, Current Flower Users, and Current Dab Users.
| Substance Use Variable | Total Sample (N = 4077) M (SD) or n (%) |
Current Flower Users (N = 3744) M (SD) or n (%) |
Current Dab Users (N = 869) M (SD) or n (%) |
|---|---|---|---|
| Current Alcohol Use | |||
| Daily | 116 (2.85%) | 109 (2.91%) | 17 (1.96%) |
| 3–6 Days/Week | 358 (8.78%) | 339 (9.05%) | 66 (7.59%) |
| 1–2 Day(s)/Week | 517 (12.68%) | 482 (12.87%) | 126 (14.50%) |
| 1–2x/Month | 836 (20.51%) | 762 (20.35%) | 192 (22.09%) |
| Several Times/Year | 1029 (25.24%) | 950 (25.37%) | 211 (24.28%) |
| Never | 1221 (29.95%) | 1102 (29.43%) | 257 (29.57%) |
| Non-Response | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) |
| Non-Cannabis Substance Use a | |||
| Using ≥ 1x/Month | 306 (7.51%) | 291 (7.77%) | 57 (6.56%) |
| Using < 1x/Month | 3771 (92.49%) | 3453 (92.23%) | 812 (93.44%) |
| Non-Response | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) |
| Cannabis Demographics | |||
| Age First Tried Cannabis | 15.18 (4.75) | 15.00 (4.32) | 14.27 (3.22) |
| Age of Regular Cannabis Use | 19.98 (8.49) | 18.92 (8.33) | 17.43 (6.88) |
| Age First Tried Concentrates | – | – | 33.47 (13.46) |
| Current Flower Use | |||
| ≥ Once Day | 2649 (64.97%) | 2649 (70.75%) | 733 (84.35%) |
| > Once/Week but < Once/Day | 686 (16.83%) | 686 (18.32%) | 96 (11.05%) |
| ≤ Once/Week | 409 (10.03%) | 409 (10.92%) | 36 (4.14%) |
| Not a Current User | 257 (6.30%) | 0 (0.00%) | 4 (0.46%) |
| Non-Response | 76 (1.86%) | 0 (0.00%) | 0 (0.00%) |
| Preferred Mode of Cannabis Use | |||
| Joint/Blunt/Spliff | 1276 (31.30%) | 1168 (31.20%) | 175 (20.14%) |
| Bowl/Pipe/One-Hitter | 955 (23.42%) | 882 (23.6%) | 113 (13.00%) |
| Bong/Water Pipe/Bubbler | 590 (14.47%) | 533 (14.24%) | 97 (11.16%) |
| Dabbing | 560 (13.74%) | 534 (14.26%) | 359 (41.31%) |
| Edibles | 320 (7.85%) | 288 (7.69%) | 53 (6.10%) |
| Vaporizer/Vape | 317 (7.78%) | 296 (7.91%) | 66 (7.59%) |
| Non-Response | 59 (1.45%) | 0 (0.00%) | 0 (0.00%) |
Other substances queried: cocaine, speed/amphetamines, heroin, hallucinogens (e.g. LSD, mushrooms), steroids, prescription drugs taken recreationally (e.g. Adderall, Xanax, opioids), and other drugs such as ecstasy, cough syrup, and inhalants.
3.2. Patterns of cannabis concentrate use (dabbing)
Of the 4077 respondents, 58% reported dabbing at least once. Among those who had tried dabs, 45.04% reported regular use of dabs (defined as “once a month or more”) at some point in their lives, and 36.54% reported current regular concentrate use; see Fig. 1. Of note, 13.74% of all respondents indicated that their preferred mode of use was dabbing (Table 2). Patterns of use were also examined among the 869 current, regular concentrate users in terms of frequency, magnitude, and money spent on concentrates per month; see Table 3. Nearly three-fourths of those who endorsed current dabbing reported using at least once a week. Moreover, 37.17% of current users reported dabbing more than once per day, the most frequently reported pattern of use. Over half of respondents reported using between 1–5 g per month, but a significant number of individuals (20.94%) also indicated that someone else buys/gives dabs to them and were, therefore, unable to report total amount used.
Table 3.
Patterns of Current Dab Use (n = 869).
| Variable | n (%) |
|---|---|
| How often do you currently use dabs? | |
| More than once a day | 323 (37.17%) |
| Once a day | 83 (9.55%) |
| 6–7 times a week | 24 (2.76%) |
| 4–5 times a week | 35 (4.03%) |
| 2–3 times a week | 113 (13.00%) |
| Once a week | 69 (7.94%) |
| 2–3 times a month | 130 (14.96%) |
| Once a month | 87 (10.01%) |
| Non-Response | 5 (0.58%) |
| How much are you spending on concentrates for dabbing each month? | |
| < $25 | 97 (11.16%) |
| $25–$50 | 125 (14.38%) |
| $50–$75 | 101 (11.62%) |
| $75–$100 | 123 (14.15%) |
| $100–$150 | 76 (8.75%) |
| $150 or more | 160 (18.41%) |
| Someone else buys it or gives it to me | 182 (20.94%) |
| Non-Response | 5 (0.58%) |
| What quantity of concentrates are you buying or making each month? | |
| 1/4 g | 14 (1.61%) |
| 1/2 g | 32 (3.68%) |
| 1 g | 188 (21.63%) |
| 2–3 g | 203 (23.36%) |
| 3–4 g | 1 (0.12%) |
| 4–5 g | 159 (18.30%) |
| 5–10 g | 17 (1.96%) |
| 10–15g | 24 (2.76%) |
| 15–20 g | 10 (1.15%) |
| 20–30 g | 11 (1.27%) |
| 30+ g | 15 (1.73%) |
| Someone else buys it or gives it to me | 144 (16.57%) |
| Other (please specify) | 46 (5.29%) |
| Non-Response | 5 (0.58%) |
Analyses examining patterns of use based on legalization status (recreational vs medical vs prohibited; Fig. 2) indicated that age of onset of cannabis use was similar across groups (18–19 years old; p = .135). Although results suggested a significant between-group difference for age at which individuals first tried dabs (F = .118, p = .044), post hoc analyses revealed only a trend between recreational states and medical states (p = .051). Interestingly, the age at which individuals first tried dabs was slightly older in recreational states (37.16 years old) versus medical states (35.42 years old). No differences were observed between states with prohibition (35.83 years old) and those with recreational and/or medical legislation. Group differences also emerged regarding patterns of use for both flower products and dabs (Table 4). Specifically, significant differences were noted between groups in terms of the proportion of individuals reporting current flower use (X2 = 40.058, p < .001) and the proportion reporting current dab use (X2 = 58.786, p < .001). Perhaps not surprisingly, more individuals from recreational states reported using flower products “daily or more,” relative to those from states with only medical cannabis or where cannabis is prohibited. This same pattern was observed for dabs; dabbing “daily or more” was reported most often in recreational states. These statistics represent data from the currently sample only and are not meant to serve as estimates of national prevalence.
Fig. 2.
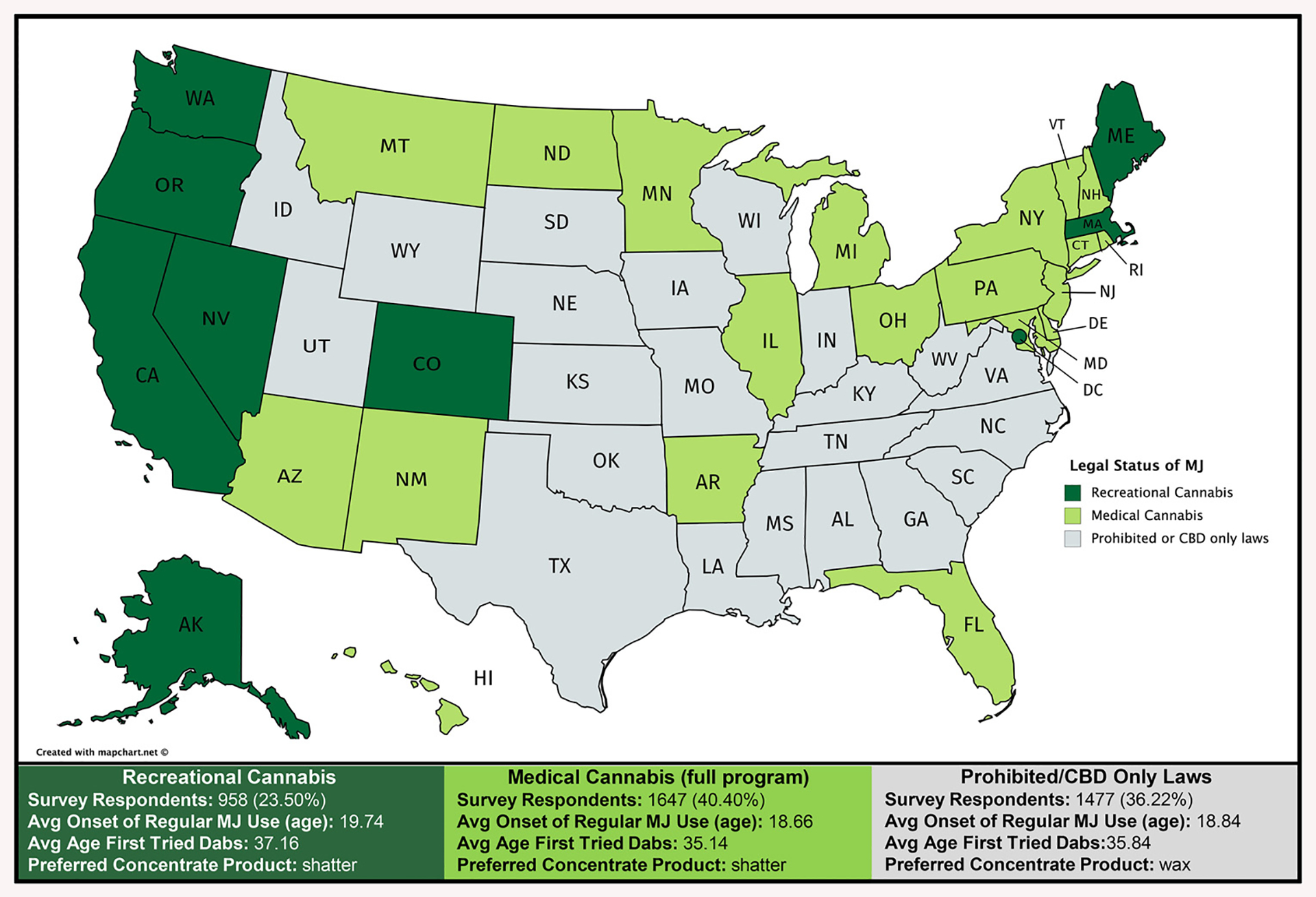
Information about cannabis and concentrate use based on 2016 legal status.
Note: States were categorized into three groups based on cannabis legalization status in 2016, the time at which the survey was launched: 1) recreational (and medical) cannabis legalized, 2) medical cannabis programs and 3) prohibited or only allow limited access to CBD. For each of these three groups, the number of respondents, average age of onset of regular cannabis use, average age that individuals first tried dabs, and preferred type of concentrate product are provided.
Table 4.
Comparison of Cannabis Use Frequencies based on Cannabis Legalization Status.
| Recreational Cannabis | Medical Cannabis | Prohibited or CBD Only | ||||
|---|---|---|---|---|---|---|
| Count | Percent | Count | Percent | Count | Percent | |
| Use of Flower | X2 = 40.058, p < .001 | |||||
| ≥ Once Day | 673 | 72.0%a,b | 1091 | 67.3%a,c | 885 | 61.3%b,c |
| > Once/Week but < Once/Day | 130 | 13.9%a,b | 288 | 17.8%a | 268 | 18.6%b |
| ≤ Once/Week | 93 | 9.9% | 144 | 8.9%a | 172 | 11.9%a |
| Not a Current Flower User | 39 | 4.2%a | 99 | 6.1% | 119 | 8.2%a |
| Use of Dabs | X2 = 58.786, p < .001 | |||||
| ≥ Once Day | 194 | 49.1%a,b | 137 | 33.9%a | 75 | 28.2%b |
| > Once/Week but < Once/Day | 60 | 15.2% | 70 | 17.3% | 42 | 15.8% |
| ≤ Once/Week | 100 | 25.3% | 119 | 29.5% | 67 | 25.2% |
| Not a Current Concentrate User | 41 | 10.4%a,b | 78 | 19.3%a,c | 82 | 30.8%b,c |
Superscript letters denote significant between-group differences between recreational, medical, and/or prohibited/CBD only states (2-group analyses), α = .05.
3.2.1. Marijuana motives measure (MMM)
Frequencies of responses across items of the MMM were calculated for both flower products and dabs (Table 5). The most common reasons for cannabis use, regardless of product type, were related to the perceived low risk associated with use (“safer than alcohol,” “not a dangerous drug”), and enjoyable effects. Moreover, results revealed several significant differences in motives for use of flower products versus dabs. The following reasons were endorsed significantly more often for flower relative to dabs: enjoyable effects (p < .001); to cope with problems, depression, or medical symptoms (all ps < .001); using cannabis while drunk (p < .001); celebration of a special occasion (p = .009); to relax when feeling social anxiety (p < .001); perceived relative low risk/danger (ps < .001); and to facilitate sleep (p < .001). A trend was also noted for flower users to endorse cannabis use as a result of boredom (p = .080). Interestingly, only one reason was more highly endorsed for dabs, which was experimentation (feeling “curious,” p < .001), although a trend also emerged for reasons of conformity (“to be cool,” p = .062). Use of flower and dabs did not differ based on ability to achieve altered states of perception (p = .103) or access to products (p = .450).
Table 5.
Differences in Marijuana Motives Measure (MMM) Ratings for Flower and Concentrates Products in Individuals Who Reported Trying Concentrates: Paired Wilcoxon Signed Rank Tests (n = 2777).
| MMM Variable | Cannabis Product | Almost Never/Never (1) | Some of the Time (2) | Half of the Time (3) | Most of the Time (4) | Almost Always/Always (5) | Wilcoxon Signed Rank Testa (1-tailed) | ||
|---|---|---|---|---|---|---|---|---|---|
| Mean | 95% CI | p (r) | |||||||
| Enjoyment | |||||||||
| To enjoy the effects of it | Flower | 51 (2.24%) | 237 (10.41%) | 206 (9.05%) | 487 (21.39%) | 1296 (56.92%) | 4.20 | 0.467, 0.591 | <.001 |
| Concentrate | 303 (13.31%) | 344 (15.11%) | 182 (7.99%) | 410 (18.01%) | 1038 (45.59%) | 3.67 | (.218) | ||
| Conformity | |||||||||
| To be cool | Flower | 2106 (92.49%) | 123 (5.40%) | 14 (0.61%) | 5 (0.22%) | 29 (1.27%) | 1.12 | −0.043, 0.001 | .062 (.025) |
| Concentrate | 2103 (92.36%) | 100 (4.39%) | 29 (1.27%) | 10 (0.44%) | 35 (1.54%) | 1.14 | |||
| Coping | |||||||||
| To forget your problems | Flower | 1249 (54.85%) | 669 (29.38%) | 170 (7.47%) | 80 (3.51%) | 109 (4.79%) | 1.74 | 0.136, 0.212 | <.001 |
| Concentrate | 1537 (67.50%) | 440 (19.32%) | 144 (6.32%) | 64 (2.81%) | 92 (4.04%) | 1.57 | (.121) | ||
| You were depressed | Flower | 790 (34.69%) | 836 (36.71%) | 281 (12.34%) | 177 (7.77%) | 193 (8.48%) | 2.19 | 0.369, 0.451 | <.001 |
| Concentrate | 1321 (58.01%) | 551 (24.20%) | 151 (6.63%) | 105 (4.61%) | 149 (6.54%) | 1.78 | (.244) | ||
| To relieve medical symptomsb | Flower | 93 (4.09%) | 248 (10.90%) | 261 (11.47%) | 448 (19.68%) | 1226 (53.87%) | 4.08 | 0.506, 0.610 | <.001 |
| Concentrate | 397 (17.44%) | 323 (14.19%) | 240 (10.54%) | 316 (13.88%) | 1000 (43.94%) | 3.53 | (.257) | ||
| Experimentation | |||||||||
| You were curious about cannabis | Flower | 1701 (74.70%) | 372 (16.34%) | 47 (2.06%) | 48 (2.11%) | 109 (4.79%) | 1.46 | −0.321, | <.001 |
| Concentrate | 1516 (66.58%) | 351 (15.42%) | 114 (5.01%) | 102 (4.48%) | 194 (8.52%) | 1.73 | -0.223 | (.150) | |
| Boredom | |||||||||
| You had nothing better to do | Flower | 1487 (65.31%) | 541 (23.76%) | 122 (5.36%) | 67 (2.94%) | 60 (2.64%) | 1.54 | −0.005, 0.066 | .080 (.023) |
| Concentrate | 1625 (71.37%) | 384 (16.86%) | 121 (5.31%) | 55 (2.42%) | 92 (4.04%) | 1.51 | |||
| Alcohol | |||||||||
| You were drunk | Flower | 1793 (78.74%) | 381 (16.73%) | 45 (1.98%) | 20 (0.88%) | 38 (1.67%) | 1.30 | 0.068, 0.122 | <.001 |
| Concentrate | 1989 (87.35%) | 191 (8.39%) | 49 (2.15%) | 16 (0.70%) | 32 (1.41%) | 1.20 | (.102) | ||
| Celebration | |||||||||
| It was a special occasion | Flower | 779 (34.21%) | 975 (42.82%) | 181 (7.95%) | 109 (4.79%) | 233 (10.23%) | 2.14 | 0.018, 0.119 | .009 (.035) |
| Concentrate | 958 (42.07%) | 790 (34.69%) | 170 (7.47%) | 126 (5.53%) | 233 (10.23%) | 2.07 | |||
| Altered Perception | |||||||||
| To alter your perspective | Flower | 994 (43.65%) | 686 (30.13%) | 204 (8.96%) | 208 (9.13%) | 185 (8.12%) | 2.08 | −0.006, 0.081 | .103 (.022) |
| Concentrate | 1137 (49.93%) | 554 (24.33%) | 181 (7.95%) | 161 (7.07%) | 244 (10.72%) | 2.04 | |||
| Social Anxiety | |||||||||
| To relax in an insecure situation | Flower | 374 (16.43%) | 724 (31.80%) | 274 (12.03%) | 395 (17.35%) | 510 (22.40%) | 2.98 | 0.419, 0.527 | <.001 |
| Concentrate | 772 (33.90%) | 644 (28.28%) | 209 (9.18%) | 248 (10.89%) | 404 (17.74%) | 2.50 | (.226) | ||
| Relative Low Risk | |||||||||
| It is safer than drinking alcohol | Flower | 256 (11.24%) | 187 (8.21%) | 98 (4.30%) | 307 (13.48%) | 1429 (62.76%) | 4.08 | 0.305, 0.423 | <.001 |
| Concentrate | 511 (22.44%) | 159 (6.98%) | 90 (3.95%) | 218 (9.57%) | 1299 (57.05%) | 3.72 | (.157) | ||
| It is not a dangerous drug |
Flower | 289 (12.69%) | 77 (3.38%) | 43 (1.89%) | 219 (9.62%) | 1649 (72.42%) | 4.26 | 0.374, 0.497 | <.001 |
| Concentrate | 474 (20.82%) | 121 (5.31%) | 100 (4.39%) | 224 (9.84%) | 1358 (59.64%) | 3.82 | (.179) | ||
| Sleep | |||||||||
| You are having problems sleeping | Flower | 176 (7.73%) | 618 (27.14%) | 371 (16.29%) | 393 (17.26%) | 719 (31.58%) | 3.38 | 0.504, 0.608 | <.001 |
| Concentrate | 609 (26.75%) | 562 (24.68%) | 284 (12.47%) | 277 (12.17%) | 545 (23.94%) | 2.82 | (.265) | ||
| Availability | |||||||||
| It is readily available | Flower | 1122 (49.28%) | 582 (25.56%) | 167 (7.33%) | 147 (6.46%) | 259 (11.37%) | 2.05 | −0.036, 0.073 | .450 (.010) |
| Concentrate | 1176 (51.65%) | 527 (23.14%) | 161 (7.07%) | 150 (6.59%) | 263 (11.55%) | 2.03 | |||
Significant differences at p ≤ .05 are noted in bold.
Unless otherwise stated: n=2277.
n=2776.
3.2.2. Severity of Dependence Scale (SDS)
Analyses were performed on data from participants who completed both the SDS and provided information about current patterns of dabbing (n = 1037). Among those with a history of regular dabbing (at least once a month), SDS responses were compared between current (n = 865) and former dab users (n = 172). Results indicated that current users more frequently endorsed being “worried about cannabis use” relative to former users (X2 = 8.149, p = .044). No differences were observed across the remaining questions which assessed thinking that cannabis use was “out of control,” being anxious at the thought of not using cannabis, wishing they could stop cannabis use, and finding it difficult to stop using cannabis. Further, no significant between-group differences were observed for total SDS scores.
Additional analyses examining potential moderating factors for the SDS findings were also completed. While analyses revealed that current and former dab users were well-matched for age, education, income, age of onset of cannabis use, use of alcohol, and use of other substances, the two groups differed with regard to frequency of conventional flower use (X2 = 7.675, p = .022). Specifically, significantly more current dab users reported weekly and daily cannabis use compared to former dab users. However, when conventional flower use was included as a covariate in the analyses, SDS results remained unchanged, although it was a significant contributor to the model (p = .018).
4. Discussion
This national online survey suggests that dab use is common among US cannabis consumers and supports the feasibility of conducting survey studies among individuals who use cannabis-based products. Although the survey required approximately 20 min and provided no remuneration, more than 4000 respondents provided data, suggesting that individuals who identify as cannabis consumers are willing to provide information regarding patterns and motives for use as well as positive and negative outcomes, which is critical for public policy. In addition to current findings, data from several other types of studies suggest that concentrate use is on the rise. Online searches and tweets related to concentrates have increased (Cavazos-Rehg et al., 2016; Zhang et al., 2016), and concentrate sales in legal cannabis markets have increased sharply (Carlini et al., 2017; Smart et al., 2017). Two recent surveys also suggest that concentrate use is growing, both within the US (Daniulaityte et al., 2017) and internationally (Chan et al., 2017).
As states continue to pass legislation for medical and recreational cannabis, concentrates are gaining popularity and individuals appear to be engaging in use for several reasons. Regarding motive, concentrates are considered novel products, so it is not surprising that individuals were significantly more likely to report “curiosity” as a motive for using dabs compared to flower products. Concentrates are also newer products, which likely contributed to an older age of onset of concentrate use (mid 30’s) relative to the age of onset of flower cannabis (18–19 years old). Interestingly, users indicated that they were more motivated to use flower than dabs for reasons including enjoying the effects, coping, celebrating a special occasion, relieving social anxiety, alleviating sleeping difficulties, and perceived low risk. This suggests that respondents were more motivated to use flower products to achieve positive effects, especially important in light of previous research which reported that concentrate use is related to stronger negative effects and weaker positive effects relative to high-potency flower (Chan et al., 2017). Taken together, data may indicate that users tend to seek out dabs for new experiences but may not experience positive effects to the same extent they do with flower products, raising questions as to why users continue to use dabs if they derive greater pleasure or relief of negative symptoms with conventional flower products. It is possible that individuals initially seek out dabs for new experiences but continue using them for other reasons. Previous studies note that dab use is related to self-reported increases intolerance and withdrawal symptoms (Loflin and Earleywine, 2014), and in the current study, regular dab users endorsed being more worried about their cannabis use compared to those who had only tried concentrates. Notably, current dab users also reported a higher frequency of cannabis use overall, which significantly contributed to higher SDS scores; however, when flower use was controlled for, SDS results remained unchanged, suggesting that dab use is related to increased worry about cannabis use. Additional insight regarding why dab users initiate and maintain use is critical in order to better understand risk factors and consequences associated with use.
Regardless of motive, concentrate use appears to be prevalent and increasingly popular. Interestingly, over 26% of all survey respondents identified as regular (at least monthly) concentrate users, and more than one-third of these individuals reported use multiple times per day. Although the amount of money spent on concentrates varied widely, it is likely that some individuals make their products, spending less money, while those buying from friends or a dispensary may spend more. Interestingly, motives to use dabs did not appear to be influenced by availability, which may indicate that concentrates are as readily available as flower products to many consumers, yet the more frequent use of dabs was noted in states with recreational cannabis laws, perhaps suggesting that social norms and “cannabis culture” influence dab use.
High rates of regular dab use raise potential concern given previous data reporting an association between higher THC levels and decrements in cognitive performance (Kowal et al., 2015; Ramaekers et al., 2006) as well as altered brain structure (Rigucci et al., 2016). It remains unclear, however, whether the use of dabs and other concentrate products will have a more deleterious effect on these measures relative to flower products, especially as the potency of flower products has continued to rise over the past several decades. Further, it is likely that specific product selection (e.g., shatter, wax, oil), mode of use (e.g., dabbing, vaping) and frequency/magnitude of use will significantly impact outcomes, as these variables affect THC exposure. While some suggest that individuals who use higher potency cannabis products may titrate their use accordingly and use less to get the desired effect (Freeman et al., 2014; van der Pol et al., 2014), others posit that users may not regulate their intake as a function of THC content (Chait, 1989). Moreover, it is unclear if the use of higher potency products confers additional risk or vulnerabilities for decrements previously noted in recreational users, especially among younger consumers.
To date, no studies have directly assessed individuals who predominantly use dabs or concentrates compared to those who use conventional flower products. Specifically, the neurocognitive consequences of concentrate use remain unknown, an important area for future studies. Interestingly, Daniulaityte et al. (2017) recently noted that the most common “health-related” risk reported by daily dab users was “poor memory,” underscoring the importance of directly assessing the effects of concentrate use on cognitive and clinical domains. Future studies should also examine safety with regard to accidents related to making concentrate products and those related to high levels of intoxication often associated with concentrate use.
Although this survey generated critical information about dab use across the US, several limitations must be considered. First, non-probability sampling was used to gather data from respondents, which limits generalizability, as the study sample is inherently limited to only those targeted through social media who were willing to spend time answering questions for approximately 20-min about their substance use without any financial incentives. However, given that this survey collected information about drug use which remains illegal at the Federal level, self-selection methods were utilized in order to maximize honest reporting. Further, self-selection and promotion allowed the survey to reach more individuals. This survey also collected data on the amount of money spent on concentrate products. Given differences in US state markets and cost-of-living expenses, and since many make products for themselves and others, this metric may be influenced by additional factors. For this reason, information regarding frequency and amount consumed was also collected as a more objective measure of concentrate use. However, some respondents may have included the amount they make for others when asked, “What quantity of concentrates are you buying or making each month?” Finally, as the survey specifically targeted cannabis concentrate users, frequency of use reported by the current sample may not reflect national use rates and may, therefore, overestimate concentrate use among the general population. Nonetheless, this survey provides key information about rates of use within a targeted and growing population of cannabis consumers.
5. Conclusions
Despite the growing popularity of concentrates, few have examined the extent of use across the US or consequences related to these highly potent products. This survey provides a critical, preliminary step in understanding the scope of dabbing and motives for use. Current findings suggest that dab users may engage in use because of curiosity/experimentation, but they do not tend to report positive motives for use (enjoyable effects, relief of negative symptoms, etc.) to the same extent as they do with flower products. These data underscore the need for direct assessment of concentrate users in order to clarify the neurocognitive impact of these products as well as psychological effects and issues related to safety.
Acknowledgments
The authors wish to thank Dr. Scott Lukas for his consultation on this project.
Role of funding source
This work was supported private donations, and Dr. Gruber recieved partial salary support from the National Institute on Drug Abuse (NIDA) [grant number R01 DA032646] during completion of this project.
Footnotes
Conflict of interest
No conflict declared.
References
- Bhattacharyya S, Morrison PD, Fusar-Poli P, Martin-Santos R, Borgwardt S, Winton-Brown T, Nosarti C, O’Carroll CM, Seal M, Allen P, Mehta MA, Stone JM, Tunstall N, Giampietro V, Kapur S, Murray RM, Zuardi AW, Crippa JA, Atakan Z, McGuire PK, 2010. Opposite effects of delta-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology 35, 764–774. 10.1038/npp.2009.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlini BH, Garrett SB, Harwick RM, 2017. Beyond joints and brownies: marijuana concentrates in the legal landscape of WA State. Int. J. Drug Policy 42, 26–29. 10.1016/j.drugpo.2017.01.004. [DOI] [PubMed] [Google Scholar]
- Cavazos-Rehg PA, Sowles SJ, Krauss MJ, Agbonavbare V, Grucza R, Bierut L, 2016. A content analysis of tweets about high-potency marijuana. Drug Alcohol Depend 166, 100–108. 10.1016/j.drugalcdep.2016.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chait LD, 1989. Delta-9-tetrahydrocannabinol content and human marijuana self-administration. Psychopharmacology (Berl.) 98, 51–55. [DOI] [PubMed] [Google Scholar]
- Chan GCK, Hall W, Freeman TP, Ferris J, Kelly AB, Winstock A, 2017. User characteristics and effect profile of butane hash oil: an extremely high-potency cannabis concentrate. Drug Alcohol Depend 178, 32–38. 10.1016/j.drugalcdep.2017.04.014. [DOI] [PubMed] [Google Scholar]
- D’Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu YT, Braley G, Gueorguieva R, Krystal JH, 2004. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology 29, 1558–1572. 10.1038/sj.npp.1300496. [DOI] [PubMed] [Google Scholar]
- Daniulaityte R, Nahhas RW, Wijeratne S, Carlson RG, Lamy FR, Martins SS, Boyer EW, Smith GA, Sheth A, 2015. “Time for dabs”: analyzing Twitter data on marijuana concentrates across the U.S. Drug Alcohol Depend 155, 307–311. 10.1016/j.drugalcdep.2015.07.1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daniulaityte R, Lamy FR, Barratt M, Nahhas RW, Martins SS, Boyer EW, Sheth A, Carlson RG, 2017. Characterizing marijuana concentrate users: a web-based survey. Drug Alcohol Depend 178, 399–407. 10.1016/j.drugalcdep.2017.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Forti M, Marconi A, Carra E, Fraietta S, Trotta A, Bonomo M, Bianconi F, Gardner-Sood P, O’Connor J, Russo M, Stilo SA, Marques TR, Mondelli V, Dazzan P, Pariante C, David AS, Gaughran F, Atakan Z, Iyegbe C, Powell J, Morgan C, Lynskey M, Murray RM, 2015. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet Psychiatry 2, 233–238. 10.1016/s2215-0366(14)00117-5. [DOI] [PubMed] [Google Scholar]
- ElSohly MA, Mehmedic Z, Foster S, Gon C, Chandra S, Church JC, 2016. Changes in cannabis potency over the last 2 decades (1995–2014): analysis of current data in the United States. Biol. Psychiatry 79, 613–619. 10.1016/j.biopsych.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman TP, Winstock AR, 2015. Examining the profile of high-potency cannabis and its association with severity of cannabis dependence. Psychol. Med 45, 3181–3189. 10.1017/S0033291715001178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman TP, Morgan CJ, Hindocha C, Schafer G, Das RK, Curran HV, 2014. Just say’ know’: how do cannabinoid concentrations influence users’ estimates of cannabis potency and the amount they roll in joints? Addiction 109, 1686–1694. 10.1111/add.12634. [DOI] [PubMed] [Google Scholar]
- Fusar-Poli P, Crippa JA, Bhattacharyya S, Borgwardt SJ, Allen P, Martin-Santos R, Seal M, Surguladze SA, O’Carrol C, Atakan Z, Zuardi AW, McGuire PK, 2009. Distinct effects of delta-9-tetrahydrocannabinol and cannabidiol on neural activation during emotional processing. Arch. Gen. Psychiatry 66, 95–105. 10.1001/archgenpsychiatry.2008.519. [DOI] [PubMed] [Google Scholar]
- Keller CJ, Chen EC, Brodsky K, Yoon JH, 2016. A case of butane hash oil (marijuana wax)-induced psychosis. Subst. Abus 37, 384–386. 10.1080/08897077.2016.1141153. [DOI] [PubMed] [Google Scholar]
- Kowal MA, Hazekamp A, Colzato LS, van Steenbergen H, van der Wee NJ, Durieux J, Manai M, Hommel B, 2015. Cannabis and creativity: highly potent cannabis impairs divergent thinking in regular cannabis users. Psychopharmacology (Berl.) 232, 1123–1134. 10.1007/s00213-014-3749-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Large M, Nielssen O, 2017. Daily use of high-potency cannabis is associated with an increased risk of admission and more intervention after first-episode psychosis. Evid. Based Ment. Health 20, 58. 10.1136/eb-2017-102630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loflin M, Earleywine M, 2014. A new method of cannabis ingestion: the dangers of dabs? Addict. Behav 39, 1430–1433. 10.1016/j.addbeh.2014.05.013. [DOI] [PubMed] [Google Scholar]
- Meier MH, 2017. Associations between butane hash oil use and cannabis-related problems. Drug Alcohol Depend 179, 25–31. 10.1016/j.drugalcdep.2017.06.015. [DOI] [PubMed] [Google Scholar]
- Pierre JM, Gandal M, Son M, 2016. Cannabis-induced psychosis associated with high potency “wax dabs. Schizophr. Res 172, 211–212. 10.1016/j.schres.2016.01.056. [DOI] [PubMed] [Google Scholar]
- Piontek D, Kraus L, Klempova D, 2008. Short scales to assess cannabis-related problems: a review of psychometric properties. Subst. Abuse Treat. Prev. Policy 3, 25. 10.1186/1747-597X-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raber JC, Elzinga S, Kaplan C, 2015. Understanding dabs: contamination concerns of cannabis concentrates and cannabinoid transfer during the act of dabbing. J. Toxicol. Sci 40, 797–803. 10.2131/jts.40.797. [DOI] [PubMed] [Google Scholar]
- Ramaekers JG, Kauert G, van Ruitenbeek P, Theunissen EL, Schneider E, Moeller MR, 2006. High-potency marijuana impairs executive function and inhibitory motor control. Neuropsychopharmacology 31, 2296–2303. 10.1038/sj.npp.1301068. [DOI] [PubMed] [Google Scholar]
- Rigucci S, Marques TR, Di Forti M, Taylor H, Dell’Acqua F, Mondelli V, Bonaccorso S, Simmons A, David AS, Girardi P, Pariante CM, Murray RM, Dazzan P, 2016. Effect of high-potency cannabis on corpus callosum microstructure. Psychol. Med 46, 841–854. 10.1017/S0033291715002342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons J, Correia CJ, Carey KB, Borsari BE, 1998. Validating a five-factor marijuana motives measure: relations with use, problems, and alcohol motives. J. Couns. Psychol 45, 265–273. 10.1037/0022-0167.45.3.265. [DOI] [Google Scholar]
- Smart R, Caulkins JP, Kilmer B, Davenport S, Midgette G, 2017. Variation in cannabis potency and prices in a newly legal market: evidence from 30 million cannabis sales in Washington state. Addiction 112, 2167–2177. 10.1111/add.13886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stogner JM, Miller BL, 2015. Assessing the dangers of “dabbing”: Mere marijuana or harmful new trend? Pediatrics 136, 1–3. 10.1542/peds.2015-0454. [DOI] [PubMed] [Google Scholar]
- van der Pol P, Liebregts N, Brunt T, van Amsterdam J, de Graaf R, Korf DJ, van den Brink W, van Laar M, 2014. Cross-sectional and prospective relation of cannabis potency, dosing and smoking behaviour with cannabis dependence: an ecological study. Addiction 109, 1101–1109. 10.1111/add.12508. [DOI] [PubMed] [Google Scholar]
- Winton-Brown TT, Allen P, Bhattacharyya S, Borgwardt SJ, Fusar-Poli P, Crippa JA, Seal ML, Martin-Santos R, Ffytche D, Zuardi AW, Atakan Z, McGuire PK, 2011. Modulation of auditory and visual processing by delta-9-tetrahydrocannabinol and cannabidiol: an FMRI study. Neuropsychopharmacology 36, 1340–1348. 10.1038/npp.2011.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Zheng X, Zeng DD, Leischow SJ, 2016. Tracking dabbing using search query surveillance: a case study in the United States. J. Med. Internet Res 18, e252. 10.2196/jmir.5802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuurman L, Ippel AE, Moin E, van Gerven JM, 2009. Biomarkers for the effects of cannabis and THC in healthy volunteers. Br. J. Clin. Pharmacol 67, 5–21. 10.1111/j.1365-2125.2008.03329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


